HORSLEY, 1857-1916
DEJERINE, 1849-1917
VAN GEHUCHTEN, 1861-1914
IN MEMORIAM
Title: Shell-shock and other neuropsychiatric problems
Presented in five hundred and eighty-nine case histories from the war literature, 1914-1918
Author: Elmer Ernest Southard
Release date: May 19, 2016 [eBook #52105]
Language: English
Credits: E-text prepared by Brian Coe and the Online Distributed Proofreading Team (http://www.pgdp.net) from page images generously made available by Internet Archive (https://archive.org)
| Note: | Images of the original pages are available through Internet Archive. See https://archive.org/details/shellshockother00sout |
THE
CASE HISTORY SERIES
CASE HISTORIES IN MEDICINE
BY
Richard C. Cabot, M.D.
Third edition, revised and enlarged
DISEASES OF CHILDREN
BY
John Lovett Morse, M.D.
Third edition, revised and enlarged
Presented in two hundred Case Histories
ONE HUNDRED SURGICAL PROBLEMS
BY
James G. Mumford, M.D.
Second Printing
CASE HISTORIES IN NEUROLOGY
BY
E. W. Taylor, M.D.
Second Printing
CASE HISTORIES IN OBSTETRICS
BY
Robert L. DeNormandie, M.D.
Second Edition
DISEASES OF WOMEN
BY
Charles M. Green, M.D.
Second Edition
Presented in one hundred and seventy-three Case Histories
NEUROSYPHILIS
MODERN SYSTEMATIC DIAGNOSIS AND TREATMENT
Presented in one hundred and thirty-seven Case Histories
BY
E. E. Southard, M.D., Sc.D.
AND
H. C. Solomon, M.D.
Being Monograph Number Two of the Psychopathic Department of the Boston State Hospital, Massachusetts. (Monograph Number One was A Point Scale for Measuring Mental Ability by Robert M. Yerkes, James W. Bridges and Rose S. Hardwick. Published by Warwick and York. Baltimore 1915.)
SHELL SHOCK and other NEUROPSYCHIATRIC PROBLEMS
Printed in five hundred and eighty-nine Case Histories
BY
E. E. Southard, M.D., Sc.D.
Being Monograph Number Three of the Psychopathic Department of the Boston State Hospital, Massachusetts
HORSLEY, 1857-1916
DEJERINE, 1849-1917
VAN GEHUCHTEN, 1861-1914
IN MEMORIAM
PRESENTED IN FIVE HUNDRED AND EIGHTY-NINE
CASE HISTORIES
FROM THE
WAR LITERATURE, 1914-1918
BY
E. E. SOUTHARD, M.D., Sc.D.
Director (1917-1918), U. S. Army Neuropsychiatric Training School (Boston Unit); Late
Major, Chemical Warfare Service, U. S. Army; Bullard Professor of Neuropathology,
Harvard Medical School; Director, Massachusetts State Psychiatric
Institute (of the Massachusetts Commission on Mental Diseases);
Late President, American Medico-Psychological Association
WITH A BIBLIOGRAPHY BY
NORMAN FENTON, S.B., A.M.
Sergeant Medical Corps, U. S. Army (Assistant in Psychology to the Medical Director,
Base Hospital 117 A. E. F.); late interne in Psychology, Psychopathic Department,
Boston State Hospital; Assistant in Reconstruction, National Committee for
Mental Hygiene
AND AN INTRODUCTION BY
CHARLES K. MILLS, M.D., L.L.D.
Emeritus Professor of Neurology, University of Pennsylvania
BY VOTE OF THE TRUSTEES OF THE BOSTON STATE HOSPITAL
MONOGRAPH NUMBER THREE
OF THE
PSYCHOPATHIC DEPARTMENT
BOSTON
W. M. LEONARD, Publisher
1919
COPYRIGHT, 1919, BY
W. M. LEONARD
To
THE NATIONAL COMMITTEE FOR
MENTAL HYGIENE
AND
ITS WORK IN
WAR AND PEACE
This compilation was begun in the preparedness atmosphere of the U. S. Army Neuropsychiatric Training School at Boston, 1917-18. This particular school had to adapt itself to the clinical material of the Psychopathic Hospital. Although war cases early began to drift into the wards (even including some overseas material), it was thought well to supplement the ordinary “acute, curable, and incipient” mental cases of the hospital wards and out-patient service with representative cases from the literature.
As time wore on, this “preparedness” ideal gave place to the ideal of a collection of cases to serve as a source-book for reconstructionists dealing with neuroses and psychoses. Shortage of medical staff and delays incidental to the influenza epidemic held the book back still further, and, as meantime Brown and Williams had served the immediate need with their Neuropsychiatry and the War, it was determined to make the compilation the beginning of a case-history book on the neuropsychiatry of the war, following in part the traditions of various case-books in law and medicine.
With the conclusion of the armistice, there is by no means an end of these problems. Peace-practice in neuropsychiatry is bound to undergo great changes and improvements, if only from the influx into the peace-community of many more trained neuropsychiatrists than were ever before available. This is particularly true in the American community by reason of the many good men specially trained in camp and hospital neuropsychiatry, both at home and in the A. E. F., through the enlightened policy of our army in establishing special divisions of the Surgeon-General’s Office dealing separately with those problems.
Though a book primarily for physicians, some of its material has interest for line-officers, who may see how much “criming” is matter for medical experts, by running through the boxed headings (especially of Sections A and B) and[ii] reading the simulation cases. As Chavigny remarks, “shooting madmen neither restrains crime nor sets a good example.”
But parts of the book look ahead to Reconstruction. Surely occupation-workers, vocationalists, war risk insurance experts, and in fact all reconstructionists, medical and lay, must find much to their advantage in the data of Section D (Treatment and Results). Had time permitted, the whole old story of “Railway Spine”—Shell-shock’s congener—might have been covered in a series of cases from last century’s literature, together with others illustrating the effects of suggestion and psychotherapy; but this must be a post-bellum task.
The compiler, who has personally dictated (and as a rule redictated and twice condensed) all the cases from the originals (or in a few instances, e.g., Russian, from translations), hopes he has not added anything new to the accounts. The cases are drawn from the literature of the belligerents, 1914-1917, English, French, Italian, Russian, and—so far as available here—German and Austrian.
I would call the collection not so much a posey of other men’s flowers as a handful of their seeds. For I have constantly not so much transcribed men’s general conclusions as borrowed their specific fine-print and footnotes. The lure of the 100 per cent has been very strong in many authors; but the test of fine-print, viz., of the actual case-protocols, saves us from premature conclusions, and the plan of the book allows us to confront actualities with actualities. One gets the impression of a dignified debate from the way in which case-histories automatically confront each other, say in Section C (Diagnosis).
Obligations to the books of Babinski and Froment, Eder, Hurst, Mott (Lettsomian Lectures), Roussy and Lhermitte, Elliot Smith and Pear, and others are obvious. Yealland’s book came too late for sampling its miracles, though cases of his in the periodical literature had already been incorporated in my selection.
Some of the cases in Section A, I, had already been abstracted in Neurosyphilis: Modern Systematic Diagnosis and Treatment (Southard and Solomon, 1917).[iii]
What we actually have made is a case-history book in the newly combined fields now collectively termed neuropsychiatry. The more general the good general practitioner of medicine, the more of a neuropsychiatrist! And this is no pious wish or counsel of perfection. Neuropsychiatry, mental hygiene, psychotherapy and somatotherapy—all these will flourish intra-bellum and post-bellum, in days of destruction and in days of reconstruction. And who amongst us, medical or lay, will not have to deal in reconstruction days with cases like some here compiled? A minor blessing of the war will be the incorporation of mental hygiene in general medical practice and in auxiliary fields of applied sociology, e.g., medico-social work.
Subsidies aiding publication are due to the National Committee for Mental Hygiene; the Permanent Charity Foundation (Boston Safe Deposit and Trust Company); Mrs. Zoe D. Underhill of New York; Mr. H. T. White of New York; and Dr. W. N. Bullard of Boston—to all of these the various military recipients of the book will be under obligations, as well as others who would otherwise have had to pay the great majoration de prix due to war times.
Of those great dead contributors to neurology laid (in the Epicrisis) at the feet of the neo-Attila, perhaps only Sir Victor was in a narrow sense the Kaiser’s victim: still, but for the war, they might all remain to us.
By the way, just as I found John Milton had said things that fitted neurosyphilis, so also Dante is observed in the chosen mottoes to have had inklings even of Shell-shock. To the Inferno it was natural to turn for fitting mottoes (Carlyle’s renderings mainly used). The pages might have been strewn with them. A glint of too great optimism might seem to shine—in the pre-Epicrisis motto—from the lance of Achilles with its “sad yet healing gift;” but out of Shell-shock Man may get to know his own mind a little better, how under stress and strain the mind lags, blocks, twists, shrinks, and even splits, but on the whole is afterwards made good again.
E. E. Southard.
Washington,
November, 1918.
The duties of an introducer, whether of a platform speaker to an audience, or of a writer to his anticipated readers, are not always clearly defined. It has been sometimes said that the critic or reviewer may meet with better success if he has not acquainted himself too thoroughly with the contents of the book about which he writes, as in that case he will have a larger opportunity to indulge his imagination, but a critique thus produced may have the disadvantage of possible shortcoming or unfairness. In the case of this volume, however, I have felt it worth while to acquaint myself with its contents, no light task when one is confronted with a thousand pages.
The great war just closing has done much to enlighten us as to the causes, nature, outcome, and treatment of injuries and diseases to which its victims have been subjected. The object of this book is to present both the data and the principles involved in certain neuropsychiatry problems of the war. These are presented in a wealth of detail through an extraordinary series of case records (589 in all) drawn from current medical literature, during the first three years of the conflict. Case reporting is here seen at its best, and the experiences recorded are largely allowed to speak for themselves, although comments are not wanting and are often illuminating.
Many criticisms have been heard on the use of the term Shell-shock as applied to some of the most important psychiatric and neurological problems of the recent war; but that the designation has meaning will be evident if Dr. Southard’s book is not simply skimmed over by the reader, but is studied in its entirety. The symptoms of a very large number, if not the majority, of the cases recorded, had for their initiating influence the psychic[vi] and physical horrors of life among exploding shells. As the author and those from whom he has received his clinical supply not infrequently point out, in many cases it would appear that purely psychic influences have played the chief rôle, but in others physical injuries have not been lacking. Much more than this is true: in many instances the soil was prepared by previous defect, disease, or injury, or to use one of Dr. Southard’s favorite expressions, “weak spots” were present before martial causes became operative.
While the contributions to the medical and surgical history of the war have been somewhat numerous in current medical journals and in monographs, few comprehensive volumes have appeared. The reasons for this are not far to seek. The conflict has been of such magnitude, and the demands on the bodily and mental activity of the medical profession have been so intense and continuous, that time and opportunity for the careful and complete recording of experiences have not been often available; but works are beginning to appear in the languages of all the belligerent countries and these will increase in number and value during the next lustrum and decade, although it may be that some of the most important contributions will come after a decade or more is past. The great work before me is one that will leave its lasting impress, not only upon military but on civil medicine, for the lessons to be drawn from its pages are in large part as applicable to the one as to the other.
Looking backward to our Civil War, one is strongly impressed with the fact that the present volume, one of the earliest works of its kind to appear in book form, deals largely with psychiatry and functional nervous diseases, whereas during and after the American conflict the most important contributions to neurology related to organic disease, especially as illustrated by the work of Weir Mitchell and his collaborators on injuries of nerves. This is the more interesting when it is remembered that Mitchell not very long after the close of the Civil War became the most prominent exponent of functional neurology, from the diagnostic[vii] and therapeutic sides. To him the profession the world over has been indebted for the development of new views as to the nature of neurasthenia and hysteria and new methods for combating these disorders. In this fact is to be found matter for thought. Those who handled best the neuropsychiatric problems of the present war were in large part qualified not merely by a knowledge of psychology and psychiatry, but far more by a thorough training in organic neurology. The problems of psychiatry can be grasped fully only by those who have a fundamental knowledge of the anatomy, physiology, and diseases of the nervous system.
Dr. Southard, preëminently a neuropathologist, is well grounded in organic neurology, and shows at every turn his capabilities for considering the neuroses, psychoses, and insanities from the standpoint of the neurologist. Moreover, he clearly shows training and insight into the problems of non-neurological internal medicine.
The ideal method of training a student for neuropsychiatric work—if one had the opportunity of directing his course from the time of his entry into medicine—would be to see to it, after a good grounding in the fundamental sciences like anatomy, physiology, and chemistry, that medicine and surgery in their broadest phases first received school and hospital attention; that the fields of neurology, pure and applied, were then fully explored; and that psychology and psychiatry received late but thorough consideration. When after America’s entrance into the world war the writer assisted in preparing medical reserve officers for neuropsychiatric service, those men did best both during their postgraduate work and in base hospitals and in the field, who had built from the bottom after the manner indicated.
At the outset of Dr. Southard’s book, for more than two hundred and fifty pages, the author considers under ten subdivisions the acquired diseases and constitutional defects which may predispose the soldier to functional and reflex nervous disease.[viii] Neurosyphilis, on which Dr. Southard and Dr. Solomon have already given us a valuable treatise, the pharmacopsychoses, especially alcoholism, and the somatopsychoses covering fevers like typhoid and paratyphoid, are considered in numerous carefully chosen case reports. The reader needs only to look closely into the case records of the first quarter of the volume to get a knowledge of the affections chiefly predisposing the soldier or civilian to functional and reflex nervous diseases. To those familiar with the medical history of the war it is well known that one of the reasons for the efficiency of the American Expeditionary Force resided in the fact that the preliminary examinations of the recruits received the fullest attention not only from the points of view of acquired and inherited disease, but also from those of special psychiatric and even psychological deficiencies. Our country, however, had for its guidance the experience of nations which were fighting for three years before we entered the arena and in addition had a large surplus of material from which to cull out the weaklings.
Among the predispositional affections considered—besides syphilis, alcohol, and other drug habits, and the somatopsychoses—are the feeble-mindednesses or hypophrenoses, the epilepsies, the psychoses due to focal brain lesions, the presenile and senile disorders, the schizophrenoses including dementia præcox and allied affections, the cyclothymoses like manic depressive insanity, the psychoneuroses, and the psychopathoses. The last two subjects indicated, considered in special chapters, seem to some extent to be receptacles for affections which cannot well be otherwise placed,—hallucinoses, hysteria, neurasthenia, and psychasthenia,—and under the psychopathoses, pathological lying, Bolshevism, delinquencies of various sorts, homosexuality, suicide and self-mutilation, nosophobia, and even claustrophobia with its exemplar who preferred exposure to shell-fire to remaining in a tunnel.
Under the encephalopsychoses are found interesting illustrations of focal lesions and the general effects of infection and[ix] toxemia. Cases of brain abscess, of spinal focal lesions, and meningeal hemorrhage are in evidence, aphasias, monoplegias, Jacksonian spasm, and thalamic disease receiving consideration.
All neurologists know the difficulties in diagnosticating epilepsy in the absence of opportunities to see attacks and to receive the carefully analyzed statement of the observers of the patient. All this and much more is well brought out in the chapter on the epileptoses. Many epileptics found their way into the armies either through the carelessness of examiners or by suppression of the facts on the part of those who desired to serve.
The fact that an imbecile can shoot straight and face fire comes out in one or two places, but this does not seem to prove that a good rifleman is necessarily an all-round good soldier.
A book like Dr. Southard’s could be made of much use in teaching students, especially postgraduates, by having them, when a particular subject like epilepsy or schizophrenia, for instance, is under discussion, use as collateral reading the case reports of this work.
Dr. Southard’s book will prove useful to many workers—to the medical officer whose duty it is to examine recruits for the service or to pass upon and treat them while in service; almost equally to the medical officer in time of peace; to authors of textbooks and treatises and to contributors to neurological and psychiatric journals; to lecturers and clinical demonstrators; to the examiner for the juvenile courts; and to members of the psychopathic, psychiatric, and neurological staffs of our hospitals.
One is not called upon in an introduction to review at length the contents of the volume, but it may prove of value to the reader to dip here and there into the pages of the work to which his attention is being invited.
It will be remembered that fifty years ago and much later, down to the time of Babinski’s active propaganda in favor of the theories of suggestion, counter-suggestion, and persuasion in hysteria, various affections of a vasomotor and thermic type[x] were included in the list of hysterical phenomena. These and some other phenomena sometimes classed as hysterical, Babinski and those who accord with him now find it necessary to sweep entirely from the domain of hysteria, which being produced by suggestion and cured by counter-suggestion or persuasion cannot include symptoms which are beyond the control of the will and intellect of the patient.
According to the new or rather revived pronouncement, these must be due either to definite organic lesion, or to a disorder of reflex origin, connoting the occurrence of changes in the nervous centers as long ago taught by Vulpian and Charcot. In the records of cases and in the discussions thereon this differentiation receives much consideration.
It is held that the paralysis in the reflex cases is more limited, more persistent, and assumes special forms not observable in hysteria. The attitudes in hysterical palsies conform more to the natural positions of the limbs than do those observed in reflex paralysis. Probably the presence of marked amyotrophies in the reflex nervous disorders is the most convincing factor in separating these from pithiatic affections. These atrophies correspond to the arthritic muscular atrophies of Vulpian, Charcot, Gowers, and others, and cannot for a moment be regarded as caused by suggestion or as removable by counter-suggestion or persuasion. They are influenced, discounting the effect of time and natural recuperation, only by methods of treatment designed to improve the peripheral and central nutrition of the patient. Pithiatic atrophies are slight and probably always to be accounted for by disuse or the association of some peripheral neural disorder with the hysteria. Affections of the sudatory and pilatory systems are more definitely pronounced in reflex cases than in those of a strictly hysterical character.
Some of the facts brought forward by Babinski and Froment to demonstrate the differentiation of reflex paralyses from pithiatic disorders of motion are challenged in the records of this volume by others, as for instance, by Dejerine, Roussy, Marie,[xi] and Guillain. Babinski tells us that in pithiatism, properly so designated, the tendon reflexes are not affected. He believes that even in pronounced anesthesia of the lower extremities the plantar reflexes can always be elicited and are not abnormal in exhibition. Dejerine, however, produces cases to illustrate the fact that in marked hysterical anesthesia of the feet plantar responses cannot be produced. I have personally studied cases which lend some strength to either contention. In some of these I was not able to conclude that either the use of the will or the presence of contractions in extension was sufficient to exclude the normal responses.
Differences in muscle tonicity, in mechanical irritability of the muscles, and the presence or absence of fibrotendinous contractions are indications of a separation between the reflex and purely functional cases, as apparently demonstrated in some of the case records. True trophic disorders of the skin, hair, and bones observed in the reflex cases are also said to have no place in the illustrations of pithiatism.
The delver into the case histories of this volume will find numerous instructive combinations of hystero-reflex and organo-hysterical associations which are not to be enumerated in an introduction. The great importance of what all recognize as pathognomonic signs of organic disease—Babinski extensor toe response, persistent foot clonus, reactions of degeneration, marked atrophy, lost tendon jerks, etc.—is, of course, continuously in evidence. Extraordinary associations of hysterical, organic, and reflex disorders with other affections due to direct involvement of bone, muscle, and vessels and with the secondary effects of cicatrization and immobilization are brought out on many pages. In quitting this branch of our subject it might be remarked that considerable changes must be made in our textbook descriptions of nervous diseases in the light of the contributions to the neurology of the present war.
One is reminded in the details of some of the cases of the discussions some decades since on the subject of spinal traumatisms;[xii] of the work of Erichsen which resulted in giving his name and that of “railway spine” to many of the cases now commonly spoken of as traumatic hysteria and traumatic neurasthenia; of the rejoinders of Page and his views regarding spinal traumatisms; and of Oppenheim’s development of the symptom complex of what he prefers to term the traumatic neurosis. One who has taken part in much court work cannot but read these case records with interest, for the neurology of the war as presented in this volume and in numerous monographs which are now appearing, throws much light upon many often mooted medicolegal problems. I recall how many able and honest neurological observers have changed their points of view since the early days of Erichsen’s “railway spine,” a pathological suggestion which is said to have cost the corporations of England an almost fabulous sum during a score of years. I recall also that a certain Court of Appeals in one of our states even felt itself called upon to promulgate an opinion intended to exorcise entirely the plea for damages for alleged injuries if it could be shown that these were due to fright. The data of this book do not put weapons entirely into the hands of the attorney and the expert for either the plaintiff or the defendant.
Some of the French writers on the neurology of the war, as illustrated in the records collected by Dr. Southard, have brought to our attention distinctions which they draw between états commotionnels and états émotionnels—happy terms, and yet not sufficient in their invention or in the explanations which accompany them, fully to satisfy the requirements of the facts presented. These writers seem to think of the commotional states as denoting some real disease or condition of the brain, and yet one which is really curable and reversible. They explicitly tell us, however, that these commotions fall short of being lésionnel. After all, is this not somewhat obscure? Is it not something of a return to the period of “railway spine” when one of the comparisons sometimes made was that the injury suffered by the nervous tissues produced in them a state[xiii] comparable to that of a magnet which had been subjected to a severe blow? At any rate, in commotion thus discussed the nervous structures are supposed to sustain some real injury of a physiochemical character, whereas in the emotional states the neurones are, as Southard puts it, affected somewhat after the manner of normal emotional functioning, except perhaps that they are called upon to deliver an excessive stream of impulses. The latter would be classed among the psychopathic, the former among the physiopathic affections, and yet the distinction between the two is not always quite clear.
In not a few instances of Shell-shock—although these are not numerous, so far as records have been obtained—actual structural lesions have been recorded even in cases in which no direct external injury of a material kind was experienced as a result of the explosion of shells. In others the evidences of external injury were relatively unimportant. Various lesions, in some cases recognizable even by the naked eye, were present. Mott, for example, found not only minute hemorrhages, but in one instance a bulbar extravasation of moderate massiveness, the patient not showing external signs of injury. Cases are also recorded of hematomyelia; others with edematous or necrotic areas in the cord; and still others with lesions of the ependyma or even with splitting of the spinal canal, reminding one of the classical experiments of Duret on cerebral and cerebrospinal traumatisms.
It has been argued that too much stress should not be laid on a few cases of this sort—but are they as few as they seem to be? The fact is that necropsical opportunities are not often afforded. May not such scattered lesions often be present without resulting in death or even in long continued disturbance? There is no essential reason why minute hemorrhages into the brain and spinal cord, and especially into their membranes, may not undergo rapid absorption or even remain unchanged for some time without dire results.
One of the reported cases in which lung splitting occurred from[xiv] severe concussion without external injury is not without interest in this connection, reminding one, as the commentator says, of those cases of severe concussion in which the interior of a building is injured while the exterior escapes. In the same connection also the cited experiments of Mairet and Durante on rabbits are not without instructiveness. As a result of explosives set off close to these animals, pulmonary apoplexy, spinal cord and root hemorrhages, and extravasations, perivascular and ependymal, and into the cortical and bulbar gray were found. Russca obtained direct and contrecoup brain lesions, etc., in a similar way.
Here and there throughout the book will be found references to symptoms and syndromes which will have a particular interest for the reader—soldier’s heart, trench foot, congealed hand, tics, tremors, convulsions, sensory areas variously mapped, and forms of local tetanus, the last being distinctly to be differentiated from pithiatic contractures and those due to organic lesions of the nervous system. Cases of an affection described by Souques as camptocormia, from Greek words meaning to bend the trunk, were shown to the Neurological Society of Paris in 1914 and later, the main features of this affection being pronounced incurvation forward of the trunk from the dorsolumbar region, with extreme abduction and outward rotation of the lower limbs, pain in the back, and difficult and tremulous walking. In some of these cases, organic lesions of the trunkal tissues were present, but in addition psychic elements played a not unimportant part, and the cases were restored to health by a combination of physical measures with psychotherapy, enforced by electrical applications.
The part of this book given over to the discussion of treatment will doubtless to some prove the most interesting section. The presentation of the subject of therapeutics is in some degree a discussion also of diagnosis and prognosis; and so it happens in various parts of the volume that the particular subject under consideration is more or less a reaffirmation or anticipation of remarks under other headings.
Similar results are brought about by various therapeutic procedures. Nonne, Myers, and a few others bring hypnosis into the foreground, although non-hypnotic suggestion plays a larger rôle by far.
Miracle cures are wrought through many pages. Mutism, deafness and blindness, palsies, contractures, and tics disappear at times as if by magic under various forms of suggestion. Ether or chloroform narcosis drives out the malady at the moment when it reveals its true nature. Verbal suggestion has many adjuvants and collaborators—electricity, sometimes severely administered, lumbar puncture, injections of stovaine into the cerebrospinal fluid, injections of saline solution, colored lights, vibrations, active mechanotherapy, hydrotherapy, hot air baths and blasts, massage, etc. Painful and punitive measures have their place—one is inclined to think a less valuable place than is given them by some of the recorders. In some instances the element of suggestion, while doubtless present, is overshadowed by the material methods employed. Persuasion and actual physical improvement are in these cases highly important. Reëducation is not infrequently in evidence. The patient in one way or another is taught how to do things which he had lost the way of doing.
It is interesting to American neurologists to note how frequently in the reports, especially of French observers, the “Weir Mitchell treatment” was the method employed, including isolation, the faradic current, massage, and Swedish movements, hydrotherapy, dietetic measures, reëducative processes, and powerful suggestion variously exhibited, especially through the mastery of the physician over the patient. It is rather striking that few records of Freudian psychoanalytic therapy are presented.
When all is said, however, counter-suggestion and persuasion, in whatever guise made use of, were not always sufficient and this not only in the clearly organic cases, but in those which are ranked under the head of reflex nervous disorders. In these the long-continued use of physical agencies was found necessary to[xvi] supplement the purely psychic procedures, these facts sometimes giving rise in the Paris Society of Neurology and elsewhere to animated discussion as to the real nature of the cases. The pithiatic features of the case at times disappear, but leave behind much to be explained and more to be accomplished. The cures wrought are not always permanent and in some cases post-bellum experiences may be required to prove the real value of the measures advocated. The reader must study well the detailed records in order to arrive at just conclusions; nevertheless, the tremendous efficacy of suggestion and persuasion stands out in many of the recitals.
Perhaps the author may permit the introducer a little liberty of comment. His non-English interpellations, especially Latin and French, may be regarded by some as overdone or perhaps pedantic, but are rather piquant, giving zest to the text. Diagnosis per exclusionem in ordine is sonorous and has a scholarly flavor, but does not prevent the reader who lives beyond the faubourgs of Boston from understanding that the author is speaking of an ancient and well-tried method of differential diagnosis. Passim may be more impressive or thought-fixing than its English translation, but this to the reader will simply prove a matter of individual opinion. Psychopathia martialis is not only mouth-filling like Senegambia or Mesopotamia, but really has a claim to appreciation through its evident applicability. It is agreeable to note that the book seems nowhere to indicate that psychopathia sexualis and psychopathia martialis are convertible terms.
The bibliography of the volume challenges admiration because of its magnitude and thoroughness and is largely to be credited, as the author indicates, to the energy and efficiency of Sergeant Norman Fenton, who did the work in connection with the Neuropsychiatric Training School at Boston, resorting first-hand to the Boston Medical Library and the Library of the New York Academy of Medicine. After Sergeant Fenton joined the American Expeditionary Force, Dr. Southard greatly increased the value of the bibliography by his personal efforts.
This bibliography covers not only the 589 case histories of the book, but it goes beyond this, especially in the presentation of references for 1917, 1918, and even 1919. Owing to the time when our country entered the war, American references are, in the main, of later date than the case histories. They will be found none the less of value to the student of neuropsychiatric problems.
The references in the bibliography number in all more than two thousand, distributed so far as nationalities are concerned about as given below, although some mistakes may have crept into this enumeration for various reasons, like the publication of the same articles in the journals of different countries. The list of references includes French, 895; British (English and Colonial), 396; Italian, 77; Russian, 100; American, 253; Spanish, 5; Dutch, 5; Scandinavian, 5; and Austrian and German, 476. It will be seen, therefore, that the bibliography covers in number nearly four times the collected case studies, most of these records being from reports made during the first three years of the war. The author has wisely made an effort to bring the bibliographic work up to and partially including 1919.
The manner in which the French neurologists and alienists continued their work during the strenuous days of the terrible conflict is worthy of all praise. The labors of the Society of Neurology of Paris never flagged, its contributions in current medical journals having become familiar to neurologists who have followed closely the trend of medical events during the war. Cases and subjects were also frequently presented and discussed at the neurological centers connected with the French and allied armies in France.
It may be almost invidious to specify names, the work done by many was of so much interest and value. Dejerine in the early days of the war, before his untimely sickness and death, contributed his part. Marie from the beginning to the end of the conflict continued to make the neurological world his debtor. The name of Babinski stands out in striking relief. Other[xviii] names frequently appearing among the French contributors are those of Froment, Clovis Vincent, Roussy and Lhermitte, Léri, Guillain, Souques, Laignel-Lavastine, Courbon, Grasset, Claude, Barre, Benisty, Foix, Chavigny, Charpentier, Meige, Thomas, and Sollier.
For a work of this character not only as complete a bibliography as possible, but a thorough index is absolutely necessary, and this has been supplied. The author has not made the index too full, but with enough cross-references to enable those in all lines of medical work interested to cull out the cases and comments which most concern them.
My prologue finished, I step aside for the play and the player, with the recommendation to the reader that he give close heed to the performance—to the recital of the cases, the comments thereon, and the general discussion of subjects—knowing that such attention will be fully rewarded, for in this wonderful collection of Dr. Southard is to be seen an epitome of war neurology not elsewhere to be found.
Charles K. Mills.
Philadelphia, May, 1919.
| SECTION A. PSYCHOSES INCIDENTAL IN THE WAR | |||
| I. The Syphilitic Group (Syphilopsychoses) | |||
| Case | Page | ||
| 1. | Desertion of an officer | Briand, 1915 | 8 |
| 2. | Visions of a naval officer | Carlill, Fildes, Baker, 1917 | 9 |
| 3. | Aggravation of neurosyphilis by war | Weygandt, 1915 | 10 |
| 4. | Same | Hurst, 1917 | 10 |
| 5. | Same | Beaton, 1915 | 10 |
| 6. | Same | Boucherot, 1915 | 11 |
| 7. | Same | Todd, 1917 | 12 |
| 8. | Same | Farrar, 1917 | 13 |
| 9. | Same | Marie, Chatelin, Patrikios, 1917 | 14 |
| 10. | Root-sciatica | Long, 1916 | 15 |
| 11. | Disciplinary | Kastan, 1916 | 17 |
| 12. | Same | Kastan, 1916 | 18 |
| 13. | Same? | Kastan, 1916 | 19 |
| 14. | Hysterical chorea versus neurosyphilis | de Massary, du Sonich, 1917 | 20 |
| 15. | Traumatic general paresis | Hurst, 1917 | 22 |
| 16. | Head trauma; shell-shock; mania; W. R. positive | Babonneix, David, 1917 | 23 |
| 17. | Head trauma in a syphilitic | Babonneix, David, 1917 | 24 |
| 18. | Shell wound: general paresis | Boucherot, 1915 | 25 |
| 19. | “Shell-shock” ocular palsy: syphilitic | Schuster, 1915 | 26 |
| 20. | Shell-shock: general paresis | Donath, 1915 | 27 |
| 21. | Shell-shock: tabes | Logre, 1917 | 28 |
| 22. | Same | Duco, Blum, 1917 | 28 |
| 23. | Pseudotabes (Shell-shock) | Pitres, Marchand, 1916 | 29 |
| 24. | Shell-shock neurosyphilis | Hurst, 1917 | 30 |
| 25. | Shell-shock neurosyphilis | Hurst, 1917 | 31 |
| 26. | Pseudoparesis (Shell-shock) | Pitres, Marchand, 1916 | 32 |
| 27. | War strain and Shell-shock in a syphilitic | Karplus, 1915 | 34 |
| 28. | Shell-shock recurrence of syphilitic hemiplegia | Mairet, Piéron, 1915 | 36 |
| 29. | Shell-shock (functional!) amaurosis in a neurosyphilitic | Laignel-Lavastine, Courbon, 1916 | 37 |
| 30. | Shell-shock (functional) phenomena in a neurosyphilitic | Babonneix, David, 1917 | 39 |
| [xx]31. | Vestibular symptoms in a neurosyphilitic | Guillain, Barré, 1916 | 40 |
| 32. | Syphilophobic suicidal attempts | Colin, Lautier, 1917 | 41 |
| 33. | Simulated chancre | Pick, 1916 | 42 |
| 34. | Exaggeration | Buscaino, Coppola, 1916 | 43 |
| II. The Feeble-minded Group (Hypophrenoses) | |||
| 35. | A feeble-minded person fit for service | Pruvost, 1915 | 44 |
| 36. | An imbecile superbrave | Pruvost, 1915 | 45 |
| 37. | An imbecile fit for barracks work | Pruvost, 1915 | 45 |
| 38. | A feeble-minded inventor | Laignel-Lavastine, Ballet, 1917 | 47 |
| 39. | A feeble-minded simulator | Pruvost, 1915 | 49 |
| 40. | Enlistment for amelioration of character | Briand, 1915 | 49 |
| 41. | An imbecile fit for service at the front | Pruvost, 1915 | 50 |
| 42. | An imbecile with sudden initiative | Lautier, 1915 | 51 |
| 43. | Emotional fugue in subnormal subject | Briand, 1915 | 52 |
| 44. | Regimental surgeon versus alienist re feeble-mindedness | Kastan, 1916 | 53 |
| 45. | An imbecile rifleman | Kastan, 1916 | 55 |
| 46. | An imbecile hypomaniacal | Haury, 1915 | 57 |
| 47. | Feeble-minded desire to remain at the front | Kastan, 1916 | 58 |
| 48. | An imbecile sent back by Germans | Lautier, 1915 | 60 |
| 49. | Unfit for service: feeble-mindedness? | Kastan, 1916 | 61 |
| 50. | Oniric delirium in a feeble-minded subject | Soukhanoff, 1915 | 62 |
| 51. | Shell-shock and burial: situation not rationalized | Duprat, 1917 | 63 |
| 52. | Shell-shock in weak-minded subject; fear, fugues | Pactet, Bonhomme, 1917 | 64 |
| III. The Epileptic Group (Epileptoses) | |||
| 53. | Epilepsy: neurosyphilis | Hewat, 1917 | 65 |
| 54. | Epilepsy brought out by syphilis | Bonhoeffer, 1915 | 66 |
| 55. | Syphilis in a psychopathic subject | Bonhoeffer, 1915 | 67 |
| 56. | Epileptic imbecile court-martialed | Lautier, 1916 | 68 |
| 57. | Psychogenic seizures in feeble-minded subject | Bonhoeffer, 1915 | 69 |
| 58. | Drunken epileptic: responsibility? | Juquelier, 1917 | 71 |
| 59. | Epilepsy: disciplinary case | Pellacani, 1917 | 74 |
| 60. | Same | Pellacani, 1917 | 76 |
| 61. | Desertion: epileptic fugue | Verger, 1916 | 78 |
| 62. | Specialist in escapes | Logre, 1917 | 80 |
| 63. | Epilepsy and other factors: disciplinary case | Consiglio, 1917 | 82 |
| 64. | Strange conduct and amnesia in epileptic | Hurst, 1917 | 83 |
| 65. | Epilepsy after antityphoid inoculation | Bonhoeffer, 1915 | 84 |
| 66. | Shell-shock: Jacksonian seizures—decompression | Leriche, 1915 | 86 |
| 67. | Blow on head: hysterical convulsions—cure by neglect | Clarke, 1916 | 87 |
| 68. | Epilepsy with superposed hysteria | Bonhoeffer, 1915 | 88 |
| 69. | Musculocutaneous neuritis: Brown-Séquard’s epilepsy | Mairet, Piéron, 1916 | 89 |
| [xxi]70. | Bullet wound: reactive epilepsy? | Bonhoeffer, 1915 | 92 |
| 71. | Epilepsia tarda | Bonhoeffer, 1915 | 93 |
| 72. | Convulsions by auto-suggestion | Hurst, 1916 | 95 |
| 73. | Epilepsy, emotional | Westphal, Hübner, 1915 | 97 |
| 74. | Hysterical convulsions | Laignel-Lavastine, Fay, 1917 | 98 |
| 75. | Desertion: fugue, probably not epileptic | Barat, 1914 | 100 |
| 76. | Epileptic episode | Bonhoeffer, 1915 | 102 |
| 77. | Narcoleptic seizures | Friedmann, 1915 | 103 |
| 78. | Sham fits | Hurst, 1917 | 106 |
| 79. | Epileptoid attacks controllable by will | Russel, 1917 | 106 |
| 80. | Epileptic taint brought out at last by shell-shock | Hurst, 1917 | 107 |
| 81. | Shell-shock epilepsia larvata | Juquelier, Quellien, 1917 | 108 |
| 82. | To illustrate a theory of Shell-shock as epileptic | Ballard, 1915 | 110 |
| 83. | Same | Ballard, 1917 | 110 |
| 84. | Same | Ballard, 1917 | 111 |
| 85. | Epileptic equivalents | Mott, 1916 | 112 |
| IV. The Alcohol-Drug-Poison Group (Pharmacopsychoses) | |||
| 86. | Pathological intoxication | Boucherot, 1915 | 113 |
| 87. | Same | Loewy, 1915 | 116 |
| 88. | Desertion in alcoholism: fugue | Logre, 1916 | 117 |
| 89. | Alcoholic amnesia experimentally reproduced | Kastan, 1915 | 118 |
| 90. | Desertion and drunkenness | Kastan, 1915 | 119 |
| 91. | Desertion by alcoholic dement | Kastan, 1915 | 121 |
| 92. | Desertion by alcoholic with other factors | Kastan, 1915 | 124 |
| 93. | Alcoholism: disciplinary case | Kastan, 1915 | 126 |
| 94. | Atrocity, alcoholism | Kastan, 1915 | 127 |
| 95. | Atrocity, alcoholic | Kastan, 1915 | 128 |
| 96. | Alcoholism and amnesia: disciplinary case | Kastan, 1915 | 129 |
| 97. | Post-traumatic intolerance of alcohol | Kastan, 1915 | 130 |
| 98. | Adventure with Parisian stranger | Briand, Haury, 1915 | 131 |
| 99. | Morphinism: tetanus | Briand, 1914 | 131 |
| 100. | Morphinism: medicolegal question | Briand, 1914 | 132 |
| 101. | Two morphinists | Briand, 1914 | 132 |
| 102. | |||
| V. The Focal Brain Lesion Group (Encephalopsychoses) | |||
| 103. | Aphasia and left hemiplegia: local and contrecoup lesions | L’Hermitte, 1916 | 133 |
| 104. | Gunshot head wound and alcohol: amnesia | Kastan, 1916 | 135 |
| 105. | Bullet in brain: cortical blindness and hallucinations | Lereboullet, Mouzon, 1917 | 136 |
| 106. | Content of existent psychosis changed by head trauma | Laignel-Lavastine, Courbon, 1917 | 139 |
| [xxii]107. | Meningococcus meningitis; apparent recovery: dementing psychosis | Maixandeau, 1915 | 141 |
| 108. | Meningococcus meningitis | Eschbach and Lacaze, 1915 | 143 |
| 109. | Shell-shock: meningitic syndrome | Pitres and Marchand, 1916 | 145 |
| 110. | Brain abscess in a syphilitic: matutinal loss of knee-jerks | Dumolard, Rebierre, Quellien, 1915 | 147 |
| 111. | Spinal cord lesion: early recovery | Mendelssohn, 1916 | 149 |
| 112. | Shell explosion and meningeal hemorrhage: pneumococcus meningitis | Guillain, Barré, 1917 | 150 |
| 113. | Ante bellum cortex lesion: shrapnel wound determines athetosis | Batten, 1916 | 151 |
| 114. | Hysterical versus thalamic hemianesthesia | Léri, 1916 | 152 |
| 115. | Shell-shock: multiple sclerosis syndrome | Pitres, Marchand, 1916 | 154 |
| 116. | Mine explosion: hysterical and organic symptoms | Smyly, 1917 | 156 |
| 117. | Same | Smyly, 1917 | 156 |
| VI. The Symptomatic Group (Somatopsychoses) | |||
| 118. | Rabies: neuropsychiatric phenomena | Grenier de Cardenal, Legrand, Benoit, 1917 | 162 |
| 119. | Tetanus, psychotic | Lumière, Astier, 1917 | 164 |
| 120. | Tetanus fruste versus hysteria | Claude, L’Hermitte, 1915 | 165 |
| 121. | British officer’s letter concerning local tetanus | Turrell, 1917 | 166 |
| 122. | Dysentery: psychosis | Loewy, 1915 | 168 |
| 123. | Typhoid fever: hysteria | Sterz, 1914 | 169 |
| 124. | Dementia praecox versus posttyphoid encephalitis | Nordmann, 1916 | 170 |
| 125. | Paratyphoid fever: psychosis outlasting fever | Merklen, 1915 | 171 |
| 126. | Paratyphoid fever: psychopathic taint brought out | Merklen, 1915 | 172 |
| 127. | Diphtheria: post diphtheritic symptoms | Marchand, 1916 | 173 |
| 128. | Diphtheria: hysterical paraparesis | Marchand, 1915 | 174 |
| 129. | Malaria: amnesia | De Brun, 1917 | 175 |
| 130. | Malaria: Korsakow’s syndrome | Carlill, 1917 | 176 |
| 131. | Malaria: ventral horn symptoms | Blin, 1916 | 178 |
| 132. | Trench foot; acroparesthesia | Cottet, 1917 | 180 |
| 133. | Bullet injury of spine; bronchopneumonia: état criblé of spinal cord | Roussy, 1916 | 181 |
| 134. | Shell-shock (shell not seen); sensory and motor symptoms: decubitus; recovery | Heitz, 1915 | 183 |
| 135. | Shell-shock; later typhoid fever: neuritis (ante bellum hysteria) | Roussy, 1915 | 185 |
| 136. | Bullet wound of pleura: hemiplegia and ulnar syndrome | Phocas, Gutmann, 1915 | 186 |
| 137. | Tachypnoea, hysterical | Gaillard, 1915 | 188 |
| 138. | Soldiers’ heart | Parkinson, 1916 | 190 |
| 139. | Soldiers’ heart? | Parkinson, 1916 | 191 |
| 140. | War strain and shell wound: diabetes mellitus | Karplus, 1915 | 192 |
| 141. | Dercum’s disease | Hollande, Marchand, 1917 | 193 |
| [xxiii]142. | Hyperthyroidism | Tombleson, 1917 | 195 |
| 143. | Hyperthyroidism?, neurasthenia | Dejerine, Gascuel, 1914 | 196 |
| 144. | Hyperthyroidism | Rothacker, 1916 | 197 |
| 145. | Graves’ disease, forme fruste | Babonneix, Célos, 1917 | 198 |
| 146. | Shell-shock hysteria: surgical complications | Oppenheim, 1915 | 199 |
| VII. The Presenile and Senile Group (Geriopsychoses)—No cases. | |||
| VIII. The Dementia Praecox Group (Schizophrenoses) | |||
| 147. | Hatred of Prussia: diagnosis, dementia praecox | Bonhoeffer, 1916 | 200 |
| 148. | Dementia praecox: arrest as spy | Kastan, 1915 | 201 |
| 149. | Fugue, catatonic | Boucherot, 1915 | 203 |
| 150. | Desertion: schizophrenic? | Consiglio, 1916 | 204 |
| 151. | Schizophrenia; alcoholism: disciplinary case | Kastan, 1915 | 206 |
| 152. | Schizophrenia aggravated by service | de la Motte, 1915 | 208 |
| 153. | Shot himself in hand: delusions | Rouge, 1915 | 209 |
| 154. | Dementia praecox volunteer | Haury, 1915 | 210 |
| 155. | Hysteria versus catatonia | Bonhoeffer, 1916 | 211 |
| 156. | “Hysteria” actually dementia praecox | Hoven, 1915 | 213 |
| 157. | Hallucinatory and delusional contents influenced by war experiences | Gerver, 1915 | 214 |
| 158. | Iron cross winner, hebephrenic | Bonhoeffer, 1915 | 215 |
| 159. | Occipital trauma; visual hallucinations | Claude, L’Hermitte, 1915 | 217 |
| 160. | Shell-shock: Dementia praecox | Weygandt, 1915 | 219 |
| 161. | Same | Dupuoy, 1915 | 220 |
| 162. | Shell-shock; fatigue; fugue; delusions | Rouge, 1915 | 221 |
| IX. The Manic-Depressive Group (Cyclothymoses) | |||
| 163. | A maniacal volunteer | Boucherot, 1915 | 222 |
| 164. | Fugue, melancholic | Logre, 1917 | 223 |
| 165. | Apples in No-man’s-land | Weygandt, 1914 | 224 |
| 166. | Trench life: depression; hallucinations; arteriosclerosis; age, 38 | Gerver, 1915 | 225 |
| 167. | War stress: manic depressive psychosis | Dumesnil, 1915 | 226 |
| 168. | Predisposition; war stress: melancholia | Dumesnil, 1915 | 227 |
| 169. | Depression; low blood pressure; pituitrin | Green, 1916 | 228 |
| X. The Psychoneurotic Group (Psychoneuroses) | |||
| 170. | Three phases in a psychopath | Laignel-Lavastine, Courbon, 1917 | 229 |
| 171. | Fugue, probably hysterical | Milian, 1915 | 232 |
| 172. | Hysterical Adventist | de la Motte, 1915 | 234 |
| 173. | Fugue, psychoneurotic | Logre, —— | 235 |
| 174. | Shell-shy; war bride pregnant: fugue with amnesia and mutism | Myers, 1916 | 236 |
| [xxiv]175. | A neurasthenic volunteer | E. Smith, 1916 | 237 |
| 176. | War stress: neurasthenia in subject without heredity or soil | Jolly, 1916 | 238 |
| 177. | Arterial hypotension in psychasthenia | Crouzon, 1915 | 239 |
| 178. | War stress: psychasthenia | Eder, 1916 | 240 |
| 179. | Ante bellum attacks: neurasthenia | Binswanger, 1915 | 241 |
| 180. | Antityphoid inoculation: neurasthenia | Consiglio, 1917 | 244 |
| 181. | Neurasthenia (one symptom: sympathy with the enemy) | Steiner, 1915 | 245 |
| XI. The Psychopathic Group (Psychopathoses) | |||
| 182. | Claustrophobia: shells preferred to tunnel | Steiner, 1915 | 246 |
| 183. | Pathological liar | Henderson, 1917 | 247 |
| 184. | Psychopath almost Bolshevik | Hoven, 1917 | 249 |
| 185. | Hysterical mutism: persistent delusional psychosis | Dumesnil, 1915 | 250 |
| 186. | Psychopathic inferiority brought out by the war | Bennati, 1916 | 251 |
| 187. | Psychopathic episodes | Pellacani, 1917 | 252 |
| 188. | Maniacal and hysterical delinquent | Buscaino, Coppola, 1916 | 253 |
| 189. | Psychopathic delinquent | Buscaino, Coppola, 1916 | 254 |
| 190. | Psychopathic excitement | Buscaino, Coppola, 1916 | 255 |
| 191. | Desertion: dromomania | Consiglio, 1917 | 256 |
| 192. | Suppressed homosexuality | R. P. Smith, 1916 | 257 |
| 193. | Psychopathic: at first suicidal, then self-mutilative | MacCurdy, 1917 | 258 |
| 194. | Bombardment: psychasthenia | Laignel-Lavastine, Courbon, 1917 | 259 |
| 195. | Nosophobia | Colin, Lautier, 1917 | 261 |
| 196. | Psychopath: Attacks of disgust and terror | Lattes, Goria, 1915 | 262 |
| SECTION B. SHELL-SHOCK: NATURE AND CAUSES | |||
| 197. | Shell explosion: Autopsy—hemorrhages; vagoaccessorius chromatolysis | Mott, 1917 | 265 |
| 198. | Mine explosion: Autopsy—hemorrhages | Chavigny, 1916 | 270 |
| 199. | Mine explosion: Autopsy—hemorrhages | Roussy, Boisseau, 1916 | 271 |
| 200. | Shell fragment in back: Autopsy—softenings in spinal cord | Claude, L’Hermitte, 1915 | 272 |
| 201. | Shell explosion: Autopsy—lungs burst! | Sencert, 1915 | 274 |
| 202. | Shell explosion: Hemorrhage in spinal canal and bladder | Ravaut, 1915 | 276 |
| 203. | Shell explosion: Hemorrhage and pleocytosis of spinal fluid | Froment, 1915 | 277 |
| 204. | Shell explosion: Pleocytosis of spinal fluid | Guillain, 1915 | 279 |
| 205. | Shell explosion: Pleocytosis of spinal fluid as late as a month after explosion | Souques, Donnet, 1915 | 280 |
| 206. | Burial: Thecal hemorrhage | Leriche, 1915 | 282 |
| 207. | Shell explosion: Hypertensive spinal fluid | Leriche, 1915 | 283 |
| 208. | Bullet wound: Hematomyelia; partial recovery | Mendelssohn, 1916 | 284 |
| 209. | Shell explosion, subject prone: Hematomyelia | Babinski, 1915 | 286 |
| [xxv]210. | Struck by missile: Hysterical paraplegia? Herpes; segmentary symptoms | Elliot, 1914 | 288 |
| 211. | Mine explosion: Head bruises, labyrinth lesions, canities unilateral | Lebar, 1915 | 291 |
| 212. | Shrapnel wounds: Focal canities; hysterical symptoms | Arinstein, 1915 | 292 |
| 213. | Burial: Organic (?) hemiplegia | Marie, Lévy, 1917 | 293 |
| 214. | Shell explosion; no wound: Organic and functional symptoms | Claude, L’Hermitte, 1915 | 294 |
| 215. | Gassing: Organic symptoms | Neiding, 1917 | 296 |
| 216. | Gassing: Mutism, battle dreams | Wiltshire, 1916 | 297 |
| 217. | Shell explosion: Organic deafness; hysterical speech disorder | Binswanger, 1915 | 298 |
| 218. | Distant shell explosion not seen or heard: Tympanic rupture, cerebellar symptoms | Pitres, Marchand, 1916 | 300 |
| 219. | Mine explosion: Organic and functional symptoms | Smyly, 1917 | 302 |
| 220. | Shrapnel skull wound: Differential recovery from functional symptoms | Binswanger, 1917 | 303 |
| 221. | Shell explosion shrapnel wound: Battle memories, scar hyperesthetic | Bennati, 1916 | 305 |
| 222. | Shrapnel wounds, operation: Hysterical facial spasm | Batten, 1917 | 306 |
| 223. | Shell explosion: Tremors and emotional crises | Myers, 1916 | 307 |
| 224. | Shell explosion, comrades killed: Tremors, crises | Meige, 1916 | 308 |
| 225. | Under fire: Tremophobia: French artist’s description | Meige, 1916 | 310 |
| 226. | Shell explosion: German soldier’s account of Shell-shock symptoms | Gaupp, 1915 | 312 |
| 227. | A British soldier’s account of shell-shock | Batten, 1916 | 315 |
| 228. | Blown up by shell: Crural monoplegia; hysterical four days later | Léri, 1915 | 317 |
| 229. | Shell explosion nearby: Description of treatment to demonstrate hysterical nature of characteristic symptoms | Binswanger, 1915 | 318 |
| 230. | Leg wound: Pseudocoxalgic monoplegia and anesthesia | Roussy, L’Hermitte, 1917 | 323 |
| 231. | Leg contusion: Crural monoplegia, hysterical; later crutch paralysis, organic | Babinski, 1917 | 324 |
| 232. | War strain: Arthritis; crural monoplegia and anesthesia; hysterical “conversion hysteria” | MacCurdy, 1917 | 325 |
| 233. | Lance thrust in back; Crural monoplegia | Binswanger, 1915 | 326 |
| 234. | Shell explosion: After six days, crural monoplegia (“metatraumatic” suggesting persisting hypersensitive phase after shell-shock) | Schuster, 1916 | 329 |
| 235. | Wound of foot: Acrocontracture, seven months’ duration; psycho-electric cure at one sitting | Roussy, L’Hermitte, 1917 | 330 |
| 236. | Shell explosion: Trauma; emotion; hysterical paraplegia | Abrahams, 1915 | 332 |
| 237. | Shell explosion: Burial; paraplegia | Elliot, 1914 | 334 |
| 238. | Shell explosion: Paraplegia and sensory symptoms, organic? | Hurst, 1915 | 335 |
| [xxvi]239. | War strain and rheumatism; no emotional factors: Paraplegia, later brachial tremor | Binswanger, 1915 | 336 |
| 240. | Emotion in fever patient from watching barrage creep up: Paraplegia | Mann, 1915 | 338 |
| 241. | Incentives, domestic and medical, to paraplegia | Russel, 1917 | 338 |
| 242. | Bullet in back: Hysterical bent back; “camptocormia” | Souques, 1915 | 339 |
| 243. | Shell explosion: Camptocormia | Roussy, L’Hermitte, 1917 | 340 |
| 244. | Shell explosion; burial: camptocormia | Roussy, L’Hermitte, 1917 | 342 |
| 245. | Shell explosion; burial; Paraplegia, later camptocormia | Joltrain, 1917 | 344 |
| 246. | Bullet in thigh: Astasia-abasia. Wound of neck: Again astasia-abasia | Roussy, L’Hermitte, 1917 | 346 |
| 247. | Shell explosion: Wound of thorax; astasia-abasia | Roussy, L’Hermitte, 1917 | 346 |
| 248. | War strain and fall in trench without trauma: Dysbasia | Nonne, 1915 | 347 |
| 249. | Shell explosion: Partial burial; hysterical symptoms in parts buried | Arinstein, 1916 | 349 |
| 250. | Wound of hand: Acroparalysis | Roussy, L’Hermitte, 1917 | 350 |
| 251. | Wound of arm: Hysterical paralysis | Chartier, 1915 | 351 |
| 252. | Wound in brachial plexus region: Supinator longus contracture | Léri, Roger, 1915 | 353 |
| 253. | Contusion of muscle with “stupefactive” paralysis of biceps (supinator longus still functioning) | Tinel, 1917 | 355 |
| 254. | Wound of arm: Blockage of impulses to hand movements | Tubby, 1915 | 356 |
| 255. | Shell explosion: Bilateral symmetrical phenomena | Gerver, 1915 | 357 |
| 256. | Shell explosion: Paralytic symptoms on side exposed: Contralateral irritative symptoms | Oppenheim, 1915 | 359 |
| 257. | Shell explosion: Bilateral asymmetrical symptoms | Gerver, 1915 | 360 |
| 258. | Shell explosion: Sensory disorder on side exposed | Gerver, 1915 | 362 |
| 259. | Shell explosion: Hysterical deafness and other symptoms; relapse | Gaupp, 1915 | 363 |
| 260. | Shell explosion: Deafness | Marriage, 1917 | 365 |
| 261. | Mine explosion: Deafmutism; recovery on epistaxis and fever | Liébault, 1916 | 366 |
| 262. | Shell explosion: Deafmutism | Mott, 1916 | 367 |
| 263. | Shell explosion: Deafmutism and convulsions | Myers, 1916 | 368 |
| 264. | Gunfire: Aphonia | Blässig, 1915 | 370 |
| 265. | Shell-shock mutism: (a), observed, (b) dreamed of, (c), developed by victim of shell explosion | Mann, 1915 | 370 |
| 266. | Mortar explosion: Deafness | Lattes, Goria, 1917 | 371 |
| 267. | Shell-explosion: onomatopœic noises | Ballet, 1914 | 371 |
| 268. | Shell explosion: Gravel in eyes; eye and face symptoms | Ginestous, 1916 | 372 |
| 269. | Shell explosion; burial; blow on occiput; Blindness | Greenlees, 1916 | 373 |
| 270. | Shell-shock amblyopia: Composite data | Parsons, 1915 | 374 |
| 271. | Factors in shell-shock amblyopia: Excitement, blinding flashes, fear, disgust, fatigue | Pemberton, 1915 | 375 |
| [xxvii]272. | Shell explosion amblyopia | Myers, 1915 | 376 |
| 273. | Shell windage without explosion: Cranial nerve disorder | Pachantoni, 1917 | 378 |
| 274. | Initial case in Babinski’s series to show chloroform elective exaggeration of reflexes | Babinski, Froment, 1917 | 380 |
| 275. | Wound of ankle: Contracture, chloroform effect | Babinski, Froment, 1917 | 383 |
| 276. | “Reflex” disorder of right leg: Chloroform effect | Babinski, Froment, 1917 | 384 |
| 277. | Bullet in calf: Hysterical lameness cured—reflex disorder associated therewith not cured | Vincent, 1916 | 385 |
| 278. | Trauma of foot: Hysterical dysbasia and reflex disorders; differential disappearance of hysterical symptoms | Vincent, 1917 | 386 |
| 279. | Shell-shock and paraplegia: Vasomotor and secretory disorder twenty months later | Roussy, 1917 | 387 |
| 280. | Tetanus clinically cured: Phenomena reproduced under chloroform anesthesia | Monier-Vinard, 1917 | 388 |
| 281. | Example of a “reflex” disorder after shell explosion at great distance | Ferrand, 1917 | 390 |
| 282. | Shell fire: Shell-shock symptoms delayed | McWalter, 1916 | 391 |
| 283. | Shell-shock symptoms early and late | Smyly, 1917 | 392 |
| 284. | Wounds: Gassing; burial; collapse on home leave | Elliot Smith, 1916 | 393 |
| 285. | Late sympathetic nerve effect after bullet wound of neck | Tubby, 1915 | 394 |
| 286. | Hysterical crural monoplegia after fall from horse under fire (reminiscence of similar ante bellum accident) | Forsyth, 1915 | 395 |
| 287. | Shell explosion, cave-in: Right leg symptoms (ante bellum experiences) | Myers, 1916 | 396 |
| 288. | Shell explosion, wound of back: Paraparesis (subject always weak in legs) | Dejerine, 1915 | 397 |
| 289. | Wound near heart: Fear; paraparesis (subject always weak in legs) | Dejerine, 1915 | 399 |
| 290. | Wounds: Tic on walking and recovery except frontalis tic (emphasis of ante bellum habit) | Westphal, Hübner, 1915 | 401 |
| 291. | Fatigue and emotion: Hysterical hemiplegia (similar hemiplegia ante bellum) | Roussy, L’Hermitte, 1917 | 402 |
| 292. | War strain: Hemiplegia (similar hemiplegia ante bellum, subject’s father hemiplegic) | Duprés, Rist, 1914 | 403 |
| 293. | Shell explosion and burial: Deafmutism (speech difficulty ante bellum) | MacCurdy, 1917 | 405 |
| 294. | War strain: Shell-shock and psychotic symptoms determined to parts ante bellum | Zanger, 1915 | 406 |
| 295. | Mine explosion: Emotion; delirium (previous head trauma without unconsciousness) | Lattes, Goria, 1917 | 407 |
| 296. | Sniper stricken blind in shooting eye | Eder, 1916 | 408 |
| [xxviii]297. | Anticipation of warfare: Fall while mounting sentry; hysterical blindness | Forsyth, 1915 | 408 |
| 298. | Spasmodic neurosis from bareback riding (similar episode ante bellum) | Schuster, 1914 | 409 |
| 299. | Ante bellum spasm of hands | Hewat, 1917 | 409 |
| 300. | Quarrel: Hysterical chorea, reminiscent of former attack and itself reminiscent of organic chorea in subject’s mother | Dupuoy, 1915 | 411 |
| 301. | Hallucinations and delusions of ante bellum origin: Treatment by explanation | Rows, 1916 | 412 |
| 302. | Tremors and convulsive crises in a poor risk | Rogues de Fursac, 1915 | 413 |
| 303. | Emotionality and tachycardia in a martial misfit | Bennati, 1916 | 415 |
| 304. | Hereditary instability | Wolfsohn, 1918 | 416 |
| 305. | Genealogical tree of a shoemaker | Wolfsohn, 1918 | 417 |
| 306. | Traumatic hysteria without hereditary or acquired psychopathic tendency | Donath, 1915 | 418 |
| 307. | Mine explosion, burial: Neurosis in perfectly normal soldier | MacCurdy, 1917 | 419 |
| 308. | Shell explosion: Tremophobia | Meige, 1916 | 421 |
| 309. | Frozen in bog: Glossolabial hemispasm | Binswanger, 1915 | 424 |
| 310. | Bruise by horse: Invincible pain—subject cured by performing heroic feat | Loewy, 1915 | 426 |
| 311. | Kick by horse: Hysterical symptoms including monocular diplopia | Oppenheim, 1915 | 427 |
| 312. | Windage from non-exploding shell: Emotion; homonymous hemianopsia | Steiner, 1915 | 428 |
| 313. | Shell-shock psoriasis | Gaucher, Klein, 1916 | 429 |
| 314. | Croix de guerre and Shell-shock got simultaneously: Hallucinatory bell-ringing reminiscent of civilian work | Laignel-Lavastine, Courbon, 1916 | 430 |
| 315. | Waked by shell explosion: Nystagmiform tremor (occupational reminiscence in cinema worker) and tachycardia | Tinel, 1915 | 432 |
| 316. | Synesthesialgia: Foot pain on rubbing dry hands | Lortat-Jacob, Sézary, 1915 | 433 |
| 317. | Shell-shock and burial: Clonic spasms, later stupor | Gaupp, 1915 | 435 |
| 318. | War stress (liquid fire) and shell-shock: Puerilism | Charon, Halberstadt, 1916 | 437 |
| 319. | Bombed from aeroplane: Battle dreams; dizziness; fugue | Lattes, Goria, 1917 | 439 |
| 320. | Hyperthyroidism after box drops from aeroplane | Bennati, 1916 | 440 |
| 321. | Shell dropped without bursting: Stupor and delirium | Lattes, Goria, 1917 | 441 |
| 322. | Subject carrying explosives is jostled: Unconsciousness, deafmutism, later camptocormia | Lattes, Goria, 1917 | 443 |
| 323. | Grazed by sliding cannon: Stupor and amnesia | Lattes, Goria, 1917 | 444 |
| 324. | Shell explosions nearby: Emotion and insomnia | Wiltshire, 1916 | 445 |
| [xxix]325. | Shell explosion: symptoms after hearing artillery twelve days later | Wiltshire, 1916 | 446 |
| 326. | Exhaustion (heat?): Hyperthyroidism, hemiplegia | Oppenheim, 1915 | 447 |
| 327. | War strain and rheumatism: tremors | Binswanger, 1915 | 448 |
| 328. | Shell explosion; emotion: Fear and dreams | Mott, 1916 | 451 |
| 329. | Under fire; barbed wire work: tremors and sensory symptoms | Myers, 1916 | 452 |
| 330. | Shell explosion: Emotional crises; twice recurrent mutism | Mairet, Piéron, Bouzansky, 1915 | 453 |
| 331. | Shell explosion: Emotional crises (fright at a frog) | Claude, Dide, Lejonne, 1916 | 455 |
| 332. | War strain; wound; burials; shell-shock: neurosis with anxiety and dreams: Relapse | MacCurdy, 1917 | 457 |
| 333. | Bombed by airplane: Suicidal thoughts; oniric delirium; “moving picture in the head” | Hoven, 1917 | 460 |
| 334. | Shell explosion; emotion at death of best friend: Stupor and amnesia | Gaupp, 1915 | 462 |
| 335. | Emotional shock from shooting comrade: Horror, sweat, stammer, nightmare | Rows, 1916 | 463 |
| 336. | Emotion at death of comrade: Phobias | Bennati, 1916 | 464 |
| 337. | Shell explosion: Fright; delayed loss of consciousness | Wiltshire, 1916 | 465 |
| 338. | Shell explosion; burial work: amnesia; unpleasant ideas reflexly conditioned by shell whistling | Wiltshire, 1916 | 467 |
| 339. | Comrade’s death witnessed: Suicidal depression | Steiner, 1915 | 468 |
| 340. | Marching and battles: Neurasthenia? | Bonhoeffer, 1915 | 469 |
| 341. | English schoolmaster’s account of dreams | Mott, 1918 | 470 |
| 342. | War dreams shifting to sex dreams | Rows, 1916 | 472 |
| 343. | Shock at death of comrade: War and peace dreams | Rows, 1916 | 474 |
| 344. | War dreams including hunger and thirst | Mott, 1918 | 475 |
| 345. | Burial work: Olfactory dreams and vomiting | Wiltshire, 1916 | 476 |
| 346. | War dreams: Phobia conditioned on postoniric suggestion | Duprat, 1917 | 477 |
| 347. | Service in rear: War dreams not based on actual experiences | Gerver, 1915 | 478 |
| 348. | Hysterical astasia-abasia: Heterosuggestive “big belly” | Roussy, Boisseau, Cornil, 1917 | 479 |
| 349. | Collapse going over the top: Neurasthenia | Jolly, 1916 | 481 |
| 350. | Battles: Mania and confusion | Gerver, 1915 | 483 |
| 351. | Machine-gun battle: Mania and hallucinations | Gerver, 1915 | 484 |
| 352. | Attacks and counter-attacks: Incoherence and quick development of scenic war hallucinations | Gerver, 1915 | 485 |
| 353. | Hysterical stupor under shell fire after 2 days in the trenches | Gaupp, 1915 | 486 |
| 354. | Monosymptomatic amnesia | Mallet, 1917 | 488 |
| 355. | Aviator shot down: Mental symptoms, organic | MacCurdy, 1917 | 489 |
| 356. | Shell fire and corpse work: Daze with relapse; mutism | Mann, 1915 | 491 |
| [xxx]357. | Mine explosion: Confusion | Wiltshire, 1916 | 492 |
| 358. | Shell explosion: Alternation of personality | Gaupp, 1915 | 493 |
| 359. | “A Horse in the Unconscious” | Eder, 1916 | 497 |
| 360. | Shell explosion, gassing, fatigue: Anesthesia | Myers, 1916 | 498 |
| 361. | Shell explosion and burial: Somnambulism; dissolution of amnesia under hypnosis | Myers, 1915 | 499 |
| 362. | Shell explosion with injuries: Somnambulism | Donath, 1915 | 502 |
| 363. | Shock: Stupor as if dead | Régis, 1915 | 503 |
| 364. | Emotions over battle scenes: Twenty-four days’ somnambulism | Milian, 1915 | 504 |
| 365. | Putative loss of brother in battle: Somnambulism and mutism twenty-seven days | Milian, 1915 | 506 |
| 366. | Shell explosion: Trauma, windage: Somnambulism four days | Milian, 1915 | 508 |
| 367. | Burial, head trauma; gassing: Tremors, convulsions, confusion, fugue | Consiglio, 1916 | 509 |
| 368. | Shell explosion: Hysterical symptoms and tendency to fugue | Binswanger, 1915 | 510 |
| 369. | Burial: Dissociation of personality | Feiling, 1915 | 512 |
| 370. | Ear Complications and hysteria | Buscaino, Coppola, 1916 | 516 |
| SECTION C. SHELL-SHOCK DIAGNOSIS | |||
| 371. | Value of lumbar puncture | Souques, Donnet, 1915 | 524 |
| 372. | Meningeal and intraspinal hemorrhage: Lumbar puncture | Guillain, 1915 | 525 |
| 373. | Burial: Slight hyperalbuminosis | Ravaut, 1915 | 526 |
| 374. | Paraplegia, organic: Lumbar puncture | Joubert, 1915 | 527 |
| 375. | Gunshot of spine: Spinal concussion, quadriplegia, cerebellospasmodic disorder | Claude, L’Hermitte, 1917 | 528 |
| 376. | Trauma of spine: Anesthesia and contracture, homolateral, with trauma | Oppenheim, 1915 | 529 |
| 377. | Mine explosion combining hysterical and lesional effects | Dupouy, 1915 | 530 |
| 378. | Shell explosion: Hysterical and organic symptoms | Hurst, 1917 | 532 |
| 379. | Gunshot: Cauda equina symptoms, combined with functional paraplegia | Oppenheim, 1915 | 533 |
| 380. | Intraspinal lesion: Persistent anesthesia | Buzzard, 1916 | 534 |
| 381. | Functional shell-shock: Erroneous diagnosis | Buzzard, 1916 | 534 |
| 382. | Retention of urine after shell-shock | Guillain, Barré, 1917 | 535 |
| 383. | Same | Guillain, Barré, 1917 | 536 |
| 384. | Incontinence of urine after shell-shock and burial | Guillain, Barré, 1917 | 536 |
| 385. | Struck by missile: Crural monoplegia; plantar reflex absent | Paulian, 1915 | 537 |
| 386. | Shell explosion: Crural monoplegia; sciatica (neuritis?) | Souques, 1915 | 538 |
| 387. | Functional paraplegia and internal popliteal neuritis | Roussy, 1915 | 540 |
| [xxxi]388. | Bullet in hip: Local “stupor” of leg | Sebileau, 1914 | 542 |
| 389. | Localized catalepsy: Hysterotraumatic | Sollier, 1917 | 544 |
| 390. | Contracture: Hysterotraumatic | Sollier, 1917 | 545 |
| 391. | Crural monoplegia, tetanic: Recovery | Routier, 1915 | 546 |
| 392. | Spasms, contracture, crises—tetanic | Mériel, 1916 | 548 |
| 393. | Shell explosion, windage, flaccid paraplegia, not “spinal contusion” | Léri, 1915 | 550 |
| 394. | Scalp wound: Quadriparesis; paraplegia, cataleptic rigidity of anesthetic legs | Clarke, 1916 | 551 |
| 395. | Shell explosion: Spasmodic contractions of sartorii, persistent in sleep | Myers, 1916 | 553 |
| 396. | Shell explosion: Brown-Séquard’s syndrome, hematomyelic? | Ballet, 1915 | 555 |
| 397. | Question of structural injury of spinal cord | Smyly, 1917 | 557 |
| 398. | Dysbasia, psychogenic round an organic nucleus (cerebellar?) | Cassirer, 1916 | 557 |
| 399. | Shell explosion: Dysbasia, in part hysterical, in part organic? | Hurst, 1915 | 558 |
| 400. | Peculiar walking tic | Chavigny, 1917 | 559 |
| 401. | Mine explosion: Camptocormia. Hospital rounder twenty months—cure by electrotherapy, 1 hour | Marie, Meige, Béhagne, Souques, Megevand, 1917 | 561 |
| 402. | Astasia-abasia | Guillain, Barré, 1916 | 563 |
| 403. | Shell wounds: Abdominothoracic contracture, tetanic, four months after injury | Marie, 1916 | 564 |
| 404. | Shoulder dislocation: Hysterical paralysis of arm | Walther, 1914 | 566 |
| 405. | Gunshot: Paralysis of arm increasing in degree | Oppenheim, 1915 | 567 |
| 406. | Wound of wrist: Differential glove anesthesias | Römner, 1915 | 568 |
| 407. | Hysterical contracture combined with edema and vasomotor disorder | Ballet, 1915 | 569 |
| 408. | Hemiparesis with syringomyelic dissociation of sensations: Hematomyelia? | Ravaut, 1915 | 570 |
| 409. | Brachial monoplegia: Tetanic | Routier, 1915 | 571 |
| 410. | Paralysis of right leg: Hysterical? Organic? “Microörganic”? | Von Sarbo, 1915 | 572 |
| 411. | Shell explosion: Burial: Paralysis on third day | Léri, Froment, Mahar, 1915 | 573 |
| 412. | Shell explosion: Hemiplegia. Plantar areflexia | Dejerine, 1915 | 575 |
| 413. | Shell explosion: Tic versus spasm | Meige, 1916 | 577 |
| 414. | Shell explosion: Tremors, anæsthesias | Mott, 1916 | 580 |
| 415. | Hysteria, appendix to trauma | MacCurdy, 1917 | 582 |
| 416. | Peripheral nerve injury: Neurasthenic hyperalgesia | Weygandt, 1915 | 583 |
| 417. | Soldier lead worker: Peripheral neuritis | Shufflebotham, 1915 | 584 |
| 418. | “Peripheral neuritis” cured by faradism | Cargill, 1916 | 585 |
| 419. | Late tetanus | Bouquet, 1916 | 586 |
| [xxxii]420. | Spasmodic neurosis and neurasthenia | Oppenheim, 1915 | 588 |
| 421. | Hysterical and reflex (“physiopathic”) disorders | Babinski, 1916 | 590 |
| 422. | Bullet wound: Paralysis non-“organic,” non-hysterical, i.e. reflex | Babinski, Froment, 1917 | 592 |
| 423. | Asymmetry of reflexes under chloroform | Babinski, Froment, 1917 | 594 |
| 424. | Reflexes under chloroform | Babinski, Froment, 1915 | 595 |
| 425. | Same | Babinski, Froment, 1915 | 596 |
| 426. | Shrapnel wound: Monoplegia, hysterical and organic | Babinski, Froment, 1917 | 597 |
| 427. | Gunshot, later Erb’s palsy: “reflex”? | Oppenheim, 1915 | 598 |
| 428. | Paralysis hysterical? Organic? | Gougerot, Charpentier, 1916 | 600 |
| 429. | Same | Gougerot, Charpentier, 1916 | 602 |
| 430. | Same | Gougerot, Charpentier, 1916 | 604 |
| 431. | Reflex “paralysis” | Delherm, 1916 | 606 |
| 432. | |||
| 433. | Shell explosion: Functional blindness, monosymptomatic | Crouzon, 1915 | 609 |
| 434. | Retrobulbar neuritis (nitrophenol) | Sollier, Jousset, 1917 | 611 |
| 435. | Eye symptoms, hysterical | Westphal, 1915 | 613 |
| 436. | Sandbag on head: Eye symptoms: Lenses | Harwood, 1916 | 615 |
| 437. | Hemianopsia, organic or functional? | Steiner, 1915 | 616 |
| 438. | Hysterical pseudoptosis | Laignel-Lavastine, Ballet, 1916 | 617 |
| 439. | Shell explosion: Rombergism | Beck, 1915 | 620 |
| 440. | Case for otologists and neurologists | Roussy, Boisseau, 1917 | 622 |
| 441. | Jacksonian syndrome: Hysterical | Jeanselme, Huet, 1915 | 625 |
| 442. | Leg tic: Phobia against crabs | Duprat, 1917 | 627 |
| 443. | Convulsions reminiscent of fright | Duprat, 1917 | 628 |
| 444. | Fatigue, delusions, fugue | Mallet, 1917 | 629 |
| 445. | Obsessions and fugue | Mallet, 1917 | 631 |
| 446. | Aprosexia and birdlike movements | Chavigny, 1915 | 632 |
| 447. | Shell explosion: Unconsciousness (45 days): Mutism | Liébault, 1916 | 633 |
| 448. | Shell explosion: Recurrent amnesia | Mairet, Piéron, 1917 | 634 |
| 449. | Shell explosion: Comrade killed: Amnesia | Gaupp, 1915 | 635 |
| 450. | Shell explosion: Recurrent amnesia | Mairet, Piéron, 1915 | 636 |
| 451. | Soldiers’ heart, neurotic and organic | MacCurdy, 1917 | 639 |
| 452. | Soldiers’ heart, neurotic | MacCurdy, 1917 | 640 |
| 453. | Shell explosion: Hysteria: Malingering (?) | Myers, 1916 | 642 |
| 454. | Officer who could not kick | Mills, 1917 | 644 |
| 455. | “Simulation”: Diagnosis incorrect | Voss, 1916 | 645 |
| 456. | Wound: Hysterical edema? | Lebar, 1915 | 646 |
| 457. | Head trauma: simulation? Hysteria? Surgical? | Voss, 1916 | 648 |
| 458. | Disease and disorder to avoid service | Collie, 1916 | 649 |
| 459. | Yes-No test in anesthesia | Mills, 1917 | 651 |
| 460. | Guardhouse test | Roussy, 1915 | 651 |
| 461. | Light in a dark room | Briand, Kalt, 1917 | 652 |
| [xxxiii]462. | Mutism simulated | Sicard, 1915 | 654 |
| 463. | Deafmutism simulated | Myers, 1916 | 655 |
| 464. | Same: Explained by patient | Myers, 1916 | 657 |
| 465. | Deafmutism: Appearance of malingering | Gradenigo, 1917 | 658 |
| 466. | A lame rascal | Gilles, 1917 | 659 |
| 467. | Picric acid jaundice | Briand, Haury, 1916 | 660 |
| 468. | Swelling of hand and arm, 7 months | Léri, Roger, 1915 | 663 |
| 469. | Shell-shy German | Gaupp, 1915 | 664 |
| 470. | Germany sends back a simulator | Marie, 1915 | 664 |
| 471. | Simulation of Quincke’s disease | Lewitus, 1915 | 665 |
| 472. | “Pensionitis” | Collie, 1915 | 666 |
| SECTION D. SHELL-SHOCK TREATMENT AND RESULTS | |||
| 473. | Deafmutism: Spontaneous cure | Mott, 1916 | 672 |
| 474. | Two returns to the front | Gilles, 1916 | 675 |
| 475. | Vicissitudes in 15 months | Purser, 1917 | 676 |
| 476. | Deafmutism: Spontaneous cure | Jones, 1915 | 678 |
| 477. | Course of an oniric delirium | Buscaino, Coppola, 1916 | 679 |
| 478. | Same | Buscaino, Coppola, 1916 | 681 |
| 479. | Paraplegia: Cure by Iron Cross | Nonne, 1915 | 682 |
| 480. | Mutism cured by getting drunk | Proctor, 1915 | 682 |
| 481. | Mutism cured by working in vineyard | Anon, 1916 | 683 |
| 482. | Deafmutism: Spontaneous recovery of speech. Recovery of hearing by isolation | Zanger, 1915 | 684 |
| 483. | Excess of sympathy on furlough | Binswanger, 1915 | 685 |
| 484. | Hysterical seizures treated by hydrotherapy | Hirschfeld, 1915 | 688 |
| 485. | Low blood pressure treated by pituitrin | Green, 1917 | 690 |
| 486. | Manual contracture: Various treatments | Duvernay, 1915 | 691 |
| 487. | Massage and mechanotherapy | Sollier, 1916 | 692 |
| 488. | Mine explosion; headache: Lumbar puncture | Ravaut, 1915 | 693 |
| 489. | Hysterical clenched fist: Treatment by fatigue of flexors | Reeve, 1917 | 694 |
| 490. | Hysterical adduction of arm: Treatment by induced fatigue | Reeve, 1917 | 695 |
| 491. | Hysterical cross-legs: Treatment by induced fatigue | Reeve, 1917 | 696 |
| 492. | Hysterical torticollis: Treatment by induced fatigue | Reeve, 1917 | 697 |
| 493. | Claw foot (2 years): Cure by induced fatigue | Reeve, 1917 | 698 |
| 494. | Traumatic and post-traumatic effects: Surgical treatment | Binswanger, 1917 | 699 |
| 495. | Vomiting: Cure by restoration of self-confidence | McDowell, 1917 | 701 |
| 496. | Self-accusatory delusions: Treatment by “autognosis” | Brown, 1916 | 702 |
| 497. | Deafmutism in three men shell-shocked at one time | Roussy, 1915 | 703 |
| 498. | |||
| 499. | |||
| 500. | Vomiting; incontinence, abasia: Cure by persuasion | McDowell, 1916 | 705-706 |
| 501. | Hysterical convulsions cured by an explanation | Hurst, 1917 | 706 |
| [xxxiv]502. | Course of a case with crises of trembling | Roussy, 1915 | 706 |
| 503. | Two cases of lameness cured by persuasion | Russel, 1917 | 707 |
| 504. | |||
| 505. | Head trauma: Treatments by bandage, isolation, open air and to-and-fro transfers | Binswanger, 1915 | 708 |
| 506. | Rationalization of war memories | Rivers, 1918 | 712 |
| 507. | Same | Rivers, 1918 | 713 |
| 508. | Same | Rivers, 1918 | 714 |
| 509. | Same | Rivers, 1918 | 715 |
| 510. | Same, without redeeming feature as nucleus of rationalization | Rivers, 1918 | 716 |
| 511. | Paraplegia cured by removal of crutches | Veale, 1917 | 717 |
| 512. | Same | Veale, 1917 | 718 |
| 513. | Paraplegia: Chocolates versus isolation | Buzzard, 1916 | 719 |
| 514. | Blindness, mutism, deafness. Immediate spontaneous recovery from the first; gradual recovery from second; deafness cured by “small operation” | Hurst, 1917 | 720 |
| 515. | Deafness: Treatment by stimulating vestibular apparatus | O’Malley, 1916 | 721 |
| 516. | Mutism: Treatment by operative manipulation | Morestin, 1915 | 722 |
| 517. | Visual impairment: Treatment by suggestion, faradism injections | Mills, 1915 | 724 |
| 518. | Aphonia: Treatment by manipulation in larynx | O’Malley, 1916 | 725 |
| 519. | Same | Vlasto, 1917 | 727 |
| 520. | Mutism, amnesia: Treatment by faradism; climatic cure in dream | Smyly, 1917 | 728 |
| 521. | Blindness: Cure by injections in temple | Bruce, 1916 | 729 |
| 522. | Deafness cured by suggestion in writing | Buscaino, 1916 | 730 |
| 523. | Reproduction of Shell-shock story in hypnosis: Recovery | Myers, 1916 | 732 |
| 524. | Same | Myers, 1916 | 733 |
| 525. | Automatism, amnesia, deafmutism: Recovery by hypnosis | Myers, 1916 | 734 |
| 526. | Mutism: Recovery by hypnosis | Hurst, 1917 | 736 |
| 527. | Stammering: Cure by hypnosis | Hurst, 1917 | 737 |
| 528. | Mutism and amnesia: Cure by hypnosis | Myers, 1916 | 739 |
| 529. | Victoria Cross winner: Bayonet clutch contracture revealed by hypnosis | Eder, 1916 | 741 |
| 530. | Contracture: Hypnotic cure “indecently quick” | Nonne, 1915 | 742 |
| 531. | “Doll’s head” anesthesia: Mutism: Cure by hypnosis | Nonne, 1915 | 744 |
| 532. | Mine explosion: Tremors (also ante bellum tremors): Cure by hypnosis | Grünbaum, 1916 | 745 |
| 533. | Astasia-abasia: Cure by hypnosis | Nonne, 1915 | 747 |
| 534. | Crural monoplegia: Cure by hypnosis | Hurst, 1917 | 748 |
| 535. | Tremors and sensory disorders: Cure by hypnosis | Nonne, 1915 | 749 |
| 536. | Paraplegia of gradual development: Cure by repeated hypnosis | Nonne, 1915 | 751 |
| [xxxv]537. | Visual impairment and dysbasia: Cure by hypnosis | Ormond, 1915 | 752 |
| 538. | Blindness cured by hypnosis | Hurst, 1916 | 753 |
| 539. | Postoperative retention of urine: Relief by hypnosis | Podiapolsky, 1917 | 754 |
| 540. | Postoperative pains: Relief by hypnosis | Podiapolsky, 1917 | 755 |
| 541. | Stereotyped war dream and ante bellum headache: Cure by hypnosis | Riggall, 1917 | 756 |
| 542. | Amnesia and ante bellum headache: Cure by hypnosis | Burmiston, 1917 | 757 |
| 543. | Convulsions cured by hypnosis | Hurst, 1917 | 759 |
| 544. | Two attacks of mutism: Spontaneous recovery from one in 18 months, from the other by hypnosis | Eder, 1916 | 759 |
| 545. | Neurasthenic symptoms cured by repeated hypnosis | Tombleson, 1917 | 760 |
| 546. | Neurasthenic symptoms: Improvement under repeated hypnosis | Tombleson, 1917 | 761 |
| 547. | Convulsions “Jacksonian” and dysbasia: Cure by hypnosis | Tombleson, 1917 | 762 |
| 548. | Agoraphobia: Cure by hypnosis | Hurst, 1917 | 763 |
| 549. | Manual tremors: Treatment by forcing and isolation | Binswanger, 1915 | 764 |
| 550. | Mutism: Psychoelectric cure | Scholz, 1915 | 766 |
| 551. | Hemiplegia and deafmutism; (also convulsions by heterosuggestion): Improvement by faradism; full recovery by suggestion | Arinstein, 1915 | 767 |
| 552. | Deafmutism, cures, relapses and eventual cure by anesthesia | Dawson, 1916 | 768 |
| 553. | Deafness: Cure by suggestion on emerging from ether | Bruce, 1916 | 770 |
| 554. | Aphasia, hemiplegia, hemianesthesia, and (by medical suggestion) trismus: Cure by anesthesia and suggestion | Arinstein, 1915 | 771 |
| 555. | Triplegia, mutism, jumping-jack reactions: Cure by anesthesia, verbal suggestion, faradism | Arinstein, 1915 | 773 |
| 556. | Mutism and musical alexia: Cure by anesthesia | Proctor, 1915 | 775 |
| 557. | Deafmutism: Deafness cured by anesthesia | Gradenigo, 1917 | 776 |
| 558. | Interaction of two cases (deafmute and mute) under treatment | Smyly, 1917 | 777 |
| 559. | |||
| 560. | Dysbasia: Cure by stovaine anesthesia | Claude, 1917 | 778 |
| 561. | Same | Claude, 1917 | 779 |
| 562. | Deafmutism | Bellin, Vernet, 1917 | 780 |
| 563. | Monoplegia: Cure by electricity administered with a bored and authoritative look | Adrian, Yealland, 1917 | 782 |
| 564. | Monoplegia after sling: Technique of electrical suggestion and “rapid” reëducation | Adrian, Yealland, 1917 | 783 |
| 565. | Hysterical “sciatica”: Treatment by faradism and verbal suggestion | Harris, 1915 | 785 |
| 566. | Prognosis of intensive reëducation in reflex (physiopathic) disorder | Vincent, 1916 | 786 |
| [xxxvi]567. | Hysterical contracture (with physiopathic features) brutally conquered | Ferrand, 1917 | 788 |
| 568. | Paraparesis: Cure by exercises electrically provoked | Turrell, 1915 | 790 |
| 569. | Astasia-abasia: (“Lourdes-like” cure) | Voss, 1916 | 791 |
| 570. | Abasia: Rapid cure | Schultze, 1916 | 792 |
| 571. | Heterosuggestive brachial paresis: Electric suggestion and recovery in five days | Hewat, 1917 | 794 |
| 572. | Contracture of right index finger and thumb: Psychoelectric cure | Roussy, L’Hermitte, 1917 | 795 |
| 573. | Brachial monoplegic able to descend ladder with arms only | Claude, 1916 | 795 |
| 574. | Brachial monoparesis: Vicissitudes of treatment | Vincent, 1917 | 796 |
| 575. | Paresis and sensory disorder: Reëducation | Binswanger, 1915 | 798 |
| 576. | Seizures (of ante bellum origin), astasia-abasia, anesthesias: Reëducation | Binswanger, 1915 | 800 |
| 577. | Progress in case of paresis of foot and spasticity of hip | Binswanger, 1915 | 805 |
| 578. | Mutism (Reëducation) | Briand, Philippe, 1916 | 808 |
| 579. | Stammering: Isolation and reëducation | Binswanger, 1915 | 810 |
| 580. | Deafmutism: Phonetic reëducation | Liébault, 1916 | 814 |
| 581. | Aphonia: Pressure on sternum and respiratory gymnastics | Garel, 1916 | 816 |
| 582. | Stammering: Reëducation | MacMahon, 1917 | 817 |
| 583. | Speech disorder: Reëducation | MacMahon, 1917 | 818 |
| 584. | Camptocormia: Psycho-electric cure: lameness cured by reëducation | Roussy, L’Hermitte, 1917 | 819 |
| 585. | Deafmutism: Speech recovery by suggestion and reëducation: Hearing by reëducation | Liébault, 1916 | 822 |
| 586. | Mutism; stammering; Reëducation; hypnosis | MacCurdy, 1917 | 823 |
| 587. | Anesthesias: Spontaneous gradual recovery: “Paralysis” cured by reëducation | Binswanger, 1915 | 824 |
| 588. | Deafmutism; head movements, anesthesia: Cure by faradism, massage and reëducation | Arinstein, 1916 | 827 |
| 589. | Amnesia and paralysis: Reëducation | Batten, 1916 | 828 |
| SECTION E. EPICRISIS | |||
| PARAGRAPH | |||
| Terminology | 1-8 | ||
| Diagnostic Delimitation Problem | 9-39 | ||
| The Nature of War Neuroses | 40-74 | ||
| Diagnostic Differentiation Problem | 75-99 | ||
| General Nature of Shell-shock | 89-102 | ||
| Treatment: General Observations | 103-114 | ||
The data from all the belligerent countries, collected in this book, go far to prove that, whatever at last you elect to term Shell-shock, you must pause to consider whether your putative case is not actually:
A matter of spirochetes?
The response of a subnormal soldier?
An equivalent of epilepsy?
An alcoholic situation?
A result of neurones actually hors de combat?
A state of bodily weakness (perhaps of faiblesse irritable)?
A bit of dementia praecox?
One of the ups and downs of the emotional (affective, cyclothymic) psychoses?
An odd psychopathic reaction in which the response is abnormal not so much by reason of excessive stimulus as by reason of defective power of response?
On a simpler basis, is not our Shell-shocker just a banal example of hysteria, neurasthenia, psychasthenia; and is not this psychoneurotic more peculiar in his capacity to be shocked than are the conditions that purvey the shocks?
Put more concretely in the terms of available tests and criteria, open to the psychiatrist, does not every putative Shell-shock soldier deserve at some stage a blood test for syphilis? Should we not be reasonably sure we are not facing a man inadequate to start with, so far as mental tests avail? Should we not verify (even at considerable expense of time and money by so-called “social service” methods) the facts of epilepsy and epileptic taint? Of alcoholism? And so on? There can be no two answers to these questions.
Upon the following page is a practical grouping of mental diseases, devised in the first place, not for war psychoses, but for the initial sifting of psychopathic hospital cases. Now[2] the psychopathic hospital group of cases constitutes in peace practice the closest analogue of the mental cases met in active military practice, because the “incipient, acute, and curable”[1] cases, for which psychopathic hospitals are built and which flock to or are sent to the wards and outdoor departments of such hospitals, are precisely the cases that early come forward in active military practice. They are precisely the cases in which that pathological event—whatever it is—we know as Shell-shock may be expected to develop. It is precisely the “incipient, acute, and curable” instances of mental disease which we hope to exclude from our American army by cis-Atlantic winnowing-out at the hands of neuropsychiatric experts—the best preventive we hope both of Shell-shock and of other worse mental conditions, if such there be. Military mental practice plainly deals, not so much with frank and committable insanity, as with mental diseases of a medically milder but a militarily far more insidious nature.
[1] Official phrase for the scope of the Psychopathic Hospital, Boston, Massachusetts.
A further inspection of this grouping of mental diseases shows not only that it contains many conditions not usually termed “insanity” (such as, e.g., feeblemindedness, epilepsy, alcoholism, sundry somatic diseases, psychoneuroses), but that these conditions are presented for practical purposes in a certain seemingly arbitrary order. Without attempting to justify this selection of scope (not too wide for modern psychiatry, most would readily acknowledge), I shall draw out a little further what I consider to be the virtues of the order selected. In the first place, all will concede, some order of consideration of collected data is a prime necessity to the tyro. Without an order of consideration the diagnostic tyro is but too apt to find in the best textbooks of psychiatry (even more easily the better the textbook) all he needs to prove that the case in hand is—almost anything he selects to make his case conform to! And how much more dangerous this debating-society method of diagnosis (by choice of a side and matching a textbook type) may become in the fluid and elastic conditions of psychopathic hospital practice, can readily be observed by one who contemplates the formes frustes and entity-sketches that the “incipient, acute, and curable” group of cases presents.
The order adopted for these groups (which roughly correspond to botanical or zoological orders) is a pragmatic order for successive exclusion on the basis of available tests, criteria, or information: the actual diagnosis is a product of still further differentiation within the several groups.
The case-histories of this book will show that
(a) most shell-shock is in group X, Psychoneuroses,
(b) the diagnostic delimitation problem is chiefly against I. Syphilopsychoses, III. Epileptoses, VI. Somatopsychoses,
(c) the finer differentiation problem is between X. Psychoneuroses and V. Encephalopsychoses. (See Epicrisis, propositions 9-12, 40-43, 72-73.)
| I. | Syphilitic Psychoses | SYPHILOPSYCHOSES |
| II. | Feeblemindedness | HYPOPHRENOSES |
| III. | Epilepsy | EPILEPTOSES |
| IV. | Alcoholic, Drug, and Poison Psychoses | PHARMACOPSYCHOSES |
| V. | Focal Brain Lesion Psychoses | ENCEPHALOPSYCHOSES |
| VI. | Symptomatic (Somatic) Psychoses | SOMATOPSYCHOSES |
| VII. | Presenile-Senile Psychoses | GERIOPSYCHOSES |
| VIII. | Dementia Praecox and Allied Psychoses | SCHIZOPHRENOSES |
| IX. | Manic-Depressive and Allied Psychoses | CYCLOTHYMOSES |
| X. | Psychoneuroses | PSYCHONEUROSES |
| XI. | Other Forms of Psychopathia | PSYCHOPATHOSES |
No conclusions are intended to be drawn in these introductory pages. Such conclusions as are risked are placed in the Epicrisis (see Section E). But so much can be said: If we are ever to surround the problem of Shell-shock (intra bellum or post bellum), we must approach it with no artificial and à priori limitations of its scope. We must not even agree beforehand that Shell-shock is nothing but psychoneurosis: that would be a deductive decision unworthy of modern science. In the collection of these cases, I have tried to place the topic upon the broadest clinical base. Samples of virtually every sort of mental disease and of several sorts of nervous disease have been laid down, some obviously not instances of Shell-shock, some mixed with clinical phenomena of Shell-shock, others hard to tell offhand from Shell-shock—the whole on the basis that we shall earliest learn what Shell-shock, the pathological event, is by studying what it is not. As the sequel may show, we are perhaps not entitled to regard Shell-shock, the pathological event, as always associated with shell-shock, the physical event. We shall, therefore, find in Section A (see tables on pages 6 and 7).
(1) Cases without either physical shell-shock, or pathological Shell-shock—psychoses of various kinds incidental in the war (--+).
(2) Cases with physical shell-shock but without pathological Shell-shock—psychoses of various kinds seemingly liberated by, aggravated by, or accelerated by the physical factor of shell-shock (+-+).
(3) Cases without physical shell-shock but with both symptoms of pathological Shell-shock as well as of other psychosis (-++).
(4) Cases with physical shell-shock, with clinical phenomena of Shell-shock, as well as of other psychosis (+++).
At the end of Section A, accordingly, we shall be left with two more formulae for discussion in Sections B, C, and D, viz:
(5) Cases without physical shell-shock but with symptoms of pathological Shell-shock (-+-).
(6) Cases with physical shell-shock and pathological Shell-shock (++-).
The data of Section A will solidly prove that Shell-shock, however picturesque the term for laymen or in the argot of the clinic, is medically most intriguing. As we cannot get rid of the term (even by suppressing it in parentheses or by condemning it to the limbo of the so-called), we must make the best of it by calling Shell-shock just the ore in the clinical mine. To say the least, the term is harmless: it merely stimulates the lay hearer to questions. These questions he must ask of the expert. But every time that the expert suavely states that Shell-shock is nothing but psychoneurosis, that expert runs the risk of hurting some patient who may or not have a psychoneurosis but has been called psychoneurotic. All the while, of course, the suave expert is perfectly right—statistically. In fine, the man you have called a victim of Shell-shock is probably a victim of psychoneurosis, but only probably!
Section A shows how he may—not probably, but possibly—be a victim of say ten other things. But it is not that he has an even chance of being one of these ten other things. As the reader watches the procession of cases in Section A, he will perceive that, amongst the ten major groups there studied, some have far greater diagnostic likelihood than others. Thus, syphilis, epilepsy, and somatic diseases will in the sequel prove more dangerous to our success as diagnosticians than, e. g., feeblemindedness or even perhaps alcoholism. But now let us look at these cases systematically, just as if we dealt with so many cases of Railway-spine or any other “incipient, acute, and curable” cases.
| ⎧‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾⎫ | |||
|---|---|---|---|
| ⎧‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾⎫ | |||
| SHELL-SHOCK (THE PHYSICAL FACTOR) |
SHELL-SHOCK (NEUROTIC SYMPTOMS) |
PSYCHOSIS (SYMPTOMS NON-NEUROTIC) |
|
| Absent | Absent | INCIDENTAL | |
| Present | Absent | LIBERATED, AGGRAVATED, ACCELERATED PSYCHOSES | |
| Absent | COMBINED NEUROSES AND PSYCHOSES [2](Formula -++) |
||
| Present | COMBINED NEUROSES AND PSYCHOSES (Formula +++) |
||
| Absent | NEUROSES (Quasi Shell-shock) |
Absent | |
| Present | NEUROSES (True Shell-shock) |
Absent | |
| ⎧‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾⎫ | |||
|---|---|---|---|
| ⎧‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾‾⎫ | |||
| S, N, P[3] = | SHELL-SHOCK (THE PHYSICAL[4] FACTOR) PRESENT |
SHELL-SHOCK (NEUROTIC SYMPTOMS) PRESENT |
PSYCHOSIS (NON-NEUROTIC SYMPTOMS) PRESENT |
| P = | - | - | + |
| SP = | + | - | + |
| NP = | - | + | + |
| SNP = | + | + | + |
| N = | - | + | - |
| SN = | + | + | - |
[3] In the literal formulae, S = Shell-shock, N = Neurosis, P = Psychosis.
[4] These plus-or-minus formulae are not intended to imply that the physical factor, where present (+), must have worked a physical effect upon the nervous system: the effects of the physical factor might be wholly emotional or otherwise psychic.
An officer of high rank deserts his command in a crisis: alienists’ report.
M. X. was an officer ranking high in the French army, having military duties of a critical nature and of great importance (social reasons forbid Briand’s giving informatory details). Suffice it to say that he was brought before court-martial for abandoning his post at the very moment when his presence was most urgently required. He turned tail, without taking the most elementary military precautions.
M. X. was passed up to alienists. He was not a case of Shell-shock unless of the anticipatory sort. He was somatically run-down and of lowered morale and now 65 years of age. The campaign had been fatiguing.
The alienists decided that the officer had not been responsible for his non-military acts. He had been, they found, in a state of mental confusion at the time of desertion, such that amnesia for his duties and heedlessness of consequences had allowed him to leave the front without looking behind him or securing substitution. This state of mental confusion had been preceded by overwork and several nights of insomnia.
Moreover he was palpably arteriosclerotic. Blood pressure was high. The history was one of slight shocks and a mild hemiplegia. The confusion at the front was only the most recent of a series of transitory attacks of confusion. At the time of examination this high officer was actually in a state of mild dementia.
M. X. was an old colonial man, malarial, and had been a victim of syphilis.
A naval officer sees hundreds of submarines: General paresis.
A naval officer, 36, during August, 1916, asserted that he could see hundreds of submarines. At one time he imagined that he was receiving trunk calls in the middle of the ocean. He was admitted to Haslar, and the Wassermann reaction of the serum was found strongly positive. The spinal fluid was not at this time examined. The officer recovered to some extent, was given no special treatment, and was sent on leave.
He came under observation again in October, 1916, having become very strange in his manner, on one occasion passing water into the coal box, and talked about impending electrocution. His ankle-jerks were found sluggish and there was a patch of blunting to pin pricks. The diagnosis of general paresis was made. The spinal fluid was afterward examined and found to be negative to the Wassermann reaction but contained 15 lymphocytes per cubic mm.
Three full doses of Kharsivan freed him from delusions and left him apparently absolutely sane. It was recommended that he should be kept at Haslar to continue treatment. However, he had been certified insane and was therefore sent to Yarmouth, from which he was discharged in February, 1917, having been in good mental health throughout his stay there.
Re syphilis and general paresis of military officers, as in Cases 1 and 2, Russo-Japanese experience was already at hand. Autokratow saw paretic Russian officers sent to the front in early but still obvious phases of disease. These paretics and various arteriosclerotics, Autokratow saw back in Russia in the course of a few months.
Re naval cases, see also Case 5 (Beaton). Beaton thinks that monotonous ship duty, alternating with critical stress of service, bears on morale and liberates mental disorder.
Neurosyphilis may be aggravated or accelerated under war conditions.
A German, long alcoholic and thought to be weakminded, volunteered, but shortly had to be released from service. He began to be forgetful and obstinate, cried, and even appeared to be subject to hallucinations. The pupils were unequal and sluggish. The uvula hung to the right. The left knee-jerk was lively, right weak. Fine tremors of hands. Hypalgesia of backs of hands. Stumbling speech. Attention poor.
It appeared that he had been infected with syphilis in 1881 and in 1903 had had an ulcer of the left leg.
The military commission denied that his service had brought about the disease.
An English colonel thought himself perfectly fit when he went out with the original Expeditionary Force. He had had leg pains, regarded as due to rheumatism or neuritis. He was invalided home after exhaustion on the great retreat. He was now found to be suffering from a severe tabes. He improved greatly under rest and antisyphilitic treatment. He has now returned to duty.
An apparently healthy man, serving on an English battle-ship, severed a tendon in a finger. The injury was regarded as minor. The tendon was sutured and the wound healed. During the man’s convalescence he was accidentally discovered to have an Argyll-Robertson pupil and some excess reflexes. Neurosyphilis had probably antedated the accident. But from the moment of this trivial injury, the disease advanced rapidly.
Overwork in service; several months exacting work well performed: General paresis.
A lieutenant of Territorials, aged 41 (heredity good, anal fistula at 30, with ulceration of penis of an unknown nature at the same period). In 1907 when off service and married, his wife gave birth to a child; no miscarriages. Had been a good soldier in service before the war. The lieutenant was called to the colors August 2, 1914, and was detached for special duty, for the performance of which he was much praised by the commanding officers. The work, however, was too much for him and on April 1 he had to be evacuated to the hospital with a ticket saying “Nervous depression following overwork in service.” On April 14 he seemed well enough for a convalescent camp, but, apparently through red tape, was sent to a hospital at Orléans. On June 23 he had to be evacuated to the Fleury annex. His eyes were dull and features flaccid; his whole manner suggested fatigue. His pupils were myotic, tongue tremulous, speech slow and stumbling. Knee-jerks were exaggerated and gait difficult, the right leg dragging. Headaches. He could not perform the slightest intellectual work and was the victim of retrograde and anterograde amnesia. He was aware of the decline of his mental power and was fain to struggle against it, becoming restless and sad. The gaps in his memory grew deeper, he became more and more impulsive, even violent, and had spells of excitement. Dizziness and palpitation developed. Sometimes there were auditory and visual hallucinations of such intense character that he tried feebly to commit suicide with a penknife. He fell into semicoma, and then had a number of apoplectiform attacks. W. R. +
Apparently the moral and physical situation of the lieutenant was absolutely normal when the campaign began and, as he fulfilled detail duties with absolute correctness for a number of months, Boucherot argues that here is an instance of general paresis declanché by overwork.
Syphilis contracted before enlistment. Neurosyphilis aggravated by service.
A laboring man, 42, who always strenuously denied syphilitic infection, proceeded to France eight months after enlistment. He had not been in France three weeks when he dropped unconscious. He regained consciousness, but remained stupid, dull in expression, and with memory impaired. His speech was also impaired. There was dizziness and a right-sided hemiplegia.
He was confined to bed four months and was then “boarded” for discharge.
Physically, his heart was slightly enlarged both right and left; sounds irregular; extra systoles; aortic systolic murmur transmitted to neck; blood pressure 140:40. Precordial pain, dyspnoea.
Neurologically, there was a partial spastic paralysis of the right thigh which could be abducted, could be flexed to 120°, and showed some power in the quadriceps. There was also a spastic paralysis of the right arm, but the shoulder girdle movements were not impaired. There was a slight weakness on the right side of the face. There was no anesthesia anywhere.
The deep reflexes were increased on the right side, Babinski on right, flexor contractures of right hand, extensor contractures of right leg, abdominal and epigastric reflexes absent, pupils active, tongue protruded in straight line.
Fluid: slight increase in protein. W. R. + + +
The Board of Pension Commissioners ruled that the condition had been aggravated by service (not “on service”).
Re general paresis, Fearnsides suggested at the Section of Neurology in the Royal Society of Medicine early in 1916, that in all cases of suspected Shell-shock the Wassermann reaction of the serum should be determined, and went on to say that cases of so-called Shell-shock with positive W. R. often improve rapidly with antisyphilitic remedies.
Duration of neurosyphilitic process important re compensation.
A Canadian of 36 enlisted in 1915, served in England, and was returned to Canada in February, 1917, clearly suffering from some form of neurosyphilis (W. R. positive in serum and fluid, globulin, pleocytosis 108).
There is no record of any disability or symptom of nervous or mental disease at enlistment. The first symptoms were noted by the patient in May, 1916, six months or more after enlistment. The case was reviewed at a Canadian Special Hospital, October 11, 1916, by a board which reported:
“The condition could only come from syphilitic infection of three years’ standing” (a decision bearing on compensation); but the general diagnosis remained:
“Cerebrospinal lues, aggravated by service.”
The picture which the medical board regarded as of at least three years’ standing was as follows:
History of incontinence, shooting pains, attacks of syncope, general weakness, facial tremor, exaggerated knee-jerks, pupils react with small excursion. Speech and writing disorder, perception dull, lapses of attention, memory defect, defective insight into nature of disorder, emotional apathy.
1. Was the conclusion “aggravated by service” sound? On humanitarian grounds the victim is naturally conceded the benefit of the doubt. But it is questionable how scientifically sound the conclusion really was.
2. Could the condition come only from syphilitic infection of at least three years’ standing? Hardly any single symptom in this case need be of so long a standing; yet the combination of symptoms seems by very weight of numbers to justify the conclusion of the medical board.
Farrar’s case and thirteen others of “Neurosyphilis and the War” were included in a general work on Neurosyphilis (Case History Series, 1917, Southard and Solomon). For military syphilis in general, see Thibierge’s Syphilis dans l’Armée (also in translation).
General paresis lighted up by the stress of military service without injury or disease?
In apparently good health a French soldier repaired to the colors, in August, 1914, being then 23 years old.
Two years later, August, 1916, symptoms appeared: speech disorder with stammering, change of character (had become easily excitable), stumbling gait. He became more and more preoccupied with his own affairs, grew worse, and was sent to hospital in October, 1916.
He was then foolish and overhappy, especially when interviewed. There was marked rapid tremor of face and tongue. Speech hesitant, monotonous, and stammering to the point of unintelligibility. His memory, at first preserved, became impaired so that half of a test phrase was forgotten. Simple addition was impossible and fantastic sums would be given instead of right answers. Handwriting tremulous, letters often missed, others irregular, unequal, and misshapen.
Excitable from onset, the patient now became at times suddenly violent, striking his wife without provocation. After visit at home, he would forget to return to hospital. Often he would leave hospital without permission (of course the more surprising in a disciplined soldier). No delusions.
Serum and fluid W. R. positive; albumin; lymphocytosis.
Neurological examination: Unequal pupils, slight right-side mydriasis, pupils stiff to light, weakly responsive in accommodation, reflexes lively, fingers tremulous on extension of arms.
The patient had, December 5, 1916, an epileptiform attack with head rotation, limb-contractions and clonic movements. Should this soldier recover for disability obtained in service? Marie was inclined to think military service in part responsible for the development of the paresis. Laignel-Lavastine thought so also, but that the amount assigned should be 5%-10% of the maximum assignable.
SYPHILITIC ROOT-SCIATICA (lumbosacral radiculitis) in a fireworks man with a French artillery regiment.
No direct relation of this example of root-sciatica to the war is claimed nor was there a question of financial reparation.
There was no prior injury. At the end of March, 1915, the workman was taken with acute pains in lumbar region and thighs, and with urgent but retarded micturition.
Unfit for work, he remained, however, five months with the regiment, and was then retired for two months to a hospital behind the lines. He reached the Salpêtrière October 12, 1915, with “double sciatica, intractable.”
There was no demonstrable paralysis but the legs seemed to have “melted away,” fondu, as the patient said. Pains were spontaneously felt in the lumbar plexus and sciatic nerve regions, not passing, however, beyond the thighs. These pains were more intense with movements of legs; but coughing did not intensify the pains. Neuralgic points could be demonstrated by the finger in lumbar and gluteal regions and above and below the iliac crests (corresponding with rami of first lumbar nerves). The inguinal region was involved and the painful zone reached the sciatic notch and the upper part of the posterior surface of the thigh.
The sensory disorder had another distribution, objectively tested. The sacral and perineal regions were free. Anesthesia of inner surfaces of thighs, hypesthesia of the anterior surfaces of thighs and lower legs. The anesthesia grew more and more marked lower down and was maximal in the feet, which were practically insensible to all tests, including those for bone sensation. There was a longitudinal strip of skin of lower leg which retained sensation.
Position sense of toes, except great toes, was poor. There was a slight ataxia attributable to the sensory disorder—reflexes of upper extremities, abdominal, and cremasteric preserved, knee-jerks, Achilles and plantar reactions absent.
The vesical sphincter shortly regained its function, though its disorder had been an initial symptom. Pupils normal.
The “sciatica” here affects the lumbosacral plexus.
As to the syphilitic nature of this affection, there had been at eighteen (22 years before) a colorless small induration of the penis, lasting about three weeks. There was now evident a small oval pigmented scar. The patient had married at 20 and had had three healthy children.
The lumbar puncture fluid yielded pleocytosis (120 per cmm.). Mercurial treatment was instituted.
The treatment has not reduced the pains. Long thinks it was undertaken too long (six months) after onset. The warning for early diagnosis is manifest. There was somehow a delay under the medical conditions of the army.
Re syphilis in munition-workers Thibierge has much to say of French conditions. Throughout his work on syphilis in the army, he stresses the large number of venereal cases in men mobilized for munition-work. Medical inspections ought, according to Thibierge, imperatively to be made in the munition-works and upon all mobilized workmen, whether French or belonging to the Colonial contingents. These men are under military control in France, but they have more opportunities than the soldiers for contracting and disseminating syphilis. They are, in point of fact, very often infected and in a higher proportion than are the soldiers at the front. The munition-workers should also be obliged to report their infections to the physician, whether or no they are under treatment by military or by private physicians.
Thibierge devotes a chapter to syphilis as a national danger. Not only do available statistics prove that there is more syphilis in the population since the outbreak of war, but the number of married women going to special hospitals for syphilis is abnormally high and entirely out of proportion to the number of married women resorting to these clinics in peace times. A certain number are contaminated by their husbands on leave. Thibierge calls attention to the fact of the extraordinary frequency of syphilis in young men (two or three, sixteen to eighteen years of age, at Saint-Louis Hospital at each consultation).
A disciplinary case: Syphilitic?
Reports varied about a certain German soldier who came up for discipline. Inferiors thought he was harsh and tricky. A lieutenant declared that the man always wanted to have proper respect paid to him, and that he was unduly excited by trifles. The man had become latterly very nervous on account of battle strain and protracted shelling.
July 28, 1915, the man, who had been drinking with comrades the night before, was excitedly talking to an officer concerning relief of a guard. The soldier stated, “As a sergeant on duty with a service record of 15 years, I think it is my affair.” The lieutenant replied, “So far as I am concerned, the matter is settled.” The sergeant yelled, “As far as I am concerned, it is settled also. By the way, my name is Mr. Vice Sergeant …,” and with that the sergeant wrote down the lieutenant’s words and refused to obey the lieutenant’s order to “Stop writing.” The lieutenant drew his sword and said, “Take your hands down.” The sergeant replied, “Surely I am permitted to write.” Lieutenant: “Subordination; don’t forget yourself, Vice Sergeant.…” The sergeant jeered, “You forgot yourself anyhow;” whereupon the lieutenant: “Well, such a thing never happened to me before.” The sergeant, jeeringly, “Nor to me either. If I were not in undress I should know what to do.” The lieutenant: “Vice Sergeant …, remain here. This matter will be settled at once.” The sergeant: “It is Mr. Vice Sergeant …,” whereupon he gave his notebook to a hornblower and said, “Write.” The lieutenant: “Stay.” The sergeant: “What, stay here. No, I’ll not stay,” and made off. The lieutenant called after him, “Put on your service dress and see the captain.” He made ready but said, “This half-idiot gives an order like that to a sergeant with 15 years’ record.”
The examination showed that the man had a hypalgesia. He complained of violent headaches. He said that he had had syphilis 10 years before; there were no bodily stigmata.
Regulations broken: General paresis.
A German 1st-lieutenant, on active service before the war, had left the service because there was not enough for him to do in peace times. During his war service, he became drunk and had two soldiers bound to a doorpost, with coats unbuttoned and without their caps—a process quite verboten. While in Königsberg, he reported himself ill, and failed to go to a designated hospital. He was accordingly treated as a deserter. He ran up bills with landlady and servant girls, saying that he was going to receive money from his wife. Under hospital examination, he said he was only a Baden man with a lively temperament. He got angry at the phrase test feeding, refused food, got excited when asked to help in the care of other patients, and wrote a letter saying, “If it is the idea to make me nervous by removing the air from me, by prescribing rest in bed—a punishment only suitable for a boy who cannot keep himself neat—and such chicaneries, these philanthropic attempts are bound to fail on my robust peasant nerves. Of course I know that money considerations make the stay of every paying patient desirable, but I am really too good for that. [The expenses were being borne by the state.] I have openly stated what is being here done with me is foolery, and I stick to that phrase. The food, already poor enough, is no better, when the meat of a half-rotten cow comes twice to the table.” This patient was, according to Kastan, a victim of general paresis.
Re general paresis and delinquency, Gilles de la Tourette long ago maintained that there was a medicolegal period in paresis. Lépine in his work on Troubles Mentales de la Guerre speaks of the unexpected frequency of general paresis in the army, and calls attention at the outset to the medicolegal period. The danger of overt delinquency is, in fact, greater under military than under civilian conditions on account of the closer surveillance of the soldier. Desertion and thievery are the main forms.
Unfit for service: General paresis.
Kastan describes a non-commissioned officer, who came voluntarily into the clinic. It seems that he had absented himself (?) from the army in the suburbs of Königsberg, September 3, 1914. He was arrested October 7th. Once before he had been brought to Kastan’s clinic on the suspicion of general paresis, but had been dismissed as non-paretic. Brought in again in a condition of marked fear, he declared that he had to fall behind his company while he was on the march on account of a feeling of weakness. He had been taken to a hospital and then carried to the suburbs of Königsberg, examined, and found unfit for service.
He had in his 20th year become infected with syphilis, and had recently become forgetful, subject to fears, and easily excitable. He had been very unhappily married with a woman who was hysterical and threatened to shoot and poison him. He lived in a condition of continual quarrels with her. The symptoms that he felt on the march were numbness of the legs and a rush of blood to the head. In the clinic, he was subject to much dreaming and raving about the war. There was excessive perspiration.
1. As to the proper interpretation of this case, details are lacking as to the physical and laboratory side. In fact, it would appear that the suspicion of paresis at his first reception in a clinic was dismissed without resort to laboratory findings.
There are no neurological symptoms in the case clearly suggestive of neurosyphilis, except perhaps the numbness of the legs. The remainder of the picture appears to be entirely psychic. Sensory and intellectual symptoms are missing unless we count the war dreams and mania as intellectual. It appears wiser to count these as emotional in the sense that they were roused by emotion-laden memories. The fear, perspiration, and feelings of head flush are perhaps to be best interpreted as satellites about an emotional nucleus.
Hysterical chorea versus neurosyphilis.
There were various complications in the case of a lieutenant (nervous tic in childhood; travel 23 to 30), who was at Antwerp during the period of mobilization. He was taken there by the Germans; was a prisoner in their hands for 55 days; and succeeded under great strain in escaping.
He then entered his regiment, and, passing the examinations, was made an adjutant, and went to the front, March, 1915. He stayed ten months in the Verdun region, under heavy bombardment, and in June was bowled over and buried by a 210. He seemed to be fearless, getting no sensation from shell-bursts except a griping sensation in the bowels.
However, his character had altered in the direction of irritability; and by the end of January, 1916, he had to be evacuated for the first time from the front, for general weakness, with the diagnoses: neurasthenia, neuralgia, dyspeptic troubles, great general fatigue, marked depression. In fact, at Narbonne he was asked no questions for several days on account of his obvious depression. He was given ice-bags for violent headaches, complete rest in bed, cacodylate and sodium nucleinate. In two weeks he was up and about.
At this time appeared choreiform movements, which reached their maximum in two or three days, whereupon he was sent, March 4, 1916, to the neurological centre at Montpellier. Here W. R. positive! Neosalvarsan on the second injection (0.45 and 0.60) yielded a strong reaction, with fever, delirium, vomiting, and then jaundice.
About a month later, he was given twenty more intravenous injections, whereupon the choreic movements now decreased, and July 15 he was given convalescence for three months. October 15 he went back to his dépôt cured; and October 20, on request, went to the front. He was potted and under machine-gun fire at times during the next three months, but the choreic movements did not reappear. January 1 he left the trenches as the division went into billets.[21] January 8, suddenly, without any emotional cause, he began to “dance” again. Accordingly, he was evacuated for the second time, January 10, 1917, with the diagnosis: choreic movements, especially on left; evacuate to special centre.
At Royallieu, a lumbar puncture showed a slight lymphocytosis. The headache improved. He was evacuated January 24, 1917, to Val-de-Grâce, with a diagnosis: Recurrent chorea; first attack followed commotio cerebri, nervous depression, inequality of pupils, various pains, contracted in the army. Another W. R. was positive. Twelve intramuscular injections of oxygen cyanide were given, besides baths. He was then sent to Issy-les-Moulineaux with a diagnosis of tic. He showed choreiform movements affecting the legs alone. When sitting, legs extended and flexed, the knees would abduct, then adduct; the thighs flexed. When standing, flexor movements were produced alternately on the left and the right, the knee being raised high, sometimes striking the patient’s hand. In walking, the thigh and lower leg flexion was always out of proportion to the required step. There was thus a sort of saltatory chorea limited to the legs. The reflexes so far as they could be tested were normal save that the left pupil was fixed to light and accommodation; the right pupil was sluggish to light but accommodated normally. Leucoplakia of the cheeks; nocturnal headaches; and pains resembling lightning pains in arms and legs. Lumbar puncture, March 26, showed blood-stained fluid, and the puncture was followed by headache, vomiting, and slow pulse. The fluid showed a slight lymphocytosis; W. R. negative.
It is clear that a diagnosis limiting itself to the leg trouble would probably content itself with “hysterical chorea.” The lieutenant said that when he saw people “dance” he did have a tendency to imitate them; and when he was cured of that, he did not want to go to Lamalou because he would see the ataxic patients there and might fall back into his “dancing.” However, in view of the pupillary inequality, the lymphocytosis, the leucoplakia, the W. R., and the initial neurasthenia and depression found in the very first hospital in which he was examined, we probably should be entitled to consider that general paresis played a part in the chorea.
Shrapnel fragment driven through skull: General paresis.
A private, 31, was wounded December 7, 1916, by a shrapnel fragment which entered the skull above the left ear and lodged in the brain, an inch above and 2½ inches below the middle of the right orbital margin. At Netley, December 30, he proved to show a complete internal and external left sided ophthalmoplegia, with the exception of the external rectus. On the right side, there was a complete paralysis of the superior rectus and a partial paralysis of the inferior rectus and levator palpebrae superioris. There was a paresis of the left side of the face. The right plantar reflex was said to have been extensor at the clearing station, but at Netley it and the other reflexes proved to be normal, as were the optic. The patient was stuporous and had incontinence of urine and feces for two days. Shortly after admission, slurring of speech with a long latent period occurred. It was clear that the shrapnel fragment must have passed far above the crus, and it was not plain how isolated lesions of the third and seventh nerve nuclei could have been brought about without injury of the long tracts of the crus.
The Wassermann reaction of the serum was negative, but that of the spinal fluid was positive. Iodide and mercury secured considerable improvement in the mental condition and some diminution in the paralysis. The patient is now extremely pleased with himself and has a speech suggestive of paresis.
Head trauma: Shell-shock effects, over in a few months. Manic-depressive (?) attack more than two years later. X-ray evidence suggesting brain lesion. Serum Wassermann reaction positive.
A bullet glancing from his gun barrel November 28, 1914, wounded a man in the head, whereupon he lost consciousness and was carried to a hospital and trephined. On coming to, he found that he could not hear and felt pains; but the latter disappeared in a few months. He was given sedentary employment and did his work properly until February, 1917, when he suddenly became sad, wept, slept poorly, stopped eating, had an absent air, and began to complain of his head. He passed whole days without moving, in a sort of stupor, which was then followed by a hypomaniacal agitation in which he walked furiously up and down in the room and threw objects about.
He was found subject to a generalized tremor and he was distinctly weaker on the right side. The tendon reflexes were excessive. The bony sensibility, as well as the pain and temperature sense, and the position and stereognostic senses were completely abolished on the right side. The scar lay on the left side. It was deep and very sensitive to pressure, so that if it was touched ever so slightly the patient began to weep. X-ray indicated loss of substance in the posterior part of the left parietal region. Remains of the projectile were found subcutaneously in the right supraorbital region. The W. R. of the serum was positive. There was no lymphocytosis in the spinal fluid.
Interpretation of this case is manifestly difficult. Four possibilities exist: Syphilis, manic depressive psychosis, traumatic brain disease, and functional shock effects. More than two years had passed between the trauma and the change of character.
Skull trauma in a syphilitic.
A soldier, 31, sustained fracture of the occiput from shell-burst, and thereafter showed confusion and total loss of memory. Operation November 11 withdrew bony fragments and clots, whereupon the man returned practically to normal. He developed, however, a few seizures, in which he struggled, fell, and lost consciousness, afterward suffering from headache. The tendon reflexes were increased. The occipital cicatrix was a little depressed and slightly painful on pressure.
Lumbar puncture showed a very slight lymphocytosis (5 to 6 cells), practically negative globulin reaction, and a low albumin titer. There were no signs of syphilis in the eyes. The W. R. in the serum was strongly positive. Very possibly the traumatic phenomena in this case can be safely disengaged from the syphilitic phenomena.
Re the mechanism by which trauma evokes or accelerates the course of neurosyphilis, it is probable that most neuropathologists believe that the commotio cerebri causes sundry chemical or physical effects in the nerve tissues such that spirochetes are moved into new and more dangerous places, or such that more appropriate food is supplied to the organisms, which then begin to multiply. Whether the organisms live in a kind of symbiosis in the tissues under ordinary circumstances in the pre-paretic period of the development of neurosyphilis, is unknown. Possibly fat embolism should be added to the list of possible causes of the hastening of the neurosyphilitic process. Fat embolism in the brain has been shown by various authors to be accompanied by minute hemorrhages, in the midst of which by proper stains the fat embolism can be made out.
Shell-wound in battle: General paresis.
A soldier in the Territorial Infantry, 42, a gardener who went to taverns, as he said, “like everybody else,” a widower with two children, a good worker though irascible, had had syphilis as a youth. He was called to the colors at the outbreak of the war and got on well despite tremendous strain. March 9, 1915, he was in a bayonet charge with his regiment and was bowled over by a shell of which a fragment wounded him above the knee and several fragments in the thorax. All these fragments were extracted at a temporary hospital, March 11. The man now became strange, refused to obey orders and did a number of peculiar things so that he was sent to Orléans temporary hospital whence he was evacuated to Fleury Asylum, March 19. He refused to give up his things because he was the master. He did not want to go to bed and wanted to keep on walking constantly. He was without sense of shame, satisfied with himself, grandiose as to his millions in bank and the thirty-six decorations he believed had been awarded him. He mistook the identity of the landscape and of the people about him.
Tongue tremulous; pupils unequal; knee-jerks exaggerated; dysarthria; gaps in memory. In May occurred a number of violent reactions.
In June, however, there was a remission; the ideas of grandeur disappeared first, then the tremors and reflex disorder and finally the speech disorder. There was a slight seizure at this point and the man said he had had another such just before he came to the army. July 20 he was invalided out much improved.
In this case of general paresis there is, besides the syphilis, also alcoholism to consider, so that it is not entirely plain that the exertions of campaign liberated the paresis.
Re wounds and paresis, see also Case 5 (Beaton), in which neurosyphilis advanced rapidly from the time of a trivial injury.
Shell-explosion: Syphilitic ocular palsy.
Schuster notes briefly a curious result of the explosion of a shell, which caused the patient in question to lose consciousness. Shortly after the explosion, the patient came to his senses again, but a surprising paresis of the eye muscles had developed. This paresis looked precisely like a syphilitic paresis clinically.
Examination of the blood serum yielded a strongly positive Wassermann reaction.
According to Schuster, the explosion of the shell had brought about hemorrhage in vessels supplying the region of the eye muscle nerves or nuclei. The reason for the selection of these vessels for rupture due to shell explosion is, according to Schuster, that the vessels were probably already syphilitically diseased.
Re hemorrhages in the neighborhood of the oculomotor nuclei, the phenomena of polioencephalitis may be recalled. In that disease, the predisposition to hemorrhage is presumed to be alcoholic, as the cases of ophthalmoplegia of this group almost always appear in alcoholics. However, the first case of hemorrhagic superior polioencephalitis was a non-alcoholic one of Gayet (1875), in which the symptoms followed three days after a boiler explosion.
A tabetic lieutenant “shell-shocked” into paresis?
An apparently competent German professor in an intermediate school, a lieutenant of infantry reserves, 33 years old, on the 17th August, 1914, was stunned for a while by the shock of a cannon-firing 25 feet away. Urination became difficult. Headaches and limb pains ensued, with paralysis of fingers, gastric troubles, forgetfulness, especially for names, insomnia, and general scattering of mental faculties.
Neurologically, the pupils were irregular, left larger than right; Argyll-Robertson reaction. Right knee-jerk livelier than left. Achilles reactions absent. Slow and dissociated pain reactions in feet, lower thighs and lower quarter of upper thighs, with hypalgesia or analgesia. Station good; gait steady. Mentally depressed, slow of thought. Speech poor and of indistinct construction (mild dementia). Calculation ability poor. No pleasure in work.
Wassermann reaction of serum weakly positive.
It seems that for a year the patient had been subject to spells of anger. He was irritated by his wife who had been nervous since an earthquake.
On the occasion of the earthquake, 1911, the patient himself had had a spell of difficulty with urination. The spell had lasted two or three months. The patient had had a chancre in 1902, “cured” in four or five weeks with xeroform. In 1908, when about to marry, he had had six mercurial inunctions.
Re tabes, Lépine shows that tabetics are numerous. They are numerous among officers and also in the auxiliary service, in which latter tabetics are maintained on desk duty. Perhaps they had been admitted to such work as unable to march or fight, on the basis of having had so-called[28] “rheumatism.”
Shell-explosion may precipitate neurosyphilis in the form of tabes dorsalis.
An artilleryman, 38, had a large calibre shell explode very near him and afterward could not hear the whistle of a shell without falling down in a generalized tremor, sweating profusely, urinating involuntarily, in a mental state approaching stupidity. Here was a case that might be regarded as one of morbid cowardice in a psychopath, following violent emotion.
The artilleryman proved to be a victim of tabes and of general paresis. The incontinence of urine under the influence of emotion was nothing but an effect of tabetic sphincter disorder. The crisis of cowardice proved nothing but an initial symptom of general paresis.
Shell-explosion; burial: Tabes dorsalis incipiens.
A French soldier was buried by effects of shell explosion September 8, 1914. He sustained no wound or fracture.
Incontinence of urine developed. Anesthesia of penis and scrotum. Reflexes absent; pupils sluggish. Wassermann reactions suspicious.
The diagnosis tabes dorsalis incipiens was made (hematomyelia of conus terminalis eliminated).
The patient was estimated to be “40% incapacitated,” according to the French “échelle de gravité” of conditions. A full pension would not be justified in the opinion of the French authors.
SHELL-SHOCK PSEUDOTABES (non-syphilitic, serum W. R. positive). Improvement.
Innkeeper B., 36, a shell-shock and burial victim June 20, 1915, was looked on by a number of physicians as a case of genuine tabes.
Even eight months after the episode, he still showed (when observed by Pitres and Marchand, February 3, 1916) absence of knee-jerks and Achilles jerks, a slight swaying in the Romberg position, pupils sluggish to light, incoördination, delayed sensations. There was also a history of pains in the legs, compared by the patient to those of sciatica. These pains came in crises, the longest of which had lasted 30 hours.
It seems that this soldier’s troubles began the day after his shock with a feeling of swollen feet and of cotton wool under them. He stayed on service, however, walking with increasing difficulty.
At the time of his evacuation, July 10, he could walk with great difficulty. “Strips of lead were between his legs.” He could hardly control movements in the dark, or descend stairs. Often his legs would bend under him. Vesical function sluggish.
After a few months the patient could walk better. In February, 1916, he walked thrusting his legs forward trembling, and dragging toes a little. He could not support himself on either leg. Jerkiness and incoördination in extension or flexion of leg on thigh.
The muscular weakness was decidedly against tabes or at all events a pure tabes. The incoördination proved to be due, not to loss of position sense (which was intact) but to unsteady muscular contractions. Deep sensibility was intact.
There were no mental symptoms. There was a slight hesitation in speech and doubling of syllables, but nothing demonstrable with test phrases.
The serum W. R. was positive.
Shell explosion; unconsciousness: Neurosyphilis.
A private, 31, was in the retreat from Mons, was blown up by a shell and buried in May, 1915, went back to the front after two months leave, was knocked unconscious by a shell December, 1916. He came to himself two days later in the hospital, but remained confused and lethargic. In England, December 21, his legs were still weak and walking was unsteady. The right pupil reacted neither to light nor to accommodation and was irregular, eccentric, and dilated. The left pupil showed the Argyll-Robertson reaction. There was early primary optic atrophy. The right knee-jerk was slightly exaggerated. The vibration sense was reduced over sacrum and malleoli. At this time the man’s mental condition was practically normal.
The Wassermann reaction of the serum and spinal fluid proved positive. Improvement followed rest, iodide, mercury, and seven injections of salvarsan. By the middle of February he was able to walk well. The right pupil regained its power to react to accommodation, but remained inactive to light. Meanwhile, the left pupil had regained a slight power to react to light.
Re treatment of syphilis, both Thibierge and Lépine give warning of some bad results with arsenobenzol treatment, though Thibierge states that the number of serious accidents and especially of deaths has diminished more and more now that no arsenobenzol (drug No. 914) is given. Encephalitis is the gravest of the untoward results of injection, sometimes appearing in young and vigorous subjects. Hemorrhagic encephalitis appears to occur more frequently after the second injection than after the first, and according to Thibierge may be especially suspected in subjects who after the first injection present much fever, congestion of face, and cutaneous eruptions. Treatment in these cases should be suspended or given in moderate doses.
Shell-explosion: Neurosyphilis. Fit for light duty.
A corporal, 26, blown up by a shell December 7, 1916, was admitted to the hospital on the 13th, dazed and with symptoms of a left-sided hemiplegia of organic origin. The right pupil was larger than the left. There was a bruise of the scalp in the right parietal region. The man had had syphilis at 16. The Wassermann reaction of the serum was strongly positive. Rest, salvarsan, mercury, and iodides were given, and the general symptoms and hemiplegia gradually disappeared, until on December 12 there was only a moderate weakness of the left side, with knee-jerks in excess, abdominal reflexes absent, and the Babinski reaction.
The Wassermann reaction was still strongly positive. Salvarsan, mercury, and iodide were continued. January 6, 1917, the plantar reflex had become flexor. The abdominal reflex returned. Babinski’s second sign (combined flexion of thigh and pelvis) was now the only evidence of organic disease. Further antisyphilitic treatment removed this sign also. February 28, the man was discharged fit for light duty, with unequal pupils and positive Wassermann reaction, and a complete amnesia for the four weeks following his blowing up in the trenches.
Re fitness for light duty, see remarks on Case 20 concerning desk duty for certain tabetics.
Re the premature or unexpectedly early appearance of neurosyphilis under war conditions, the early claims of some authors have not been maintained. In the above instance, the infection was at 16 and the shell explosion occurred at 26, namely, at about the right interval for the development of neurosyphilitic signs. Gerver states that military service brings out the lesions of paresis earlier than they would otherwise come. Bonhoeffer has been unable to show that cerebrospinal syphilis is favored in its development by the exhaustion factor.
SHELL-SHOCK PSEUDOPARESIS (non-syphilitic). Recovery.
June 19, 1915, a shell exploded some distance from Lieutenant R. He remembers the gaseous smell, the bursting of several shells nearby and a sensation of being lifted into the air. When he recovered consciousness, he was in hospital at Paris-Plage, covered with bruises and scratches. They told him he had been delirious and had vomited and spat blood.
June 24, his wife came to see him, but this visit he could not remember. Nor could his wife at first recognize him, he was so thin. He roused a few moments and recognized his wife, but relapsed into torpor again. Speech was difficult and ideas confused.
A few days later he was able to rise; but his mental status grew worse, especially as to speech and writing, the latter quite illegible. There was insomnia, or, if he slept, war dreams.
August 7, he began a period of five months’ convalescence passed with his family, depressed, given to spells of weeping, confined to bed or couch, unable to “find words,” conscious of his state and troubled about it, speaking of nothing but the war, and afraid to go out for fear of ambuscade. There was at first a slight lameness of the right leg. Although he could walk, he felt pain in the knee on flexing the right leg on the thigh. He walked holding this leg in extension.
On going back to the colors, he was immediately evacuated to the Centre Neurologique at Bordeaux, January 20, 1916.
Examination found a bored, impatient, irritated man, vexed that a man who was not sick should be sent up “comme fou.”
Omitting negative details, neurological examination showed slight lameness as above, body stiff and movements jerky, difficult, unsteady gait. The lieutenant could stand for some time on either leg. Tongue and face tremulous during speech. Limbs moderately tremulous, especially in the performance of test movements.
Knee-jerks and Achilles jerks absent. Other reflexes, including pupillary, normal. Segmentary hypalgesia of right leg, especially about knee. Tremulous speech and writing. Patient would stop short in speaking for lack of words.
Malnutrition. Appetite good, but a bursting feeling after meals.
Skin dry, scaly on legs, fissured on fingers.
Serum W. R. negative. Fluid not examined.
Mental examination. Conscious and complaining of his troubles, Lieutenant R. claimed persistently that he was not sick. Memory for recent events was in general poor. Errands easily forgotten. Lost in the street. Complaint of corpse odors round him. Everybody is looking at him and making fun of him. He was apt to insult bystanders. He was afraid of German spies. Things in shops angered him as they seemed to him to be of German manufacture.
There were frequent periods of depression, with pallor and no spontaneous speech for some hours to a half-day. Headaches coming on and stopping suddenly.
As to diagnosis, the first impression, say Pitres and Marchand, was that of general paresis. The progress of symptoms after the shock was consistent with this diagnosis. The mental state and the physical findings seemed consistent, although the pupils were normal. His partial insight into his symptoms was not inconsistent with the diagnosis. He had a characteristic self-confidence. There had been four stillbirths (two twins); two children are alive, 11 and 13. Typhoid fever at 30. Syphilis denied. No mental disease in the family.
The patient had never done military duty, having been invalided for “right apex.” But he had volunteered and been accepted in September, 1914.
How was Lieutenant R. cured? Apparently by rest in the Centre Neurologique. Pitres and Marchand do not speak of the subtle relation between mental state and the idea of non-return to military service. This motive might still work even if Lieutenant R. kept protesting sincerely that he wanted to go back into military service.
War strain; shell explosion; unconsciousness. Sensory and motor disorders. Subject an old syphilitic.
A captain, 34, was under much stress and strain in the field and gave himself over to excesses of alcohol and tobacco. August 25, 1914, at the Krasnik battle he suddenly saw at his right a gleam of fire and was afterward able to remember very distinctly the words of a lieutenant standing near by, “The man is dead.” Three or four hours later he came to himself at a relief post, vomited and bled a good deal from nose and mouth. He heard later that he had been thrown on his back.
Manual tremors and general pains developed in the next few days. Two weeks after the accident a slight nystagmus on looking to the left appeared, but there was otherwise no disorder of head or extremities. He was able to sit up, supported by his arms, and he was able to contract his abdominal muscles normally. As for his legs, active movements were limited and weak. He could not lift his legs. The paralysis was more marked distally. He could walk with the support of two persons, but was unable to lift his feet from the ground. The right upper abdominal reflex was elicited, and both patellar reflexes were tolerably active. Cremasteric and plantar reflexes were absent. Neither of the Achilles jerks could be produced. There was hypesthesia and hypalgesia of the lower extremities, and of the back up to a horizontal line corresponding with the ninth dorsal segment; thermo-hyperesthesia and disorder of vibration sense in the lower legs. Both the motor and the sensory disorders were more marked on the right than the left. Insomnia and battle dreams.
The gait disorder and paresis gradually improved. There was no alimentary glycosuria and adrenalin produced no mydriasis. In the course of several weeks the patient gained seven kilograms, began to sleep well and showed gradual[35] improvement in his gait and in the execution of various movements with his feet. The abdominal reflexes were now both present, but there were no plantar reflexes and the Achilles were still both absent. The sensory disorder remained unchanged, so far as the skin was concerned, but the deep sensibility improved. Both legs from the knee down were somewhat cold.
This man had had syphilis at twenty-two, had gone through an inunction cure, and repeated W. R.’s came through negative. He had suffered from vomiting spells and anxiety feelings for a number of years which had been diagnosed by physicians as cardiac neurosis. Yet for a year before going into the war he had felt absolutely well.
Shell-explosion: Amnesia; syphilitic hemiplegia. Recovery except for amnesia as to brief period and loss of occupational skill.
A man of 40 underwent shell shock June 15, 1915, and had no remembrance of what happened up to July, 1915, when in hospital at Tunis he felt “born again.”
Examined in January, 1916, it was found that he had a left hemiplegia (in fact, he had a syphilitic hemiplegia on that side, several years before, which had disappeared under antisyphilitic treatment). This hemiplegia passed, but he then had crises of depression due to his despair at not being able to know who he was and what he was doing. He could speak French and Spanish, and knew from the hospital ticket that he was born in Spain; but he had no idea what had happened to his relatives or what he was doing in France. He had, however, a very correct idea of what happened during six months after July, 1915.
One morning in April, 1916, his old memories came back all of a sudden on waking. The gap was filled up to the moment of the shock. There was no gap left except for a period of about 25 days following the shock. He now found that he knew a little English but that he had lost his stenography as well as his professional skill at typewriting.
Re French statistics for the occurrence of general paresis, Lautier found 27 cases in 426. Early in the war, Boucherot at Fleury received four cases of paresis among 107 cases; the majority of these, however, had not left the interior. Consiglio in Italy received two cases out of 270.
Re hemiplegia in this case, it may be inquired whether the hemiplegia which developed after the shell explosion on the same side of the body on which the patient had a true syphilitic hemiplegia, was really syphilitic or not. Was it not, perhaps, in some sense psychogenic? A similar question may be raised concerning cases in which the locus minoris resistentiae becomes the site of symptoms. See Cases 409-414.
Shell-shock: Hysterical blindness. Signs of cerebrospinal syphilis: Nevertheless, amaurosis functional.
A soldier of the class of 1906 underwent shell-shock August 13, 1914, regaining consciousness 20 days later, but blind. The light of the shellburst, he said, was the last thing he had seen.
For sixteen months, he was transferred from hospital to hospital, looked on sometimes as blinded; sometimes as feigning. Finally, on the isolation service of Maison-Blanche, December 15, 1915, he received an ophthalmologist’s diagnosis namely, hysterical amaurosis. At this time there were found: stereotyped winking, with slight lachrymation, a slight left external strabismus, limitation in movement of all the extrinsic muscles of both eyes, especially to the right and in convergence and elevation; pupils slightly smaller than normal—and the general impression of a genuinely blinded or amblyopic subject. He seemed to be able to distinguish faint whitish spots, without contour or color, in objects brought to a distance of at least 40 cm.
He also complained of bad feelings inside his head on the left side, and he proved to have a left-sided hemianesthesia of hysterical nature. There were no other sensory disorders and no reflex disorders.
The nasolabial fold on the left side was flattened out, and there was also on the same side a slight diminution in the lower abdominal skin reflexes, and no response to plantar stimulation. Examination of the mouth showed leucoplakia, and the history showed that the man’s fifth child was born before term and died at two months. Lumbar puncture yielded lymphocytosis (55 cells) and an excess of albumin. The fundus examination showed a slight papillary disorder, suggesting a retrobulbar affection of the optic nerves.
However, the preservation of the pupil reflexes seemed to indicate that nine-tenths, at least, of the amaurosis was[38] functional. After mercurial treatment the headache grew less and the man was able to see somewhat better with his right eye.
Laignel-Lavastine and Courbon suggest that there was a dynamic disorder in this case, bearing the same relation to vision as mental confusion bears to the process of ideation. Analogous phenomena have been found in the sense of hearing, in such wise that the victims can, as it were, passively hear but do not listen.
Re functional eye cases, see below, especially Cases 432-437.
Shell shock (functional) phenomena in a syphilitic.
A marine, 26, on land service March, 1916, was buried by the explosion of a large calibre shell which killed most of his comrades. He remained for a time in a sort of lethargy. Coming to, he found himself victim of a right hemiplegia and deafmutism, which phenomena vanished under electricity.
In July, however, he had to be sent to a hospital on account of his sufferings, which received the diagnoses commotio cerebri, disorder of consciousness, disorientation, delirium, amnesia, over-emotionality. He was sent back to the front in December, 1916, but promptly reported sick, with headaches and insomnia.
Examination showed nonorganic nervous disorders, consisting in a variable and patchy anesthesia of the legs, anesthesia of the conjunctiva and pharynx, and over-reaction, with sighing, during the course of the examination. The organic signs were: exaggeration of tendon reflexes, equilibration disorder, and incapacity to stand on one foot or execute a half turn or to stand still with eyes closed, and disorder of position sense. The lumbar puncture showed no cells, a slight globulin reaction, and an albumin titer within the normal. There was a leucoplakia and a positive W. R. The man was emaciated, febrile, and showed signs, with the X-ray, of bronchial lymph node disease. According to Babonneix and David, the normality of the fluid indicates that the phenomena here were Shell-shock phenomena, despite the indisputable syphilis of the blood serum.
Re occurrence of functional phenomena in syphilitics, Freud’s remark may be recalled to the effect that a large proportion of his hysterics and other psychoneurotics are the offspring of syphilitics.
Consider in this connection also Case 28: an old syphilitic hemiplegia was followed by a probably psychogenic or hysterical hemiplegia on the same side.
Vestibular symptoms in a neurosyphilitic.
A soldier, Colonial, 29, was twice in the 6th Army neurological centre. The first time, February, 1916, he was under observation for astasia-abasia, having been invalided twice for this disease,—once in 1915. This man had had syphilis at 21, and was then taken care of at Saint-Louis Hospital and at Cochin. A volunteer for the duration of war, September, 1914, he had intermittent disorders of station and walking, which caused his invaliding January, 1915. As the trouble stopped, he asked to go back to the front in September, but the same difficulty reappeared with fatigue, and he was sent to the army neurological centre. When standing, there was a ceaseless trembling of the whole body but especially of the legs, with tendency to propulsion. In walking also, there was a trepidant abasia, sometimes dizziness, and even a sudden fall. Standing on one foot he trembled and fell.
Examined on his back, muscular strength was found intact in all limbs, and there was no trembling or incoördination or intention tremor in the performance of any movements, though there was a slight trembling of the raised fingers and hand. Reflexes were normal. The right pupil was dilated; the left pupil reacted sluggishly. There were lateral nystagmiform movements to the left. Caloric nystagmus appeared from the right ear in 15 seconds, from the left in 30. Rotatory nystagmus appeared in 35 seconds on both sides. Lumbar puncture yielded a fluid with a slight lymphocytosis; albumin, .3 grams; chloride, 7.30; sugar normal.
Rest in bed improved the astasia-abasia, and the man was sent back to his corps, February 20, 1916. He came back March 16, having had a dizzy spell, with suffocation feeling and a fall, whereupon the trepidant astasia-abasia had reappeared. There were none of the so-called defensive reflexes. The neuromuscular excitability of gastrocnemii was less on the right than on the left. A von Graefe sign was sometimes found; no diplopia save on looking far to right.
Lay reflections on syphilis: Suicidal attempts.
A man was called to the auxiliaries at the outbreak of the war, and served as stretcher-bearer at the Marne. He then became an attendant at the Grand-Palais. Acquiring gonorrhoea, he was cared for but he grew depressed. The blood was examined and the W. R. found positive. The physician immediately made known the result without circumlocution, and knowing vaguely that the W. R. meant syphilis, the patient felt an irresistible impulse to suicide, and cut his throat. It seems that he had often before said that if he got syphilis he would kill himself. Recovering from his wound, he was invalided to Villejuif, Sept. 19, 1916, breathing through a cannula and responding to questions in writing. He had always been a nervous and emotional man, a farmer in Auvergne; he was married and the father of several children.
Examination showed that the recurrent nerves had been cut and that the man must needs always breathe through the cannula. In point of fact, the W. R., only partially positive at the outset, did not indicate syphilis, and the gonorrhoea was now cured. But though the patient knew these facts, his hypochondria persisted, basing itself upon the suicidal wound. He said that his larynx had been stolen and he wondered why. He said that he had violent crises of suffocation, though there was, as a matter of fact, no difficulty with his breathing. Verdigris, he said, was forming on his cannula. Self-accusations about the suicide developed. On being transferred to his department asylum, he made a suicidal attempt on the trip.
Of course the gonorrhoea may have served as a partial factor in the genesis of the case, and his own mental attitude toward the contraction of syphilis may have been another factor.
The imitation of chancre.
A married German farmer, 32, was in Prague hospital in 1908 during his period of military service and was then treated by inunction for a local chancre. He was given mercurial injections a year later for rash.
In 1912, he had signs of syphilis in the mouth.
He was sent home from service in 1913, with ulcers of hand.
At the beginning of the war he was found to have ulcers on the knee, legs, and mouth, and was sent home for six months.
Again called up in 1915, the ulcers were still in evidence; he got inunctions in a military hospital four months.
He was sent to his corps in July and had no relapse until July, 1916, when he was detailed for active service. Thereupon, ulcers began on the left hand and right leg. He reported sick, but was sent nevertheless to the front. In hospital he was found to have several scars about one inch across on each leg, on the dorsum of the left hand, at the right of the left index finger, and elsewhere. These scars were deeply pigmented. One of them was square! There were other recent ulcers that closely resembled tertiary ulcers. The most recent of these ulcers was angular, intensely red, and showed remains of a collapsed vesicle. There was a deep dark scab on the mucous membrane of the left cheek.
There is no doubt that these ulcers were produced by some caustic, the nature of which remains unknown. The patient had, however, been able to evade military obligation during peace time and for two years during war time.
Re simulation, according to Pick, some 5 to 7 per cent venereal diseases in the German army have been simulations. Gonorrhoea is simulated by soap, balanitis by cantharides, soft chancre by soap and mercuric or mercurous chloride mixed, hard chancre by a fluid or powder containing NaOH, Na2CO, and NaCl. Secondary syphilitic signs are imitated by cantharides or garlic, producing scrotal dermatitis. Tertiaries are imitated with caustics.
Ramón to Rosina: a soldier’s letter to his fiancée.
“I am here to stay a month. Believe me, it is better here than in the army. There is a rule that we may eat as much as we can and everything is of the very best. The servants treat us like brothers. Do not think it is a nuisance to be inside four walls with a wee bit of a garden. No, indeed! But I have got to act the fool and from the very first day I began to play and act crazy with a kitten, so that if you had seen me you would say: “Ramón is really crazy.” Rosina, dear, to avoid paying taxes you have got to be a smuggler. And now that I am at the ball I have got to dance. I want to see if after all the suffering I cannot get something better. I am better off here than at the regiment. I sleep in a fine warm bed, and they have only cold straw; I have good food and drink and plenty of milk, and they have poor food and drink and so little.
“I expect to go home in about three weeks. I would have been there before if some fool of a spy at our place had held his tongue and minded his own business. At the same time, Rosina, dear, remember what I told you at Leghorn: that they had some officers sent there to get information and instead of going home they asked somebody else and were told that I had never been sick and had never had neurasthenia. When this information was got from the officers I was called to the office and they read to me that all that I had said and done was not true. I kept on acting the fool, and as they were still doubtful they sent me here, where there is a professor who passes me every morning in the garden and says: “How are you?” I always say: “I am the same,” acting like a crazy man. Let me tell you, Rosina dear, not to say anything contrary to this in your letters because they open and read everything in order to find out everything that happens and everything that is said. Now what you must do is to ask me how I am feeling, and whether my headaches are gone, and whether I have them all the time as formerly, and any other trifle that will help me.”
Rosina’s fiancé had a strongly positive W. R. in the serum. It was negative in the fluid. He was returned to the front.
Moron of use at front (alienist’s report).
Vigouroux reports concerning a tanner of 19 who could not read, write or calculate (3 plus 8 equals 14) and had been of the 1916 class in an infantry regiment at Brest, on the occasion of his asking to be sent to the front more speedily:
Mental weakness, with insufficient school and theoretical knowledge but with the ability to assimilate practical ideas, though not knowing how to read, write or calculate; seems to have earned his living in several lines.[45] “As a soldier, he does not know the insignia of the different ranks but understands how to obey a superior officer. Understands a gun and can tell a chargeur from a Le Bel gun. Moreover he seems to be perfectly stable, fixed in his wishes, persistently and intelligently wants to go to the front and kill Boches. He appears to be well disciplined and educable. Although feebleminded, he appears to us able to be useful at the front, though he should not be employed in any undertaking requiring initiative or foresight.”
An imbecile, superbrave.
A loquacious, active fellow, 22, with very slight school knowledge and no idea of military ranks (treated his superiors like his comrades), was often punished in the barracks. He did not get on well with his instructors. His activities were never interrupted by any obstacles or by derision. He kept singing and talking enthusiastically during the mobilization. He was the butt of his section.
At Dinant he did very well; though his section was losing a good many men he remained calm. He was careless of danger and remained at his post firing ceaselessly at the enemy and giving a magnificent example to the few comrades who remained with him. In fact, he remained so long in his shelter that he was surrounded and taken prisoner. He escaped, swam the Meuse and got back to his regiment.
An imbecile of service in barracks work.
A farmer, 36 (father alcoholic, mother always sick, two brothers at the front; patient had typhoid at an unknown age; had gone to school at 13 but “learned nothing”; worked in fields with his brother who gave him some pennies on Sunday), was put into the auxiliary service by the Council at 20. Patient said he was not strong enough for this service. In 1914 the Council reconsidered the case and put him into a regiment of infantry. He could not be given military instruction or execute the most simple drilling manual. He said that 4 plus 2 equalled 7; 4 plus 3 equalled 5. He was of an excellent character, very docile and easily directed. He did all his comrades’ barracks work and was very proud because, as he said, “I do everything they tell me to do.” He was happy in working, everybody was good to him, but he had no comrades. He had no general knowledge and knew nothing about the war but that they were fighting the Boche.
Re imbeciles, Colin, Lautier and Magnac found amongst 1000 soldiers entering Villejuif, 53 imbeciles. Twenty-four of them had been either exempt or retired at the outset of the war, when military surgeons had reviewed them and considered them fit for service. Several of the 29 others also had shown previous evidence of imbecility.
Of course, French military surgeons may have felt that a number of these men would be of just such service in barracks and otherwise as Case 37 (Pruvost). But for one or two cases like Cases 37 and 41 of Pruvost, there are great numbers of other imbeciles who prove quite useless in the army. Two of the Villejuif cases had been volunteers: one volunteer declared that, if he had been intelligent, he never would have enlisted! Ten cases proved unable to use a gun; one turned his gun upon his mates. One regularly forgot the password. One (see Case 42 of Lautier) thought the war too long and tried to take command of the company in order to finish the war one way or the other. Three of the imbeciles had to be evacuated for desertion (unmotivated fugues); two of them cursed their officers. Some of the imbeciles had an emotional diarrhoea throughout their service.
Colin suggests that line officers and military surgeons ought to agree that these men are not fit for service, and that the civil authorities of the home towns should advise the review boards about known imbeciles and criminals. In point of fact, previous knowledge of imbecility could have been obtained quite readily in 27 of the 53 cases observed by Colin.
A feeble-minded inventor.
A jockey of Nîmes, 31, entered the service May 15, 1917. He retired before the war. He was in the auxiliaries at the moment of mobilization. Nothing is known as to any pathological episodes in his past. He said he had been a poor scholar, had left the primary school at eleven hardly knowing how to write or spell, but he had a lively imagination and was a happy-go-lucky youth, playing many tricks on the trades people. He tried a variety of ideas in the industrial or commercial world with very varying success. He had a mechanical taste. The Colonial Exposition at Marseilles caused him to float a variety of projects, from that of having the visitors photographed on a camel to the sale of lemonade. He said he had been a jockey and then a trainer and had finally become a valet de jockey at Maisons Laffitte. He was a gambler and invented a “system.” He made various inventions in relation to horses. At the end of 1914 he had plans for a bomb thrower and placed his discovery at the service of the War Minister. He was not discouraged by the lack of success of the bomb thrower. He now made an aerial torpedo carrier. He had the idea of the tanks. However, he found the secret of his torpedo carrier printed in a magazine. There was a slight difference between the German apparatus and his own.
From this time he began to be mistrustful, and now he jealously avoided entering into any details about his inventions and he did not let his officers see his plans. The Commandant offered to give a place in the safe to his documents, but he could not embrace the offer. He now invented a counter-torpedo machine. He went on leave to Paris, asked an audience of the Minister of Marine, who put him in relation to the Committee on Inventions, who put him off, desiring that he should forward all his plans. He emerged from one of his interviews so excited that there was a scandal on the public street and the police commissary evacuated him to Val-de-Grâce, but the patient says he does not remember[48] this incident. He came on service of Laignel-Lavastine May 15. He shortly wrote again to the Minister, who again referred him to the Committee on Inventions. He protested to the President of the Republic and wrote directly to the King of England, who referred him to the Military Administration. He is now occupied in creating a machine to destroy the first line trenches and continues to write to the Ministry. He has documents buried underground in a secret place. He still talks with great vivacity of his discoveries.
According to Laignel-Lavastine, we deal with a feeble-minded person who has for many years had a délire raisonnant of the inventing group.
Re feeblemindedness in the British Army, Shuttleworth found 70 who had joined from special schools for the feeble-minded in London, and 100 from Birmingham in the year 1915. The institutional “children” were in general good at drilling and obeying. One of them, given to lying and stealing, got into constant trouble in Flanders.
Sir George Savage stated that he had sometimes run the risk of allowing enlistment of men who had shown earlier in life a weakness for lying and pilfering, and remarked that such men might make good soldiers. A case like the above (38) would run counter to this view. On this matter, see below Case 183 (Henderson), one of pathological lying.
An imbecile who walked lame.
A soldier, 20, eight days after being called to the colors, complained of pain in the knee and hip. He was observed for 18 days in hospital and then sent back to his company; but he continued to complain of the pains, and the regimental surgeon sent him to a neurological center where the joints were found to be normal and where no sensory, motor or reflex disorders were in evidence. The man continued to walk lame and insisted he could not get about without a cane. He also complained of his mouth and his belly and, though he was very ruddy, said he was á bout de forces.
It was a question of simulation. The man, however, was a feebleminded person who could not read, write or calculate. He was invalided as such.
Enlistment to improve character.
A village boy had passed for simple ever since typhoid fever at 8. He had learned to read and write, but had always been impulsive and subject to fugues, running to see his grandmother, or off as a truant. It was decided that he, at 19, should enlist to improve his character. But one fine day, even before the war, he deserted. He said, in explanation, that he had lost his way, and he was being examined mentally when mobilization began.
He looked ape-like, with spread ears; had a low forehead, a head flattened behind, an asymmetrical face, prognathous jaws, an arched palate, and defective teeth. He talked freely of homosexual relations, and said he wandered off because it occurred to him to do so. He was determined to be unfit for service.
An imbecile who may be sent to the front.
A Parisian sandwichman, 25, of unknown parentage and a state ward, placed out with a farmer at 12, escaping with a friend to Bordeaux at 14, thence leading a wild, improvident life at Lyons, Marseilles and Paris, sleeping in fields and hedges, earning 22 sous a day but in no case mixing with the police, was examined for physical inefficiency at 20 years. He wanted to enlist but was refused. He insisted and was very proud of the fact that he got in as the Major said to them, “Let him go in.” He could hardly read, write or calculate but was by reason of his adventurous life full of practical resources. He was irascible and frequently crimed, whereupon he would cry under the Captain’s window, “Robber band, idiots, I shall write to the Minister.” He was passionately fond of military life, though he had but the vaguest notions about the commands, the names of generals and the like. He wanted to drill. His comrades played practical jokes upon him asking him to look for a trajectory, for the squad’s umbrella and the key to the drill ground. They also told him he had been proposed to be corporal, whereupon he was greatly overjoyed and immediately sewed stripes on his sleeve and began to give commands. He said if they put him among the auxiliaries he would throw the adjutant in the water. He sang and swung his gun with joy when he went to the front. He thought there were stripes hanging to the barbed wire and wanted to pick as many as possible. Such a man may be safely sent to the front although he will bear watching. At the date of report this man had been at the front two months doing very well.
Re the comparative success of the Germans in the matter of excluding imbeciles, Meyer found that 8 per cent of the mental cases in the army were cases of mental defect.
Imbecile with sudden initiative.
A soldier, 41, a farmer, from the Department of the Marne, married, childless, was called to the colors August 31, 1914. He was on guard duty until May, 1915, watched prisoners until October and was finally sent to the front, February, 1916, where he fell sick.
“He was tired in his head.” “His commanding officer made him drill without rhyme or reason; he would have been able himself to have commanded with greater intelligence.” He once attempted to put himself at the head of the company to lead them against the Boche; this idea arrived to him all of a sudden in a phase of perfect confidence and sang froid. He thought his comrades would follow him and that the officers would do likewise. He hoped thus to be able to end the war one way or the other. He was getting tired of the war and regretted his family life and kept saying that this was no existence for family men. “We ought to attack or ask for peace.” No one followed him and his comrades said he was un peu fou but he did not share this opinion.
In point of fact he hardly knew how to read or write and at home lived with his relatives, submitting himself entirely to their guidance. He was much afraid of being punished and often feared that he had done badly as he had trop de conscience. He was non-alcoholic and without hereditary or acquired neuropathic taint. He had no pronounced stigmata of degeneration. He was rather reticent about certain mystical ideas of a political tinge. At Villejuif, whither he was brought February 17, 1916, he received a diagnosis of imbecility.
Emotional fugue in a subnormal subject.
A soldier in the Territorial Army, 40, appeared before the examining board in a depressed, dejected-looking state, speaking slowly but collectedly and lucidly. Mobilized the second day, this man was much afraid that he could not get through the marches, and asked for a special examination to determine whether his feet did not make him unsuitable for fatigue. Two physicians thought he was unsuitable for marching, and another thought he put it on. A trial march was not executed well. He was kept in barracks but jumped the wall, put on civilian clothes, and made off for Paris. But a relative, warned by his wife, finally got him to go to the authorities. He was told that he ought to return in the afternoon, when suddenly he was arrested.
It seems that the man relied on the opinion of the two physicians and discounted that of the third. He thought himself the victim of an injustice, and not knowing how to get on, it occurred to him that he would abandon the regiment and get out of the difficulty. It was without resistance, however, that he gave himself up as a prisoner. This fugue was neither unconscious nor amnestic, nor was it due to an irresistible impulse; nor can we say that it was due to a genuine intellectual disorder. It was an emotional fugue, and partly due to the man’s long-standing depression. It seems that he had inherited this character from his father. He was below normal intelligence, had a very poor education, lost his wife, and grew more and more sombre. He married again, but this time a neuropath. He began to be preoccupied with his health and he had even some ideas of suicide. At the time of his leaving the regiment, he had passed through a phase of depression of about 6 months’ duration, and at this time had a number of hypochondriacal ideas with poor appetite and loss of weight.
Diagnostic dispute between regimental surgeon and alienist.
Julius Q. was sent on guard April 14, 1915, with orders to remain there. While on guard he made a noise and made a movement as if to take a knife from his pocket. Ordered to empty his pockets, he attacked the other guards. The witnesses said that he was drunk.
Upon examination, it appeared that he had recognized and called by name those present in the guardhouse, despite his supposed intoxication. There were red spots on the skin and a certain amount of analgesia. His powers of computation and reasoning were poor. He was unable to explain the meaning of a picture shown him. He maintained that he had an indomitable desire for drink. A diagnostic draught of alcohol yielded no reaction. Upon dismissal, he got drunk at once again, and had again to be imprisoned in a state of excitement. What the outcome in this case was is not stated by Kastan.
The previous history seems important. Julius Q. had been a state ward. He had escaped several times from the institution but had always to be brought back again because he could not be trained at home. He had once attacked a supervisor in the state institution with a knife. It seems that he had at this time been drunk, having been brought back drunk to the institution.
Two years before the war he had been taken to the Breslau Hospital for the Insane on account of fits of insanity. In 1913 he had been a patient in Wuhlgarten on similar grounds. The diagnosis there had been epileptoid degeneration, psychopathic constitution, imbecility, or epilepsy(?). He had been convicted of crimes a number of times and put to labor. He had been given to cruelty in childhood.
Despite this, he was declared perfectly healthy in mind and body by the regimental surgeon.
In 1914, Q. fell suddenly ill in prison (he was presumably in prison for a military offence), and smeared the cell with feces, saying that he was able to do that as he could pay for anything. He stared at the floor and failed to answer questions. He remarked, however, that he had frequently been convicted for breach of the peace and assault and battery, and he said his father had been a drunkard, and he acknowledged hallucinations to the extent of saying that he heard his name called when he was alone.
The story of this case warrants our inquiring why such a patient was kept in the army. He was kept there clearly on account of the report of the regimental surgeon, who could not have taken seriously the previous history of the case, or else thought the patient perfectly good cannon fodder.
The hypothesis of syphilis apparently need not be entertained. That of feeblemindedness is possibly the fundamental diagnosis, yet epilepsy was considered by the German diagnosticians, doubtless on account of the sudden violent attacks and breaches of peace on the part of the patient. There is clearly something behind mere alcoholism in the entire story of this state ward. On the whole, the periodicity of the attacks is equally consistent with the picture presented by numerous feeble-minded persons, and the institutions that had to deal with Q. regarded him rather as epileptoid. There seems to be evidence of actual intellectual defect. Accordingly it seems wiser to consider the case of Julius Q. one of feeblemindedness, possibly of the moron group. We should then consider the epileptoid features as part and parcel of the feeblemindedness. We should consider the intellectual defect a part of the process; and the uncontrollable impulse to drink, the sudden violent attacks, and the cruelty in childhood would then be regarded as merely symptomatic of the feeblemindedness. It seems clear that either mental tests by the regimental surgeon or an examination of the patient’s previous history would tend to exclude such a patient from the army.
How can a rifleman be an imbecile?
Anton K. was down in the list as “missing.” He was found at home. He said his feet had become sore from the marching. He had lain down and become unconscious. Coming to his senses, he was possessed only of trousers and a shirt but he got a civilian suit in a village. He had gone home part way by train, part way on foot. It seems that he did not tell his father any details about his coming back although he expressly denied deserting.
It seems no mental weakness had been noticed in the army. It had been observed, however, that after seeing the first corpses he was deeply impressed and did not want to see any more. On examination in the hospital he gave the impression of indifference and low spirits. He had to be urged to eat and work. No great amount of intelligence defect could be determined, though his knowledge and capacity were below the average. The physician examining him thought his depression was either caused by or increased by his imprisonment; but this examiner thought that the protection of Section 51 did not extend to the patient at the time of his desertion. The examiner thought that an examination by a psychiatrist was not necessary, though both judge and prosecutor urged it.
When examined in the clinic, he seemed to be disoriented for time. He claimed to have been able to stand the shooting and the sight of the corpses. After becoming unconscious, he had wakened and eaten cucumbers and carrots in the fields, wandering on for a period of three or four weeks, until he came to a place where he had formerly worked. The reason he had thrown away his uniform was because Russians had been about. He had not known that it was his duty to report to the army again.
It was found that the patient’s father was poorly developed as to mind, that his brother was subject to periodic mental disturbance so that he had to be watched. It was found also that K. himself had had a similar mental disturbance,[56] lasting a week, two years before. Moreover he was not considered mentally right in his home town. In fact, no one there wondered really at his desertion because he was so stupid. His school work had been poor and limited.
He himself said that his people were of sound mind; that during school days he had felt bad in his head, once running into the woods after being told something. He was able to give the names of his former superiors. His calculations were only partly correct. He was poor at reasoning and at simple distinctions; for example, asked the difference between a bird and a butterfly, he replied that a butterfly was a bird too. He did not know the difference between a river and a lake. He thought Russia, England, and Austria were the enemies of Germany.
He sat about or lay on the floor, motionless and indifferent, with a newspaper stuffed into his trousers, unoccupied although saying that he wanted to work, and even allowing his fingers to be burned by cigarettes he was smoking.
He was tried once more and the first medical expert still adhered to his former opinion, pointing out that K. was a rifleman and that only an intelligent man could be a rifleman. The court, however, accepted Kastan’s opinion and granted K. the protection of Section 51.
In comment upon this case, it seems clear that ever so slight a knowledge of K’s home town reputation would have naturally excluded him from the army. However, what is to be said “when doctors disagree,” as noted by Kastan in this very case? It seems impossible, also, that his comrades should not have noticed something odd about him (over and above the deep impression on seeing the first dead) which might have given occasion to the regimental surgeon for a special mental examination. However, to the military mind, mayhap the man seemed to be sufficiently “effective.”
Re imbecility in a rifleman, the compiler has studied somewhat elaborately the brain of a feeble-minded murderer with some North American Indian blood in him. This man was a crack shot despite his subnormality. It would seem that the German regimental surgeons castigated by Kastan as above were very properly so castigated.
Hypomania in an imbecile.
A brusque little man, of a somewhat bold and talkative disposition, though giving a good first impression, was evidently a bit feebleminded, though (as Haury says) of the active group. He had a sister like himself, whose children were taken care of by the State, and at home he had had a number of fugues, about which details were lacking. It was soon evident what sort of soldier he would make, and he was put in one of the Territorial regiments, but it was not noted that he had a genuine mental disorder, as he was thought to be just a peculiar person.
His new relations caused him to do a number of eccentric things. He shortly proved to be in a sort of rudimentary maniacal state; talkative, restless, scheming rather feebly to go back to his village. He said that he couldn’t walk on account of corns, and that these corns required a certain drug, which he wanted to get from home. He said that he had been struck by lightning twice; that he had fires in his body, etc. He wanted only to be retired on a pension of one or two hundred francs so he could take care of his farm, his hay and his fields. There was no need of trying to get land by means of bullets, he said, since he had enough.
The mental disorder of this man was much deeper than appeared, and in fact, he did a number of dangerous things compromising the security of the entire regiment.
Re the dangerous tendencies of Case 46, see the remarks above drawn from Colin, under Case 37.
Insubordinate desire to remain at the front.
Friedrich L., on March 4, 1915, was ordered to go back to the baggage-train. He did not obey. He said to the non-commissioned officer who then came to him, “I am not going; you have nothing to say anyhow, you ox-tender!” He stood with his hands in his pockets, and, when the officer seized him angrily by the collar, L. struck the officer’s face.
He stated at his hearing that no one had the right to send him back. At that time even he conveyed the impression of being not quite normal and was let off with his arrest only. Later he refused again to go on guard duty, saying, “You have nothing to say at all. Perhaps you will find out that we shall meet each other again in hell tomorrow morning.” He was taken before the physician, who considered him mentally inferior and not entirely appreciative of the nature of his acts. He was told that the death penalty would meet such behavior, whereupon he remarked, “I am not afraid of the death penalty,” staring excitedly at the officer and trembling throughout his body. It seems that he had already made an impression of mental inferiority in the troop, and had once before said to an officer who wanted to send him to the front, that he would not go; this had been regarded as almost a breach of discipline. He had been in the habit of not reacting to the calls of his superiors, and had smiled at their reproaches. He seemed to hold the opinion that not even a company commander had power to order him to go back. Examined in the clinic he held to the same opinion, that there was no need of his going back; that they took volunteers; and that he wanted to remain at the front. On the day of the deed, he had drunk a rye whiskey. He had shaken off the non-commissioned officer because the leader had seized him by the throat. In the clinic he often smiled and wrinkled his forehead. He gave evasive and inadequate answers. Asked about oaths and perjury, he remarked,[59] “I prefer to remain silent.”
He said that one of his sisters was a little stupid. Study of his previous history indicates that Friedrich L. had formerly been a quiet and steady man, although he often had attacks of rage, breaking out upon sudden excitements. As to his capacity in school, nothing could be learned, since the Russians had taken the school registers away.
The analysis of this case seems to reduce to the question of feeblemindedness and schizophrenia, unless some form of inborn qualitative inferiority of mind be preferred as the diagnosis. On the whole, possibly, the diagnosis of feeblemindedness seems preferable. The entire symptom picture seems to relate to the patient’s one mental attitude about sticking at the front, ruat coelum.
A French soldier who admired Germans.
A man with the extraordinary first name of Agapithe (Laurent insists on the frequency of strange first names in degenerate families) came from Val-de-Grâce to Villejuif June 5, 1916, with the diagnosis of mental weakness, interpretative ideas of persecution, mental excitement, recrimination, logorrhoea, and a tendency to revengeful reactions.
On arrival the patient said he must be in an insane asylum because he heard spiritiques talking together. He, however, was “not insane” and began expounding his plans for revenge with the words “Kill,” “Cut-throat.”
This man had been placed in the auxiliary service by the Council, called to the colors December 13, 1914, and finally sent to the front in May, 1915. In July he was made prisoner in a brush. He said, “I cried out, ‘Comrades, what difference does it make to me whether I am German or French? My officers are imbeciles that drink the blood of us unlucky ones!’” He was interned in some camp whose name he could not exactly give and reported that the Germans were very gentle with him, that his real enemies were the French, for the French were against him night and day. “As a matter of fact, among Germans the French are nothing but cochons malades. The Germans are fine types.”
He was repatriated in May, 1916. He kept making verbose and neologistic eulogia of the Germans. He had been a farm boy in Brittany, where he had had headaches. He had been at Quimper Asylum in 1910. In fact, he said his parents had tried to poison him and to have him assassinated; they had charged him with setting fire to their house. His mother was an imbecile, he said, who believed she was the Queen of France. His recriminations did not stop short of himself. He had been accused of kissing a girl and stealing apples; as a matter of fact he knew what to do with girls.
He had a coarse face and a number of stigmata besides his name Agapithe. He was kept at Villejuif as an imbecile.
Unfit for service: Question of feeblemindedness.
Walter N. was declared unfit for military service in 1912, on the ground of mental incapacity. He had shown this clearly during his period of training. He committed a number of slight offences secretly, but not so secretly but that they were immediately discovered and punishment meted out therefor. He could do nothing without aid. It appears that his mental weakness had not been noticed in school, but that his employers had thought him both feebleminded and irresponsible. Nevertheless he always executed orders properly. While in hospital in 1912, he had occupied himself very little, sitting indifferently, quiet and dreaming. At that time, he had shown poor calculating ability and decreased power of perception. It also appears that he did not grasp the nature of simple orders, the requisite associations being disturbed.
Despite this history, on September 11, 1914, he found himself being transported. He claimed to be very tired. Upon reaching the city, he picked up a large stone and raised his arm as if to strike the transport leader. While N. was being bound by the transport leader in consequence, he kicked at his leader’s shins.
In the clinic he resisted examination, moving his legs without speaking, staring at the floor, moaning frequently, sitting motionless with head hanging, answering monotonously repeated questions, but turning his head at a loud noise. He felt ill. It appeared that he was oriented and that his knowledge was well preserved although his calculation ability was poor.
It would seem that psychiatric examination, possibly with the aid of psychological work, would have excluded Walter N. from the army.
Oniric delirium (Régis) in a somewhat feebleminded Esthonian.
An Esthonian, 21, a soldier in a reserve regiment, came to a psychiatric section towards the close of 1914. He was negativistic, mumbling, restless, fugacious; later more tranquil. One day he entered the physician’s office, walking up and down, mute, looking at articles and attempting to take them away.
February 21, 1915, he was evacuated to the Notre Dame Hospital for the insane at Petrograd,—a tall, healthy, agitated-looking youth with a rapid pulse. He explained in poor Russian how he was now among Germans and feared that they were going to hurt him. At first in the hospital he was seclusive and morose. March 9 he became excited, and tried to break through the door. He was placed in the bath, agitated and yelling. An Esthonian interpreter did not quiet him. The Germans were going to make a martyr of him. After an hour of this he grew quieter, and next day complained only of head weakness and malaise, was in good humour, smiling, and reading an Esthonian paper, and well behaved in church, though tired and pale.
He now got better, began to work and wrote letters. It seemed as if he had waked up from a painful dream. He explained how he thought he had been in captivity; that he was going to be hanged. He had thought that the Germans could talk Russian. He had had hard work in his regiment, as he did not understand Russian and had never before left his little village in Livonia. His mental disorder had started in the autumn, but all that was now like a dream. He said that he had had a mental disorder of short duration following some bodily disease, at the age of thirteen. According to Soukhanoff, this is a case of Meynert’s amentia, in a somewhat feebleminded person. The twilight state might well receive (according to Soukhanoff) the term “oniric delirium” invented by Régis.
Shell-shock; burial: Incapacity to rationalize the situation.
A soldier, 39, a herdsman, was shell-shocked at Hill 304 May 23, 1916, buried twice, slightly wounded in right eye, and carried unconscious to Bar-le-Duc. He was then forty days in a semi-confusional state with headaches and dreams of the Boches wanting to behead him. Some of these dreams came in the waking state, in which state he could recognize them as imaginary. In April, 1917, he said he had always been afraid, even in daytime, that he would be hurt and had been especially troubled by the fear of shells. He was also bothered by nocturnal enuresis which might become an incurable disease and bring impairment of memory and attention. Although not feebleminded the man was of but moderate intelligence, and his emotions, according to Duprat, were such as to defeat any complete resolution of his plight by the intellect.
An affective complex, passing from the surprise of the shell-shock over to a fright based on clear though wrong ideas of what might happen to him, had left him without sufficient power of autocritique.
Weakling, twice buried by shell explosions in one day: Change of character; fear; three fugues (“It is stronger than I am”).
An infantryman, Class of 1913, at the front from September, 1914, had a somewhat infantile build physically but was intellectually of average powers, having been a type-setter (three years in a job). However, the confined life had borne hard upon him and his father put him on a farm. He passed through his military service successfully, though he was given two weeks in the guardhouse for overstaying Easter leave. He was suggestible enough at this time to think that he would not be punished very severely, since there were other men whose leaves did not expire at the same time as his own.
He was buried twice in the same morning, March, 1915, at Bois Le Prêtre, spent four or five days in hospital, and went back to his battalion. But now there was a change in his character. Formerly indifferent to danger, he was now apprehensive every time he went to the line and felt an almost irresistible impulse to make for the rear. He was condemned to five years in prison, June, 1915, but was finally sent back to the front.
However, in July he left his company a second time as it was going into the trenches, and this time the captain simply asked him to do better. A third fugue, a few weeks later, sent him back to court-martial, and thence to be examined by alienists. He was perfectly conscious at the time of the fugues and understood his duties and possible punishments. All he would say was, “It is stronger than I am.” Fear outweighed every consideration after the episode of the shell burials.
The man may be regarded as a hypobulic, somewhat feebleminded person, able to get on in civil life but thrown out of gear by war. Of course, the concept of fear as a disease can easily be overdone; however, here was a case in which three desertions occurred; the third after severe punishment. In the differential diagnosis, epilepsy, alcoholism, impulsive poriomania, must be considered, as well as feeblemindedness.
Diagnosis “epilepsy” revised to neurosyphilis.
A Scotch soldier, in the Royal Navy, 43, was admitted to the Royal Victoria Hospital at Netley, as major epilepsy. He had been 12 years a stoker, and 16 years before admission had suffered from syphilis, a chancre locally treated with black wash, without secondary rash.
After leaving the Navy, he had worked in a fire-brigade and as dock laborer. He had been very alcoholic when funds permitted, although never “primed.” His first convulsive seizures came at 40, while working at the docks, following a night on which he had drunk a bottle of whiskey. He thought he had been about half an hour in the fit.
He joined the A. S. C., January, 1915; served in France; later at Salonica. He had eight convulsive seizures, some in France, and others at Salonica, always after much rum.
The man was tall, powerfully built, without visceral disease, speech defect, or other symptoms except that both pupils showed the typical Argyll-Robertson phenomenon. The deep reflexes of arms and lower legs were increased. The superficial reflexes were diminished, and the Wassermann reaction strongly positive. A seizure was observed by Hewat and the diagnosis of major epilepsy was revised. The diagnosis of cerebrospinal syphilis, non-paretic, was preferred to that of paresis on account of the absence of all the ordinary symptoms of paresis and of tremor. It might be asked whether these fits were chiefly alcoholic in origin. However, the patient had two or three fits while in hospital during a period of eight teetotal weeks. Hewat remarks that the case suggests that the serum of any patient developing epileptiform seizures for the first time say between 35 and 50 years of age, should be given the Wassermann test.
Syphilis may bring out epilepsy in a subject having taint.
A man of 35 in the Landwehr acquired syphilis some time in the summer of 1914. He was a good soldier, passed through several clashes, and was promoted to Unteroffizier.
To understand what followed it must be stated that he had been a bed-wetter to 11, had been practically a teetotaler (Bonhoeffer’s point is perhaps that otherwise epilepsy might have developed sooner?), and, when he did drink, vomited almost at once, and had amnesia for the period of drunkenness. His father drank. His sister had fits as a child.
February, 1915, the Unteroffizier lost appetite, got headaches, and went to hospital for a time. Upon getting better, he was sent on service to Berlin. In a Berlin hotel he had his first convulsions and unconsciousness, biting his tongue. He was confused for several days, and, when he had become clear, had a pronounced retrograde amnesia together with a tendency to fabricate a filling of events for the lost period.
This retrograde amnesia is uncommon in epilepsy and suggests organic disease. No sign of such was found, or signs of the epileptic make-up. The serum W. R. was negative. On the whole, Bonhoeffer regards the epilepsy as “reactive” to the syphilis, as a syphilogenic epilepsy.
Alcoholism caused amnesia in this man in the same way as the syphilitic epilepsy now did.
Re epilepsy and syphilis, Bonhoeffer states that he has repeatedly seen syphilis giving no other symptoms than epilepsy develop in the campaign. At the same time, Bonhoeffer does not find that the incubation period in paresis can be shortened by war factors; at all events, by the exhaustion factor in war (see Case 25). It might be questioned whether the above case (54) was not psychogenic; that is, whether the syphilis did not act in combination with being sent to Berlin on service as a psychic factor. However, this epilepsy on the whole seemed not psychogenic.
Syphilis in a psychopathic subject. Convulsions 5 days after Dixmude.
A soldier in the reserves, 23, was, subsequently to his being brought to hospital, described by his wife as a rather over-sensitive fellow, who could hardly look at blood and was meticulous about the household. He had always been subject to headaches, especially after hard work. However, he had passed through his military training well in 1910, not even having been bestraft.
He began service in October and fought at Dixmude on the 19th. On the 24th in the trench and while being carried back, he had several spells of pallor, falling stiff, and then having convulsions. Brought finally to the Charité in Berlin, he had more spells of sudden pallor, collapse with brief convulsions, tossings in bed, as well as absences, post-convulsive headaches, and mild bad humor.
There were numerous attacks several days apart in the first seven weeks. The patient was not of an “epileptic” disposition, though readily dissatisfied and headachey.
The serum W. R. was positive. Treatment by mercurial inunctions. No further convulsions. Prognosis doubtful.
Re epilepsy and the war, during the first six months Bonhoeffer observed 33 cases in the Charité Clinic in Berlin. Twenty of these 33 cases, unlike Case 55, had attacks before the war, although ten of these had become epileptic rather late, namely, after the period of active military service, at ages from 22 to 27. The development of epilepsy like Case 55’s is not without frequent precedent.
Bonhoeffer states that aside from epilepsy directly due to brain injury by shells, there has been no certain case in which we have the right to regard the war itself as the total cause of the epilepsy. Some, like Case 55, are of syphilitic origin. No subject with a severe long-standing epilepsy has been able to get into the field, according to Bonhoeffer; when they do, they prove constitutional subjects.
An epileptic imbecile, court-martialed.
A Belgian soldier was condemned by court-martial February 27, 1915, to five years imprisonment for leaving his post in the presence of the enemy. It seems that he was mounting guard with two of his comrades and all three left to eat as no food had been brought to them.
A physician examined the Belgian soldier and declared him responsible, although a little sick. All three were condemned to imprisonment. The Belgian attracted attention in prison through crises of anxiety and agitation; he had terrible nightmares, seeing Germans in his cell and hearing gunshots. He was accordingly sent to a special infirmary of the dépôt, whence July 24 to Sainte-Anne, July 26 to Villejuif. He talked Flemish, hardly understanding French, and spoke slowly and with difficulty. He hardly knew how to read or write. He had been a truckman.
At 18, this soldier, according to his own account, began to have nervous crises in which he fell, lost consciousness, bit his tongue, foamed at the mouth and urinated involuntarily. The attacks were somewhat rare. His father sent him in 1910 to Gheel where he stayed two years. Returning home he helped his father in the trucking work.
When the Germans came the family fled to France and, about the end of 1914, he was put into the military service and sent to the front after a very short period of instruction.
The man had followed the example of his two comrades without taking the slightest thought. He did not understand the gravity of his act. He was not remorseful, regretful or angry against his judges. He was well oriented but quite indifferent. He was a tall, intelligent looking man with adherent lobules, slight facial asymmetry and evidence of tongue biting. He wrote like a child and read slowly, spelling out the complicated words. He was employed at various manual tasks during his sojourn at the asylum and had no epileptic attack. He was given over to the Belgian military authorities October 5, 1915.
Seizures in a feebleminded subject—psychogenic components.
A 21-year old tailor, unused to marching, went into the field in August. A month later, after a period of long standing, he was nauseated and fell in a faint. Upon waking, his fingers were stiff and he had pains in his legs. He got better in the reserve hospital and was sent back to the line. On the way he had a similar seizure, with nausea and fainting. On the way back to Berlin, he had a seizure in the railway station, and was carried to the Charité Clinic. At the clinic he stated that he could feel an attack come on; that he first had Angst all over his body, and that it was hot inside of his head. Latterly he had been able to stop an attack by clenching his teeth, after which the attack would not proceed except that all became black before his eyes.
He was observed for four weeks but no seizure appeared. He was somatically negative; his Wassermann reaction was negative. There was nothing hysterical about his make-up; he was somewhat surly and of low mental grade. He was unwilling to walk alone for fear of attacks.
As to the heredity of this soldier nothing is known. He had been an illegitimate child; he was a sleep-walker in childhood; he had sometimes spoken out loudly in sleep as a boy. At school he had been somewhat backward, fought readily with his mates, and often complained of dizziness and headaches. He could not stand smoking or drinking well, getting drunk upon two glasses of beer. He had not held positions well. He became a pionier in 1914, working chiefly as a tailor.
Early in his time as a soldier he had obtained an ulcer of the glans, which had been excised and burned. There had been no secondary symptoms.
According to Bonhoeffer, this is an example of a not infrequent condition. Although the attack itself and the habitus of the patient did not look hysterical, the manner in[70] which the attacks repeated themselves speaks for psychogenic components. Just as genuine hysterical attacks may be looked on as reactions to unpleasant situations, so may these attacks. In fact, we are probably dealing with an hysterical fixation of the symptoms of emotional fright like those in the true hysterias following shell explosion. A great many of the phenomena of Shell-shock, to use the English phrase, are not in and of themselves of a psychogenic nature, but they are, according to Bonhoeffer, psychogenically liberated under the influence of unpleasant ideas.
Re reactive epilepsies, Bonhoeffer considers that there is a group of reactive epilepsies in which the war process plays an important part. The prognosis of these cases ought to be relatively favorable. In point of fact, Case 57, although a feebleminded subject, seems to have had a relatively favorable prognosis: at all events, no new seizures appeared under prolonged medical observation. These reactive seizures may occur in cases with a labile vasomotor system. They are, according to Bonhoeffer, aligned rather more with hysteria than with genuine epilepsy. Genuine epilepsy has not been developed in the war cases observed by Bonhoeffer except where an endogenous factor was clearly in evidence; or else where there was the requisite antebellum soil for the development of an epilepsy. In short, genuine epilepsies developing in the war are all, according to Bonhoeffer, predispositional. The antebellum soil was clearly in evidence in Case 57. Even before the war, according to Bonhoeffer, many German soldiers during the period of military service gave evidence of their epileptic soil by sundry suspicious phenomena. Among these were fainting spells during hard drilling and other exercises, spells of enuresis, abnormally deep sleep, and even phenomena of somnambulism. One of the Bonhoeffer epileptics had been released during his reservist practice as unfit for military service, and had only been put into the line at his own urgent request at the outbreak of the war. Three volunteers concealed their epileptic history. One man, who had had merely petit mal attacks before the war, regarded them as of little consequence, entered the service, and developed epilepsy.
Responsibility of a drunken epileptic.
The question of responsibility arose in the case of a soldier who left his camp the morning of October 23, 1916, and went to a neighboring place, where he drank, with four others, two quarts of wine. At about three o’clock in the afternoon, his captain met him on the street, lost, and looking drunk. He told him that he would send him to the trenches in the evening. The man lay down and went to sleep. At about six o’clock, it was found that he could not put on his equipment alone, and in fact threatened the other men with his bayonet, and then went to sleep. He woke up and explained that he had had one of his nervous crises. He remembered the matter of the bayonet but had forgotten everything else about the struggle.
This soldier was 29 years old, the son of an alcoholic, and the ninth child of a mother who died shortly after her tenth pregnancy. He had had measles and bronchitis as a child, and in childhood had had bad dreams; at the age of ten he had swooning spells. He became a quarryman and a habitual drinker, subject to dyspepsia, nightmares, and nocturnal cramps. There had never been any crises, however, up to wartime.
January, 1916, when a shell burst near him, the first sharply-defined epileptoid crisis came, and was followed by a number of others, either on leave or on service, March 8, June 2, and July 13. These attacks showed a sudden fall without warning, loss of consciousness, convulsions, tongue biting, incontinence of urine, a period of more or less coördinate agitation at the time consciousness was reappearing, sometimes a fugue, and often amnesia for the whole. He had a scar on the left border of the tongue.
Should this epilepsy be regarded as entailing irresponsibility? He left camp before the crisis, accordingly in a period when he was in full possession of consciousness and will, and he had gotten into an irregular situation by drunkenness[72] before his epileptic crisis started in. His struggle with his comrades, however, appears to be a portion of a post-critical dazed state. The medicolegal decision, therefore, was that he was guilty of leaving his command but not of the other misdemeanor. Considering the general nature of epilepsy, the responsibility of this man for the whole adventure is rather slight. The Council, however, condemned the man to five years of labor, without admitting that the crisis following so soon the actual misdemeanor should argue a diminution of responsibility.
Re epilepsy in the army, Lépine notes the serious theoretical and practical problems to which it gives rise. In the first place, epilepsy occurs in the army more frequently than in the same number of men in civilian life. Consequently, the diagnosis as to the really epileptic nature of the attacks observed is not too easy. Again, the situation affords much opportunity for simulation (see, for example, the case of sham fits (Case 78, Hurst), and the case of epileptoid attacks controllable by the will (Case 79 of Russell)). Wounds may produce it, and even wounds which do not affect the brain; besides which, a variety of war conditions, short of trauma, may produce it. When the ordinary impulsiveness of the epileptic turns into automatism and to epileptic equivalents (états seconds), much of medicolegal interest may happen. Case 58 was just short of a murderer. Cases of actual murder in epileptic equivalents have been known under military conditions. Fugues with amnesia for the phenomena (which look to the military man like intentional desertions) form another group of epileptic events; but aside from the manias and the fugues, there are still more dubious epileptoid phenomena of a delusional and confusional nature, such that the proof of epilepsy comes only afterward, when frank convulsions supervene. Re fugues and desertion (the most frequent of military delinquencies according to Régis), we may think of the fugue reaction, according to Lépine, as a natural reaction on the part of both the true delinquent and the mentally sick subject. The loss of liberty, alcohol, fatigue, minor phenomena of commotio cerebri, may lead to states of mental depression that favor the fugue. It is an[73] affair of the greatest delicacy for the expert to build up again the exact plight of the soldier at the time of his desertion. Special inquiry must be made of the man’s mates. Only in this way can the wheat be separated from the chaff and punishment allotted to those only who deserve it.
According to Lépine, there are fewer guilty fugitives than there are innocent ones, or at least partially innocent ones. In the decision, one takes account of the duration, the course, and the peculiarities in the termination of the suspicious flight. According to the military code, there are cases like Case 58 in which the fugue itself was carried out in an unconscious state, and yet in which the martial responsibility of the man was absolute. Drunkenness is no excuse for the fugue, even if the latter is automatically carried out. Of course, the paretic is not responsible for his fugue any more than the organic dement, the delirious uremic, or the chronic alcoholic, who is already severely demented. For a case of this sort, see Case 1 (Briand).
In the differential diagnosis, we must also consider that fugues may be carried out in confused states as well as at times in various paranoid states, and even in melancholia.
A disciplinary case: Epilepsy.
A Milanese workman, 28, was exposed to the sun on sentry-go and had an attack of convulsions, on awaking from which he found himself in hospital. He always had attacks in reaction to emotion. One day, in a quarrel provoked by jealousy concerning a prostitute, he apparently lost his mind, whipped out a hunting-knife, and wounded a comrade. Thereafter he lay unconscious until the next day. The court-martial decided that he was not fully responsible.
Eventually, he was sent from the front for having insulted and struck a superior officer. The report read also that he was a prey to delirium and had frothed at the mouth. In the interior he had convulsive attacks, with falling and loss of consciousness. He told of arguing with a sergeant about a bicycle, of seeing darkness before his eyes like a veil, and of subsequent amnesia. In hospital he had intense headaches at times, with spells of sullenness, hostility, and complaints concerning nurses and attendants and other patients. At other times, he was quiet and comfortable. One day he went into an excitement and wept, asking to be sent back to the army, striking the table with his fist and head. He then screamed, flew into a passion, and fell to the ground in semi-stupor, shaking his body and trying to kick and knock away those who intervened. He was placed in bed but remained agitated and unconscious, with anesthesia and frothing at the mouth. The abdominal and cremaster reflexes were absent in this attack, and the pupils were rigid and myotic. The pulse was rapid and the blood pressure high. Afterwards he was sleepy, stupid and weary, and showed fine rapid tremors of hands, tongue, and eyelids. The abdominal reflexes now returned in excess, and a marked dermatographia developed.
Upon investigation, it was found that the patient’s father was also an epileptic and was alcoholic; that one paternal uncle had died in an asylum; another of apoplexy; that two[75] maternal uncles were chronic alcoholics (one in an institution); that an alcoholic brother had been six times convicted of assault and battery; that a sister had howling, crying, and hair-pulling spells, throwing herself to the ground. The patient himself had had an early Bright’s disease and had always been an undisciplined, excitable, and impulsive boy, sometimes kept out of school. His first conviction was at 18, for assaulting a policeman, and he had been arrested four further times for assault and battery. He stated that his convulsive attacks with the veil before the eyes came on when he was irritated or had taken cold, or had drunk to excess, or had over-exerted himself. He said he suffered from intense headache, weariness, and sleepiness after an attack. He always bit his tongue at the same period. Irritation and exertion sometimes caused attacks of dizziness and vertigo without unconsciousness. Alcoholism; ulcer in an inguinal gland. He had been confined in an asylum 40 days for epilepsy, attacks of which had become more frequent after he had heard of his father’s death.
Re violence and epilepsy, Lépine remarks that a pure epilepsy unclouded by alcoholism may occasionally give rise to acts of extreme violence, but these pure epileptic violences are infinitely rarer than the alcoholic ones. The Milanese was in point of fact alcoholic, and in his ancestry were a number of alcoholics as well as epileptics. According to Lépine, when subjects are “out for blood,” they are almost always either, like this Milanese, hereditary alcoholics, or else strongly predisposed subjects, or even the offspring of the insane.
A disciplinary case: Epileptic attacks with amnesia.
A Veronese, 23, quarrelled with his comrades, and one day wounded one. Another time, when reproved by a superior, he struck him with a shoe; and at still another time, hurled himself upon his superior officer and bore him to the ground. Yet he seemed to have a perfect amnesia for all these violent acts. At other times, he had convulsive attacks with a mental state which seemed to combine anger and depression, after which he would fall to the ground, lose consciousness, go into clonic spasms, spit bloody saliva, and cause wounds and abrasions upon his body. Once, after such an attack, he passed into a brief excited spell. Finally he was so insubordinate and violent to superior officers, that he was brought under hospital observation, having been excited and confused for a day.
Next day he was lucid, oriented, and tranquil; entirely amnestic for what happened the day before, though his acts were sufficiently unusual. He had threatened his superior officer and been reproved and sent to prison to think it over. In prison he had suddenly thrown himself against another innocent person and clutched him tightly about the neck. He threw another violently to the ground and then ran to help the previous victim! Bound fast, he had succeeded in freeing himself and thrown himself furiously against the prison door, whereupon he had fallen to the ground in an epileptic fit. He had tachycardia (120) and a generalized hypalgesia. The vasomotor reactions were excessive.
Upon investigation it proved that his mother had been subnormal and that the patient had been constitutionally excitable and unstable, given to attacks of anger and impulsiveness from youth up. In fact, he had been in prison several times for violence. He described himself in his restless spells as feeling a trembling all over his body as if his blood were boiling in his heart and his head, whereupon he would lose knowledge of what he was doing. He had been a[77] quarrelsome boy, pursuing his mates with knives and stones. Once, after arguing with a car conductor, he had broken the car windows, turned everything upside-down, and thrown the conductor into the street.
Case 60 is clearly in the same group as Case 59. The Veronese falls into the same frame with the Milanese except that he appears not to have been alcoholic. The insubordinations of the Veronese were apparently carried out in a state of unconsciousness. The majority of insubordinates appear not to be epileptics. Some authors have called attention to pathological politeness as an occasional symptom in epilepsy. Perhaps the majority of insubordinate cases are feebleminded or schizophrenic.
Desertion in epileptic fugue.
A blacksmith from the Rochefort Arsenal, 27 (nothing known as to grandparents; father, now in the fifties, for 30 years in an asylum with frequent attacks of furor; mother, 45, well and apparently well-balanced; brother with the colors, wounded and decorated with the military medal; a cousin-german, who has had a typical epilepsy—in the patient himself enuresis up to 13 or 14, later, less frequently; apparently no tongue-biting; no information as to infectious diseases; graduate from primary school, apprenticed to a blacksmith; an unskilful worker; never able to rise to the level of a frappeur), in 1909 had passed the board of review and been put in the sixth division of the line. Antebellum there was a history that one night at supper, he had slipped away from quarters and gone 30 kilometres, home. His astonished mother sent him back to the military post by railway.
Upon the night of May 26-27, 1915, this soldier found himself in the position of a sentry, opposite the enemy. He told his comrade that he had to go away for a time, leaned his gun against a tree, disappeared, and did not return. It was then one o’clock in the morning. At six o’clock, he was found two kilometres away from the lines, in a village. He was in front of a barn where his company had been quartered before taking possession of the advanced posts.
He was brought up before the military authorities; but upon stating that in civil life he had wandered off several times without knowing where he was going, he was submitted to neurological examination. There was available a letter from his family physician relative to his antebellum military service. It appeared that he had committed a number of breaches of discipline, and that he was regarded by the physicians as a déséquilibré. He had lived with his mother a very quiet and good life; there was no history of sexual irregularity, and no history of illness except a slight catarrhal jaundice. He had frequently suffered from headaches; there[79] had been slight attacks of vertigo of very brief duration. He had never fallen in these fits. From his story it was elicited that he had had absences; his comrades had noticed that he sometimes stopped stock-still with vague eyes, then shortly regained his wits and continued upon his task. Sometimes he would not work without being able to explain why he went away. He would go off for a period and, upon coming to, discover that he had not eaten his meals. There were never, however, any convulsive crises by day or night. He sometimes felt sick, and although there was no medical treatment, from time to time he took bromides upon his own authority, saying he had been ordered to do so by his father. Although habitually of a gentle demeanor, nevertheless he was subject to excessive anger upon slight occasion.
During the mobilizing and first months of the war, both in quarters and at the front, however, his conduct had been that of a good soldier. Suddenly, about March or April, 1915, the nocturnal enuresis began to be frequent again, occurring twice or three times a week; but the patient hid this misfortune as far as possible from his comrades. The captain thought he looked tired and depressed sometimes. Upon the days following the nights with enuresis, there was intense headache and marked moral and physical depression. There was no proof of nocturnal convulsions, and it is very problematical whether there was tongue-biting.
Another odd feature was that the patient, who had been sober in civil life, had become intoxicated several times after going into the army. Physically, he was of low stature, but otherwise well built. Neurologically, he was entirely negative. There was no sign of venereal disease. There were a few stigmata of degeneration; for instance, there was very little hair upon the face, the ears were unequal in size, and the teeth were somewhat anomalously set. Mentally, he was below par; for instance, he could not add mentally two numbers of two digits.
As to his desertion, the patient says he does not know what he did; that he learned of his act only from his comrades in the morning; that he remembered having left his duty pour aller satisfaire un besoin.
A specialist in escapes (epileptic fugues).
An epileptic fugue with recidivism is described by Logre. He described himself as a specialist in escapes. As a schoolboy, he had practised escapes and run away without purpose, and without remembering fully what he had done. His father would bring him back to school. At first they had punished him and then would pardon him. These escapades in his work as a shoemaker caused him to lose various places, but he had been kept by one employer for a long time nevertheless. From 11 years on, this patient had never ceased living either in foreign parts or in prison.
The fugues on military service began to multiply. The military chiefs did not abide the escapades like the schoolmaster or the employer. Every punishment he received had to do with some fugue. Three times he gave himself up to the military authorities. Three times after a few more days’ service or a week in prison, he left the barracks or escaped. There had never been any appeal throughout this history to an alienist. On the declaration of war, he had returned to Belgium and was put into the army; whereupon in January, he carried out a fugue of a few hours which was rewarded with eight days in prison. There was a five-days fugue in July, whereupon he was taken before the council.
Upon investigation, these fugues seemed to have the classical features of epileptic fugues. They were sudden, unconscious, blindly automatic, almost completely forgotten afterwards and of a stereotyped and recidivistic nature. Most of the fugues had been preceded by a slight excess in drinking. An investigation was made to see if there were any convulsive antecedents; none were found. This mental epilepsy, then, it was thought, must be an isolated symptom, free from every motor symptom. But his mother and one of his brothers had also shown a number of attacks of some sort of epilepsy. In all three cases there was impulsivity, unconsciousness, absurdity, recidivism, and refractoriness to[81] treatment. On these grounds the fugue was regarded as pathological and as epileptic probably. The patient himself thought that these coups-de-tête and this mania for running away without knowing where, made really a very ugly fault, particularly in a soldier.
Re such specialists in escapes as Case 62, Lépine speaks of a type of military delinquent which he calls Ceux qui sautent le mur. Some of the fugue subjects, as well as other types of imbalance can apparently be held by no possible kind or degree of discipline. They jump any guardhouse or any other form of imprisonment through what amounts to a wild instinct for liberty. In some cases, this instinct appears in a relatively pure form; that is, without any combined tendency to dipsomania and without any sexual factor. Some of them are, in fact, very good soldiers, especially in shock troops. They, in fact, belong to what one might call the good element among delinquents. In the French Army some of them have been old legionaries and have even been, as in Case 62, previously condemned for desertion. They form a curious minority among the wall jumpers. Wall-jumping makes, so to say, the entire pathological phenomenon, and the recidivism is a part of the disease.
A disciplinary case: Epilepsy and other factors.
An Italian private in the artillery (father dead of general paresis) had been a victim of infantile convulsions and of convulsions with loss of consciousness up to 18 (convulsions with shouts and violence in the streets of Rome; had to be put in a straight-jacket at the municipal hospital).
He developed more convulsions during antisyphilitic treatment in the military hospital. He was a very poor soldier, of the rough and violent sort, and after eight months of service had to be assigned to a special disciplinary company, with which he remained for fifteen months. Here also he was punished frequently, and was given a period of four months’ imprisonment for refusal to obey the officers. Then for a period of several years he had no convulsions whatever.
During the war he was given to alcoholism, and one day in June, 1916, he struck an officer and ran away to arm himself. He was at this time observed by psychiatrists and declared sane. He was regarded as an emotional and alcoholic epileptic but not as neurotic or psychopathic. He was again placed in a special disciplinary corps.
Re the convulsions which this Italian developed during antisyphilitic treatment, it would be interesting to know whether intravenous injections were used. In case they were used, one might compare the case of this Italian with Bonhoeffer’s volunteer who developed epileptic convulsions after antityphoid inoculation.
Re the insubordination and violence of this Italian, compare remarks of Lépine noted under Cases 59 and 60. Re the “other factors,” compare remarks of Bonhoeffer noted under Case 57.
An epileptic goes through Mons and two years fighting without symptoms. Then strange conduct with amnesia.
A private, 26, epileptic from 11 to 18 (mother also epileptic) entered the army at 20, attempted to commit suicide in 1912 (amnestic for this attempt), and went to France with the expeditionary force in August, 1914. The retreat from Mons and further fighting caused no recurrence of the symptoms. September, 1916, he was in fact put in charge of eight men doing guard duty. At this time he was able to get to bed only every other night. The charge of the telephone worried him, as he had never before been made to assume responsibility. After two months of this, he was found one night arresting civilians without cause and driving them before him with fixed bayonet. He was let off court-martial on the medical evidence, and at hospital remained confused and suspicious. November 16, he was seen by a medical officer in a typical attack of petit mal. Of all this, on reaching England December 19, he had no recollection, and was keen to return to duty.
Re the remarkable delay in the return of epilepsy to this soldier of Mons, Bonhoeffer remarks that one of the epileptics observed by him at the Charité Clinic had passed through nine battles, and another through 18 battles before the first attack of epilepsy. Bonhoeffer regarded the strenuous marching as a liberating factor of epilepsy in five cases, actual fighting in seven cases, shell explosions in two cases, and bullet wounds in three.
Re the apparently psychogenic factor in Hurst’s case (epilepsy coming on after assumption of too great responsibilities), compare remarks of Bonhoeffer under Case 57 concerning psychogenic factors. Sir George Savage has called attention to a form of functional epilepsy following shock or injury, in which recovery occurs after removal from the strain, but in which there is a relapse if the men go back to duty.
Therapeutic (antityphoid inoculation) epilepsy.
A volunteer without psychopathic signs except a slight stuttering, and without psychopathic history of any sort, went into service at 17. After he had been a short time in the field, a shell fragment injured him in the upper part of the thigh. He lay up in hospital four weeks. He then spent four weeks in the reserve.
He was then given antityphoid inoculation, and a half hour afterward had epileptic convulsions. These appeared four times more during the next fortnight, as a rule followed by a delirious excitement. No fever was reported. After the fourth attack, he was transferred to the Charité Clinic.
At the clinic there were no attacks, and there was nothing epileptic to discern in the make-up of the patient. His nervous system was normal to examination. There was, however, one fact in the family history of note, namely, that an older brother of the patient, 20 years of age, suffered from convulsions.
What is the relation of the antityphoid inoculation to the epilepsy? According to Bonhoeffer, we must not forget the family history even if we regard the inoculation as the liberating factor. Curiously enough, the shell injury did not itself serve apparently to bring out the epilepsy. Bonhoeffer has seen three other instances of epileptic attacks or epileptoid phenomena following antityphoid inoculation. However, in the hundreds of thousands of inoculations, it is not to be wondered at perhaps that there should be a number of instances of epileptic attacks. One was a man with severe epileptic taint; in the others, there was a question of pathological intoxication.
Re antityphoid inoculations, a French observer—Paris—remarks that these inoculations may occasionally start up the symptoms of general paresis. Compare in this connection also Case 63, in which a syphilitic developed convulsions during antisyphilitic treatment. The psychogenic factor of intravenous injection itself, with its possible effect[85] upon glands of internal secretion, can hardly be distinguished from purely serological effects. Paris goes so far as to state that he regards it as imprudent to vaccinate a syphilitic subject. He thinks it might be better for a syphilitic subject to contract typhoid or paratyphoid fever than to run the risk of developing paresis. If the soldier happened to be not only syphilitic but alcoholic, then the danger would be larger. Possibly, however, both Bonhoeffer’s case of antityphoid inoculation epilepsy and the cases alluded to by Paris of antityphoid inoculation, are merely statistical accidents.
Shell-shock; (apparently slight) scalp wound: Jacksonian seizures. Operation, decompressing the edematous upper Rolandic region. Recovery.
A Moroccan of the Seventh Tirailleurs was thrown to the ground by the explosion very near him of a large calibre shell, lost consciousness, and woke up with a slight contusion of the right side of the head. The date of this injury is unknown. He was evacuated to the interior, but stopped May 25, 1915, at the evacuation hospital because his pulse in the train stood at 51. An hour later in the hospital he had a Jacksonian epileptic attack, followed by a left-sided flaccid, brachial monoplegia, and after a quarter of an hour a second crisis, and then a third,—a sort of epileptic status occupying an hour. The attack seemed to start in the left hand. After the crisis, hand and arm became flaccid and inert.
Lumbar puncture in the crisis gave fluid under small tension in a few absolutely limpid drops. The wound was a superficial skin wound as big as a 25-centime piece, near the middle line, roughly corresponding with the upper Rolandic region. It was hardly a wound—a mild abrasion not passing the epidermis; periosteum and bone intact.
The patient was trephined and a thin layer of clot was found over the dura mater. The clot was removed and a crucial incision was made into the dura mater. The brain seemed a little edematous, hemorrhagic and bruised. It soon began to beat and was tamponed.
May 26, complete brachial monoplegia without seizure.
May 27, seizure at 2 in the afternoon, starting in left arm.
The wound was going well and from this time forward no more seizures. May 28, a cast was made for the hand.
June 4, lumbar puncture yielded a clear liquid under the pressure of 58. That evening an hour after the puncture, the brachial monoplegia disappeared. The arm was still a little weak June 5. June 8 the man was evacuated to the auxiliary hospital at Laversine. June 18, complete recovery.
Fall and blow to head: Hysterical convulsions. Cure by studied neglect.
Clarke had seen in the war but one case of hysterical convulsions, though this particular patient had severe hystero-epileptic fits occurring in series. The man had never suffered from epilepsy and was 20 years of age. He received a slight wound and fell back into the trench a distance of six feet, striking but not contusing the back of his head.
On admission to the hospital he was found drowsy and dull. Fits occurred a week later, following one another at brief intervals in series that lasted one or two hours. The arms would be raised and extended in clonic spasm; the patient would resist violently if held, and then turn to his right side with rigid extension of legs and back in opisthotonos. The eyeballs underwent irregular movements, and there was a well marked hippus. Though the tongue was protruded in these attacks, it was never bitten. It was doubtful whether there was a complete loss of consciousness. Between attacks, the patient was morose and sullen, and showed a varying incoördination of the movements of the left leg, which was anesthetic to the knee. There was also a glove anesthesia of the right forearm and hand. Fields of vision were contracted.
The fits recurred with intervals of a day or two, for a fortnight. The patient was then strictly isolated in a small room with an observation window. His bed was made up on the floor. He then had very slight attacks, as a rule when the nurse came into the ward; no notice was taken of these attacks and in a fortnight they ceased. The paresis of the leg and the anesthesia also cleared up without treatment. He remained in the general ward three weeks longer, at first dull and listless, but later cheerful and active. Clarke suggests that this patient was below normal intelligence.
Shell injury with unconsciousness; delayed attacks of epilepsy: superposed hysterical hemihypesthesia. Previous history consistent with the hypothesis that a genuine epilepsy had been developed.
An excellent soldier, of good build, 29 years, a member of the Landwehr, passed unscathed through eleven battles in the 1914 campaign, but finally succumbed to fragments of shell which struck his chest and the lower part of his thigh. He fell down, nauseated, and lost consciousness. He is said to have struck about him with his arm and to have voided urine. There was a second attack three weeks later, in which he fell upon his face.
In the Charité Clinic he had three attacks, two of them nocturnal, one in the daytime, followed by a long period of somnolence. He once cried out suddenly in the night as if warding off an attack. He complained of headaches, and was often irritated and out of humor. Somatically, there was a hemihypesthesia on the side of the injury.
The history indicates that this patient up to his sixteenth year had been a victim of occasional enuresis, often cried out in his sleep or even rose from bed. Occasionally he suffered from such violent sudden headaches that he would have to sit down. He was easily irritated, and had once been arrested for assault. As a soldier, however, he had never been guilty of any breach of discipline. Mild headaches would follow drinking. These phenomena in the history pointed in the direction of epilepsy. According to Bonhoeffer, we cannot entirely exclude contusion of the brain from the shell injury. However, there were no cerebral symptoms, and the interval before the occurrence of the attacks rather indicates that we are dealing with a genuine epilepsy. As for the hemihypesthesia, this is a hysterical “superposition,” which does not interfere, according to Bonhoeffer, with the genuineness of the epilepsy.
Shell-wound; musculocutaneous neuritis: Brown-Séquard’s epilepsy.
An infantryman, 30, a gardener, was wounded in the right forearm by a shell fragment, which fractured the ulna, September 7, 1914, at Revercourt. Despite much fragmentation of the bone and suppuration, the wound healed with two cicatrices, where the fragments had gone in and had come out. The scarring process was over in December.
However, in the middle of January, 1915, this man began to suffer from headaches and insomnia, with vertigo and buzzing in the head, “as if an airplane inside.” Sometimes arms and legs would stiffen, and the man would tremble, have to lie down, and even lose consciousness for a quarter of an hour, waking up tired, wandering, and with feelings in his head. These crises, at first occurring every week, later grew frequent. Finally there was a very complete attack, in which he fell out of bed, got up, made several turns about the room, and went back to bed; and in the morning, was dull and disoriented. Accordingly, he was sent to the central military neuropsychiatric service of the general hospital at Montpellier, November 10.
Besides the two extensive cicatrices, there were motor disorders. Pronation and supination were almost impossible, as well as extension of the hand and fingers and abduction of the thumb. There was a radial paralysis without R. D. Electrical excitability of the extensors was diminished on the right. The hand was weak. The right thumb was atrophic. There was a hypertrichosis as well as redness, heat and perspiration of the right hand. There was a hypesthesia for all forms of stimulation in the hand, especially in the radial region; less in the ulnar region. This hypesthesia rose along the posterior surface of the forearm and covered all the territory of the ulnar nerve; but there was a corresponding hyperesthesia in the musculocutaneous distribution, as well as in the internal cutaneous distribution. Above the[90] scar there was a region of complete anesthesia. The hyperesthesia rose higher along the circumflex nerve and the posterior branches of the cervical nerves and included the great occipital distribution, even involving the superficial cervical plexus, though not the territory of the trigemini. There was some hyperesthesia of areas governed by a few dorsal intercostal nerves. There were also spontaneous pains in these hyperalgesic regions. The musculocutaneous nerve could be felt to be thick and swollen, indicating a perineuritis. There were no neuropathic stigmata, but the knee-jerks were exaggerated a little more on the right side.
The convulsions appeared two or three times a day, the pain would get worse along the arm, rise to the head, following the hyperesthetic zone, then invade the interior of the head, whereupon objects would appear to turn and the ears would buzz. The right leg, and especially the right arm, would begin to tremble. The man would have to support himself to avoid falling. He saw shadows moving, colored trees, occasionally persons. When the vertigo got stronger, he lost consciousness. The extremities of the right side stiffened and carried on jerky movements. These sometimes extended to the left side. The seizure lasted from five to fifteen minutes, and sometimes occurred in the middle of the night. Fatigue followed but headache disappeared after an attack.
The diagnosis of Brown-Séquard’s epilepsy was made. If the musculocutaneous trunk was compressed, a crisis was produced with pain radiating to the head, obscuration of vision, numbness in the arm, and tremors. Electrical treatment was resorted to for analgesic effect. There was a certain improvement during May, so that the diurnal dizziness disappeared. May 19 he had a period of 24 hours without any vertigo. In June no further improvement occurred.
An operation was performed June 23, 1915. The two cicatrices were excised, and some fragments of cloth were removed. Three Jacksonian crises followed the operation, and there was another seizure next day. Frequent headaches followed without crises. More seizures appeared in[91] the night during July, and their frequency increased. Pains persisted along the arm and in the back of the head; the musculocutaneous perineuritis was still intense. Prolonged baths for the arm were begun August 4, two baths of two hours each, at 40 deg. each day. Following August 10 there was an improvement, which stopped as soon as the baths were omitted, with diminution of the vertigo and the hyperesthesia. This improvement continued; the baths were made to last three hours. There were no attacks from August 21 to 26 whereupon they then returned for two days. The pains had much diminished in the arm but persisted in the occiput. A few night attacks occurred August 30 and 31, September 5 and 6, as well as September 19 and 20, 25 and 26, and 27.
The occipital pain had now become less; the musculocutaneous nerve was not so large. Only a few headaches followed during the months of October, November, and December. After November 3 the baths were stopped and the arm was kept wrapped in a warm compress. There was still a certain hyperesthesia, the knee-jerks had become less exaggerated. Massage and mechanotherapeutic exercises were begun. There were no more attacks after September 27.
Re Brown-Séquard’s epilepsy, Lépine remarks that besides the case of Mairet and Piéron, Hurst and Souques have published cases. Lépine himself has observed two cases: one followed a nerve wound in the foot; another, a penetrating wound of the chest. As a rule, such Brown-Séquard epilepsies appear a number of months after trauma; as a result of irritation in the scar. Lépine’s subjects were taken for simulators because they had not received any cranial wound. The prognosis should be guarded, though the outcome in Case 69 appears to have been favorable.
Epileptic episode at 24 years following bullet-wound of hand, in a soldier who had had convulsions in childhood (sister epileptic). Reactive epilepsy? Epilepsia tarda?
A man in the reserve, 24, bore the stresses of the war very well in the campaign in East Prussia until he was shot in the hand at Deutsch-Eylau. He had always been well aside from rheumatism, and was discharged with a good record from his military service.
Sent to the reserve hospital for his hand injury, he had, two or three times in the night, convulsions with loss of consciousness and dilated pupils; after which there was a thirty-six hour period of depression with refusal of food. Thereafter this soldier had amnesia for both the seizures and the subsequent depression. He was observed six weeks longer in the Charité Clinic but had no more attacks, and indeed nothing more of note either mentally or somatically.
The history showed that there had been convulsions in the third and fourth years of the patient’s life. There had been, however, nothing epileptoid in the later childhood or developmental years of the patient. However, a sister of the patient had suffered since childhood from convulsions. It remains a question whether this episode is to be regarded as reactive epilepsy—reactive, namely, to experiences in the war—or whether we are dealing with a true epilepsia tarda.
Re this episode following bullet wound, the compiler has placed it after Mairet and Piéron’s case of Brown-Séquard epilepsy, but apparently Bonhoeffer regards his case as probably a reactive one. Unlike the case of Mairet and Piéron, Bonhoeffer’s case had an epileptic soil (convulsions in childhood and epileptic sister). Re the so-called reactive epilepsies, see remarks by Bonhoeffer under Case 57.
Epilepsia tarda in a lance-corporal without hereditary taint or previous history save dizzy spells and excitability.
A reserve lance-corporal, 24 years—a soldier from 1911 to 1913 without disciplinary record, and in his second year becoming lance-corporal—was in the campaigns in Belgium, East Prussia, and Poland, making long marches and going through several battles. In the middle of October, 1914, he fell from a horse and suffered a contusion of the thorax, after which blood appeared in the sputum. In November he was brought to the reserve hospital in Berlin, and there had convulsive seizures. Before transfer to the Charité Clinic, a seizure occurred, and he was brought into the clinic in a characteristic dazed state. Thereafter he was clear but often out of humor and irritated. Three weeks later came a brief attack, probably epileptic in nature, with restless half-delirious sleep following.
There was nothing in childhood or in the family history to indicate epilepsy. However, the patient himself stated that from 1913 onward, after his period of military service, he had from time to time felt attacks of dizziness after exertion, and that he had become more easily excitable than before.
The attacks in the lance-corporal are probably not to be attributed to the thoracic contusion, according to Bonhoeffer, because of the long period that elapsed after the thoracic injury, and their development nocturnally without special occasion. According to Bonhoeffer, we are probably here dealing with a late epilepsy.
Re late epilepsy, see also under Case 57. Bonhoeffer makes a considerable point of the lateness in attacks of epilepsy in some of the military cases, pointing out their beginning at the ages of 22 to 27 in the period of peace practice undergone by soldiers. The theory is that cases of severe and long-standing epilepsy are known to the authorities, so that[94] they would not ordinarily be in military service except under conditions of concealment or in case of error. The present case (71) appears to be the nearest that Bonhoeffer has found to a case of epilepsy without heredity and without acquired soil. All that can be regarded as evidence of soil is the dizzy spells and excitability.
Re thoracic contusion, compare remarks of Lépine under Case 69, on Brown-Séquard epilepsy following thoracic wound.
Convulsions by autosuggestion.
A private, 27, is described as a typical martial misfit—in private life a music hall falsetto singer, and afterward a valet. He joined the army in 1915 and proceeded to France, and worked in a canteen. A week later, men broke in and threw a mallet at him, whereupon he immediately had a fit, and was dazed, dumb, and unable to walk for two days. Thereafter occasional further fits occurred, with nervousness and insomnia. He was sent home in September, 1916. Discharged to duty, he again in December returned to France, had six fits in the first week—three in hospital, two on the boat, and between two and four for four days after admission. The diagnosis of genuine epilepsy was made in France by a medical officer who had seen one of the convulsions. However, he had never passed urine or bitten his tongue, had no family history, and had never had fits before going to France.
He was hypnotized and given the suggestion that he would have a fit. In the convulsion which followed the plantar reflexes remained flexor, but otherwise the convulsion was quite like the genuine epilepsy. He was told that he would not have any more convulsions, nor did he have any more except on Feb. 16, 1917, when some talk was made to him about returning to duty. Bromides used in France did not help the epilepsy at all. This patient developed a gait and speech defect copied from two patients in the wards. These symptoms, due to autosuggestion, disappeared on persuasion.
Re autosuggestion, Bernheim has returned to the fray (1917) in a book on automatism and suggestion, dealing only in small part with war problems. The most general formula for suggestion appears to be that it is an idea accepted. A suggestion offered but not accepted is in effect not a suggestion at all. Any accepted idea, says Bernheim, is from the psychological point of view as well as from the medical point of view, a suggestion. A suggestion may be direct or indirect, reasonable or unreasonable, brought about by
(a) mere verbal assertion,
(b) hypnotic state,
(c) persuasive explanation, rational or emotional,
(d) emotion (that is, emotion not the effect of any form of suggestion offered by the physician, but emotion brought about by some event affecting the sentiments of the subject).
Epilepsy of emotional origin.
A lieutenant without neuropathic tendencies (except that his mother was in a hospital for the insane) was under shell fire for some time. Finally, a shell burst near him, whereupon headaches and transient spells of confusion followed. Shortly upon the news of the death of his Major, he had a spell of violent excitement and confusion, dancing about on the ground and breaking things up. He passed into a stuporous condition with a suggestion of catatonia. There were a few isolated delusions to the effect that he was poisoned. After sleeping a long time, he suddenly cleared up. There was an extensive amnesia covering a period of weeks. He had forgotten the Major’s death and everything thereafter. He complained of headache, difficulty of thinking, and forgetfulness. An agoraphobia developed, as well as great sensitivity to sounds, and a feeling as if the bed and surrounding barracks were moving. There were a few illusions of a visual nature. He had complete insight into his condition. Conduct was normal. There was general hyperesthesia and ageusia.
According to Westphal, this case of deep disorder of consciousness of some duration in a healthy person is probably one of a dazed state following the so-called “affect epilepsy.”
Is Case 73 Shell-shock? Note that, in Case 73, the shell explosion at first occasioned mere headaches and confusional spells. The true occasion of the convulsions appears to have been the news of the death of a superior officer. It is, of course, possible that the transient spells of confusion were actually epileptic equivalents. Lépine remarks that Pierret and others, observing such spells of confusion often accompanied by agitation, have inquired whether manic depressive psychosis is not a kind of epilepsy. This question remains unresolved. These phenomena of epilepsia larvata (see also Case 81 of Juquelier and Quellien) are to be sharply distinguished from attacks of confusion occurring in pronounced epileptics. These latter attacks often follow a crisis and suggest exhaustion; sometimes they last several days.
Fatigue; fear; hysterical convulsions. Visual aura (approaching fire wheel) built up after the third crisis (scotoma after look at sun).
A sapper, 23, with his company under heavy bombardment, October, 1916, was overcome by weariness and fear (he had always been of a timorous disposition). The order for the rear came, but the convoy was hardly en route when the sapper felt a griping in the pit of the stomach and the blood going to his head; whereupon he lost consciousness and went into convulsions.
This incident seems to have made a powerful impression upon the sapper. A fortnight later, while working in the trenches, he had more epigastric sensations with vague discomfort. He thought about the earlier crisis and about his wounded comrades, and again fell down and had more convulsions lasting a quarter of an hour. The tongue may have been slightly bitten in this seizure. In the genesis of this second seizure we may consider that the feeling of discomfort and the epigastric sensations served to recall the first seizure, so that the second one may be regarded as due to autosuggestion—that is, as hysterical.
A little later, on a hot day in the trench, while working, the sapper turned to a comrade and saw a great black spot on his face. He turned toward another and saw another great black spot on this face also. He was frightened, felt strange sensations, fell, and had a third convulsive crisis. The black spots that he saw were due to a scotoma, the result of a transient glance at the sun.
After this scotomatous episode, his crises always had a visual aura. He would feel rather uncomfortable, leave the supper table, feel a gastric sensation, warmth in the face, and oppression. He would go out in the cold for the air, look about for something, appear frightened, fix his gaze upon a certain point, and cease to reply to questions. His head would jerk back suddenly, and he would utter strangled cries[99] of fear. He was now evidently prey to a terrifying hallucination. In ten minutes, everything had gone again, leaving him trembling with emotion. He would then relate how, after the epigastric sensation had begun, he tried to see if he could make out something abnormal; whereupon a little fiery wheel would appear and roll up nearer and nearer, so as to almost touch his eyelids. He could see his comrades to the right and to the left of the wheel; he could hear questions but could not answer. Just as the fire wheel was about to blast him, consciousness was lost and the fits came on.
War strain; anxiety; confusion; fugue. Demotion and detail to the interior.
A lieutenant, 25, an officer in a regiment on active duty near the front, was called before a special board charged with desertion in the face of the enemy. He had been assigned to a certain position but not only had not complied with the order, but had wandered off to the British sector and been arrested there as a spy.
The prisoner was well developed, without stigmata; heredity, negative. His career in the army had been courageous and he had been advanced several ranks and was about to be given a medal for bravery. He said that he had been under a severe strain for several days.
One evening he had been given the order to attack. The artillery opened fire. He found that the Germans had erected barbed wire defences. The loss of men was terrific. His order was to shoot all who held back. A poor territorial crouched down and would not go forward—supplicating the prisoner not to shoot him. The prisoner spared him.
The next night the order to attack the German trenches was again given. This time he was overcome with anxiety and discouragement. The last he remembers was the order to attack. Next day he felt sick and his mind was foggy. He remembered leaving his regiment and wandering round for several days until he fell into the hands of the British and was arrested. Then he understood what he had done.
The prisoner asked to be allowed to return to the front. The testimony of one of the lieutenant’s men verified his statements. On the day before he left the front he had been anxious, had cried often, and would speak to no one. On the day he left the trenches without permission, he was nervous and disoriented.
There was no doubt that simulation could be ruled out; the differential diagnosis lay between a “confused state of emotional origin” and an[101] “epileptic dazed state.”
For epilepsy there was a history of attacks with falling to the ground and loss of consciousness, without involuntary micturition or biting of tongue, during the time when he was a sergeant. Moreover, irritability and unwarranted suspiciousness had been present at these periods. However, there were no other epileptic symptoms; these two attacks were isolated and of quite long duration, leaving no headache or malaise after them. Also there was no basis for the diagnosis “epileptic dazed state,” since there was no abrupt commencement; the loss of consciousness was never complete (the subject was able to converse with persons while the attacks were on); and some remembrance was present of incidents during the attacks.
For Barat, the important points are that the attacks were preceded by long periods of anxiety and the disturbances resulted more from moral than physiological causes.
The importance of the psychological factors lead the author and his colleagues to the diagnosis “Mental confusion of emotional origin.”
The board decided to return him to the interior and give him a barracks position at the reduced rank of drill sergeant.
A solitary epileptic episode in an artillery officer (slight concussion of the brain two years before) following extraordinary campaign stress (38 artillery battles in two months).
A first lieutenant of artillery, 35, was able to count 38 artillery clashes in which he had taken part in two months of very strenuous, almost daily fighting. Then appeared headaches, anxiety, dizzy feelings, insomnia. Finally one day suddenly, after eating, the lieutenant sustained a loss of consciousness with convulsions, which sent him to his home reserve hospital. The officer had felt nothing before his convulsions came on. The medical report, however, yields no doubt of the epileptic character of the attack.
When he was examined, there was a slight psychopathic depression with a feeling of insufficiency, anxiety, insomnia, restless dreams, over-sensitiveness, and a pessimistic outlook on the future. There were no epileptic traits whatever. There was nothing alcoholic, luetic, or arteriosclerotic about the officer. There was nothing in the childhood or youth of the patient, though there had been a fall two years before, with phenomena of concussion without sequelae. In fact, this fall with concussion had led to no medical examination.
As to the relation of the concussion two years before to the epileptic attack, Bonhoeffer is inclined to interpret the case as one of genuine “reactive” epilepsy on the basis of continuous overstrenuous work for a period of weeks. He regards the previous concussion as soil for this epilepsy.
Re amount of stress occasionally required to bring out epilepsy, compare Hurst’s Cases 64 and 80. It may be recalled that Bonhoeffer is decidedly of the belief that exhaustion has not brought about any actual psychoses, calling attention to the remarkable absence of psychoses among the Serbians after their exhausting campaigns. A general review of war experience indicates, according to Bonhoeffer, the marked power of resistance of the healthy brain.
Nocturnal narcoleptic seizures accompanied by spells of somnolence in the day, both to be regarded as due to the “brain fag” of trench life.
A tradesman, 23, had been in the German infantry since the beginning of the war. Never sick, he had been, in a general way, nervous; and a brother had had, at the age of 30 years, some sort of severe brain disease, in which he became blind, dying a year later.
The man was for a long time in the trenches and proved himself a courageous and stalwart soldier. He went to hospital after a slight bullet wound of the leg, with a benign paralysis of the peroneus.
In the hospital he began to show a somewhat pronounced emotional depression, with a nervous tachycardia.
Friedmann reports the case on account of certain peculiar seizures which, upon the man’s own story, had begun five weeks before, in the field, although he had told no one about them. He had never felt anything like them before. At first, they came three to five times almost every night. He would suddenly wake and find himself unable to move, to speak, or even to think. These seizures, however, were not accompanied by any feeling of anxiety or any respiratory distress. Consciousness remained clear, and after 10 or 15 seconds, he could begin to think normally again. It was clearly a question of psychopathic absences of a mild narcoleptic type, occurring, however, only at night.
Daytimes, also, throughout the whole period in which the nocturnal absences occurred, there were seizures of another description. During the many hours in which he had to sit in the trench, about twice a day for half an hour long, he would plunge suddenly into a sort of irresistible lethargy. Without any external occasion whatever, there would be a feeling of great fatigue. In the spell he could not move or think, would lean his head upon his hand. He was unable to overcome the feeling of weariness and became convinced[104] that he was ill, and that the fatigue could not be natural. However, he did his work like the rest. Friedmann interprets these spells as a kind of imperfect sleep.
The patient was physically healthy and stalwart, mentally not excitable, and tolerably tranquil in the midst of shell fire. He would never have been reported sick had it not been for his wound. Aside from the tachycardia, of which he himself complained little, nothing wrong was found in the hospital. There was, to be sure, a feeling of discomfort without any hysterical tinge, and sleep was restless. Aside from the peroneus palsy, the injury made a good recovery. The nocturnal attacks persisted; bromides and even luminal failed of effect. There was, however, no longer any somnolence by day. In fact, for the five weeks of observation, there was no change in his condition.
Friedmann states that mild emotional alterations are not infrequent in the trenches with minds disposed thereto, although emotional shock, especially in shell fire, is the most frequent cause. However, these particular seizures are quite unusual. The stresses of field service lead to a sometimes complete paralysis of mental power, interfering transiently with service. There is no evidence of sudden circulatory disturbances such as would bring about dizziness, pallor, nausea, or fainting spells. According to Friedmann, the regulative brain functions, especially those that maintain consciousness, become weak on account of a condition which he terms Gehirnmüdigkeit, or, as we should say in English, brain fag. The situation forbids due completion of sleep. Thus, the explanation of the daytime attacks follows rather obvious lines of brain fag. The accidental awakening it is, which at night produces the absences; the wakenings are due to the general restlessness of the patient. The general weakening of cerebral function produces the disorder at the moment of wakening, since the regulative factors of consciousness are already out of order. The condition in the absence rather closely resembles the state of consciousness just before going to sleep, and also perhaps the state of consciousness during the process of awakening. It is as if the process of waking were somehow delayed a few moments. Friedmann[105] is interested to show the relation of such absences to the so-called gehäuften kleinen Anfälle, originally described by him in 1906 as occurring in children, and distinguished from epileptic attacks. These attacks, after lasting for years, finally disappeared completely. The same sort of thing in adults was symptomatic of some other disease, such as neurasthenia, and was not a true entity. In children these attacks failed to be attended with any mental injury, nor were there any pronounced epileptic phenomena. Bromides had no effect upon them, and they already showed a somewhat striking and peculiar appearance, involving interruptions ten seconds long of capacity to think, speak, or move, without disturbance of consciousness or automatic movements. Sometimes the attacks occurred from six to 100 times in the day, without in any respect interfering with the general condition of the child. The occurrence of such series of mild seizures is nothing but a syndrome. To be sure, some cases turn out to be cases of genuine epilepsy with an eventual degenerative process. Some forms belong in the spasmophilia group, and some among the hysterias. However, according to Friedmann, there is a narcoleptic petit mal that is an entity by itself, proceeding after a period of years to complete recovery without complications. It is this form which may be regarded as a peculiar kind of brain fag. The case of the soldier may be supposed to be one which will prove to have this benign outcome.
Sham fits.
An unwilling conscript developed numerous fits on board ship coming from Jersey, three days after enlisting. Fifty more developed during two days in hospital. He was sent to Netley.
On the hypothesis of hysteria or malingering, he was hypnotized. A fit was suggested to him, but did not come off. The Sister was informed in the patient’s hearing that the man was clearly shamming, as in all genuine cases a fit would occur after this treatment. A fit with marked opisthotonos immediately occurred. This fit immediately stopped when he was ordered to stop it and to wake up.
The man after waking promised to have no more fits.
Epileptoid attacks, controllable by will.
A man was received in No. 3, General Hospital: Diagnosis, epilepsy. He was shortly sent to the convalescent camp and then returned, having had two attacks. Russel watched for another attack, felt it was not genuine and “put the situation up to” the soldier whose story was as follows: He had been at the front without leave for twelve months since the German retreat. Leave was due him. A sister’s letter said his brother was severely wounded and his mother was praying for his return. When he thought these things over an attack came. He could, however, control the attacks. Russel told him, if he would play the game, he would be sent to the base with a recommendation for leave. In ten days the man was remarkably changed and had no further attacks.
Hereditary epileptic taint brought out by two years service with eventual shell-shock and burial thrice in one day.
A private, 24, in the army from 16, never epileptic (sisters epileptic), was wounded four times in the war from September, 1914. Shell fire did not worry the man, but he gradually became depressed after his father and five brothers had died in active service. He was blown up and buried three times in one day in July, 1916. He was unconscious for two hours after the second blowing up, but carried on for two hours more until blown up for the third time.
After this, he became nervous and shaky, and began to sleep badly, and a month later had a typical attack of major epilepsy. Fits occurred with increasing frequency. As many as 19 occurred in a single day. Rest and bromides caused the fits to cease, and there had been none for six weeks at the time of his discharge.
Re the extraordinary delay in the bringing out of this epileptic’s taint, refer back to Case 76 of Bonhoeffer, with its discussion, and to another case of Hurst (64).
Re Shell-shock and its relations to epilepsy, see below, discussion under Cases 82-84 of Ballard, who has erected a theory of Shell-shock as in some sense epileptic.
Shell-shock: Epilepsia larvata.
A soldier, 29 (father alcoholic, died in hospital for the insane), a decorative painter without plumbic history, non-alcoholic, non-syphilitic, was wounded once, September, 1914, but returned to the front in 1915.
May, 1915, a shell burst near him. He lost consciousness, regained it a few days later at Brest, and was so far recovered that he could go on leave in seven days. While on leave, he had short attacks of delirium, followed by a total amnesia; there was, however, no crisis, fall, or convulsion. After the first attack, he had for 24 hours malaise and headache, but got well and went back to his dépôt. Shortly afterward more attacks of this sort recurred, and he went to hospital and thence to the neurological centre at Tours. Whence, August 9, 1915, he got a two-months’ leave for “mental disorder post-confusional, second état, probably hysterical (commotio cerebri), and organic hemiparesis.”
November, 1915, after returning to the dépôt, there were more spells and he went again to hospital. Invalided December, 1915, he passed a year at home, but the spells continued. Although the epileptic nature of these attacks was maintained by Francais at Évreux, he was placed in the auxiliaries, December, 1916, but had to go to hospital almost at once, and, February 28, 1917, entered the neurological centre of the 9th Region for the second time. Here, when called to be examined two days after admission, he was observed in an attack. He suddenly rose from the bench, made a few steps, seemed to be listening and anxious, as if he ought to be on guard. He looked up, seemed to be looking for something whose noise was approaching, lowered his head, made a slight jerking movement, and said, “Poum!” as if to express the noise of an explosion. He took a few more steps, the same movements were repeated, and the same “Poum!” was uttered. This lasted for about a quarter of an hour, during which the patient was unaware of his surroundings. He could be guided all about the hall without[109] resistance, but did not respond to orders, commands, noises, or contact. In short, the patient was in the midst of a hallucinatory dream at his post in the trenches, undergoing a bombardment. He was placed in a chair; remained motionless for a few seconds, woke up, and answered questions. “Where am I? Oh, yes; I must have been sick because my head feels bad.” In answer to the question. “What did you see; what was there?”, he said, “I don’t remember anything. I never remember. I don’t know.” The patient was dull and weak after the spell.
These spells varied in number but occurred once a week. The patient was able to tell of certain attacks that had occurred while he was out of doors at home.
Now and then, there was another theme in the hallucinatory delirium, namely, a pencil drawing of a woman’s picture, of no great artistic worth but carefully done, at which the patient was much astonished on awaking.
It seems as if auto- and hetero-suggestion can be eliminated from the genesis of these attacks. Neither hysterical nor epileptic crises have preceded or ever alternated with these seizures. Nevertheless, on the organic side, the patient had a general increase of tendon reflexes on the left side, most marked in the knee-jerk, and fell to the left in voltaic vertigo. There was a left hemiparesis, apparently of organic origin, which had been determined as far back as July, 1915.
There was no true dementia. Past memories were but slowly recalled, and inattention interfered with the fixation of recent memory. He complained of troubles in his sleep and dreamed of war experiences somewhat analogous to those in his attack of amnestic delirium. After the seizure, there was a marked hebetude and mental inactivity, torpor, and a severe headache. The case was presented to a special commission as one of epilepsia larvata in a person hereditarily predisposed who had never before presented epileptic signs, suffering from a disease characterized by frequent short attacks of hallucinatory and delirious automatism, following shell explosion which had at the same time produced a slight left-sided hemiparesis and mental inhibition.
To illustrate an epileptic theory of Shell-shock; three cases:
1. Fugue; minor symptoms: later, epilepsy.
2. Epileptic confusion eight months after explosion.
3. Mine explosion: stammering replaced by mutism; mutism replaced by epilepsy.
Atmospheric concussion from shell explosion, October, 1915, was followed by unconsciousness in a soldier described by Ballard.
Blindness for a month followed recovery of consciousness. “Neurasthenia” (anxiety neurosis) after return of sight. Apparently nearly complete recovery after latent period of a few weeks. Return of blindness in one eye in December. Five days automatic wandering (the man was found in a west country town five days after leaving home to rejoin his dépôt and seen by a medical officer who reported that he was dazed and amnestic for that period); admission to second Eastern General Hospital, December 15.
On admission he proved to be suffering from minor hysterical symptoms such as an inability to open his eyes and to see clearly when the lids were raised. The symptoms rapidly cleared up under suggestive conversation and did not return except for amnesia and slight emotional depression. He remained well until December 25. On that day he began for the first time to have definite epileptic fits and nocturnal epileptic delirium. In January he was discharged as an epileptic. There was no epileptic temperament or feeblemindedness. Finally, there had never been any personal or family neuropathic or psychopathic history.
A soldier was blown up, April, 1915, and had a spell of unconsciousness. Later, pains in the head, slight amnesia and a condition of asthenia developed.
He was eventually admitted to the second Eastern General Hospital at Brighton, January, 1916. At the time of admission he was semiconscious, stuporous, confused, disoriented, anxious in a dull sort of way, talking about his expectation of “a sailor with a card.” Speech was intelligible, though fragmentary and infrequent. The man obeyed commands but gave no replies to questions. The mental processes were slow and impaired.
According to Ballard, we have here a case of epileptic confusion, eight months after the initial concussion. This particular attack ceased three days later, leaving amnesia for the attack and a certain amount of mental retardation. The man was not epileptic in temperament and his personal and family history proved negative.
A soldier was buried in a mine explosion, October, 1915, and for several days thereafter was unconscious or semi-conscious. He emerged deaf and subject to stammering and a condition termed “neurasthenic.” The stammering was soon replaced by mutism, which lasted several weeks. The mutism was then supplanted by epileptic fits.
He was observed by Ballard in a dreamlike, disoriented and inaccessible state, in which he was anesthetic to pin pricks, lay awestruck, dumbly following with his finger hallucinatory airplanes. Flexibilitas cerea was also shown at this time.
Next day he emerged from the dreamlike state with mental processes somewhat slowed, disorientation for time, amnesia for the attack, memory disturbance and a return of the stammer. On the next day following, all these symptoms had disappeared except amnesia for the attack. Another spell of epileptic fits occurred later. It seems that the man had had a convulsion thirteen years before and occasional convulsions since. In fact, he, seven years before, had had what was called “a stroke” and residuals of a slight hemiplegia were still present. (There is no statement in the case report relative to syphilis.)
Emotion; shell fire: Epileptic equivalents.
A man, 19, suffered from shock due to emotional stress and shell fire. He had terrifying dreams. After a short time, he developed paroxysmal attacks of maniacal excitement. Just before the first attack he had been helping in the kitchen, lay down on his bed, went to sleep, woke, startled, flushed, and sweating, and made for the door as if terrified. He remained in this state as if suffering from hallucinations of sight and hearing, and without ability to recognize his wife, the doctors, or the Sisters. When two strangers in uniform came in to observe him, the adjutant became violent, as if the uniforms had started terror anew. The attacks lasted from a few hours to a few days, coming on suddenly, without apparent cause. One day he tried to get over the wall of the playground. He came back and buried his head in his hands. Major Mott spoke to him, whereupon he got up, looking terrified, made for the door, and four orderlies were required for his restraint. At Napsbury Hospital, to which he was sent, he made a complete recovery.
Mott suggests that we are dealing with a psychic equivalent of epilepsy.
Re epileptic equivalents, compare notes from Lépine under 58 and 59.
Pathological intoxication.
A Territorial infantryman, aged 37, was in the habit of drinking a good deal without getting drunk, and at the front drank a good deal of bad brandy. He had just taken a considerable quantity when his regiment got the order to charge. The charge was hardly over when the man became greatly excited and hallucinated. He thought he was surrounded by Germans and tried to transfix his comrades with the bayonet. Howling and struggling he was carried to the rear.
He was soon brought to the asylum at Fleury after howling all night and seeing the Boches and animals fighting among themselves. His hands and tongue were tremulous and there were cramps in the calves of his legs. On the 6th he expressed astonishment to find himself in hospital and was found to have but slight memory of what had happened. He remembered, however, that he had tried to kill his comrades. With the deprivation of alcohol he became rapidly normal and was sent back to the dépôt in a few days.
Re alcoholism under army conditions, Lépine remarks that alcohol has played in this war a rôle analogous to that of malaria in the epidemiology of some countries. Many of the victims are, to start with, unbalanced subjects and détraqués who are hereditary alcoholics. Alcoholism, according to Lépine, dominates the pathology of the interior and has a marked bearing upon conditions at the front. In fact, alcoholism would have been disastrous in France had not measures been taken against it; measures still insufficient (1917). More than one-third of 6000 cases studied by Lépine during three years have shown alcohol as a sole or, at all events, principal cause of the difficulty. It would be within[114] reason to state, according to Lépine, that if we throw in cases in which alcoholism was a partial factor, more than half, or even more than two-thirds, of the mental cases had been strongly influenced by alcohol. Lépine thinks there may be effects like those of anaphylaxis. Certainly, the startling and sudden effects in so-called pathological intoxication, as in Case 86, suggest the critical and vehement effects seen in the sensitized anaphylactic subject.
| I. | Antebellum phase of Psychiatric Neglect: Groundless fear that recruiting would be disorganized by psychiatric sifting processes. |
| II. | Phase of Alcoholism of Mobilization: Hospitals unprepared. |
| III. | Phase of the Marne: Alcoholism restrained by law; psychoses few; psychiatrists optimistic. |
| IV. | Phase of Trench Warfare: Overemotionality; and of High Explosives (January, 1915); now psychiatric services were systematically established along evacuation lines. |
| V. | Phase of Systematic War Psychiatry: Filterwise system of management (a) near trenches, (b) in main body of army, (c) on evacuation lines, (d) special hospitals. |
Chiefly from data of Chavigny, 1915.
Pathological intoxication: criminal prosecution stopped.
An orderly, in private life a teacher, one day about noon-time, when going on duty, called the commanding officer to account because he (the orderly) had had to wait. He said he had been ordered to come at two o’clock and it was already long thereafter! He was severely reprimanded but addressed a number of the officers present with questions having no relation to military service. In fact, he seemed to have forgotten entirely that he was on military service.
This was the more remarkable as the teacher-orderly had many times distinguished himself upon dangerous patrol expeditions and in critical situations, winning the confidence of his superiors and the likelihood of promotion to corporal. He had been a discreet, earnest, and clever soldier.
Loewy observed him during this affair and noticed that he did not by language or movement suggest intoxication or hilarity but merely a certain excitement. He was entirely oriented for time, place and person, and his outward behavior was correct enough except for his military rank.
Sent to his quarters near by, he gave the impression to his immediate superior officer of deep drunkenness. He murmured something and soon fell into a deep sleep. After waking, he had an almost complete amnesia, knowing only that something disagreeable had transpired. He remembered that he had been offered several little glasses of cognac brandy by a comrade, and that he had drained them off quickly before going on duty. He said that he had never drunk cognac before, and in fact had drunk nothing for a long time.
The diagnosis of pathological intoxication was made, and the soldier was thereby cleared of his dangerous situation; a criminal prosecution was not instituted. He thereafter behaved with entire sobriety and modesty, and he achieved his corporalcy and later became file leader.
Desertion in alcoholism may deserve the term “pathological.” Case of fugue.
A “deserter” said: “I went because I drank a glass. I just went, comme ça, without any motive.” He was somewhat feebleminded and, in explaining the impulsivity of his act, he added: “I went like a broken-down beast. I walked straight ahead, without knowing where I was going and if I had been going to be killed, it would have been all the same to me.” He could not that afternoon remember very well; but next morning, after having slept, he regained full consciousness. He said that he then found himself in a field near a cemetery. He had carried his gun and equipment with him, but had lost them somewhere, and from a military point of view, his desertion was complicated by loss of effects. On coming to, he said to himself, “Where am I? How foolish after fifteen months in the line! Probably I have deserted again.” In fact, he had a month before left his post under exactly the same conditions in the midst of a period of alcoholic excitement.
This alcoholic fugue is typical: drunkenness, impulsive and subconscious ambulatory automatism, with partial amnesia, disorientation, with mislaying of objects, followed by sleep and immediate return to normality.
Re fugue, see discussion under Cases 58 and 59. The French military code cannot excuse victims of fugue even though executed in a quite unconscious state, if the fugue is due to alcohol. There was a certain procursive suggestion in the fugue of Case 88, who went “like a broken-down beast,” straight ahead, without knowing where he was going.
Alcoholism: Amnesia experimentally reproduced.
February 15, 1915, a German soldier drank beer in the canteen and at roll-call appeared tipsy. He then went to bed, but rose an hour later to go to town. A quarter of an hour later, he went to a clerk’s house and asked for paper, on the ground that the next day he was going to march to Warsaw. The clerk gave him no paper, which he then tried to get by force. A policeman arrested him and he said, “You just wait, lame dog!” Upon examination he denied that he had ever been guilty of any crime but had been in institutions on account of delirium. In point of fact, this man had grown up in very bad surroundings, amongst quarrels and disputes of his parents, who kept a disorderly house. At 19 he had been convicted of incest. He finally admitted having been convicted for rape. It was found that he had once run out into the front trenches; had been removed by an advance guard to a stable, and then wondered why he was not in school. He described a number of attacks of delirium although he had not drunk more than moderately.
He was given an experimental dose of 50 c.c. of alcohol, and in ten minutes became excited, tried to get out of bed, attacked other patients without reason, and was able to speak neither spontaneously nor in response to questions. In a period of two hours he became clear and asked what the trouble was. He knew only that he had taken alcohol.
Re the experimental excitement produced in Kastan’s case by the exhibition of alcohol, it is of note that Bérard has been much impressed by the agitation that surgical cases of alcoholism undergo when anesthetized. It may be that the anesthetics act similarly to the experimental alcoholism of Kastan’s case. According to Bérard, these phenomena of the anesthetized wounded (who are men recently evacuated from the front and other hospital cases) are of larval alcoholism brought out by the anesthesia. Bérard wonders whether rum issues at the front are at all responsible therefor.
Desertion, drunk. Contributory factors.
Gottlieb S. left the barracks, January 25, 1915, met friends and drank with them, remaining all night in the railway restaurant and waiting room. He was promptly arrested.
According to the patient, he had always drunk a good deal and had once fallen from his horse in the campaign, and become unconscious. After this fall, he said he had been able to stand less alcohol than before.
There is doubt as to the syphilis of Gottlieb. He said he had been infected once, but his further statement that he had six relapses is, of course, questionable. As to the hypothesis of feeblemindedness, it appears that in childhood he had learned badly and had been a stammerer. He had been a herdsman, and after that a laborer. He finally became a travelling man for a specialty photographer.
He had previously been convicted of an embezzlement, brawling, and breach of the peace.
As to his military crime, he said he had been celebrating the emperor’s birthday the last three days, being urged on by acquaintances and drinking whiskey. He was, in fact, on a spree and did not eat properly. He had met a student in the railway station and had forgotten all about his military service. He remembered having spoken with the waiter, remembered telling the student that he was going to commit suicide, and the student had drunk seltzer with him. January 29, he for some reason drank no more, and then it occurred to him that he ought to go back to duty. He remembered that he was easily led astray. He had once thought of becoming a tanner but had been dissuaded from the trade because of its bad smell.
The analysis of this case must consider, first, syphilis. Supposing, however, that this hypothesis is not substantiated by laboratory findings, the hypothesis of feeblemindedness might well be raised. It seems possible, if not probable, that this patient was in the subnormal group, lying between normality and feeble-mindedness[120] proper. The value of mental tests would here be extreme. There seems to be no evident epilepsy, and the majority of the phenomena can perhaps best be explained by alcoholism. Possibly the case is one of so-called pathological intoxication. The patient’s own story that, although he had been always subject to drink, he had been less tolerant of alcohol since a fall from his horse, seems to be entirely consistent with the post-traumatic history of numerous cases, so that it would hardly be wise to consider that alcohol accounts for the whole story. We must raise then in succession the hypothesis of syphilis, feeblemindedness, alcoholism, and coarse brain disease, bearing in mind also early stammering. As to the utilization of such a man, it would appear that a supervision of him with absolute countermanding of alcohol in view of the decrease in tolerance of alcohol since the fall from his horse might perhaps preserve this man for some form of military service.
Re German and French war alcoholism, Soukhanoff remarks that the conditions in these countries were in strong contrast to those in Russia. In Russia there was a great decrease in the number of cases of acute alcoholic psychosis; particularly at the time of mobilization, there were few cases of alcoholic psychosis. He says that during the Russo-Japanese war, alcoholic psychoses constituted a third of all the mental cases observed. This figure corresponds with that quoted above from Lépine (see under Case 86). Soukhanoff, writing in 1915, had not observed personally a single case of alcoholic psychosis. Incidentally, the number of cases of psychosis in the Russian army had remained in general small.
Desertion by mild alcoholic dement.
Emil S. made a number of statements when he came for examination. He had once had a treatment by injections. Both his mother and his grandmother had been insane. He said that his brother was an officer in the navy, but this statement was found to be false.
According to his story, he had lost touch with his troop at the end of September, 1914, and had lived in several lodgings in T—— up to October 19, when he was arrested. He said that he did not know that a man who had lost touch with his troop had to report.
A week after his arrest, S. entered a shop and asked for coffee, saying that he had a furlough of 24 hours and wanted cake for his comrades. He said he was the owner of an estate and would send a roebuck for the cakes. The shop-man gave him cakes to the value of one mark. Bystanders said that he had been lodging in T—— for about two weeks. It seems that he had told his landlady that a city official had quartered him upon her and that he was on furlough. He went away in the morning and came back in the evening. He had written to a bank of which he had once been a representative, asking for money. One night he had lodged with another landlady, being given a meal, and he had there stated that he was in the City of T—— on duty and that his horse was in the barracks. He offered a thousand marks for his board and lodging.
At another lodging he had given himself out as a courier. In fact, the letter to the above-mentioned bank had been signed “Otto S., Land-owner, at present, courier.”
“If I do not revoke this in person or by writing on January 1, 1915, I beg you to pay to Mr. and Mrs. M. of T——, one thousand marks and deduct it from my balance.
“This is to be considered as my last will. As witness: present: Joseph B.”
The letter was addressed “To the direction of Commercial-Counsellor P——.” There was no stamp on the letter.
A second letter reads:
“Honored Sir, Commercial Counsellor:
I beg you to send by return mail to the address given below 1000 marks, and deduct this amount from my account. I have been in Russia. Well, things are moving now. Thank God, we have reached the point we have. Write me please more in detail about my property and estate and give me your very valuable advice.
With best regards to your esteemed wife, I remain
Sincerely and respectfully yours,
Otto S., at present courier, otherwise, land-owner.”
As for this Commercial-Counsellor P., P.’s son stated that his father had been dead for three years and a half.
S. gave himself out in T—— as a land-owner, falsifying his name, asking for beer to the amount of a mark a day, borrowing from his landlady ten marks, paying nothing, but remaining on friendly terms with the landlady and her women lodgers, making a contract with a superintendent ostensibly for his estate, and borrowing money from him.
Observed in the clinic, he said he was a bank representative and had been very nervous since being divorced in 1911. The divorce was due to his wife’s adultery. Sometimes he would not know really what he was doing, once even tried to shoot himself, and again once threw a burning lamp into his wife’s face without knowing it.
He had gone to the City of T—— without furlough in October because others used to, too. Only five days later had he noticed that his troop was no longer there; and upon inquiring about the troop he could find nothing as to its whereabouts.
He had been a heavy drinker and was always somewhat intoxicated, which, according to the patient, made him forget everything. He had drunk 20 glasses of beer and liquor daily. He wrote to P. because he knew his father.
As for the frauds, he said he knew nothing about them. He did not know even the baker from whom he had gotten the cakes. In fact, he had been drunk the whole day long.
He said that he had learned badly in school and had not passed any examinations. In active service he had already been convicted of drunkenness once. Referring to his treatment by injections, he said he would rather be dead. He had only sought diversion in looking over estates. Both his ability to reckon and his memory had suffered greatly. He and another patient eloped from the clinic one day but were captured a few hours later.
Remarks: Details are lacking as to the physical and laboratory side of this case. On the whole, there appeared to be no convincing features of paresis or cerebrospinal syphilis. The phenomena are very possibly in part alcoholic. There appeared to be no sensory disorders, and in particular no hallucinations. The intellectual disorder is chiefly amnestic. There is little or no evidence of emotional abnormality. The curious conduct seems hardly to indicate a primary disorder of will. The main feature psychologically appears to be amnesia coupled with an inability to reckon. To be sure, the letters are written externally in sufficiently good form; the amnesia does not appear to extend to details. It is a question of whether the disorientation which one suspects is not merely amnestic. On the whole, however, it would appear that there must have been at various times disorder of consciousness, as indeed is indicated by the patient’s own account of his ignorance of the cake-roebuck episode.
Dismissing the hypothesis of a syphilitic dementia, we might cling to that of alcoholic dementia more or less punctuated by acute alcoholism. Yet it is also possible that the patient was actually somewhat feeble-minded; this would be consistent with his own statement. The question might arise whether this soldier could have been excluded by careful psychiatric examination before entering service. It would seem that a knowledge of the insanity of the mother and grandmother, and an inspection of school records, if available,—to say nothing of the episodes which may or may not have been accurately related, between himself and his afterwards divorced wife—would have sufficed to throw doubt upon the military effectiveness of this man. We know also that he had already been convicted of drunkenness on military service before the episodes mentioned.
Desertion by alcoholic. Contributory factors.
Carl B. was a soldier about whom the captain thought that his intellectual power had been weakened by drink. An inquiry after arrest showed that he had been odd also at home. He had once been sued for perjury, but the suit had been stopped for lack of evidence. He had been several times convicted of drunkenness. It appears that on March 30, 1915, after mounting guard, he said nothing and went home, remaining at home until the next day and then returned to the guardhouse in the street-car. He declared, this time, that the non-commissioned officer had given him permission to leave, although this statement was not correct.
Again, on April 6, B. was about to leave the quarters, but the surgeon, finding him drunk, kept him back. He did not go home that night, and the next day when he was wanted at the hearing, he could be found only in the afternoon. He replied confusedly and somewhat irrelevantly to the questions asked. On arrival at the clinic he was in tears and much depressed. Given 50 grams of alcohol, he became somewhat livelier. Upon examination, his perceptions were found diminished; he felt, he stated, a cracking and crackling in his neck. In his cell he had felt as if sparrows were roosting in his face; he had heard voices and seen pictures, and had not known what he was doing. He asserted his innocence, blaming his imprisonment for all his troubles. He had been in the habit of drinking three liqueurs and two glasses of beer a day. He had been drawing a pension since a fall from a scaffold.
A sister had suffered from continual headaches. The patient himself had three sickly children and ten of his children were dead; there were also two premature births.
The analysis of this case would clearly show the benefit of considering, first, the hypothesis of syphilis. Not only is the history of his children suggestive, but the impairment of mind noted by the captain as due to alcohol may very possibly be syphilitic in origin.[125] Examples in division he could not solve, and it is a question whether his leaving guardmount is not in part related to disorientation for time. There appears to be no evidence of feeblemindedness and none of epilepsy (though a sister suffered from continual headaches). Alcohol may account possibly for the entire picture and is particularly consistent with the false voices and figures, the sparrows in the face, and the sensations in neck and the tickling in the ears. It is possible, also, that intolerance to alcohol had set in since the fall from the scaffolding for which a pension was being received. It does not appear necessary to consider any further of the groups of mental disease. Syphilis, alcohol, and a post-traumatic brain condition, all may play a part. Alcohol is able probably by itself to produce a number of these symptoms, and these alcoholic symptoms would be probably the more readily produced in virtue of the post-traumatic intolerance that we may assume.
A disciplinary case: Alcoholism.
A German soldier, brought up for examination for disobedience and insubordination with intoxication, was found already to have been convicted 33 times of a variety of crimes. Once he had drunk a bottle of shoemaker’s polish, evidently with suicidal intent.
In the canteen he had assaulted superior officers and tried to strike a sergeant. He said he had been attacked by the sergeant and pushed into a cell, whereupon he had lost his mind.
He came from a family of drunkards, and had been himself very alcoholic formerly. On the day in question, however, he had drunk very little. According to his account, he had fits of this sort if any one injured him. He was amnestic and had forgotten his previous convictions. Anything he might have done, he said, had happened a long time ago, in his youth. For example, concerning a theft, he said that it was merely that he had fallen into some Christmas trees and stuck fast there, and no one wanted to be paid. Tremors of hands, feet, head. Analgesia of thorax.
Re alcoholism and disciplinary cases, we find alcoholism bulking large in Lépine’s account of military delinquency. Fugue subjects are not infrequently alcoholic. Minor disobedience is also often alcoholic. Acts of violence are characteristically alcoholic, or executed by subjects with hereditary alcoholic taint. (Such acts were in France especially common before the anti-absinthe law in 1915.) Alcoholic episodes and impulses often culminate in arson. No doubt, espionage employs alcoholism for a portion of its technique, though delusional mystics and subnormal hypersuggestibles are more often the purveyors of information to the enemy. The theft list, also, shows its share of alcoholics. Alcoholics are less common amongst those who, contrary to rules, assume shoulder-straps or other decorations. Here the sub-normals and victims of imbalance, as well as the drug cases, are more likely to figure if the matter is psychiatric at all.
Remarks upon an atrocity.
April 15, 1915, a German soldier went with three comrades to a farm, to select a sheep for slaughter; they were obliged to go to three farms. The man carried a revolver and cartridges in his pocket. He threatened the farmer that he met with this revolver, and desired to rape the farmer’s daughter. He was very drunk, and said to the non-commissioned officer who was called in at the time, “You have served only a year longer than I have.” He staggered, struck violently with his hand at the sergeant, and gave insolent replies.
He had already choked the peasant’s daughter, scratched her face, and bitten her fingers, hand and arm. She could not run away as she was lame. The soldier held the revolver to her face and shot it off several times, offered sex assault, scratched her feet with his spurs, and tried to twist her neck. The non-commissioned officer threatened to shoot him, and he then became still. He said to the first-lieutenant before whom he was taken, that he would do anything but allow himself to be beaten, and at this moment moved his arms about in the air, and bloody foam came from his mouth. The first-lieutenant previously had always thought him to be normal except for a strange flicker and unrest of the eyes. There was a history that he had already once attacked a servant girl. The man had amnesia for the affair, only remembering how the non-commissioned officer had come on a white horse. He remembered nothing about the peasant and the girl. He said that he had been given to earache on the right side in winter. There was a history of his having fallen from a tree in childhood, becoming unconscious. He had been a sufficiently good scholar up to the second class in school. He had been an excellent soldier.
Alcoholism: Atrocity.
September 15, 1914, a German soldier was missed. He had said that he wanted to get to the enemy quickly, and that he was going to march alone against the Russians. A shot was fired that night by this soldier, on the ground that he had been insulted by a civilian, although no civilian was present.
September 21, a farmer in a wagon reached a farm, where he found the soldier aiming at a woman. He fired, wounded the woman severely, and jumped on the farmer’s wagon and rode off with him. It seems that the soldier had come to the farm at noontime and accused the woman of treachery, ordering her to come with her husband to a certain farmhouse, where she should be placed against the wall and be shot. The soldier had shot her and wounded her husband also. According to the woman, the idea was to take revenge because she had denounced certain persons as spies.
He was arrested during the night, and told how he had left his troop because he could not get at the enemy. He had been informed that there were spies who ought to be shot; there had been talk in a certain inn about it. He did not know he had wounded the husband, and he only wanted to give that dangerous woman a piece of his mind.
After wounding the woman, he had given himself no further thought about her, but had gone to partake of the holy sacrament at the pastor’s. He then had drunk another glass of beer and gone to bed. He was, in fact, still drunk at the time of arrest. He had not been aware that he would be punished for the crime of going alone against the Russians.
Some days later, he wrote that he did not intend to kill the woman, that he had been drunk at the time and was always a bad man when drunk; that he had other times when he absented himself from home for days when drunk. He had had, he said, a number of attacks of delirium, in which he had seen animals. At one time, he had fallen on his head. On the day in question, he had drunk 1½ litres of liquor. He was remorseful for his deed.
A disciplinary case: Alcoholism; amnesia.
A German soldier, New Year’s Eve, 1915, got away from his company, drank whiskey, and came back drunk. He bothered his comrades so that the non-commissioned officer had to call for help; whereupon the soldier said, “A man who comes on late and hasn’t been in much, hasn’t much to say. If it is a non-commissioned officer, I shall hit him in the snout.” The officer kept talking to him kindly but he cried “Halt’s Maul, you crooked …!” He staggered up to the lieutenant without saluting, but at a slight push fell prone into the straw.
It transpired that the man had not been intoxicated enough to lose all control of himself. He did not remember anything about what he had done; he had drunk a half-bottle of rum during the evening. There was a demonstrable lack of memory. He did not know the German provinces, and thought that Bismarck had once been war minister. There was a tremor, hypalgesia of the left leg and analgesia of the left arm and left shoulder.
It was found that he came from a strongly tainted family, with two insane sisters and three insane cousins. He had been a good soldier during his service, but had accused his father of alcoholism baselessly. He had always been difficult to manage when drunk and had been convicted nine times: five for dangerous assault and battery. He drank up to 1⅓ litres of whiskey a day if he got time, and also took ether. For some ten years he had been amnestic for what he did while drunk; nor, according to his wife, had he been able recently to stand so much alcohol. He said that he had had a fall from a wagon in 1911 or ’12, after which he had been unconscious.
Antebellum, run over by an automobile; intolerance of alcohol; episodes of amnesia after moderate alcohol.
A German soldier was advanced in rank February 26, 1915, and in honor thereof drank six or seven glasses of beer. On his way home, he met a captain and failed to salute him. When called to account, he said he could not see, and made remarks about regrettable behavior. He refused to go along with the officer. Afterwards he remembered that he had been stopped by an officer but had forgotten subsequent happenings.
March 24, he was riding in an electric car with a lieutenant. He said to the lieutenant who had unbuckled his sabre, “It is a piece of insolence and improper to unbuckle the sabre.” He repeated the phrase on questioning. He was then asked to give his name, and replied, “I know my name but what is your name, Mr. Lieutenant?” He looked drunk at the time but afterwards remembered nothing.
Physically he was tremulous and showed blepharospasm. His face grew red on bending over.
This man had been run over by an automobile in 1910, after which he had become excitable, slow-thinking and forgetful. The spinous processes were painful on pressure, as was also the hip joint. The history showed that he had been convicted six times of various crimes, such as disturbing the peace, embezzlement, and the like. Since this accident he had not been able to work effectively. He had gone into the army in a spirit of enthusiasm.
Adventure with a stranger in Paris.
A soldier had seven days’ leave in Paris, beginning December 27, 1915, and the first day drank a good deal of wine with another man on leave. They met, in some place that the patient had forgotten, a well-dressed man whom they did not know, and all three fell to drinking. The stranger told them he knew a trick to prolong the leave to 3 or 4 weeks. “All I have got to do is to prick you, and it will cost only 100 sous.” The operation was done at the café after payment in advance. The operation was a puncture with a needle between the middle and ring fingers of the left hand. Next day there was a phlegmon of the dorsal surface of the hand, and he was put into hospital saying that he had gotten a barbed wire prick in the trenches. The surgeon who opened the phlegmon was surprised at its gummy appearance, gangrenous odor, and greenish tint. In point of fact, petrol had been injected.
Morphinism: Tetanus.
Mdm. L. was a morphinist. After the outbreak of the war, she went to a general hospital to recover from morphinism, but was too excited to be kept there. Accordingly, she had to be sent to Sainte-Anne, but upon arrival she developed distinct signs of tetanus.
It seems that Mdm. L. was the widow of a Colonial who had given her the first injections ten years before, for dysentery. She tried several times to stop. Daily dose 1.5 grams.
She was in a cachectic state, and according to her mother, took no care of her syringe, trailing it about everywhere. Her thighs, arms, and anterior aspect of the body were covered with scars. There were small phlegmons in places. Did she inoculate herself with bacillus tetani from an infected needle? In any case, she died of tetanus.
Medicolegal question concerning a morphinist.
A man worked in Paris on the ’Change, where there are a number of syringe victims. He had been brought up in Paris but was not a Frenchman. Enthused by his friends and the prey of deep emotion, he enlisted. He was of an introspective nature and himself wondered whether the morphine did not have something to do with his enlisting. He said, “I had been unnerved for a number of days by reading the papers, and after a number of heavy injections, I went to a recruiting station and signed on.” In his regiment, he continued the injections, but shortly found that he would be unable to replenish his diminishing stock of drug. He explained his unhappy fate to the corps physician, and was sent to Val-de-Grâce. He asked to be retired, alleging that he was under the influence of a poison when he went to the recruiting office and had therefore committed an illegal act.
Fernand and Emilienne were two recidivists in morphinism. Although neither was over 22 years of age, both had been several times convicted of shop-lifting. They stole only if they had no money for morphine. Prostitution served to care for Emilienne, while Fernand was at times a cocaine seller, and at times made money in devious ways at Montmartre. Emilienne’s patronage scattered with the war, and it was the same with Fernand’s. Accordingly, there was no money for either morphine or cocaine. Moreover, the shops being not crowded were easier to watch. As Emilienne did not care to be arrested and sent off as an undesirable, she presented herself at the hospital for the insane at Sainte-Anne. Fernand shortly joined her there.
Left-sided hemiplegia and aphasia: Contrecoup and local lesions.
A soldier of 23 was wounded in the left parietal region and showed a left-sided hemiplegia with aphasia. The speech difficulty, although very marked, retrograded almost completely, but the hemiplegia remained severe. This hemiplegia was a spastic one, of a classical nature, with Babinski sign and exaggeration of tendon reflexes. Lhermitte thinks that the left hemisphere was directly affected by the contusion, as in point of fact there was an actual loss of bony tissue, but that it would not be necessary to suppose the ipsilateral hemiplegia was due to an absence of pyramidal decussation. The transient aphasia was probably due to direct affection of the tissues on the left side of the brain; the permanent hemiplegia was doubtless due to a lesion of the opposite hemisphere produced by contrecoup. It appears that sometimes a surgeon may be led to superfluous surgical intervention in a case of such paradoxical hemiplegia, since the surgeon may believe that a bullet or shell fragment has traversed the brain substance to the opposite side of the skull, when as a matter of fact the brain parts have been injured merely by contrecoup.
Re such amnesia, it is of note that many head cases, even if they do not show amnesia, show a conspicuous euphoria and lack of understanding of the seriousness of the injury in question and of the necessary treatment. According to E. Meyer, there are constantly to be found in head cases disturbances of perception and lack of coördination (especially for time), perseveration, difficulty in thinking and calculating.
| I. | Senses: Asymmetrical hyp- or anesthesia (with hyperalgesia and osseous hyperesthesia). |
| II. | Motility: Disorder, muscular or reflex. General or unilateral hyperexcitability. |
| III. | Vasomotor Control: Dermatographia. Cardiac, splanchnic disorder; also, Headaches, Vertigo. |
| IV. | Emotions: Disorder. |
| V. | Intake of Ideas: Disorder. Persistent lacunae of memory. |
| VI. | Intelligence: Disorder of recollective memory. Speech-disorder. Intellectual inertia. Overimagination (hallucinations, tremors). |
Mairet, Piéron, Bouzansky.
Gunshot wound of head; alcoholism: Amnesia.
A German soldier had a bullet pass through his right eye and lower jaw, leaving a fistulous opening from the mouth. He said that he was completely blind, but ophthalmological examination cast doubt upon the blindness. There had been immediately after the injury a number of severe attacks of dizziness, which lasted several hours; and another attack developed after he had come back from hospital, to which he had gone by reason of his pains.
He was to be arrested on account of a disciplinary crime and had ostensibly gone to his mother’s house, there to await arrest. The non-commissioned officer found him in a saloon. As soon as the phrase, “You are my prisoner!” was said, the soldier lost track of his surroundings. He had drunk a few glasses of beer but did not himself think he was drunk at the time. He was insulting and violent when asked to proceed with the officer, and a policeman was called in to take charge. He then lay down in the street and had to be put upon a wagon, still firing abusive phrases at his captors.
Upon examination, aside from the effects of the gunshot, excessive knee-jerks and tremors of the body were found. The eyebrows met but there was no other sign of bodily stigmata. There seems to have been no hereditary disease, or any history of severe alcoholism, though the man had been convicted previously of violence and theft. The amnesia is to be ascribed to effects of the head injury.
Bullet in brain: Crises; cortical blindness; vertigo; hallucinations.
An invalided soldier, 40, was sent to be observed, Oct. 23, 1916, because he wanted his pension renewed. He had been retired a year before for diminution of binocular vision with impaired perspective of objects in the right half of the visual field. He had now become completely blind.
He had been wounded, March 12, 1915, in the Argonne, without losing consciousness. He was wounded at ten o’clock at night and waited until the next day to walk to the ambulance and was at this time able to see perfectly. Arriving at the ambulance he lost consciousness. He was trephined but remembers nothing about the trephining.
His memory grew better from his arrival at a hospital in the rear in April. An attempt was made to remove the bullet in May, 1915. Though the surgeon’s finger was pushed as far as the tentorium the patient did not lose consciousness or sight, but on leaving the operating room he fainted and, after a few days of restlessness and delirium, he became completely blind. There was a cerebral hernia difficult to reduce. Vision became a little better and light and persons could be distinguished at the time when he was retired. A month after the operation there was a convulsive crisis beginning in the left arm, affecting the legs and ending in unconsciousness. Several similar crises occurred in August, sometimes with and sometimes without loss of consciousness. Later these crises began to be limited to the left side and then to be ushered in by visual hallucinations. At home he was unable to care for, clothe or feed himself. The crises became more frequent. The visual hallucinations began to dominate.
This situation lasted to February, 1916, when the blindness which had been increasing since the onset of the hallucinations became complete. The crises now became less frequent and intense. Headaches not severe were exaggerated after seizures. The patient acted like a totally blind[137] person and said that he had before him a uniform and constant gray without any light or dark spots or any color. Upon this background bizarre pictures, caricatures, disguised persons, animals or nameless things appeared colorless without relief, in silhouette, but highly suggestive of reality to such a degree that at first, according to the patient, he had made gestures to reach, or push aside these pictures. The crises were Jacksonian.
Pallor, perspiration, shivering, irresponsiveness, clonic spasms of left arm followed. The patient always had a premonition permitting him to get into bed if he was sitting, for example, in his chair. Sometimes there was a dizzy sensation as if the body were being rotated to the left. This sensation did not occur at the beginning of the seizure and the patient fought against it, turning to the right. Sometimes he felt as if he were sliding at great speed down an inclined plane. Headaches and sleepiness followed, but there was never any complete loss of consciousness of memory.
The eye grounds proved normal and all the photomotor reflexes were normal, though there was no pupil reflex to pain. The patient could write readily to dictation printed letters. It would seem that these printed letters mean that he had visual memories, as he traced the characters as if from a design. Speech was monotonous with some stuttering; but his speech had always been of this sort according to information. He walked with difficulty, not merely on account of his visual but on account of his equilibration disorders. Outside of his seizures he always turned to the right and if left to himself standing he turned to the right. If asked to walk straight ahead, he always turned to the right. Silent and uncommunicative, he was amiable and sometimes even gay. He often had troublous dreams, sometimes seeing his relatives. He said he could bring up in his mind the faces of his relatives and even the appearance of the Salpêtrière. Reflexes and sensations were normal. There was a traumatic rupture of the tympanum. Lumbar puncture showed a slight excess of albumin and 1.8 lymphocytes to the cubic millimeter. The Mauser bullet was found by X-ray in the left calcarine region with its base touching the median line, and[138] applied to the inner table of the skull about a centimeter above the internal occipital protuberance pointing forward, outward, and upward. He was treated on a salt free diet with bromides. The seizures grew fewer and at the time of report two months had elapsed with nothing but a slight vertigo and frequent nightmares. Intellectually also the patient had improved.
The case is one of cortical blindness. The seizures are explained by the vicinity of the right Rolandic region to the lesion. The rotatory vertigo is to be explained by the contact of the Mauser bullet with the tentorium and vermis of the cerebellum, which may also explain the difficulties in orientation that occurred between the crises. The visual hallucinations are doubtless due to lesion of the calcarine region.
Tunisian theopath with mystical hallucinations; gun-shot wound of occiput (bullet extracted): After the trauma, Lilliputian hallucinations and micro-megalopsia.
A. ben S. was sent to Villejuif with the diagnosis: “depression, feeling of impotence, discouragement,” having been found on the public street. He was indifferent, almost completely mute, and was at first considered not to understand French. In a fortnight, however, he was talking freely and was then found to be afflicted with hallucinations, melancholia, and delusions, apparently following trauma to the skull.
A. ben S. might have been about thirty years old, and was of a rich family, indigenous in Tunis, well educated in the Koran and Arabic literature.
Upon examination, this Tunisian gunner showed contraction of visual fields, poor color vision, and general hypalgesia. During examination, the man seized the needle and plunged it deeply under his skin, exclaiming that a prophet felt nothing and that he could be cut into bits without feeling pain.
It seems that he had had divine visions from early childhood. In his youth he had once gone to a mountain near his home and talked with Mohammed and Allah. Of course, Allah did not appear in human form, but he appeared like a ball or a wheel of fire, slowly turning. Mohammed was a tall man, with a long white beard, his eyes darting rays of fire, and his forehead bearing a gleaming bright body. Allah was heard talking to Mohammed. Orders were given concerning the sun and stars. Subterranean treasures were displayed, as well as Paradise full of yellow, blue, and green houris, transparent, such that, when food was taken, it could be seen going down their throats. Hell too was visible, and the devil very tall and black, an eye behind and another on top. There were also many genii—little men who climbed over the Tunisian’s body. Sometimes in dreams, Allah carried him to all countries of the earth. It was hard to tell[140] whether these effects were hallucinations or vivid imaginings. The Tunisian had been wounded after several months of service by two bullets in one day: the one causing an insignificant lip-wound; the other entering the skull behind. After several months the bullet had been extracted by trephining.
His further history was obscured by the fact that he wove delusional elements into his story. He said, for example, that he had been court-martialed, though there was no evidence that this was a fact. It is probable that after his wound the patient in a delirium felt that he was going to be shot. The visual hallucinations were very interesting, being Lilliputian. He would see three or four hundred Tunisian gunners walking along, knee-high or taller. Sometimes they all would stop and aim at him. He also showed micromegalopsia, real objects changing their height under his eyes. Both the Lilliputian hallucinations and the micromegalopsia dated from the trauma to the skull. There was no change whatever in the mystical delusions concerning Allah and Mohammed. These he had before the trauma.
Meningococcus meningitis with apparent recovery: Dementing psychosis.
A soldier in the Heavy Artillery, 42, developed occipital headaches and Kernig’s sign, December 27, 1915.
December 31, at the Hôtel-Dieu, he showed myosis, slight photophobia, meningitic tâche, temperature 39.6, pulse 84, heart sounds dull. Lumbar puncture: hemorrhagic fluid.
January 1, the headache was intense, neck stiffness increased, Kernig’s sign less marked; morning and afternoon temperature 39.2. Lumbar puncture yielded hypertensive cloudy fluid and 30 cubic centimeters of serum were administered.
This dose was repeated January 2 and January 3, on which date there was no headache.
January 4, Kernig’s sign and neck stiffness were diminished; fine râles at the bases without dulness. 30 cubic centimeters of electragol were injected intravenously.
January 5, Kernig and neck stiffness slight. Meningitic tâche; exaggerated knee-jerks; unequal pupils; temp. 36.6 morning, 39.4 afternoon; respiration 36; pulse 120; no râles; splenic enlargement.
6, no headache or photophobia; constipation; fine râles, right base; spartein; meningococci found in hypertensive spinal fluid. 30 cc. serum.
7, more râles; exaggerated heart sounds; intestinal worms in stools.
8, temperature fell to 37; pulse to 90.
9, patient worse; involuntary stools; Kernig’s sign; stiff neck; fever. 30 cc. serum injected.
10, 20 cc. injected.
11, delirious all night; tetaniform stiffness of neck; more râles.
12, delirious, incoherent words, Cheyne-Stokes breathing.
13, less stiffness, Kernig almost absent; pupils normal; Romberg sign slightly developed; pulse 120.
14, a few râles at right base.
15, pains in elbows, knees and hands with joint swelling; moist râles; temp. 38.4; pulse 140. Digitalon.
16 and 17, serum erythema of thorax; edema of left knee; pulse 150; spartein 16.
17, ice pack over heart.
18, edema of knee diminished; no headache, delirium or pupillary sign.
19, improvement. Temperature normal thereafter.
20 and 21, fine râles. Then all symptoms disappeared.
Recovery was predicted, but on January 28 it was observed that the patient was untidy, made mistakes in dressing, such as trying to put his legs into the armholes of his shirt, and denied the most evident facts: His képi on his head, he said it was not. Face drawn; skin yellow. Appearance of asthenia. Deep depression and hebetude. At this time the knee-jerks were exaggerated, pupils unequal, vermicular tremor of tongue; the patient walked on a broad base with tremulous legs suggesting contracture and weakness.
February 8, in a similar state the patient wandered about his room, moving his bed and chairs about, answering questions with an absent air. He had now been taught to be less untidy.
March 5, stiff neck and Kernig’s sign were distinct. He made believe he was on his farm. Ecchymosis of right upper eyelid: he had fallen (his sheep had pushed him over!). The improbability of this idea did not persuade him to think it had not happened. He walked after the manner of a tabetic.
In April he became bedridden, unable to walk, with marked stiffness and Kernig’s sign. He had at this time periods of excitement in which he would tear the bedclothes. He was invalided as demented.
Meningococcus meningitis.
During his eleven months captivity at Grafenwöhr, Eschbach and Lacaze had the opportunity of observing the case of a soldier, 24, who sustained a shell-wound in the left lung and was made prisoner August 20, 1914, at Chateau Salins. He got well of his wound, but February 16, 1915, began to cry out and was restless in the night. He was found on the straw muttering words among which only the word, “Head, head,” could be distinguished. He was irresponsive, possibly deaf. Suddenly he had a convulsive crisis and whenever touched he would have jactitations and cry out. Otherwise, he was calm and stuporous. The pupils were widely dilated. In short, he showed a mental confusion associated with paroxysmal excitement due to cerebral and cutaneous hyperesthesia. The first symptoms had occurred the morning before, when he leaned his head against a wall and complained.
Lumbar puncture yielded intra- and extracellular meningococci. The patient was isolated. In the afternoon he became less agitated, kept his eyes closed, mumbled, repeated gestures, would spit in his hands, rub his hands together, rub his neck, shoulders and body, or else he would pass his hands over his forehead and through his hair. Occasionally he would seize the straw and draw it to him with all his strength. Once when asked, “What is your name?” he said, “Not true. Not true.” Hallucinations appeared to have been added to the situation. The neck was a little stiff to forced flexion. Temperature 37.8. Lumbar puncture under chloroform anesthesia; antimeningococcus serum was injected. Next day quieter; able to get up and walk. Slept, mumbled less, was able to answer simple questions, desired to urinate and finally succeeded.
February 19, no mental disorder. Headache and lassitude. Neck stiff, Kernig’s sign marked. Lumbar puncture yielded a fluid now puriform; antimeningococcus serum injected. February 20, lifting the head produced opisthotonos. Labial herpes. The fluid yielded, besides meningococci,[144] also endothelial cells. Serum injected. February 21, fibrin in fluid; serum injected. February 22, no head symptoms. Herpes more intense, involving also arms. Tongue coated. Temperature 37.5, evening 38.3. February 23, meningococci and lymphocytes in fluid. February 24, left knee swollen. Serum injected; puncture fluid showed meningococci and polynucleosis. Fluid from knee showed polynuclear cells without organisms. February 25, patient reached evening temperature of 39.5; serum injected. A few meningococci, altered polynuclear leucocytes. February 26, patient rigid, tongue coated, serum injection. Rare meningococci, degenerated polynuclear leucocytes. February 27, rigidity decreased, evening temperature 37.7. February 28, Kernig’s sign absent. Herpes dry. Serum injection. Fluid clear; lymphocytes and polynuclear cells; no meningococci. March 6, painful inguinal gland on the left side. March 7, epididymitis left (mumps two years before, with headache two weeks and double orchitis). March 9, serum eruption. March 17, epididymitis practically absent. Lymph node painful. Later data impossible to get, except that there was apparently an arthritis of the hip and a sacral decubitus with eventual recovery.
Shell-explosion: Meningitic syndrome, fourteen months.
A soldier sustained shell-shock at the distance of a meter at Saint-Hilaire, September 26, 1915. He lost consciousness and blood flowed from his ears. He arrived, September 28, at the neurological center in Bordeaux in a semistupor, knowing that he had been shocked and had lost consciousness. He groaned, cried out, and kept stroking his head with his right hand; lay on the right side; showed Kernig’s sign right, ptosis, and stiff neck. Headache was increased on moving and noises. Patient constantly asked for food, but refused to drink. Lumbar puncture yielded a yellowish fluid, due to laked blood. October 3, headache, ptosis, left internal strabismus, temperature 38.5. October 4, lumbar puncture, slightly blood-tinted fluid. October 5, improvement; gap in memory for period since shock. No strabismus, ptosis diminished, temperature normal, improvement continued. Kernig’s sign and headache persisted. He lay doubled up on the right side, eyes closed, right hand on pillow. Defense movements on touching the neck or occipital region. The condition of semistupor often passed off in the afternoon, when he could talk, write or play cards. He had always smoked, even at the beginning of his disease. Lumbar puncture yielded a normal fluid December 12, 1915. He was sent February 23, 1916, to a hospital in the country, but came back May 9.
It seems that several days after transfer he had had an attack of delirium in the night, having lost consciousness, and tried continually to get up out of bed, saying that he wanted to go to Verdun to fight. This spell lasted several hours and on the days following came mutism, refusal of food, and a state of stupor. Nutritive enemata were given. As he grew better he sometimes ate a great deal, sometimes nothing, even wanted poison from his family, and wrote to a comrade that he wanted to commit suicide.
May 9, he was clearer, told of seeing the shell, which he said he had not heard, nor did he know how he had gotten to a hospital. His head and spine had hurt him ever since the shock. He had had difficulty in urination for two days after the shock. He could not remember the delirious attack in the country hospital. He gave various data about his life, but not fully. He refused to lie on the left side, or to walk, because of pain. He could lift either leg from the bed, but hardly both. There was an irregular coarse tremor of the extremities. The right hand was weaker than the left; there were no reflex disorders; no change in the eye grounds. There was a patchy analgesia. May 26, stupor reappeared as before, with semimutism. June, the patient presented the appearance of a dementia praecox in stupor, with stereotyped gestures and attitudes, without catatonia. The patient was sent to a hospital for the insane at Cadillac. November 9, 1916, he returned to the neurological center, as mental and cerebral disorder had disappeared. There still persisted a difficulty in remembering facts since the shock and there was still a functional paresis of the legs.
We here deal with a case of a meningitic syndrome following shell-shock and lasting fourteen months.
Brain abscess in a syphilitic: Matutinal loss of knee-jerks.
An unmarried subaltern officer, 30, entered an army neuropsychiatric center, April 8, 1915, looking exhausted and bearing a ticket “nervous asthenia, evacuated for neurological examination.” He said he had had scarlet fever at ten; strongly denied syphilis, of which he presented no trace; had not been excessively alcoholic and had had no nervous seizures. Detailed information showed that he had been a normal child. He left his two years’ military service with promotion and was a man of above the ordinary intelligence.
He was wounded in the right buttock with a shrapnel bullet about the end of September, 1914. He went back to his regiment two months later and had shared in a number of actions up to the time of his evacuation. He said he had been very tired for several weeks, and had finally been sent to the physician. There were pains in the kidney region and in the head, especially on the right side. The head felt empty. He could not sleep, but did not dream. Ideas were not distinct. Memory had become impaired. He could not keep his accounts right, and was afraid something might go wrong.
There was no pain or nervous or reflex disorder of any sort except for the knee-jerks and Achilles jerks (see below). A special examination proved complete normality of eyes. There was a slight hesitation in words, but no dysarthria. There was a slight tremor of the tongue and fingers.
As to the tendon reflexes, April 9, on waking, the knee-jerks were absent, but later in the day gradually came in evidence again. The Achilles jerks were also absent at first, but could be obtained after a prolonged examination and after percussion of the calf. In the afternoon, after exercise, the knee-jerks and Achilles jerks were easily demonstrable. The left Achilles jerk was always a little weaker than the right. Massage brought these jerks out to virtual normality. April[148] 10 and thereafter, similar findings; percussion of the muscular masses of the thighs and calves always brought out the reflexes.
Lumbar puncture yielded a clear fluid with hyperalbuminosis, 20 cells per c.mm. (lymphocytes and mononuclear cells 95 per cent) and a positive W. R. Iodide of mercury treatment was given April 18.
April 23, the patient went into a coma, with trismus, stiff neck, Kernig’s sign, sluggish pupils, incontinence. He was transferred to a special hospital, showed on lumbar puncture, April 23, 85 per cent polynuclear leucocytes, and died April 27. The autopsy showed a yellowish, quasidiffluent softening of the size of a small egg in the first occipital gyrus on the right side. The authors comment on the fact that the only objective sign in this case was the variable tendon reflexes of the lower extremities,[149] “l’unique cri de souffrance des centres nerveux.”
Early recovery from a spinal cord lesion.
Mendelssohn reports a soldier, who was sent to a Russian hospital, April 12, 1915, with a diagnosis of chronic appendicitis. Operated on next day, the patient appeared to be passing through a normal convalescence, when ten days later, he had an intense headache and some trouble in vision, which disappeared the next day, only to be followed, two days later, by the patient’s complaint that he could no longer urinate or rise from bed.
In fact, Mendelssohn found a complete flaccid paraplegia with urinary retention, without fever or pain. Knee-jerks and Achilles jerks were absent, and there was a slight extension of the great toe on plantar stimulation. There was disorder of sensation, with heat sensibility abolished, painful points poorly localized, and position sense poor. Electric reactions normal. Pain on pressure in and about the lumbar vertebral region. Cerebrospinal fluid showed lymphocytosis and an excessive albuminosis.
This paraplegia lasted six weeks. At the end of May, the patient began to be able to move his toes and to lift his heel. Improvement was gradual and progressive. Early in June he could walk if supported. The weak knee-jerk then began to reappear and the urinary retention gradually disappeared.
This patient was not hysterical, although a bit emotional. Perhaps, according to Mendelssohn, an organic lesion was grafted on a neurosis. Perhaps the spinal lesion was infectious. At any rate, a presumably organic paraplegia had recovered in two months and a half.
Shell-explosion: Meningeal hemorrhage: Pneumococcus meningitis.
An infantryman, 20, came to the Sixth Army Neurological Center, October 13, 1916, as a case of “choluria, due to shell explosion; epistaxis needs watching.” He was somnolent, had waked vomiting, pulse 108. Kernig’s sign, defensive movements of the legs on stimulation, with flexion of leg on thigh and of thigh on pelvis, plantar reflexes flexor. Puncture showed typical meningeal hemorrhage. Two days later, temperature 40, pulse 70, that is to say, a bradycardia in proportion to the fever. Vomiting, pulse persisted. Next day the patient was moaning and semi-delirious and showed stiff neck, Kernig’s sign, accentuation of vasomotor disorder, plantar response flexor with leg retracted, thigh flexion both homolateral and contralateral. The spinal fluid upon the next day, that is, four days after his arrival at the clinic, showed a purulent fluid in which there was an excess of albumin, no sugar, diplococci extracellular (proving on culture to be pneumococci and able to kill a mouse in twenty-four hours).
As a rule such hemorrhages remain aseptic, and in fact meningeal hemorrhage is said by Guillain and Barré to have, as a rule, a favorable prognosis. The above described case was the only one of infected meningeal hemorrhage that had occurred in the Sixth Army Neurological Center.
ANTEBELLUM cortex lesion: right hemiplegia; recovery. Struck by shrapnel on right shoulder: Athetosis.
A British soldier, aged 27, showed a somewhat remarkable phenomenon. It appears that at five years of age, this man had had poliomyelitis, affecting the left leg. At 20 years of age, he had had pneumonia, and this had been followed by a paralysis of the right arm and leg with a loss of speech. The man recovered from this illness, although he never quite regained full control of the right hand. It is evident that this lack of control was not marked, else the man would not have been enlisted, and it is Dr. Batten’s opinion that at all events he could not have shown pathological movements of the right hand at the time of enlistment.
However this may be, in October, 1914, the soldier was struck on the right shoulder with shrapnel. Apparently he was not wounded, but thereafter he was not able to use the right arm well, and in two months’ time he had become unable to manipulate his rifle. On January 13, 1915, he was sent home. The remnants of the old poliomyelitis of the left leg were shown in a general weakness of that leg as compared with the right. The movements of the right hand were those seen in athetosis. The movements were independent of volition. The patient had difficulty in releasing his grasp. He improved rapidly during the six weeks he was in hospital, although the movements of the right hand never became entirely normal.
In this case, according to Batten,[152] “the stress was sufficient to bring into prominence the symptoms due to an old cerebral lesion.”
Hysterical versus thalamic hemianesthesia.
A soldier, 40, had been suffering for a number of months with pains in the left side of the trunk and feelings of weakness in the left arm and leg. In the summer of 1915 he was on leave and while walking, fell, lay down, and found he could hardly move his left arm and leg. Two or three weeks later he got up, walking with a stick. After some time in hospital, he was sent back to the trenches, a little weak.
He had shortly, however, to be examined neurologically again. He could hardly raise the left leg and his passive resistance was poor on this side. The left side was almost completely anesthetic to all forms of stimulus, although an intense faradic current yielded a feeling like that of a fly. Nor was the tactile sensation absolutely nil, as it could be got with a flat finger on the upper arm and thigh. Cold and heat sensations not well localized. The hemianesthesia was sharply limited at the median line and affected the buccal, lingual and nasal mucosa. Deep sensibility was almost abolished on the left side. Stereognostic sense was lost and the sense of position was lost absolutely for hand and foot.
The patient said that he heard less well on the left side. There was also a slight contraction of the left visual field. The reflexes were lively, but equal on both sides. A diagnosis of hysterical hemianesthesia was apparently called for, but psychoelectric treatment failed. The plantar reflex was, in fact, completely absent on the left side, as well as the corneal reflex. The faradic current failed to produce as marked a dilatation of the pupil on the left side as on the right. The forehead wrinkles were less marked on the left side. The mouth deviated slightly to the right. The left nasolabial fold was a little less marked. The tongue did not deviate, but was a little narrow on the left side. The palate deviated a little to the left. The left side of the trunk seemed a little less developed than the right, and the scapula stuck a little less closely to the body on the left side, when the arms were raised. The left buttock was a little narrower than the right[153] and the left gluteal fold was less marked. In combined flexion of thigh and trunk the left foot readily left the floor. There was a left-sided hypotonia in forced flexion of the forearm. There were no tremors of the limbs in repose, except a few contractions of the left lower extremity. In movement, however, there was a marked tremor and in coördination the finger to nose test could not be performed. Speech was slow and hesitant, sometimes stuttering. Food was sometimes taken into the air passages. Headaches were localized on the right side. They had begun when the first symptoms began. There was mental disorder, with gaps in memory. In short, the case is probably one of thalamic disease, though there were no pains except a few in the left side of the trunk at the beginning of the disease. The diagnosis of hysteria was at first made in this case, but the rule that hysterical hemianesthesia is never found without auto- or hetero-suggestion caused the alteration of diagnosis to thalamic.
Shell-explosion: Syndrome suggesting multiple sclerosis.
A soldier, 40, carriage painter, underwent shell-shock at Voquois, May 2, 1915, following ten hours’ bombardment. At the time he felt tinglings. The bombardment had just ceased when he fainted suddenly while repairing a telegraph line. There was no loss of consciousness. He could not move his arms or legs, was able to spit, and did not suffer at all except for the tingling. He was evacuated to the interior, where the diagnosis of psychopathic double paraplegia, Kernig’s sign, zones of anesthesia in the legs, was made. He was immediately treated with gray oil, and got an injection of neosalvarsan, and iodides. He grew slowly better. He could lift a leg from the bed, but then both legs began to tremble. The arms had recovered their movement, before the legs, but always trembled in movement.
November, 1915, he was able to get up; two months later, he walked alone.
At the neurological center, which he entered December 17, his gaze was fixed and there was a slight exophthalmos. The folds of the face were smoothed out. The nose was deep set (as a result of a fall at the age of eight). In the upright position he could not remain still, but trembled markedly on the left side, so that he had to make a few steps to keep his balance. He was unable to stand on his left leg. He walked on a broad base, in little steps, and rather unsteadily on account of tremors augmenting upon movement. General muscular weakness; left hand slightly weaker than right. He could not lift both legs more than 20 cm. from the bed and in the process they both trembled, trembling together. There was also intention-tremor of the arms, a little less marked than that of the legs, of an irregular rhythm. The arms trembled as a whole. In a state of rest there was no tremor. There was a slight muscular stiffness and the patient himself felt difficulty in relaxing. Patellar reflexes absent,[155] even on reinforcement; Achilles jerks absent. Speech monotonous and tremulous, but not scanning; syllable doubling observed by the patient. Manuscript tremulous and, on account of tremors, illegible. Hypalgesia of legs, more marked distally. Deep sensibility of tendo Achillis and patellar reflexes lost. Pain on compression of eyes diminished. Formication in arms. W. R. of blood negative. Slow improvement followed and the patient left the neurological service May 4, 1916, able to walk more easily and without tremor. The knee-jerks and Achilles jerks were still absent.
We here deal with a syndrome in part that of a multiple sclerosis, that is, the intention-tremor, gait disturbance, muscular rigidity, and weakness.
Re multiple sclerosis, Lépine remarks that there are numerous army cases of pseudo multiple sclerosis which are actually hysterical or hystero-traumatic cases of hypertonus and tremor. The true cases of multiple sclerosis, according to Lépine, are of interest inasmuch as they are usually found in officers. These men have apparently at first but a slight motor disorder, quite compatible with desk work. We have usually under-rated the cortical element in multiple sclerosis. Spells of confusion, delusional ideas, sometimes grandiose, start up without warning in these cases. To be sure, alcohol and syphilis sometimes also enter these cases etiologically. Any case of localized tremor ought to be carefully examined psychically, and such cases in general ought not to be given responsibility.
A soldier was blown up by a mine and rendered unconscious. Upon recovery of consciousness, he was dumb, unable to work, very nervous, paralyzed as to left arm and leg. The paralysis improved so that in the hospital at home the patient became able to get about. However, he threw his legs about in an unusual fashion. Several months later, the patient was much improved.
Shortly, however, there was a relapse. Transferred to a hospital for chronic cases, the patient was unable to walk without assistance on account of complete paralysis of the leg. Insomnia, general tremor, and a bad stuttering developed, with a habit of starting in terror at the slightest noise.
Hypnotic treatment was followed by almost complete disappearance of the tremor. The patient began to sleep six or seven hours a night; nervousness diminished, and the stuttering slowly improved; but neither the paralysis nor the anesthesia of the left leg was affected by suggestion. The leg remained cold, livid, anesthetic, and flaccidly paralyzed to the hip. Though a slight improvement has since been produced by faradization, the patient still can walk only with assistance.
A man was injured in 1906 by the fall of a heavy weight on his back. In 1914 he went to France as a soldier, and eight months later was hurled into a shell hole so that his back struck the edge. He was rendered unconscious. Upon recovery of consciousness, the right leg was found to be swollen, and there were severe pains in the legs and back.
Since return home the patient had gone from one hospital to another, for the most part unable to walk, suffering from agonizing pain in the head and eyes, unable to sleep, and in the night subject to horrible waking dreams.
| I. | Hyperextension of forearm (hypotonia). |
| II. | Platysma sign: Contraction absent on paralyzed side. |
| III. | Babinski’s flexion of thigh on pelvis (spontaneous, upon suddenly throwing seated subject into dorsal decubitus). |
| IV. | Hoover’s sign: Complementary opposition (on request to raise paralyzed arm, presses opposite arm strongly against mattress). |
| V. | Heilbronner’s sign of the broad thigh (hypotonia). |
| VI. | Rossolimo’s sign: flexion of toes on slight percussion of sole. |
| VII. | Mendel-Bechterew sign: flexion of small toes on percussion with hammer of dorsal surface of cuboid bone. |
| VIII. | Oppenheim’s sign (extension of great toe on deep friction of calf muscles); or Schaefer, or Gordon (on pinching tendo Achillis). |
| IX. | Marie-Foix sign: withdrawal of lower leg on transverse pressure of tarsus or forced flexion of toes, even when leg is incapable of voluntary movement. |
At first able only to bring himself to an upright position and to rush a few steps, he later acquired considerable control of his feet and legs through crutches. The insomnia persisted.
Smyly regards this case, like Case 116, as more neurological than mental.
Re organic neurology, much of great value has been reported.
Sargent and Holmes say that, contrary to expectation, there have been few war cases of bad sequelae of cerebral injuries, such as insanity and epilepsy. During early stages, after infection of the head wounds, there is dulness and amnesia, irritability and childishness,—symptoms which disappear during and after repair of the wounds. Mental disorder requiring internment is surprisingly rare. During 12 months only eight cases were transferred from the head hospital in a year to the Napsbury war hospital, where cases of insanity attributable to the service are sent; and in but two of these could the persisting mental symptoms be attributed to head injury.
Col. F. W. Mott confirms the opinion of Col. Sargent and Col. Holmes, remarking that from all the London County Council Asylums, only one case of insanity associated with gunshot head wound had been admitted, and that this was one of a Belgian who died from septic infection of the cerebral ventricles. Yet all cases of insanity in invalided soldiers belonging to the London County Council area (about one-seventh of the population of the United Kingdom) are transferred to these asylums.
Again Sargent and Holmes point out that both generalized and Jacksonian epileptiform seizures are comparatively rare in patients suffering from recent head wounds; even convulsions in later stages have been as yet less common than was feared. Thus, after evacuation to England, fits occurred in 37 (6 per cent) of 610 cases with complete notes, and in only eleven of these 37 cases were the convulsions frequent. Sargent and Holmes remark, however, that the practice of giving bromides regularly to all serious cranial injuries until the wound is healed, and for some months afterwards, seems[159] advisable. In 33 of the 37 convulsive cases there have been severe compound fractures of the skull, and in four of these a missile was still present in the brain. Five secondary operations were performed with good results, after drainage of small abscesses in two and removal of spicules of bone in three. The In-patient and Out-patient records of the National Hospital for the Paralyzed and Epileptic were searched for epileptics already discharged from the army, but notes of but two patients attending this hospital for epilepsy were found.
As for other neurological complications aside from septic infection and hernia formation, there are a few subjective symptoms that may necessitate the invaliding of soldiers. The most common of these is headache, usually in the form of a feeling of weight, pressure, or throbbing in the head, which headache is increased by noise, fatigue, exertion, or emotion. Attacks of dizziness also occur, and nervousness or deficient control over emotions and feelings. Changes of temperament are found in some soldiers, who become depressed, moody, irritable, or emotional, and unable to concentrate attention.
Foix, under the direction of P. Marie, worked upon aphasia in 100 cases, reporting results at a surgical and neurological meeting, May 24, 1916, in Paris. Only lesions on the left side of the brain have produced important and lasting speech disorder, although lesions on the left side may leave behind them a little dysarthria or difficulty in finding words in conversation. It is, of course, hard to tell speech disorder from stupor or clouding of consciousness. Foix notes certain specialties in speech defect according to which region of the left brain is affected.
First: Prefrontal lesions produce a transient dysarthria, lasting but a few weeks, and right-sided prefrontal lesions produce just as much disorder.
Occipital lesions produce no speech disorder.
Second: Patients with right-sided hemianopsia due to lesions of occipital regions were not aphasic and could read or write perfectly. Lesions of the left visual centers certainly do not affect reading. If, however, the injury is not to the[160] visual centers, but is upon the lateral part of the occipital lobe, then alexic phenomena appear, and these the more the lesion approaches the temporal-parietal region.
Third: Central convolutional lesion produces a variety of disorders according to the site and extent of the lesion. There is no aphasia with the crural monoplegia due to superior paracentral disorder. But slight aphasic disorder accompanies the brachial monoplegia of middle central lesion, though writing, reading, and calculation are slightly affected, and the more so the more the lesion extends posteriorly to the stereognostic regions. The lower down in the precentral region the lesion appears, the more likely is the Broca syndrome to be observed. But if the hemiplegia is chiefly a brachial monoplegia, the aphasic disorder may remain slight, involving reading, writing, understanding of words, the spoken word, articulation, and calculation.
Fourth: Lesions of the lateral-frontal region produce more or less marked aphasic disorder, just as do those of the inferior part of the precentral gyrus. This aphasia is more apt to occur when the wound is deep. However, no case of permanent aphasia has been observed in cases of lesion of the lateral-frontal region (termed in Foix’s nomenclature, the precentral region, but referring to the tissues in front of the precentral (or ascending frontal) gyrus of the more familiar nomenclature). Almost absolute, or absolute, anarthria follows the wound, and the patient is hemiplegic. This hemiplegia may last from ten days to two or three months. After a time there is no longer more than a slight dysarthria, and writing becomes good again; reading remains, perhaps, a little difficult. A complete or almost complete cure is the rule.
Fifth: When the retrocentral region is injured, various aphasic syndromes appear. The retrocentral region is the parietal-temporal lobe except the superior part of the parietal lobe and the anterior part of the temporal lobe, which latter two regions when injured do not allow any marked aphasic disorder. Lesions of the middle or posterior temporal region are particularly important for speech, and produce more marked disorder than lesions of the angular gyrus or the[161] supramarginal gyrus. At first, words cannot be spoken, for a period of a fortnight to three months. Speech returns progressively, with an increased power of comprehension. At the same time, the patients begin to read and write. But there is no further spontaneous progress after a period of six or eight months, and then special reëducation must be started. These speech disorders of retrocentral (parietal-temporal) origin are either aphasic syndromes or slight remains of psychical disorders, or again, a disorder practically limited to alexia. The true aphasic syndromes concern the spoken word, understanding the words, writing, and calculation. The disorder is not especially dysarthric and consists particularly in loss of vocabulary. It might be called an amnestic aphasia (Pitres). These cases have well-marked intellectual disorder and their power of calculation is especially poor. As to the aphasic traces, which are more important to understand than they are extensive in point of fact, they relate particularly to calculating power, to vocabulary (slowness in finding words), and to reading (reading without comprehension). As to the cases of alexia, these are cases of lesions of the posterior part of the parietal-temporal lobe, and are usually accompanied by a hemi- or a quadrantanopsia.
To sum up, cases with central lesions (precentral and postcentral gyrus) have hemiplegia and a Broca aphasia without much tendency to cure. Cases with lesions anterior to the central convolutions have a transient anarthria and their recovery is ordinarily complete. Cases with retrocentral lesions have an aphasia suggestive of Wernicke’s aphasia, and ordinarily leave behind them extensive defects in intelligence and language. These cases should be taken account of from the standpoint of compensation, since they are much worse off for work than many cases with amputations; and though their disorder looks slight, it quite interferes with working at a trade. From the point of view of military effectiveness, the retrocentral cases are not very good soldiers, and especially not good officers, as they do not understand commands completely.
Neuropsychiatric phenomena in rabies.
A farmer, 34, mobilized in veterinary work, fell sick at a station for sick horses, April 25, 1917. He breakfasted well, drank coffee, and went to the abreuvoir at eleven o’clock. He told his mates that he felt bad in his head. He fainted over a table at the eating house, refused to eat or drink. At noon he went out into the court, vomited and went to lie down. A physician thought he was suffering from angina because of the pronounced dysphagia. He entered the hospital at eleven o’clock at night on the 25th. He was found next morning on his back, with a fixed and haggard look, crimson face, masseter and phalangeal spasm at times. Respiration irregular, interrupted by moans. The pulse would go up to 120 during agitation and then go down to 50 as soon as the patient lay down again. Pupils slightly dilated and unequal. As the patient came from a sick horse dépôt, the first question was that of tetanus, suggested somewhat by the jactitation of the limbs and the trismus. A violent headache began and the patient cried out, “My head! My head!” Painful vomiting movements, with very slight bilious material. Convulsive movements increased. The pulse was slow. The diagnosis “meningitis” was suggested, despite the absence of fever and the absence of Kernig’s sign. Lumbar puncture gave limpid fluid with a normal lymphocytosis, without increase of albumin or reducing substance. The bacteriological smear and culture were negative.
Soon another sort of symptoms appeared. The patient would rise, cry out, threaten his neighbors. He was calmed with morphine. There were periods of excitement alternating with periods of calmness, during which he would reply sharply but accurately, being somewhat vexed by the questions, and would walk up and down without offering a word. When a glass of water was offered to him, as soon as his glance met the glass his eyes expressed fear. He drew back in repulsion[163] and cried out in terror. When the liquid was out of his sight the hydrophobic spasm ceased. This hyperesthesia of the sensorium was so intense that the mere sight of the shining glassware of the laboratory brought out a sharp crisis.
He was sent that evening to the neuropsychiatry center, walking jerkily and as if slightly drunk, with a number of small gesticulations and murmurings. He was immediately isolated, undressed himself and went to bed. He did not move in his bed, and seemed to sleep. The next day he got up, dressed and had a small spell of excitement, but was quiet enough on the medical visit, though the floor was soiled with urine and vomitus and the clothing was in disorder. He now had a pronounced phase, deep sunk eyes, drawn features and anxious look; dilated pupils and an expression of mixed fear and anger. His breathing was hard and he kept his hand on his heart. He was oriented. He suddenly rose and said, “I am thirsty.” A glass of milk was given him. He hesitated a moment, plunged his mouth and hands into it and aspirated the drink without making any swallowing movements. He pushed away the glass, spat a little, and vomited a small quantity of a black liquid. Then followed an anxious crisis, and he fell upon his side, absolutely immobile, without breathing for a few seconds. Again in the sitting posture, he was taken with contractions of the limbs and face. The tendon reflexes were at this time normal.
A quarter of an hour later the attendant found him dead, in the sitting posture, leaning against the wall, mouth open, arms dependent, hands extended, pupils dilated—a death in syncope. The brain was found congested. There was a slight effusion of blood over the posterior aspect of the brain. There were no hemorrhages or softenings in the brain substance. The muscles were of a dark red to black. The adherent lungs were very slightly congested at the base. The stomach contained a quarter of a liter of black, inodorous fluid in which there was much bile and little blood. There were numerous small hemorrhages of the mucosa near the great curvature. The spleen was large, the liver congested. The Pasteur Institute confirmed the diagnosis of rabies. There is no history of the man’s having been bitten by a dog.
Tetanus: Psychosis.
A soldier wounded May 18, 1916, was given antitetanic serum May 26th. The wounds healed, but on June 16, that is, 29 days after the trauma, contractures began, at first localized. There had been numerous wounds of legs and scrotum by shell fragments and the contractures were limited to the right leg and scrotum. There was no trismus or any lumbar symptom.
During the next few days the contractures became general, the temperature rose, a shell fragment was found by X-ray at the root of the thigh and was surgically extracted. B. tetani was found upon inoculation of media with material from the shell fragment. Persulphide of soda and antitetanic serum 90 cc. in three days were given intravenously. The temperature fell and the general health was greatly improved. July 6, hallucinations and terrors, worse at night, set in. The man believed himself surrounded by flames, that daggers were being plunged into his old wounds, that his hair was being pulled. These symptoms lasted a fortnight only, whereupon the patient recovered.
This case and six others accompanied by cerebral disturbances all recovered, and all the patients retained a perfect memory of their delirium and of their hallucinations.
The chronological distribution of these cases was odd. One case was found early in the war; then no other cases of cerebral disorder presented themselves until the group observed at the end of 1916. Besides flames and daggers, zoöpsia was several times observed. One of the cases showed these symptoms without having been given antitetanic serum.
Re tetanus in the war, see in the Collection Horizon a book by Courtois-Suffit and Giroux on Les formes anormales du tétanos.
Tetanus fruste versus hysteria.
Claude and Lhermitte describe a condition of tetanos fruste. The neck was absolutely rigid. The patient had not been wounded in any way and, being regarded as a pure neuropath, was sent to the Centre Neurologique at Bourges.
The differential diagnosis lay between true tetanus and the hysterical pseudotetanus or pseudomeningitis. In pseudotetanus there is a contracture of the superficial and deep neck muscles, especially the trapezii, sternomastoid, and deep muscles. The condition somewhat suggests that of acute meningitis or tetanus, and especially suggests tetanus because it is often associated with masseter contracture (hysterical trismus). The head is immobile, stiff, and inclined backward; eyes directed above, throat slightly prominent. Upon attempts to move the head, intense pain occurs. The pain and contracture sometimes even suggest a suboccipital Pott’s disease. This form of hysterical pseudotetanus is of sudden onset, as a rule following burial in a trench or else contusion, or a slight wound in the cervical region. Pressure on the spinous processes produces no pain, nor does a blow upon the head; and an X-ray examination will definitely eliminate the hypothesis of Pott’s disease.
To return to the Claude-Lhermitte case of limited true tetanus: It showed marked modifications in the tendon and bone reflexes. Upon percussion of the zygoma, of the occiput, or of the clavicle, there was a marked further contraction in the contractured muscles. Although there was no apparent spasticity in the legs, there was an ankle clonus and a bilateral patella clonus, combined with a distinct exaggeration of all bone and tendon reflexes. In such cases also there is hyperexcitability of the nerves and muscles to faradic and galvanic currents.
An officer’s letter concerning local tetanus.
The following letter from an officer who had had local tetanus and was treated by Turrell by ionization Dec. 6 and 7, 1915, by diathermia Dec. 7 to 22, and occasionally by static breeze ionization and chlorine ion to relieve contractions from Dec. 29, 1915, to Feb. 4, 1916. The tetanus was in the muscles of the legs. Of course diathermia is a purely symptomatic treatment and does not replace antitoxin serum or other specific treatment; thus its effect in relieving the contractions of local tetanus is precisely like its effect in the treatment of sciatic neuritis or lumbago.
November 15, 1916.
“Dear Major Turrell,
[167]“I have been meaning to write to you for some time, as I knew you would be interested to hear how I was getting on. Your letter has just been received, and I am only too happy to give you any information I can with regard to my leg. I was wounded in the left leg on October 13, 1915, by high explosive shell, and arrived at Oxford on October 22. There was no operation as the surgeon in charge did not consider it advisable to remove the pieces of shell: my leg seemed to be getting better, and after about a month I was able to hobble round with sticks. My foot at this time used to swell a great deal towards night, and the foot seemed then to gradually stiffen up with violent pains at intervals, this gradually spread up the whole leg to about the knee, and I was compelled to take to my bed again. The pain at times was very bad, similar to a very bad attack of cramps, and then my leg became rigid and stiff, and at other times used to get horrible jumps and it was impossible to keep it still, and whenever the doctor or nurse looked at it it used to stiffen up at once. The night seemed to be the worst, and consequently I got very little sleep. I often had to get up in the middle of the night on crutches to try and obtain relief, my leg was so cramped and sore. It was about this time that you first visited me and prescribed a course of electric treatment for my leg, and I shall never be able to thank you enough for the relief it gave me. I cannot remember the names of the different treatments, but the first one—diathermy, or heat pads—certainly relieved the pain, and after the first two or three visits to you I got immense relief. I never looked back after this, and, although the progress was slow, I gradually lost all pain and was able to get sleep at night. The nervous jumps slowly disappeared and my leg became gradually normal except for contraction of the tendons. I was unable to straighten my ankle or knee, and it was thought at one time that my tendo Achillis would have to be severed. Gradually the knee straightened and I was able to get my heel to the ground. I was for some time on crutches, and was able to leave the hospital on February 5, 1916, walking with sticks.… I am now able to walk comfortably, but am unable to flex the ankle more than at right angle to my leg. The circulation is not very good, and I feel anything tight round my calf. I am still getting Boards, and have not been passed fit for overseas yet.”
Dysentery: Psychosis.
Out of a large number of dysentery patients, many of whom had very serious symptoms, but one of Loewy’s patients became psychotic. Loewy in fact had discharged this one as normal, and he had been put on the wagon train (no opium or alcohol) to go to a sanatorium. As the fighting shifted, the sanatorium site changed and could not be reached with the wagon. Finally, the wagon train met the battalion once more and Loewy was told that the man was “dying.” At this time he was afebrile, without collapse symptoms, with a strong and normally frequent pulse, and with few signs of exhaustion. Yet the guard had thought that he looked moribund. Both upper eyelids were drawn rigidly up but conveyed a different impression from that in maniacal or anxious conditions. The expression was that of staring astonishment, helplessness, and apathetic lack of orientation. The patient recognized Loewy, spoke to him as “Herr Doctor,” said he was doing quite well; he was found to be well oriented. There was no fabricating tendency even as to the number of stools (although Loewy had noted such in bad dysenteries of the Shiga-Kruse type). He was apparently hard of hearing, as if at the beginning of a typhoid fever. He showed a retardation in his intake of ideas, and his voice in answering sounded absent-minded. There was an expression of absent-mindedness, and the patient seemed markedly unconcerned about his health, the direction of the journey, the terrible rain, etc. These phenomena are attributed by Loewy to attention disorder.
The patient had been out of reach of fire for days. Loewy reports the case as one of beginning amentia or as an exhausted state resembling a Korsakow condition, recalling one of emotional hyperesthetic weakness (Bonhoeffer).
Typhoid fever: Hysteria.
A soldier entering hospital for typhoid fever, October 2, 1914, was discharged to another hospital and again, November 10, to a hospital for nervous disease. The typhoid was serious and complicated by delirium. After defervescence, the patient was weak and could not stand or walk, especially on account of pains and weakness in the left leg. Sometimes he had had pains in the sacrum and left hip. He complained of tinnitus, deafness, dizziness, headache. He said he had fallen from a cart, had been sick for three months, since which time he had been under medical treatment for his present condition. He had, he said, been given a small pension.
The gait disorder sometimes amounted to a real astasia-abasia. The left leg became stiff and was dragged behind. There was a paresis demonstrable in dorsal decubitus, of the left side, especially of the leg, without atrophy. There was a hypesthesia of the whole left side of the body, with the exception of the head. Hyperesthesia of the left leg, hip and upper sacrum. The left corneal reflex was diminished. Moody, hypochondriacal, lachrymose. The general attitude of the patient was affected and theatrical. Paradoxical innervations were frequently found on test. There was no neurological disorder except for the absence of the right Achilles jerk.
The absence of this Achilles jerk may be regarded as a residuum of the previous accident. The localization of the pains points to a neurotic lumbosacral plexus disorder on the left side. Superimposed upon this picture are the hysterical phenomena. The typhoid fever and its attendant neuritis are therefore to be interpreted as the liberating factor for a severe hysteria in a subject already disposed to such symptoms through previous accident.
Dementia praecox versus post-typhoidal encephalitis.
A butcher, 29 (aunt insane, sister melancholy, one child stillborn, deformed), had had several days convulsions at eight; went through military service without incident; was at the Marne and was evacuated October 19, 1914, with typhoid fever,—a severe fever with a delirium prolonged into the last weeks. Three months convalescent leave was given, passed at Paris with the man’s aunt, but he had become strange. One day he wanted to strangle neighbors of German origin; another day departed for Dunkirk and then returned, having lost all his documents.
February, 1915, he went back to the front, did strange things and was soon evacuated to Tarascon. In April he went back to his dépôt; May 18, to the hospital at Rennes for erythema. June 15, he was given 15 days in prison for setting off a cannon too quickly and then running off through the fields. August 11, he was interned at Rennes for stealing a priest’s cap. September 12, two months convalescence. December 10, headaches. Back to Rennes January 14, February 18, Val-de-Grâce, then Maison Blanche.
Here he was found sometimes sad, immobile; at other times laughing and singing. He was very irritable on small occasion. Once on leave he had a fugue with complete amnesia, though alcohol may account for the latter. His memory was vague, especially for his crimes and for recent events. He was emotional, indifferent even in the presence of his wife or aunt. Sexual indifference. He often complained of his head, saying that he felt it blocked and that he could not think. The headache was frontal and would last several hours. The man would, however, not complain spontaneously. He was physically, in general, negative.
This case might possibly be due to a post-typhoidal encephalitis, but Nordman believes rather that it is a case of dementia praecox. Perhaps the convulsions at eight produced a slight brain lesion, brought to an issue by the typhoid fever.
Paratyphoid fever: Psychosis outlasting fever.
A Breton farmer, 34, had paratyphoid alpha. Admitted to hospital September 3, 1915, he had headache, anorexia, asthenia, coated tongue and tense abdomen, algosuria; later, abdominal swelling, borborygmi in the right iliac fossa, rose spots, dicrotism, albuminuria, bronchitic rales. The disease was severe, and was complicated by sacral decubitus and ran a month.
At first somnolent, September 8th the patient went into a state of mental excitement with agitation and delirium. He got out of bed, cried out, sang, talked to his neighbors, complained that his papers (colis) had been stolen, as well as his watch and tobacco; that his horses’ hoofs had been injured, and the like.
He grew calmer in a few days, and now no longer tried to get up, remaining inert in his bed. The occupation delirium persisted—he was not being paid what he owed, and the like. He had hallucinations; looked for scissors, and one day said, “Here they are!” At intervals he appeared lucid and responded appropriately to questions.
The fever dropped and the paratyphoid disease appeared past, but the mental state remained for three weeks without change, having the same periods of lucidity when he would be regarded as cured, but falling again forthwith into his post oniric ideas. He was soon sent to a convalescent hospital and was not wholly well for another month.
Psychopathic taint brought out by paratyphoid fever.
A soldier, 31, was a victim of paratyphoid alpha, entering hospital October 21, 1915, with the usual symptomatology: fever, asthenia, headache, abdominal swelling, tongue coated and red along its edges, diarrhoea. After admission he passed into a deep toxic state.
He woke up in the night with a cry, got up afraid, and refused to go back into his own bed. He was mute, except for curses addressed to the nurses. After two hours he went to bed and to sleep. Next day he sat quietly with a depressed look, occasionally groaning deeply, talking in brief phrases about his anxiety, wanting his wife telephoned to, saying that he would not see his children, was going into the four planks, and the like.
This situation lasted about a week. He became afraid of medicines and thought he had been poisoned, saying that he would rather be shot than poisoned and complaining that, though he had served France for fourteen months, they now wanted to kill him. In the night time he was agitated. He gave vent to cries, and threats, but this delirious state rapidly decreased and he became calm the night of September 27th. The upper extremities showed a tendency to catatonia. From this time forth, during the remaining month, the patient was immobile, mute, fearful, and mistrusting, depressed and always wore a cunning look. His disorientation decreased and he passed good nights. He would answer questions by groaning. He would say, “They think I am a Tartar.” The end of the mental disorder coincided with the cure of the paratyphoid fever. According to Merklen, the paratyphoid bacillus in these cases serves to bring out a psychopathic taint. This particular patient had always been of a sad demeanor, uncommunicative, very impressionable and emotional. Two other cases had always been somewhat below normal.
Diphtheria: Post-diphtheritic symptoms.
A farmer, 37, was evacuated March 20, 1916, for diphtheria. April 1, paralysis of tongue and uvula, impairment of vision. These symptoms rapidly improved, but paralysis of the legs appeared and then of the arms. This paralysis lasted until he was sent to the neurological center June 28 for post-diphtheritic paralysis, wherein it was found that voluntary movements of the legs could be performed, though painfully and of slight extent, that walking was impossible, that there was a considerable atrophy of legs and arms, that the knee-jerks, Achilles jerks and plantar reflexes were absent. There was complaint of pains in the legs and over nerve trunks.
Improvement followed, the atrophy gradually passed away, and the voluntary movements of the legs became more extensive; but by October the reflexes had not yet reappeared. Yet the patient had begun to walk on crutches and soon was able to get on with canes only. The improvement did not continue. He did not raise his heels and dragged his toes. There was now a clonic tremor of the legs as soon as the weight of the body was put on them. During movements of legs carried on in dorsal decubitus there was found an irregular tremor of the legs with twisting of the trunk. The muscular strength was well preserved. There was a slight muscular atrophy. The tendon reflexes had now come back, though the right Achilles jerk was weak and the plantar reflexes were absent. There was a hypalgesia of the legs which ceased sharply at the middle of the thighs. There was a slight hypoacusia on the left side. Visual fields normal. The patient complained of feelings in the inside of his bones. Electrical reactions normal.
Diphtheria: Hysterical paraparesis.
A soldier, 24, was evacuated June 24, 1915, from Roussy for diphtheria and was treated by serum, receiving 80 cc. in 8 injections. A few days later there was a paralysis of the uvula with regurgitation of liquids from the nose; but patient was able to go on convalescence July 21. A few days later, however, he noticed that his legs were weak. Vertigo, vomiting and painful walking followed, and his convalescence was increased a month. The paralysis got progressively worse. September 10, he went by automobile to Libourne where he stayed two months. He arrived at the Neurological Center at Bordeaux November 9 with diagnosis “polyneuritis of legs.” He could not walk and could hardly flex thighs on pelvis or legs on thighs. Voluntary movements of extension and flexion of feet and toes were limited. There was neither atrophy, pain nor reflex disorder. Both legs were analgesic, as was also the abdomen up to the umbilicus. There was complaint of dorsolumbar pains and of stomach trouble and lack of appetite; vomiting after meals frequent, pulse 120.
January 3, the patient was able to lift his legs a few centimeters above the bed but not together. There was now a slight muscular atrophy especially on the left side. Knee-jerks lively, analgesia limited to legs, no vomiting, pulse rapid.
The patient was sent to a hospital in the country May 8 to July 8. He was now much better. His legs were able to support his body but he could not walk. Slight atrophy of left leg. There was hypalgesia now in the feet and legs below the knee. There was no pain on pressure over the nerve trunks. The electric reactions normal. The patient could now walk on crutches. He was invalided on the temporary basis, December 12, 1916.
It does not appear that in this case the hysterical paralysis was preceded by polyneuritis.
Malaria: Amnesia.
A soldier lost all memory of his hospital stay in Salonica and the voyage home. He could only remember a little about the hospital at Bandol. There is a period of transition to full memory in malarial cases characterized by sure memory, vague on certain points, alternating with phases of almost complete amnesia. The soldier in question had very inexact memories of the Bandol Hospital, and could only remember about his fevers, that they began about noon and terminated about four o’clock. Twice he had been found in his shirt, walking, unconscious, in the passageway of the hospital. Having obtained leave for convalescence, three months after his memory gap began, he went to Paris, and probably had attacks at home. He vaguely remembered afterward being carried by automobile to the Pasteur Hospital, December 1. There he remained to the end of March, 1917, without preserving anything but the vaguest memories of an intermediary period of more than six months. The memory in these malarial cases often remains permanently altered and there may even be a retrograde amnesia, carrying back to facts prior to the gap and an anterograde amnesia relative to facts after the main gap.
Thus, there is in the febrile period a retrograde amnesia and in the post-febrile period a retrograde or anterograde amnesia. One group of subjects are severe cerebral cases, and the memory gap appears to run back to a period of true mental confusion. But there is another group of patients who preserve throughout the febrile period an absolute consciousness of all acts, and yet the memory gap is just as sharp and definite as in the confusional cases.
Malaria: Korsakow syndrome.
A stoker, 45, was admitted to the Royal Naval Hospital, Haslar, November 6, 1916, from the Fifteenth General Hospital in Alexandria, to which he had come from a hospital in Bombay about three weeks before. At Alexandria he was anemic and showed an edema of legs which had been present for six weeks. Cylindruria; no albuminuria. At Haslar there was no cylindruria and no edema, and nothing but weakness, gouty arthritis of left wrist, right ear and left great toe. Red cells 4,650,000, leucocytes 10,000 (52 per cent polymorphonuclear, 46 per cent lymphocytes). He was rather dull mentally. December 10th, Dr. Fildes found malarial organisms in the blood on the occasion of a hyperpyrexia (104°). Quinine was given. December 14th, he was transferred neurological. According to the patient’s own story, he was born June 10, 1868, lived in Fulham, had a daughter aged 12 years, had recently seen his wife at the hospital: all this seemed plausible enough.
Later, however, he said that the year was 1899, that King Edward was king, that the war was between England and some field forces, etc. This well-nourished, pale, simple-looking stoker spoke quietly and politely; told about intermittent fever; about being eight years on the active list, becoming a reservist and being called up for the war. He read intelligently, could do sums, but did not know the name of the hospital and was confused about the war. He recognized that his memory was not as it should be; constantly stroked his moustache and chin. He was happy and contented.
The gait was normal, systolic blood pressure 140 mm.; no evidence of alcoholism. Blood, January 15, 1917, contained 5,050,000 reds, 10,300 leucocytes (63 per cent polymorphonuclear, 37 per cent lymphocytes). There was a bilateral absence of the ankle-jerks, repeatedly confirmed at subsequent examinations. Wassermann reaction was negative. Puncture fluid contained no cells.
Instead of living at Fulham, this stoker lived at Portsmouth, and had not been seen by his wife for four years. He had done 18 years’ active service and had last sent his wife a letter from the Sailors’ Home at Bombay, November, 1916. They had been married 21 years. He caused astonishment with his wife and friends by announcing that Lord Roberts and General Buller were in command at the battle of the Falklands. He continued to say that he lived at Fulham. He was discharged home, January 22. It seems as if he were living through the period of the Boer war.
Carlill considers that alcoholism may be ruled out, and there is no likelihood that the gout was the cause of the neuritis. He believes that the neuritis was probably malarial. Possibly the illness suffered in Bombay may have been beriberi or it may have been malarial nephritis.
A complication of malaria.
A Senegalese corporal of machine gunners, 21 (early life normal save for sore throats and coughing), was a robust, well-developed man of 75 kilos when he entered the hospital at Konakry, February 15, 1916. He was given the diagnosis: malarial anterior spinal paralysis.
It seems that he had joined a Colonial regiment, April 8, 1915, attended classes as a recruit, left Bordeaux November 1 for Dakar, arriving there November 11. He stayed there some sixteen days, during which time he slept without mosquito-netting. November 16, he left for Konakry, and had his first febrile symptoms November 27, with vomiting, headache, and prostration. His temperature ran as high as 41, but by December had fallen to normal, after quinine.
The corporal was sent away, cured, to his company at Kouronesa, December 6. There was more fever, headache, and vomiting during the railway trip. Quinine again relieved the fever, but a bloody diarrhoea set in so that it was only at the end of January that he could go on service.
February 6, another attack of fever, with shivering and perspiration, lasted for some three hours. He could hardly stand by himself and had to be helped in walking. Next day, another spell of three hours of fever; definite paralysis set in, affecting both legs. February 8 the arms were attacked by paralysis which, unlike that of the legs, was a progressive one, attacking first the shoulders, then the elbows, the wrists, and finally the hands. All the body muscles were in a state of flaccid paralysis, as well as the muscles of the face. The patient was now afebrile. February 9 there was a slight speech defect; the tongue was slightly paralyzed, and swallowing became painful. The jaw movements remained normal. The muscles of the face were intact and the patient could whistle, move his lips, and move his eyeballs normally. Vision normal. The pupils were fixed in dilatation, more widely on the left side. There was a slight[179] contracture of the vesical sphincter, necessitating the catheter. The tendon and cutaneous reflexes were lost.
By February 14, when the patient was sent to the Bellay Hospital, muscular atrophy had made its appearance. No plasmodia could now be found in the blood, which showed 71 per cent polynuclear leukocytes, 20 per cent mononuclears, 9 per cent lymphocytes.
This state lasted til February 25. Despite the fact that the patient ate well, emaciation rapidly progressed. The buttock showed a very few signs of decubitus. Upon this date there was pain from a marked orchitis of the left side, the cause for which remains unknown (no history of gonorrhœa; catheter used for the last time, February 15). The temperature which attended the orchitis came down in three days; the patient’s appetite was singularly good, but the muscular atrophy increased. The speech defect meantime disappeared, and the patient swallowed more readily.
March 7 a slight and hardly perceptible movement could be noted in the fingers of the left hand. Two days later, similar movements appeared in the right. March 11 he could spread his fingers in a kind of creeping movement. Next day slight movements were possible with the legs, and March 13 the knees were movable. March 14 the patient could lift his head from the pillow. The range of movement now increased all over the body. According to the patient, those parts were the first to regain power that had been attacked last. This certainly seemed to be the case with respect to the left upper limb, in which first the hand and wrist, then the elbow and shoulder, successively recovered power. The legs regained their power in the same way proximad. March 17 the patient could sit up and grasp objects with the left hand. The cremaster and plantar reflexes appeared,—the former, more on the right; the latter, more on the left. The left pupil remained in wider dilatation than the right.
The treatment was by quinin and potassium iodide, with massage. The patient was apparently on the highroad to complete recovery, and left for France March 21, weighing 63 kilos.
Trench-foot: Acroparesthesia.
A fantassin, 36, carpenter by trade, went into the trenches October, 1914, and had two attacks of trench-foot, first in January, 1915, when there was a painful swelling of the foot and secondly in July, 1916, when there were some bullae on the dorsal aspect of the feet. These were not serious and the fantassin did not report sick.
He was wounded, August 27, 1916, by shell fragment on the right elbow, was evacuated to the ambulance where the fragment was extracted and then to a hospital which he left cured with a seven days’ leave. Although he had not suffered in any way from his feet while in hospital, and had not been exposed to cold, the bullae reappeared on the feet just as they had been in July. They in fact now formed a sort of exanthem occupying symmetrically the dorsal surfaces of the toes. The bullae contained serum. They were confluent, varying from pin head to a nut in size, were as a rule round, but sometimes irregular. The eruption went on to a cure rapidly and on the twelfth day the bullae had dried up. This patient had hypesthesia up to the knees, hypesthesia of the dorsal surfaces of the feet, hyperesthesia of the plantar surfaces and ankles, hypesthesia of the forearm and the elbow and of the dorsal surfaces of the hands with possibly exaggerated sensibility of the palma surfaces. Hypesthesia of the face was limited to a small part of the right ear. The reflexes were normal and there was no atrophy. The name “paresthetic trench acrotrophodynia” was given to it.
In a service of eighty beds Cottet found within two months fifteen instances of these acroparesthetic disorders regarded as neuritic changes in trench-foot of a latent and lasting character which would have remained unobserved unless there were disorders of sensibility. In fact similar disorders of sensibility may be found without any history of gelure des pieds, forming a latent type of neuritic alteration hardly noticed by the patient himself. In twenty-six cases Cottet found sixteen with hypesthesia of the ears and of the nose.
Bullet injury of spine; bronchopneumonia: état criblé of spinal cord.
As to the development of eschars, Roussy reports the case of a lieutenant wounded September 25, 1915. There was a penetrating wound of the interscapular region. The bullet had entered on the posterior aspect of the right scapular region and had emerged at the level of the first dorsal vertebra. October 1, a neurological examination showed flaccid paraplegia, knee-jerks normal, Achilles jerk weak on the right, plantar reflexes flexor, cremasteric reflex absent on the right, and both abdominal reflexes absent. There were pains in the legs and arms. There was retention of urine with overflow. A slight dulness on the right; temperature from 38 to 39 degrees.
Four weeks later the knee-jerks had become very weak, and the Achilles jerks were now absent. There was an extensive diffuse atrophy of the lower leg and thigh muscles, and a hypesthesia of pronounced degree had developed throughout the legs, over the buttocks, and in the lumbar region. Anal and vesical sphincters relaxed; dejections voluminous; sacral decubitus as well as healed eschars. December 5, the patient was transferred to the Army neurological center; temperature rose; there was much expectoration; paracentesis yielded no fluid; pneumococcus in the sputum. Cystitis had developed despite extreme care. Extensive edema of the legs developed. There was increased dulness on the right side, coughing and dyspnea. Death, January 17.
The autopsy showed a bronchial pneumonia of the right lower lobe, confluent, imitating a lobar pneumonia. The left lung also showed extensive confluent bronchopneumonia at the base as well as disseminated areas and edema of the middle and apical portions. Infectious splenitis, large fatty liver, swollen kidneys, no pyonephritis.
The spinous processes of the 6th and 7th cervical vertebrae[182] were injured. There was no obvious gross disease within the theca except that there was a slight adhesion between the dura mater and the anterior surface of the spinal cord at the level of the 7th cervical and highest dorsal vertebrae. There was, however, a depression on the anterior surface of the spinal cord at a lower level, namely, at the level of the 4th dorsal vertebra. Microscopic examination showed myelomalacia with small cavities in the 1st and 4th dorsal segments, suggesting the état criblé.
According to Roussy, these patients injured in the spinal region are particularly sensitive to cold and support transfer badly even when the disease is short. Such patients should be evacuated to the interior after the shortest delay possible. Sometimes these patients show rib fractures; these are in the posterior portions of the ribs and are due to the fall of the man when struck. It might be possible even that the spinal lesions should through the action of the sympathetic nervous system favor lung infection.
Shell-explosion: Hystero-organic symptoms; decubitus; radicular sensory disorder.
A soldier, 32, was bowled over in a first-line trench by the bursting of a shell that he did not see coming, September 14, 1914. He regained consciousness only in the middle of the night, finding himself half covered with water. He was taken up by the stretcher-bearers at eleven in the morning. Paralysis in the legs was then absolute. There were pains in the legs and in the back, but there was no evident lesion. Knee-jerks, plantar reflexes, and abdominal reflexes absent; cremasteric reflex absent on the left, weak on the right. Tactile sensations, on the contrary, were almost intact except for a slight diminution over the feet and the external aspects of the lower legs. Sensitiveness to pin-prick, however, was abolished throughout both lower extremities, and diminished in the abdomen and back up to two or three centimeters above the level of the umbilicus; that is, including the territory of the first lumbar and the last three dorsal roots. Sensibility to heat was abolished in the feet, the external aspect of the lower legs, and the posterior aspect of the thighs, but was preserved in the second and third lumbar territory, in the anterior aspect of the thighs, as well as in the region below the umbilicus. Micturition was impossible. Constipation the first few days yielded spontaneously September 20. There were signs in the bases of both lungs, corresponding with a suffocating feeling. September 22, he was evacuated, almost well, without signs of pulmonary congestion, having regained the power of urination and some capacity to move the legs sidewise. February, 1915, after evacuation to a hospital at Vic, he showed sacral decubitus, soon reaching the size of a hand, as well as trochanteric decubitus; traces of albumin in the urine, sacral and sciatic pains (recalcitrant to morphine).
He began to improve December 25. Camphorated oil and the sitting posture relieved the pulmonary congestion;[184] the temperature, which had oscillated round 38 degrees, fell; the decubitus scarred over; the knee-jerks reappeared to some extent, and movements began. February 5, the patient had become able to walk without crutches. There was still a two-franc sized area of decubitus over the sacrum, and still a little spinal pain in walking.
It is difficult to consider this case only functional in view of the decubitus, to say nothing of the radicular distribution of the sensory disorder. Heitz brings this and the previously given case (No. 1) into relation with Elliot’s case of transient paraplegia (see Case 210) and Ravaut (see Case 201).
Shell-shock (windage?); typhoid fever; “neuritis” actually hysterical.
A Colonial soldier was sent back from the front, September 12, 1914, for nervous disorder due to the shock of the windage of a bullet. He had not lost consciousness. Under observation at his station, he got typhoid fever, and was cared for at Paris from the beginning of October. About October 15 he began to feel pains in his left shoulder, neck, and arm. The diagnosis, neuritis, was made and was strongly borne in upon the patient, so that upon the cure of his typhoid, he went out on two months’ leave with a complete impotence and much pain of the left arm. At the end of his relief, he was evacuated to Villejuif. January 24, it was found that he had no somatic phenomena whatever, despite the fact that the left arm and a part of the forearm was powerless, and so painful that the patient cried out when his arm was moved. There were a few cracklings in the scapulo-humeral joint.
Hot air and reëducation cured the man in less than two months (March 20), though the disorder had lasted for four months. The patient had been retired for hysteria before the war and had re-enlisted.
Bullet wound of pleura: Reflex hemiplegia and double ulnar syndrome.
A soldier, 26, was wounded in the enfilading of an Argonne trench December 17, 1914. He felt the bullet like an electrical shock, and fell. He had been leaning forward at the time and suddenly felt the left half of his body go paralyzed and his mouth pulled to one side. He did not lose consciousness, and spat up a good deal of blood five minutes after falling. He lay in the trench all night, unable to move his left leg except by the aid of his right. He was evacuated next day. There was a five-franc piece wound at the upper border of the left scapula, four finger-breadths from the median line. There were a few lung signs which rapidly cleared up. December 28, the hemiplegia was better, although neurological examination showed weakness of left upper extremity, abolition of deep reflexes, and certain skin changes of the left hand with edema (main succulent), decreased resistance of muscles of lower extremity to passive motion, especially of adductors and flexors, exaggerated polykinetic left knee-jerk, ankle clonus, Babinski reflex, abdominal and cremasteric reflexes absent on left, platysma paralysis left, with complete paralysis in the inferior distribution of the facialis; whistling impossible. Also the left eye could not be closed singly. Synergic movements of the lower part of the paralyzed face when the right hand of the patient was grasped.
There were also sensorimotor disorders in the ulnar distribution on both sides, with complete anesthesia to pin prick. There was also an area of hyperesthesia of the anterior and postero-internal aspect of the right forearm from below the elbow to the wrist. The tendon reflexes were weak but distinct on the right side. The left arm had feelings of pain, with élancements and formication from the shoulder to the fingers on the ulnar distribution. There was, of course, also, local hyperesthesia due to the wound of the thorax.
Lumbar puncture showed a fluid normal in all respects. We deal with a hemiplegia of organic nature, associated with the bilateral ulnar syndrome. The hemiplegia followed the trauma immediately. When the ulnar phenomena appeared is unknown.
The lung complications cleared. The pains disappeared; motion returned up to the level of the facialis. The patient got up and three months later went on convalescence, still presenting Babinski, exaggerated knee-jerk and weak arm reflexes on the left side. The bilateral ulnar syndrome had disappeared six weeks after the patient entered hospital. Phocas and Gutmann cite a considerable literature on nerve complications of pleural trauma, among them syncopes of grave prognosis; a relatively frequent pleural epilepsy (forty-five per cent fatal) or epileptic status (seventy per cent fatal); and the rare hemiplegia. Accidents and death have followed exploratory puncture of the pleura. Air embolism is probably not the cause. Phocas and Gutmann prefer the theory of a reflex disorder starting from the pleura.
Hysterical tachypnoea.
A man, 23, came to the Lariboisière November 29, 1915, in a hurry to show evidence that he had been invalided for valvular lesion of the heart. In point of fact, the interne found a murmur at the base. Yet there were things in the military papers suggesting caution. The patient next morning showed no malaise, dyspnoea, or any evidence of serious disorder. The contractions of the thorax beat in time with contractions of the alae of the nose, about 112 per minute. Here, then, was a cardiopulmonary patient. The heart impulse was exaggerated; the patient could not or would not stop breathing to aid the auscultation, but almost absolutely normal sounds could be heard at the apex and the base. A valvular lesion could be excluded. The lungs were perfectly normal. The patient was requested to stop his gymnastics, which might have succeeded elsewhere but could not at the Lariboisière!
How could the man have established the synchronism of pulse and respiration and synchronous tachypnoea and tachycardia? Why should he persist in this form of sport, since he had already been invalided? The family history was not especially suggestive (father albuminuric, died at 59; mother well, probably tuberculous). Scarlet fever at eight; occupation, tourneur. After four months of service there was gastric disorder followed by typhoid fever (despite vaccination, according to the patient). Convalescent leave at Paris, during which leave he had swollen legs and albuminuria. May, 1915, gastric difficulty; valvular lesion determined; examination; invalided. At home, a variety of complaints, for which treatment was unsuccessful.
During further examination it was noted that in auscultation the head of the examiner was lifted, as if there were hypertrophy of the heart or an aortic aneurysm. The synchronism was less exact on December 2; 112 beats to 128 respiration. Was this man a simulator? Had he become[189] the victim of his own enterprise? There was no evidence of simulation. It was a question of a monosymptomatic hysteria. Gaillard discontinued the manière forte and undertook a softer treatment, but the manière forte had caused the family to want to take him away. Perhaps they feared a too efficacious treatment. He then escaped observation. It is probable that the tachypnoea ceased during sleep. It was not so marked after the medical visit was over.
Soldier’s heart.
A corporal, 21, who had been a miner and entirely well up to enlistment in August, 1914, went to France in 1915. In June, came shortness of breath and palpitation on exertion; later, precordial pain (fifth space, between nipple and median line) and giddiness on walking. Like all cases of true so-called “soldier’s heart,” this soldier had no physical signs indicative of heart disease, yet reported sick for cardiac symptoms on exertion. In this particular case, as in about half of forty cases reported by Parkinson, there had been no disability in civil life.
August, 1915, the soldier was admitted to the casualty clearing station, where the apex beat was found in fifth intercostal space internal to the left nipple line. The first sound was duplicated in all areas. The second sound was duplicated, though not loudly, at the base. After nine months’ treatment, this man went back to light duty with slight symptoms.
According to Parkinson, the absence of abnormal physical signs in the heart of a soldier should not prevent his discharge from the army if under training or on active service he shows breathlessness and precordial pain whenever he undergoes exertion well borne by his fellows. A simple exertion test, such as climbing 25 to 50 steps, reproduces the symptoms in such a patient. The rate of the heart at rest is a little higher than that of normal men, though the increase on exertion is greater. Nevertheless, it has been proved that the increase of rate on exertion bears no relation to the symptoms elicited and is therefore without value in judging the functional efficiency of the heart.
Soldier’s heart?
A sergeant, 36, had been in the army from 17 to 29, but in 1908 he had acute rheumatism and was discharged from the army. He then became a furnace man and had shortness of breath and palpitation on severe exertion with syncope three times.
He re-enlisted in August, 1914, and had an attack of orthopnea and edema after exposure at a review. However, he improved and went to France in May, 1915, where he again had symptoms; namely, precordial pain and breathlessness on severe exertion. One day while carrying telephone wire under fire, the sergeant felt a sudden pain in the region of the apex beat, shooting down the right arm. “I thought I was shot.” He fell down, very short of breath. His left arm remained sore and weak. Two days later came a similar attack, this time with unconsciousness, and the left arm was now useless. Two days later he was admitted to hospital, where slight breathlessness but no pain and no enlargement of cardiac dulness could be found. No further details are available but it seems clear that this man is unfit for duty. According to Parkinson, it is probable that the infection indicates the presence of some degree of myocardial disease.
Strain and shell-shock: Acceleration of diabetes mellitus.
An infantryman, aged 22, previously healthy and from a healthy family, was struck by a shell fragment in the forehead and lay for several hours unconscious. He did not vomit. He had a number of furuncles on his body and his urine, upon examination, showed a severe diabetes mellitus which increased despite treatment. Upon an attempt to withdraw carbohydrate, the sugar suddenly sank from six to four per cent. Acetone at the same time increased. An abrasion had been noticed by the patient a few days before the shell explosion on the spot rubbed by the tornister. The patient said that since his accident he had had to urinate every night several times and was often very thirsty, neither of which tendencies had he had before. A month before he became merod he had had an injury of the hand produced by a shell fragment. He had undergone tremendous strain.
The chances are that the excitement and the strain had more to do with the diabetes mellitus than the shell explosion.
Dercum’s disease.
An adjutant in a chasseur battalion was buried by a shell explosion, which killed his lieutenant beside him, January 5, 1915, at Hartmannsweilerkopf. Hematuria followed; ten days later, fever with anorexia, and the appearance of two or three lipomata on the anterior surface of the thighs. Remaining at his post, the adjutant took part in an attack, March 5; was evacuated on the 8th; “lipomatosis with febrile reactions.” He spent eight days at Bussang, and thence went to the hospital at Pont-de-Claix. Here marked albuminuria was noted; the lipomata increased in volume; others appeared in the arms. The patient was transferred to the Des-Genettes, where the diagnosis nephritis was added to the previous diagnosis, and a milk diet was prescribed. Convalescence of five months was proposed. The lipomata increased in volume and in number. The patient was then hospitalized at Avenue Berthelot, placed in the auxiliaries, and stationed eight months at his dépôt.
When he was observed by Hollande and Marchand, four nut-sized tumors were found on the anterior surface of the left thigh; two smaller tumors: one of them painful to pressure, lay on the inner aspect, another the size of a small egg lay in the right thigh, and there were two others on the internal aspect and two on the external aspect of the thigh. A nut-sized tumor was found on the inner border of the right forearm, and below it another lenticular tumor. A nut-sized tumor was found on the left forearm below the elbow on the internal border. Small tumors were found on the buttocks. There were no tumors below the knees, in the upper arms, or on the thorax. There were 14 tumors in all. The smaller the tumor the more sensitive, and there was more pain when the tumor had just appeared and during the first days of its growth. There was no spontaneous pain; pain only upon a blow or pressure. Diminished knee-jerks, especially the right; no other neurological disorder, although the patient complained of often having something before his[194] eyes. There was a marked diminution in the memory. Heart was in the 5th space on the nipple line, pulse 110; Wassermann reaction negative; red blood cells, 3,520,000, white cells, 6500; albuminuria, hematuria, leucocytes, and urethral cells in the urine. The temperature had now become normal. The lateral lobes of the thyroid were slightly larger than normal, but not painful. Sella turcica was unchanged upon X-ray. Exploratory puncture of a tumor showed much free fat, without fatty acid crystals and with some fat cells. The cells could not be cultivated in test tube. The authors believe it doubtful whether this instance of Dercum’s disease is related with the shell explosion.
Hyperthyroidism.
A private, 22, was selected by Col. Garrod for hypnotic treatment by Tombleson from among the hyperthyroid cases. He was admitted April 3, 1916, with a typical hyperthyroidism, with manual tremor, enlarged thyroid, pulse 120, blood pressure 136-40, and hemic murmur. Tombleson induced deep somnambulism at the first hypnotic sitting and suggested an increase of nerve strength and steadiness. The suggestions under somnambulism were repeated for ten days. An occasional added suggestion was given as to lessening of the thyroid. At the end of the ten days the patient declared himself quite well.
Eight of twenty consecutive functional cases treated by hypnotism by Tombleson were cases of hyperthyroidism and in virtually all of these an effect like the above was registered.
Shell-shock; thrown against wall, stunned, emotional: Paroxysmal heart crises six days later, observed for two months. Neurasthenia? Mild Graves’ disease?
An infantryman, 29, was sent to auxiliary hospital No. 274, for heart trouble, a little thin but looking vigorous enough (typhoid fever at 13 and some diseases of unknown nature and of brief duration while in military service).
September 24, a large calibre German shell burst and threw him against a wall, producing no wound or contusion. He was momentarily stunned, emotionally much affected, and noted at the time extreme palpitation. He was evacuated to Paris September 30, six days after the shock. His pulse was 130-134, regular, and the heart seemed not to be anomalous in any respect.
But there were paroxysmal crises in which the pulse rose to 180 and in which the patient fell into a state of great anxiety. The mouth temperature in the midst of such crises would always rise to 38°, and this temperature would outlast the rest of the seizure. The man was mentally depressed and apparently indifferent, preoccupied with his heart and his insomnia, but at the same time emotionally easily affected. In short, he was a neurasthenic. There was no change in mental state, tachycardia, or paroxysmal seizures in two months, except that he gained weight. Walking and climbing stairs produced dyspnoea. Urine was negative. According to Dejerine, such a case should be treated by psychotherapy.
Alquier, in discussion, called attention to the slight but distinct tremor in this case, dermographia, and spells of perspiration. He suggested that the case might be one of mild Graves’ disease.
Hyperthyroidism three months, following ten months’ service, at times under protracted shell fire.
A man in service ten months, under strong excitement and at times under protracted shell fire, complained of palpitation, insomnia, dizziness, and dyspnoea. Hospital notes showed that the left lobe of the thyroid was somewhat enlarged. Before the war his neck could not have been very thick; he had served his year out without difficulty. His mother is said to have suffered at one time from thick neck. According to the patient, he had never suffered with heart trouble. Heart not enlarged; blowing first sound over the apex. Graefe, Stellwag and Möbius signs negative. Heart rapid, not irregular; pulse strong. There was fine tremor of the hands, as well as a tremor of the tongue. Knee-jerks increased.
The patient was at first sleepless and excited, but after three weeks in bed the heart murmur had disappeared. After three months, he was ordered to Ersatz with the left side of the neck measuring 20 as against 18 cm. on the right. There was a soft pulsating swelling of the thyroid. First sound over apex still impure; heart action now regular; pulse 64; blood pressure 120 Riva-Rocci; after test exercises, slight dyspnoea. No cyanosis. The outstretched hands were no longer very tremulous. The knee-jerks were still increased. The man had begun to sleep well. His neck was apparently much diminished in girth.
Here then was a case of Graves’ disease of acute development, brought out by nervous stress and excitement as well as by 10 months of war work and exposure to shell fire,—with approximate recovery after three months of rest.
Graves’ disease, forme fruste.
A farmer, 31, entered the Rosendael Hospital, Jan. 25, 1917. He had been two years in active service. The family history was negative except that one of his sisters had had dyspepsia. The patient denied venereal disease and alcoholism and had always been well. At the Battle of the Marne he was slightly wounded in the left knee. January, 1915, he was exposed to gas bombs and explosive shells. He was several days in the hospital spitting, or perhaps vomiting blood and was sent on a long convalescence. On returning to the front, he had to be sent back to hospital with a note, “not fit for service, nervous troubles and paroxysmal tachycardia.” In point of view he now showed a number of symptoms suggestive of Graves’ disease, such as a definite exophthalmia which, according to the patient, started up a short time after the shock and a tachycardia (110-120) with circulatory excitement, a tumultuous heart, neck arteries contracting, almost dancing in their contractions, together with a systolic murmur maximal in the pulmonary area, not retaining, variable,—in short, suggestive of an inorganic murmur. There was also a generalized rapid tremor and a variety of vasomotor disorders, such as blushing and paling, perspiration, exaggerated reflexes, emotionality, logorrhea, jactitation. There were also digestive troubles, regurgitation after meals and the patient had become thin and weak.
There was, however, no swelling of the thyroid gland nor any eye signs other than the exophthalmia. In short this case is doubtless one of the forme fruste of Graves’ disease. It seems to show that Graves’ disease may have a traumatic origin.
Somatic complication in a shell-shock hysteria (Trauma).
Musketeer. No faulty heredity, but was always somewhat nervous. On October 26, a shell burst one meter in front of him, burying him under the anterior wall of the trench. He was dug out and taken to the field hospital, where he remained unconscious until the next morning. On October 29, he was taken to the reserve hospital. Severe pain in the head, entire scalp tender on pressure, especially in the left frontal region, left side upper lip swollen, bluish and discolored. Left tenth and sixth ribs broken. Fracture of skull(?). November 10, at eight o’clock at night, sudden attack of vomiting, and the patient was found in a faint in the water closet. Almost complete paralysis of speech and all of the four extremities. Consciousness obscured; no sensory disturbances. November 11, severe headache and vertigo. Speech somewhat more intelligible. Pulse, 60 to 68. “Evidently secondary hemorrhage in the brain.” November 12, to Augusta Hospital. November 20, admission to nerve hospital. Typical aphonia. Limitation of motion in all four extremities, but no paralysis—anergy. Reflexes normal. Unable to stand and walk. Sensibility preserved. Under suggestive treatment, curative gymnastics, as well as electrotherapeutics, the aphonia and abasia disappeared in a few days, but the patient continued to complain of headache and insomnia. December 16, an attack of nausea, headache, vomiting, loss of consciousness, followed by epistaxis, marked tachycardia. January 4, in his sleep he felt a prick in his left upper arm, as if he had pushed a sewing needle into the arm. X-ray examination showed a needle in the arm. This was extracted under local anesthesia.
[5] VII. Geriopsychoses (senile-senescent group) not represented in war cases (see page).
The Sister’s ear boxed for blow to a German soldier’s pride: Diagnosis PSYCHOPATHIC CONSTITUTION! A true psychosis develops: hate of Prussia and the Junkertum: Diagnosis, DEMENTIA PRAECOX!!
A sick soldier in a military hospital kept complaining of being waked up too early, and of poor food. His reactions looked like the irritable weakness of a psychopath. One day he went into a room where a woman was being examined, without knocking. When ordered out, he boxed the Sister’s ear.
He said himself, on transfer to the psychiatric clinic, that he had always been quarrelsome as a child with his brothers and sisters, subject to fainting spells, and poor and stubborn in military service,—all of which seemed to clinch the diagnosis of psychopathic constitution.
But he seemed to show a decided lack of autocritique. About boxing the Sister’s ear on her saying “Please go out,”—his idea was that he could not let a thing like that happen to him,—a German soldier and a patient! Moreover, “It should not be thought that perhaps I had a love affair with her! There was a cynicism about her.” The Sister had a strong sex impulse, he could see that by her nose: she was, so to speak, “hypochondriacal.” Both in speech and writing he used stilted phrases. The ego at last swelled to the point of his saying that he was an inhabitant of the World and hated Prussia and Prussian Junkertum.
Then came unmotivated states of excitement, with pressure of speech and motion, and eventually negativism. Accordingly, the diagnosis hebephrenia finally replaced that of psychopathic constitution.
Dementia praecox, arrested as spy.
A German private, called to the colors, was supposed to take his civilian clothes to the post office along with his comrades on March 21, 1915. He did not get his package ready in time and was ordered to go with another troop. At an opportune moment, he left the barracks with the package of clothing. When later arrested, he said that he had gone by railroad to Dirschau; then he had visited Berlin. After this, he had walked to Bromberg, Schneidemühl, and Landsberg.
At last he had ridden back to Küstrin. At Küstrin some children told a railway official that the man was making drawings. There was a petroleum tank near by. Accordingly, he was arrested as a possible spy. He claimed that he was not a soldier.
In the clinic, he looked dull and smiled a good deal. It seems that, before being called to the colors, he had been very angry with his wife and had even threatened her. He now explained this anger as his wife’s fault. She had attacked him, he said. He said that he sometimes had attacks of weakness, which used to last two days at a time, but they had recently lasted for a shorter time. He said that his thoughts always wanted to be somewhere else. In fact, he had not performed military duty. His uniform had been gotten for him, but he had had no further orders. Sometimes in a fever or dream his head seemed to be as big as a room, as if there were no space for it. There was an itching in his legs, he said, which often fell asleep so he could not stand on them. He had had syphilis seven years before, after which he had been hoarse, forgetful, and anxious.
Examination showed perceptive power and knowledge to be good. He played the violin, but always the same tunes. He said that he had not worked in Berlin during the winter of 1914. He spoke as if he had been in another sanitarium, where he did nothing but dream by himself, taking no interest[202] in things, and lying indifferently, with a blanket over him.
He said that when he received the uniform he had a longing for clean underclothes. Requested to explain the meaning of the uniform, he remarked: “Why, many have these things on.”
Re dementia praecox, Lépine states that in the French army instances of dementia praecox have been numerous in the interior, both at the time of mobilization and at the time of calling out sundry new classes. He notes that the courtmartial and invaliding experts have neither the leisure nor the experience necessary to keep these men from going into the army. The somewhat frequent remissions in dementia praecox make the task all the more difficult. To be sure, the stuporous and catatonic cases are not very much in evidence in the army; when such cases do occur, it is easy enough to evacuate the patients to a hospital for observation. Far more troublesome are cases of a less advanced or milder nature. Here are cases in which judgment is deficient, and in which quite unsystematic, incoherent, and transient delusional ideas occur. The patient looks quite normal to the non-psychiatric expert. Something odd happens which quite suddenly reveals the delusional ideas. For example, there is a fugue, or else the soldier goes to his superior and aggressively chides him for having troubled him the night before. These particular psychopaths are among the most dangerous to be found in the army.
Fugue, catatonic.
A gunner, aged 23, enlisted on the expiration of his regular period of service and was a good soldier, in excellent health, up to June, 1915. He then began to have a few vague ideas of persecution. In a short time these became more definite and he caused talk by requesting to go into another corps because his comrades did not like him. He told his brigadier that the soldiers were frightening him by magnetism. He had hallucinations of hearing people say, “He will get it.” He kept by himself, would not eat and stood motionless for long periods of time before his mess-tin. He was often found in a dreamy state of apathy. One day he left the cantonment without leave, wandered through fields, had coffee in a village and then started off in no special direction. The police took him without resistance the next day. He said, “My comrades are in politics; they are going to cheat me.” He was brought to Fismes and the ambulance surgeon said that he found he did not know what he was about. He was amnestic for the fugue, explaining that he went because he was frightened. It was hard to get him to eat.
July 14, he was evacuated to Fleury protesting arrogantly, but this phase of excitement passed and he became absolutely indifferent and disoriented. He became untidy in his person and in no way could his attention be attracted whether by mentioning his family or the war. He sometimes made ape-like grimaces and sometimes laughed causelessly. He was occasionally negativistic, but in general was perfectly compliant with the requirements of the hospital. Now and then he started off impulsively to escape but was brought back quite indifferent. Now and then he went into bizarre contortions on a medical visit or aped gestures of bystanders. He began then to go into stereotypical attitudes. This case is the only catatonic one found by Boucherot in his war group.
Desertion: Schizophrenic-looking behavior. Adjudged responsible.
An Italian private in the artillery, a telephone operator at the front, came up for desertion in the face of the enemy. It seems that he had often left his post, going off for a number of hours and drinking. At last he lost his position in the battery, went off and got drunk again, and was removed to a hospital and held as a neurasthenic and psychopathic patient. At the territorial hospital he was regarded as a melancholic. He still showed signs of alcoholism, was hallucinated, did a number of peculiar things, was impatient of medical examination, and was given a furlough of two months for convalescence. He apparently grew somewhat better in his father’s home, but went to a physician there and presented his certificate as a mental case. His behavior was so peculiar on subsequent arrest that he was sent for observation to Consiglio.
It appeared that he had been in military service from August, 1912, and had been imprisoned for a space of eight weeks for disobedience when he had been in military service for six months. He had been punished in the army nine times, once being given 70 days for lying. He was regarded as an undisciplined soldier but not as a nervous or mental case.
At hospital he was in a semi-stupor, claimed that he was forgetful, was apathetic concerning home and relatives, complained of pain in the head, and altogether preserved a strange and stolid attitude with occasional gestures, mimicry, and stereotyped reactions. As he had come to be operated upon, he looked about for the cannon that was to be used in the operation. Accordingly the question of dementia praecox might well be raised.
His indifference turned out actually to be assumed and pretentious. He preserved throughout an arrogant tone, and there were features in his voice that strongly suggested simulation.
According to Consiglio, we are dealing with an epileptic degenerate, addicted to alcohol, lying, and immorality. The question concerning responsibility was settled in the affirmative. Of course, it might be thought that the case was one of pathological intoxication, in which case, the man might be regarded as only semi-responsible. However, the phenomena of simulation, not merely in the observation hospital but also in the period of apparent depression and strange conduct immediately following his arrest for desertion, led to the decision that the man, despite his nervous abnormality, was responsible for his act. He was condemned to 20 years in prison.
Re dementia praecox, Buscaino and Coppola found a number of cases of dementia praecox amongst soldiers admitted to hospital during the period of mobilization; cases amongst men who had not yet been at the front. These mobilization cases, in fact, were as a rule either cases of dementia praecox, cases of a psychopathic constitution, or cases of alcoholism.
A disciplinary case: Schizophrenia, alcoholism.
In October, 1914, a German soldier returned to his barracks late from a drinking bout. He insolently called for order, brandishing his arms, and when the captain rebuked him, he kept a cigar in his mouth. Examined in hospital (Allenberg), he was very reticent at first but wrote his name up over the bed with the additional word “Dead.” He answered, “I don’t know” to most questions. Although it was December, he said the season was summer. He was to be shot for disrespect, he said, but showed more disrespect at every remonstrance. “What is your regiment?” “I am no soldier at all, you know. I have already been discharged as unfit for service.” “Have you been in prison?” “I don’t know. My father often thrashed me.” Then suddenly, after a moment, “I was in prison five, seven, and two years, and my father was in prison four, six, and three years.” He said that he had drunk ether and urged the physician to try it, as one saw all sorts of beautiful pictures and figures and heard music.
Upon investigation, it was found that the man had been in a provincial sanatorium for some form of degenerative mental disease with excitement. He, at this time, had given a number of fantastic stories concerning his wanderings. For example, he said he had come from Australia, where he had eaten snipes and crows; that he was on his way home and would get there in half an hour (real distance 10 hours). Or again, he would roll his eyes, assume a false name and say that he had come from Morocco, or that he was the emperor and would not play soldier. When asked to repeat digits, he habitually omitted the last digit. He had been a poor scholar, and of a tricky and treacherous character.
Despite this history, he had behaved well in the army at first, though insolent to superiors. On July 5 he had a heavy drinking bout, and wrote next day to his mother that he was going to commit suicide. At this time he had been put for safe keeping in a cell, where he saw foxes making as if to bite[207] him. He also said that he was a rich nobleman, a cavalry captain with a servant (asked to be given his pressed clothes and his cigarettes), and was being pursued. He rode his pillow as if it were his horse, and hid it in the horse’s stable, namely, the bed. He ate nothing, as he thought everything was poisoned; smeared himself with faeces and drank urine as “strawberry punch.”
We are evidently here dealing with a psychopath of schizophrenic tendencies, strongly colored, however, by alcoholism. The patient’s father was a drunkard, and a brother and sister were insane.
Re schizophrenia in the German army, Saenger remarks that like paresis, so also latent dementia praecox becomes acute under war conditions. E. Meyer states that amongst 1126 officers admitted to his hospital, August 1, 1915, there were 352 that had either psychoses or neuroses, amongst which were 148 psychogenic cases (either psychopathic or hysterical), 128 with what he terms a congenital psychopathic diathesis, and 76 with traumatic neuroses. The cases of congenital diathesis were somewhat difficult to diagnose, since but 44 of these were clearly psychopathic and in the remainder the question of dementia praecox or of cyclothymic conditions arose.
Stier gives statistics for 1905 and 1906 in the German army, namely 35 per cent of dementia praecox cases. Under war conditions the army has developed far fewer cases: Bonhoeffer, 7 per cent; Meyer, 7.5 per cent; Hahn, 13 per cent. But although dementia praecox figures so much less frequently in the mobilized army than in the army of peace times (manic depressive psychosis is also less in evidence under war conditions), the psychopathic constitutions, hysterias, traumatic neuroses, and the like, run from 17.5 per cent (Stier, 1905-1906) to 54 per cent (Bonhoeffer), 37.5 (Meyer), 43 per cent (Hahn).
Schizophrenic symptoms. Aggravation by service.
A Landsturm recruit, 20, and somewhat peculiar in early life, got whipped by his comrades for getting back too late from leave. The next day he was commanded to carry a machine gun. He threw the gun down and made for the barracks. He was put under psychiatric observation, as he said he did not know what he was doing. His conduct seemed normal at first and he explained that he had heard noises and singing in his head,—pointing to the left ear where there was an otitis media. His skill, knowledge, and general experience seemed well in hand. However, he was not very communicative. Eventually a series of schizophrenic symptoms came to light. He had been hearing threatening voices of varying intensity for two years, sometimes a veil seemed to be before his eyes, sometimes he heard his thoughts, and felt that his whole personality was changing. He began to think that his facial traits were gradually turning into those of the physician. The hallucinations were so insistent that sometimes he did not know what he should do. He was evidently unfit for military service, and the decision was also made that the mental disease had been aggravated by service.
Re schizophrenia in the service, most authors point out that there was either patent or latent schizophrenia before mobilization. E. Meyer attempted to make a study of the influence of the war on psychopaths. He found that the ego of the psychopath remained relatively unaffected by the war. Naturally, the paretics and the seniles were unaffected. The grandiosity and self-centredness of the alcoholics remained as prominent as ever. Seventeen schizophrenic cases were studied, and some of these yielded entire apathy with respect to the war; others had the content of their delusions somewhat affected. Saaler remarks on the military tinge which dementia praecox assumes under war conditions. Dementia praecox and manic-depressive psychosis alike show war changes.
Shot himself in hand. Delusions.
An infantryman, 26, left for the front August, 1914, was slightly wounded, recovered, went back to the front, and then is said, in March, 1915, to have shot himself in the hand. When up for military review a delusional state set in. It seems that he had been interned in several hospitals for examination, but escaped four or five times because physicians wanted to poison him and had partially succeeded.
He came to the Lemioux Custodial Institution, July 12, 1915. His brother, 15, was a voyou; his sister, 16, was an imbecile. The patient told about his military history and how he had shot himself in the left hand, to be with a certain woman, how attempts had been made to poison him, especially a certain man in Bordeaux, who wanted to possess the woman in the case. In point of fact, the physicians could not save him from this enemy.
The patient now became calm and indifferent, lived secluded and almost immobile. In November, however, he began to sit down and eat like others, making low, timorous answers, vague and confused. He smiled cheerfully on questioning, but had many sad ideas. He would smilingly say that he was going to die soon.
Re schizophrenia in the French army, Boucherot found eight cases amongst 107 soldiers admitted to Loiret in the first year of the war. He remarks upon the fact that the schizophrenic cases were often disciplinary. The group is a disciplinary group. Damaye remarks upon the difficulty of diagnosis betwixt feeblemindedness and dementia praecox as observed in the French army.
Volunteer: Dementia praecox.
N. enlisted voluntarily for three years in the Infantry, September 10, 1912, and immediately gave indications of abnormal mentality by his conduct. He made mistakes all day long. At reveille he had to be called several times, and when his corporal objected, he said, “It is cold; I don’t see why I must get up; I am free to remain in bed until 8 o’clock.” In reply to his corporal’s remonstrance about his continued latenesses, he once said, “I can’t get ready; I have no mirror to wash before.” This was rather surprising conduct from an intelligent printer-engraver, who had lived and gone to school in the town of Lyons. He was unable to make his own bed or to perform the simplest of exercises in the manual of arms. He was violent on several occasions, once attacking a comrade who had given him an order, and again when another had taken his place in the line. His reasoning faculties were those of a young child. He continued doing these strange things, and was finally discharged.
Re dementia praecox amongst American troops, Edgar King, before the war, concluded that some 5 to 8 per cent of the American cases of mental disease in the army belonged to the paranoid form of dementia praecox. King lays special emphasis upon dementia praecox, finding that more than one-half of the army admissions for mental disease belong to this group. He calls attention to the number of desertions and undesirables in the group. He found that 70 per cent of the cases showed some heredity.
Hysteria versus catatonia.
A reservist, 31, was in the hospital about Christmas, 1914, for rheumatism, when suddenly he became excited and was sent to the Charité Psychiatric Clinic. He was restless all night, moving about in bed, grinding his teeth, and continually getting up. He had a blank and astonished expression; his breathing was rapid and forced. There were no pyramidal tract symptoms, but muscular power was diminished,—more on the right than on the left. While the knee-jerks were being tested, the legs moved (seemingly psychogenic). Irregular hypalgetic zones were found, and pain was less well felt on the right side than on the left. Answers to questions on mental examination were made with the appearance of effort, the patient breathing deeply and rapidly, head drooping, forehead wrinkling, and eyes glancing about in an astonished way. “How many legs has a horse?” After long cogitation, the man counted slowly,—1, 2, 3, 4. “What’s your wife’s name?” “Marie—Marie, I think.”
In the interpretation of this case, the functional paresis and hypalgesia of the right side, the functional pseudoclonus obtained during the knee-jerk test, the mental situation,—rather suggestive of a hysterical pseudodementia or a “Ganser” dazed state,—make the probable diagnosis at first sight psychogenic. Left to himself, however, the patient assumed a stereotyped unchanging posture; he would suddenly cry out, without particular emotion, that he was to be shot or executed; there was a tendency to rhythmic repetition of certain answers to questions, with the suggestion of perseveration.
After a time, pronounced rhythmic, and then stereotyped, movements started in. Suddenly negativistic phenomena, with refusal of food and self-accusatory ideas set in; speech stopped altogether. Information from his relatives showed that he had been peculiar for some time and had for years occasionally said that he was going to be shot.
Here then, instead of a hysterical pseudodementia, was a case of hebephrenia or perhaps catatonia. Possibly there had been no pseudodementia, but actually an elementary disorder in the associative process. Possibly the defects which the patient early showed, in his responses, for example, were really genuine schizophrenic blocking.
According to Lewandowsky, almost all cases of neurasthenia, of hysteria, and of the so-called traumatic neuroses, stand out very clearly as functional. Bonhoeffer is far less certain that the diagnosis can be made readily in all cases. Antebellum conditions have not been continued in wartime; hysteria was a female affair antebellum, but under war conditions, it is found necessary to draw many differential diagnoses in the male betwixt schizophrenics, epileptics, and psychotics, on the one hand, and hysterics on the other.
Re the so-called Ganser symptom, Hesnard has dealt especially with the value of what he calls the symptom of “absurd answers,” finding the differential diagnosis between dementia praecox and simulation particularly difficult. Hesnard states that incoherence is very hard to simulate. The answers of the Ganser patient are not always incorrect, and not always absurd. The patient strikes one as intact except for the absurd answers; intimidation and other external conditions affect the symptom greatly. Drugs are refused by the Ganser patient.
“Hysteria”—actually dementia praecox.
A shell burst about twenty-five meters away from a soldier, 21, but he continued in the military service thereafter for one month, having only one symptom, a trembling of the arm. This persisting, he was evacuated to Calais, then to Dury to the hospital for the insane where he stayed six months. He was transferred from Dury to the Belgian Hospital for the Insane at Chateaugiron on August 20, 1915. He remembered nothing of his stay at Dury, Calais, or of anything that happened after the shell-shock. He had no complaint and wanted to go back to the front. He was well oriented for time and space and had no disorders of association or perception. Besides the persistent, retrograde amnesia, he showed certain neurological disorders, occasional slight vertigo, a generalized tremor especially affecting the arms but disappearing almost completely at rest, lively tendon reflexes, intense dermographia and cardiac erethism. Diagnosis was made of acute, convulsional psychosis with agitation, convalescent phase.
During March he was quiet and worked about the hospital. In April the patient had a number of seizures of an hysterical nature. In June it was possible to evacuate him to full convalescence. He went back to the front and stayed there, but shortly developed catatonic signs with visual hallucinations and delusions of persecution of a non-systematized nature, such as poisoning, being magnetized, etc. He was at this time poorly oriented for time, assumed bizarre and theatrical attitudes, showed Ganser’s symptom, was oversuggestible and agitated and sleepless. Diagnosis of dementia praecox was now clear.
Hoven remarks that this case is important in that it suggests that a diagnosis of hysteria may easily be mistaken.
Influence of war experience on the content of hallucinations and delusions.
In one of the divisional field hospitals Gerver examined a patient with a very vivid paranoic condition. The following were some of his hallucinations and delusions:
The patient asserted that everyone considered him a spy. Voices continually told him: “You are a spy.” “What? Spy? Caught? What?” “You will be shot by the Germans for espionage.” About three months before his present trouble, the patient had been wounded in left shoulder by a fragment of a large projectile. The wound healed and examination showed a big scar with attachments to the bone. The patient asserted that now he could not touch anything with his left hand, as there immediately go from it “some currents” to the Germans in the trenches and they at once begin shooting at the Russian position. Later, the patient could not even look in the direction of the German front, for all he had to do was to throw a glance in that direction and the Germans would at once begin a bombardment.
All these phenomena he explained as being due to the fact that the fragments of the large projectile which entered his shoulder were poisoned and charmed. Through these fragments there went currents from his hands to the Germans. The patient always supported his left hand with his right, in order not to touch anything with it. He slept only on his right side, so as not to touch the bed or floor with his left hand. During the examination and conversation the patient tried always to look downwards, so as not to throw a chance look in the direction of the German front and call out their fire.
An Iron Cross winner had a hysterical-looking attack (reminiscence of a bayoneted Gurkha). Later he begins to talk of “this damned war that is so vulgar” and of “atrocities, concrete and abstract”: Shortly the diagnosis, hebephrenia, had to be made.
An Iron Cross winner, 21, in the field from August, 1914, to the middle of March, 1915, at first in France, later in Russia, finally went to hospital for rheumatism and sciatica. Three months later he had to be transferred to the Charité in a state of delirious excitement.
The attack began suddenly. He thought he was in the field telephoning with his captain, trembled, threatened to injure people about him, said he could not hold the position with the few men he had, and the like. Next day he quieted down and became oriented for time and place. He explained that he had seen a Gurkha coming upon him with a mallet, by way of revenge upon him because he had stuck his bayonet in the Gurkha’s breast. Behind a little hill he had seen Frenchmen and Englishmen, from which he drew the conclusion there was going to be an attack that night. A little cloud of dust he thought was enemy cavalry. In point of fact, he said he had once on patrol stuck a Gurkha through and the Gurkha’s eyes had since followed him in his mind. He had seen him crawling along the ground one evening and heard his step. The patient had imperfect insight into these hallucinations when questioned about them during the daytime, and still talked somewhat as if the experience was a real one.
At first the situation seemed probably one of hysterical delusion, for which the Gurkha experience served as material. In point of fact, further observation in the clinic showed that the diagnosis of hysteria was wrong. He was induced to write out his experience in a style quite like his conversation; and there was a queer tendency in his writing to the use of[216] foreign words, somewhat improperly used. After a time he began to sit about dully and at times to run about and throw himself into and out of bed, or strike rhythmically with his shoes on the floor, or draw his shoulders together, making grimaces, rolling his eyes and breathing deeply. He said he had to make these movements involuntarily if he were in some way excited. But the peculiar conduct also often occurred without any emotional prod. His emotions were variable, but on the whole indifferent and not always quite suitable.
He frequently said he wanted to get into the field again, giving vent to superficial phrases, such as “atrocities, concrete and abstract,” and “this damned war that is so vulgar.” Yet a few minutes later he would say he wanted to go to war at Amsterdam as Amsterdam had pleased him very much. He said he now had a good many thoughts and ideas which formerly he had not had. He had not been promoted, he said, because he had once angered an officer in another company.
His field hospital history told of certain oddities, such as his lying stiffly in bed heedless of what was going on about him, falling into causeless depression, failing to sleep, and wandering about.
As to previous life, only his own data were available. He had been a moderate scholar, had been rather irritable and thought a peculiar character. In the ward, he showed baseless antipathy to certain patients and said they were well. He seemed to have no insight into his condition, yet wrote in a letter that the insane state in which he was had very much “augmented his mental organism.” The diagnosis of early hebephrenic disorder could now be considered established.
Occipital trauma. Mystical visual hallucinations and explanatory delusions.
A soldier, 33, single, was wounded in the right occipital region by a shell burst September 25, 1915. There was no sign of focal lesion, but a trephining operation was done, which healed perfectly. No disturbance of vision ensued. The soldier was sent to convalesce two months after having been examined by P. Marie at the Salpêtrière. He went back to his regimental station and was put into the auxiliary service April 26, 1916.
In the early days of September, that is to say, a year after his injury, he had a vision. Above the church cross at Chantenay, where he then was, he saw a rainbow-colored bird, passing slowly in the sky. He lowered his eyes and the apparition followed and was projected on the white walls around him. After some time it disappeared. The soldier himself wondered whether his brain injury might not have something to do with the vision, but none of his comrades wounded in the head had had any such vision. So then he thought of tobacco, of which he was a moderate user, and stopped smoking, but the vision returned in the same intensity four months later. On examining the bird’s face carefully, he found that it was the Holy Virgin’s. In dreams he also had analogous visions and in the dreams the Holy Virgin spoke to him, but what she said he did not remember. The bird’s head did not speak to him. The soldier was now convinced that it really was the Holy Virgin who had visited him in the form of a bird. He remembered that he had asked Notre Dame de Lourdes to protect him on the day when he was injured. He had, in fact, eaten a bit of cheese that day upon which he had inscribed a prayer to the Holy Virgin.
Sometimes he saw a red globe shining like a church lamp; sometimes white or black ladies descending from the sky; sometimes other visions. Now the Holy Virgin was to direct[218] all the soldier’s life, but why should he be specially favored? Was he not to be called sooner or later to hold a high rank? He confessed, in fact, that he was to be the King of France, and, like Joan of Arc, was to save his country. Now the soldier began to understand the hidden significance of his surroundings. Everything around him was symbolic, thus, white, of purity, order and royalty; red, of anarchy, disorder and atheism. Some white ship which he saw outstripping some darker ship showed him how the kingdom of France was arriving once more. In fact, there was a symbolism in the whites and yolks of eggs, and the proportion of yolk to white was as one to five. He made talismans to exorcise bad spirits.
Were there auditory hallucinations? If so, they were only episodic and took no part in either the construction or the fixation of the man’s delusional system. Thus, a voice once said to him, “All is not lost. You will be ——.” May 25, 1917, he entered the neurological center at Bourges.
As to the interpretation of this case, it seems that the patient’s mother had crises of depression which at one time caused her to be interned in the Charité. The contributors of this case do not believe that there can be any causal link set up between the mystical delusions and the brain injury.
As an auxiliary the soldier has a right to twenty per cent compensation for his head wound with loss of substance without bulging of the dura mater. Of course, as an insane person he must be retired. The aggravating or accelerating part played by fatigue, emotion and cranial trauma must, from the standpoint of compensation, be taken into account.
Shell-shock dementia praecox.
A subaltern who had been in the service since 1909 was on patrol under shell fire from the enemy, but shortly thereafter came with his detachment into the zone of the German fire. Six men, two steps away from him, were killed by a shell. The officer remained stationary with the rest of his detachment until darkness set in, then returned, made his report in due order, but thereafter tremors set in over his whole body and he lost consciousness. He was carried to the hospital and on the way met his best friend whom he did not recognize. Arrived at the hospital he was unable to give answers to questions or obey requests for two or three hours. He thought he was hearing calls, commands and a dull dröhnen. If an automobile passed he was frightened and cried, “Auto! Auto!” He remained subject to inhibition, anxiety and insomnia for a long time; pulse accelerated; visual fields somewhat contracted for red. Face asymmetrically innervated and dermatographia. Sent to the reserve hospital, he was still apprehensive, especially at night, but in the course of a few days became perfectly tranquil. Only if he took part in the singing of war songs did he feel transient sensations in his knees.
Here is a case of psychic shock with many traits, such as inhibition and hallucinations, suggestive of dementia praecox. The Abderhalden reactions (cortex, white matter, testes, not thyroid) all, according to Weygandt, are suggestive also of dementia praecox.
Shell-shock dementia praecox.
A machine gunner, 23, was the sole survivor, March 18, 1915, of the explosion of a large calibre shell in a block house containing ten men. He worked himself out of the débris and came to Dupuoy’s attention in September, when an extension of leave was asked for him.
There were two groups of symptoms; persistent headache, painful hyperacousia, vertigo, tremulous walk, cervical spinal column stiff and painful both spontaneously and to pressure, muscular weakness, tremor of hands, hypesthesia of extremities especially upper, exaggeration of tendon and bone reflexes with tendency to ankle clonus and patellar clonus, sterno sign lively, frequent nosebleeds (two to four times a week), profound sweating, unequal pupils.
On the mental side it was clear that the man’s character had changed, according to information supplied by the mother. Aprosexia, impairment of memory, recollective and retentive, inability to give age, birth date and similar data. Words came with difficulty. Some disorder of comprehension; stereotyped replies; negativism; indifference; he would sit hours in a chair or on a bed silent and inactive. Fixed attitudes; dull glance; eyelids half closed. In short, it seemed as if this patient was a case of catatonic dementia praecox.
Re dementia praecox and shell-shock, Stansfield remarks upon the similarity of certain symptoms found in Shell-shock to those of dementia praecox; for example, apathy, retardation, amnesia and speech defect. According to Stansfield, one often gets the impression in a Shell-shock case as though the trench and shell fire stress had merely brought out a latent dementia praecox.
Re his new “sterno” sign (sternomastoid contraction on percussion of neck at level of third dorsal vertebra), Dupouy claims it negative in normal subjects, positive in concussion, meningitis, and general paresis.
Shell-shock; fatigue; fugue; delusions. Recovery.
A sergeant, 40, had had nineteen years of service and had been married five months when he was recalled to the colors when war broke out, and sent to the front. March, 1915, he was exposed to bomb explosions during a very intense bombardment. He then got into the way of saying that he was akin to everybody. April 20, he was evacuated on the score of general fatigue, rejoined the company May 17, left his comrades at the end of June, and was taken up as a deserter by the police, who, observing his state, brought him to a hospital. He there showed “cerebral overexcitement” with “incoherence and nervousness.” In two or three days he was much better. He was evacuated on the sixth day to the hospital at Vichy.
There was amnesia for the fugue and he could remember no further back than the extraction of a tooth at the Vichy hospital. In fact, he attributed the fugue to this dental operation. His wife took him home, but he soon threatened her with a revolver; got better in the night and next day went about apparently normal, buying things, however, extravagantly. His delusional state began once more, and two days later he was brought to Limoux. It seems that, while in Mauretania, he had formerly shown signs of mental disorder, having a mania for wireless and airplane inventions and the like. A cousin-german had also been in a hospital for the insane twice, recovering each time. There was a lingual and manual tremor. The man had not been recently alcoholic. He was a little irritable and showed a little megalomania, but worked hard and made himself useful. He went out, recovered, November 12, 1915.
Analysis indicated that this sergeant received a moral shock as a consequence of his fatigue and the shell fire, which emerged in a spell of confusion. It may be that his predisposition had something to do also with this spell and the fatigue. In any event, it seems as if the latter phenomena were not all assignable to war stress.
A maniacal volunteer.
An Alsatian became the object of much attention when he enlisted at the outbreak of the war in the infantry at the age of 59. He was interviewed and soon became more than naturally exuberant. The peculiar things he did soon brought him to Fleury in a gay and expansive mood, singing and talking as hail fellow with everyone he met.
The next day he grew more excited, disrobed and threw his things out of the window, filled his bed with excrement and wanted to smear the orderly therewith. He took other attendants for old friends and wanted to kiss them. His language and ideas were incoherent. He broke glass.
This situation of alternate joy and anger lasted one month, leaving him in an excitable, unruly state. He wrote many prolix letters to the prefects and the ministers, insisting on the discharge of certain patients and offering plans for the defense of France. He got better and finally, in October, 1914, was invalided home still slightly exalted.
Re the cyclothymias, Montembault remarks that manias have been less numerous than melancholias in the present war, whereas in 1870, manias were more common than melancholias. Morselli likewise remarks upon the rarity of manias amongst the Italian soldiers. Butenko reports upon the maniacal cases amongst the Russians and how the men wish to enter the ranks, the women the nurse corps. E. Meyer, for Germany, found 4 per cent manic-depressives. Birnbaum quotes from Bonhoeffer (3 per cent) and Hahn (2 per cent) for war times as against Stier’s 9.5 per cent of cyclothymic cases in the antebellum period, 1905-1906.
Fugue: melancholia.
Logre classifies as a melancholic fugue the adventures of a man who had been depressed for some days, had stopped talking and eating, and ran away suddenly in the middle of an attack of anxious agitation. He was very anxious over the health of his daughter, whom he thought to be severely ill. It was, in fact, to go to Paimpol that he deserted, but he deserted with his arms and without any money. He went off on foot “in the Brittany direction.” He had gone 50 kilometers, the next day, and was picked up near Chateau-Thierry by two gendarmes, who fell upon him, seeing his regalia, and cried, “Give yourself up!” He replied in a firm voice, “No, I shall not give myself up!” and seizing his gun he made at one of the gendarmes. There was a fight. The gendarme declared in his report that he judged it opportune to retreat behind a tree. The soldier, knowing his trench lore very well, barricaded himself behind a pile of beets. There he would have held the gendarmes in check for some time if another had not succeeded by a détour through some woods, in catching him. He gave himself up after firing several ineffective shots, but not without getting a bullet in his left thigh himself. With the charge of desertion and attempt to murder, he was handed over for mental examination. He was, in fact, a melancholic patient, subject to attacks of anxiety, and requiring long observation at a neuropsychiatric center for diagnosis.
Chavigny observed numerous victims of melancholia characterized by war terror. He remarks a somewhat curious fact that, whereas the melancholics were numerous and their mental states related to the war, on the other hand, the paretics were rather apt to be maniacal than melancholic. Soukhanoff, however, remarks on the occurrence of depression in a great number of types of psychosis, as was found in the Russo-Japanese war. Soukhanoff found frequent instances of schizophrenia, wherein the melancholia tends to conceal the actual dementia praecox. Soukhanoff predicted that depression will figure largely in the war.
Apples in No-Man’s-Land.
A soldier in November, 1914, suddenly climbed out of the trench and began to pick apples from an apple-tree between the firing lines. The idea was to get a bag of apples for his comrades, but he began to pelt the French trenches with apples. He was called back and on account of his strange conduct sent to hospital. Here he was at times given to pressure of speech and restlessness; he would climb the posts of the sleeping room and then loudly declare he wanted to get back to the trenches; he did not want to go back to Germany alive; did not want to live over to-morrow; was guilty of a sin; had a spot of sin, Schand, on his heart. Sometimes he refused food and said anything else tasted better. It seemed he had formerly talked about the Iron Cross.
After being transported to Germany, he was at first a little negativistic and apparently blocked. He talked about his experiences and said he wanted to go to Russia. He explained the episode of the apples on the basis that they were all really hungry and that he had sought to encourage his comrades who were unused to war. He had noticed the French all shot too high.
Physically there was a somewhat uneven innervation of the face, unilateral epicanthus and an areflexia of pharynx. Now and then the man was very irritable, but in general he was in an elevated frame of mind.
Weygandt interprets this case as one of hypomania, remarking that war influences may serve to bring out preëxisting manic depressive tendencies.
Re differential development of mania and depression, see remarks under Cases 163 (Boucherot) and 164 (Logre).
Four months in trenches: Depression; war hallucinations, arteriosclerosis (aged 38).
A Russian reservist, a private, 38, went into the trenches, March, 1915. Without taking part in any battles or sustaining any injury, he four months later became depressed and had to be evacuated to a hospital and thence to the interior, little changed for the better.
He was an ill-nourished man, of middle height, with pallid skin and membranes; arteries sclerotic; face, eyelids, and tongue finely tremulous; hands tremulous; slight dermatographia; exaggerated tendon reflexes; pulse 100.
He seemed disoriented for time and place; looked weary; walked with back bent over; spoke in whispers, and appeared somewhat unclear. Thinking was slow and difficult.
He occasionally shuddered and looked to one side, said he was afraid, and was constantly troubled by thoughts of fire. The Germans were pursuing him; he could hear their voices and footsteps. He himself was doomed, and his family also; he felt he was the cause of all the domestic woe. His own heart was dying away; he had fits of anguish and causeless fear, and was under the constant expectation of death.
One day, he escaped from the hospital and went to the chief physician’s tent, where he lay on the ground. When he was found and asked why he was there, he begged the physician to save him from the Germans. The man was not alcoholic and had no previous history of mental disease.
Re early arteriosclerosis, Maitland in the second interim report of the British Association Committee on Fatigue in Warfare, speaks of the many Serbians, who, after six years of nearly continuous Balkan war, show a marked arteriosclerosis. Maitland remarks that the line officers were already showing (1916) a growing delicacy of perception as to the “breaking point.” Men that do not break may return from the lines, pale, with low blood pressure, and a faiblesse irritable, shown by restlessness of hands and feet.
War stress: Manic-depressive psychosis.
A naval officer, 22, transferred from sea service, went into Belgium, November, 1914, in a Fusilleur brigade of marines and there greatly distinguished himself, growing very weary and enervated, however, about the middle of April, 1915. His attitude to the men altered: he sometimes struck them; gently, though, according to his account. They must do in ten seconds what they really could not do under ten minutes. The officer, in fact, had lost all notion of time. He went about agitatedly, contradicted his superior officers and was troubled because, as he said, they often were men of inexperience as compared to himself. He grew irritated, too, because there were Free Masons in the army and when he was sent to the asylum in July, 1915, said it was the doing of the Free Masons. He did not seem to have any hallucinations. His ideas and sentiments were very labile, and a bit confused, and not all his interpretations dealt with Free Masons and occultism. August 5, however, the phase of calmness was again followed by agitation; he broke things and laughed explosively. August 10, another attack occurred, with destructiveness. During the next few days there were alternate phases of depression and excitation. He was negativistic, resistive and struck attendants.
Re war stress and psychoses, Morselli finds the acute cases on psychopathic soil. First in the list, he places the neurasthenias and psychasthenias, and second, the hysterias, two groups which, more than the remainder, may be said to constitute the so-called Shell-shock group. Third, he found depressions ranging over into a delusional state with suicidal ideas; fourth, a species of stupor, occasionally catatonic, recalling dementia praecox; fifth, transient hallucinatory states; sixth, confusions (Meynert’s amentia?); last, manias.
The above case of Dumesnil appears to be a pure case of manic-depressive psychosis developing on the war basis, but perhaps merely comes from a latent cyclothymia.
Predisposition; war stress: Melancholia.
A farmer, 30, was mobilized August 2, 1914, and was wounded in the hand September 27. He went back to his dépôt in December and stayed there until March, 1915, when he was sent to Dunkirk. Before leaving the dépôt he said that he had heard soldiers declaring that he was not doing his duty, that he was going to be court-martialed, that life was at an end for him. At Dunkirk he said these same soldiers continued to say the same things about him, forming a band about him, led off by a subaltern officer who meant to frighten him and to make him talk. One night sulphur was thrown at him for poisoning purposes; he complained of this to a sergeant and declared he did not understand why he should be thus pursued. After the bombardment of Dunkirk the hallucinations grew more intense. He was sent to hospital and was so harried by the voices that he wanted to throw himself down a staircase but was caught in time. At the hospital for the insane he complained that his thoughts were being heard and loudly repeated; he was made to make incoördinate movements; was treated as a spy. He thought he must be a German or they would not treat him so. He waited for death as he wanted to be executed at once.
This man’s father was alcoholic. He himself at the age of fourteen had had a period of neurasthenia with some sort of nervous seizure for a period of five months. At 28 he had a rheumatic seizure which kept him in bed fifty days. A daughter born to his wife had died a few days after birth.
Dumesnil’s analysis is melancholia with delusions of persecution, due to war stress in a predisposed person.
Re melancholia and the war stress, see remarks under Case 167. Re manic-depressive psychosis in the Russians, Khoroshko found 9.4 per cent of manic-depressive cases, the same percentage of epilepsies, 10 per cent of paretics, and 20.4 per cent of schizophrenic cases amongst a group of 318 neuro-psychiatric cases. Almost all his manic-depressive cases had been patently so antebellum.
Depression; low blood pressure. Pituitrin.
A private, 22, was sent back from Germany as insane. He had been in the asylum at Giessen seven months, and a prisoner in all fifteen months.
August 16, 1916, he was admitted to Mott’s wards at Maudsley in a markedly depressed and lethargic condition. He had improved somewhat in October, but still had periods of depression. He was put on thyroid extract (Green’s treatment was in doses measuring from gr. ¼ to gr. 1, t.d.s.; according to Green, the effect of thyroid extract is more rapid when coupled with pituitrin). In December he was given pituitrin extract gr. 2, t.d.s. In January, 1917, he was no longer depressed or lethargic. He complained of pain in his back, found to be due to a bullet. This was removed.
Re prisoners, Imboden found amongst 20,000 French soldiers taken prisoner at Verdun after the severest drum fire and strain, only five neurotic cases (data of Mörchen), and Wilmanns found but five neurotic cases amongst 80,000 prisoners. Lust reviewed 20,000 war prisoners in Germany and found singularly few instances of neurosis. Shunkoff notes, however, that there are a number of psychotic cases amongst the prisoners because the mentally diseased who do not disturb the military routine are kept in the line. Bonhoeffer found amongst Serbians taken prisoners by Germany, emaciation, atrophy, heart disease, and frequently tuberculosis. (See Case 166.) Bonhoeffer noted the absence of psychoses amongst these Serbians, drawing the general conclusion that campaign stress was unable to bring out psychoses. But, although the exhaustion psychoses are not found, there are exhaustion neuroses or states of acute nervous exhaustion, characterized by somnolence and depression, followed by a mild degree of overemotionality. vum Busch states that interned German civilians have gone into psychosis frequently. It is said that one in 10,000 war prisoners in Germany has committed suicide. Bishop Bury found at Ruhleben 60 or 70 cases of psychosis.
Hallucination in the field (surprise by BOCHES); scalp wound: Three psychopathic phases—(a) over-emotionality, (b) obsessions, (c) loss of feeling of reality (victim a “constitutional intimiste”).
A cashier, 31 (of rather weak constitution but without hereditary or acquired mental taint—a religious man and for religious reasons chaste, always given to metaphysical speculation and introspection, but on the other hand, much interested in sports and very sympathetic with English manners), was about to go to live in the country on the advice of his physician when the war broke out. He was called to the colors and shortly lost his tendency to bronchitis, put on flesh, and felt delighted with his situation.
After almost two years of effective service, June 2, 1916, when his troop was cautiously advancing into a trench at the end of which they might be taken by surprise, suddenly the officer cried, “Sauve qui peut! The Boches are on us!” The patient remembered seeing Germans emerge from every side, remembered his fear, how he had turned about and crossed over a palisade, and then no more until he found a scalp wound being staunched by his comrades in the trench. He put on his own dressing and followed his comrades on foot.
He quickly got well of his scalp-wound but remained in hospital, very weak, extremely impressionable, jumping at every noise. He got somewhat better with the rest in bed, though even a month after his hallucination, he had a spell of insomnia, thinking about his future and the possibility of a relapse, and having war dreams from which he would awake in a sweat. Once on awaking, he distinctly heard a voice saying, “Well, Charles?” This hallucination occurred five times, under exactly the same circumstances, except that once it was in the daylight. Adrenalin was given, 1:1000, 10[230] drops the first day, 20 the second, 30 the third, and a like amount on the following days. After three days of such treatment, the patient said he felt much better. Later he had a period in which he had lost self-control and could no longer take any initiative. Thus, if he wanted to reply to his mother, it seemed to him that some one not himself was ordering him to write. He now asked himself if he were not really dreaming. He would not be sure of his actual existence unless something happened to prove it, such as the nurse’s bringing him a plate.
In short as the first phase of diffuse over-emotionality had been succeeded by a second of obsessions, so the obsessive phase was succeeded by a third phase of mild loss of the feeling of reality. The first phase following the wound was one of disorder of attention, of memory, and in fact of all the mental functions, associated with tremors, tachycardia and dizziness. The second phase seemed, as it were, to crystallize intellectually the anxious apprehensiveness of the first phase. There were fears that the ceiling would fall; there were scruples concerning the past; there were fearful premonitions for the future (such as, that any bomb he might pick up would burst). According to Laignel-Lavastine and Courbon, there may have been a predisposition in the vegetative system of this subject, or even a basis in his tuberculosis, of which, in fact, the X-ray showed still some slight evidences. The obsessions appeared at night, at a time, namely, when the vital rhythm is passing from a sympathotonic period over into a vagotonic period, at a time when the organic sensations are apt to swim to the fore. According to this analysis, these somatic sensations, precisely those that the battlefield had also brought out, brought out again the other emotions which he had felt on service. It was always the emotions first developed in military service that were revived in the disease. In the third phase, the physical condition of the patient had grown much better pari passu with disappearance of the obsessions and the onset of the personality disorder. The adrenalin raised arterial tension, and going down to the sympathetic caused the anxiety and war emotions linked therewith to disappear; but the adrenalin treatment,[231] according to Laignel-Lavastine and Courbon, disturbed the organic sensations so suddenly that there was a break between the new conscious status and the old. In consequence, the patient felt that these new sensations no longer really belonged to him but were of a xenic character, imposed upon him from without in such wise that he continually asked himself whether he was really dreaming or no. This man was a constitutional intimiste; a psychasthenic en herbe.
Re neurasthenia, Lépine notes that there are transient and relatively permanent cases. The term is often used to cover graver disorders, such as various melancholias and anxieties. As a rule, in France, the neurasthenics are evacuated for fatigue. There have been a number of cases in officers, who find themselves unable to make decisions on the minute and to remember military facts, or perhaps are unable to make any physical or intelligent effort whatever. A true neurasthenic, however, ought not to be a confused person. He is a man with a rather unusual clarity of view as to his situation; and his trouble appears to him to be somatic rather than as of the nature of a depression. He feels that, if he could only rest, he could be cured. Neurasthenia, according to Lépine’s war experience, is practically always the disease of a highly cultivated nervous system, and appears in men who have undertaken responsibilities. There is a group of young men who have never been physically strong, bowled over at last by some small event, such as a diarrhoea, and unable to carry on. Such men, perhaps, are likely to have some traces of an old tuberculosis, an adrenal insufficiency, or insufficient hepatic function. Martinet has found them hypotensive and rather poorly aerated. There is another group of neurasthenics (Maurice of Fleury) that are old arthritics, with increased tension. These cases are not found at the front because conditions there rather tend to reduce the trouble; but they are found doing office work in the interior. Besides these cases of the “cultivated” group, Lépine also finds a number of neurasthenics amongst the peasants, in whom anxious ideas may lead to hypochondria.
Fugue, hysterical.
The fugue of an adjutant who left his regimental relief post at Palameix Farm and was found several days later with his family at Castelsarrasin, was reconstructed from partial records as follows:
November 27, 1914, after a night in the trenches, when two shells burst near him, the adjutant turned up at the relief post with wild eyes and a complaint of fatigue, and of an old wound and headaches. The wound he had gotten in a fight which gained him his grade of adjutant. The physician prescribed rest. He sat down by the stove, silent and dejected, and at about four o’clock, in the presence of the medical assistant, made preparations to go, leaving sack and saber behind, but taking outer garments and revolver case. On the way from the farm, he met comrades and told them he had been evacuated to his dépôt on the colonel’s order, and walked with them, Indian file, in the midst of falling shells, the others talking but the adjutant himself silent. At nightfall, he said, “Good evening,” and parted from them. Of his further course to his home, all recollection was lost by the adjutant; in fact, he did not remember anything beyond the Palameix Farm, where he had seen a comrade wounded in the head. He got home November 29th, at eight in the morning. He had most of his money with him, having traveled by train some distance without a ticket; moreover, without asking for a ticket, and without having eaten. When the ticketman in his home town asked him whether he was back from the war, he looked at him vaguely and went out without replying; nor did he reply to a newspaper man on the road home. This was the more strange as he was ordinarily an affable person.
He had a convulsive crisis at home, after which he was exhausted and apparently unable to move or reply. A physician said that he had had a cerebral shock. When the police arrived, two hours later, he was apparently delirious, saying[233] such things as, “The Christians want to shoot me but I know the rules! Come, boys, stay in the trenches!” “There are two more dead ones!” etc. During the day he recovered consciousness and was greatly disturbed at his military crime.
In point of fact, he had had, at the age of 17, analogous crises, as was certified by Régis, who had cared for him from 1907 to 1909 for hysteria with sudden somnambulistic attacks and amnesia.
While in prison after his arrest, he also had hysterical crises with agitation, flushed face, hard attempts to vomit, respiratory disorder due to interference in the throat (globus hystericus), and delirious phenomena (“Germans had followed him home”).
After his birth his mother had had two miscarriages and a stillborn child. The adjutant was declared irresponsible and acquitted. This is apparently an instance of hysteria without stigmata.
Hysterical Adventist.
An engineer, 31, in the Landwehr at the outset of the campaign, was first put on sentry service in Berlin on the ground that he was an Adventist. He was later put into the military service and had difficulty because he did not want to serve on Sunday. He was shoved from one company to another. He refused to be inoculated and was arrested therefor. In the prison, he began to hear God’s voice calling to him distinctly to tell his fellow-men that the end of this was going to be the end of all things. Back in the barracks, he again heard a voice—“Come forth!”—“Go!” He went! He had his revelations then published in the form of tracts, and held Bible readings day and night among his friends in Bremen—looking for the signs of the times in the Bible sayings. One of his fellow Adventists finally warned the police, and the military authorities put him under psychiatric observation. He proved to have numerous stigmata of hysteria. He talked freely about his visions, and was aware that he was punishable.
Here, then, was a case of hysterical psychosis, liberated by military service.
Fugue, psychoneurotic.
The question, Is this escape really a fugue? is brought up not only in epileptic, alcoholic, and melancholic cases, but also in cases suggestive of psychoneurosis. A son of an insane person was subject to what may be called a phobic or obsessive fugue. The case may be called one of morbid cowardice and was observed in a soldier in the trenches. In point of fact, the man had always been an anxious and fearsome person, given to phobias. He had night terrors and fear of diseases and death. He was agoraphobic in adolescence, and had to have a policeman or passerby go with him through a public place. He had had also suicidal and homicidal obsessions, and periods of psychoneurotic anxiety.
This man’s sojourn at the front put his morbid personality to a cruel test. He was soon known by all in the trenches as a froussard. He had a terrible fear of the guns, jumped, grew pale, trembled, complained of palpitations, lumps in the throat, etc. He was the laughing-stock of his comrades; but according to the patient himself, he was more afraid of his own emotion than of the shells, although his comrades couldn’t understand it. He was employed as a kitchenman, in a post not much exposed. A more resolute comrade helped him to escape, escaping also himself, thus bringing up the problem of fugue á deux. Limited responsibility was decided for the case, although the fugue had been aided by his morbid anxiety. Of course, his place was not in the trenches at all. He was condemned to two years in prison. After his sentence, he was given a chance to rehabilitate himself by sending him again to the trenches, but he had to be evacuated a few weeks later on account of his increasing emotionality.
Shell-shy; war bride pregnant: Fugue with amnesia and mutism.
A rifleman, 30 years old, was brought to a casualty clearing station, looking like an imbecile, with a history of having wandered about aimlessly, not knowing where he was or what he was doing. On questioning, he remained absolutely speechless and terrified. Four days later, in conversation with Major Myers, he was got to speak in a faint voice about his wife, home, and occupation, saying that the month was October (when it was actually August) and that he had been in France two months, when it was actually twelve. He described emotionally certain trench scenes, and then thought of his wife sewing.
Hypnotized, he remembered going into a dug-out after running away from shells; he was made to talk in a loud voice. Next day, during hypnosis, proper orientation for time reappeared. He was got to write an ordinary soldier’s letter to his wife. The following day he was active, making beds, but was mute (there was a case of mutism in the same ward). Under hypnosis speech returned. He had gone to a horse show, and upon his return, something hit his back; shells had begun to fall. Found hiding in a shack, he was carried to a hospital in an ambulance. After this hypnotic treatment, the power of speech was maintained, although his voice became faint or failed whenever he was asked about the incidents described above. Next day he waked speaking normally, nudging his neighbor and asking, “Is it me that’s talking?” He had before appeared dull and depressed, but now appeared an intelligent, agreeable, and garrulous fellow. It appears that his wife was a war bride and he had heard some months since that she was pregnant. He had been troubled, thinking she was in money difficulties and kept thinking about a friend whose wife had lost her first baby. Recovery appears to be complete except for occasional headaches, and the patient is now serving in his reserve battalion.
A neurasthenic volunteer.
A man who volunteered for service at the outbreak of the war (he had recently been an inmate of a sanatorium) was sent back to England as neurasthenic after three trying months at the front. The case sheet read that he was subject to dazed conditions. In hospital he suffered from insomnia, and before his slight periods of sleep he constantly had visions of two comrades who had been terribly lacerated at his side. These hallucinations in their reality aroused in him a fear that he was insane.
There were also terrifying dreams, beginning with episodes at the front and ending with sex experiences. These dreams were ended by seminal emissions. These formed a second cause for the patient’s belief that he was insane, as he said he remembered literature read as a boy concerning spermatorrhoea.
In the treatment of this case the writings of psychologists who had studied hypnagogic experiences were used and the absence of hallucinations during waking hours was stressed. The remembered literature regarding spermatorrhoea was discounted by the rational explanation of his state.
He seemed to be getting on well when a trivial accident caused a relapse. While he was saying goodby to his wife, who had visited him, she was taken ill, and he went home with her. He was punished for being late in returning to the hospital. Although no moral stigma attaches to confinements in barracks in most soldiers’ minds, in this man a depression was produced and suicidal talk followed. It seems that his father had been sent to jail when he was a child, and he felt he had been tainted by his father in such wise that his “criming” was due to heredity. With the removal of this misconception he became more rational and immensely improved.
Five months’ war experience: Neurasthenia in subject without heredity or soil.
A 38-year old soldier is Jolly’s example of a neurasthenia produced in a person without previous neurasthenic traits or hereditary factors. This soldier had been a moderately good student and never ill. He went into the battle line in December, 1914, and came out in May, 1915, on account of exhaustion. The case is not wholly convincing since the patient had a shrapnel injury of the skull, described as of so inconsiderable a degree that he was not put on the sick list on its account. The patient finally arrived at the Nuremberg Hospital, complaining of pressure in the head, as if there was a band around the head, and dizziness. He wept a good deal saying that the sight of the dead had frightened him. Sleep was restless and there were unpleasant dreams of the battle field. Intelligence was not in any degree disturbed. The supra-orbital points were sensitive to pressure. The tongue showed a marked tremor and was coated; the mechanical excitability of the muscles was increased; and there was reddening of the skin on stroking. There was a fine tremor of the extended fingers, less tremor of the head and of the body at large. Knee-jerks normal. Nutrition well preserved. Partial recovery in the hospital.
Importance of arterial hypotension in the diagnosis of psychasthenia.
A man of 32 (never well, with general weakness, ideas of consumption and vacuous thinking following a good recovery from bronchitis at 28, unsuccessful in business, subject to weaknesses) had had eighteen months antebellum of what might be called psychasthenia. There were spells of loss of consciousness without convulsions, and probably of hysterical nature. There had been for two years insomnia and a general hypobulic slowing down of work.
In military service the crises became more frequent, coming two or three times a week. Tuberculosis could not be shown, nor was there any organic lesion of the nervous system. The arterial tension (Potain sphygmomanometer) stood at 11.
According to Crouzon, arterial hypotension is an objective sign tending to assure the organic nature of a psychasthenia. Whereas simple neurasthenics are hypertensive, others have long been recognized as hypotensive; but heart experts have recognized this asthenic hypotension more than psychiatrists or neurologists. In differential diagnosis it is necessary to consider and exclude the early hypotensions of pulmonary tuberculosis and those of Addison’s disease. This hypotension is most frequently observed in constitutional neurasthenics and psychasthenics. Hypertensive drugs, adrenalin, tincture of colchicum, have produced a transitory improvement in a number of cases, but the amelioration has halted with the stoppage of the drugs.
Re hypotensive and hypertensive cases, see remarks of Lépine under Case 176. See also Case 169, illustrating some contentions of Green, from Mott’s clinic.
Service in France and Salonica: Psychasthenia.
A man, 29, after some months’ service (three months in France and later in Salonica) was invalided for backache, insomnia, and enuresis. It seems that this married man had never done any work after leaving school at 18, having substantial private means. He had been married for 3½ years, had a son, and was, according to Eder, perhaps morbidly attached to his wife and child. He had been a sportsman and was selected for sniping work in France. The son of a shipbuilder, he had always planned all kinds of ships and engines, never to be used. After seeing the world, he was about to enter his father’s business when he had to take care of his father in a nervous breakdown. After a second attack, the man never entered business.
February 6, 1916, wide-spread patchy analgesia and lumbar hyperesthesia were found. He thought sluggishly, being restless and holding attention poorly. He began twenty letters, destroying each after finishing a few lines. He was shy and felt that everybody was looking at him. He became speechless if he had to address his commanding officer. He had an obsession to mark each flagstone and touch each post, and various counting and arranging obsessions.
The Horme (Jung) was elusive. A dream: “I was in a cargo boat in the river; we were steering straight into ferry and harbor. The pilot rang down ‘Full speed to stern’; I pushed him out of the way, and rang down ‘Full speed ahead, two points to starboard.’ We went straight past ferry and harbor without accident.” Again, a few days later, “In a motor car, came to some rocks which sprang up in front of me. The machine broke down. I abandoned it and clambered over the rocks. It was tough work. My object was a ship. I got to the ship, took hold of the wrench, and signalled ‘Let go.’” Herein, according to Eder, are certain obvious symbolic conversions.
Antebellum attacks, with dizziness: Fainting on horseback. Neurasthenia.
A harness-maker, 37, a corporal, was called to the colors on the second day of mobilization. He was attacked by a slight dizziness in the evening (see previous history below). He went into the field on August 7 and had repeated attacks of dizziness, despite which he took part in several skirmishes. He could not ride on horseback, since dizziness, ringing in the ears, headaches, and trembling of the whole body would develop. October 27 a severe fainting attack came while he was sitting on a horse. He woke ten hours later, vomited several times and felt dazed. Two weeks later hearing in the right ear began to be impaired. During several transfers from hospital to hospital near the East front, there were two more severe attacks of dizziness and vomiting. Brought back to Germany, the patient finally came to the Jena Hospital, May 20.
The estimate of this case depends somewhat on the previous history. He appears to have come from a healthy family, was married, and had two healthy children. His bodily and mental development had been normal; he had been an unusually good scholar, but he stammered from his tenth year without apparent reason. He had had treatment in an institution for stammerers at 17, achieving a complete cure in six weeks. His military service was as a cavalryman, 1897-1900, after which he had married. There was no excess in alcohol; he was not a smoker. From his own account, he had always been somewhat nervous, had trembled easily, and had fallen to stammering when excited. In 1913 there had occurred, after physical exertion, three violent attacks of fainting, with dizziness, vomiting, and excessive perspiration, each attack lasting from two to three hours. However, from that time to just before the war, he had been free from attacks.
On examination at the Jena Hospital, the patient complained of general weariness, a feeling of pressure in the back[242] of his head, a hammering all over the head, ringing in the right ear, impairment of hearing in this ear, a feeling of dizziness on raising the head, palpitation of heart, especially at night, occasional trembling of the whole body, and absolute inability to walk.
The man was slenderly built, of medium height, in moderate nutrition; pale of face and mucosae; pulse small, regular, and 114. Neurologically, the deep reflexes were generally increased, and the skin reflexes decreased. Percussion on the back of the head elicited marked pain. There were no pressure points. The movements of the arms were free; there was a marked tremor of both hands, more marked on the right. The left grasp was 45, the right, 20, by the dynamometer.
When lying upon his back, the patient could move his legs, but he moved them only slowly and with tremor. The heel-to-knee test was successfully executed despite the tremor; nor could it be demonstrated that there was a genuine ataxia. Placed upon his feet, he would collapse, nor could he be made to walk at all. With trunk supported, he was able to make only a few unsuccessful attempts to drag the feet forward.
Associated with this apparent paralysis, the sensitiveness to touch had entirely ceased in the legs, as well as sensitiveness to pain. The zone of analgesia, however, was more extensive than the anesthesia, spreading upwards three or four cm. farther in front. Ticking of the watch could not be heard even at the meatus of the right ear, although hearing of the left ear was entirely normal; bone transmission on the left side. Whispers could be heard close to the meatus. On speaking, the patient stammered in starting sentences.
He looked extremely anxious during the first few days in the Jena wards, claiming that he could not raise himself. When his trunk was raised, he would let himself sink feebly back into dorsal decubitus. However, when believing himself unobserved, he was found to be able to move himself in bed somewhat quickly. He was able to get a box from beneath the bed, to open the drawer of the night-stand, and to take remarkable care of his moustachios. He complained[243] more and more of headache, though his appetite and sleep were good. He was often irritable.
Treatment at first consisted of cold packs of the legs twice a day, salt-water baths, active and passive exercises of the legs in the position of dorsal decubitus. The patient declaimed against this treatment. There was slight improvement after a week of treatment. He was then able to raise himself in bed, seat himself on the edge of the bed, and stand without support, all the time, however, groaning and moaning. After a few moments, he would fall back on the bed, complaining of violent headache and dizziness. While standing, both legs trembled.
Antityphoid inoculation: Neurasthenia.
A corporal, 39, began to be sleepless and weary, with headache, pains in the back, and dizziness. He was homesick. Upon hospital examination he was very variable in mood, rather hostile in attitude, and at the same time suggestible. He was so confident of being sent home that he anticipated the diagnosis by sending his belongings back to Sicily at the time he was transferred to hospital from his regiment.
After a month’s rest and psychotherapy, the man’s general condition was greatly improved; he was no longer sleepless and had no longer any sign of neurotic disorder. He still maintained that his memory was weak, although in point of fact his memory was very good and quick. He could narrate all the facts about his neurasthenic state. The man’s complaints were out of all proportion to any demonstrable somatic disorder. He was discharged, cured, to be put to work at shoemaking, with the diagnosis, neurasthenia. This neurasthenic state developed after antityphoid injection.
Re the occasional curious effects of antityphoid injection, see Case 65.
Neurasthenia (monosymptomatic: Sympathy with the enemy).
A non-commissioned reserve officer, 26, in civil life a merchant, had a strong hereditary taint, having been also in peace times very nervous and on that account obliged to give up his studies. At the age of 14, he had seen a man fall down from a roof and was much excited about it.
At the beginning of mobilization he suffered a functional aphonia for a few days. He could not let his men shoot at the enemy because of an idea that occurred forcibly to him: that the enemy’s soldiers had wives and children! He felt badly on this account. Later he had a constant taste of blood in his mouth and a smell of corpses in his nose. Toward nightfall all these symptoms would change for the worse, and the symptoms would become especially bad whenever he had anything to do with the wounded. He tended to weep much and was easily frightened and had also various physical symptoms of neurasthenia.
Re the amazing sympathy with the enemy, see Case 229 (Binswanger) and Case 554 (Arinstein), in which chloroform lifted from a German and a Russian consciousness respectively opposite emotional tendencies.
Shell-shock CLAUSTROPHOBIA: Preferred shell exposure to shell-proof tunnel.
A colleague of Steiner, an army physician, 35 years of age, with strong hereditary taint, having two sick sisters (one dementia praecox), had been incapacitated for work through a neurasthenia a few months before mobilization. However, at first he felt very well, marching through Belgium and into Northern France.
On the night of the 17th of October, 1914, a shell struck the house next where he was and startled him up out of sleep. After that, especially at nightfall, upon entering a cellar he would have the feeling of the ceiling falling down, and he would go restlessly from one space to another. Afterwards, any closed room, however secure or distant from the front and free from shells, would give him the feeling of the ceiling about to fall down. He could no longer sit quietly anywhere, but walked about and avoided the company of others.
A characteristic observation is the following as described by the physician himself: There was an absolutely shell-proof tunnel running to the position at the front where he was on duty. It took about 25 minutes to go through the tunnel, but on account of his feelings he could not bring himself to use this tunnel but walked over the exposed hill which was frequently shelled. Curiously enough, after the appearance of the first symptoms, a shell exploded nearby without any marked psychical effect. This happened about noon. The obsessions were stronger in the evening. Objectively, there were neurasthenic symptoms of a bodily nature; there was vasomotor excitability. He was depressed, wept easily, and showed lack of decision; he had tormenting thoughts that he had not fulfilled his duty.
A case of Pathological Lying occurring in a soldier.
No. 27369, a private, attached to the 15th Battalion Durham Light Infantry, was admitted Oct. 14, 1916, to Lord Derby War Hospital from Netley.
September 11, 1916, he had been admitted to Number 3 General Hospital, France, in a noisy, excited, insolent state: said he saw spirits of the dead; heard his sister urging him to lead a better life. Admitted to Netley early in October, 1916: now said he was a spiritualist, a Frenchman, had a quarrel with parents and enlisted in British Army, in army service; went to France August 12, 1914, was wounded at Loos, September, 1915, returned to front in February, 1916, “shell-shocked” June 1, 1916; lost consciousness after this—did not know where he was until July 22, 1916, when he had been arrested as deserter.
Admitted to Lord Derby Hospital October 14, 1916,—quiet, orderly, coöperative: desired to return to his regiment. He now gave a history: Enlisted British Army 1908, went to France, August, 1914, wounded February, 1915, at Neuve Chapelle; recovered; then attached to 45th Durham Light Infantry; blown up July 22, 1916, came to August 5, 1916, in hospital in Boulogne; then back to his regiment—but month later left without leave to pay off old score on a former comrade who had insulted his sister—arrested later by military police; put under observation in 65th Field Ambulance. No deterioration noted, school knowledge fairly well retained; no hallucinations or delusions (maintained he was a spiritualist, also that following shell-shock had suffered from insomnia and seemed to hear sister’s voice). Physically—small, well nourished, effeminate looking.
Oct. 23, 1916, he broke parole, but a month later returned to hospital under arrest. The police reported he had been[248] masquerading as wounded French soldier attached to British army as interpreter; imposed on people; had two leaden types in his possession: “Interpreter R. le Auldere, attached to 1st Division.”
Story in hospital on return:—Born in France, did well in school, entered military academy at Paris. Quarreled with father—ran away to sea. Adopted by a French lady at Pembroke Dock. On account of drunken habits, quarreled again; joined army at Bristol, 1908. Went to France in August, 1914; January, 1915, invalided home because of “trench feet”—discharged as unfit. Reënlisted June, 1915, in Durham Light Infantry. January, 1916, again ordered to France. Blown up on Somme, July, 1916, by shell—remembered nothing until brought to No. 3 General Hospital. He remembers being accused of desertion but sentence was not passed, as he was held by the medical officer to have been irresponsible (as a matter of fact he was, at that time, considered to be a case of dementia praecox.)
Said that during twenty-five days, due to drunkenness, his friends had taken him to Manchester with them; arrested by police as he attempted to get back to hospital. He was now accused of wilfully lying and, confronted with his police record, at first denied it, but later gave following approximately true story:
Born, England, 1890; early life of a roving disposition, good at school, liked books of adventure. Drank early. Ran away at sixteen; was returned home. Ran away again—convicted of drunkenness. Three-year sentence to reformatory in 1910 for stealing: escaped. Rearrested for stealing in 1911: released in 1913, enlisted in army and deserted. Arrested in January, 1914, for stealing; sentenced to three years: released to rejoin army in June, 1915. Arrested as deserter: imprisoned but released in January, 1916; left for France. August, 1916, “shell-shocked,” sent to Field Ambulance No. 3, General Hospital, Netley, and Lord Derby War Hospital. Court-martialed for desertion: nothing came of it on account of medical evidence.
After breaking his hospital parole, he masqueraded in district as “R. le Auldere,” “Le Marchal” and imposed on various persons.
Psychopath almost Bolshevik.
A sergeant, accountant in civil life (father insane, mother pulmonary, grandfather alcoholic, cousin insane; patient himself anemic as a boy, victim of chronic gastritis and gonorrhea), was evacuated from the front to Chateaugiron in March, 1916. It appeared that instead of watching over his men as a sergeant should, he gave utterance to baroque theories of the divine right, the influence of the grace of God on man, and the end of the war. He went so far as to ask leave to transmit to the Inventions Bureau of the War Ministry an invention with respect to the problem of locomotion, and he sent to the King of Belgium a manuscript to the effect that he had received from heaven a mission to reëstablish the world’s balance. He was, in fact, the victim of delusions of a mystical nature with visual hallucinations. To explain his mission, he wrote, “It was my duty to take supreme command of war operations.… I have the power, the right and the duty to give the following order … general armistice … peace will be symbolized by the house undivided and will be constituted by general Christian religious unity … as a consequence of what we shall say they will give up our territory to us of their own accord.”
This case of paranoia apparently took its coloring in part from the war situation itself.
Hysterical mutism: Persistent delusional psychosis.
A sergeant, aged 23, evacuated from the front to a hospital for the insane, had been mute, though not deaf, since February 28, 1915. If asked to cry out he grew black in the face and could utter only a raucous scream which made everyone jump. He wrote very frequently, stating in February that as he was still a sergeant and had no hope of advancement, he cared nothing more for life. “The idea of death got anchored in my head.” In this state of mind, on the afternoon of the 27th two bombs came. “I saw the first one coming and cried out a warning. Coming back I saw the second one. The bombs were coming rather softly. From this moment on and up to the time when they burst, I thought I had gone, that I had been carried off and crushed. I was quite astounded at finding myself covered with earth and stones … but I could not talk any more, I could just say in a low voice ‘Papa,’ and the next day in an ambulance I could not talk at all.”
There was complete pharyngeal anesthesia. The man had been a foundling and was clearly a degenerate. He had always been of a depressed disposition and given to thoughts about his misfortunes. Over and above the mutism gradually ideas of persecution and revindication developed (such as that he merited adjutant’s rank and was being mocked and treated as a simulator). He drew up a long letter to the War Ministry in which he stated his desire to be sent back to the front. He complained to the police about a hospital sergeant and offered a duel in an elaborate and inflammatory style, “with whatever weapons shall please you, either sabre of 1845, revolver of 1902 or bayonet of 1886 or the chassepot. One of us two must disappear.” He had become dangerous enough to be interned and in hospital remained mute with the same ideas of persecution and revindication, the same alternate phases of calmness and excitation. According to Dumesnil: hysterical mutism with persecutory delusional psychosis.
A peasant’s psychopathic inferiority brought out by the war.
An Italian peasant began to feel sick on being called to arms. Antebellum he had been an even-tempered, good-natured man, according to his own story, satisfied even with stale food, and always enjoying his sleep. He had been in the war about a month, doing construction work, sentry duty, and chores. Though he lived in the trenches under damp conditions, there had really not been much excessive war strain. He shortly developed migraine and war-weariness, as well as middle-ear disease.
A number of times he heard shooting nearby, and was subject in his sentry duty to a good deal of anxiety and painful associations. On sentry duty he had digestive disorder, vomited, and became intolerably weary; in point of fact, a fever, regarded as malarial, then developed, together with diarrhea.
Upon hospital observation, he was found fatigued, given to terrible dreams, tremulous in the fingers, with skin reflexes a little excessive, and the Moebius phenomenon. The thyroid was somewhat swollen. The pulse stood at 80. The Mannkopf sign was well marked, as well as that of Thomayer (80-120), and Erben (120-87). The oculocardiac reflex was prominent.
Psychopathic episodes.
A Neapolitan, 26 (neuropathic stock: mother epileptic, brother psychopathic; patient had previous criminal record; married and then appeared to behave himself for several years; had always been excitable and of violent temper), after but one severe day in the trenches, woke and found his night clothes soaked in urine. Another time, his comrade had awakened him because he was gnashing his teeth in his sleep. Again, his grief became very violent at learning of his wife’s infidelity, and during the night he bit his finger. He thereafter suffered from severe headaches, dizziness and vertigo though without falling. He was granted a furlough, but the condition was aggravated on account of his wife’s abandonment of him, and one day, finding her with her lover, he threw himself at them, wounding her severely in the face: he did not remember this impulse later. Many hours later, on awakening in prison with his wounded hand, he recalled the entire episode. He showed a confused and excited condition, which, however, quickly diminished. He became lucid and tranquil, though easily aroused. He cried at the thought of his daughter, whom he wanted to save. Insomnia, instability of reaction, habitual migraine, and dizziness. Tremors of the fingers and of the eyelids. Exaggerated reflexes. Very striking cutaneous analgesia.
Maniacal and hysterical delinquent.
An Italian soldier, 25, a foundling, was always off and on in a military prison. At a tavern one night the man unsheathed his sword and threw three bottles at the host. Bystanders overpowered him and carried him to the local police station. Handcuffs were put on to stop the mania. His pupils were dilated and he was sweating profusely. Alcohol could absolutely be excluded from the history of this incident.
Observed in clinic, the patient was rather silent, but on the whole normal and without delusions or hallucinations. It seems that he had committed a number of crimes in the army that were always excused on account of his mental state. He had been strongly alcoholic, although not at the time of the incident mentioned. He was covered with tattooings of an obscene and violent nature.
He showed pharyngeal and conjunctival anesthesia and concentric limitation of the visual fields of unusual degree, and a remarkable hypalgesia. The knee-jerks were lively. The man was, in point of fact, sent back to military service, with, however, the suggestion of reform school.
Psychopathic delinquent.
An Italian, 20 (family history negative), was described by officers as of an odd disposition, at times thoughtful and again chattering and presumptuous, and often very vulgar in talk and manner. He had tried several trades, with little success.
While in the army he discharged his gun three times, claiming to have heard noises in a nearby field. On account of the inopportune repeated discharges, he was condemned to the barracks for ten days. The following day, instead of returning to the barracks, he abandoned his musket, cartridge box and uniform, and, returning to town, left for Leghorn. Being sent to prison, he began to scream that he was thirsty. He tore his jacket into strips with his teeth, and making a noose of it, attempted to hang himself.
On being transferred to the military hospital, he was often very restless, screaming and making a great uproar. On being questioned, he answered indifferently and had a vacant stare. During his stay at the clinic, patient was always quiet. Once, however, he had a spell of intense psycho-motor agitation, brought on without any known cause and followed by a short period of bewilderment, lasting altogether half an hour.
Patient had insomnia and his visual fields showed concentric contraction for white. He was sent to a military convalescent hospital.
Psychopathic excitement.
An Italian soldier, 22 (father and brother both committed to insane asylums), since his enlistment had been conducting himself strangely, being impulsive, undisciplined and unbalanced. He had been in Libia from January to August, 1913, and was returned to Italy on account of persistent severe headaches. A month later he was returned to a regiment in camp.
September 23, 1914, the patient, who had been reproved by a superior officer to whom he had given a disrespectful answer, began to be excitable. He was calm during the day, but acted in a sullen and gloomy way and kept entirely to himself, avoiding even his most intimate friends. When, however, he suddenly recalled his punishment of the morning, he began to race around the yard and finally threw himself upon the ground, remaining there in a cowering and squatting position. At the beginning of the attack he was possessed of a paroxysm of fury, which made a great impression upon those present: eyes agape, face swollen and distorted. He resisted being transferred to the hospital and a furious struggle followed. He tried to bite and scratch everyone. It required ten persons to carry him by his hands and feet safely to the hospital, where he arrived in a state of great excitement and rage.
At the clinic, during the period of observation, he was always tranquil, rather silent, gloomy, somewhat hostile; said he did not remember why he was brought there. Often he was not able to sleep, especially during the first few days of his stay. Has had painful headaches and feeling of dizziness. Several times he showed a tendency to be untruthful. Bodily examination revealed the absence of conjunctival and pharyngeal reflexes. W. R. of serum was negative.
Patient was sent to an interior hospital for convalescence.
Desertion: Dromomania.
An Italian private, 19, came up for desertion in the face of the enemy. He had had a good record during a year of military service and his army conduct in the war was regarded as very good.
He felt sad and preoccupied for a number of days, but all of a sudden “some indomitable force” thrust the idea into him to go out into the country a distance of some 20 kilometers from the front, with the definite object of praying in a certain church. It seems that this same impulse had occurred to him several times before but not so forcibly. These prayers were to be said in memory of some sad events in his life.
Upon examination he was found in a sad and self-accusatory state, much discouraged with ideas of his guilt, unworthiness, and ruin. He had a variety of gloomy fears and obsessions, all of which contributed to the dromomania that culminated in desertion.
As to his previous history, he had had a depressive psychosis two years before, but the delusions at that time were of persecution. He had also suffered from typhoid fever a few weeks thereafter.
Suppressed homosexuality.
A man, 32 years, of high intellectual attainments and unblemished moral character—a teacher—enlisted as a private. He apparently found his associates in camp very uncongenial and undesirable. He grew physically tired, then mentally tired and unable to concentrate attention. He began to neglect his uniform, could not keep his equipment in order, became introspective and depressed. The drums he heard seemed to point to his funeral. There was but one thing to do in his opinion: that was to humiliate himself by committing sodomy. He thought of committing suicide.
Upon discharge from military duty, he began to show improvement. Smith regards this case as one of suppressed homosexuality.
Of the cases in which change or excessive work is the precipitating cause, four out of six of Smith’s cases were men.
Re homosexuality in the Italian army, Lattes has made a special study. The effeminate homosexual is decidedly unfit for the army, being unable to stand the war stress. Homosexuals diminish army morale. The cases of functional effeminacy with normal physique are likewise unfortunate for the morale of active units, though they may be employed in garrison duty and office work. The medical decision in these cases may prove difficult unless a broad interpretation of the concept “psychopathic” is allowed to prevail.
Psychopathic: suicidal, then self-mutilative.
An English soldier as a child had night terrors and fear of the dark; as a youth wanted to throw himself down from heights; took delight in seeing animals killed; was shy with both sexes; was never able to run great distances; was taken from school at the age of fifteen for weakness, and had always been subject to headaches, somewhat improved by lenses.
During training sharp pains appeared in the left groin that grew better when the man lay down. These pains were regarded as hysterical. Thereafter began shortness of breath, pain above the heart, with palpitations and occasional attacks of dizziness. After a short sick leave he insisted upon going to the front, though his superior officer thought it unwise, and, after a period of seventeen months training, was finally sent to France in September, 1916.
He was at first somewhat afraid of shells and, though he soon got used to the shells, the horror of the war grew on him, with pity for the Germans as much as for the British. He became depressed over his weakness and when his commanding officer committed suicide got obsessed with the idea of committing suicide himself. He went so far as to drive a knife into his upper lip and to smash a looking-glass to avoid seeing himself. After a long spell of trench duty he had to be sent home incapacitated.
In hospital in England he was depressed and suicidal. He began to want to mutilate himself, yet found that a slight pain and the drawing of blood was all that he really craved. Of course, he had been a failure, but now he rationalized the failure by a comfortable conviction that he should never have been sent to the front. He complained of memory and attention disorder, insisted that he was physically incapable of outdoor exercise, complained of headache if he stayed indoors. He said he wanted to go back to the front; knew, however, that he could not, and even refused to consider the possibility of getting well to work at home. At the time of report he argued there was nothing left but suicide.
Bombardment: Psychasthenia?
A twenty-year old engineering student of high grade and without hereditary taint, a scientific and non-introspective man of a brilliant and gay disposition, not very religious, without special sexual abnormality, was mobilized in class 1914, was put into the artillery, and was soon appointed maréchal des logis. He left for the front April, 1915, yet had to be evacuated in November. One afternoon, at the end of a bombardment, he rose from a recumbent attitude and immediately felt a dreamy, bizarre feeling, as if a fog lay between him and his surroundings. Next day, after a good night, he woke in the same state. Everything was bizarre and novel despite the fact that he recognized men and things. A physician ordered rest and after a few days evacuated him.
He was cared for in various hospitals, but the psychasthenia increased. He felt a terrible and causeless anguish, with precordial constriction. He felt as if he were about to be executed. His fears appeared after seeing some turning object, such as a wheel or a cane twirling. Gradually this fear was transformed into a genital excitation, though lascivious pictures did not excite him. Seeing anything turning gave him a voluptuous feeling in proportion to the speed of the rotation. It seems that all sexual interest had been at a standstill for several months in the early part of his disease, when suddenly this new aberration appeared. It seems that a portion of the man’s work in the artillery caused him to use screws and cogwheels every day. Attacks of vertigo occurred, with the appearance of an infinity of small, colorless spheres turning over one another, the whole forming a sort of animated system of rotation. In the night this system was luminous and somewhat like what one feels on compressing the globes of the eye. There was a retraction of the visual field. The man would be found in the dream state, especially after waking in the morning or when some novel kind of act was being performed. He[260] got somewhat better and did not wish to go on leave, because he feared the recurrence of these psychasthenic paroxysms. However, he took a leave July 14th. In the first part of his journey he had some vertigo and some of the voluptuous sensations, but in the next two days he was much better. He returned to hospital without trouble.
The authors somewhat doubtfully term this case one of a quiet psychasthenia, but in discussion still further talk arose as to the diagnosis.
Re psychasthenics, Lépine notes that the lack of any out-standing symptoms in many psychasthenics allows them to stay in the army longer than would epileptics or hysterics of the same degree of disease. The line officers tend to consider them exaggerators or simulators. The fact that they besiege the line officers and the physicians with their troubles may add to the impression of falsification. The basis of the psychasthenia is often also, genuinely enough, a fear. Lépine divides the military cases into anxiety neuroses and hypochondrias. The anxiety cases are hypotensive and given to tachycardia. They have very labile vasomotors. When it comes to the necessary exclusion of malingering, it is the history, with its hereditary and collateral taint, that tells the tale. A history in the patient himself of alcoholism, typhoid fever, syphilis, or especially cranial trauma may play a part. An agoraphobic may actually be in general a courageous man except for his crises of anxiety about open spaces.
As to the hypochondriacs, fear of syphilis must be noted. Akin to the syphilophobics are a group of pseudo genitourinary cases that fear effects of an old gonorrhoea. See Case 195 (Colin and Lautier) below.
Gonorrhoea: NOSOPHOBIA, depression, suicidal attempt. Recovery, thirteen months.
A munition worker came to Villejuif, December 6, 1915, with cord marks on his neck and conjunctival ecchymoses. He had tried to hang himself.
Non-alcoholic, he had, however, long since shown signs of imbalance; his father had died insane, in an institution. When the man came in, he wept and groaned and made vague complaints of having contracted a venereal disease, insisting that his genital organs were purple.
After a few days, he grew less anxious and told how he was married and how his wife had made life a hell for him, giving herself up to drink and becoming a sloven; how several months since he had contracted gonorrhoea; how though told that the condition was cured, he had found filaments in the urine and had tried a variety of drugs, spending most of his money; how he found more and more filaments, thought himself incurable and unable to live with his wife; how at last, desperate, he had tried to hang himself.
He got well quickly, though his convalescence was interrupted by several periods of depression a few days in duration, with anxiety and tears. February, 1916, he was discharged well.
He returned four months later; he was still occupied with his disease, still going to physicians and buying drugs. It took six months more before the man could be discharged from the service, at the end of 1916.
This man appears to be a hereditarily predisposed subject, who simply affixed his delusional ideas to a disease which had begun some time before the mental trouble itself. The family plight is important and practically constant in this group of cases. The fear lest the disease shall be revealed by the physician to the family is deep-grounded and impossible to overcome by mere statements concerning professional secrecy. The impulse to suicide is extraordinarily keen.
A soldier (neuropathic taint) after hardships for two days stumbles over a corpse; unconsciousness: Stupor; episodes of fright with war hallucinations; look of premature old age; paresis; anesthesia.
An Italian soldier (a shoemaker with an epileptic mother and two nervous brothers; himself always irritable and for long periods melancholic; at 15 condemned to nine years in prison for homicide in a quarrel) took part in a number of attacks at the beginning of the war. His company was heavily engaged in October, 1915, and there was no sleep two nights, and only a bit of cold food. He was dazed.
October 24, the company had to advance at night in the rain and under a heavy rifle fire. The shoemaker stumbled over a corpse, fell, and lost consciousness for a time that he thought was very long. He woke up in a camp hospital, remembering all the experiences he had undergone up to the time of losing consciousness. He now fell into a state of torpor, occasionally jumping out of bed and shouting with fear, hurling himself at non-existent persons, assuming a position of defence, and suddenly awaking in anxiety.
October 29, he was transferred to a second hospital, and October 30, in a third hospital, was examined and found well and strongly built, but looking prematurely old. He was inactive, depressed, and stuporous looking. He fell to weeping often and rarely gave any answer to questions. Sometimes he refused food. There was a slight paresis of the left arm, and the left pupil was smaller than the right; both pupils reacted poorly to light. The larynx and cornea did not respond to stimulation. Skin reflexes were poor, and the plantar reflex lacking. The left side about the shoulder and hip showed large patches of anesthesia to touch, pain and heat; but deep sensibility was present in these areas. He slept well at night. Status unchanged for two weeks. He was experimentally sent to the guardhouse, but was soon back in hospital with the same symptoms as ever.
Bombardment; shell explosion nearby: Mania; death in 24 hours. The AUTOPSY showed superficial punctate hemorrhages of brain and congestion of pia mater. CAUSE OF DEATH—small bulbar hemorrhage, congestion of veins, and nerve-cell changes of a local and differential nature (chromatolysis of vago-accessorius nucleus). SHELL-SHOCK SYMPTOMS due to capillary anemia and chromatolysis of various regions.
A soldier became rather nervous at the Somme, and later underwent intense bombardment for some four hours, February 22, 4 to 8 P.M. Although he said he “could not stand it much longer” he carried on for twelve hours more when perhaps six shells went over, February 23. One of the shells burst about ten feet away, just behind the dugout. The first day of the bombardment he was tremulous and depressed; later coarsely tremulous in the limbs. February 23 there was crying and inability to walk or do any sort of work. Questions were not answered. The pupils were dilated. The evening of February 23 the man was admitted to the field ambulance in acute mania, shouting: “Keep them back! Keep them back!” He was quieted with morphine and chloroform and slept well during the night. There were at least two hypodermic injections of morphine in the ambulance. He woke up the morning of February 24 apparently well, but suddenly died.
The autopsy showed small scratches on the anterior chest wall, but otherwise no sign of external violence. Both lungs were edematous; the left lower lobe showed a considerable hemorrhage. The heart was enlarged and the right side dilated. The liver was somewhat congested. The kidneys were small, but otherwise showed no gross change (urine without sugar or albumin).
After Vincent and others
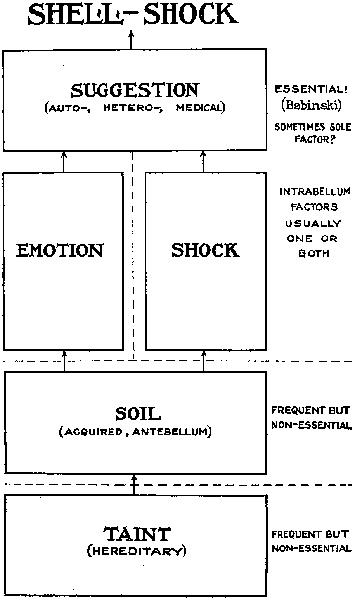
The scalp showed a slight frontal bruise. The brain was extremely congested. On each side of every superficial vessel there was an ecchymosis. A number of minute punctate hemorrhages was found on the surface of the brain in connection with very small vessels. The brain substance was soft, but not markedly edematous. The cerebrospinal fluid was tinged with blood. On each side of the great sinuses of the skull there was considerable ecchymosis. This examination was made by Capt. A. Stokes, R.A.M.C., in the mobile laboratory. There were no areas of large hemorrhage anywhere in the brain substance and no smaller petechiae, except the superficial ones above noted.
Microscopically Mott confirmed the pial congestion and macroscopic subpial hemorrhages described in the gross. He found besides congestion also actual hemorrhage in the vascular sheaths of the corpus callosum, internal capsule, pons and bulb. Now and then blood corpuscles were found extravasated into the nervous tissue.
The microscopic examination showed a generalized early chromatolysis in the nerve cells of varying intensity, especially affecting the small cells. The Nissl granules of the larger cells were also somewhat abnormal, being smaller and packed rather loosely together.
The small cells of the bulb and pons were slightly swollen and their nuclei large and clear. As to the larger cells of the bulb and pons, there was less evidence of this swelling and nuclear change.
According to Mott, this chromatolysis may perhaps be regarded as a sign of loss of biochemical neuropotential. The chromatolysis indicates a relative degree of exhaustion of the kinetoplasm. Mott assumes that the cells of this victim of shell-shock are in a state of beginning nervous exhaustion. He remarks that the cells of the vago-accessorius nucleus show more signs of this nervous exhaustion than others. With respect to cerebellar findings Mott remarks that the changes found are very similar to those described by Crile in the case of an exhausted and wounded soldier. Mott correlates the mania shown on the evening of February 23 with the venous congestion of the cortex, the small subpial hemorrhages and evidence of scattered arterio-capillary collapse.
Punctate hæmorrhages in corpus callosum from a case of shell-shock and burial; very probably accompanied by gas poisoning while lying unconscious and buried. Observe the small white area in the centre of the hæmorrhage, in the middle of which is a small vessel which, under a higher magnification, will be seen to contain a hyaline thrombus. (× 20.)

Hyaline thrombus of vessel in centre of a punctate hæmorrhage. The thrombus was stained brown by dissolved pigment. Around the blocked vessel is a white area of brown substance containing numbers of leucocytes; outside this is the hæmorrhage, not very distinctly seen. The specimen was prepared from the subcortical white matter of the frontal lobe. (× 345.)

Leash of small perforating optostriate arteries filled with pigment granules. Two of the arterioles show miliary aneurisms. (× 350.)

Three punctate hæmorrhages showing optostriate arterioles filled with pigment granules. (× 30.)
NOTE THAT THE CHANGES IN CELLS OF FIG. 3 ARE DIFFERENTIAL FOR NUCLEUS AMBIGUUS: CELLS NEARBY PROVED NORMAL
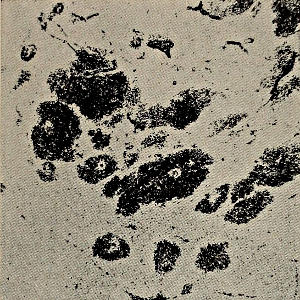
Fig. 1.—Photomicrograph of section of corpus callosum from case of shell-shock showing the capillary punctate hæmorrhages. In several a small white area is seen of brain tissue in the centre of which is a small artery or vein. (Magnification 20 diameters.)
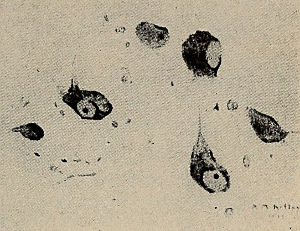
Fig. 2.—Section of medulla oblongata from case of gas poisoning, stained by Nissl method, showing the swollen cells of the nucleus ambiguus. Observe the enlarged, clear, eccentric nucleus; the surrounding cytoplasm shows an absence of Nissl granules. In not a single cell is the nucleus seen in the centre as it should be. (Magnification 450.)
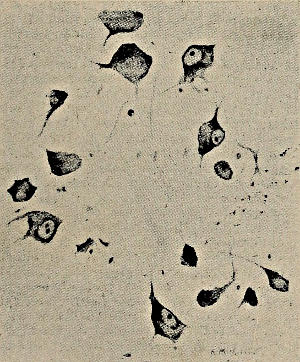
Fig. 3.—Section of medulla oblongata from case of shell-shock with burial, stained by Nissl method, showing the swollen cells of the nucleus ambiguus. Observe the enlarged, clear, eccentric nucleus; the surrounding cytoplasm shows an absence of Nissl granules. In not a single cell is the nucleus seen in the centre as it should be. (Magnification 450.)

Fig. 4.—Section of third cervical segment of spinal cord from case of concussion, stained by Nissl method, showing the medium group of anterior horn cells corresponding to the nucleus diaphragmaticus. They show certain amount of perinuclear chromatolysis. But all the cells exhibit the Nissl granules. Even at the seat of concussion, the fourth segment, an external group of cells remains showing Nissl granules. Concussion therefore does not destroy the Nissl granules. Probably the cells of the nucleus diaphragmaticus show a certain amount of chromatolysis because they were continually discharging impulses along the phrenic nerves, and the few cells that were left of the nucleus had therefore much more work to do. (Magnification 300.)
Mott suggests that the sudden death of the case may be due to a hemorrhage into a sheath of a fair-sized vessel in the median raphe of the bulb; the general venous congestion; and the almost complete chromatolysis of the vago-accessorius nucleus (adjacent hypoglossal nucleus normal).
According to Mott, also, many Shell-shock symptoms, e.g., headache, giddiness, amnesia (anterograde and retrograde), dizzy feelings, lack of power of attention, and fatigue, stupor, inertia, mental confusion, terrifying dreams, are to be explained on the basis of capillary anemia and chromatolytic changes.
Mine explosion. Ecchymoses; no bone or visceral consequences seen at AUTOPSY (third day after explosion) except SUBDURAL HEMORRHAGE and PUNCTATE HEMORRHAGES OF BRAIN.
A sergeant in a Chasseur Battalion was in a mine explosion and entered hospital June 19, 1915, so agitated that he had to be tied to the stretcher during transfer from the railway. There were remains of epistaxis and blood in the right ear, not proved to be due to otorrhagia; blue-black ecchymoses of both eyelids; and small ecchymoses of the bulbar conjunctiva of the right eye. No other sign of trauma or fracture. The explosion had probably taken place on June 17 or 18. Patient was but semiconscious and irresponsive; rolled upon the mattress, beating the air with arms and legs, assuming fighting postures and uttering cries. Urinary incontinence. No fever.
There was doubt as to the diagnosis, which lay between fracture and concussion. The persistent agitation and oniric delirium pointed rather to concussion. Without further sign, however, the patient died on the night of June 20.
The autopsy was extremely careful and showed no sign of cranial fracture of vault or base. The cerebrospinal fluid was strongly bloodstained. The inner surface of the dura mater had a thin sheet of hemorrhage, hardly 1 mm. thick, covering both hemispheres and the cerebellum and spreading over the bulb. There was no distension of the lateral ventricles. Serial sections of the brain showed no lesions of the substance, except for slight hemorrhagic points.
According to Chavigny, so slight a meningeal hemorrhage is incapable of producing a mechanical disturbance of the brain and the cause of death could not be said to be meningeal hemorrhage. Massive multiple gas embolism through sudden decompression is not a suitable explanation of a case with death delayed, as in this instance, even if Arnoux’s explanation is suitable for cases of immediate death.
Mine explosion: no skin, bone, or visceral consequences seen at AUTOPSY (death in seven days) except slight LOCALIZED MENINGEAL HEMORRHAGE.
A soldier entered Val-de-Grâce February 27, 1915, in a state of confusion following mine explosion the night before. He was delirious, thought himself on leave, and had spells of excitement. Lumbar puncture, February 29, showed a slightly darkened fluid, with approximately normal amount of albumin, one or two lymphocytes and rare red blood cells.
A brief period of slight improvement followed, but the restlessness and delirium increased once more, became particularly severe March 3, and the patient died on the night of the third, seven days after the explosion.
The autopsy showed slightly congested lungs; no other lesion except a sharply defined hemorrhage in the cervical spinal meninges and over the meninges of the temporal and occipital lobes. Microscopic section of the brain failed to show any hemorrhages within the brain substance.
Here is a case of death following explosion without external wound. The meningeal hemorrhages are hardly enough to explain the death. The explanation of the death must probably be made after histological examination.
Concussion of spinal cord from shell burst—WITHOUT spinal fracture, WITHOUT penetration of splinters of shell or bone into canal or cord substance: Microscopic demonstration of intraspinal AREAS OF SOFTENING with classical secondary degenerations. Such a case forms a link in the argument that serious lesions of the nervous system may develop as a result of VIOLENCE directly TRANSMITTED through investing tissues EN BLOC.
A man, 23, was struck in the left thorax and shoulder, in both thighs and the neck, by fragments from a bursting shell March 27, 1915. One fragment was imbedded near the vertebral column.
Twenty days later there was an absolute, flaccid paraplegia, yet the legs occasionally gave spontaneous, jerky movements. Tactile anesthesia reached the fourth dorsal root-level, except that the perineoscrotal region and the penis were somewhat sensitive. There was anesthesia to pain and heat, as well as in bones and joints, along with the tactile anesthesia. There was a hyperesthetic region on the right side, corresponding with the distribution of the fourth dorsal root. All the cutaneous reflexes up to the abdominals were gone; but defense reflexes could be brought out in foot and leg by skin, bone or joint stimulation. The deep reflexes of the legs were also lost, whereas those of the arms were increased. Retention of urine without incontinence; no retention of feces. Sacral, trochanteric and heel decubitus had developed in the course of the three weeks following injury. A lymphangitis ran all the way up the right thigh from one of the sores, with a corresponding hyperpyrexia.
Surgical intervention was indicated from the evidence of spinal compression at a definite level, but the lymphangitis grew worse. Oniric delirium, and finally a stuporous state, set in, with death May 6, forty days after the wound, a death[273] due to septicemia, without special alteration in the paraplegia itself or in the sensory and reflex situation.
At autopsy the spine and dura mater proved normal; but microscopically serial sections through the fourth and fifth dorsal segments showed softening of the right anterior horn and posterior columns, with cavitation in the radicular zones, and the white matter of the fifth dorsal segment was in a state of acute degeneration. There were also ependymal changes, namely, at the fifth dorsal level a dilatation with deposit of albumin; in the lumbar region, breakage of the ependymal wall, with cellular gliosis. The dilated ependyma was surrounded by an area of fibrillary gliosis which had proliferated in the form of a septum in the interior of the canal. (According to Claude and Lhermitte, these data concerning hydromyelia, which they regard as secondary to trauma, are an argument in favor of the traumatic origin of certain syringomyelias. They regard the breakage of the ependymal wall as due to hypertension of the spinal fluid due to mechanical lesions.) Their interpretation of such acute degeneration as was found in the fifth segment is that this degeneration, as well as that of the posterior roots, is due to the direct impact of the cerebrospinal fluid upon the cord structure. As for the softenings with cavitation, they regard them as surely due to spinal concussion and as very possibly due to an ischemic necrosis, suggesting that older work by Duret and Michel on concussion of the brain indicates the possibility of a temporary ischemia of the spinal cord from the violent impact of the spinal fluid upon the cord due to shock of the spinal column. The transient hypertension of the spinal fluid might well induce, they believe, a vascular spasm with anemia, to which the gray matter is well known to be especially sensitive. In the present case, a period of somewhat less than six weeks had sufficed to produce secondary degenerations above and below the fifth dorsal segment, of a quite classical sort.
Accordingly, we here deal with a severe form of spinal concussion due to a shellburst, in which intraspinal lesions were produced without spinal fracture or penetration either of bone or of shell fragments into the spinal cord or the spinal fluid.
Shell explosion (1 meter distant) kills a soldier by bursting both lungs within the intact thoracic cage.
A man of the 26th Regiment of Infantry was brought October 26, 1914, to Ambulance No. 6 of the Twentieth Army Corps at the Chateau d’Henu. Weakly and jerkily the man was able to tell how, as he was going forward, a large calibre shell fell less than a meter in front of him and exploded. He fell back and lost consciousness, was picked up in the evening and carried to the relief post and then to the ambulance, where he arrived ten hours after the fall. There were signs of a considerable shakeup, with pale and anxious face, nose pinched, hollow eyes, rapid superficial respiration, small pulse, 120, and a feeble voice. There were small skin wounds of the right arm, a finger, and ear, but there was otherwise no wound. The thorax and abdomen were somewhat painful all over, but there was no especial point of pain. The chest showed a slight dulness at the bases. Examination of the abdomen produced defensive movements and the man vomited blood during examination. He was put on his back, kept warm, given artificial serum, hypodermic injections of camphorated oil and caffeine, and carefully watched. In the night he had another bloody vomiting, his pulse became smaller and smaller, dyspnea became more and more intense, and he died late in the night.
The autopsy showed that the abdomen was free of lesions and that all the organs were of a normal appearance and color. There was no sign of perforation or of peritonitis. The stomach itself was filled with blood and there was a generalized ecchymotic appearance of the mucosa, with small, submucous hematomata and a number of tears in the pyloric portion.
The pleurae were found filled with blood, almost a quart in each cavity. The right lung showed a large tear at the level of the middle lobe, 15 cm. long. An orange-size, black bit of lung protruded through the tear. There was no sign of rib fracture opposite this tear, and no subpleural, intercostal[275] or subcutaneous contusion. The thorax wall was perfectly normal.
The left lung showed, in the middle portion of the upper lobe, a somewhat analogous pleural tear, almost as big as that on the right, with another large hernia of black lung. Bits of the herniated lung sank in water. The thorax wall was intact. The pericardium was free from blood. There was nothing else abnormal about the body.
Re effects of an explosion upon structures with intervening objects left intact, Fauntleroy notes that a shell bursting three yards from an aneroid barometer may force its levers into an abnormal position. A further fact will indicate how permanent is the physical state into which the levers are forced; for when the barometer with its levers placed right was placed under a bell-jar and the pressure therein was reduced to 410 mm., the levers resumed the position into which the explosion of the big shell had thrown them.
Re windage and internal effects in the human body, Ravaut recalls the fact that the internal and intraneural hemorrhages of Caisson disease (“bends”) are well known. The external hemorrhages of aeronauts and mountain climbers belong in the same physical class. Dynamite exploded in a pond kills fish. Dynamite may break pillars inside a building without damaging its front. Cases like Chavigny’s (198), Roussy and Boisseau’s (199), Claude and Lhermitte’s (200), as well as Ravaut’s own case (202) are in point.
Shell explosion near by: Paraplegia, interpreted as due to windage. Two foci of HEMORRHAGE (SPINAL CANAL, BLADDER) clinically proved to exist in a case without external sign of injury.
An infantry sergeant was brought to the ambulance, one day in November, 1914, with a paralysis which had set in immediately upon the explosion of a large shell a short distance away. Both legs were paralyzed and there was anesthesia to the navel. He could not urinate. It was early in the war, and Ravaut thought he would find an injury to the vertebral column, but on undressing the soldier there was no wound. The skin was intact, and there was not even an ecchymosis. The patient was suffering not at all, but said that after the shell exploded he felt a forcible shock, was stunned for a moment, and when he wanted to rise, found that his legs were inert. His state did not change during the day and he did not urinate. Catheterization showed a urine full of blood. This indicated a lumbar puncture, and a bloody fluid emerged under great pressure. Thus two foci of hemorrhage were proven to exist in this patient despite the fact that there was no external lesion.
Re windage effects, see suggestions of Ravaut under Case 201. Ravaut also suggests that certain cases of emotional jaundice may be similarly explained on the basis of internal lesion due to windage. Sundry cases of gastro-intestinal disorder and of hemoptysis fall into the same class; possibly the cases of death in a fixed posture belong there, too. Ravaut thinks, despite the look of hysteria about the shell-shock cases of paraplegia, deafness, mutism, and the like, that the cases are actually ones in which there has been at the beginning a slight or severe hemorrhage, clearing up in a few days. He states that there is a pretty definite parallelism between the course of the clinical symptoms and the chemical characteristics of the spinal fluid.
Shell-explosion in confined space; paraplegia after fifteen minutes; slight hemorrhage and LYMPHOCYTOSIS of spinal fluid; Hematomyelia.
A Sergeant lying down in a small dugout space, 2 × 1 m. high, had a 77 shell burst behind his head and between his head and the back of the dugout. The patient was not moved by the explosion, but was buried in a small amount of earth and stones to a depth of about 20 cm. He was not wounded and showed no ecchymoses either then or later. Aided by stretcher bearers, he was able to walk to the relief post about 400 meters from the trench. He did not lose consciousness, and got to the relief post about a quarter of an hour after the shell burst. Thereafter, however, he was unable to move his legs. The accident happened February 6 at 4 o’clock. He was examined 24 hours after the trauma. The accompanying diagrams show the variations in sensory disorder at intervals during six months.
A lumbar puncture, February 8, 1915, showed hypertensive clear fluid without macroscopic clot on centrifuging, but showing a number of red blood cells and lymphocytes—3 or 4 to the microscopic field. There was a slight hyperalbuminosis. The development of the muscular atrophy and hypo-excitability of the left lower extremity, the exaggeration of the left knee-jerk, together with the spinal fluid appearances, seemed to prove the organic nature of the paraplegia. There was an intense rhachialgia, with radiation along the sciatic nerve. This outlasted all other symptoms. Thermo-analgesia was the most prominent sensory disorder. There were no sphincter disorders.
During the first days, the anesthesia was of a pure segmentary type, with nothing about it to suggest that it was later to be supplanted by a radicular type of disorder. Hematomyelia was, years ago, thought—according to Froment—to tend to yield sensory disorders of a segmentary nature. At the outset this anesthesia was total, though there was a[278] vague, poorly localized feeling on intense painful excitations,—as with energetic pricking or burning. Thus the protopathic sensibility of Head had remained, whereas the epicritic sensibility had disappeared.
Detailed examination of this case showed extreme errors in the position sense. For example, pricking the foot might be localized as pinching above the knee. The cremaster reflex was extremely marked and would appear upon even slight excitation of any part of the lower extremity, even at times when the patient declared he felt nothing. These phenomena at the beginning early gave place to a syringomyelic type of anesthesia.
At the time of report, July 29, 1915, Froment regarded this case as analogous to hematomyelias of divers, although there is not such a degree of decompression; the suddenness of the decompression is more marked in these Shell-shock cases than in divers.
Shell explosion; bowled over; loss of consciousness: Hemiplegia with reflex signs thought to be organic; hypertensive spinal fluid; LYMPHOCYTOSIS.
A corporal in the engineers was going the night of June 7th to a creneau of mitrailleuses, when he was bowled over by a bursting shell. He lost consciousness and was carried to the cantonment by his comrades. Next morning he complained of headache and pain in the back; had a convulsion; and proved on examination to have a left-sided hemiplegia. He was given the diagnosis of hysterical hemiplegia.
He was sent to the 6th Army neurological center, and there showed a complete left-sided hemiplegia with tendency to contracture. The left knee-jerk and arm reflexes were exaggerated, and there was ankle and patella clonus with Babinski sign. There was a dysesthesia on the left side, with wrong interpretation and poor localization of painful stimuli, and non-recognition of cold and heat sensations. Muscle sense and stereognosis were impaired. There was a slight dysarthria. Lumbar puncture yielded a clear hypertensive fluid with a slight lymphocytosis.
The situation remained without change for a month, when the patient was evacuated to the rear. Thus, a shell-burst can produce destructive nerve lesions without evidence of external injury.
Re hypertensive spinal fluid, Sollier and Chartier cite Dejerine as having brought the proof of hypertension in the cerebrospinal fluid in Shell-shock cases. They also believe that the Shell-shock hysteria is built up on a physical basis, more or less after the model of Charcot’s hysterotraumatism. Shock, windage, and gas may bring about the same kind of result. They rely especially on the cases of Sencert (201) and Ravaut (202) for their argument (1915). They recall the fact that Charcot found a hysteria due to lightning stroke and to high tension electric accidents. They quote Lermoyez as attributing like results in ear cases to labyrinthine shock, tympanic rupture, and ear hemorrhages.
Shell-shock: Hemiparesis, amnesia. Lumbar punctures early (but here as late as one month after shock and after disappearance of hemiparesis) showed PLEOCYTOSIS and hyperalbuminosis.
A French sergeant, a machine gunner, was the victim of shell-burst September 25, 1915, was evacuated with a diagnosis of commotio cerebri, and, when examined at Paul-Brousse October 5, showed a right-sided hemiparesis, clouding of consciousness and somnolence, the hemiparesis involving the face, with deviation of tongue to right, Babinski reflex right, cremasteric and abdominal reflexes abolished on right. Normal respiration and pulse.
Lumbar puncture October 7, that is, thirteen days after the injury, yielded a clear fluid with an excess of albumin, 144 small lymphocytes (some degenerate) and a single endothelial cell.
October 12, the knee-jerk was a little less lively on the right side. The plantar reflex varied between extension and flexion on the right side. The cremasteric reflex had been weakly regained on the right side.
The patient was now less stupid and could tell how he jumped when the shell burst, and how he had been in the air ten minutes (!) and fell, getting up at once, with nothing wrong except nosebleed. After a half-hour he felt weaker and was ordered to leave the post, whereupon, on the road, his weakness increased and he tended to fall to the right, but reached the ambulance on foot.
October 23, there was no longer any evidence of hemiparesis, the Babinski reflex had entirely disappeared; there was no complaint except of dizziness and headaches. He got back his autocritique on the matter of remaining in the air ten minutes, but there was still an amnesia for the ten day period between the shock and his arrival at Paul-Brousse. He forgot that he had had a lumbar puncture October 7.
Another puncture, October 25, yielded some 14 or 15 lymphocytes to the cmm. There was still an excess of albumin. The lymphocytes decreased further according to a puncture November 2. Had this patient been examined some weeks after the shock there would have been no signs of an organic paresis, no special modification of the spinal fluid, and no reason for regarding the man as other than an hysteric. Early spinal puncture is, accordingly, important.
Of course, the question whether the lymphocytes and hyperalbuminosis of the fluid might not be syphilitic must be raised. At the Hospital Medical Society meeting, October 29, 1915, Souques states that Ravaut and Guillain believe that simple shell-shock often produces “syphilitic” chemical, physical or cytological changes in the spinal fluid. Roussy is cited as thinking such changes rare.
Shell-shock; burial: Coma and semicoma; BLOOD-STAINED SPINAL FLUID. Improvement on puncture. Persistent astasia abasia with spasticity.
A man was buried March 15, 1915, following the bursting of a large calibre shell. He is said to have had hemoptysis and arrived at hospital March 17 in coma. He kept moaning while asleep. March 18, he was still stupid and as if stunned. He did not talk or understand what was said, but was able to write a few words. The knee-jerks were a little exaggerated. There was a slight spasticity of the limbs, which was exaggerated on emotion into a sort of spasmodic crisis.
Lumbar puncture gave a reddish fluid under strong tension. After lumbar puncture the man came out of coma and the next day, after another puncture (fluid slightly yellowish), there was further improvement and the patient spoke. The third puncture, March 20, yielded yellow fluid. The spastic phenomena still persisted, however. The patient could not walk or stand. Every time he touched the ground he had a clonic crisis. He was evacuated to a neurological center.
Re astasia-abasia, Nonne found these cases heading a group of 63 cases of war hysteria treated in a twelvemonth. Figures as follows:
| Astasia-abasia | 14 |
| Generalized tremor | 12 |
| Brachial monoplegia | 11 |
| Isolated contracture | 6 |
| Crural paraplegia | 5 |
| Mutism | 5 |
| Isolated tic | 4 |
| Hemiplegia | 3 |
| Isolated respiratory convulsions | 2 |
| Isolated sensory disorder | 1 |
Fifty-one of the 63 cases were freed by therapy from their main symptoms (twenty-eight cases cured in one or two hypnotic sittings).
Prolonged bombardment; shell explosion (nearby?): Depression; suicidal attempt; hypertensive spinal fluid.
A patient entered an evacuation hospital June 27, having come from an ambulance with a ticket reading, “Melancholic depression, with stupor—attempt at suicide (threw himself into a pond)—sprained ankle—to be evacuated, lying down, on a milk diet.” The patient was depressed, indifferent to surroundings, irresponsive, and did not even look at an interlocutor. There was no other somatic sign except a pulse of 62. He did not eat, and remained lying down, without movement. Lumbar puncture in a sitting posture yielded a clear liquid under pressure of 34. June 30, another lumbar puncture yielded clear fluid of a dichroic appearance when looked at from above. 25 c.c. were removed. July 1, there had been a good deal of improvement. The patient said he was better and began to take a little milk. July 2, there was still some improvement. Pulse 60. He said that his condition had lasted a month and that it followed a violent and prolonged bombardment for ten days in his sector. July 3, he was much better, began to look about, talk, and eat a little. July 4, lumbar puncture yielded a clear fluid with a pressure of 30, reduced to 22 after withdrawal of 20 c.c.
According to Leriche, explosion of large calibre shells or of a mine can produce cerebral or spinal symptoms, some of which are removed by lumbar puncture. The fluid is red shortly after the explosion and under hypertension for some days. Such hypertension may be found even in shell cases that have no other sign of cerebral condition. This particular melancholy patient had a relapse and another depression with fugue.
Example of HEMATOMYELIA, indirect result of bullet wound. Partial recovery.
An infantry subaltern, 23 years old, was injured September 24, 1914, by a rifle bullet, which entered above the left clavicle and emerged between the right scapula and the vertebral column. The patient leaped into the air when he was struck, but fell at once and found that his legs were paralyzed. A feeling of cold crept up from the feet to the region of the umbilicus. Consciousness was preserved. There was hemoptysis because of the bullet’s passing through the left lung. The wounds all healed quickly. There was retention, followed by incontinence, of urine and feces; and the situation was complicated by eschars in the gluteal and trochanteric region.
For three months there was no change in the paraplegia, except that at the beginning of the third month the patient could move his fingers a little and raise his knees slightly. He was transferred back through three hospital units, with a diagnosis of spinal cord lesion or fracture due to a vertebral column lesion at the second and third dorsal vertebrae.
Seven months after injury, he reached a Russian hospital for a laminectomy, incapable of standing or walking without support, although able to sit and rise with extreme difficulty. He could now very slightly flex and extend the knees, and very slightly flex and rotate the ankle, and weakly move the toes. Passive movements could be carried out without much difficulty, though there was a slight joint and muscle stiffness. Both quadriceps muscles were markedly atrophied. There was slight amyotrophy of the lower legs. Tendon reflexes were exaggerated, and there was a marked ankle clonus, a Babinski reflex, and an abolition of the abdominal and cremasteric reflexes.
There was a sensory disorder of an incomplete syringomyelic pattern, with diminished sensibility to heat and complete abolition of pain sensibility. Touch and electric[285] sensations were somewhat delayed. There was a diminution in the faradic and galvanic excitability of the legs and feet; vasomotor disturbance (slight hyperidrosis) of the paralyzed limbs. Two of the eschars had not yet cicatrized. The sphincteric disturbances had diminished. For the rest the patient was normal. The second and third vertebrae showed deformity and were painful to pressure and percussion of spinous processes.
The patient was treated by galvanization of the spine, with a current descending at first and then ascending, and by faradization of the paralyzed muscles. There was progressive improvement, irregular but constant. At the time of report, July 1, 1915, he was perfectly well, able to take long walks, and without sphincter or sensory disturbance. The tendon reflexes were still exaggerated, and there was still a slight ankle clonus and Babinski. The abdominal and cremasteric reflexes were still abolished. The last of the seven eschars had not yet healed over.
For the organic nature of this lesion, the numerous early eschars, the persistent sphincter disturbances, the limited paresis of the legs, the reflex disorders, and the dissociation of sensations seem abundant evidence. It is probable that there was no fracture of the vertebrae (X-ray confirmation), and it is probable that there was a meningeal hemorrhage, together with some hemorrhagic foci in the spinal cord substance, especially in the gray matter. A good deal remains doubtful: Mendelssohn remarks that the sphincter disturbances ought to be related to disorder of the fourth and fifth sacral segments, and the knee-jerk and Achilles jerk absence with disorder of the lower lumbar, and sacral region; the abdominal reflex disorder with the low thoracic lesion; the distribution of the anesthesia ought to indicate a lesion in the lower part of the spinal cord. Was not the hemorrhage therefore lower down than the spot where the vertebrae were displaced? It is surely of prognostic note that the eschars did not necessarily foretell a fatal outcome; in fact, the patient had become functionally well before the seventh eschar was healed over.
Shell explosion with subject lying down applied to machine-gun; no contusion: HEMATOMYELIA. Partial recovery.
A veterinary student, six months captive in Germany, wrote out for Babinski the following:
“September 1, 1914, I was about to operate a machine gun when a shrapnel shell exploded very near me,—probably about two or three metres overhead. I base this estimate on comparisons made with shells I saw exploded beside me before this one.
“Just after the explosion, which deafened me and at the same time took my breath away a little, from the powder, I felt a rather severe pain in the kidney region,—a pain which then persisted without interruption. I moved my left arm, to find the effect produced by a bullet which I heard whistle by my ear and which struck the upper part of the left shoulder without entering. At the same time, I tried to turn to see what had become of my legs, and had a feeling that they had vanished. Almost immediately I felt little prickings, not very painful, in the lumbar region and in the upper part of the thighs. Just then, seeing my comrades going away I tried to imitate them, but could not. All these feelings passed very rapidly.
“A comrade then came near to tell me to go back. I told him that I could not move and that I must have been wounded in the lumbar region. He looked at my kit and my coat and said there was no trace of shot or tear. Not wanting to leave me, he lifted me by the armpits and knees. I could not help him get me up, and my legs hung flexed and inert. After a few steps he had to put me down, and tried to stand me up. I immediately crumpled. I had no sensation of my feet touching the ground. I sent my comrade back, asking him to tell my brother, who was in my squad. I did not lose consciousness or any feeling of my situation, or of the danger being run by my comrade.”
The man remained four days on the battle field without food. He was on the edge of a stream. He did not defecate, nor for two days did he urinate. Eventually the bladder and[287] rectal functions were re-established, though they remained irregular. Catheterization was never resorted to. The lumbar pains were diffuse, fixing themselves a few days after the accident in the region below the umbilicus. There were pains at the waist predominating on the left side. The paralysis of the lower extremities grew rapidly better. Movements in the right leg reappeared, and 27 days after the accident the man was able to stand and walk around his bed. Still further movement followed (left leg weaker).
At the time of the report, May 28, 1915, the patient could walk without a cane, but he could get about only slowly. The left toes would rub against the ground, and he could not support himself for any length of time on his legs. The knee-jerks were exaggerated, especially the left. The Achilles jerks were increased. There was a Babinski reflex on the left side and an abduction of the fifth toe on plantar stimulation. The same reflexes were found on the right side, but less marked. Abdominal reflexes absent, except the right superior reflex, which was distinctly present. Cremasteric reflexes absent. Anal reflexes preserved. The defense reflexes were exaggerated, but more markedly on the left side. The zone from which the defense reflexes could be elicited on the left side included the whole lower extremity and rose as far as 2 or 3 cm. above the nipple. Stimulation of the lateral parts of the left lower extremity would even produce defense reflex movements on both sides of the body. On the right side, however, the defense reflex movements could only be tried out by scratching the anterior surface of the ankle, which was then followed by a flexion of the foot.
Sensibility to touch and deep sensibility were preserved; but sensibility to temperature and pain, normal on the left,—i.e., paralyzed—side, was weak in the right leg. There was a marked sudation on the left side, limited by the white line, the inguinal fold, the iliac spines, and a horizontal line passing through the umbilicus.
Here, then, paralysis followed a shell explosion while the subject was lying down. No contusion therefore was possible. According to Babinski, we are dealing probably with a hematomyelia, the result of shell explosion.
Struck by missile in back; unconsciousness; no wound: Hysterical paraplegia? HERPES and SEGMENTARY Hyperalgesia suggest radicular and spinal injury. Recovery.
November 1, 1914, a sergeant in the 20th Hussars, with other dismounted cavalrymen, was chasing Germans with a bayonet, over turnip fields pitted by shells. Several hours later, he found himself in a house in a nearby village, to which he had been carried unconscious. Probably he had been struck by some missile in the back, as the bottom of his haversack had been torn off. His face was blackened with smoke, and his clothes were muddy. He had no wound. His left arm was weak and his legs powerless and numb. The passing of water was painful, but there was no blood in the water and no hemoptysis.
Five days later, he was examined at a base hospital and found to be paralyzed and numb in the legs. The knee-jerk and ankle-jerk were retained upon the right side only. Pain occurred on passive movements of the legs, which were flaccid; there was a hyperalgesia about Poupart’s ligament, more marked on the left side. Lower abdominal reflexes were weak on the left side; pain in lower abdomen with bladder full and at outset of micturition. Pain and paresis also affected the left arm, but there was no numbness. Pain on pressure over lumbar and cervical vertebral spines. There was no evidence of bruising.
The physicians were inclined to regard the phenomena as hysterical. Three days later, the arm movements became much freer, and after another three days, the arm movements were fairly powerful, and the legs much stronger, although the patient could not yet stand or walk. He still had pain if his bladder was full.
After Ballard
As against the diagnosis of hysteria, three herpetic clusters appeared on the skin of the left thigh, from three to six inches above the knee. Elliot regards it as certain that the posterior root ganglia were injured. He regards the case as one of injury to the spinal nerve roots. The hyperalgesia about the body of course suggested damage to the spinal cord. According to Elliot, therefore, this case is one of organic disease; whether of the roots or of the cord was uncertain. At any rate the cases of this type, though not functional, recovered.
Mine-explosion; burial; labyrinthine lesions and head bruises, more marked on left side: Focal canities (WHITE HAIR developing OVERNIGHT) on left side.
A soldier, 23, in the Argonne was blown up by a mine in a trench, fell, and was covered by a mass of earth, from which he extricated himself. He immediately became deaf from what was medically determined to be a double hemorrhagic labyrinthitis. There were also superficial powder burns of the face, as well as several bruises on the head, especially on the left side.
The next day, at the English hospital at Arc-en-Barrois, the patient noticed tufts of white hair on the left side of the head. There were four islets of gray hair in the left fronto-parieto-occipital region, separated from one another by normal hairs. The gray hairs were gray completely from the roots to the ends of the hair. The longest hairs were as white as the shortest. There was not a brown hair amongst them. The gray hairs were solidly implanted, and could be pulled out only by strong traction. There was a discoloration also of the bulbar swelling of the hair. The rest of the head hair was dark brown. His hair was described in the military description: “deep chestnut brown.” There was no other symptom aside from an incessant twitching of the left eyelids. The place of whitening was apparently determined by the region of the scalp injured. Not only were the bruises on the left side of the head and face, but the labyrinthine lesions were more marked on this side and the twitching of the eye-lids was confined to the left side.
Shrapnel wound of skull; focal canities over wound; shell-shock and shrapnel wound of right leg. Head tremors and contractions, changing in relation to posture; glove anesthesia and local anesthesia of trunk.
A Russian private, 24, was wounded twice: once in the head by a bullet, and at another time by a bit of shrapnel that imbedded itself in the skull. The hair over the injured spot became gray.
Later, September 16, 1915, the soldier was subjected to shell-shock, and at the same time wounded by shrapnel fragment in the right leg (operated next day).
Upon examination at Petrograd, the hearing was found diminished and the eardrum was pulled in. At first the patient could not speak or open his eyes, and made incessant lateral movements of the head, jerking backwards and to the right. The right half of the face gave convulsive movements, which began at the lip and spread upwards. During sleep, there was an entire cessation of these head shakings and jerks. In the lying posture, the head shook at a rate of 100 to 120 per minute. The jerking movements became more marked when the patient sat up or walked. He carried his head bent toward the right shoulder. When he sat down, the side-shaking movements disappeared, only to reappear when he lay down. The swallowing reflexes were absent. The sensitiveness to touch, pain, and temperature was lost in the upper part of the trunk including the neck, to the level of the tenth dorsal vertebra. There was anesthesia of the arms as far as the elbow on the right, and as far as the shoulder on the left. The mucosae of the mouth were anesthetic. Dermatographia was strongly marked.
Shell explosion; burial: Hemiplegia, probably organic.
A soldier was blown up by a shell and then buried at Vaux, March 29, 1916, and entered the Salpêtrière, July, 1916, with a right-sided hemiplegia and contracture without evidence of wound. He remembered nothing for the first fortnight after the trauma. When he came to himself, he was paralyzed and was unable to say more than a few words, but at the end of a month his aphasia ceased and he began to walk.
The hemiplegia was spastic. There was pronounced contracture. The arm was extended, hand open, fingers stretched. Finger movements were diminished, as well as extension of the wrist, but the arm was otherwise normal. The leg was not so stiff. The great toe was in a state of continuous extension. The toes could not be moved, and the foot scarcely; but the leg could be strongly flexed and extended on the thigh. The tendon reflexes of the right side were more lively than on the left. Cloniform movements followed tapping the patellar tendon on the right side, and a patellar clonus and ankle clonus could also be demonstrated. Plantar reflex, flexor on the right. Distinct adduction of the foot. Slight disturbance of tactile sensibility in the paralyzed limbs; marked disorder of position sense and gross disturbance of stereognostic sense. Moderate dysarthria.
Ten months after the traumatism, the hemiplegia and spastic walk remained. The upper limb was now carried in extension back of the body, with hand supinated, fingers sometimes in extension, sometimes in flexion, index finger separately from the others. Finger movements difficult and shoulder movements limited. The leg, however, was almost normal except that the toes could not be moved. The tendon reflexes were more lively and cloniform on the right, but there was no longer patellar or ankle clonus. Stereognosis slow, but finger movements were naturally difficult. W. R. of blood, negative. Probably this is an organic case.
Blown up by a shell; no skin or bone lesion: Mixture of organic (e.g., lost knee-jerks) and functional (e.g., urinary retention) disorders.
A man, 38, was blown up in a trench without sustaining skin or skeletal lesions, April 5, 1915. He lost consciousness for a half hour and, coming to, found a crural paraplegia and urinary retention. Examined July 24, in addition to the paraplegia were found tactile and algesic hypesthesia of the legs with preservation of deep sensibility. Pains were felt in the legs, especially in the hips. The knee-jerks were abolished; the Achilles jerks were preserved, as well as the flexor plantar reflexes and somewhat weakened cremasteric and abdominal reflexes. Micturition was difficult. Constipation. Slight paresis of left arm. Lumbar puncture, July 28, yielded a clear fluid of normal tension without chemical or cytological changes.
The sphincter disorders gradually disappeared. The knee-jerks reappeared in a weakened form August 31. The legs could, at the time of report, be moved somewhat, though not above the level of the bed.
We here deal, presumably, with a mild form of concussion of the spinal cord, in which, however, some of the transient symptoms are very possibly merely functional in origin.
Re complicated pictures of organic and functional nature, some experimental work has been carried out. Mairet and Durante set off explosives, such as melinite, at a distance of 1 to 1.5 metres, near rabbits. Some died at intervals from an hour to thirteen days; others lived. Pulmonary apoplexy was found in the cases dying early. Spinal cord and root hemorrhages, hemorrhages in the cortical and bulbar gray, perivascular and ependymal hemorrhages were found, always small and without diffusion, suggesting rupture by rapid decompression following the first wave of aerial compression. The functional effects are thought to be brought about through the anemia of the areas supplied by the ruptured[295] vessels. Russca of Berne got similar results and notes direct and contrecoup brain lesions, tympanic perforations, intra- and extra-ocular hemorrhages, thoracic, cardiac, and splenic hemorrhages, ruptures of kidney, stomach, intestine, and diaphragm. As in the work of Mairet and Durante, the lung proved the most sensitive organ. (Compare also the human case of Sencert [Case 201].) Some experiments with fishes yielded lesions of the swimming bladder. Persalite and other explosives were used.
GASSING: Organic-looking picture.
A German soldier, 21, was a serious case of gassing. He was unconscious two days (venesection twice). When he came to, he could not walk and felt as if he were drunk. October 22, 1916, he was incoördinate in walking and tended to fall forward when standing with eyes closed. The ataxia of the legs was demonstrable in the position of dorsal decubitus, and there was also a slight ataxia of the arms. The pupils were dilated and reacted poorly to light.
December 12, all symptoms had disappeared. The clinical picture in this case was somewhat like that of a multiple sclerosis. According to Neiding, the disorder is not a functional one but an organic cerebellar disorder.
Re the neurology of gas poisoning, Neiding regards the condition as a new nosological unit. We do not know what the ultimate results of apparently cured cases will be. Court questions of importance will doubtless arise with reference to their compensation. Ninety-six of Neiding’s 274 cases failed to show any nerve symptoms whatever; forty-six cases showed one symptom only, such as headache, dizziness, abnormality of reflexes, or abnormality in sensation. One hundred and thirty-two cases presented a fairly full picture. The picture of a complete traumatic neurosis not infrequently appears, aided perhaps by the psychic features of the gas attacks; and possibly some cases are entirely psychogenic from the beginning. Such symptoms, for example, as dermatographia, rapid and irregular heart, hyperidrosis, blepharospasm, mental perturbation, hypochondria, etc., do not necessarily point to any directly toxic effect of the gases. Thirty-seven of Neiding’s cases showed pupillary changes, hyperreflexia, and analgesia. Thirty-one showed analgesia and absence of laryngeal and corneal reflexes. Twenty-six showed pupillary changes and hyperreflexia, four of these latter showing also an absence of laryngeal and corneal reflexes. One case yielded hyperalgesia alone; ten yielded headache, dizziness, and analgesia.
GASSING: Mutism, tremors, depression, battle dreams.
An infantryman, aged 27, had been at the front for three months. He was wounded a month before coming to hospital; but when the wound healed he went back to the front, quite mute but intelligent and able to write the following:
“We were on our way to the trenches, and as we were going through the railway cutting they started to shell us, with gas shells mostly, and we had not been there more than quarter of an hour when I was compelled to lie down from temporary blindness and weakness through getting a dose of gas through my mouth and eyes. I was lying down for about ten minutes when a shell came somewhere near, and was struck by something in the face and on my left knee and I remembered no more until I found myself in hospital. I was all of a shake and while lying down would frequently jump up and wonder where I was.”
The patient had been mute thereafter, depressed, and given to dreams about fighting and shells. There was a fine tremor controllable by the will; the knee-jerks were increased. On lateral deviation, there was difficulty in fixing the eyes. There was a slight deafness due to an old discharging left ear. According to Wiltshire, Shell-shock is only exceptionally caused by chemical poisoning from gas.
Re poisoning by certain German asphyxiating gases, Sereysky reports in 1917 that these gases contained, among other poisons, a nerve poison. He found that poor heredity was a favorable soil for the action of this nerve poison. The clinical pictures in the gassed soldiers rather suggested cerebral arteriosclerosis. He remarks that the logical distance between the “exogenous” and “endogenous” is greatly reduced in these gassed cases, as the syndrome of “exogenous” gassing closely approximates that of various “endogenous” disorders.
Hysterical speech disorder related to mechanical disorder of auditory apparatus.
Whenever a German officer’s servant, 23 years, was addressed on the ward in the Jena Nerve Hospital, his hands would tremble and the muscles of his face would fall into grimacing associated movements. He had a peculiar infantile type of speech, talking with a fixed glance and an anxious mien. He would carefully utter, as a rule, separate words, chiefly only nouns or infinitives. He would gesticulate with both hands to make what he said understood. Thus (freely translating the German) runs his description of a battle:
“Well—because—I—we had—no artillery and so many losses—then got in position again, then we—laid down a long time—perhaps until four o’clock in the afternoon—five—and—and it happened that—lay in Rübenfeld—couldn’t go back—then shell near me—fell in and I right near, how—how far—I don’t know and—grown better. Comrade said—10 meters—don’t know—un—unconscious.”
Long compound German words could not be repeated, since after the first or second syllable there was a severe emotional excitement; syllable articulation and phonation ceased. Finally, however, the patient could be gotten to pronounce the whole word. Reading aloud was very difficult: syllable sounding and omission of difficult syllables; after a time, weeping.
The patient was a somewhat small, muscular, well-nourished man, with a murmur at the apex, a somewhat rapid pulse, increased reflexes, especially skin reflexes, painful supra- and infra-orbital points, temples painful to percussion, pressure over spine painful from second thoracic to third lumbar vertebrae. There was an increased sensitiveness to touch and pain over the whole body. There was a bilateral, somewhat marked tremor, more marked on the left side than on the right. Swaying in Romberg position was slight. Tremor of tongue.
This patient was first brought to Jena November 23, 1914. An illegitimate child, a moderately good scholar, he had worked as a mason until he went into the army, in 1912. He worked as a soldier chiefly in the officers’ casino because he got pains in his legs and knees in long drills. At the outset of the campaign, however, he withstood the heavy marching, although with difficulty. He was in his first actual skirmish September 20. A shell struck nearby and threw him several meters; whereupon he became unconscious and was carried away by the hospital corps. When he woke up he could not speak or hear. Ten days later, however, speech returned, and hearing returned in right ear; October, deaf in the left ear, and he could not hear a watch tick on the right side at a distance of 16 centimeters. He was examined at the otological clinic in Jena October 12, where the drum membranes were both found opaque, without reflexes or normal contours; hysterical attack on the caloric test. The next day, on the medical visit, there was a screaming attack. His plight seemed not so much simulation as one of traumatic hysteria.
Again, after his stay at the nerve hospital, another hysterical outburst was produced by a hearing test with vestibular apparatus, in the ear clinic, February 6, 1915. The diagnosis was nervous deafness with involvement of left ear.
The insomnia was successfully treated by sodium bicarbonate. There was a slight improvement in speech. In March body weight had improved, but there was a marked tremor of the right hand. In the next few months there was a progressive improvement in general well-being, in speech disorder, and in tremor. The auditory disorder remained unchanged. The man now works in his father’s garden.
This case appears to show a combination of psychic and mechanical injury. There are severe hysterical auditory and speech disorders. Although the auditory disorder is of mechanical origin, the speech disorder appears to be of psychogenic nature. It is somewhat remarkable that the ear tests almost every time produce hysterical attacks in the form of convulsive crying. Rather unusual is the general cutaneous hyperalgesia, more marked about the ears.
Shell-shock (distant, neither seen nor heard); left tympanum ruptured; semicoma eight days: Cerebellar syndrome and hemianesthesia. Recovery, nine months.
A lieutenant underwent “shell-shock” either at night or in the early morning, September, 1915, the shell bursting at a distance. He neither saw nor heard the shell, lost consciousness and was eight days semicomatose, failing to recognize his wife.
On recovering his senses, he could not get about, as he had lost his memory, having to write down his room number and be warned of meal times. He was led about like a child. He had a continuous headache on the right side and pains in the occiput and along the spinal column, as well as in the right leg as far as the heel. These leg pains were lightning pains. Walking was difficult, staggering, leaning to left. Weakness of right arm and leg; right-sided hemianalgesia. Complete insomnia. During November there were frequent urgent desires to urinate day or night. Evacuated to the oto-rhino-laryngological center in Bordeaux, December 13, for examination of ears. The right ear was found normal, but there was a rupture of the left tympanum. There was at this time a trismus. The jaws were opened with the dilator and the man had a syncope during this operation. The question of surgical intervention for a cerebral lesion was raised, but he was first sent to the neurologists at Bordeaux. There, December 31, he was found with a facies of anguish, unstable gait, inclination to the left in walking; no Rombergism; occasional dizzy spells. In walking, the right foot was pointed outward and on request to direct it forward he complained of pain in the loins, reaching as far as the scapula. Walking with eyes closed, he leaned to the left and lost balance. With eyes open, no disorder of balance. With eyes closed, the body leaned backward. If requested to go back, he failed to flex his legs to keep balance. If he was asked to[301] put a foot upon the chair in front of him, he immediately fell backwards. He could not support his body on the right leg more than a few moments. He had difficulty in raising both legs from the bed at one time and he could lift the right leg not so high as the left. Movements of the legs were performed hesitatingly and slowly and with greater difficulty with eyes closed.
He could not thread a needle and could hardly dress himself. Eyes closed, he could with difficulty perform the finger to nose test; eyes open, with much less difficulty. Adiadochokinesis; muscular strength less in right than left; plantar reflexes absent; knee-jerks lively; hemianalgesia, right side. Loss of deep and bony sensibility on right side and diminution of testicular sensibility. Retraction of visual field, right; diminution of smell and loss of hearing, right; position sense absent on this side; stereognostic sense preserved. Mentally, memory was poor; he was unable to read or do mental work. He slept little and had bad battle dreams. He was very impressionable and emotional and constantly complained of occipital pain. He had lost 8 kilos weight.
He grew gradually better. In May he could go out alone. The muscular strength increased. The adiadochokinesis and synergic disturbances lessened; the hemianesthesia persisted. In June there was greater improvement; in fact, there was no sign of disorder left except irregular sleep.
We here deal with a cerebellar syndrome plus a hemianesthesia.
Mine explosion: Tremors, mutism, hemiplegia. Tremors cleared by hypnosis. Mutism replaced by stuttering. Persistent hemiplegia, probably organic.
A soldier was blown up by a mine and rendered unconscious. Upon recovery of consciousness, the patient was dumb, unable to work, very nervous, paralyzed as to left arm and leg. The paralysis improved so that in the hospital at home the patient became able to get about. However, he threw his legs about in an unusual fashion. Several months later the patient was much improved.
Shortly, there was a relapse. Transferred to a hospital for chronic cases, the patient was unable to walk without assistance on account of complete paralysis of the leg. There was insomnia, a general tremor, bad stuttering, and a habit of starting in terror at the slightest noise.
Hypnotic treatment was followed by almost complete disappearance of the tremor. The patient began to sleep six or seven hours a night; nervousness diminished, and the stuttering slowly improved; but neither the paralysis nor the anesthesia of the left leg was affected by suggestion. The leg remained cold, livid, anesthetic, and flaccidly paralyzed to the hip. A slight improvement has followed upon faradization but the patient still can walk only with assistance.
Smyly regards this case as probably not a true case of Shell-shock, depending as he states[303] “more on a lesion in the nervous system than in the psyche.”
Shrapnel bullet WOUND of skull: Unconsciousness (three weeks), followed by agraphia (three weeks), insomnia (six weeks), amnesia (six to eight weeks), hemiplegia (twelve weeks), impairment of vision (twelve to sixteen weeks), dreams (seven months). Recovery save for slight overfatiguability.
A French tailor, aged 22, of healthy stock, was wounded in the left frontal bone in August, 1914. The shrapnel bullet, from an unknown distance, made a penetrative wound. The man was able to remember how at the moment he was injured he felt a sort of strain in his brain, felt his head with his hand, found he was bleeding, took out a bandage from his kit, removed it from its cover and without unfolding it put it on his head. At this moment he fell unconscious and there was then complete loss of memory for three weeks. This patient, who was intellectually keen, distinguished exactly between what he could himself remember and what he was told by his comrades. One of these had told him that he had cried out indistinctly that in a matter of fifteen days he would be well. He estimated the interval between his wound and the loss of consciousness as about five minutes.
After three weeks, the tailor came to and remembers that the first word he heard was Munich. Astonished to be in Bavaria he asked for paper and pen to write to his people, but found he could not write, though still able to dictate a little to his comrades. Besides agraphia there was hemiplegia on the right side, marked exhaustion, rapid fatiguability of vision, power of concentration but slightly diminished, and apathy for his surroundings; emotions normal.
Three weeks later the power to write returned; after six weeks, sleep; memory was restored in from six to eight weeks; the paralysis disappeared in twelve weeks; vision became normal in three or four months; the dreams ceased after seven months. The mood for the first two months after regaining consciousness was slightly elevated; for another two months slightly depressed. The mood then became normal.[304] There was, then, in this case complete recovery save for slight overfatiguability in a period of seven months. There were still a few residuals of hemiplegia. An operation in November, 1916, removed a shrapnel ball, one centimeter in diameter, from a dural scar.
This is a case of acute reaction psychosis of exogenous origin lasting three weeks and leading to complete recovery in an after phase of from four to seven months.
Normal subject, wounded and thrown to ground by shell explosion: Recurring MEMORIES of battle scene; persistently HYPERESTHETIC healed shell WOUND, with pupil and pulse changes on pressure of the scar.
A lieutenant of artillery, student (one of his brothers dead of meningitis), suffered somewhat from diarrhœa on the battlefield. He was, however, always able to obtain the best of food. External conditions did not seriously interfere with sleep. In particular there was no excessive dampness where he was. He was preoccupied with having to act as substitute for the commandant of the battery. He was not afflicted by the thought of his parents far away; their financial affairs were entirely satisfactory.
This almost normal man was wounded after a day of incessant fighting five months after going to the front. When firing ceased, he withdrew with his soldiers to a trench. Here he was followed by an enemy gas shell which killed some and wounded others. While outside the trench shifting mutilated soldiers to the rear, he was hit by another shell of which a chip wounded him in the left thigh. He felt a terrible spanking blow that threw him to the ground and gave him great pain. He was carried on a stretcher to the medical post across the zone of fire; thence to a field hospital and from there to a hospital further from the front. He had been for almost seven hours in a sector of the fighting line which had been almost continuously active.
The wound healed in less than a week. But what he had seen and felt kept tormenting his mind. There remained slight numbness in the wound where there was to be seen a spot of pigment, the size of a two-cent coin, with somewhat obscure outlines. The pain was irritated by damp weather, in certain positions, and by touch, and the pain on pressure was reflected in the pupils and in the pulse.
No other disturbance, organic or functional, was found.
Wounds; operation: Hysterical FACIAL SPASM.
A 23-year old soldier was admitted to the National Hospital for the Paralyzed and Epileptic, June 18, 1915, in the following state: He sat in bed, gasping, with the left side of the face set in a strong tonic spasm and jaws tightly set. The contraction of the masseters was such that his mouth could not be forcibly opened. He himself could separate his teeth for about a half a centimeter, but the jaws came together when a spatula was brought for insertion and then failed to relax. The facial spasm increased as the jaw was clenched more tightly. The patient said he was unable to breathe excepting when sitting upright, and when put into dorsal decubitus he breathed violently through his clenched teeth and held his breath as long as he could, “assuming a purple tinge,” as Dr. Batten states, “which was apt to be disconcerting until one was accustomed to it.” Faradism and force permitted the removal of false teeth but only to the accompaniment of shrieks, foaming, and violent movements of the arms, lacrimation, and sweating. During sleep, the face was at rest. The spasm of left face and of jaw would come on a few seconds after waking, when an observer was perceived. Attempts to force the mouth open invoked the same procedure as before in spite of the fact that the patient ate well. In a month he was virtually normal.
It appears that May 13, about five weeks before, the patient had been struck by shrapnel on the right hand, forearm, and shoulder, and base of the nose, while in France. He had been dazed but had not lost consciousness, and the wounds had completely healed before arrival at hospital. It was about a week after being wounded that the patient was operated upon for removal of shrapnel from the face. Upon recovery from the anesthetic, the patient found himself unable to move the right side of the face. Unable to remove his teeth, he had been fed by rubber tube.
Shell-shock: Hyperesthesia and over-reaction.
A stretcher-bearer, 19, who had had 18 months’ service and 6 months’ service in France, sent to Lieut-Col. Myers the day after admission to a base hospital, showed a remarkable condition of hyperesthesia and over-reaction.
It appears that four days before, he had been blown up three times by aero torpedo mortar shells while attending the wounded. One had blown him into the air, another had blown him into a dug-out, and a third had knocked him down. Two or three hours later, having finished the job of carrying wounded to the dressing station, everything seemed to “go black” in the dug-out where he was resting, and from that time on he had been shaky. It seemed that he had hardly slept for several days before he finally gave in.
There were irregular spasmodic movements of the head, arms (especially the right), and legs (especially the left). There were coarse tremors and incoördination in moving the arms. With eyes closed, he touched his nose with uncertainty. Cotton-wool touch on arms or head provoked lively movements. “I was always ticklish,” he explained, “but never like this; I can’t stand it, Sir.” Pinpricks produced almost convulsions. There was perspiration, rigidity of legs, and spasm such that knee-jerks were unobtainable. Plantar reaction, flexor. There were also visual hallucinations of bursting shells, and these were also heard when dozing.
Improvement followed with rest, but about two weeks later, on waking to find himself being carried back to his tent to avoid a shower, he was so terrified that a special nurse became necessary. He was still jumpy the next day, alarmed at footsteps, and afflicted with headache. He improved further in three days; remained two months in hospital in England, had one month’s leave, and then returned to light duty.
Shell-shock; thrown against wall; comrades killed; no visible trauma, or loss of consciousness: Persistent TREMORS, augmented in intentional movements; CRISES of agitation following noise or emotion.
A corporal (an expert gunner) and his squad had just entered a mine shaft on Nouvron Plateau, January 13, 1915, when a shell, bursting above them, threw him violently against the wall and killed or wounded several of his comrades. The corporal himself was not wounded, nor is it clear that consciousness was lost. The man lay waiting on the ground for some time until a communication trench could be finished and he could be evacuated without much danger from the mine shaft. He had already begun to tremble, and trembled still more while going back in the trench.
He carried on there for a fortnight, always trembling, but not eating and no longer able to handle a gun. He was evacuated a month later and sent successively to Villers-Cotterets, to Meaux, to Courneuve (a month), again to Meaux, and finally to the neurological center at Villers-Cotterets, where he remained for two months (April 13 to June 15, 1915). Here he was given the diagnosis of hysterical chorea by Guillain, and showed lively knee-jerks and Achilles jerks and great emotionality. The tremors were greatly increased when the cannon grew loud or bombs burst nearby. Lumbar puncture here showed a perfectly normal spinal fluid. He was then sent to the Salpêtrière, June 19, 1915, and was evacuated July 13 to a civil hospital until September 24, whence he was sent for convalescence to his home village, October 6 to December 15, from which he was returned to the Salpêtrière.
Throughout these transfers there had been no change whatever in his status. For almost a year, as the result of a shell explosion, he had been trembling in precisely the same way. All four extremities trembled equally, unless the right arm and the left leg might be thought to tremble a bit more. The[309] tremor was equally pronounced in dorsal decubitus as in the sitting or upright postures, but ceased during sleep. The tremors were worse in the evening and it was hard for the man to get to sleep. The eyelids and tongue showed a few irregular, jerking movements, not synchronous with the tremor of the extremities. The head showed few tremors. The patient was able to diminish the trembling of the arms somewhat by keeping the elbows flexed at a right angle and held firmly to his body. If the tremor of the legs got more energetic, the patient would get up and take a few steps. Any movement, such as laying hold of an object, carrying a spoon or a glass to the mouth, led to an exaggeration of the tremors in such wise that the tremor of multiple sclerosis in its most extreme form was recalled. It was very hard for the man to eat. If the eyes were closed, the tremors grew more marked. The emotion caused by sudden noise or sharp command or memory of his trench life caused motor crises, with coarse, generalized movements, and even loss of balance. This agitation grew gradually less marked, but the tremors persisted. An attempt to test reflexes led to violent generalized contractions. There was no sensory disorder. The pulse was variable; at rest it stood at 60; if a table near by was struck suddenly, the pulse would go up to 120.
Sharp gunfire: TREMORS; TREMOPHOBIA. A patient’s (an artist) description of his feelings.
One of Meige’s victims of shell-shock tremors was an artist. He stood the hardest sort of trench life for many months without disorder. Under particularly sharp fire, “the machine went off the track,” as the artist said, and he began to tremble. Both arms and head trembled, but especially the head, which was subject to small sidewise oscillations, variable in degree, and almost permanent,—a sort of vibration which the patient could diminish somewhat by stiffening his neck muscles. His manual tremor was not exaggerated by voluntary movements. Superficially he resembled a Parkinsonian case. He presented a curious appearance of combined vibrations and stiffness.
There was no doubt that this tremor had an emotional origin. In fact, the psychopathic status of the patient was described by the artist himself.[311] “My nervous state, which I thought ought to last not more than a fortnight, still persists more than three, or almost four, months after being evacuated, although the trembling is a little less. I am calmer and palpitate less, and my hands perspire less when I am emotional or making an effort. At first, the slightest shock immediately ran through me, followed by an uncontrollable trembling. Now there is an appreciable delay between the shock and the trembling; I can control it for a few seconds but not longer. The subway gate noises, a flaring light, a locomotive whistle, the barking of a dog, or some boyish prank is enough to set off the trembling; going to the theater, listening to music, reading a poem, or being present at a religious ceremony, acts the same way. Recently when a flag was being raised at the Invalides, I thought at first that I was going to be cured by so moving a spectacle, but then I suddenly began to tremble so violently that I had to cry out, and I had to sit down, weeping like a child. Sometimes the trembling comes on suddenly without any cause. I went to a novelty shop to do some errands with my wife. The crowd, the lights, the rustling of the silk, the colors of the goods—everything was a delight to me to look upon,—a contrast to our trench misery. I was happy and chatted merrily, like a schoolboy on a vacation. All of a sudden I felt that my strength was leaving me. I stopped talking; I felt a bad sensation in my back; I felt my cheeks hollowing in. I began to stare, and the trembling came on again, together with a great feeling of discomfort. If I can lean against something, sit down, or better, lie down, the trembling gets better and pretty soon stops. There are three conditions in which I feel well: first, upon waking after 11 or 12 hours’ sleep; next, after a meal, especially if it is a good one; and lastly, and above all, when I get the electric douche. Then, as if by magic, my ideas get clear, cheerful, and regain color; I feel myself again. That lasts for an hour or so; then I relapse into my sad state.”
As to the tremophobia, this patient says “In the tramway or in the subway, I perceive that people are looking at me, and that gives me a terrible feeling. I feel that I am inspiring pity. Some excellent woman offers me her seat. I am deeply touched; but if they look at me and say nothing, what are they thinking of me? This anxiety makes me suffer a good deal. If I am able to speak it is less painful to me, for then it is obvious that, despite my trembling, I am not a coward. What a sad situation this is!”
Meige remarks that therapeutics is not especially successful in these cases of tremor. Sedative drugs, hyoscyamin, hyoscin, duboisin, and scopolamin, do not last long and should be used cautiously. Static electricity works well in some cases. Rest, isolation, and calm.
As for the military prognosis, a period of observation of some three to four months may be necessary to learn the nature of the tremor. If the tremor then fails to alter, a convalescent leave for one or two months may be given. The patient should then be re-observed by the same physician. Upon persistence of tremor, temporary invaliding. Tremors may be wittingly cultivated for medicolegal purposes (Brissaud’s sinistrosis.)
Letters of a German soldier about his shell-shock.
A volunteer, 21, who had been in civil life a lackey, wrote as follows upon arrival in Gaupp’s clinic:
“On account of our privations and the various terrible scenes that you have to see, my nerves went back on me. Like the rest of the front, we too had to suffer terribly heavy artillery fire from December 20 onwards. December 29 at eight o’clock in the evening, when I was about to mount guard at the camp, I was thrown down by a shell that unexpectedly struck near me across the earth pushed out into a trench. I ran at once to cover as some more shots followed directly. I couldn’t be made to do anything on the thirtieth nor can I very clearly remember the events of that day. There was a terrific cannonade again, then cries of the wounded and the sight of the dead, etc. I was told afterwards that I fell down, cried, struck about me, and remained lying, dazed. The first that I can remember was that I was lying on a floor. I was then carried into another house, into a better room. Then I regained consciousness and could hear again after the noise in the ears had stopped, but I could not talk or walk. I was unconscious for two days. I got into the hospital train at R. the next day but had to be carried in as I could not walk. Travelling in the train made me quite foolish in my head and gave me bad headaches; I could not form any clear thoughts.”
It seems that this volunteer had not been quite up to the hardships of the war from the beginning; always a weakling, he had to be spared on the marches. In fact, he had been refused by the army at the first examination as unfit. He had been a nervous, tender, somewhat anxious fellow since childhood.
At the clinic there was an astasia and an abasia without any signs of organic disease. The striking feature was mutism. He could understand things spoken and written, but he was entirely mute, nodding and shaking his head properly for affirmatives and negatives. He carried with him a few slips[313] of paper with written requests, like: “Please, can I have salt; otherwise I can’t eat the soup;” “Are we going to ride farther, I have such a bad headache. The doctor must not come. The one who wanted to shoot me if I couldn’t speak. They are all bad.”
Treatment by suggestion (laryngeal faradization, lively verbal suggestion to pronounce single vowels, syllables, and whole words and sentences with enunciation of them) removed the mutism in a few days. At first the man’s speech was low and somewhat retarded, but later it became entirely normal. Within ten days the abasia cleared up and the patient became lively and cheerful. He was depressed on finding that he had lice, but after losing them became happy and childlike again.
February 1, however, on learning that he would be able to do garrison duty again, he took the news very soberly, and grew more quiet, trembled and seemed anxious.
February 7, he was sent to the garrison, increasingly excited. His own account of it in a letter written to a hospital nurse, runs as follows:
“As you will see, I did not reach Dn. but only got as far as here [Another hospital]. I will tell you how it happened. Probably I ought to have remained in Tübingen for a while longer and perhaps then nothing would have happened to me. You will remember that I was more nervous and excited the last days than I had been before, and the cause was also known to you. I wanted to get home in some way and so I pretended to be as well as possible. That crying attack, or whatever it was [an outcry in a frightful dream] had not been thought of by the physician any further, you know, and so I didn’t think anything about it either. Then the head doctor asked me once if I had any trouble left. Well, I spoke out everything I had to say, but no further attention was paid to that either. Then when I took a walk and after walking slowly two hours could hardly stand, was trembling all over and had a high pulse and also a violent acute pain in the region of the heart, that wasn’t of any importance either. Well, then I just got better from day to day and so I got what I wanted only too easily because they wanted the space and I certainly would have gone home and not to Dn. as I should have. [His reserve battalion was at Dn.] I got into the wrong train at St. so as to go home. I kept saying to myself, ‘You can’t do that, it will be punished.’ Nevertheless I couldn’t act any other way because I was really sick from longing for home.”
Here he described an episode in a comrade who had lain beside him in the clinic, had gone off with him and had a hysterical excitement in Heidelberg so that he had to be detrained.
“I was so awfully sorry to see him so miserable. I began to cry and was startled by every train coming from the opposite direction and by every loud noise. I was stared at by everybody in Frankfort and I could only cry more. Then a soldier scolded me because I was running senselessly up and down. Finally I got into the Leipzig train. Another guard questioned me. Everything then got more and more confused in me; I heard my mother call; then I heard shooting again; and finally I was entirely confused. I came to my senses in a room in the station toward evening, and was frightened again at a loud noise somewhere or a passing train. Then I was told what I had done in the train. I had cried out and raved, tried to get out of the car, called for my father and mother, wanted to go home, imitated shooting; allowed myself to be calmed a little, but began to shout again at every loud noise. When I was out of the train I bit a soldier and tore his whole coat open, so then I was carried to the hospital here in an auto. Up to this time I have been able to calm myself very well. The physician said that it was quite natural that I should not have very strong nerves yet. I must have beaten about and got knocked against things a good deal. There are bruises on my head and I am covered with black-and-blue spots.”
A British soldier’s account of his shell-shock.
A British soldier, 22 years, who went out to France in November, 1914, remained well until March 12, 1915, when after shell explosion, he became unconscious for half an hour, and on recovery found he was deaf and dumb. He was able to think of words but could not say them. He remained dazed and frightened for a time, and still wakes up with a start at night.
He was admitted to the National Hospital for the Paralyzed and Epileptic, March 25, 1915, and on March 27 recovered his speech suddenly and spontaneously. By March 29 he had completely recovered and talked well. Dr. Batten remarks “how perfect the memory may be up to the time of concussion, and how complete the mechanism is for expressing the ideas in written words when that for spoken words is abolished”; which may be seen from the patient’s own account, as follows:
I went out to France on the 3/11/14 and I was two days at Le Havre and then we went on to our 1st Batt. When we arrived at our destination the regiment was in the trenches so we had to go in. It was snowing hard and I felt it very cold. This was at Givenchy. We were relieved the following night and we went back for a rest. The next place we went to was just opposite Neuve Chapelle on the La Bassée Road and it was awful, the trenches were up to the knees in mud and water. The first night was very quiet, but the following morning about 9 p.m. the Germans started shelling and continued all day; the next was the same, but about 1 o’clock the Germans were seen to be coming up in masses. They got to within a distance of about twenty-five yards, then they turned. They commenced shelling us again and they had another try about three o’clock but they did not get far. One of the men on my left had the half of his face blown away and we had about ninety-two killed and wounded. We got relieved after being in five days, then we went back for three days’ rest. The next place we went to was Rue[316] de l’Epinette and we had an awful time there just before Christmas. We went into the trenches and we were up to our middle in water and in some places it would have taken you over the head. We were in these trenches for twenty-four hours. There was nothing unusual happened and we got relieved by the Royal North Lancs.; but we did not get far away; we had just got into our billets and were making some tea when the fall-in went and we were told that the Germans had broken through the North Lancs. We went away without any great-coats, and into the trenches we went for other seventy-two hours, and if the Germans had attacked again we could not have fired a shot as we were hardly able to stand for the cold and with the wet kilts on our legs it was awful. We got nothing to eat except three biscuits that some of the men went out and got. When we came out of the trenches on Christmas Eve we looked all like old men and a lot of them had to be carried. We went back for a rest to (Nervaille?) about thirty kilometers from the firing line for a month. When we came back again we went to La Bassée and had a pretty hot time there. The next place we were at was at that big fight at Neuve Chapelle when 472 guns bombarded the German trench for thirty-five minutes. At about 7 p.m. the word was passed along that we were to charge the German trench in front supported by the City of London Territorials. We got the trench all right and I got orders about 4 p.m. to go back to our own trench and bring along the belt-filling machine belonging to the machine gun. There was not a proper communication trench, there was a small dry ditch that ran out in the direction of the trench we had taken for a distance of 150 yards, the other 100 yards you had to come across the open. We got into our trench all right, and I got this box on my back and started back to the trench. I was just stepping out of the trench when a shell burst just over my head and I went down. When I came to my senses I was lying in our support trench where I had been carried by two of the men of the 4th Black Watch. One of them said something but I could not hear him and I tried to tell him so, then I discovered that I could not speak.
Shell-shock by windage: Hysterical crural monoplegia, of gradual development beginning four days after accident. Recovery by suggestion.
A number of chasseurs were doing the “tortoise-shell” under bombardment, when the last chasseur in the line was blown forward above his comrades by a shell bursting about a meter behind him. He was projected some four or five meters, got up, walked four or five kilometers, found an automobile, and was carried to Nancy. He passed, according to his story, red urine three or four times. He was six days at Nancy, where a slight abrasion of the side was treated. He began to feel heavy in his left leg on the fourth day. At Vendôme, the paralysis got worse, and by November 17 he had apparently a complete paralysis of the left lower extremity, called “spinal contusion.” He walked upon two canes, dragging left leg behind and had to be carried upstairs on a stretcher. The reflexes were normal except that there might have been a very slight excess of the left knee-jerk. There was a slight hypesthesia of the left leg, sharply limited above.
These phenomena were strikingly modified, at a single sitting, by verbal suggestion and faradism, but the man was one of those with mauvaise volonté. He did not want to get well so quickly, so that his complete cure was delayed a while.
NATURE OF SHELL-SHOCK: At the nerve clinic the patient presents, e.g., sundry CONTRACTURES, of such a nature that they may be caused to DISAPPEAR BY SUGGESTION, e.g., by mental influences during recovery from chloroform narcosis (note battle-dreams). PAINS and ANESTHESIAS disappear PARI PASSU with the contractures. The history is of shell explosion so near as to burn patient’s clothing, fall with nosebleed, eight hours unconsciousness, crural monoplegia with anesthesia (crawled 3 meters, however).
The treatment of a German private, 22, for contracture of the left leg and other phenomena, culminated in narcosis. Binswanger lays stress upon the mental influence to be exerted upon the patient at the conclusion of narcosis, at the moment in which the patient is particularly accessible to verbal suggestion. Treatment (see diagnostic details below) was carried out as follows:
After a few days of essentially suggestive treatment with continued attempts at passive movements of the contracted joints (knee, ankle, toe), with steady concentration of the patient’s attention upon the joints, a slight mobility in the toe joint on passive movement was obtained.
After a few more days, the ankle became passively mobile to some degree; the patient exerted a certain resistance to passive flexion of toes and ankle. A week later, reflex contractions of the toes could be evoked by deep pin-prick. There had been an analgesia of both lower thighs and of the soles of the feet, and this analgesia remained unchanged. At this point, the subjective complaints of the patient, namely, noises in the head, especially in the left ear, and other cephalic sensations, tended to disappear and the patient felt subjectively better; yet there was still an intolerable itching of the head and spine.
A month after the admission of the patient to the nerve hospital of the psychiatric clinic in Jena, there had been no essential change in the immobility and contracture in extension in the left leg. Accordingly, with the permission of the patient, he was placed in deep chloroform narcosis, and the knee-joint was bent at a right angle and fixed in approximately that position with a bandage. This experiment failed because, while the patient was waking out of his narcosis, the leg slipped back into extension, breaking the bandage. Accordingly, deeper narcosis was undertaken, and the leg fixed at a right angle in a plaster cast.
While the patient was coming out of narcosis, it was evident that he had been dreaming of battle scenes. In fact, Binswanger remarks that these dream pictures and the words spoken while going under and coming out of narcosis, are curiously demonstrative of “sympathy with the enemy,” for while waking out of narcosis, he cried: “Dost see, dost see the enemy there? Has he a father and mother? Has he a wife? I’ll not kill him.” At the same time, he cried hard and continually made trigger-movements with his right forefinger.[6] In point of fact, throughout his waking treatment, no one was able to learn what was going on in his mind, his sleep was good and deep, and his emotional state was entirely quiet and patient.
As the patient was coming out of chloroform and regaining consciousness of his surroundings, he was repeatedly and persistently assured that the bending of his leg was now accomplished and the cramp removed. All that he would now have to do was to get back the strength of his leg.
During the next few days he complained of violent pains in his left knee-joint and in the ankle-joint, but he remained in good spirits and full of confidence. Accordingly, in five days the plaster was removed and the contracture in the knee-joint was found to be completely absent; the knee was easily movable. The ankle-joint was but slightly movable. He could accomplish slight active flexion of the knee-joint[320] while lying in bed, and the toe-joint had already, before the narcosis, been both actively and passively mobile. After a few days, exercises in walking were begun. The patient had a little difficulty with his left knee-joint in walking, walking in fact as if with knock-knee. The foot was not well raised from the ground on account of the persistent stiffness of the ankle-joint. Walking, however, improved daily. He walked for three hours, resting at intervals.
A sensory examination showed that the upper limit of the analgesia had come down five centimeters from its former level, now occupying the left foot and leg up to the junction of the lower with the middle third. There was now a zone of anesthesia interposed between the normal skin of the upper thigh and the anesthetic-and-analgesic skin of the lower thigh and leg. Upon the posterior aspect of the leg, the analgesia and anesthesia had disappeared to a point at about the middle of the upper thigh.
About five weeks after the narcotic experiment, the extended left leg could be actively raised while lying in bed, up to the full extent, with slight tremors. The patient described himself as fatigued by the active movements of this leg. The ankle-joint remained less effective. There was still a trace of resistance to passive movements. Although the passive movements of the toes were normal, active movements of these were weak and hard to execute. There was still a trace of difficulty at the knee in walking and the gait was awkward, trepidant, precipitate. He could get about without a cane, however. If unobserved, his posture was more certain and free. If he exerted himself hard, severe parietal headache on the right side would develop.
It was then proposed to the patient that another narcosis would rid him of the stiffness in his ankle-joint. He feared narcosis and was told that regular and energetic voluntary movements would also rid him of the stiffness. These will exercises consisted in his directing his whole attention to his left ankle-joint until he felt it. Then he was given the command: “Let go the joint”—whereupon he would take his attention away from the ankle-joint at once. In this way, he was told, his will would make the ankle-joint mobile.[321] Meantime he was given twice daily a gram of bromophenacetine for his parietal headache.
The result was a rapid recovery. There were still a few traces of difficulty at date of report. The zone of sensory loss had retreated to the ankle, with a cuff-like zone of hypalgesia above the definite zone of analgesia and anesthesia.
As to the previous nature of this case, although there was neuropathic heredity on the mother’s side, there had been no sign of any individual neuropathic disposition. He had been a volunteer since 1911 in a guard regiment of infantry. His military training had been well borne; in the war he had fought through 20 battles. On November 11, 1914, in a storming attack, he had had his breeches burned from the effects of a shell. He had fallen, unconscious; the unconsciousness lasted about eight hours. He found on awaking that he had had nosebleed. When he wanted to get up, he found that his left leg was completely paralyzed and insensible; in fact, he thought it had been cut away. He crawled for about three meters to a trench in which there were several wounded. In the evening he was taken by automobile to a field hospital, and on the 17th was removed to a reserve hospital at Erfurt. Thence he was transferred to the Jena Hospital, January 25, 1915.
A strongly built man, with many reflexes increased and a lively dermatographia. The reflexes of the left, or contractured, leg were lacking; the mastoid processes were painful, and the occiput and temples were painful to percussion. The spinous processes of the vertebral column in the lumbar region were painful. The other phenomena have been sufficiently indicated above. The head sensations were peculiar; there were no pains but a peculiar itching. Contraction of the fingers of the left hand was painful. There was a feeling as if there were lice under the skin in the left upper thigh. There was itching in the nose, which the patient described as due to the sulphur “out there,” meaning shell gases. Sleep and appetite were good. Memory was imperfect: he could no longer remember the names of the battles, and of late had had to count on his fingers to find out how much was 2 times 2. As to the curious parietal headache, contralateral[322] to the contractured leg, Binswanger inquires whether we may not here have to do with localized vascular phenomena of the brain part which might conceivably be related with the innervation of the leg. Binswanger remarks that if the plaster cast be left on too long, it may happen that hysterical contracture will take place in the new position.
As to the will exercises used in the present case, Binswanger remarks that the patients must be intelligent and attentive, and naturally they must desire to get well. Fortunately, many of the war hysterics do want to get well, since the contrary experience is had in various industrial cases.
Wound of thigh: Pseudocoxalgic monoplegia with anesthesia. Cure of anesthesia by faradism at one sitting. Cure of lameness by reëducation and electricity in one month.
An infantryman, observed at Villejuif, February 9, 1915, was suffering from a right-sided crural monoplegia of a pseudocoxalgic type, following a wound September 9, 1914. The wound had been a through-and-through one in the upper right thigh. Every active movement could be performed as well on the right side as on the left; but the strength of the movements was less on the right, especially that of leg-extension. The reflexes were normal, the lameness was slight, with toeing out; the sole came down flat upon the ground. There was an absolutely complete anesthesia of the entire right leg and side up to the umbilicus.
Energetic faradization of the skin caused the anesthesia to disappear the day the patient was brought to the hospital. The cure of the lameness required a month of reëducation and electricity.
According to Roussy and Lhermitte, crural monoplegia is less frequent than brachial monoplegia. The flaccid form is rare, and when it occurs, complete, though the patient always remains capable of executing some voluntary movements and can walk with crutches or cane. During the automatic movements of walking, some muscles may be observed to contract that remain immobile when the patient is being examined recumbent. Naturally such a difference in contractions standing and lying, would be very exceptional in a case of organic monoplegia.
Contusion of thigh: HYSTERICAL right crural MONOPLEGIA. An ORGANIC CRUTCH PARALYSIS develops in the right arm, unobserved by the patient whose main concern is his useless leg. Cure of leg by psychotherapy.
A certain lieutenant, following contusion of the right thigh, developed a crural monoplegia of hysterical nature. In fact, although the paralysis had lasted several months, the tendon reflexes, the skin reflexes, and the electrical responses of the muscles, were absolutely normal. Moreover, the good effects of psychotherapy confirmed the hypothesis. But besides the hysterical crural monoplegia, there was a radial paralysis on the right side, clearly organic in nature, due to the nerve compression by the crutch which the patient had employed on account of the paralysis of his leg.
Babinski notes that this association of conditions was remarkable in that it demonstrated that hysteria and simulation should not be confounded with one another. To be sure, it is difficult to tell simulation from suggested phenomena, for there are no objective characters that demarcate the two. Babinski had himself said that hysteria was a demi-simulation; but a demi-simulation is not a simulation. The patient was in fact, sincere enough in his belief that he could not move his leg. To obviate this paralysis, he had in fact leaned so conscientiously upon his crutch that an organic paralysis had resulted. In fact the radial palsy had only been discovered incidentally, and the paradox appeared that a purely imaginary trouble occupied in the patient’s mind for a long time a much more important place than the genuine organic trouble which accompanied it.
Bombardment; war strain; gassing?; collapse; arthritis: Hysterical MONOPLEGIA and ANESTHESIA of leg, interpreted as a “PROTECTIVE” reaction. Later, monoplegia and anesthesia of arm.
A corporal described as normal (“except for some shyness with the opposite sex”) adapted himself well to training and went to France in May, 1915, where he was at once thrown into 18 days of almost continuous bombardment. After some initial fright, he settled down to work well enough, but, when the weather got bad in September, 1915, grew tired of the situation. Bad dreams began (falling into a deep hole; being shelled). He thought of suicide, wanted a shell to incapacitate or kill him, began to have pains in the head, arms and legs, and was already groggy when a gas attack came. Whether he got a whiff of the gas or not, he at any rate felt giddy, got a swallow of water, and when the gas passed got out of his dugout in the open air. He was fatigued and much relieved when the company was ordered back. Now, however, he got shaky and fell in a collapse on a pile of straw, without, however, losing consciousness.
Apparently he had an attack of acute articular rheumatism. There was a sore throat and a pain in the head, radiating to left shoulder and to finger tips, with pain also in legs. The pain was worse in the right leg on moving the knee-joint. These pains lasted for a month in hospital. The leg had been like a log since the collapse on the pile of straw. Even after the pains left him a month later, the right leg was paralyzed and anesthetic. He walked with a crutch and developed a crutch palsy. After a month a hysterical paralysis of the right arm, with superficial anesthesia, supervened. During a period of eight months thereafter improvement was steady under reëducative measures.
According to MacCurdy’s analysis, the acute arthritis led to paralysis as a protective reaction. The paralyses are disabilities that would ensure absence from the front.
Lance-thrust in back, rapidly healed. Paralysis of right leg, disappearing with rest and exercises. Later, psychotic symptoms, with recovery.
N. H., 21, a laborer, industrious and sober (mother healthy, father insane and a suicide; patient somewhat sickly in childhood after pneumonia, a good scholar) volunteered at the outbreak of the war. Early in November he was on the Eastern front. November 17 to 22 he was in a number of small reconnoitring skirmishes almost daily, as a cavalryman. On the 22d, there was a clash with a Cossack patrol of far superior numbers. Eight German horsemen cut their way through, riding about 4 kilometers back to their squadron.
While dismounting, N. H. discovered that his back was wet. It occurred to him at once that he had been wounded. However, he successfully dismounted and then collapsed, feeling as if his right leg had fallen asleep. His companions found a wound in his back, which had come from a lance-thrust. The wound was bandaged. He was transported to Germany on a peasant’s wagon, the trip occupying six days, and on December 6 he came to the surgical clinic in Jena. The wound was insignificant and healed quickly.
The leg remained motionless, and on December 10 the patient was referred to the nerve hospital. He was a small, slenderly-built man, with poor nutrition, weighing 108 pounds. The scar, about 1 cm. long, alongside the thoracic vertebra, was still somewhat red and but slightly sensitive to pressure. Neurologically, the knee-jerks and Achilles jerks were greater on the right than on the left, and there was on the right side a distinct patella and ankle clonus. There was no Babinski reaction on either side.
The movements of the right leg were not of wide excursion, and flexion and extension of the knee and ankle-joints, while lying on the back, were slowly and hesitatingly performed, with an expression of pain, and with visible effort by the[327] quadriceps muscles. Flexion and extension of the toes were likewise difficult, and when the toes were stretched there was a distinct contraction of the tibialis anticus. Electrically the muscles were normal. On passive motion, there was slight spastic tension in the musculature of the right leg, and the patient said he felt marked pain. In walking, the right leg was moved with a limp and with the evident design of sparing it. The knee was imperfectly bent and the sole of the foot was dragged along the ground. There were short out-throwing movements of the lower leg.
Pain sense was normal, or possibly slightly in excess. There were painful points on pressure on the lower part of the os sacrum and coccyx and over the right sciatic and tibial nerves. Intelligence examination showed school knowledge to be extremely poor and calculation ability poor. Critical judgment and reasoning power were deficient. Memory and perception were without marked disturbance. The patient was dull and without interest in his surroundings. He complained that his right leg was as if dead and that he felt great pain in any attempt to move it. He also complained of pains at night in the region of the right shoulder and neck. His nerves, he said, had been very weak since his trip back from the front, during which trip he had been very cold and poorly cared for.
Treatment consisted of rest in bed, application of moist packs to the right leg, active and passive exercises of the right leg. After ten days he made his first independent attempts to walk, and active movements of the right leg in dorsal decubitus became unrestricted and painless. He remained somewhat unsteady in station, showing bilateral twitchings and movements of the right leg muscles. In walking the right leg was dragged behind in a spastic-paretic fashion. Appetite improved; spasms decreased; but at the end of December foot clonus was still persistent.
Upon January 10 there was an odd mental change. He became seclusive and suspicious. January 15 he expressed ideas of poisoning; his sister, he said, wanted to poison him, and others were watching him suspiciously; his room-mates were talking about him; in fact, he thought one[328] comrade was an Englishman. Sleep was poor. At the end of January, after a short period of improvement, he again had ideas of being poisoned, and had dream-like, unclear thoughts. His actions became incoherent: he would undress suddenly in the daytime and go to bed, getting up five minutes later and dressing. Senseless postcards were written.
This condition lasted a few days only, whereupon the mental and bodily condition greatly improved. Daily walks were then taken in the garden and in the city without exertion. The ankle-clonus on the right side was now decidedly weaker but did not entirely disappear. The muscle power on the right side was somewhat less than on the left.
The patient was very homesick, and on March 14 was sent home.
Shell-shock—six days later, crural monoplegia, cured by suggestion. “Metatraumatic” hysteria. HYPERSENSITIVE PHASE AFTER SHELL-SHOCK.
On August 13, 1915, a soldier was knocked unconscious by the explosion of a shell nearby. He woke up several hours later with headache, noises in the ears, itching, but no trace of paralysis.
Six days later, on August 19, he was released from hospital, still free from paralysis. On the railway journey he met some people of his district by whom he sent greetings to his wife, meanwhile becoming greatly excited. When he tried to get out of the train he noted a weakness of the left arm and left leg; this weakness somewhat quickly grew into a severe paralysis, so that when observed in Berlin the left leg was entirely paralyzed, not a single muscle of which could be moved when the patient was examined by Schuster one month after the accident. There was also a hypesthesia on the left side with total anesthesia of the left leg, which anesthesia was related stocking-wise to the hypesthesia of the trunk. There was tremor of the hands as well as generalized increase of reflexes. The plantar reflex, though weak, was flexor. The pulse rapidly ran up under excitement. In short, the patient seemed to be suffering from hysterical palsy. Waking suggestion did so well with the man that after three weeks normal sensibility was restored to the leg, and he could walk tolerably well without a cane.
The point of interest in this case is that the symptom of greatest importance, namely paralysis of the left leg, did not arise until six days after the shell explosion and then only after the man became excited by thoughts of his home and family through meeting his town people. The term metatraumatic is suggested by Schuster for cases of this sort. The emotions and stresses of war may be regarded as labilizing and sensibilizing the nervous system sometimes for months.
Wound of left foot: ACROCONTRACTURE. Psychoelectric cure, about seven months later, at one sitting, except for some residuals that cleared shortly afterwards.
A soldier, 21 years, was observed at the Centre Neuropsychiatrique, August 30, 1916. He had been wounded in battle, March 16, 1916, near the left internal malleolus. Infection followed and inguinal adenitis, for which he was in hospital a month.
Even before the abscess began, the foot had begun to twist inward. After the abscess had been cured, a contracture set in permanently, and at entrance to hospital was irreducible. The knee-jerk and Achilles jerk were more active on the side of the equinovarus contracture. There was even a slight amyotrophy of the calf. There was no appreciable vasomotor disorder. The foot and lower part of the leg were a little warmer on the left side.
Cure followed a single sitting with psychoelectric treatment, at least so far as the contracture went. Pain and swelling remained in the evening, followed by fatigue. The patient was discharged cured, October 12, 1916.
Hysterical pes equinovarus shows the foot immobile as if frozen (figé). The foot is extended with the toes lowered and the internal border incurved, as if revolved about the axis of the leg. The surface of the sole is directed inwards and much furrowed. The tendon of the tibialis anticus is very prominent. The internal malleolus is hardly visible, while the head of the astragalus is easily made out. No passive movement is possible and the tibiotarsal and mediotarsal joints are quite out of function. Upon palpation, the excessive contracture of the anterior muscles of the leg is striking. Upon request to move the foot, the foot is not moved, but muscles of the lower leg may contract, and even those of the thigh.
There were no sensory disorders in the present case, though they often do occur in this form of acrocontracture. It is doubtful whether the skin changes sometimes seen, such as hypothermia, hyperidrosis, cyanosis, and glossiness are due to circulatory disorder induced by the contracture or to the prolonged immobility. It has been proved by Meige, Benisty and Lévy, that even in a normal subject prolonged immobility may cause a difference of temperature of several degrees. Circulatory disorders sometimes cease immediately upon cessation of the contracture. Roussy and Lhermitte insist upon energetic and early treatment of these psychoneuropathic acrocontractures, which are apt to proceed less favorably than the acroparalyses. If not treated energetically and early, actual nerve, tendon, and bone lesions may ensue.
Shell-shock; shell-wound; emotion: Hysterical paraplegia. Approximate recovery.
A private of the First East Lancs could remember a shell’s bursting and striking a wagon near him when he was carrying food to the firing-line. He also thought a spare wagon wheel might have fallen on him. A period of unconsciousness of four or five days duration elapsed, on recovery from which he found himself suffering from a shell-wound in the left buttock, complete paralysis of both legs, and pain in the back, by the fourth lumbar vertebra. He thought that he had suffered from sphincteric paralysis for eleven days after the accident; but by September 25, there was no sign of this. Besides the paraplegia, there was complete loss of sensation below Poupart’s ligament in the right leg, reaching as high as the iliac crest behind; and an anesthesia of the left foot including heel and sole, with anesthesia to light touch throughout the limb (pin-pricks being appreciated in a normal way as far as the ankle); and there was an anesthesia to touch and pain in the ulnar distribution.
April 20, 1915, the patient was found to be a robust, somewhat microencephalic slowly cerebrating subject. Total flaccid paralysis of legs; right knee-jerk slightly exaggerated; no plantar response of any sort was obtainable. Right leg entirely anesthetic; left leg and both arms showed a diminution of sensibility; suggestion of glove and stocking anesthesia; trophic changes absent. The scar of the healed bullet-wound lay over the trunk of the left sciatic nerve.
It seems that the man’s companion had both his legs blown off at the time the shell burst. It is questionable whether the paraplegic patient actually saw the legs blown off, or merely heard about the accident. Another psychic feature lay in the fact that the patient had a paralyzed sister—a possible financial burden.
April 30, nitrous acid anesthesia. During the temporary rigidity, the legs were found to stiffen slightly; the legs were[333] flexed. Upon the return of consciousness, the patient was told that the legs had moved during anesthesia, and was asked to place them in a more convenient position. The thighs moved slightly, and throughout the day movements were encouraged against resistance.
The next day he was gradually raised to the vertical position and supported upright. But at this stage he had become mentally resistant and resentful. During the day the upright position was at intervals resumed, and the patient was made to walk between two attendants. The next day he walked alone and his mental resistance had broken down. There was no longer any evidence of exhaustion and effort in the movements, and the patient began to take pleasure in his recovery.
Improvement was progressive. A pronounced hysterical element persisted, encouraged by the perpetual attentions of visitors. When discharged, there was a slight hemi-anesthesia throughout the right side, and a doubtful patch of anesthesia on the dorsum of the foot, sole, and plantar surface of the heel.
Shell-shock; burial; flexion of spine: Paraplegia.
A reservist, 34, formerly army instructor in gymnastics, a member of the 1st Battalion King’s Royal Rifles, was subject to injury from the bursting of a “Black Maria” on his trench. He was sitting with bent back in his shelter, with legs fully extended. He was in a small dug-out, a recess excavated under the earth backward from a narrow trench and not timbered. The “Black Maria” burst and covered him up to the chin in a heavy clay soil. After building up the breach twenty minutes later, his comrades dug him out.
He had received on his body the violent impact of the mass of earth pushed laterally from the crater excavated by the bursting of the shell. Accordingly his vertebral column was forcibly flexed, its ligaments were stretched, and hemorrhages were produced in the great muscles of the back. As the twelfth thoracic vertebra is the weakest spot in the spine, the roots of the cauda equina opposite this weak spot were probably injured. Such accidents are met in mines.
The legs were powerless and numb. There was nausea, no vomiting, no gas, no dizziness or trouble in the head, not even pain in the small of the back. The accident had occurred at 8 A.M. Upon nightfall, he was removed on a stretcher to the field hospital, arriving at the base hospital four days later; and on the fifth day power began to return to the legs. Knees, ankles, and toes would move slightly November 6, though passive movements of the legs caused pain in the back. The deep reflexes were weak, the plantar reflexes flexor. The left cremasteric reflex was weaker than the right. Impairment of sensation was slight in both extremities, but the left leg was a little more numb than the right. The left lower abdominal reflex was lost. A band of hyperalgesia corresponded with the left eleventh and twelfth thoracic segments November 12, slight reflex disorders and some degree of paresis of the legs.
Shell explosion: Paraplegia; sensory symptoms.
A lieutenant, 23, came to the ambulance September 15, 1914, having the morning before been to the firing-line with his company and thrown to the ground on his back by the explosion of a shell which he had seen falling behind him. He had not lost consciousness, but was unable to rise. After a night in the relief post, he was brought by automobile 12 kilometers to the ambulance. He complained of pain in the back, though no wound or ecchymosis could be found there, nor any painfulness of spinous processes or irregularity of bone. He had not emptied the bladder from the time of the shock. Preparations were made to catheterize on the morning of the 16th, when the patient after effort became able to micturate. There was crural paraplegia such that he could not sit or walk even when supported. Lying down, he could move his legs slightly sidewise. Anesthesia to pin-prick and temperature was complete to the groin; but tactile anesthesia was found only in the sacral root territory, namely in the feet, the outer aspect of the legs, the posterior surface of the thighs, and the scrotum. There was loss of sense of position for the toes. The plantar reflexes were abolished; but there were no other reflex disorders; nor was there any evidence of other disorder.
September 20, the man was evacuated by sanitary train in the same status as at entry. January 27, 1915, the patient could walk on crutches, supporting himself in part on the left leg. The lumbar pain had largely disappeared.
Hurst regarded this case as one of organic origin due to commotio spinalis.
Wet, cold, heavy marching; leg pains, rheumatic; no other somatic factor or any emotional factor discoverable: Transient paraplegia; two months after period of exposure, brachial tremor, hysterical. Recovery incomplete.
A German soldier, 34 (non-alcoholic; married, father of five healthy children; on military service 1901-3; regarded as a very good soldier; father alcoholic), got bad leg pains from wet and cold in West front trenches September 8-13, 1914. Still he was able to march some 30 kilometers. But two days later (he had lain down in wet clothes in a barn), his legs became quite immobile. He was in a reserve hospital from November 3. The rheumatism disappeared, and suddenly, early in the morning of November 8, when he was washing, a lively tremor and shaking of the right arm set in.
Examination at Jena January 30, 1915, showed no special physical disorder. The sense of touch was slightly diminished on the right side; the pain sense was normal; movements were free. While at rest there was a continuous shaking tremor of the right arm and hand, which consisted of very rapid pronations and supinations, and shaking movements of the upper arm. At times the tremor would completely cease, and when attention was diverted the tremor became slighter or quite disappeared. The tremor increased when it was talked about in the man’s presence. The left grip was stronger than the right.
January 31, after he had been in bed one day and treated with moist packs, the shaking suddenly ceased. He then complained only of mild pains in the right shoulder and wanted to get up.
February 23, he was given three days’ home leave, which he stood very well. He now began to take part in the medical gymnastic work, but complained afterwards of more pains in right shoulder and arm. There was a lapse into the[337] shaking tremor, which lasted with varying intensity for several weeks. Loud noises or calling made it worse.
Hypnotism and suggestive treatment of the tremor were without effect March 25. March 26, on passive extension of the right arm, patient complained of pain in shoulder and arm. Next day the tremors were more marked, but March 29, the tremors suddenly stopped altogether. April 4, the pains stopped never to return. April 15, he was given leave to go home for spring farm work.
Four weeks later he returned, sparing his right arm, which he held stiffly beside his body when walking. If he let the arm hang free in walking, rhythmical movements in it began. He complained of painful involuntary contractions in the right arm even when in complete rest. Nor did the condition afterward essentially change; the patient went home at the beginning of July.
The remarkable feature of this case is the complete lack of any emotional shock. The total genesis seems to have consisted in the prolonged exposure to wet and cold, and the heavy marching. The tremors, limited to the right upper extremity, occurred without any demonstrable psychic or bodily trouble, and set in after the disappearance of the so-called rheumatic disorder. Although there is no one psychogenic factor to single out, the psychic influencibility of the case is unmistakable; moreover, the incompleteness of the cure is doubtless, according to Binswanger, a matter of the imperfect suggestive therapy employed.
Fever patient watches barrage coming: unconsciousness, paraplegia: recovery.
A lieutenant was lying with fever in a farmhouse in upper Alsace, watching from his window the shelling of a battery about 400 meters away. He saw that the enemy was to reach the farm with shell in due course of time. The shells came nearer, say up to about 100 meters, and the lieutenant was able to reckon closely when he would be reached. He was quite defenseless and unable to get to safety. At the very moment, he thinks, when the shells began to strike the house, the lieutenant lost consciousness from fear. He was unconscious an hour before being carried to the cellar. The shelling lasted several hours more. Immediately upon coming to the patient found that, although he bore no external wound, both legs and the right arm were paralyzed.
There were never any signs of organic disorder. The patient recovered completely with purely suggestive treatment.
Incentives to paraplegia.
A young Canadian paid $150 to have his teeth repaired to be accepted for service and then married. The wife became pregnant. He reported sick after falling out on a route march in a heavy rainstorm. The medical officer said he had weak feet and ankles. He lay around the huts, was excused duty, and got worse in the wet and cold. He was admitted to hospital and came to Russel’s wards on a stretcher showing paralysis of both legs with slight power of movement at the knee. Stroking anesthesia to pin prick from the knee down. Reflexes not abnormal. He walked back upstairs!
According to Russel the wife’s pregnancy had furnished a sufficient incentive, and the M. O.’s suggestion had fallen on fertile soil.
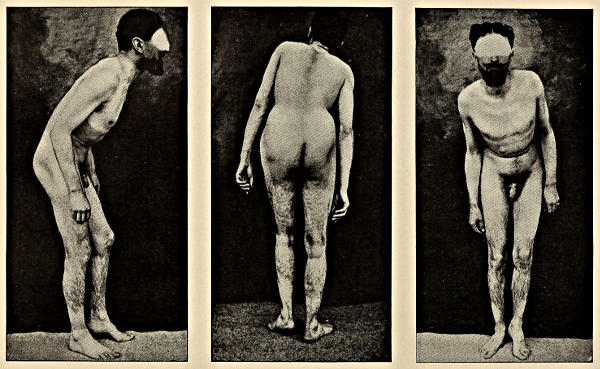
WOUNDED SEPTEMBER 3, 1914. THROWN INTO AIR BY SHELL-BURST; UNCONSCIOUS. FEBRUARY, 1915: PLASTER JACKET, 3 WEEKS; SECOND JACKET, 3 WEEKS. CURED. SENT TO GRAND-PALAIS.
Bullet wound of back: Hysterical bent-back—camptocormia.
A man was wounded September 6, 1914, by a bullet that entered along the axillary border of the scapula and emerged near the spine. He spat blood for several days; but the skin wounds quickly healed.
When he got up, his trunk and thighs were found to be in a state of moderate flexion upon the pelvis, the trunk being bent almost at a right angle; the legs were flexed somewhat upon the thighs. The man could not voluntarily extend his trunk, but he could extend his thighs to a moderate degree. He could bend his trunk still further forward than its habitual contractured position, being able to pick up an object from the ground. If the man was put in the ventral position, the trunk could be straightened to a considerable degree. Curiously enough, the man felt no pain, nor had there been any pain since the healing of the wound. No motor, sensory, reflex, trophic, vasomotor, electrical, visceral, or X-ray disorders could be found. It was evident that there was a contraction of the muscles of the abdominal wall and of the iliopsoas, yet it was also clear that these muscles were not contractured on account of the subject’s ability to flex his trunk and to extend his thighs.
Here, then, is a vicious attitude crystallized (in the phrase of Souques) in the form of a pseudocontracture.
Blown up by shell; unconsciousness: Camptocormia (bent-back, “cintrage”). Cure by corsets.
Camptocormia with antero lateral bending is described by Roussy and Lhermitte in an infantryman observed at Villejuif, February, 1915, after having been wounded September 3, 1914. The infantryman had been thrown into the air by the bursting of a shell, had lost consciousness, and came to with violent pains in the back. The trunk was found to be bent strongly forward and to the right side, and remained in this position thereafter. There was no evidence of wound.
In February, 1916, a plaster corset was applied by Souques, which brought the patient partly to normal station in three weeks. The trunk was now no longer bent forward, but was still bent to the right. A second corset was applied for three more weeks, with which the patient became absolutely straightened out again. He was discharged cured and sent to the Grand-Palais for the reëducation course.
This condition is a form of trunk contracture in the nature of a kyphosis (scoliotic and lordotic forms of contracture are also found in the hysterical group), for which the terms plicature of trunk, traumatic kyphosis, pseudo-spondylitis, and camptocormia have been in use. The term camptocormia has been proposed by Souques and Rosanoff-Saloff. The poilus speak of the condition as cintrage (arching). In these cases the trunk is held almost horizontally, with the head in hypertension and neck muscles and thyroid cartilage jutting. The patient looks fixedly straight forward, with eyes wide open, and carries his legs extended or half flexed. The normal folds of the abdominal wall are very deeply marked, and at the level of the groins, the epigastrium and the pubis, there are deep folds. Viewed from behind, the median lumbar fold has disappeared or is faintly marked, as are the sacro-lumbar and other masses of spinal muscles. The whole lumbar region is elongated and flattened. The dorsal[341] spines of the back are accentuated; the buttocks are flattened and broadened transversely. The back of the neck is marked by deep transverse folds, and the seventh spine does not stand out. The patient can walk perfectly, though sometimes there is a pseudocoxalgia and lameness. Attempts to straighten the body lead to visible forcible contractions of various muscles, but the kyphosis remains persistent. There is a sense of active resistance on the part of the patient, which can be demonstrated by palpation. If an active attempt at straightening is made, lumbar or sacral pain develops, followed by a very lively and emotional state of anxiety on the part of the patient, with interrupted and accelerated breathing, an expression of terror in the face, and a rapid pulse. The patient then subsides into his earlier attitude, and his anxiety disappears in a few seconds. It is much easier in many subjects to reduce the camptocormia in the position of dorsal decubitus than upright.
Burial after shell explosion; lumbar ecchymoses; regionary pains; camptocormia, 5½ months. Cure by three months’ plaster cast about trunk.
An infantryman was buried after shell explosion August 25, 1914, but he sustained no wound or bone injury. There was, however, a large ecchymosis of the lumbar region, and he had felt violent lumbar pains. The trunk was carried flexed, symmetrically bent over and quite incapable of being straightened completely. A plaster corset was applied March 16 by Souques. Three months of this was followed by a complete straightening, which lasted after the corset was removed. The patient was discharged well.
As to these cases of camptocormia, some authors regard them as due to anatomical changes in the vertebral column itself, or in the ligaments and muscles, and accordingly regard the condition as a form of spondylitis, syndesmitis, or psoitis. This view is held by Sicard, who bases the idea upon the local pains and the results of cerebrospinal fluid examination. According to Roussy and Lhermitte, hyperalbuminosis of the fluid is extremely rare, and one case of their own with hyperalbuminosis was nevertheless cured with great rapidity. Roussy and Lhermitte even inquire whether the fluid albumin may not be due in some way to an interference with venous and lymphatic circulation.
In some cases, this condition may be at first a response to pain, a pseudospondylitis dolorosa, such as may be sometimes observed in hospitals near the front. Later, however, the suffering in camptocormia is due more to the abnormal position of the trunk, with strain upon vertebral ligaments, than to the persistence of any original pain. Moreover, these patients recover almost immediately from their pains when the contraction is relieved.
In differential diagnosis, one has to consider, according to Roussy and Lhermitte, Pott’s disease, traumatic spondylitis, as well as Bechterew’s vertebral ankylosis, Pierre Mari[343]e’s rhizomelic spondylosis, Kocher’s intervertebral disc contusions, and Schuster’s myogenic ankylosis of the vertebral column; but in Pott’s disease, the fixed pain points, rigidity of column, fluid examination, and signs of myelitis, should suffice for the differential diagnosis. Traumatic spondylitis follows the contusion after months and after a phase of neuralgia. Ankyloses do not so much concern the trunk as the vertebral column itself; disc contusion produces disorders in standing and gait as well as pains and edema. Schuster’s disease shows paresis, hyper reflexia, and amyotrophy not shown in camptocormia.
Shell explosion; partial burial; forcible flexion of spine. Paraplegia, cured by suggestion. Then camptocormia, also cured.
An infantryman in the Côte du Poivre was sitting on the ground in the opening of a dugout eating soup, when a shell burst and the roof of the sap fell in on him. The planks and the stonework fell heavily on the dorsolumbar region. The patient was almost bent in two, head to knees, legs buried, hardly able to breathe. He did not lose consciousness and cried out, feeling for a moment very anxious and fearful that his comrades had left. Only two hours later was it possible to dig him out. He said he had been absolutely unable to make any movement, had kept his body bent, and felt violent pains in the back. He was carried back twelve hours later and reached the dressing station in eight more hours, eventually reaching the neurological service two days and a half after the accident. On entrance he was prostrated, complained of lumbar pains and of inability to move, and was able to make only a few contractions on the left side when asked to try. The right leg was flaccid. The left knee-jerk was stronger than the right. Other reflexes normal. Hyperesthesia to pin prick on the right side. Slight saddle hypesthesia, reaching to the iliac crests above and perineum below with preservation of touch sensation. Slight forward posture of vertebral column. The patient complained of pain on pressure of the spinal processes and the lumbar spine. There was slight ecchymosis about the left iliac crest.
Lumbar puncture showed clear fluid without hypertension, in which were a few lymphocytes. There was a large amount of albumin. The blood pressure was normal. There had been a slight diarrhea following the accident which disappeared on entrance to the hospital. The question was raised whether the case was one of slight hematomyelia or was pithiatic.
Suggestive therapy was tried, and liquid was injected into the muscles of the lumbar region and the posterior surfaces[345] of the thighs. In a quarter of an hour the patient found himself able to raise the foot above the bed. There remained an extensor paralysis of the right leg. When the patient was made to raise the foot he began to show the phenomenon of Souques, called camptocormia. He could walk, nevertheless, and took a few steps sustaining the weight of his body by placing his arms on his thighs. Though he complained of lumbar pain, it was finally possible for him to pick up an object from the ground and lean sidewise. He could not, however, stand up. Yet when the patient was made to lie down, his back was spontaneously straightened. Treatment of the camptocormia was also successful.
Astasia-abasia: Two cases from (a) thigh wound, and (b) shell-shock and wound of thorax. Cures by faradism.
An infantryman was wounded September 23, 1914, by a bullet in the anterior and middle part of the left thigh. From the moment of the trauma, he had not been able to walk, but gradually regained his ability to stand, and then to walk. He was returned to the front (January, 1915).
Slightly wounded again in the neck, January 6, 1915, he was evacuated and operated on. After the operation he could neither walk nor stand. His reflexes were normal; he could perform all movements when lying down, although the movements were executed very slowly. As soon as he could sit upright, he was taken with tremors and could not hold himself in a vertical standing position, nor take a single step. If he was given crutches, he dragged the two legs.
Under the influence of electric treatment—a mild faradic current—he was cured at a sitting so that he could both stand and walk (March, 1916).
Astasia-abasia after shell explosion occurred in an infantryman observed by Roussy and Lhermitte at Villejuif, July 8, 1915.
The patient had been wounded September, 1914. The wound was a superficial one in the thoracic wall, under the right nipple. He had been cast into a very deep shell hole, but had been able to get back to the aid station alone, taking very short steps only.
As soon as he reached the station, his gait became spastic, trembling and hesitant. Given two canes, he could walk painfully, trembling. At each step, he would balance his body back and forth. He gave the impression of a man drawing some sort of vehicle, who had to make a considerable effort at each step.
The faradic treatment cured this patient at one sitting.
War strain; fall into water-filled trench: Dysbasia, tremors, vasomotor disorders. Cure by hypnosis. Case to demonstrate “traumatic” hysteria WITHOUT somatic TRAUMA.
An artilleryman (without hereditary or acquired neuropathic taint) underwent much stress and strain in the war in Belgium, Lorraine and Flanders. One night, on leaving his observation post, he fell into a trench filled with water. He felt pricks in the groin and gradually developed a pseudospastic tremor of the lower extremity, paraparesis inferior, depression, irritability, pressure sensations in the head, and sleeplessness. He passed through three hospitals before arriving at Hamburg and received the diagnosis of concussion of the brain and cord.
Nonne found an emotional state of depression with hypochondriacal fear, disturbance of sleep, deficient appetite, constipation and pollakisuria. He walked upon two crutches, dragging his legs inertly after him. There was marked cyanosis, lowered temperature and hyperidrosis of the feet and lower legs; exaggeration of tendon and skin reflexes and pseudoclonus; no Babinski or Oppenheim reaction. There was anesthesia of the lower extremities and of trunk as high as the ribs. Pulse 130. Visual fields normal. Sensory disorders absent.
After the first hypnotic treatment the patient was able to stand and take a number of steps, and the tremor gradually diminished. After two treatments standing became normal and walking was much improved, the tremor ceased, cyanosis and hyperidrosis disappeared, and the movements of the bowels and urination became normal. Thereafter the patient had no attention paid to him deliberately and in a week’s time became well.
Here is a case in which, as Nonne states, the somatic trauma required by Oppenheim as the basis of every traumatic neurosis did not occur. Moreover, the sudden cures[348] by hypnotism, or by any other method in these cases, warrant us in supposing that there are no such fine molecular changes as Oppenheim and von Sarbo assert. Such experience as the cures in this group of cases confirms, according to Nonne, the surprising result first achieved in this war (Bonhoeffer, Wagner von Jauregg, Karplus, Wollenberg, Westphal) that the most severe neuroses produced by somatic and psychic traumata can be cured in an astoundingly rapid manner without residuals.
Re the controversy over Oppenheim’s traumatic neurosis, Nonne holds with the Charcot school that traumatic neurosis is clinically identical with hysteria. Oppenheim admits the part played by psychogenesis, but has always laid a greater emphasis upon the actual injury of the neuronic apparatus in which he believes. He thinks that small hemorrhages, inflammatory processes, and degenerative processes affect the neurones unfavorably, and permit the psychogenic effects to occur more readily. Of course the insurance-company attitude and the attitude of railway corporations saw malingering in all cases, and to this day, neurologists are inclined to see a great deal of “indemnity neurosis” in these cases. Opposed to the corporation men and the neurologists were the psychiatrists, who chiefly upheld an emotional theory of genesis—whence we began to hear of the neuroses of fright and of accident.
Oppenheim claims to have established with war cases the fact that an entirely normal person without heredity and without antebellum acquired soil, may develop a neurosis through war stress. Oppenheim concedes that there may be purely psychic cases, but holds that there are nevertheless, numerous purely physical cases and a great number of cases of a compound nature, which are both physical and psychical in their etiology. Oppenheim’s point is not that every single symptom described may not be upon occasion psychogenic, but that the data of this war prove that neuronic injury, particularly injury of the peripheral neurones, can also produce these effects. Nonne, Forster, Lewandowsky, and others, opposed Oppenheim’s views vehemently. See especially comments by Zeehandelaar.
Shell-shock; BURIAL HEAD DOWN: Brachial monoplegia, head-shaking, speech disorder, corneal and conjunctival reflexes absent. Determination of hysterical phenomena to parts buried.
A Russian private was buried after a shell explosion, September 13, 1915, head down, so that only his legs stuck out of the débris. Afterward his right hand refused to move, and there was edema of the right wrist, with pain referred to the shoulder joint. The head shook and made jerky movements during the day, but ceased them in sleep. Speech was retarded; words were uttered clearly enough but in a sing-song fashion; sometimes the man stammered. Hearing was diminished in the right ear. Pupillary responses were lively, but the swallowing reflexes were diminished, and the corneal and conjunctival reflexes were absent. The tendon reflexes were lively on both sides. There were no pathological reflexes.
At the end of October—six weeks later—the patient was sent home on convalescence for three months, and improved rapidly after a short time in family surroundings. He was examined again, two months after discharge, and found normal in all respects. He returned to the ranks.
Re Shell-shock in Russians, Arinstein concludes that concussion hysteria may occur in a perfectly normal person, yet be innocent of all organic signs indicating destruction of peripheral or central neurones. Rifle or machine-gun fire had not in his experience brought about concussion hysteria, which was invariably due to the bursting of a large projectile. With reference to Schuster’s remark that a sleeping man never acquires hysteria from the bursting of a shell near by, Arinstein confirms Schuster, finding amongst 2000 cases no instance in a soldier sleeping at the time the shell burst.
Re effects of cannonading, Gerver reports Russian instances of a kind of hysterical clavus, or sensation of a nail being driven into the back of the head, in men who have been a number of days under stiff shelling.
Multiple wounds and bullet wound of palm: ACROPARALYSIS. Cure, five months.
A patient was observed at Villejuif, February 5, 1915. He had been wounded, January 2, 1915, and showed scars of a bayonet wound on the anterior surface of the right thigh, of a lance wound on the dorsal surface of the right foot, and of a bullet wound in the palm of the left hand.
There was left wrist drop with fingers extended. On the sensory side, there was a glove anesthesia and analgesia up to the bend of the elbow. The right leg showed a paresis and contracture, but there were no sensory disorders in the legs. Reflexes were normal. The patient was discharged cured, in May, 1915 (psychoelectric method).
This is an example of the so-called acroparalyses, paralyses limited to the hand or foot, many of which have developed in this war, after grazing wounds or more severe injury. More rarely they appear as if spontaneously. Sometimes they are preceded by slight arthralgia or vague pains.
The condition in the hand suggests a radial paralysis. The patient is unable to flex his fingers, though he probably is able to make some movements with his thumb. Sometimes, on request to move the hand, a series of coarse oscillations follows, somewhat like a tremor. These oscillations are, according to Roussy and Lhermitte, apparently pathognomonic, and depend upon the contraction of the muscles antagonistic to those whose movement has been requested. These antagonistic muscles, themselves entirely incapable of voluntary movement, are seen to be contracting effectively and jerkily to meet the action of the agonists, also seen making jerky movements. If the forearm is moved passively and rapidly, the hand flops about inert, like the hand of a marionette, although not to the degree of hypotonia in organic paralysis. The hand is often cold, moist, and cyanotic, and even possibly analgesic and hypesthetic.
Bullet wound of arm: Apparent radial paralysis, not resolved by self-preservative swimming movements. Paralysis actually hysterical.
A professional acrobat, 22, Corporal in an African Chasseur regiment, was rather instructively tattooed and had apparently performed some of his service in disciplinary companies. In short, one might have a legitimate suspicion of the objective value of any manifestations he might present. However, one of his chiefs had written a favorable letter concerning his services. He had had various crises of a hysterical character since adolescence, and there was alcoholism in the family.
He was wounded May 4, 1915, by a bullet which passed through the outer and lower part of the right upper arm, and thereafter the forearm and hand became completely inert, both for flexion and extension. There was a considerable hyperesthesia. The wound healed quickly, without complications.
August 5, about 10 o’clock at night, the man—then at his dépôt—tried to commit suicide (motive not related with the war). He threw himself into the Rhône from a height, where the water was deep and the current rapid. His brother and a comrade, who knew that he was going to make the attempt, saved him. Chartier himself happened to see the whole scene, and noted that throughout the affair the forearm and hand of the patient remained inert. It seemed as if there was a radial paralysis. This was the more likely as the man had been wounded in the arm. First care was given. The man had not known of Chartier’s presence. He had been under water about two minutes.
From hospital he was evacuated three weeks later with a diagnosis of radial paralysis, coming on service September 11. Examination showed a slight paralysis of the extensors and flexors of hand and fingers, and of the hand muscles. There was also a slight contracture of these muscles, more marked in[352] the flexors. There was pain upon reduction, with some jerking of the muscles. Electrical reactions proved normal in nerves and muscles. There was a segmentary anesthesia to pin prick, reaching to the level of the elbow; deep hyperesthesia of the finger joints. There was no trophic or vasomotor disorder.
In short, here was a case of functional paralysis with contracture of the right hand, to be regarded as hysterical in the classical sense of the term, both by reason of the anesthesia and absence of trophic disorder, and on account of the hysterical history of the patient. Functional reëducative treatment quickly improved the paralysis, so that two weeks later the patient was able to extend fingers and hand. His total recovery was hoped for, when, September 26, wishing to get out of the hospital without leave, the patient jumped from a window and broke his right leg. The functional paralysis of the hand persisted and even grew more marked.
The interesting point in this case is that despite the powerful nature of instinctive efforts with drowning persons, this patient, subject to an hysterical arm paralysis, did not make defensive movements with the paralyzed arm; yet this paralysis was such as to be greatly improved by psychotherapy.
Bullet wound in brachial plexus region: SUPINATOR LONGUS CONTRACTURE, hysterical-looking. Callus of fractured rib probably at fault: Treatment surgical.
A man was wounded, December 21, 1914, by a bullet which entered about the middle of the spinous process of the left scapula and was extracted a few days later from the posterior border of the sternocleidomastoid muscle, two finger-breadths from the left clavicle, that is, at about Erb’s point. The left upper extremity was inert for ten days, but then began to move again, although extension and flexion of the fingers did not begin at once.
October, 1915, movements were normal, except those of extension of the forearm, due to contracture of the supinator longus muscle, a contracture that had developed about three weeks after the wound and stood out along the external border of the forearm, almost suggesting a musculotendinous retraction. There was a palpable, hard callus of a fractured rib, presumably a cause of the permanent irritation of the supinator longus, being precisely at the point where lesions usually produce superior brachial plexus palsy.
Why should the supinator longus alone of the Duchenne-Erb group be affected? Perhaps a single root was involved in the irritative lesion. The biceps showed also a partial R. D. The deltoid was normal electrically and in contraction.
The treatment planned for this case of isolated contracture of the supinator longus was surgical operation of the irritative focus. According to Léri and Roger, it is sometimes dangerous to use such measures as massage and electric baths for a paralyzed limb, since the massage or electricity excite not only the affected muscles, but also the other sound muscles,—muscles that are already more powerful than the paralyzed muscles and may go into antagonistic contracture. Even in limited galvanization, it is desirable to work with weak currents, so as not to diffuse the current into non-paralyzed muscles. In case of radial or sciatic paralysis,[354] apparatus permitting the extremities to rest without over-action of the muscles antagonistic to the paralyzed ones may well be applied.
We here deal with a case, therefore, which looked purely functional, but in which careful examination and X-ray served to show an organic focus of irritation.
Re nerve concussion, Tubby offers the following definition: Nerve concussion is damage to a nerve trunk without actual destruction of the axis cylinders. The damage may consist of an effusion of blood between the nerve fibres following compression of a nerve against the bone by rapid passage of a foreign body near the nerve. Sometimes, however, the lesion which causes damage to the nerve trunk without actual destruction to the axis cylinders is nothing more than a temporary anemia or hyperemia. In most instances, both motor and sensory function are together interfered with, but in the case of large nerve trunks, e.g., the popliteal, there may be a separate concussion of motor or sensory bundles.
Contusion may effect a sort of STUPEFACTION OF MUSCLE and paralyze it by a non-psychic process: The SYNERGY in contraction of biceps and supinator longus is thus SPLIT. Biceps restored to synergy with the supinator by massage and faradism.
A man was wounded at about the middle of his biceps and three weeks later was found to be able to flex the forearm only by means of the supinator longus. The biceps remained absolutely flaccid and soft, so that the diagnosis of a lesion of the musculocutaneous nerve (unlikely as this seemed on account of the low site of the wound) was entertained.
However, the biceps and the musculocutaneous nerve proved electrically normal. In short, this paralysis of biceps was functional in nature. But, according to Tinel, there could be no voluntary suggestive or hysterical element in such a paralysis, since flexion of the forearm is normally produced by a synergic contraction of biceps and supinator longus that cannot be separated voluntarily.
Treatment by massage and rhythmic faradization caused the biceps function to return to normal, so that voluntary synergic contractions of the biceps took place along with those of the supinator longus.
We here deal, according to Tinel, with a genuine functional paralysis, nonhysterical—a paralysis due to a kind of stupor of the muscle. Such paralyses due to muscular stupor ought to get well in a few days or weeks. Should they persist, it is clear that a stuporous paralysis might be transformed into a hysterical paralysis. In short, the direct contusion of a muscle or group of muscles may be the point of departure for various persistent paralyses.
Wound of arm: Blocking of impulses to certain hand movements. Recovery with splint.
A private was wounded by a shell fragment, September 16, 1914, and admitted to the London General Hospital, September 27. A high-velocity shell fragment had passed through the soft parts of the left arm at a spot exactly corresponding to the musculospiral groove. He could extend the middle finger of the left hand, but the other fingers were held in flexion. The last two phalanges of index finger could not be moved, it was found, on account of severance of the extensor tendon some years previously. Accordingly, the loss of function due to the shell injury was that of thumb, ring, and little fingers. Supination could not be executed completely to the extent of 15 degrees; there was no R. D. upon electrical test, October 2. The sensation of affected fingers was woolly. November 3, the little finger had recovered, but supination could not be completely executed.
The treatment consisted in a bent malleable iron splint, with the wrist and affected fingers hyperextended. November 20 all power had returned with full supination, except for the two phalanges of index finger previously injured.
Major Tubby thinks this a case of physiological blocking, as from a small hemorrhage amongst the fibers or around the nerve.
Re inhibition, Myers thinks it is the functional cause of the effects of shell-shock. He thinks it is not a fixation of the idea of the paralysis of volition, but that it is a fixation of the process of inhibition itself that produces the effects we see in Shell-shock. It is a block of ascending paths that produces the anaesthesia so characteristic of Shell-shock. It is a blocking of sensory paths that produces mutism or aphonia. But according to Myers, there is also a block in certain cases of descending paths that control and coördinate various mechanisms. The result of a block in the descending paths is shown in spastic, clonic, or ataxic phenomena of, e.g., functional dysarthria. See also Case 253 (Tinel).
Eight months of war experience (often under heavy fire) without reaction; then, shell-shock; unconsciousness: Right hemiparesis; pain in the left side of head; heat sensations of right half of body; diminution of hearing in left ear; a variety of asymmetrical bilateral phenomena.
A Russian private, 24, sustained shell-shock April 14, 1915. He was observed, when the shell burst, to crouch down, and then to fall to the ground, unconscious. The unconsciousness lasted about two days, after which he was found to be oriented, though slow and stammering of speech, hardly able to concentrate attention or sustain a conversation, and giving the impression of a man stunned. There was difficulty in the expression of thoughts, and a marked over-fatigueability. After adding and subtracting accurately two-digit figures for a time, the man quickly grew confused and said that trying to solve such a problem made him dizzy.
His imagination was filled with gunshots, shell-bursts, and the killing of comrades, and during any conversation the man frequently shuddered. Concerning the shell-shock, he remembered only that a number of shells had burst near him and that he came to in the hospital. He kept looking to one side and to a distance, as if listening, sometimes bending his head downwards. He would cry and sigh during conversation, and then be quite unable to explain why. He said there were loud noises in his ears, and that his head and the whole right side of his body felt hot. Pain was felt in the left side of the head. The right hand and the right foot were weak (on distraction, this hemiparesis remained unaltered). Tremors affected all the extremities. He had a sensation, possibly hallucinatory, of the creeping of insects on his skin. The hearing of the left ear was objectively diminished. There was palpitation of the heart and difficulty of breathing. Tendency to Romberg. There was a general hypalgesia, more marked on the left side of the body. Both conjunctival[358] reflexes were diminished. Knee-jerks and Achilles jerks were exaggerated. All the reflexes on the right side were livelier than on the left. There was a moderate Babinski reaction on the right side. Mechanical over-excitability of muscles. Dermatographia. Both sides of the skull were sensitive on tapping, but especially the left side. Mannkopf sign on pressure of the left side of the cranium.
Hemorrhagic points without injury to the skin were noted on the skin of the left hand and foot. Speech was stammering. There was a marked digital tremor, sometimes spreading to the rest of the body during examination. The muscles of the face, eyelids, and tongue showed sharp fibrillary twitching. The pulse stood at 100 and frequently missed beats. Battle hallucinations, visual and auditory, sometimes occurred, the commands of superiors and the noise of guns, rifles, yelling, and groans; the man would see trenches or redoubts, or a field full of wounded soldiers or attacking columns of the enemy. He recognized the hallucinations as such. His sleep was troubled by nightmares of the same general description.
For eight months the man had been in action at the front, under heavy gun and rifle fire. He was a courageous man, who had never felt fear, regarding himself as used to battle and the bursting of shells. He had not been wounded. The entire situation seems to have developed after the single shell burst of April 14, 1915.
LOCALIZATION OF SHELL-SHOCK SYMPTOMS: Hemiparesis and hemianalgesia on side of body exposed to explosion; contralateral irritative symptoms of face and tongue.
A soldier had a shell explode to his right, October 23, 1914. He declared that the concussion launched him through the air. When he recovered consciousness three hours later, he lay in a bog and was unable to move either leg. Gradual improvement followed. The symptoms were sensations of formication in the legs, pain in the back, blurred sight, hardness of hearing, disturbance of speech, headache, vertigo, weak memory. After a fortnight weakness in right arm.
He was admitted to hospital a week after the injury, unable to walk, restless, given to palpitation and attacks of anxiety. On attempts to walk, leg spasms and tachycardia.
Transferred to nerve hospital, December 2. Sleep poor, uneasy with dreams. Tic on left side of face. On opening the mouth, left-sided faciolingual spasm. Paresis of right arm. At first, right-sided ankle-clonus and paresis of leg. Knee-jerks increased. Speech hesitating. Right hemianalgesia. Concentric contraction of visual fields. Tachycardia (120). In walking the right arm failed to swing normally. Attacks of vertigo, with falling. Patient got up at night and pushed against objects in his room.
There was only slight improvement while under observation. He became psychically more frank and even talkative, and was moving more readily when transferred.
Re Oppenheim’s conception of the strongly peripheral element in traumatic neurosis, he sums up by saying that a traumatism attacking the organism at its periphery is in line to produce a neurosis without any psychic mediation whatever. The rôle of the psychic process, in Oppenheim’s view, is contributory to the fixation of neuroses. Even when there is a free interval betwixt shell burst and neurosis, still there are physical effects of trauma upon neurones.
Shell-shock; unconsciousness; after improvement in symptoms (4 months) return to trenches; more symptoms after 5 days: Sensory disorders, especially on left side (the side more exposed to explosion); exaggerated reflexes on right side with slight clonus and with Babinski sign. Improvement.
A Russian Captain, 45 (heredity good; non-alcoholic, non-syphilitic; always in good health) sustained shell-shock in a battle in southeastern Prussia, August 13, 1914, and was unconscious for two days. He was carried to one of the provisional field hospitals, and then evacuated to Petrograd, where during a period of four months, he was given electricity, suggestion, and baths. He was feeling so much better in December, 1914, that he went back to the front and headed his company in the trenches. He stood only five days of trench work, and was sent for mental examination December 29, 1914.
The captain was of middle height, well developed but poorly nourished, of a dejected and preoccupied appearance, looking to one side in conversation, and finding difficulty in the expression of his thoughts. He talked almost exclusively of his illness. He found difficulty in adding or subtracting 2-digit figures. He seemed to have amentia, frequently being mistaken as to the most important dates in his life. He complained of general weakness and inability to work. Any endeavor to concentrate caused vertigo, irritation, and pains in the head. Day and night he was troubled about his health, his future, and his family’s future. He was going to become an invalid and a burden. He was tormented with the idea that people thought him a simulator. He complained of lumbar pains. It seems that the explosion had affected the left side of the body more than the right and he complained more of pains upon that side. In the dark his gait was unsteady, and he often had marked tremors of feet and hands. In excitement the tremor would increase uncontrollably. The patient thought that his hearing was diminished,[361] especially upon the left side, and that his left ear was weaker than the right. He slept poorly and had many nightmares; his appetite was poor, and he was constipated. There was difficulty in respiration; the pupils were slightly dilated and sluggish in their responses. There was a marked tendency to Rombergism; dermatographia marked; the skull and especially the lumbar spine was painful on tapping; hyperesthesia of the lumbar skin; paresis of left hand and left foot. The tendon reflexes were more marked on the right side than on the left, and there was even a slight ankle and patellar clonus. The Babinski sign was present on the right side. There were frequent fibrillary contractions of the muscles of the trunk and back.
Objectively the hearing was somewhat decreased in the left ear, and the vision of the left eye appeared to be somewhat impaired also. If the eyes had been held closed for a time, there was difficulty in opening them quickly. Aside from a somewhat elevated pulse and slight cardiac arrhythmia, there was no disorder of the internal organs.
This patient remarkably improved but was not absolutely well at the date of the report.
Re organic signs in Shell-shock cases, Oppenheim warns practitioners and experts against undervaluing war neuroses. He does not like to have them set down in too offhand a way, as hysteria, wish-fulfilment, and simulation. Hysteria is not likely, according to Oppenheim, in cases with permanent cyanosis, disappearance of the radial pulse, trophic disturbances, hyperidrosis, alopecia, fibrillary tremors, myokymia, cramps, dilated and sluggish pupils, and weakening of tendon reflexes. Hyperthyroidism also has been found by Oppenheim.
Shell-shock, explosion on left side: Sensory disorders especially on left side; ecchymosis of right (uninjured) leg, possibly conditioned upon shock of left hemisphere.
An artillery officer had had a shell burst to the left side of his horse, which veered to the right but did not fall. The officer’s left hand immediately became so numb and weak that he could not hold his reins with it; it shortly became more painful. The left foot showed a tendency to the same anesthesia and paresis.
Curiously enough, a number of punctate hemorrhages appeared on the right thigh and lower leg, upon the outer aspect. According to Gerver, these hemorrhages into the skin of the right leg may have something to do with a disturbance of circulation related with effects wrought upon the left hemisphere. During the course of the disease, pains occurred not only in the left arm and leg but also in the right leg.
Re brain injuries produced by shell explosions without external wound, Roussy and Boisseau have not found a single clinical instance amongst 133 cases observed, which suggested cerebral softening, or even hemorrhage into the brain substance, the cord substance, or the meninges. These 133 cases were observed in army neurological centres and contained instances of (a) mental disease (confusion, delirium, amnesia), (b) nervous disease (astasia-abasia, tremors, paralyses, contracture), and (c) an intermediary group (either mental confusion with stupor, or hysterical deafmutism).
Shell-shock; unconsciousness: Hysterical deafness, speech-disorder, gait. Recovery by reëducation. Brief relapse to deaf-mutism at noise of drums. Improvement. Relapse to numerous and severe hysterical symptoms at small guns fired on King’s birthday. Improvement. Speech wholly regained in a quarrel. Recovery.
A musketeer, 22, had been blind for a time at 11 on account of some spinal cord disease.
He was a soldier up to Christmas eve, 1914, when he was hurled backward in a trench in the Argonne by an exploding hand grenade. He lay unconscious for several hours, though without sign of physical injury. Coming to his senses, he worked himself out of the trench and crawled to another, but again fell unconscious. When he awoke he was in a physician’s care in quarters, to which he had been taken by ambulance men. Thence to the field hospital, and then to a private hospital at B.
Upon admission, January 17, he was hard of hearing on both sides, and his speech was peculiar: choked off and retarded. His gait was heavy, on a broad base. He was subject to headaches.
Exercises gradually improved the speech and the walking disorder was quickly overcome. February 5 came a relapse through fright at the rolling of drums near by. Speech was completely lost, deafness set in, and the patient ran restlessly to and fro in tears. After a few hours speech returned with still some minor difficulty.
From time to time came fainting spells and attacks of disorder of consciousness, with loss of orientation and the idea of being in the trench or under cover. He would ask whether it were raining through. His mood herein was at times cheerful and excited. Speech further improved from the middle of February, as well as did the other symptoms.
On the King s birthday, February 25, occurred another relapse due to his hearing small guns fired: Apathetic stupor, clonic spasm, aphonia, abasia, severe deafness, poor sleep, refusal of food. The next day he was still mute, but the spasms had ceased. He lay apathetically in bed, taking a little liquid food. February 27 he was still mute, though more active, not deaf, getting up alone, walking unsteadily on a broad base, and playing cards at the table. March 2 the word yes was again enunciated. March 3 he talked more freely and took a short walk. March 4 speech of a sudden came completely back on the occasion of getting excited in a quarrel among some other patients. The patient thereafter began to talk a great deal, was bright and cheerful, but still complained of a variety of nervous troubles. Speech was somewhat difficult, but he was free from any definite aphasia or paraphasia.
Re Shell-shock deafness, Jones Phillipson states that concussion deafness is due to three contributory factors: (a) cerebral concussion, (b) fatigue (violent oscillation of the perilymph, continued noises, strain of organ of Corti), and (c) temporary or permanent disorganization of the conductive apparatus.
Re concussion deafness, J. S. and S. Fraser found in four cases of actual explosion injury, a ruptured drumhead and hemorrhage into the fundus of the internal meatus in three cases. They did not find evidence of neuro-epithelial changes. Possibly the fundus hemorrhages, besides giving rise to deafness, may start up the tinnitus and giddiness that are sometimes found. In one case, there were changes in the delicate nerve endings of the auditory ampullae.
Shell-shock: Deafness
A shell burst behind an English lieutenant in 1914 without causing any wound but making him unconscious for an hour. During the hour the Germans passed by and stripped him of all articles of value. He came to and felt himself markedly deaf in both ears with an intense headache. There was no hemorrhage, no discharge, no tinnitus, no vertigo. Four days after the shell burst he could hear spoken words on each side at two feet, but could not hear a watch that could usually be heard from 3½ to 4 feet. With tuning fork C air and bone conduction proved much subnormal, though air conduction was better than bone conduction. With tuning fork C-5 air conduction was subnormal. Drums healthy. Improvement followed; hearing became normal eighteen days after explosion. The treatment was rest in bed with bromides early and strychnine later.
Marriage states that the psychical deafness due to shell-shock is usually bilateral and absolute. It is accompanied also, as a rule, by other nervous signs and symptoms, such as aphonia, tubular vision, paralyses, and anesthesias. Milligan and Westmacott state that the deafness is due to a functional suspension of neuronic impulses. They regard the brain as in a state of physical fatigue, and the mind as in a state of strain. There is no organic lesion. The neuronic impulses which are temporarily suspended are those which run from the higher cortical cells to the periphery.
Mine-explosion: Unconsciousness: Deaf-mutism. Recovery of speech after epistaxis and fever.
A soldier, 24, teacher in civil life, was in a mine explosion November 27, 1914, at Vienne-le-Château. He was unconscious six weeks and remembered nothing of what had passed. They had told him that he had been blind for a month. After regaining consciousness he was a deaf-mute and for seven months he did not speak. His mutism did not bother him, as he thought he had always been mute. He had always been able to write. He could not remember what had interfered with his speech or tell whether he could think the words which he could not utter.
May 22, 1915, there was considerable nasal hemorrhage, with fever. Upon this day he began to speak, at first a few words, telegram style, and with aphonia. A week later his voice returned. He was very irritable during the period of mutism and had ideas of persecution and of suicide and complained of becoming easily fatigued and exhausted.
His voice, however, became completely normal again and his respiration better. On the spirometer he breathed four liters, but still got out of breath easily. His diaphragmatic respiration was still imperfect. His deafness remained at the time of report about as before, though he had now been hearing for some time a slight resonance of his own voice and could hear sounds emitted a few centimeters from his ear. At time of report there was still general fatigue with insomnia.
Re war deafness, Castex states that not merely shell bursts and explosions are able to cause deafness, but the din of battle alone. There are two big groups of war deafness: one due to drum rupture, and the other due to labyrinthine shock. Labyrinthine shock—a much more serious matter—is produced when a big shell bursts. In these cases, the labyrinthine disorder is simply of the same general nature as commotio cerebri. The labyrinthine shock cases often need to be retired permanently from the front.
Shell-shock: Deaf-mutism.
A deaf-mute, 24, not of a neurotic temperament or of a neuropathic predisposition, was admitted to the Fourth London General Hospital November 16, 1915.
He wrote, “I left England the 8th of March, and went to Gallipoli on the 26th of May, and about the middle of August, one of our monitors fired short. I felt something go in my head; then I went to the Canada Hospital. They said it was concussion.” He had seen the monitors firing. He came to in a dug-out about an hour afterward. He was quite deaf and his head felt as if it would burst.
He could see and speak a little but lost his speech completely when Barany’s tests were applied. The headache then passed away, leaving the deaf-mutism. The ears, on examination, proved normal. The patient was able to cough and whistle. He wrote his wife a letter, telling her how he killed a Turkish woman sniper, but he did not remember that he had written the letter. Although he said he did not dream, while asleep he would assume the attitude of shooting with a rifle, as if pulling a trigger, and then the attitude of using the bayonet: the right parry, the left parry, and the thrust. Sometimes while asleep he would jump as if a shell were coming, and he would catch his right elbow as if hit there. He would then open his eyes wide and look under the bed. Then he would wake up and begin to cry, but without sound. Just such habitual attitudes occur in soldiers under anesthesia. In hypnotic sleep, although he trembled at his trench experiences, he did not assume these defensive attitudes.
Mott states in his Lettsomian lectures that hearing is often absolutely lost, but that sometimes a man is absolutely deaf on one side alone, either from the ruptured drum or from the violence with which wax has been driven against the drum. Mott speaks of the frequency of auditory hallucinations, and of hyperacusis—part of the patient’s general hypersensitivity—which may increase the violence of the neurosis and especially aggravate the headache.
Shell-shock: Deaf-mutism; convulsions and dream.
A private, 28, was seen by Lt. Col. Myers at a base hospital. This deaf-mute wrote, “I was standing and a shell bursted and that is all I can remember.” This might have happened six days previously. The patient wrote vaguely about a walk to “windy corner”; about being billeted in a dug-out, a train journey, and another hospital. He was deaf, deficient in sensibility throughout, especially in the left arm and left side of the face, and had severe headache. Two days later he started distinctly when hands were clapped while he was writing, but at the next hand-clapping there was no response.
After Lt. Col. Myers wrote down, “Imitate me,” and made consonant sounds, the patient succeeded imitating them. “You hear me a little now,” Lt. Col. Myers wrote. “Is this the first time you have spoken?” Patient replied, “I hope the Lord I can get my speech.” “But you did speak just now. Read this word. Say it.” Whereupon he was got to say his name and number.
The therapy was proceeding properly when suddenly he was seized with convulsions, limb movements chiefly clonic, back arched, eyes starting, later upturned. The patient pulled out a crucifix from a locker near the bed and regarded it ecstatically (pulse 85, corneal reflexes preserved). Three minutes later there was quieting down, and the patient was induced to talk. He began to talk about his wife. He had just been “seeing a farm and all the fighting.” A shell must have come in there. He had “seen the Lord Who saved him.” Intense headache and thirst followed. According to the patient the excitement was due to recovery of speech.
He later said, “It was just like a dream when I came to. I was sweating awful. I was seeing the Lord while I was in the farm by the Captain. I dreamed that I had the cross in my hand to meet him coming. I saw the trenches and the dug-outs and the wife.” In point of fact, the Captain at the[369] farm had had his arm blown off, and he had found him lying on the straw unconscious. Under hypnosis it appeared that he had gone to a dugout from the farm and that at the clearing station he had been “raving, seeing things, shells, trenches, and things like that, sir.” A slow recovery was made after evacuation to England. Seven months later he returned to the front.
This case appears to belong to the B group of mutism cases, according to the classification of Myers, namely, to the group in which the effects are psychical rather than physical. According to Myers, whether mutism occurs as an apparent result of physicochemical or of mental causes—that is, as an A or a B case—it is actually always the result of mental—that is, psycho-physiological shock. Mutism in the A cases of physical nature, where the shock must have been grosser and more profound, generally proves more severe than in the B cases. As to the appearance of unconsciousness, apparently confirmed by the patients’ statements that they “lost consciousness,” it is a question whether these cases are not really cases of deep stupor. According to Myers, the mutism is in nearly every instance closely dependent on some form of stupor, being generally the relic of such stupor after it has passed off. Let the loss of consciousness be a profound stupor due to the lifting or burial of the patient, then from this stage there will be a transition to a state of ordinary stupor in which intelligence is active but the patient is unresponsive to stimuli. The patient is in a condition called by Myers excommunication, in which the inhibitory process may be regarded as protecting the individual against further shock. As the stupor now passes away, it is natural that the inhibition should appear lost in the case of hearing and speech, which are two main channels of intercourse with others.
Dumbness is, by far, the commonest disorder of speech, occurring in about ten per cent of shock cases in the first thousand cases of shell-shock seen by Lt. Col. Myers. Stuttering and jerky speech have occurred in about three per cent. Loss of voice is rarer.
As against the view of Babinski, that mutism, being curable by suggestion, must have been produced by suggestion, Lt. Col. Myers argues that the stupor preceding mutism is the antithesis of suggestibility and is, in fact, a condition of extreme autofixity.
Naval gun-fire effects on seaman: Aphonia. Two recurrences.
A seaman from the Derfflinger was brought into a naval hospital with loss of voice, December 22, 1914, able to speak only in a whisper. As a child he had had diphtheria, but recovered without complication. He had always had a very well-controlled voice. Early in December he had had a cold owing to sentry deck duty in bad weather. Two days after the shelling of Scarboro,—December 16,—while in the munition chamber of the big guns, he suddenly lost his voice. He had been greatly upset during the firing of the guns. In two weeks he recovered speech.
February 12, 1915, he returned to the hospital with a complete aphonia. This was immediately after the naval engagement in the North Sea. Three days later he was treated with electricity directly applied to the vocal cords. March 20 he was discharged with speech completely recovered. As soon as he went on leave, however, his voice was lost for the third time, and he was still aphonic at time of report.
Shell-shock MUTES observed, then DREAMED OF: MUTISM developed the SECOND NIGHT after shell explosion.
A volunteer of 20 was made unconscious for a short time by a shell explosion, but was still fully able to speak when brought to the field hospital.
In the second night after the explosion, however, he dreamed that he had lost his speech. In the ward, meantime, he had seen a number of shell-shock mutes. Following this dream of aphasia, came several weeks of mutism, which then cleared up. According to Mann, this is experimental proof of the psychogenic origin of a mutism.
Mortar explosion: Hysterical deafness.
A young soldier, a peasant, fell down unconscious when a mortar exploded killing several men. He regained consciousness a few hours later but was deaf on both sides. He looked dazed and did not spontaneously move, having to be called for meals. Communicating by writing, he could tell all the details of the accident.
The laryngeal and corneal reflexes were absent and there was a hyperesthesia and hypalgesia of the right side of the body. No anatomical basis for the deafness could be determined.
Shell explosion: Onomatopoeic noises in ears.
A Zouave was with his squad at Tracy-les-Val Church, October, 1914, when the roof was burst in by a shell which wounded four men. The Zouave felt a strange emotion with trembling, and whistling in his ears. However, he helped his comrades into a neighboring car. From that time forward, he was very emotional, and felt noises in his ear, sometimes humming, sometimes whistling. At Compiègne Hospital a lumbar puncture was made, perhaps with a therapeutic purpose, but this gave no results. The noises were heard as a whistling pseeee followed by a boom,—an onomatopoeia recalling the whistling and bursting of the bomb. There was, in short, no labyrinthine lesion, but merely an obsessive mental phenomenon. There were no ear lesions objectively. The man developed a stuttering some time after the humming and whistling in the ear.
Injury of eyes by gravel from shell-burst: Photophobia, blepharospasm, facial anesthesia, pains.
A soldier of the Ninth Engineers, 28, a Beaux-Arts student, was wounded, December 19, 1915, by stones and gravel thrown in his eyes by a shell-burst. The eyelids swelled and the eyes filled with tears. He was treated at the relief station and then evacuated to Verdun. The edema disappeared in five weeks, but it was impossible for him to look at light. February 2 he was evacuated to Nice, where he received the diagnosis of traumatic keratalgia, blepharospasm, and photophobia. After eight days’ leave he went back to his corps; but the eye troubles persisted and he was sent to the ophthalmological center at Angers, May 18, 1915.
Both his father, 67, and his mother, 58, were irritable and odd. Three brothers and three sisters were also more or less neuropathic, and one of the sisters had been in a hospital for the insane with a persecutory mania. The patient had a daughter, fourteen months, well.
The man was a nervous, impressionable person, who wept at the slightest emotion. With an effort of will he could open his eyes, but if one tried to open them passively there was stout resistance. In the dark the occlusion was not so complete. Both eyelids were wrinkled and folded and made jerky, fibrillary movements. The conjunctiva and cornea were normal (fluorescein test), but the palpebral conjunctiva was red and injected. The patient said he had subcutaneous pains recurring at irregular intervals above and below the left orbit, brought out or exaggerated by pressure; but such pressure had no effect upon the lid movements. Visual acuity was normal, but the use of ophthalmometer was impossible, as was measurement of the visual field. There seemed to be no disorder of chromatic sense. The reflexes could not be fully examined; knee-jerks preserved. There was a zone of anesthesia to pin prick, less marked to heat, on the whole left side of the face. W. R. negative.
Shell-shock; burial; blow on occiput: Blindness.
A man in the third Wiltshire regiment was buried in a shell explosion and struck by a large mass of earth on the back of the head. When dug out, he was found blind. It was thought at the time that the severe blow at the back of the head had “concussed” the occipital cells for sight.
Some months later the man was sent to Mr. Pearson’s home for blind soldiers in London; but two months later was returned to Weymouth, under Greenlees’ charge. He thought himself worse, since now he could not see light at all. He had trained himself to take care of himself and steered confidently aside from obstacles in walking about. He was able even to learn the various colors by the sense of touch, according to Greenlees; thus, blue was diagnosticated against red: according to the patient, a piece of colored card always had a rougher feel if it was blue than if it was red. In fact, his work consisted of making colored net bags.
As to the possible interpretation of such a case, see Case No. 433 (man who could see large letters sometimes).
Re blindness, H. Campbell states that the number of cases of hysterical blindness appears to be decreasing as the war continues. The blindness he finds to be rarely an absolute one. As a rule, the vision is merely blurred or there is a contraction of the visual fields. The condition is much less frequent than that of deafmutism.
Re hysterical blindness, Dieufaloy is cited by Crouzon as describing a triad of conditions characteristic of hysterical blindness, namely, (a) sudden onset, (b) preservation of pupillary reflexes, and (c) normal fundus.
Shell-shock amblyopia (composite data).
Parsons describes a typical case of shell explosion amblyopia. After more or less prolonged fatigue from marching and trench exposure, the soldier is knocked down or blown into the air, and more or less severely injured or wounded by concussion, fracture, bullets, or shell splinters, losing consciousness, but perhaps not enough to prevent automatic walking in a dazed state to the dressing station. Memory of this phase is lost. The man is instantaneously stricken blind, possibly also deaf; and possibly smell and taste are also lost. Blepharospasm is intense; there is lacrimation; the lids are opened with such difficulty that examination of the eyes is almost impossible (nor, according to Parsons, have the pupils yet been examined at this stage).
In a week or two the blepharospasm diminishes, and the fundi, which are found to be absolutely normal, can be examined. The eyes may be found to be quite normal, the pupils reactive to light though perhaps sluggishly and perhaps unequally. Sight is now somewhat restored, light can be perceived, and large objects distinguished. The patient can grope about and usually does not stumble against obstacles. The fields of vision are markedly contracted, and more so than the avoidance of obstacles in walking would suggest.
Vision is eventually recovered completely. The right eye (the shooting eye) is often more deeply affected and recovers more slowly. Perhaps a central scotoma may persist. Sometimes on manipulation of lenses the full vision can be produced for the types. Parsons seeks to explain the psychology of traumatic amblyopia in the light of deductions of Lloyd Morgan, Mark Baldwin and McDougall.
Shell-shock amblyopia (excitement, blinding flashes, fear, disgust, fatigue).
Pemberton calls attention to the following factors in a case of amblyopia: First, excitement during a prolonged and somewhat critical attack; second, overstimulation of eyes and ears due to brilliant flashes, night firing from many batteries close together (the gunners are always subject to temporary deafness from this firing); third, natural fear from close bursting of shells; fourth, disgust at decapitated and disemboweled soldiers; fifth, fatigue from twelve hours’ work.
The artillery sergeant worked under heavy shell fire at Gun No. 1. A direct hit killed three men serving No. 2 gun. The sergeant became somewhat excited but worked his gun until the following dawn, when he collapsed across one of the disemboweled corpses. He thus had been at work for about twelve hours. The battery had fired 400 or 500 rounds.
A few hours later, the man was conscious but very feeble and much shaken. There was amblyopia and contraction of the fields of vision to rough tests, but no change in color vision. Taste sense was blunted, and salt could hardly be told from powdered quinin tablets. Smell also was practically absent, although he had never been able to smell accurately. Hearing was not more affected than that of other men in the battery, and there were no tympanic fractures. Both thighs, from about the apex of Scarpa’s triangle to the knee, showed partial anesthesia, such that a pin prick that should have been painful was felt only as a tactile sensation, whereas lighter stimulation caused no sensation whatever. The patient himself complained of numbness in these areas. The gait was slow and spastic. The knee-jerks were brisk. Sent back to the wagon lines for a week, the patient lost his sensory disturbance, but the symptoms of mental distress increased. He walked weakly and stiffly; he continually thought of the dead men at the next gun, one of whom was a friend. He was finally sent to a hospital in England.
Shell-shock amblyopia.
A private, 20, lay in the booking-hall of a station, October 28-29, not securing much sleep; motored in a bus next day to another place at 7.30 p.m.; went into billets at 8 p.m.; mounted guard 10-11.30 p.m. and 1.45 to 3.45 a.m.; and went to the firing-line for the first time at 11 a.m. October 31. The platoon advanced through two sets of trenches, which were full, and had to retire. About 1.30 p.m. they were found by the German artillery.
This man had been rather enjoying it and was in the best of spirits until the shells began to burst. The platoon was retiring over open ground. He was kneeling on both knees, trying to creep under wire entanglements, when two or three shells burst near by. Three more shells burst behind and one in front. The escape was described by an eye-witness as a miracle. He managed to get back under the entanglements and into the trench, and shortly, as the fire slackened, rejoined his company.
His sight had become blurred immediately after the shell burst. Opening his eyes hurt him, and the eyes burned when closed. The right eye “caught it” more than the left. At the same time, he was seized with shivering, and cold sweat broke out, especially about the loins. He thought the shell behind caused the greater shock, like a punch on the head without pain. The shell that burst in front had cut his haversack away, bruised his side, and burned his little finger. This shell he thought caused his blindness.
He was led to the dressing station by two comrades, opening his eyes to see where he was going but finding everything blurred except immediately after opening his eyes. There was no diplopia. Objects seemed to dissolve. He was weeping and worrying about becoming blind. The horse ambulance took him to a hospital and thence to another hospital, and thence he went by motor ambulance at night to the starting point, where he arrived five days after he had entered the field. He could remember nothing about the[377] ambulance trips. There was a slight deafness which soon passed off. In hospital he shivered almost incessantly in bed, and he kept thinking about his experience and the shell bursting. The shivering ceased November 3. No micturition from the afternoon of October 30 until the afternoon of November 2. No movements of bowels from October 30 to November 5.
It seems that this soldier had been for two months in the Aisne district, sleeping badly on account of lumbar pains and toothache. There had been albuminuria, and the patient said he had failed to pass a medical examination. The fields of vision were found to be distinctly contracted. There was difficulty in taste and smell, which the patient said he had lost since the shell-burst.
Hypnosis was tried but the patient “insisted on resisting.” The suggestions were offered during the concentration period. November 13 taste and smell began to return and the fields of vision were less contracted. He was transferred to England for further treatment, and by November 27 had become much improved and not so “nervy.” February 1 he had begun to attend hospital as an out-patient.
SHELL WINDAGE (NO EXPLOSION): Multiple affection of cranial nerves.
August 22, 1914, a French officer was leading his company to an attack and carried on, though wounded in the side by a bullet. Suddenly he felt as if he had received a terrible blow with a hammer on the left cheek and eye and as if his arm had been torn off. He fell to his knees without losing consciousness. There had been no explosion, and none of his soldiers had been hit. He felt of his arm and carried his hand to his head to make sure of the wounds. There were none, but he was bleeding from the nose and the mouth. His left eye was closed and his left cheek drawn “by an invisible hand.” His tongue had swollen until it had to be pushed out of his mouth. He was breathing hard. He fell upon his side without losing consciousness and he was carried by his men to shelter in a trench. Placed on his back he felt that he could not lift his head as “it had become too heavy.” His voice was lost. He could neither cough nor spit. In order to get air he had to remove bloody saliva from his mouth with his finger. The left side of the head was swollen. On opening his eyes he could no longer see with the left eye. His cheek was covered with ecchymoses but without wound. A few hours later he was made prisoner by the Germans. For two months he had an increase of temperature every evening and for three months he lost his voice. Six months later there was still visual impairment. He was anesthetic in the left cheek, unable to chew, paralyzed in the left facialis region. There was alteration of taste, with atrophy of the left side of the tongue deviating to the paralyzed side, and nasal regurgitation. There was continual drooling and convulsive coughing. In dorsal decubitus the head could be lifted with difficulty. There was a kind of paresis of the esophagus, as he felt the bolus stop at the level of the third ribs so that with each mouthful he had to swallow a little water. Apparently he had a paralytic state of the following[379] nerves: optic, oculomotor, trigeminal, glossopharyngeal, pneumogastric, spinal accessory and hypoglossal. There was evidence of a slight old tuberculosis at apices. The man was slightly pale. There was an atrophy of the optic nerve and some retinal swelling. No pupillary reactions to light on the left side; but the accommodation reflex and sensory reaction were preserved. Divergent strabismus of the left eye. The taste on the left side and on the anterior part of the tongue was slightly diminished. Diminution of galvanic and faradic excitability on the left side of the face. No reaction of degeneration. Bitter, salt and sweet tastes altered. Left-sided atrophy of the tongue. No reaction of degeneration in the tongue and thyroid muscles although there was a marked diminution in faradic excitability.
The author records this case of multiple lesions of cranial nerves as due to shell windage. Thirty-one months after the onset of the paralysis the cranial nerves, although manifestly regenerated, had not regained conductivity. The officer was examined by Pachantoni at Louèche-les-Bains in Switzerland.
Re windage, see remarks under Case 201.
Wound of thigh: Claudication, vasomotor disorder, hypothermia, but no exaggeration of tendon reflexes. Under CHLOROFORM, ELECTIVE EXAGGERATION OF REFLEXES, i.e., in this case, hyperreflexia of affected thigh, including patellar clonus, after other reflexes (including conjunctival) had become extinct. The case described led to the new formula of THE PHYSIOPATHIC SYNDROME (BABINSKI).
Babinski examined in August, 1915, at the Pitié, a soldier who had been wounded in the upper and outer part of the thigh. He showed a most marked claudication with outward rotation of the foot. There was a muscular atrophy of the thigh but no appreciable disorder of the electrical reactions. There was a slight limitation in the movements of the hip, namely, the movements of flexion and internal rotation of the thigh upon the pelvis; yet this limitation of movements did not seem to be in proportion to the rest of the motor disorder. The X-ray showed no joint lesion. The right knee-jerk was a bit stronger than the left, though this was controversial. Achilles reflexes were normal and equal; epileptoid trepidation of the foot, and clonus of the patella absent; the limb showed marked and permanent vasomotor disorders and local hypothermia; both phenomena were of a sharp and definite nature.
On the basis of the intensity of these vasomotor disorders, Babinski felt that, in accordance with his general ideas, he was not dealing with hysteria, and that he was in fact dealing with the so-called physiopathic syndrome. Lacking for this syndrome was the exaggeration of the tendon reflexes of the affected limb. Might it not be that the improper attitude and muscular stiffness of the limb were based simply on retractions of tendons? The patient was chloroformed. This procedure was the more warrantable as a number of physicians had thought of the patient as an exaggerator or[381] even as a simulator. Under chloroform there was in fact a slight tendon retraction; yet on the whole it was clear that the attitude and stiffness of the limb were largely dependent upon a contracture. When during narcosis all the other tendon reflexes and skin reflexes had become extinct, there was still to be observed on the affected side a hyperreflexia, and even a clonus of the patella; and the clonus lasted an hour after recovery from the anesthetic. This curious phenomenon of elective exaggeration of tendon reflexes in narcosis, Babinski has observed to be not infrequent. It is a valuable diagnostic sign for a sure proof of excess tendon reflexes in cases where doubt prevails under ordinary circumstances. Sometimes the contracture will yield, but only in the deepest sleep, outlasting even the conjunctival reflex and the reactions to pricking of the normal extremities. Moreover, the contracture would return from 20 to 25 minutes before any manifestation of consciousness. If an endeavor was made to reduce the contracture under full anesthesia and in complete unconsciousness, a spasmodic movement was provoked which exaggerated the abnormal attitude of the limb. Sometimes even the leg would be thrown into flexor contracture.
The case above described was the one which led Babinski to his new formula of the Physiopathic Syndrome. This he describes in general terms as follows:
These disorders consist in post-traumatic contractures, paralyses or paretic states, but are not attended by any of the signs of the so-called organic diseases, either of lesions of the central nervous system, or of the peripheral nervous system, or of the great arterial systems. In fact, these disorders somewhat resemble hysterical manifestations. The underlying lesions appear to be sometimes extremely small; in fact, so minimal as to be out of proportion with the functional disorders that they produce. These disorders do not correspond with any known anatomical regions, but they are singularly tenacious, and, unlike truly hysterical (pithiatic) phenomena, they are completely resistant to suggestion. Yet it is not merely in resistance to suggestive therapy that these reflex disorders differ from hysteria; for besides the[382] contracture and the paralysis or paresis found in the different segments of the extremity concerned, the complete Babinski syndrome includes also muscular atrophy, exaggeration of tendon reflexes, alterations of skin reflexes (even amounting to areflexia), hypotonia, mechanical over-excitability of the muscles with retardation of the muscular contraction; quantitative changes in electrical excitability of muscles (excess or diminution without R. D.), mechanical over-excitability, and occasionally electrical over-excitability of the nerves, disturbances in objective and subjective sensibilities (anesthesia and pains), heat regulation disorders (especially hyperthermia), and disorder of the vasomotors (cyanosis, skin redness, oscillometric lowering at the periphery of the extremity in the presence of low temperature), secretory disorders, and various trophic disorders of the bony system, the skin, and the nails.
Despite the permutations and combinations of these symptoms, according to Babinski they amount to a new group of disorders and represent a nosological species: a species of disease phenomena that lies midway between the organic affections and hysterical disorders. Babinski proposes the term physiopathic for these phenomena, a term which excludes the connotation of hysteria and all forms of psychopathia, on the one hand, and seems, on the other, to express the fact of their correspondence to a physical material perturbation in the nervous system of a novel sort.
Bullet wound of ankle: Contracture effect of chloroform.
A man was wounded, September 1, 1914, by a bullet in the left ankle. Contracture of the foot and of the four outer toes in extension followed, with a flaccid paralysis of the great toe. The left knee-jerk was a little stronger than the right; the left Achilles jerk also appeared weaker but observation was difficult on account of contracture of the foot.
Chloroformed, October 22, 1915: There was no sharply defined asymmetry of the tendon reflexes. The left Achilles reflex appeared a little weaker. In the phase of muscular resolution, the contracture disappeared entirely, but it reappeared a little after the return of the tendon reflexes. The reappearance of the contracture preceded the reappearance of consciousness from twenty to twenty-five minutes.
Post-typhoidal reflex or physiopathic disorder of right leg. Elective exaggeration under chloroform.
A typhoid patient, October 20, 1914, showed phlebitis and abscess of the right buttock with contracture of pelvic trochanteric muscles. He was sent to the Pitié on medicolegal grounds.
September 22 there was found a slight laxity of the patella tendon, as well marked on the left side as on the right. The right side was more cyanotic, due to the inactivity of the limb. There was no edema. Tendon and skin reflexes were normal. The lack of power was diagnosticated as purely functional, and the report was rendered that the soldier could begin to walk as soon as he desired. The two knee-jerks were noted to be stronger and polykinetic, and the right knee-jerk appeared a little stronger.
The patient was chloroformed, October 25, 1915. Almost immediately, the knee-jerks, Achilles jerks, plantar, and cremasteric reflexes disappeared. During the first period of anesthesia, there was no accentuation of the reflexes, but at the beginning of recovery the anticipated reappearance of the right knee-jerk was observed. This knee-jerk was already sharply defined at a moment when the left knee-jerk was still abolished. In a later phase of recovery, the right knee-jerk was very markedly exaggerated and a patellar clonus was demonstrable on the right side. Even percussion of the left patellar tendon brought about a contraction of the right adductors. There was a true clonic and tonic spasm of these muscles. On the other hand, percussion of the right patellar tendon was able to provoke no contraction of either right or left adductors. Nor was there at any time any ankle clonus.
Hysterical lameness (bullet wound of calf) cured, but the associated “reflex” disorder (in the sense of Babinski and Froment) NOT cured.
A corporal was wounded by a bullet in the calf, September 8, 1914. At the end of July, 1915, his lameness continued and he disliked to lean on his left leg which bent under him. There was a slight atrophy of the left calf. The lower leg could not be extended upon the thigh if the foot was in dorsal flexion, and the dorsal flexion of the foot was itself limited. There were no reflex, vasomotor or electrical disorders. The man was given the usual treatment by Vincent and soon learned to carry his body on either foot, and, being well disposed, speedily abandoned his lameness, acquiring such skill in movements that he became monitor over the other soldiers, watching over them in his capacity as corporal.
For about a year he thus served as monitor, and when fully dressed did not seem abnormal or look as if he were walking lame. However, after walking, say 6 kilometers, rapidly, he dragged his leg; nor was extension of the lower leg upon the thigh absolutely complete in habitual walking, though he was able to extend perfectly if requested. Dorsal flexion of the foot was also still somewhat limited, and the measurements of the two lower extremities at both calf and thigh showed a persistent slight atrophy on the left side. He was then sent into the auxiliary service and did good work as draughtsman. In the winter the left foot got cold rather easily.
This case is instanced by Vincent to support the contentions of Babinski and Froment that the truly “physiopathic” or “reflex” disorders do not completely clear up in the recovery from the associated hysterical disorders. That limb, which is the seat of physiopathic disorder, is not in a state of meiopragia.
Foot trauma: Pains and dysbasia, hysterical; slight atrophy of calf, physiopathic. Differential disappearance of hysterical symptoms; increase of physiopathic symptoms.
Clovis Vincent examined a man who had been wounded in the foot but without injury to the bones. He was first examined in July, 1915, when he complained of foot pains and was walking with crutches. The left calf was smaller than the right (4 cm.). The tendon reflexes were normal. There was no abnormality of electrical reaction. There was no proportionality between the trouble with walking and the organic status. A large part of the trouble appeared to be hysterical. In fact, upon treatment, the man was soon able to abandon the crutches and to walk, though lamely. He was put into the auxiliary military service.
However, the pains grew more marked and the lameness increased. Incapable of working, the patient was sent to the neurological center at Montpellier, whence he came to the neurological center at Tours in September, 1916. He had never been confined to bed, and had never ceased his daily walking, aided by a cane. The walking disorder was very pronounced. The patient said he was still suffering much. The difference between the two calves was now 8 cm. and the thigh was atrophied, though the atrophy had been absent in July, 1915. There was hyperexcitability of leg muscles. The right foot was colder than the left. The hysterical phenomena, so pronounced in July, 1915, were now absent, yet the reflex phenomena were sufficient to invalid the man.
Shell-shock paraplegia may AFTER TWENTY MONTHS develop vasomotor and secretory disorders: The whole to vanish on treatment.
A foot chasseur, 22, a farmer in civil life, sustained shell-shock à distance, June 2, 1915. He had no wound, but lost consciousness. He was evacuated for “contusion of back” to a hospital June 4 to 12; for “contusion of back and commotio cerebri” to Portarlier, to July 21; for “internal contusions and commotio cerebri” to Besançon, where he was in three hospitals up to May 31, 1916, and the diagnosis “hysteria, old commotio cerebri and trepidant astasia-abasia” was rendered and psychotherapy tried. The man was then evacuated to Saint Ferréol and the diagnosis “hysterical paraplegia” rendered. He finally reached Veil-Picard in February, 1917, still victim of paraplegia.
Up to this point there had been no signs suggestive of organic lesion of the spinal cord or any hysteroörganic intimation whatever. But in February, 1917, besides the motor disorder there was a hypothermia of several degrees, with cyanosis and hyperidrosis of both feet, with a marked diminution (and absence on one side) of the plantar cutaneous reflexes. The man was also victim of “hysterical pregnancy.” The cyanosis, hypothermia and hyperidrosis lasted six weeks.
March 23 the man was given treatment and for the first time in 21 months was able to stand and walk. The foot now turned from blue to red, and instead of cold became warm, even hot. In about a week the hyperthermia diminished, and, with the other troubles, disappeared. There remained only a slight swelling of the foot and ankle joints, due to the painful exercises given the patient.
It would seem, then, that a hysterical paraplegia of long duration may finally associate itself with marked vasomotor and secretory disorders and that these may be altered with extreme rapidity on the very day in which the hysterical phenomena are removed, and quite disappear in a fortnight.
Tetanus clinically cured: Phenomena in part reproduced UNDER CHLOROFORM ANESTHESIA five weeks afterward.
An infantryman, wounded at Notre Dame de Lorette, May 9, 1915, by a shell fragment in the right popliteal space, was given a preventive injection of 5 c.c. of antitetanic serum, evacuated to a hospital, May 12, and developed signs of tetanus August 1, with trismus and pains and spasms in the right leg.
The disease progressed with dysphagia, stiffness and paroxysmal hypertonia of the legs, especially of the right leg, fixed orthotonus of the trunk, neck hyperextended, arms stiff but able to move. Antitetanic serum was given daily. At the end of eight days there was a marked improvement and the whole course ran to approximate recovery in 25 days from the onset of tetanic symptoms, at which time the man was able to get up and walk on a crutch. The external popliteal nerve had been sectioned, and the foot was in a marked equinovarus.
Chloroform was administered for the purpose of straightening the foot, September 2, that is, about five weeks after the apparent end of the tetanus. The first stage of the anesthesia lasted about two minutes, but at this point the trunk and leg muscles passed into a state of diffuse contracture. In fact, a tetanic syndrome took place in the midst of the anesthesia. At a time when the corneal reflex was completely abolished, it was still impossible, with the exertion of the greatest strength, to flex the segments of the lower extremities. Moreover, the trunk was stiffly extended and the jaws were in trismus. Tonic and clonic contractions were produced by the efforts made to straighten the foot, and these contractions passed from the right side to the left. The chloroform was now increased and a transient resolution of the muscles was obtained, lasting hardly more than a half minute. As all efforts to reduce the pedal deformity failed, anesthesia was[389] stopped. The contractures and paroxysms lasted a few minutes. The knee-jerks were extremely exaggerated and there was a bilateral ankle clonus. After a brief phase of excitement, the patient emerged from anesthesia, began to talk with his comrades, and ate his usual meal without inconvenience. The chloroform anesthesia had lasted twenty minutes, and 60 grams had been administered.
It was now determined to section the tendo Achilles and the tibialis posticus. September 8 the man was chloroformed again and the same phenomena were exactly reproduced. Sixty grams of chloroform was again administered. The tendon resections permitted placing the foot in the proper attitude. Next day the patient was examined neurologically. The skin reflexes were found normal. The Achilles and knee-jerks were somewhat exaggerated, but equal on the two sides. There was no ankle clonus. Sensations proved normal. There was a mechanical hyperexcitability of the muscles of the anterior aspect of the thighs and of the calf.
In another case chloroformed 17 months after recovery from tetanus no such phenomena appeared. It would seem that the impregnation with tetanic virus or toxin must last in the nervous system a good deal longer than the apparent disease clinically lasts, but that this belated and concealed intoxication eventually passes.
The phenomena are perhaps analogous to those of Babinski and Froment’s so-called post-traumatic physiopathic or reflex phenomena. It was following the special work of Babinski and Froment upon the use of chloroform anesthesia in detecting physiopathic conditions that Monier-Vinard made his observations in cases of tetanus.
Shell-shock from falling of shell at a distance: Hysterical hemiplegia, terminating in brachial monoplegia. Case to show that the reflex or physiopathic disorders of Babinski and Froment may occur without mechanical injury in the region involved.
A soldier of the class of 1917 who never went to the front, while in training at Belfort, felt violent emotion on the occasion of the falling of a big shell in the town of Belfort. The explosion was a good distance from him. He lost consciousness a few moments, February 23, 1917, and almost at once found himself unable to move his left side. He was hemiplegic three months, but his leg shortly regained power. December 23 he entered a neurological center with his arm flaccid and a paralysis affecting the shoulder also. There was an almost complete anesthesia of the arm terminating in segmentary fashion about the shoulder, and the whole of the left side was slightly hypesthetic, although there was no disorder of motion except in the arm. The tendon reflexes of the left arm were exaggerated, and there was even contracture upon percussion of the muscles themselves. Percussion of the thenar and hypothenar eminences produced movements of the hand. There were several vasomotor disorders. Percussion led to large vasomotor plaques, and rubbing of the skin produced a reddening which passed away slowly. The hand was red and cold. Slight electrical hyperexcitability of flexors with feeble galvanic current; excitation of the extensors not associated with any contractions of the antagonist muscles. Threshold lower for flexors on the affected side in the forearm. Half centimeter atrophy of the biceps. The forearm and hand were possibly slightly increased in volume from a blue edema of the dorsal surfaces. The man was very timid, complained little, and accepted all treatment, which, however, was not very effective. This is presented by Ferrand as a case with physiopathic disorder in the sense of Babinski and Froment, though it does not present any sign of organic lesion whatever.
Shell fire: Delayed shell-shock symptoms, sub-lethal, appearing in England.
A soldier was picked up insensible in the public street and brought to hospital by ambulance, unconscious, breathing stertorously, pupils dilated, lips parched, unresponsive to stimuli, but without signs of injury or alcoholism.
The pulse grew slower, the respirations more sighing, the heart-beat more diffused and labored; but towards evening, about eight hours after admission, he began to move the eyelids and lips, and muttered a response to the request for his name. After ten more hours, respiration grew better, and Croton oil led to a movement of the bowels. Natural sleep intervened, and 18 hours after the onset of unconsciousness, the man woke up, and in the course of a few days became fairly well though still dazed and confused.
This soldier had never received any definite injury in his war service, but McWalter attributes his break-down to the effects of the constant shocks from the bursting of shells, and the scattering of shrapnel.
McWalter generalizes that a soldier, in the course of some civil occupation after the war, might develop symptoms, even fatal symptoms, and still the death in the case would be a direct consequence of the war.
Shell-shock symptoms, some initial, with recovery—others late and gradual, with deterioration.
A soldier became blind, deaf and dumb, as well as paralyzed, as a result of shell explosion. When he arrived at the hospital, he was able to see but had visual hallucinations. In a few days he recovered his hearing. There was a fine tremor of the hands, controllable by suggestion. There was an almost complete amnesia, but the patient remained able to read and write.
The pain persisted several months. The patient was physically well and seemed perfectly intelligent despite his aphasia and amnesia. One night, he sprang out of bed, shouting, “The guns are coming over us!” and from that time forward was able to speak. Amnesia, however, supervened for the months in the Dublin Hospital, and the patient believed that he was still in France. He also became unable to read or write, and was unable to recognize any letters except those he had been taught to speak during his period of dumbness. Still later he got a flaccid paralysis of the legs. From seeming perfectly intelligent, he began to seem markedly deteriorated. Hypnosis with waking suggestions had no power upon him. After a time, intelligence reappeared, but there had not been any recovery of locomotion at the time of report.
Wounds, gas, burial: Collapse on home leave.
A non-commissioned officer went through the first eleven months of the war in France and Flanders and was subjected to every kind of strain therein. He was wounded twice, gassed twice, and buried under a house, in each instance being treated in the field ambulance and returning to the trenches. Some time thereafter he was granted five days’ leave.
On reaching home, while waiting for a train, the officer suddenly collapsed and became unconscious. For months thereafter, he was the subject of a severe neurasthenia; “the whole of his trouble seemed to be due to the dread, lest on his return to the front, the added responsibilities which would fall upon his shoulders might be too much for him.” He thought his intelligence had been numbed by his experience. He thought his memory was unreliable, and that he could understand neither complex orders nor even the newspapers.
As to the reason for his maintenance of composure at the front, this may be laid to the excitement, the officer’s sense of responsibility, and the example he felt he should set his men. This kind of case[394] “demands a great deal of patient and sympathetic attention before the real cause is elicited, and then months of daily reëducation to build up anew the man’s confidence in himself.”
Bullet wound of neck: Late sympathetic nerve effect.
A Belgian was wounded, October 21, 1914, at Dixmude. The bullet wound was just below the right mastoid process. He was admitted to the London General Hospital, October 29. He said that the bullet had passed into the tonsil, lodging there, but that on the third day, while vomiting, he brought up the tonsil with the bullet in it. There was in fact a large ragged wound at the site of the right tonsil. He could swallow fluids only, but articulated clearly. There was a question of injury to the following nerves: facial, glossopharyngeal, vagus, hypoglossal, spinal accessory, and sympathetic. None of these nerves, however, appeared actually to have been injured. The difficulty in swallowing was due probably to the faucial wound, and it is hard to see how the pharynx could have been involved on account of the perfect articulation. November 3 the right sympathetic nerve was slightly affected; the right pupil was smaller than the left although it reacted to light. November 12 the patient left the hospital and nothing further is known of his history. Thus there was a late effect upon the sympathetic nerve thirteen days after the wound.
Re peripheral nerve disorders, see remarks under Case 252 (Tubby).
Fall from horse under shell fire: Crural monoplegia, hysterical. Reminiscence? Autosuggestion?
A patient of Forsyth had been exercising a high-spirited horse. Artillery fire close by made the horse leap sidewise, and the rider fell, his back striking the ground. He seemed to be curiously shaken out of proportion to the gravity of the fall. In a day or so, he lost the use of one leg.
He recalled a rather similar incident: He had taken a hand in a local uprising in a distant quarter of the world. While he was escaping up a mountain track, a rifle-shot from the enemy brought down his horse, which rolled over and threw him violently against a boulder, where the small of the back met the force of the impact. He felt intense pain and lost consciousness. Upon recovery he found he was paralyzed. At the end of several days, in a hiding-place in the rocks, he found himself still unable to move his legs. The friend who had carried him to the hiding-place refused to leave him. He thought of suicide, but then discovered that he could move: at first, the big toes, then the ankles, then the knees, and finally the hips. He was finally able to get into the saddle.
Moreover, years before, he had heard that a man who broke his back was paralyzed in the legs.
Re autosuggestion, Babinski remarks that suggestion may work in hystero-organic cases not precisely as in hysterical cases. Autosuggestion may here replace or accompany the ordinary heterosuggestion. Some temporary disturbance—a slight pain, a trivial injury, or a mere bruise—may start up a complex process of autosuggestion in which it may be difficult to unravel the part played by the patient’s own reflexes, his previous experience and beliefs (in this case, the reminiscences of a similar accident), the solicitude of his friends, and the medical examination itself. Babinski believes that hysterical paraplegia or monoplegia never appears automatically under the influence of emotion; never appears after the manner of sweating, diarrhea, or blushing.
Shell explosion; struck in cave-in: Symptoms in right leg (antebellum experience).
A private, 26 years old, had 11 months’ service and one month’s service in France. He arrived at a base hospital the day after his shock. Concussion had caused the dug-out in which he was standing to collapse. A beam struck him on the left side of the face, and pinned him to the ground on his right side. A piece of iron fell on the left side of his back, and his right leg was pinned by a cross beam on the back of his thigh. He was dazed by the shock; was released and was able to walk, but complained of a pain in the right groin and a giving-way of the right knee. The medical officer arrived about an hour later. A numbness, or state of no feeling, in the right thigh appeared, and increased to the point of total analgesia to the level of the upper margin of the patella save for a narrow strip in the mid-line on the posterior aspect of the leg. The only area of complete anesthesia and algesia was on the outside of the lower half of the leg.
According to the patient, it seems that about three years before, he had been buried four feet deep in a brick yard, beneath a heap of clay. He had felt it most in the right leg, but the thigh had been merely stiff and sore, and not numb. The patient admitted that the present accident immediately reminded him of his previous experience. There were no tremors or sensory disorders in the face, arms, chest, back, or abdomen. There was diminished sensibility to cotton wool of the left buttock (across which a plank had fallen), and there was a degree of hypalgesia of the buttock. The right thigh showed a degree of thermanalgesia and slight loss of vibratory sense. The corneal and conjunctival reflexes were diminished, and the knee-jerk was unobtainable on the right side. Three days later, there was a marked improvement with almost complete return to normal, whereupon the patient was sent to a convalescent camp.
Emotional subject, ALWAYS WEAK IN LEGS; shell explosion; wound of back: PARAPARESIS.
A Lieutenant, 25, was wounded at Arras about 10 a.m. October 20, 1914, just as he was leaning on another officer’s shoulder looking at a card in a chateau room. A shell burst in the court yard. A fragment came in the window, struck him in the back and pushed him forward, whereupon he felt pain in the back and a severe dyspnea, due to the gas from the shell. He lost consciousness several times and the dyspnea lasted for about two hours. When he was picked up he could not walk.
He was carried on a stretcher to the ambulance at Avin-le-Compte. During the fortnight there, he was also several times dyspneic. Strength left his legs and he could only get about on crutches. There was now a suppurating wound in the interscapular region where he had been struck by the shell fragment. Evacuated to Paris, he was operated upon on account of a tremendous abscess in the back, and the shell fragment and some bits of cloth were removed. The wound healed; but vague pains in the left thorax remained, especially when the man walked.
On examination, July 28, 1915, he would in the standing position hold his legs together with the feet resting on their external borders, especially on the left side. The toes were in plantar flexion, and the soles were arched upward more on the left side than on the right. In walking, the legs were always held in extension, the feet twisting outward. If an attempt was made to walk quickly, the man walked more and more upon the external borders of his feet, in such wise that the plantar surface and the heel turned up and became visible from above. He would get tired after five minutes’ walking even if he spread his legs out for a broader base of action. He could lift his legs only about 10 cm. from the bed, but could flex and slowly extend his lower leg on the thigh. He could not adduct or abduct the feet. Movements[398] of extension and flexion of leg on thigh were jerky and abruptly terminated, as also movements of thigh on hip. The patient could not sit, and when leaning forward he could not straighten up against resistance. The reflexes were normal. There was no sensory disorder. The electric reactions were normal. Pupils normal. There was slight hypertension of the spinal fluid and a slight excess of albumin. There were no lymphocytes.
In accordance with Dejerine’s idea that these neuropaths always have antecedents looking in the same direction, it was found that he had always been an emotional person, easily affected, sympathetic with other people’s troubles, given to weeping. As Lieutenant, he had not had the courage to harangue his soldiers. He had often during his life felt his legs weaken during times of emotion and had sometimes been unable to walk, though nothing of the sort had happened during the campaign. He was sure he could get well, and wanted two months’ leave in order to get back to the front. There were no hereditary features in the case. A physician had told him that he had had meningitis. This possibly followed whooping cough. He had had orchitis after mumps at 16. He had not had children, nor had there been miscarriages since marriage at 21.
Wound near heart; delayed medical care; fear of having been shot through heart: Paraparesis (antebellum always “hit in the legs.”)
An infantryman, 20, was sent as a Colonel’s bicyclist about 1 p.m. September 30, 1914, with a message to one of the battalions. He was exposed on the way to shell and rifle fire, and was wounded by a bullet which entered 8 cm. below and internal to the left mammillary line and came out in the region of the left hypochondrium. He crawled to some village houses 20 or 25 meters away. Another cyclist came to transfer the order, but could not help him. A friend came to his aid but was struck by a bullet 10 meters off and remained on the ground for an hour while the young cyclist lay behind a tree on the roadside. At 3 o’clock it was possible to take him to a house around which shells were raining. Shortly afterward the house caught fire. The man was evacuated 6 kilometers to an ambulance in the night, and that night six of his wounded comrades died in the same room. The man had lost much blood and began to think that his heart had been hit. He choked, had violent palpitations, and intense thirst. By automobile next day he was taken to the railway station at Maison and was there for a day practically without food.
That evening, 36 hours after the wound, he was evacuated to Juivisez and stayed there one night in the temporary hospital. The hemorrhage had now practically ceased. When he arrived next morning at Vincennes he could hardly move, was unable to walk, had violent palpitation, precordial pain, and two nervous seizures, with outcries and weeping. Several days later he could not walk at all or raise himself in bed. He was operated on May 29; he afterward felt the same leg weakness and was still unable to walk. Early in December, when observed by Dejerine, he was able to stand on crutches with legs flexed, toes on the ground, and heels up. In walking he would scrape the ground with the dorsum of the foot.[400] The wound was now healed. Suppuration had been intense and the scars were extensive. Lying down, the man could move, though slowly, his lower extremities in every way, nor was there any diminution in the strength of his flexors and extensors. The patient in making movements against resistance would let go quickly and jerkily. The plantar reflexes were flexor but weak. There was no other reflex disorder, no evidence of sensory disorder, nor any sign of neuritis or arthritis. Lumbar puncture gave a normal fluid without tension.
There were no hereditary features in the case. The man had been in childhood nervous and irascible, rolling on the ground, crying and weeping when crossed. He had had three attacks of appendicitis—one at 15 years and two at 19 years. After each attack he had felt weakness in the legs. He remembered, too, that after his nervous crises on being crossed, he had always felt this same weakness.
According to Dejerine, these paraplegic neuropaths, like functional gastropaths, cardiopaths, and victims of urinary disorder, have had earlier spells of the same kind, though milder than the attack which brings them to medical notice.
Wounds: Tic on attempts to walk; tremors. Recovery except for frontalis tic (ANTEBELLUM HABIT emphasized).
A substitute officer (mother nervous; always slightly excitable, easily fatiguable; had had a habit of wrinkling his forehead) sustained wounds September 8, 1914, in the foot and thigh. The wounds healed well, but in the hospital he slept badly and had battle dreams. When he essayed to walk, he had contractions of face muscles. There was a lively tic involving both face and neck muscles, with the head pulled to one side and backward. This grimacing was but slightly influencible by the will. There was a marked tremor of the arms. Gait was trippelnd. There were tremors of the whole body. There was also a slight hemi-hyperesthesia. The tendon reflexes were very lively; vasomotor disorders (feelings of cold and perspiration).
Seven months later the phenomena had all disappeared except for slight tic-like frontalis contractions.
Re heredity and soil, Mairet investigated 22 cases of Shell-shock, and found a hereditary taint in eight, and an acquired predisposition in nine. He found hereditary taint definitely absent in seven, and acquired soil definitely absent in six; whereas the rest of the cases were doubtful. He found both the taint and the soil in five cases; two cases with hereditary taint alone; no case acquired, non-hereditary.
In eight cases with head trauma, Mairet found three with hereditary taint, four without such; against one with an acquired predisposition, four without such, others doubtful.
Re cases of somatic trauma (not affecting the head), among five examined, there were none with hereditary taint, three definitely without taint, and five definitely without predisposition. According to Babinski, neither hereditary taint nor prepared terrain needs be found in hysterics.
A predisposition is not thought important by Oppenheim, especially as so many normal persons are predisposed.
War strain (fatigue, emotion): Hysterical hemiplegia. Precisely similar hemiplegia ANTEBELLUM.
A sergeant in a regiment of cuirassiers was observed at Villejuif, January 25, 1915. He had lost power on the left side as a result of fatigue and emotion, November, 1914. He had a complete paralysis of the left arm and a paresis of the left leg. There was an anesthesia of hysterical type in the left arm, and also of the left leg as far as the middle of the thigh. He dragged his leg in walking (démarche en draguant: the toe is dragged along the ground, the trunk is bent forward, and at every step plunges somewhat toward the paralyzed side. The patient is able to walk, however, by means of a cane or crutches. This walk is characteristic of hysterical hemiplegia. According to Roussy and Lhermitte, the number of cases of hysterical hemiplegia (better, hemiparesis) is not large). The plantar reflexes on both sides were those of flexion. Upon treatment (not specified), at the end of six months he went back to service in the cavalry.
The point of note in this case is that this patient had had a precisely similar phenomenon on the same side, which lasted a month, at the age of sixteen years and a half. It is noteworthy that in this case there was no traumatism and only the factors of fatigue and emotion to serve as an occasion for the hemiplegia. In fact, hysterical hemiplegia is said very rarely to follow physical trauma to an extremity. There are, however, some cases in which hemiparesis follows a slight head wound, particularly if over the region controlling the paralyzed limbs.
During the six-months’ course of successful treatment, no atrophy of limbs appeared, and there was never any inequality of the reflexes.
A good soldier (son of a tabetic sometimes hemiplegic), at 17 victim of hysterical hemiplegia, has AT 24 A RECURRENCE after two months’ field service. “Functional excommunication” of left arm and leg.
A cuirassier, 24, one month in the field, began to feel in September, 1914, crawling sensations in left arm and leg; then fingers, later hand and forearm, and finally upper arm began to work awkwardly and feel heavy, and there was a little of the same sort of thing in the leg. Hand and forearm were by the middle of October completely paralyzed, whereas the arm and shoulder were only paretic. Anesthesia at this time reached the elbow. The man had to be evacuated, after two months’ active and skilful field service, in one instance (September 19) carrying out a clever and useful interception of hostile telephone messages.
It seems that at the age of 17 also the man had had a left-sided hemiplegia, with sensory and motor symptoms, lasting two months, cured by electricity applied with a small electrode in his village. The war situation was therefore actually a recurrence of the transient hysterical paraplegia.
Moreover, the patient’s father, 52, an old tabetic, had also several times shown a hemiplegia (however on the right side), a phenomenon which had strongly affected his son.
It was curious that the slight residuals of movement which the cuirassier could perform could be made only while he was looking at the parts he was requested to move, and were impossible with eyes closed. The anesthesia was a total one when observed in November, 1914, coming to a sharp and circular termination at the shoulder and garter-wise above the knee—tuning fork insensibility in the same areas. The left patellar reflex was diminished when the eyes of the patient were leveled at the knee; but a surprise test brought the knee-jerk out normally. The hand and fingers were a little darker in color, and the whole left arm a little colder[404] than the right. There was also a slight amblyopia on the left side.
This hysterical paraplegia proved rather resistant to psychotherapy. The patient seems to have systematically eliminated from consciousness and from action the entire function of the left arm and a good deal of the left leg. Duprés and Rist speak of this as a kind of functional excommunication of the parts.
Re relapses, Wiltshire remarks that the frequency of relapses and the ways in which they are produced favor the conception that the original cause of Shell-shock must be psychic. Sir George Savage remarks that cases of Shell-shock should not return to the service under a period of six months on account of the frequency of relapse. Others have recently argued that such cases should not be sent back to the front at all. Harris notes that relapse may follow so apparently slight a factor as a vivid dream. Remarks concerning the true nature of relapses are made by Russell. Russell, for example, disapproves anesthetics in curing such a hysterical phenomenon as deafmutism. This sort of treatment does not get at the real cause of the condition, so that the man is very liable to relapse with the same symptoms. Ballet and de Fursac note the many cases of relapse after treatment and after discharge. Sometimes the relapses were due to some unfortunate happening, but in other instances no external cause could be made out. Fear of having to return to the front is a factor in certain cases, so that the true answer to the relapse question may not come until after the war.
Roussy and Boisseau insist upon the value of rapid cures (psychotherapy, electricity, cold shower, etc.), in diminishing the number of relapses. They maintain that these rapid cures abolish any chance for the man to brood over symptoms and thus to exaggerate and fixate them. These workers send their hospital return back to the regiments with a statement relative to diagnosis and the request that he be immediately returned to hospital if neurotic symptoms appear.
War strain; burial: Deafmutism. ANTEBELLUM speech difficulty.
A private 20 (always rather tenderhearted, disliking to see animals killed; rather self-conscious; a bit seclusive; “rather more virtuous than his companions”; shy with girls; sore throat a year or more before the war, with inability to sing or talk; always a lisper) enlisted in May, 1916, spent five advantageous months in training and became increasingly sociable. However, on going to the front October, 1916, he was frightened by the first shell fire and horrorstricken by the sight of wounds and death. He grew accustomed to the horrors and five months later was sent to Armentières, where he had to fight for three days without sleep. He grew very tired and began to hope that he would receive wounds that might incapacitate him at least temporarily for service.
He was suddenly buried by a shell, did not lose consciousness, but on being dug out was found to be deaf and dumb. On the way to the field dressing station he had a fear of shells. The deafmutism persisted unchanged for a month and then was completely and permanently cured in less than five minutes. He was made to face a mirror and observe the start he gave when hands were clapped behind him. He was assured that this start was an evidence of hearing; that his hearing was not lost, nor was his speech. He had no relapses during two months.
According to MacCurdy, this case is a typical one of war neurosis of the type of a simple conversion hysteria. The man never suffered from anxiety or nightmares.
Re burial cases, Grasset suggests that some of the patients probably think that they have actually died; both sensation and motion have been lost, and it is naturally these that permit a man to believe that he is still alive. The classical case is recalled, of the almost absolutely anesthetic boy who, with eyes closed, at once fell asleep. Foucault’s patient also said he actually thought he was dead after an explosion.
War strain: Shell-shock and psychotic symptoms, with determination to parts injured ANTEBELLUM.
Several years before the war, a cavalry officer had a severe concussion of the brain after a fall from his horse, but got no manifest symptoms therefrom except a mild transient deafness. There must have been a vestibular nerve injury, however, since there was a marked bilateral subexcitability of this apparatus later determined.
In September, 1914, as the result of strains and privation in the field, he got vertigo and lachrymose spells, with some obsessions as though he would have to shoot himself in the foot or spring out at the enemy from the trench.
In hospital at Jena, insomnia, anxiety, excessive perspiration and salivation, feelings of the death of various parts of the body, especially the forearms and hands, associated with hypesthesia of the parts, were determined. He had a feeling of vertigo on walking and was very sensitive to noise. He now developed a very intense and very variable degree of deafness on both sides, diagnosticated as nervous deafness. The caloric test demonstrated vestibular subexcitability above mentioned. We may suppose that in this already injured organism fresh disorder had set in on a psychogenic basis in the same region that had been injured years before.
Mine explosion; emotion at death of comrades: Unconsciousness eight days with hallucinatory delirium; later, dizziness. History of previous trauma to head with unconsciousness and dizziness.
Sent at end of May to the front, an Italian soldier (Class 1895, laundryman) was placed in an advanced post where he at once sustained great hardships.
Father drunkard, mother healthy, sister nervous. Two brothers healthy, one brother died of tuberculosis. Patient had scrofula, scarlet fever, and bronchitis (tendency to rave intensely when in fever). At four, sustained a trauma on the head (skull depression), dizziness, loss of consciousness.
June 7, a mine exploded in his vicinity, smashing several of his comrades. He did not himself fall to the ground, but was overwhelmed by a violent feeling of anguish. After a while, he lost consciousness. He woke up at Bologna, June 15, as after a long sleep. During the interval he had been in a state of intense hallucinatory delirium day and night. Then his mind began gradually to clear, first with amnesia of the shock which had caused the trauma. Then he recalled this fact too. Dizziness, however, grew in intensity so that he fell to ground many times during the day. There were intermittent tremors in the limbs.
Under observation, August 7, a sturdy, robust man. Somewhat dull in demeanor. Senses intact. Cranial nerves negative. Tendon and skin reflexes lively, especially on the right. Memory intact, except for above-mentioned oniric delirium with restlessness and shouting at night, especially while falling asleep and waking up. Frequent intense dizziness.
The condition remained unchanged for a week. Patient transferred to another department, for acute catarrhal bronchitis with fever.
Sniper stricken blind in shooting eye.
An Australian, 19, was admitted to hospital for loss of sight in the right eye. There had been a right ptosis from childhood. January 7 nothing could be perceived but light.
According to the patient, he was sniping through a loop-hole, November 15, when a bullet knocked a piece from the stock of his rifle. He continued at his post. There were five more shots, when another bullet struck the sand around the loop-hole. His right eye began to water. He shut the loop-hole and retired for an hour. His eye improved, he returned, opened the loop-hole, braced the rifle, and found he could not see the sights. He went to the physician. Vision grew rapidly worse, and in a few hours perception of light failed. He had been stricken blind in the shooting eye (the seat of a congenital deformity).
Anticipation of warfare: Hysterical blindness.
Anticipation of warfare may provoke a neurosis as in a case of Forsyth’s. The man went blind training in England.
It seems that four months before, while mounting sentry at night, marauding gypsies had felled him by a blow on the head from behind. He had returned to duty after a day or two and was now expecting to be moved to France. He said that while sitting with a friend, he began to feel giddy, turned a somersault, and fell unconscious; and that on coming to, his mind was clear but everything was dark. For ten days he had been blind, although once he could see his parents, who visited him in hospital, almost clearly. His appearance under examination strongly recalled that of a blind man. He was induced to read some large print, then smaller print, and finally very small print. He then lapsed into blindness.
He remembered that before enlisting, he had trained in a smithy, and heard that blacksmiths often went blind at the forge.
Bareback riding: Spasmodic neurosis (similar ANTEBELLUM episode).
A soldier, 32, had to do a long stretch of riding bareback. As a result, he later suffered from tonic muscular spasms whenever he had to exert himself seriously, especially whenever he had to move his legs and when sudden movements or sudden strong contacts were made. The attack appeared to be reflexly dependent on the pain. The case is regarded as one of the Wernicke Crampusneurosen, a disease somewhat related with hysteria.
A condition somewhat like the one developed in the war had occurred in this man at the age of seventeen after a drenching, but the attack was at that time much milder. He had, however, frequently had cramps in his legs.
ANTEBELLUM spasm of hands, functional.
A boy, 19, had been passed as fit for laboring work at home. He had been a farm boy from 14. Once at 17 he had developed whilst working amongst turnips in wet weather, pain in the hands, which got worse and was followed by pains in legs, arm, and neck, that kept him in bed a week, and from work ten days. Even on returning to work, his hands were swollen, though he was able to drive a horse. The fingers had been somewhat firmly flexed on the palms ever since this illness at 17.
He was sent to Netley after three weeks of army work, as having a spasm of both hands. He was found to be mentally below par, nervous, apprehensive, stuttering in speech and not readily responsive, with defective vasomotor control, though of good average bodily development except for asymmetry of chest.
Both hands were found firmly closed; tips of fingers applied to palms; thumbs freely movable; forearms well developed, especially the flexors. Counterforce was exerted upon passive extension of fingers. There was no sensory or reflex disorder, and while the patient was asleep, it was found that the first and second fingers of both hands could be fully extended. Yet there was a definite contracture of the palmar fascia which prevented full extension of the third and fourth fingers. He was awakened by this test and the fingers became firmly flexed at once.
The man was treated by milk isolation behind screens, without permission to read, smoke, or talk. Twice a day he was encouraged to move the fingers and made to perform finger exercises. He became able to extend the fingers over half their normal excursion in three days, and was then able to abduct and adduct the fingers. He was allowed up in two weeks’ time, with full diet and screens removed. The contracture of the palmar fascia was still in evidence, but the power of movement in the hands and fingers was so satisfactory that he could be sent back to duty in three weeks. The interpretation of Fergus Hewat is that the painful condition of the hands which set in in the illness at the age of 17, had caused an obsession which had developed into a functional spasm of the hands.
Quarrel: Hysterical HEMICHOREA, DOUBLY REMINISCENT, of a former hysterical chorea, itself related with an organic chorea of the patient’s mother.
A nineteen year old soldier, for some months a bit distressed and irritable, had a dispute with an old man whose jug he unluckily happened to smash. The old man said something was going to happen to him for that. That day, in point of fact, he fell and sustained an injury with water on the right knee. He was upbraided by the captain and evacuated to the ambulance. The fellow thought the old man with the broken jug had interfered, dreamed of the old man’s threats, and felt his hand on his shoulder.
Next day hemichorea developed on the right side, a partial and rhythmic chorea with jerky, regular contractions, fifty to sixty per minute, affecting synchronously the muscles of the leg, arm, face and tongue.
Dupuoy speaks of the reason for the hysterical “choice” of this disease, since his mother had had a probably organic hemichorea, also on the right side, with which she died at thirty years in a stroke. The boy was at that time thirteen years old and had had a rhythmic chorea six weeks, limited to the extensors of the hand on the forearm, treated in hospital.
This new hemichorea was quickly and completely cured by psychotherapy.
Hallucinations and delusions in a soldier, of antebellum origin. Treatment by explanation of causes.
A private, 31,—a case of Capt. W. Brown,—was admitted to hospital suffering from hallucinations of hearing and delusions of supervision by his family and friends; he heard his relatives telling him what to do and what not to do. He thought they belonged to a secret police entrusted with the task of supervising his actions and seeing that he did not again transgress as he had done. An inquiry into his past revealed the following facts:
He had been a bank clerk before the war and once because of a nervous breakdown as a result of drinking and smoking had been given a three months’ vacation. On this occasion he went with a prostitute—his first and only offence in sex matters. He later thought the behavior of his family indicated that they knew of his misdeed. He heard the voices of members of his family, became rapidly worse and more depressed, and attempted suicide.
He went to a private asylum. Later, he emigrated to Canada, but he was still pursued by the voices and he returned to England. He enlisted at the outbreak of the war and went to France. He was soon invalided and sent to Maghull.
The cause of his condition, according to Rows, was his affair with the prostitute and his previous drinking. This was explained to him as the basis of his strong feeling of self-reproach. The hallucinations and idea of suicide had developed therefrom. Recovery[413] “to a large extent.”
A poor risk (hereditary and acquired); emotionality: Tremors and convulsive crises with lowering of pulse.
A man, 36 (boat painter to 30 and thereafter a wine seller; paternal grandmother insane, father alcoholic and suicide; gonorrhea, 20; two attacks of lead colic, 25 to 30; purulent pleurisy, 31; phlegmon of mouth, 34; also a chronic alcoholic), at the time of examination showed arteriosclerosis and slightly hypertrophic liver; unequal pupils, slightly contracted and sluggish to light. He complained of frequent headaches, possibly due to a combination of plumbism and alcoholism. He was not in any respect demented, and had an excellent memory. He had always been emotional, being unable to go to a funeral without many tears, or remain in a house where there was a corpse without threatening to faint. He was always overcome if he saw a fight going on; and even in his wine shop he would escape when there was a fight and get a neighbor to bring the police.
He was mobilized on the fifth day, sent first to a territorial regiment and then, in October, put into the reserve of an active regiment and sent to the front. He reached the first line trenches in the night, greatly affected by ruins he saw on the road. He slept poorly and had nightmares. At daybreak he woke up to see a pile of corpses near by, and felt an indescribable terror on account of the corpses and the noise of bullets, machine guns, and shells. By superhuman efforts—according to the man—he mastered his emotions and took his turn at the observation post. Another sleepless night. Next day he got such tremors that his sergeant sent him to the hospital where he was at first thought to be suffering from a fever. But his temperature was found normal, and he was sent back to the trenches.
He passed another night without sleep, and next day he could not hold his gun for trembling. The Captain sent him back to be a kitchen man in the rear, and here he remained[414] six weeks—restless, trembling, eating very little. He would have anxious spells. In the morning, as he was carrying coffee to the men in his company, on seeing a pile of corpses, he dropped his pot and ran back to the kitchen declaring that whoever wanted to carry coffee might, but he would not go back. He spilled a pot of soup on his left foot. The Captain had him evacuated, saying: “Go! when you come back, I hope the war will be over!”
He was sent back to a hospital near Paris, where he was all right for a few days, happy as a prince. The burn got well, and as the time approached when he would probably have to go back to the front, the terror returned. He had visions of corpses, and imagined bullets whistling, machine guns popping, and shells bursting. He wept, lost appetite, hid in corners, made three suicidal attempts by poisoning,—though the sincerity of these attempts was doubtful (zinc oxide ointment; rose laurel leaves; verdigris). Sent back to a dépôt before getting leave, he had crises of tremor with anxiety, and was then sent to Val-de-Grâce on the mental service, and finally to Ville-Évrard. He unhesitatingly confessed his terror, becoming more and more anxious and tremulous, and almost losing his pulse while describing his experiences. He said he would commit suicide rather than return to the front. He stayed at the Hospital, working in the garden rather calmly, but when it was a question of leaving, even on convalescence, his terror and anxiety returned. Every time he was examined there was an emotional explosion, with expressions of anguish, generalized tremors and crises of clonic convulsions with respiratory disturbance even of threatening suffocation, depression of pulse. It is this latter which is the most important element in the proof that such a case is not a case of simulation.
Re war cases, Bennati remarks upon the great number that do not fall into known categories. There is, he thinks, an anaphylactic group in which the trauma acts as the secondary toxic agent; and there is another group in which exhaustion works after the manner suggested by Edinger: that is, by a physiological overwork of certain structures.
Martial misfit, dwelling on horrors of war at home; exposure; shell fire: Mental exhaustion with depression, emotionality, tachycardia.
An Italian corporal, in civil life a writer (mother very nervous; patient himself rickety, unmarried; relatives well off), was in front line trenches for some fifty days. He was repeatedly excused from service on account of fatigue, distress, poor appetite, insomnia, depression and even confusion (aimless shots fired off in the night). It turned out that he had been in just this state of mind when he left home and family and that the very thought of war had seemed dreadful to him. He did not at all enjoy leaves at night, as he stumbled and fell about in the darkness and had shells burst near by. He lived immersed in mud. He reacted unfavorably to antityphoid injection.
The very day he went on winter furlough he greatly improved, but then suddenly relapsed into depression, emotionality, inattentiveness, sluggishness of mind, and exhaustion. The tendon reflexes were lively, the abdominal reflexes sluggish. There was tachycardia (120), the Mannkopf-Thomayer tests were positive at 76 and 80, oculocardiac reflexes 84 and vagotonic. Stellwag and v. Graefe symptoms.
Hereditary instability.
An English soldier, 23, had been ten months on active service in France, when he was buried by a shell December 19, 1915. He became unconscious and later suffered from nervousness and stuttering, depression, insomnia, frightful dreams, and tremor. Improvement was such, under treatment, that he was again returned to the front. A shell burst near him once more and again he grew dazed, trembled, had lapses of memory and fell into a state of general nervousness. He improved again in hospital.
On returning to the front in a few days he saw a bomb burst some distance away. He began to stammer and to wander about aimlessly. Insomnia, tremor of legs, arms and head, fatiguability, feeling of lassitude, occipital and vertical headache, fear of aircraft and crowds, frightful dreams, absences and aimless wanderings appeared. There was one attack of deafmutism. Whenever the patient saw aircraft he ran. He was easily startled by noises.
He was the son of an excitable, alcoholic father and of a nervous and bad tempered mother. A sister had had nervous prostration. The man himself had always been more or less moody and a nail-biter. According to Wolfsohn, 74 per cent of the war neuroses have a family history of neurotic or psychotic stigmata, including insanity, epilepsy, alcoholism and nervousness; 72 per cent show previous neuropathy.
According to Wolfsohn, wounded soldiers do not show war neuroses except in rare instances. In the wounded soldiers studied by him no neuropathic or psychopathic stigmata occurred in the family history and previous neuropathic tendencies in the patients themselves were found in about 10%.
A soldier that is excessively fatigued or has been under undue mental anxiety, expecting to be blown to pieces, may go into psychoneurosis more easily than one without such emotional strain.
Genealogical tree of a shoemaker.
An English private, shoemaker, 37, was partially buried in a shell explosion and came to, stupid, shaky, weak and fearful of the dark. Twice, in a dazed state, he attempted to murder companions and was afterwards amnestic. He had always been of a violent temper and his outbursts had been followed by petit mal. He had also always been afraid of the dark. One of his children had fits; three were hysterical and had temper fits. The man’s father was in an insane hospital. Sundry other facts are shown in the genealogical tree presented herewith.
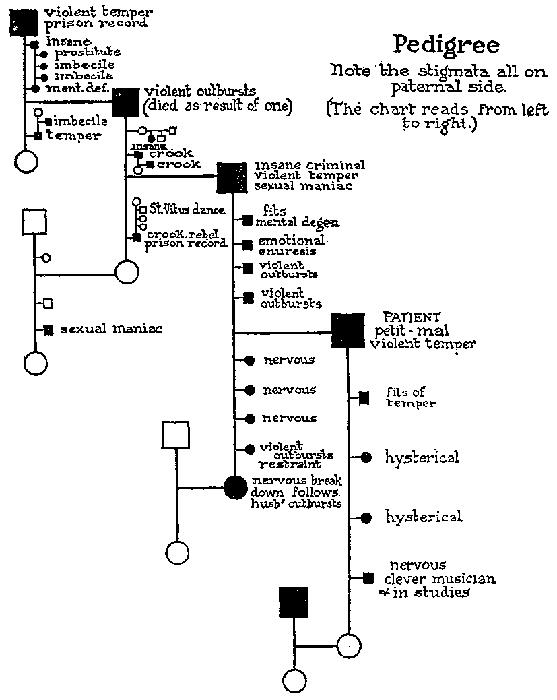
Fall from horse in battle; fear of being crushed: Hysterical crises. Case offered as showing TRAUMATIC HYSTERIA in a young physician WITHOUT HEREDITARY OR ACQUIRED PSYCHOPATHIC TENDENCY.
A physician of twenty went into the war as a volunteer Hussar. During an attack, he fell from his horse without losing consciousness, though he was at the time much afraid of being crushed. The attack ceased and he returned to the lines on horseback.
Immediately there developed an emotional crisis, and thereafter he broke into weeping on the slightest occasion. He was afraid he was going to lose his reason; that some spiritual power was going to suppress his ego and madden him. He wept as he was going under narcosis to be operated[419] upon for an intercurrent appendicitis. He became so sensitive to noise that he wanted to choke the offender. One day he bit himself on the arm in his excitement. Sensory tests could not be executed on account of his fear of the brush. Reflexes were normal.
It took four hypnotic seances to get him in proper rapport with his physician for psychotherapy.
This case is cited by Donath as one in which traumatic hysteria has been proven to exist in a man without any sign of neuropathic or psychopathic taint, either in his previous history or in his relatives.
A perfect soldier type. Mine explosion; burial; superficial wounds: War neurosis.
A lieutenant, 29, had been a regular soldier for eight years before the war and was made a non-commissioned officer almost at once after enlisting. He went out as a sergeant with the original expeditionary force and got through the retreat from Mons and the first battle of Ypres intact. He enjoyed the fighting hugely and even got indifferent to the burial work. The death of chums saddened him, but he carried on and soon forgot about the incidents. He might be regarded as a perfect soldier.
In August, 1915, there was a slight touch of rheumatism. Two or three months later the Germans exploded a mine immediately in front of the trench where he was. He went pale for the first time in his life, but kept his men “standing to.” Thereafter he began to think for the first time about danger. Mining was hereabouts the chief form of attack, and he frequently heard Germans digging beneath a dug-out. He slept well in billets, but was too restless for sleep on active duty.
He got more and more on edge during the next weeks. Six weeks after the mine explosion he was buried in a dug-out. Though he did not lose consciousness, he was dazed and had to lie down for two hours. Nervousness, chronic headache and insomnia, even in billets, followed. His imagination played upon the blowing out of dug-outs and the bowling over of men by shells. He had become company sergeant-major and the responsibility made him grow worse and worse. At times he tended to jump when the shells came, but was outwardly perfectly calm. He began to take morphia, though with little result. He had suicidal thoughts.
After two months of these symptoms he was sent to England. He began to sleep fairly well and three months later applied for light duty; was greatly bored by the company accountant work given him; got a commission and was sent[420] back to the front nine months later, January, 1917. He got on with the active fighting very well, sleeping four or five hours a night. In April he was sent to Arras. He had had a dream that he was going to be bowled over, buried and wounded in the neck. Sleep got poorer. In April he led his men in an advance and actually was bowled over, buried and hit in the neck as well as in the knee and the hand, though all the wounds were superficial. He was carried back, dazed, to hospital, where he grew fairly comfortable in ten days and even undertook a journey down to the base.
He arrived in collapse, remained in camp at the base three weeks, getting steadily worse. Something, he could not tell what, was going to happen and kill him. He could not concentrate, even to read. He thought of suicide. He slept practically not at all, waking from a doze with a start, feeling that something had hit him. He had dreams of being taken prisoner and on waking would in fancy start a fight to escape from imagined imprisonment back to the British lines. After two weeks in various hospitals he spent ten days in a hospital for nervous cases and grew better. Riding on trains he was terrorized in every tunnel lest he should be crushed.
According to MacCurdy, an anxiety neurosis would have developed had not his superiors sent the lieutenant back to hospital after the final burial in April. As this perfect soldier said:[421] “There is no man on earth who can stick this thing forever.”
Shell-shock; thrown against a wall: Tremors—TREMOPHOBIA.
Meige has studied shell-shock tremors, especially those occurring without external wound.
A corporal was with his squad on the Nouvron Plateau, January 13, 1915, when he was thrown against the wall by a bursting shell, which killed or wounded several comrades but did not wound the corporal. Whether he lost consciousness is unknown, but he lay on the ground for some time, until he could be moved through a communication trench. After the explosion he began to tremble, and was still trembling on his trip back. Constantly trembling, he lived on at the front for a fortnight, but without eating; and, although he had been a good rifleman, he had lost all his former skill with a gun.
There was a delay of a month before evacuation, but the trembling did not cease, and he was passed through various units, to the neurological center at Villers-Cotterets, where he remained for two months,—April 13 to June 15, 1915,—with a diagnosis of hysterical chorea. He was examined by Guillain, who found, besides the generalized tremors, lively knee-jerks and Achilles jerks, an excessive emotionality, particularly marked when the guns were going or bombs bursting. Lumbar puncture yielded a perfectly normal fluid.
June 19 the corporal went to the Salpêtrière under P. Marie. July 14 he was evacuated to the civil hospital of Arcueil, where he remained till September 24, when he was sent home to convalesce, from October 26 to December 15.
He returned to the Salpêtrière December 15, 1915. Throughout these various movements from hospital to hospital, his status was unchanged. At the time of report about a year after shell-shock, he was still constantly and uniformly trembling. All four limbs were affected, perhaps the right arm and the left leg more markedly. There was no tremor[422] during sleep, but there was a tremor when the patient lay awake in dorsal decubitus just as when he was sitting or standing. The tremor was worse in the evening than in the morning, and the patient could get to sleep only very late. There was slight tremor of the head; the eyelids and the tongue showed a few tremors, which were not synchronous with those of the limbs. Nystagmus was absent. To diminish the effect of the trembling, the patient held his forearms flexed and kept his elbows close to his body. If the trembling of the legs got intense, the patient would rise and walk a few steps. Any movement, such as carrying a spoon or a glass to the mouth, led to an exaggeration of the tremors; and there was at this time a suggestion of the intention tremor of multiple sclerosis. The tremor was increased when the eyes were closed. Any sudden noise or sharp command, or recalling to mind of trench service, would bring about extraordinary motor crises, in which there was an intense and generalized tremor, so the patient would lose his balance. Any attempt at eliciting reflexes would produce generalized violent tremor. Sensations were normal; tendency to hyperidrosis; pulse in repose, 60, rising to 120 if one struck the table sharply.
Meige remarks that a number of examples of tremors suggestive of Parkinson’s disease were observed in the War of 1870. Might the explosion have caused properly situated lesions in the encephalon of such a nature as to produce a Parkinsonian tremor? The tremors were stationary, and if due to some lesion, the lesion remains now exactly what it was at the beginning. There was no digital tremor such as is characteristic of Parkinson’s disease. Moreover, the intention tremor of such a patient, rather than Parkinson’s disease, suggests multiple sclerosis, of which latter disease, however, there is no other sign. Nor does there seem any evidence that these tremors were of cerebellar, paretic, goitrous, or of any definite toxic origin. On the whole, Meige regards it as a neuropathic manifestation resembling what is found in traumatic neurosis. He believes that there is not sufficient evidence that it is the consequence of any structural change in the nervous system.
Meige remarks that the analysis of any case of tremor must take the mental state into account. This patient, perfectly conscious of his tremors and their critical exacerbations, was much chagrined thereby. He suffered mentally from his impotence, especially when bystanders would intentionally bring about his paroxysms. He looked like one shuddering from fear, and it is actually probable that he was afraid of his own tremors and shuddering. He was, besides subject to tremor, also a victim of tremophobia,—a kind of phobia described some years since by Meige, somewhat resembling ereutophobia, or fear of blushing, described by Pitres and Régis.
Four hours in a freezing bog: Hysterical glossolabial hemispasm twelve hours after rescue. No sensory disorder of face or tongue; sensory disorder of arm, but no motor disorder.
A man, 27, in good health, called on the second day of the mobilization, got into the line two weeks from mobilization, first in the West, and then, from mid-September, in the East. He was in the artillery and stood shell fire in a big battle very well.
However, December 27, 1914, while engaged in transport service, on the way back with his horse, he fell into a bog and gradually sank to his neck. Attempts to get the man and his horse out failed. All that saved him from drowning was the freezing of the bog surface. After four hours he was freed by his comrades, apparently frozen stiff, but with consciousness completely preserved. On the next day, at about five o’clock,—twelve hours after his release from the frozen bog,—he had a seizure. It began with headache on the left side and loss of consciousness that lasted 24 hours. The right leg was paralyzed and very painful. He passed through various hospitals and finally arrived at the Jena Nerve Hospital, January 25, 1915.
He was a tall, powerful man, with a slow regular pulse, accelerated heart sounds, lively dermatographia, increased muscular excitability, general increase of knee and Achilles reflexes (left greater than right), slight patellar and ankle clonus present on the left side, Babinski reaction absent, plantar reflex more lively on the left than on the right, but abdominal reflex more lively right than left. Head painful to percussion in the left temporal region. Touch and pain sense segmentally absent in both right extremities. Arm movements free; tremors absent. Active movements almost impossible in the right leg; on passive movement marked pain. Slight muscular tension about knee-, hip-, and ankle-joints.[425] The patient got about with a cane, trailing the left leg. Romberg sign.
The right angle of the mouth was withdrawn slightly upward and outward, and lagged a little in active movements. The protruded tongue deviated completely into the right angle of the mouth and there remained, but without tremor. The uvula deviated to the right, and the right palate was held higher than the left. Lively palatal reflex. Speech intact. The patient’s chief complaint was attacks of coughing, which increased his headache to the point of intolerability. A harmless drug caused the coughing and headache to disappear. The patient was a quiet, willing man, who industriously went through his exercises, and on the Kaiser’s birthday was already walking in the marketplace. His tongue contractions gradually improved. His body-weight increased.
In the course of two months the glossolabial and palatal contractions had largely disappeared. The walking movements of the right leg had improved, although there was still a distinct paresis, and a stiffness in the right knee and ankle joints. Climbing stairs was impossible on account of difficulty at the hip. March 30, 1915, the sensory improvement was marked. There was a feeling as though the last three fingers of the hand were asleep; walking was improved; he could walk one or two hours a day. The walk was still slightly spastic-paretic, May 28, when he was discharged.
It is remarkable that the hysterical attack had such a long incubation period in this case: twelve hours after his removal from the marsh. There were doubtless physical factors of refrigeration, on the one hand, and on the other, psychic factors of fear of sinking alive in the marsh, at the bottom of the phenomenon. The most marked feature, of course, was the glossolabial hemispasm. In the presence of this hemispasm, it is remarkable that there should have been no anesthesia or analgesia of the face, cheek, or tongue; and moreover the paresis of the right mouth and tongue was far less marked than the contracture. It is also striking that the right upper extremity, although it had sensory disorder, failed to show motor disorder.
Slight bruise by horse: Apparently invincible complaints of pain. Cure by single-handed capture of many Russians.
An infantryman was standing below an embankment when a horse fell upon him, bruising him slightly on the left hip. This infantryman later continually complained of pains in the opposite hip though there had never been a contusion there, nor anything felt there. These complaints could not be influenced by exhortation, by diversion, or by drugs. If they were purposely ignored, the patient reacted complainingly and in a way to suggest delusions of persecution.
Nevertheless, this querulous man soon proved an effective soldier in a storming attack in which the whole battalion distinguished itself, putting himself forward particularly. In fact, by himself he captured a whole group of Russians!
Thereupon all the pains in the hip ceased, nor did they recur so long as he was under observation. Morose and complaining before, he now became cheerful.
Kick in abdomen by horse: General spasticity; tremors; eye symptoms (e.g. monocular diplopia); convulsions. Improvement.
A cuirassier was kicked by a horse on left side of abdomen, November 24, and lost consciousness. A month later, in hospital, hardness and tenderness to pressure of abdominal wall, spastic muscles everywhere, pseudospastic tremor of legs, and complaints of double vision were noted. He also had attacks of convulsions, in which he became unconscious, twitchings appeared, but the tongue was not bitten. Urine was often involuntarily passed in these attacks, but he was not always continent outside attacks, as, for instance, in coughing.
On admission to nerve hospital: Right-sided monocular diplopia; mild ptosis; ocular movements free. Rapid tremor on shaking hands. Stood with straddling legs affected by vibrating tremor. Knee-jerks considerably increased. In the dorsal position movements of the left leg were accompanied by marked tremor. He even could not go to sleep easily on account of twitching of the left leg.
His comrades observed that he had convulsions at night, and often spoke in his sleep. Inoculation against typhoid fever was made early in December. Later, permanent rise of temperature to 37.8. Several attacks, lasting about ten minutes, came under observation of the physician.
In January, progressive improvement in the motor sphere and also psychically. The urinary disturbance likewise disappeared, but the spasms persisted.
Windage from a shell; fear; fall, unconscious: Homonymous hemianopsia (organic? functional?) with blinking and vasomotor excitability.
A volunteer, 19 (never ill; no nervous disease in the family) after a period of training went into the field October 3, 1914. November 5 a shell struck near his trench, but failed to explode. Up to that time everything had been quiet. The soldier had been looking out of the loop-hole, surveying the landscape. He felt a great fear, felt a blow in the neck, and fell down unconscious. How long he was unconscious is unknown. Sometime later he walked back with his comrades.
About an hour later, this volunteer—who was a very intelligent young man, possessing some knowledge of biology, including the nature of visual fields—noticed a black spot in the field of vision, which came and went, but after a few hours remained continually without disappearing. Otherwise there was no complaint except a feeling of dizziness when stooping.
Upon examination there could be found no disorder of the internal organs. Neurologically there was blinking, vasomotor excitability, slight reddening of the face, and dermatographia. An expert in ophthalmology confirmed the existence of a homonymous defect in the fields of vision. This defect could not be influenced by suggestion or by any other treatment, nor did any other change whatever occur in the condition.
Steiner inquires whether this hemianopsia is to be taken as organic or functional. The air-pressure of the shell hissing past might have produced a concussion, or the falling unconscious might have produced a commotio cerebri or a slight hemorrhage. The tic-like blinking and vasomotor excitability, however, suggest functionality.
Shell-shock PSORIASIS. Post-traumatic eczema.
A soldier, 28, came to the Saint-Louis skin clinic, May 15, 1916, for leg lesions three months old. These lesions were cicatricial, squamous, irregular-contoured, and had developed following a wound. The lesions were eczematous.
On the trunk, arms and elbow were lesions of psoriasis. These lesions had appeared after shell-shock. The man had been bowled over June 16, 1915, by a marmite. The psoriatic lesions appeared shortly afterwards. The patient had never seen anything of the sort before.
In this case the trauma provoked eczema; the emotion, psoriasis. Gaucher and Klein say that they have been struck by the recrudescence of psoriasis since the outbreak of the war, and remark, also, that there has been a relative increase of new cases since July, 1914.
There are cases of psoriasis following nervous shock, emotion and trauma. Sometimes the psoriatic lesion develops upon the scar of a wound. In the above case, as in the case of a woman of 25, a refugee from the Arras bombardment, the psoriasis began de novo and slowly developed immediately after the catastrophe of the Jena. Five, possibly six, out of eight cases totaled, appear, unlike the case sketched above, to have developed in cases either tuberculous or of tuberculous stock.
Re psoriasis, Vignolo-Nutati remarks that this is a relatively frequent skin disease amongst Italian soldiers. He states that many of these cases are due to nervous shock. Some are related to wounds appearing near the scars. In all cases an emotional disturbance is the chief cause. Vignolo-Nutati had 86 cases of psoriasis in six months, 52 of the men coming from the front. Eighteen of the men said that they had not previously suffered from the disease.
A sergeant gets the CROIX DE GUERRE and SHELL-SHOCK together: Transient deafness; later pseudohallucinatory electric bell ringing, reminiscent of civilian work; stereotyped movements, reminiscent of war experience.
A sergeant, 24, had worked about Parisian hotels from the age of thirteen and a half. He won the croix de guerre and was evacuated for his wounds April 24, 1915.
It seems that he carried the remains of his company, which had been decimated the night before by a mine explosion, on to the enemy trench, getting there first and facing three Germans, whom he beat down. At this time, gas shells began to rain about. Making a number of violent expiratory movements to get rid of the gas, he found himself unable to progress on account of the fall of the shells, and sat motionless with his hands before his face. He was cast to the earth by an explosion, which at the same time blew off a revolver which the wounded lieutenant had passed to him. He sat up, and, observing that the soldiers had gotten the trench, went back to the lines, where he told his story.
He then found that he was deaf, and wounded in the left leg. The wounds rapidly healed, but sundry other symptoms developed. He had a peculiar sensation back of the forehead. He could not think, read or write and was very weary. He got better in a few months, but disorders kept returning.
His deafness had left him in about a fortnight, but when his hearing came back spontaneously, there were peculiar sensations. He constantly heard an electric bell, intense and continuous, like that of a French cinema advertising its films. The sounds seemed to begin in the ear and to run out as a sort of whistling. This sensation was preceded by buzzing and associated with noises like those of a musical triangle or a steam whistle. The noise kept up during waking[431] hours, but was often forgotten while he was at work. In sleep he heard nothing, except sometimes battle noises. August 20, 1915, he was given the diagnosis: labyrinthine shock—hearing returned.
About ten weeks after evacuation, when the headaches and thought blocking began to disappear, a generalized tremor, especially of the head, set in, which the patient called St. Vitus’ dance. Then a peculiar gait began, which lasted several weeks and then transiently reappeared. Every few steps his legs would bend, and he could only walk forward in the attitude of a man who is concealing his height. After resting a few minutes he began to walk regularly again and the cycle began over again. He had to walk with two canes. If he felt some sudden emotion, or sometimes without any obvious reason, he would stop short and look straight ahead, with body bent, and arms before his face. This would last but a moment, whereupon he would walk again normally.
When this anomalous walking disappeared, curious face movements and gestures began. If a strange person arrived, the forehead and eyebrows would contract, the eyelids would stand wide, which gave him an expression of surprise lasting a few seconds. At the same time the mouth would open and remain so for some moments. A forced expiration would be executed, suggesting a fish out of water. He would then imperatively strike the table with his fist, or the ground with his foot.
Laignel-Lavastine and Courbon explain the anomalous movements as stereotypies due to secondary automatism. They are not convulsive, are not preceded by emotion or followed by a sense of relief, and are not tics. They are gestures and postures without present significance, but adapted to certain former circumstances. The electric bell effect is a sort of pseudohallucination, differing from true hallucinations in little except the absence of the externalizing feature. The stereotypical movements are reproductions of things done in the battle, and the pseudohallucinations relate to the former hotel work of the soldier.
Cinema worker, two days after being waked up by a shell, develops a nystagmiform tremor of eyes and tachycardia. Graves’ disease? Tic (“occupational virtuosity”)?
A soldier was waked up with a start Sept. 22, 1914, by a shell burst. The man was not wounded or shocked, and merely felt a good deal moved. The next day but one he felt a little movement of his eyes, which was at first intermittent but in three or four days became continuous and troublesome. These movements were those of nystagmus, almost transverse and very rapid, and suggestive rather of a vibratory trembling than of a true nystagmus of the eye or of labyrinthine disease. When the patient fixed an object, the nystagmus would stop for a few seconds and then immediately reappear. There had never been any vertigo, nausea, vomiting, deafness, ocular disorder, or disorder of equilibration. During the tests for nystagmus, the morbid nystagmus would stop and be replaced by the normal nystagmus which was obviously slower and more regular. The condition had persisted from September, 1914, to the meeting of the Neurological Society, April 15, 1915. The patient said he had become very emotional and got palpitations on the slightest occasion, such as a fast walk, going upstairs, or hearing a loud noise. There was also a slight vibratory trembling of the fingers and a permanent tachycardia (120-140 beats). Tinel regards the case as one of neurosis, due to a neuromuscular hyperexcitability comparable in some ways with that found in Graves’ disease.
Meige, in discussion, called attention to the fact that not every nystagmus is of organic origin and that there is a rare form of tic of nystagmiform nature. The victim in this case was an employee in a moving picture house, and very possibly his occupation had permitted him to utilize what Meige speaks of as a “occupational virtuosity” of the eye muscles.
Synesthesialgia: FOOT pain on rubbing dry HANDS, following bullet wound of leg.
A foot chasseur was wounded, September 15, 1914, low in the right thigh, a bullet entering outside the biceps tendon and emerging on the inner aspect of the leg, 4 cm. below the knee joint. He at once began to feel pains in the right foot, which grew swollen and red. The leg began to flex upon the thigh and, after straightening under anesthesia, was placed in plaster. An arteriovenous aneurysm developed in the popliteal space; operation, October 22nd, followed November 1, by ligature. The pains in the foot grew better after this operation; but as soon as the wound was cicatrized they came back again as before.
For seven months the foot pains remained sharp and continuous, such that the man could not leave his bed. If a bright light struck his eyes, the pains grew much more marked, especially in the morning on awakening. The patient found that when his hands were dry he could not use them because of the violent pains which rubbing them would cause in the right foot. Accordingly he kept putting his hands to his mouth to moisten them. Finally he kept a wet rag by him which he could pass from one hand to the other.
The pain was what made walking difficult. Foot movements were only a bit less ample on the affected side than on the normal side. There was a general muscular atrophy of the lower extremity (30.5: 34 about calf, and 40: 49 about thigh). Right knee-jerk more lively than left. Right Achilles jerk absent. Negligible disorders of electrical excitability in the territory of the right sciatic nerve. The skin of the foot was a little thin and pale; the temperature was low; and the nails had transverse striations. The pains grew gradually a little less marked, but if the room temperature was increased or lowered or if the foot became cold, the pains became extreme. Pressure on the popliteal[434] space produced pain on the external border of the foot; likewise pressure on the calf. Lasègue’s sign could not be tested for on account of the contracture of the flexors of leg on thigh. Due to the direct action of the bullet, there was an objective hyperesthesia of the dorsum and sole of the foot. The toes were anesthetic. A cold foot bath increased the pains, and a warm foot bath diminished them (contrary to experience in analgesias).
This was a case of synesthesialgia in the right foot, brought about by rubbing dry hands, exactly as if there were a direct contact with the foot. Milder painful reactions were brought about by bright lights and loud noises; but on the whole, these other effects were insignificant. It must be remembered that the man was wounded and plainly had also organic nervous disorder. He sometimes complained of radiations of the pain up to the left hypochondrium, and sometimes he showed the classical sensation of “esophageal globus” (lump in the throat). In short, there was in him a special excitability of the nervous system which may partly explain the synesthesialgia.
Shell-shock; burial: Clonic spasms; later, stupor with amnesia.
A reservist, 28 (laborer in civil life, of a nervous family; even before mobilization had attacks of weakness at his work or in the company of others) January 3 or 4, 1915, fainted in the trench while shells were striking around him. On January 5 he was brought to hospital in deep stupor. He went to the reserve hospital at N. by hospital train, January 8, and arrived at the Tübingen clinic January 18.
A slip of paper stated that after burial in the trench he had been brought from the field unconscious. Clonic spasms of the upper part of the body are said to have occurred. At the reserve hospital in N., January 10, he was still unconscious, at times twitching his face and the upper part of his body, and once at night excited and delirious.
At first in the clinic he was apathetic, speaking not a word, looking vacantly into the air as if lost in a dream. He went to the section passively, and lay passively in bed.
In the examining room, he stood speechless with unemotional face, sometimes looking up to the ceiling, slowly scratching his head, failing to answer questions, although fixing his eyes upon the physician. He could not be communicated with in writing, playing uncomprehendingly with the pencil or scratching his head with it. He would start with fright at a sudden noise or an unexpected touch. Sometimes he would heave a deep sigh, grasp his head in his hands, or lay hold of his hair with a hopeless expression of face and shake his head to and fro.
Next day, January 19, he made a few slow, low answers. He was found to be entirely disoriented and with associations impeded, although he could get out his name and residence with difficulty. Some of his color identifications were correct, such as red and green; some impossible, as yellow, brown, violet. A comrade who was called in and could speak the Cologne dialect, was talked with at first with difficulty,[436] later more easily. Although the patient was visibly freer, he remained without apparent emotion, retaining a rigid and dreamlike expression of face. It was hard to find words, although objects were named correctly, and there was no paraphasia or agnosia. Vision and hearing were normal; walking, manual movements, eating were all undisturbed though slow. The patient had to be led to the toilet. It seemed as if all intellectual life was at rest, and that in the absence of impulses from without, there would have been complete apathy. It was made out that the patient thought he was still in the trenches.
Next day, the stupor had decreased and the patient spoke, getting his bearings for a time. There was a complete amnesia as to the cause and duration of his condition. During the next period, up to the beginning of February, 1915, consciousness cleared and the apathy was replaced with anxiety, weariness, and a dull headache.
During February, the patient gradually returned to his senses, and remained in a state of general nervous exhaustion. Amnesia was complete for at least two weeks of his life and recollections were fragmentary for the first three days of his stay in the clinic. He worked willingly in the garden with the other patients. On February 26, the patient was cured and went back to the reserve battalion in a much strengthened condition.
Battles (including liquid fire); eventually shell-shock: Hallucinatory delirium, mutism, asthenia—after a few days puerilism (history of convulsive crisis in adolescence) with regression of personality to late childhood.
Puerilism (Dupré) appeared in a soldier, 21 (uncle and cousin insane; patient had difficulty in studies at fourteen and nervous spells for two years, with loss of consciousness, fall and convulsions probably at rare intervals; a student at eighteen) after he had taken part in a number of battles with the Chasseurs Alpins. He was exposed once to liquid fire July 21, 1916. He entered the military psychiatric center at Amiens. Mental troubles had followed the bursting of a shell near him. He said a few words, such as, “Alsace; fire; blood; snow; it hurts.” These phrases, spoken in a low tone, with an anxious appearance, eyes fixed, suggested hallucination. He seemed to be listening. Aside from the isolated words above mentioned he showed complete mutism. There was physical weakness, difficulty in walking without support, exaggeration of patellar reflexes, pains in the head and limbs. After several days, he said, “Milk; bread.” After this the anxiety and the slow and difficult walking disappeared, whereupon the puerilism appeared.
Now the soldier began to run instead of walking. He galloped and gamboled like a child imitating a horse, or he would sit on a board seeming to paddle. He would skip along the halls. The puerilistic phases were rather brief and for the most part he lay in bed. There was still a certain asthenia. He made little paper boats in bed, keeping them in a small metal box along with bits of bread, looking glass and the like. If a gesture was made to take them away, he would protest and press the box to his breast, looking childish and anxious, and if the box were taken he would weep hot tears. Sometimes he would stick out his tongue at the attendants. His mother came to see him and afterwards he[438] would say, “Mamma told me to be good, to eat well, to get well and to go home.” He would use childish grammar,—“Me eat much.” Asked why he had hollowed out a small hole in the wall of the room, he answered, “I did it for fun, but I will not do it any more. Mother doesn’t want me to.” The patient was unwilling to answer a question correctly; would sometimes answer incorrectly at first and correctly afterward.
It appears that the man had adopted the language, occupations and attitude of a child, showing a regression of personality ten to twelve years backwards. There was a neurotic basis in the convulsive crises of adolescence. On the basis of this predisposition following shock there appeared an attack of confusion, upon which, several days later, supervened ecmnesic phenomena of hysterical nature assuming all the features of puerilism.
Bomb-dropping from airplane; unconsciousness: Battle dreams. Leaves of absence failed to relieve. Episodes of dizziness and fugue.
M. Alessandro, Class ’79, baker (father a drunkard; brother an idiot, in asylum), had typhus in youth, and as a boy had periods of intense “pavor nocturnus,” but no convulsions. He enjoyed good health in the army before the following event:
On July 13, 1915, a bomb, dropped by an airplane, fell near an Italian soldier, killing many comrades, and throwing the man to the ground unconscious. He awoke several hours later at a hospital in a stunned condition. During the night, under the influence of terrifying dreams, he would leave his bed to look for enemies who, it seemed to him, were throwing stones and firing. He managed to grasp a rifle and fire at the images he saw. He was given a 60 days’ leave of absence during which he did not improve; and then again 90 days’ furlough, which he spent at his home, where terrifying dreams, tremor of limbs and asthenia continued.
He came under observation February 10, after his second leave. Nutrition fair. Insomnia. Constant terrifying dreams. Coated tongue. Tremor of hands, head, body, ceasing during voluntary movements. Episodically he had spells of dizziness followed by absent-mindedness, whereupon he wandered aimlessly about, of a sudden becoming aware of being in a place, but not knowing how he came there.
Special senses intact. Several points of cutaneous hyperesthesia, particularly mammary and pseudo-ovarian on the left, pressure whereon provoked a lively emotional reaction with acceleration of pulse, redness, lacrimation. Knee reflexes lively, cutaneous reflexes normal, except the plantar which were very lively. Restless, hyperemotional, he wept for insignificant reasons and wanted to leave hospital for fear of dying there. He was discharged unimproved after a fortnight.
Nostalgic temperament; depression on entering service; rheumatism. A box falls from an airplane near by: Fear and tears; later depression, nostalgia, dreams, hyperthyroidism.
An Italian private in the infantry was recalled to military service. He was a small farmer, and being disposed to homesickness, grew depressed from the day he left for service. His sleep was disturbed, he was greatly affected by the wet and damp of the trenches, and was in a state of continual fear. Finally, pains, hypersensitiveness, and fever developed.
As an enemy airplane passed over one day, a box fell at the man’s feet and threw him into a profound fear with tears. He was conducted to a tent to rest; his regiment was shortly sent to the rear, and he remained on active service for a few days despite the fever and pains. Finally the swelling of his leg compelled him to take to bed. (Fatigue in antebellum life had always shown itself in aches of the legs.) He had now been in active service about a month and his homesickness overcame him. He was in a state of deep physical and mental depression. It was not his own troubles so much as those of his family which preoccupied him. His knees hurt him so that he had to weep; or if Sardinia was mentioned, he cried, and said, “Oh, how I love Sardinia!” He grew fatigued very easily. He had many dreams about Sardinia, his father, and the war, especially dreaming about being wounded in the legs (question of being stimulated by the joint aches). The reflexes were normal, though slight tremors set up in the legs after testing. The thyroid gland was somewhat swollen, and it appears that the patient had noticed this five days before entering hospital. The patient was rather vagotonic; pulse-rate stood at 56; oculocardiac-reflex, 56-84; Mannkopf negative; Thomayer and Erben marked (56-88 and 88-60); von Graefe marked; Stellwag present.
A shell pitches without bursting: Unconsciousness; stupor; MAMA MIA!; oniric delirium; amnesia. Recovery in five weeks.
An Italian soldier of the Class of ’95, a mechanic (mother cardiac; as a boy, pains in joints and heart; since boyhood, no illness), had a big Austrian shell pitch near him, July 23, 1915. The shell failed to explode and injured no one. The patient, however, fell to the ground, unconscious, and remained in the camp hospital for two days, quite immobile. This event followed an advance by his company under very fatiguing circumstances without sleep for a period of four days.
July 26, the patient was observed in profound stupor, non-reactive, constantly and monotonously repeating the phrase, Mama mia!, with fixed gaze and smiling as if at visions. He swallowed food. The pupils reacted poorly to light, and the cornea and nasal mucosa seemed anesthetic. The tendon and skin reflexes were lively. The muscles were hypotonic; bradycardia, 56; no control over feces or urine.
July 27-28, restlessness at night, gasping movements, and poses of terror.
July 29, he called for his mother, who had been dead for several years. He was still stuporous and insensible.
From August 1 to 10, he improved slowly and became able to carry bread to his mouth after it had been put in his hands. He still did not speak and made signs when he wished to urinate or defecate. Pulse 50-60.
August 12, the patient began to react to intense light and to pain stimuli, as well as to pressure. He ate voraciously.
August 15, visual stimuli were responded to, the pulse had risen to 80, the skin reflexes were no less lively. There began to be terrifying dreams at night, with motor reactions.
August 17, the patient looked about more alertly, promptly seeing bread when placed in the center of the field of vision and saying words to the man who might try to remove the[442] bread. He did not yet react to acoustic stimuli, nor was there any other change up to August 21.
August 22 a notable improvement set in. The hearing was now slightly diminished, questions were answered after a brief refractory period. After a few questions, however, a state of exhaustion would ensue, which would disappear only after a short rest. There was amnesia for the entire period following the day of his departure for the front, May, 1915. At this time, instead of eating voraciously, he showed anorexia. The skin and tendon reflexes, instead of being lively, were now dull. There still were battle dreams of enemies trying to kill him.
August 25, there was an area of hypesthesia on the inner aspect of the right thigh, but otherwise no disorder of sensation. The pulse stood at 80 and there were no other neurological phenomena.
August 31, the patch of hypesthesia of the thigh and the retrograde amnesia disappeared. There was still a slight diminution of hearing. The accident of the non-exploding bomb could now be recalled, but there was a memory gap for all facts up to the latter part of August.
September 2, dreamless sleep; no signs of abnormality except a slight diminution of hearing. Discharged, well.
Jostled carrying explosives; no explosion; unconsciousness: Deafmutism and foggy vision. Gradual recovery from these symptoms. Then, on rising from bed, camptocormia.
An Italian of the Class of 1891 (convulsions and pains in the spine, with rigidity, as a child; typhoid fever at 18; brother sickly, neuropathic; mother subject to periodic convulsions; father alcoholic and nervous), on the night of November 26, 1915, was carrying a number of tubes of explosives. A comrade stumbled and fell over the soldier, who fell to the ground unconscious. None of the glycerine tubes exploded, and none of the soldiers round about were hurt.
The man regained consciousness at the camp hospital, but remained deafmute and also impaired as to vision. It was as if a screen of fog lay between him and objects seen.
During fifteen days of observation at the camp hospital, he had terrible war nightmares. The mutism, the visual disorder, and the deafness then gradually disappeared without special treatment.
However, when the patient rose from bed, it was found that his lumbar vertebral column was stiff. He walked bent forward and was unable to bend or straighten the back. There was a hyperesthesia along the vertebrae, especially on pressure. X-ray examination showed no bone lesion. The larynx and cornea were sensitive, and the plantar reflexes were absent. The abdominal reflexes were present. The pupils reacted to light and accommodation. There were two areas of analgesia in the nipple regions. The expression of the patient’s face was relaxed and drooping.
A heavy cannon slides and grazes a man: Unconsciousness; stupor; amnesia (anterograde amnesia persistent). Complete recovery in less than seven weeks.
An Italian soldier of the Class of 1895, a peasant (family healthy; non-alcoholic; good scholar) was, July 19, 1915, helping drag a heavy cannon up hill. The big gun slid, hit several men, and grazed the patient, making a slight abrasion on his leg. He immediately lost consciousness, and arrived at the camp hospital in a stupor, which lasted so long that catheterization was necessary.
A week later he was observed in hospital, immobile and non-reactive, with a swollen abdomen and fecal impaction. The pupils were widely dilated and reacted poorly to light. The corneal reflexes were absent, and the nasal mucosa was anesthetic. Pulse 50. The patient failed to eat. Next day there was no change in his condition. He was quiet throughout the night.
On the morning of July 29, a number of answers were obtained to questions put in a loud voice, though he was unaware of much more than his name, being ignorant of the name of his country, his age, his division, where he had come from, what had happened to him, or where he was. He had now begun to eat spontaneously.
During the following days, up to August 4, the amnesia gradually dissolved for the facts before the trauma. He remembered having been greatly frightened at the time of the accident but could not remember the accident itself, and the gap for subsequent events was still complete. The pharyngeal reflex was still poor. August 5, he began to remember the details concerning the accident. About the middle of August there was no longer any diminution of hearing and ideation became more free and rapid.
September 4, he was discharged, well.
Shell explosions SEEN: Emotion; insomnia. Artillery HEARD twelve days later: “finished off.”
A lance-corporal, 36, had had a nervous debility four or five years before the war, caused by an overstudy of music. He had not stopped work at that time, but suffered from depression, anorexia, and insomnia, lasting for some weeks.
The lance-corporal got on well at the front for 11 weeks, until finally eight shells pitched near him. Although he was unhurt, he began to suffer from anorexia, insomnia, and depression. While in billets 12 days later, some English artillery became heavily engaged, whereupon “The noise promptly finished me off.” The insomnia, depression, and anorexia became more marked, and the patient could not sleep unless heavily drugged.
Shell-shock: Emotion. More shells: Insomnia; war dreams. Head tremor and tic, two weeks after initial shock.
The psychic trauma is, according to Wiltshire, more important than physical trauma in the following case of a sergeant of infantry, 28, a man without neuropathic taint. This man had been nine months at the front and through Mons, but had been quite well until three weeks before coming to hospital.
“Twenty-three days ago, I was issuing rations when they got the range of us—and killed the other chaps. I got blown away and knocked over. I saw everything—fellows in pieces. Then a second shell came. I got lifted and knocked about ten yards.” Then he began to shake but carried on.
Two days later, “Shells dropped on the dug-out and killed the other chaps. I have not slept properly since this. If I go to sleep, I wake up seeing people killed, shells dropping, and all kinds of horrid dreams about war.” One or two of the men killed had been pals.
A fortnight after the first incident, while in a base hospital, head-shaking began. The patient would jump at the least sound. There were spasmodic tic movements with the extension of the head, protrusion of lower jaw, and contraction of occipitofrontalis muscle. Sometimes the left shoulder girdle was affected in the same way. There was a slight fine tremor of hands and eyelids and difficulty in keeping the eyes fixed on an object.
Hyperthyroidism, hemiplegia, irritative symptoms after exhaustion (by heat?).
A man (not previously nervous, no faulty heredity, heatstroke August 21) suddenly fell down in a great heat, after a fatiguing march, and remained unconscious for several hours, waking with vertigo, headache, paralysis of left side, vomiting, and twitching of the face. On September 23, admitted to reserve hospital. Knee phenomenon increased. Urinary retention; catheter used. Speech disturbance, facial twitching. Vomiting had stopped September 10. Catheterization could be avoided through warm sitz-baths. October 30, on sitting up, occipital pain and vertigo. November 15, urinary symptoms improved. Also improvement otherwise. December 1, gait vacillating and uncertain. Headache. Admission to nerve hospital, December 3. Here complained of twitchings in the frontals and corrugators. Wide palpebral gaps. Rare, or absent, movements of lids. The extended hands showed active, rapid tremor. Tendon phenomena increased in the arms and especially in the legs. Abdominal reflexes increased. Active tremor in the legs. Gluteal tremor. Very pronounced Graves’ symptoms. Syndactylism very pronounced in the feet, between second and third toes. Later on, improvement under half-baths, etc. Worse after ten days’ leave of absence, especially marked increase of tremor (rest tremor), augmented on movement.
Re heat stroke, Wollenberg has called attention to the effect of the heat of the summer months upon German soldiers. Cases of heat stroke have not been rare in the German army. About half the cases have convulsions or epileptoid seizures, as well as tremors and nystagmus. About a quarter of the cases have shown confusion and delusions, with anxiety and mania. A degree of mental impairment has followed a number of these heat strokes, together with sundry signs of organic disorder, such as reflex changes, pupillary changes, and difficulty in speech.
Forced marches; skirmishes; rheumatism: Generalized TREMORS. On the road to recovery in six months.
A German letter carrier, 27, entered the war at the outset, made forced marches in great heat, was in a number of skirmishes and in the capture of Namur, and fell ill early in September, with swollen and painful right foot and rheumatic pains in knees and shoulders. He was put on garrison duty; but the rheumatic pains in the joints increased toward the end of September, and he was treated in hospital for rheumatism.
He became able to walk only in the second half of December, marked tremors affecting the whole body. His bodily condition had been good. He slept well, and while at rest in bed he felt entirely well; but upon every attempt to get up and put his feet down, these violent trembling motions would always reappear. Treatment by hydro- and electrotherapy remained entirely unsuccessful. February 8 he was transferred to a nerve hospital.
He had been in the postal service from 1903. He was of normal bodily and mental development and had had no previous illnesses. His military service had been executed from 1909 to 1911. He had always been a passionate smoker but had not abused alcohol. His mother is said to have been for some time paralyzed, following a fright.
Physically, the patient was a slender but strongly-built and fairly well-nourished soldier. The first sound at the apex of the heart was rough and impure, and the heart was somewhat enlarged to the left. The pulse was irregular, 106. The arteries were somewhat stiff. Neurologically, there was a marked dermatographia of comparatively long duration. The periosteal reflexes were increased; the deep reflexes could not be properly examined. The whole leg trembled and heaved unsuccessfully on attempts to raise it voluntarily. After even a slight stroke on the patellar tendon, the trembling became excessive and irregular, and[449] the leg passed into a heaving spasm which would outlast the percussion for some time. The patellar clonus could be obtained with the knee extended. The shaking movements were somewhat more marked on the right than on the left side. Similar phenomena occurred when the Achilles reflexes were being examined. The triceps reflexes on both sides were increased but there was no tremor or spasm of the arms. The plantar reflexes were very lively, and following these reflexes appeared tremors of the legs. When the spinous processes of the vertebral column were percussed, a general shaking spasm appeared. Tactile sense was everywhere normal, but the pain sense was increased. Upon slight pin-pricks in the skin of the legs, there would occur a marked shaking spasm of the leg, passing directly to the other leg. These phenomena were more marked on the right side than on the left. When sitting upon a chair with back supported, a slight tremor would appear when the hands were raised and stretched out, more markedly on the right side than on the left. Movements of the arms were normal. However, the hand-grasps were: right, 105; left, 80. In dorsal decubitus the movements of the leg were performed comparatively well at first, but after a few repetitions, the shaking spasm would occur on both sides, and the movements would become very awkward. The heel-to-knee test would then fail. If the patient were put on his feet, he would immediately fall into spasms, first in the right leg, then in the left. The trunk would now be involved, and soon the arms, whereupon the whole body, with the exception of the head, would be seen trembling and shaking, and the patient would fall forward, trying to get support by leaning against a wall, seizing a chair, or sinking down slowly. The spasms disappeared at once in dorsal decubitus and in sitting with supported back. Outward irritation by the acoustic, optic or tactile avenues would bring out spasms in the legs, always more markedly on the right side than on the left. Psychic irritations would cause spasms. The muscles of the limbs were held in great tension, the flexors and extensors being alternately affected. When the patient was moving along a wall with a difficult, swaying gait, his efforts[450] reminded the examiner of the attempts of a heavily intoxicated man to walk. Upon attempts to create passive movements of the lower limbs, severe shaking and trembling movements set in, followed by a general spastic tension of the leg musculature such that it could not be further flexed or extended.
The patient was put in the psychiatric section, as too seriously ill for the nerve hospital. He improved after a few days, being then able to walk without much support although still with some shaking and tremor. If his attention was diverted, passive movement of the leg could be carried out without developing spasm. He was treated in a room by himself with removal of all outward irritation. His legs were treated for an hour, three times daily, by means of moist packs. On account of complaints of insomnia he was given small doses of hypnotics.
The main thing here, according to Binswanger, is the psychotherapy. The patient was told almost daily in the course of conversation, first, that the illness was being cured; secondly, that upon recovery he would be employed in the future only on the postal service. He was told that he would have to avoid marked physical exertion, of course, but that he still would be fit for office work and could serve the fatherland in this way. Still he could not be transferred back to the hospital, he was told, unless he became entirely well, so that he could move with perfect freedom.
February 23 the patient was performing daily exercises in walking and standing; the spasm became very slight on standing, and often would entirely cease, but it remained still plainly present in the legs; the trunk and arms were free. External irritations were now less prone to excite spasm. Sleep became quiet and dreamless. He was transferred to the nerve hospital, able to move about freely in house and garden and only tremulous after long walks and considerable bodily and mental fatigue. He was given a week’s furlough home. He wished very much to get into the postal service; at the time of the report he had not attained this goal. He had renewed attacks of trembling upon exertion, and was transferred at the end of June to a convalescent home.
Shell-shock; emotion: Hyperkinesis, fear, dreams.
A private, 21, was with 30 men carrying sandbags in the daylight, under shell fire. He was thrown into a deep hole by an explosion, climbed out, and saw all his mates dead.
He was admitted to the Fourth London General Hospital, June 20, 1915, having been at Boulogne for a fortnight. He was lying in bed on his back, making continuous jerky lateral movements of head, and movements of arms, especially of the left arm. He was groaning slightly, now and then raising his eyelids with a staring expression of bewilderment and terror. He was able to mutter answers to questions. He would occasionally raise his right hand to his forehead. If he was observed, these movements became exaggerated. They ceased in sleep. He muttered even when unobserved. He continually said, “You won’t let me back.” Asked as to dreams, he replied, “Guns.” Voluntary movements were made, which prevented obtaining reflexes. When his pupils were to be examined by a man in uniform, he showed a marked facies of terror; his pupils were dilated; the eyes opened wide, the brows were furrowed, and there was an anxious scowl. The flash of an electric light produced the same effect.
June 24 the patient was much better. He said the explosion which had killed his friends after he had been only a few weeks at the front, was the first serious event in his service. He kept seeing it again, with bright lights and bursting shells. Sometimes he would hear the men shouting. In dreams he both saw and heard shells and men. There was pain in the back and right side of the head.
June 26 he was improved but still had pain in the back of the head, especially when trying to remember, and a slight tremor of the hands. He had been given hot baths at Boulogne on account of being very cold and shivering. He had always felt sick at the sight of blood. He was boarded for Home Service six months after admission.
Shell fire and barbed-wire work: Tremors, anesthesias, temperature and pain hallucinations.
A corporal, 39, had been working under shell fire at barbed-wire entanglements. The man was big and robust, but much depressed, complaining of noises in the head, pricking pains, unsteady legs, fatigue, irritability, loss of confidence. He showed tremors of arms and legs on movement, and stood unsteadily with eyes closed. He said: “My legs have been very unsteady, especially when some one is looking at me. They must have thought me drunk at times.”
The head and tongue were tremulous, the knee-jerks exaggerated, the soles insensitive to touch and pain; but sensibility to deep pressure was retained. There was a gradual return of right answers on further trials, aided by comparison with effects of stimuli applied to the dorsum of the foot. Though he gave correct replies on heat and cold tests over the arms, he gave wrong answers over the dorsum of the feet, less often over legs, sometimes over thighs.
Later during examination, the feet became tremulous. He felt a “silly childish fear,” and his hands began to feel cold and clammy; whereupon he began to reply hot or cold when the tubes were not applied at all (temperature hallucinations). There were apparently pain hallucinations in the soles and errors in response to the compasses.
Re the temperature hallucinations noted by Myers, these are to be distinguished from true vasomotor disorders. Babinski believes that he has definitely established that, though hysteria may cause a slight thermo-asymmetry, yet never a definite vasomotor or thermic disorder.
Re hysterical pains, the most frequent are probably those of hysterical pseudo sciatica, in which true signs of sciatica are absent, namely, (1) loss of Achilles jerk, (2) scoliosis, (3) Lasègue’s sign (pain on thigh flexion with leg extension), (4) Neri’s sign (with trunk bent forward, affected knee flexed), and (5) Bonnet’s sign (pain on thigh adduction).
Shell-shock: Emotional crises; twice recurrent mutism; amnesia. A comrade in the same explosion gets off with transient phenomena.
December 15, sitting back of a wall were three minor officers and an homme de liaison, when a 105 shell punctured the wall and burst, killing one and wounding another severely. One of these, a sous-lieutenant, lost consciousness for a quarter of an hour and had some severe headaches for a few days, but nothing more. The other, the homme de liaison, was found standing, bewildered, looking at the dead. When his name was called, he jumped and started off, weeping and crying out.
When caught, he was still somewhat clear, recognized his superior officer, answered yes and no, but kept asking, “Where is the other?” Next day he kept weeping and said not a word.
He was evacuated through a series of hospitals and was sent to convalesce with his sister at Montpellier, having now got back his speech. He had a seizure of fear in the street and was picked up by the police and was carried to a general hospital January 21. Here he could not speak, could hardly write, being unable to find his words. He walked slowly, bent over, eyes abnormally wide open, with a look of terror. The lighting of a match made him start off weeping. The symptom picture included tinnitus, vertigo, deafness, some reduction of the visual field (especially on the left side), hypesthesia and hypalgesia on the left side, hyperalgesia on the right, painful points (epigastric, inguinal, supra and infra mammary left), reflex, muscular and tendon, hyperexcitability on right side, jactitation, impairment of recollective memory, complete memory gap for the accident and everything thereafter, retentive memory reduced, imagination impaired, nightmares (awaking with a start).
A few days later he was able to pronounce his name with difficulty and to say yes and no. February 4 there was an[454] appendicular crisis, whereupon mutism became absolute again and lasted into May, despite suggestive therapy.
May 10, improvement in memory for things before the accident grew better, nightmares had become less frequent, the jactitation had continued.
There was no neuropathic predisposition in this case except infantile convulsions in two sisters, followed by nervous crises in one.
Re appendicular crisis, which was the occasion of a relapse in mutism, see remarks under relapses under Case 292.
Re mutism, Babinski counts mutism, hysteria major, and rhythmic chorea as so characteristically hysterical that no nervous disturbance of an organic nature can resemble them. The description of hysterical mutism is due to Charcot. According to Babinski, mutism is just as curable as hysterical deafness, and perhaps more curable. Yet mutism persists unchanged for many months unless it is treated properly by some form of suggestion. “It may be almost said that a subject suffering from speech defect, who nevertheless succeeds in making other people understand by all sorts of varied and expressive gestures the circumstances of his condition, is a hysterical mute and not an aphasic.” According to Babinski, no true case of hysterical aphasia has been published since the beginning of the war; all the cases have been cases of mutism.
Shell explosion; fainting: Hysterical crises of emotion; fright at a frog in the garden. Hereditary and acquired neuropathic taint.
A lieutenant, 28 (mother nervous; father had nervous spells at fifteen; patient himself nervous as a child), was under a great moral strain at the outbreak of war, and was utterly exhausted in a hard battle that lasted more than twenty-four hours.
A shell burst near him September 25 at the Somme, whereupon he fainted. He was evacuated to Amiens for three weeks; kept his bed; somnambulistic; subject to nervous crises.
He passed to the hospital of Ferté-Bernard for a month, the crises becoming more frequent. He was sent to a convalescent dépôt for three days, thence for three months to La Plisse; got better; lived at home, but went to a show where they played the Marseillaise, was profoundly moved thereby, and had more crises; accordingly went back under medical care and finally to his dépôt, where, upon seeing his old comrades, he had more crises, and was finally evacuated to the neurological center of the Eighth Region.
He there seemed mistrustful when asked to tell his story. There was a noise of cannon, whereupon he got up, ran in all directions in the garden, bumping into trees in the greatest terror, yelling, “There they are!”; gesticulating, soliloquizing: “Bomb! Shell! Bayonet!” His pulse was rapid. After he was calmed down, he began to talk again in a very clear, distinct, somewhat tremulous voice. A metallic sound made him shudder and cry out, “The drums!” and another scene of rushing about followed.
In the consulting office he wept. Battle dreams and nightmares, soliloquies and terror, seminal losses, occurred during the next few days.
August 4, while alone in the garden, he heard a noise, went toward it and spied a frog, whereupon he had another crisis[456] of fear and emotion. He got another lieutenant, and both returned, sticks in hand. Pointing to a hole in the earth, Lieutenant A. said, “Trenches! There they are!” “What? Who?” said Lieutenant B. “The Boches!” said Lieutenant A. Whereupon Lieutenant B also saw them and cried out bravely, “Go away!” However, the second lieutenant immediately saw that he had been the subject of suggestive hallucination.
Fifteen days of calm followed, during which the lieutenant became more sociable and grew better having no more crises.
Four other cases of “hysteroemotive nature” are reported by Claude, all of them showing a special constitutional basis before the war. In the differential diagnosis, alcoholism, cyclothymia, obsessive psychosis and occasionally systematized delusional psychosis may be considered. There were occasional stereotypical features in the cases, but of a very fugitive nature. Dementia praecox is hardly to be considered.
Re “hysteroemotive” cases, Babinski holds that the claim of emotion as a single factor capable of causing hysteria by itself, is a false claim. To be sure, the patients themselves may give accounts which lead to the idea of an emotional hysteria. Dide, one of the authors of the above case, states that functional disorders occur only in subjects whose emotional tone has been relaxed. The heaviest bombardments are not in line to produce these disorders when the morale of the troops is good. The bloodiest affairs may leave no single case of nervous disorder when the morale is good. Dide found in a whole year’s work but a single functional case,—an oniric delirium, following a trench mortar explosion. Roselle and Oberthür also state on the basis of intensive experience, that large projectiles do not cause any intensive emotional reactions. Clunet’s observations upon the shipwrecked La Provence II, quoted by Babinski, run in the same direction. It will be noted that the five cases called “hysteroemotive” showed a special constitutional basis antebellum.
War strain; slight wound; burials; shell-shock: Neurosis with anxiety; war dreams; apparent recovery. Relapse with depression.
A man, 27 (normal mischievous boy, successful in work, unmarried, shy with women), enlisted October, 1914; adapted himself well to training; at first enjoyed his work, though later bored with routine; and in February, 1915, went to the firing line in France. The first shell-fire experience made him break into a cold sweat with fear and slowed him down for a time. However, he enjoyed the active operations until, after eight months in the trenches, he was invalided home with nephritis. After four months’ convalescence he was recommended for a commission, obtained after two months’ training. After two further months in the regimental dépôt, he went back to France as lieutenant in June, 1916, plunging into four months of heavy fighting on the Somme, in which he was wounded slightly once and was one day buried three times by earth from shell explosion. The last time he was buried he was unconscious for ten minutes and was relieved for three days. He got frequently knocked out for short periods by shell concussion.
At the end of October, 1916, he was sent to the Ypres section, where he worked with a pioneer battalion that buried many dead. After a month of this pioneer work he became mildly depressed; fatigue set in, and now for the first time he began to jump nervously when the shells came over. To counteract this nervousness he began to drink and in a fortnight developed insomnia. The Somme front scenes kept constantly in mind as he tried to sleep. He felt as if he had to go up to the trenches next day and that he did not want to go. There were hypnagogic hallucinations of trenches and shells, recognized as imaginary and productive of no fear. Week by week he became more nervous, became unable to locate shell falls, and felt as if they were all coming at him. Early in 1917 he[458] had taken heavily to drink and grew greatly fatigued in the struggle to prevent betraying his fear to his men. The horror at bloodshed, to which he had long since become accustomed, reappeared. He actually wished that he might be killed.
He carried on until March, when one day on a raid seven men were killed around him and he was immediately thereafter buried. He reported sick and was found to be somewhat febrile. He carried on for two more days; had to report sick again; was sent to hospital and for two or three weeks had bad headaches back of the eyes and a sleep interrupted by sudden wakings with a start. Nightmares now began for the first time. They dealt with the Somme front, merciless shelling coming nearer and nearer. Finally, he would wake with a shriek when a shell landed on top of him. In the day time any noise would be interpreted as a shell. Hypnagogic hallucinations of Germans entering the room appeared. After a little over a week in French hospitals he was transferred to London; grew better; was sent to a hospital in the country where outdoor exercise and recreation helped him.
Two weeks later the death of one of his best friends depressed him a good deal. He failed in an attempt to sing at a concert, and then grew much worse, with the old dreams every night and hypochondriacal complaints of sweats and loss of weight. He was convinced that he was physically and nervously a permanent wreck.
According to MacCurdy, this case is a typical case of war neurosis of the anxiety type, except that a relapse with depression is somewhat atypical.
Re anxiety, Lépine counts trauma as one of the most important factors. The reduction of morale in physically injured cases may at times require their rapid withdrawal to a safety zone. The delirium of the physically injured sometimes takes on a melancholic tinge. Fatigue, loss of sleep, and cold are other factors of a physical nature. Among the moral factors, Lépine thinks responsibility (for certain âmes scrupuleuses) is hardly less important than the factor of felt danger. The contacts of highly cultivated men with the rougher soldier element, may also count, as well as the[459] separation from home and friends, and the factor of despair concerning the ending of the war.
Re sexual influences, the factor of sexual continence, though it may have some importance in producing morbid anxiety, seems to have less importance under war conditions, when self-preservation is more in the eye than the sexual life. On the whole, the pre-existent emotional constitution (Dupré) is of greater importance. A previous wound may cause a man to acquire such a constitution. Amongst physical states, hypotensives are candidates for depression; tuberculosis is particularly important.
Re MacCurdy’s case, the factor of alcoholism was mentioned. The importance of alcoholism, Lépine has particularly stressed. He particularly emphasizes the number of men who have taken to drink to get over their emotions and to forget. Visual hallucinations, angry excitability, sudden persecutory ideas, nocturnal occurrence of the symptoms, flushing of the face, suggest alcoholism. Some of the cases of encephalitis which are supposed to be due to some unknown bacterium, may really be alcoholic in origin. A third of Lépine’s cases were alcoholic; perhaps two-thirds really alcoholic if one took into account the factor of sensitization.
Bombardment from airplanes: Fear; suicidal thoughts; oniric delirium (“moving picture in the head.”)
A soldier (born at seven months, somewhat feebleminded, given to depression, early victim of convulsions, talking only at five years, with a history of once leaving his father’s house with suicidal ideas after being scolded, already invalided in peace times) on enlistment remained with the regiment but a few days and was then sent to a workers’ company of blacksmiths.
Toward the end of February, 1916, his cantonment was bombarded by an airplane escadrille. The patient was much frightened, ran away and hid in a ditch, felt sick, stopped eating, wanted to kill himself and had to be evacuated to Calais and then to Chateaugiron.
He was there found to be well oriented, but depressed and bewildered. There was an emotional tachycardia. At night he would fall into a delirium like the oniric delirium of Régis, always dreaming of the same bombardment scene, saying it was like a moving picture in his head. The delirium affected him so that he actually tried to make away with himself.
The dream delirium did not last long but recurred several times on very slight emotional occasions. It was possible to excite his hallucinatory dreams experimentally by showing him battle pictures.
Some cases of such delirium develop, according to Hoven, after moving picture shows of battle scenes.
Re oniric delirium, Chavigny states that mental confusion and oniric delirium are the two forms of mental disorder that come most frequently after explosions. He believes that at least 95 per cent of these cases are rapidly curable; and, in fact, found amongst 60 cases observed in his army service that only two were so severe as to require being sent to the interior: all the others were cured in six days at the outside. These cases, according to Chavigny, ought to be treated in[461] special wards at the front (bed, quiet, purgation, baths). Chavigny prearranges slight emotional shock for these cases by talking with them about their families. Their apparent apathy vanishes in a trice.
Régis, who has named the state “oniric delirium,” states that the condition never lasts more than a fortnight, is caused by emotional shock, and occurs in all cases with mental disorder following battle; but similar hallucinatory conditions have begun to appear also amongst alcoholics, in garrison or at home. There is emotional constitution in most of these cases. There is not so much evidence of heredity. Out of 50 of Régis’ cases, 22 had been wounded, and 28 not. Régis states that the psychoses are rather more apt to affect men in the reserve, and are severest in officers. These cases should not be committed to institutions, but ought to be treated in special military psychiatric wards containing separate rooms. Very fine-spun diagnosis may be necessary now and again on account of the occurrence of infectious deliria and phenomena of the banal psychoses that may closely resemble oniric deliria.
Shell-shock; emotion (best friend mangled): Stupor with amnesia.
A soldier, 23 (in civil life a turner, of Polish descent, and of a somewhat nervous and easily excitable disposition), early in August went from Strassburg into the Vosges and Lorraine. August 26 a number of shells exploded near him. The troop was excited and took refuge in a cellar. His best friend was torn to pieces by a shell. When the body was removed, the man felt sick and lost consciousness. He arrived at the clinic in Tübingen in a stuporous condition, by hospital train, August 31, 1914. He walked weakly to his bed, supported by two men, and lay in the bed, apathetic and reacting to questions only with a stare. Things put in his mouth were swallowed. He remained motionless.
Next evening he answered a low Yes to a nurse’s question about eating. A little afterwards, he said he supposed he was a prisoner in the enemy’s country. A while later he got properly oriented but still did not know how he had come. September 2, however, he was much clearer and said he had awakened out of a long dream. There was a complete amnesia, however, from the moment when he went to help remove the torn body of his friend up to September 1. Memories became clearer for the period before the shell explosion. The patient became very lively, talking vividly of war experiences, imitating the hiss of shells with an expression of intense anxiety, getting accustomed to the battle scenes, saying that he was now seeing everything again as if real. He remained anxious for some days, complaining of weight on his chest and of feelings of inner restlessness and tension.
Amnesia for the period August 26 to September 1 remained; all that he could say was that he had been thrown sidewise for some distance by the air pressure of the shell.
From September 6 onwards, he grew calmer but he was still very labile, given to lively imaginings and emotion. By mid September he could be discharged for garrison duty.
Emotional shock; shooting a comrade: Horror, sweat, stammer, recurrent nightmare. Improvement on “tracing back.” Brief recrudescence on death of child.
A man after a charge was placed on outpost duty. It was dark, and he was in a state of considerable tension. He heard a noise which he thought came from somewhere in front of him. Suddenly the space around him was illuminated by a flare of light, and he saw a man crawling over the bank. Without challenging, he fired and killed the man. Next morning, he found to his horror that he had killed a wounded Englishman, who had advanced beyond his comrades and was crawling back.
A physical expression of horror, together with an intense sweating and a very marked stammer, persisted for months. At the same time, he was tormented with a fearful nightmare, and in his sleep he was heard to say, “It was an accidental shot, sir; yes, Major, it was not my fault.” In the day time, also, his attention was concentrated on the memory of the incident, so that “I cannot forget it no matter how I skylark.” Carrying his story back to this trying time led to his recounting his terrible secret, and a marked improvement followed. The physical signs of the intense emotion gradually disappeared. The vividness of the dreams diminished, and his attention was less concentrated on the one subject. It is interesting to note that the production of a marked emotional state by the death of one of his children led to a recrudescence of his former symptoms: an expression of “horror and the stammer.” But they disappeared again in a short time.
Emotional shock: Phobias.
An Italian corporal in the infantry, a robust man of a well-to-do family, took a good deal of pleasure in the war life. One day a comrade was injured by a missile of some sort, and died almost immediately. This comrade, after being hurt, had thrown himself against the corporal, who was asleep at the time. He woke up sharply and immediately felt sick. His status was one of great terror, lacrimation, lack of spontaneity, and insomnia. He would wake up from sleep and start from a terrible dream. He had a number of phobias and was especially interested in other persons who had the same sort of mental state as himself. He was in a state noted by Bennati as one of “emotional anaphylaxis” to various events around him. There was a horizontal nystagmus, the Mannkopf sign was positive (87-72), Thomayer 90-114, Erben 114-90. There was a slight tendency to dizziness when the Erben movements were made.
Shell-shock; fright: loss of consciousness next day: Generalized tremors; “somebody above with a mallet.”
A sapper of 19, with a nervous mother, had had an attack two years before his war neurosis, of a somewhat similar nature. This former attack had been caused by overwork; there had been no accident or fright, but the man had been unable to work for five months.
At the front, he had been well up to ten days before observation. In a dugout a shell had pitched on top of the bank, followed by another shell bursting in front. There was a slight falling in of the dugout but no special damage.
The patient carried on that night but reported sick next morning, feeling queer and shaking slightly above the waist. He remembered getting half-way down the road to see the M. O., but nothing more until he came to in the dressing station (perhaps 2½ hours later). After two days in hospital, he was transferred to a convalescent camp, and then admitted to another hospital. He complained of twitching and slight frontal headache; funny feelings at night prevented his going to sleep. Thus: “A man was over my head with a mallet, going to hit me.” There was a dream of “somebody above me all the time.” Both arms, head, and tongue were in a state of constant tremor, and there were jerky movements of the legs. There was some spasm of the right leg. Both legs went into violent tremor on examination, and during examination there was free perspiration.
Re tremors, all sorts of tremors of unknown nature are apt to get the designation hysterical. Meige believes that the Shell-shock tremors, which are apt to be very persistent, are very possibly due to changes in the nervous system. Ballet has noted how the tremors, as in the above case, are often associated with expressions of fear. Now and then there is an obsessive disorder dubbed tremophobia by Meige, which produces a vicious circle. Tremors lead to obsessions,[466] and the obsessions in turn exaggerate the tremors. These Shell-shock tremors are apparently not related to (though they may need differential diagnosis from) such conditions as paralysis agitans, multiple sclerosis, hyperthyroidism, cerebellar disease, neurosyphilis, and alcoholic or other intoxication.
Roussy and Lhermitte distinguish the tremors into (a) atypical ones; that is, disorderly, irregular movements seemingly determined by the subject’s caprice; and (b) typical tremors, such as those found in the well-known nervous diseases and presumably imitated in hysteria from these well-known diseases. Generalized atypical tremors are, as a rule, combined with a variety of other Shell-shock symptoms, and often exhibit a sort of mimicry of fear.
Shell-shock; burial-work: Amnesia. Shell whistling conditions idea of something nasty.
A private, 19, in the R. A. M. C., was sent in with a field ambulance note as follows:
“Private —— was close to a shell which burst among a company standing in the road, killing 20 and wounding 20 others. He worked well in assisting the wounded, and then proceeded to clear up the fragments of the killed. Whilst doing this, he suddenly lost his mental balance and has been in his present state nearly 24 hours. He has been given bromides.”
An M. O. attached to the same ambulance wrote: “This man is suffering from mental shock caused by having to clear away the remains of a number of men killed by a shell. He does not recognize his friends, and at frequent intervals has periods of terror, exclaiming, ‘Cover it up.’ He is sleepless (without drugs); he takes food badly. He is possibly suicidal or may become so.”
According to the patient himself, he had been quite well for four months at the front. He was on the La Bassée Road with the troops after a day or two of heavy work under shell fire. “And I remember the flash of some shot and a shell burst I think, and I can’t remember anything more. I awoke in the morning, in the train” (48 hours later). “I can only remember men calling out.” He complained of a feeling in the head, as if expecting something. “Something seems to be coming,—as if something was going to happen,—something nasty, whenever I hear anything like the whistling of a shell coming towards me.” This patient was without tremor and was physically normal. So far as the patient’s own story went, the case might well be regarded as one due to physical concussion, but the notes of the medical officers give evidence of a psychic element.
Depression with suicidal thoughts after witnessing death of comrade.
A farmer, 52, volunteered and was put in charge of a drinking-water still. He had never been ill nor was there any nervous or mental disease in his family. From the end of August he was frequently under shell fire, but the only effect thereof was a somewhat poorer sleep than normal.
December 14, 1914, a young comrade, a volunteer, wanted to clean his dirty kettle at the drinking-water still. The farmer later described this volunteer as a young fellow “like milk and blood” (as we might say, “like peaches and cream”) and as the handsomest young man he had ever seen in the war. The rules forbade such use of the still, and young “milk-and-blood” was told to go down to the brook, and then come back and get the distilled water. The young man complied, but while at the brook he was shot and killed in full sight of the farmer.
The farmer grew much excited and trembled all over. Thereafter he could not eat or sleep; he reproached himself, although he knew he had acted quite correctly; wished he had been in the place of this comrade; and had suicidal thoughts. He was deeply depressed, wept easily, and showed manual tremor. Steiner terms the farmer’s account of the person of the deceased “reactive idealization.” After a week there was considerable improvement. B. was sent back to work, which he felt would be beneficial. He was put in less dangerous surroundings, and this also had a good effect.
Marching and battles: Neurasthenia?
A subaltern had been treated before the war for nervousness, dizziness, and “mattigkeit” (convulsions in infancy), but proved himself a good soldier, having gotten his rank after the first period of practice.
He was in three battles in Belgium, but on the march one day suddenly had a spell of weakness and is said to have had convulsions. There was, however, no biting of the tongue, and no enuresis. After a week in the field hospital, he was sent back to Berlin where he had some somatic feelings of anxiety without subjective disturbance or any disorders of consciousness except a certain amount of inhibition; he was sleepless and hypersensitive, cried easily, and was apprehensive on being touched; he winked violently on examination of his eyes, and while being tested for reflexes made violent contractions of a semi-voluntary nature.
After four days in bed, which was a prescription hard to carry out at first on account of the anxiety sensations, these sensations disappeared, and at the same time the fears. Weight began to increase; memories returned, except that even upon recovery he could not remember that he had ever had any true subjective feelings of fear. He was discharged 19 days later, desirous of going back into the field.
The peculiar absence of subjective feelings of fear in this case is something like what Awtokratow reported from the Russo-Japanese War, terming them neurasthenic psychoses.
Re neurasthenia, Babinski believes that, by means of his logical dismembering of the old hysteria concept, he has shown that the exhaustion phenomena at the bottom of neurasthenia are precisely these that cannot be cured by suggestion. There are numerous cases in which hysteria and neurasthenia are combined. From these combined cases, suggestion causes the hysterical or pithiatic symptoms to be removed.
English schoolmaster’s account of his war dreams.
A sergeant, who had been a schoolmaster, was asked to write down his dreams by Captain W. Brown, who had sometimes charge of Mott’s cases at the Maudsley Hospital. The first dream was as follows:
“I appeared to be resting on the roadside when a woman (unknown) called me to see her husband’s (a comrade) body which was about to be buried. I went to a field in which was a pit, and near the edge four or five dead bodies. In a hand-cart nearby was a legless body, the head of which was hidden from sight by a slab of stone. [He had seen a legless body, which was covered with a mackintosh sheet, which he removed.] On moving the stone I found the body alive, and the head spoke to me, imploring me to see that it was not buried. Burial party arrived, and I was myself about to be buried with legless body when I awoke.”
The second dream was as follows:
“After spending an evening with a brother (dead 11 years ago) I was making my way home when a violent storm compelled me to take shelter in a kind of culvert, which later turned into a quarry, situated between two houses. Men were doing blasting operations in the quarry, and whilst watching them I saw great upheavals of rock, and eventually the building all around collapsed (explosion of a mine). Amongst the débris were several mutilated bodies, the most prominent of which was legless. I tried to proceed to the body, but found that I was myself pinned down by masonry which had fallen on top of me. As I struggled to get free the whole scene appeared to change to a huge fire, everything being enveloped in flames, and through the flames I could still see the legless body which now bore the head of my wife, who was calling for me. I was struggling to get free when my mother seemed to be coming to my assistance, and I awoke to find the nurses and orderlies standing over me.”
It appears that the patient had been shouting in his sleep, beginning in a low voice and gradually becoming louder until at last he was shrieking. The legless body occurred in all[471] his dreams; the sight of this had evidently produced a profound emotional shock. He had worried a great deal about his wife, who was much younger than himself, so that we have this incongruous association of the legless body and the head of his wife calling him; finally, what more natural than the mother to come to his help. The emotional complex is not incongruous in this dream, for fear is linked up with the tender emotion.
Re war dreams, see remarks under Case 333 concerning oniric delirium. Roussy and Lhermitte say that emotion and concussion are the causal factors; but in a case like 341 we have persistent war dreams of the same general nature. Such a case as Mott’s would not be regarded as one of oniric delirium, for the patient is not living throughout the day in a dream, but merely has certain set dreams. The true oniric delirium cases may lead to fugues of medicolegal importance. Mott’s conception is that the terrifying experiences that come to light in the dreams are repressed by the conscious activity of the mind in the waking state. For this process, the phrase psychic trauma might be used. Rows speaks of a prolongation of mental disorder through memories which get revived in dreams. The memories of past and recent events pile up on one another. Elliot Smith remarks on the number of cases in which the dreams show a coalescence and blending of episodes alien to the war. Re such combinations, see Case 342 of Rows, below.
Trench experience: War dreams, shifting to sex dreams. Recovery on giving the patient an insight into the nature of his dreams.
A patient broke out of a hospital after being refused permission to leave the grounds. He grew much depressed and said he had been disgraced and would commit suicide rather than bring disgrace on his family. Investigation into this emotional outburst showed that his father had deserted the family, that he had gotten into prison, and “tainted me.” The patient was worried also about an idea of loss of sex power, gathered from a book by a quack doctor, read years ago. It appeared also that this doctor had advertised a special bread and special medicine which would preserve the nervous system, and that for years the patient had fed himself and his family with the bread and medicine. When the true state of affairs was shown to the patient, his restlessness at night disappeared. The mental condition of this man in fact became practically normal, and the marked tic of facial muscles and the general tremulousness of the man disappeared.
It is of note that this man’s dreams began with a terrible incident in the trenches and then shifted to sex acts. He woke to find the clothes disturbed.
This is an example of hallucinations dispelled by tracing them to their source, and giving the patient a clear insight into their nature.
According to Ballet and de Fursac, after the acute phase of stupor and excitement with hallucinations and delirium passes, the patient remains a depressed and psychasthenic subject. In this psychasthenia we find inhibitory phenomena, hyperemotionalism, and over-imagination. Amongst the inhibitory phenomena are many of the hysterical effects. The hyperemotionalism yields anxiety, worry, tremors, respiratory and vasomotor disorder, dizziness, convulsions. The third main disorder of the psychasthenic state into[473] which the patient relapses is over-imagination, whereunder we find bad dreams (bombardments, drum-beating, corpses, attacks), somnambulistic hallucinatory episodes. It is these hyperemotional and hyperfantastic features that distinguish the Shell-shock syndrome from ordinary psychasthenic states.
Re the sex element in this case, see remarks under preceding case (341) and also Lépine on the sex factor (Case 332). Rows believes that those cases which do not recover after a short period of rest and quiet in hospital are cases in which there is some emotional state based upon the constant intrusion of the memory of some past event. The physical expression of the emotion of fear or terror may persist for a long time quite unchanged and be proved to be due to this old factor.
Emotional shock: Recurrent dreams of war and peace incidents. Recovery followed tracing the dreams to their origin.
A soldier and a comrade were carrying a pail of water to the trenches. It was very cold and they set down the pail in order to warm their hands. The comrade placed his hand against the man’s cheek and said, “That hand is cold.” At that moment he was shot dead.
This incident was involved not only in dreams at night, but in the daytime too, if he were quiet and closed his eyes, he could feel the cold hand against his face.
He was troubled at the same time by another dream, in which he ran down a narrow lane at the bottom of which there was a well. He dipped his hands into the water, but on withdrawing them, he was horrified to find they were covered with blood. This dream was connected with a love affair, in which a good friend interfered and angered him so much that he attacked him when next they met. He left him on the ground so injured that it was necessary to take him to a hospital. The patient became anxious as to what the result might be and left the district. He traveled, but never heard whether his victim had died.
When these two dreams were traced back to their origin they disappeared: the patient made a rapid recovery and was able afterwards to bear a severe trial satisfactorily.
See remarks under Case 342.
War dreams, including hunger and thirst.
(Recorded Dream of a Second Lieutenant.)
“During the five days spent in the village of Roeux I was continually under our own shell fire and also continually liable to be discovered by the enemy, who was also occupying the village. Each night I attempted to get through his lines without being observed, but failed. On the fourth day my sergeant was killed at my side by a shell. On the fifth day I was rescued by our troops while I was unconscious. During this time I had had nothing to drink or eat, with the exception of about a pint of water.
“At the present time I am subject to dreams in which I hear these shells bursting and whistling through the air. I also continually see my sergeant, both alive and dead, and also my attempts to return are vividly pictured. I sometimes have in my dreams that feeling of intense hunger and thirst which I had in the village. When I awaken I feel as though all strength had left me and am in a cold sweat.
“For a time after awaking I fail to realize where I am and the surroundings take on the form of the ruins in which I remained hidden for so long.
“Sometimes I do not think that I thoroughly awaken, as I seem to doze off, and there are the conflicting ideas that I am in the hospital, and again that I am in France.
“During the day, if I sit doing nothing in particular and I find myself dozing, my mind seems to immediately begin to fly back to France.
“A dream that keeps on coming up in my mind is one that brings back a motor accident I had about six years ago, which gave me a severe nervous shock. I had, of course, entirely forgotten about it, except when in a motor, when I always thought of it.
“Of the fifth day I have absolutely no recollections.”
This is the one instance in which a man has dreamt the experience of hunger and thirst in addition to battle experience.
Olfactory dreams: Hysterical vomiting.
A lieutenant in the infantry (mother, of a nervous disposition) had been at the front for 3½ months when he started vomiting everything he ate.
He was transferred a fortnight later to a base hospital as “gastritis.” Physical examination proved negative, but the man complained of his nerves. He slept badly owing to trench-life dreams, from which he would wake in a sweat. He was quite unwilling to refer to these dreams.
In point of fact he had had to supervise the burial of many decomposing bodies, after which he had been haunted “by that awful smell of the dead.” Then developed states of abstraction, in which he went over and over the burying experience. He cried by himself.
It seems that the vomiting was secondary to hysterical hallucinations.
Re affections of smell and taste, Roussy and Lhermitte remark that they are rare following shock or trauma in war. Medical suggestion may produce a hemiageusia or a hemianosmia. Mott’s case above (344) showed unusual dreams with hunger and thirst. For another olfactory case, see Case 510 (Rivers) in the Treatment Section of the book, a case in which Rivers was able to find no redeeming feature upon which to ground his re-educative suggestions.
Re vomiting, Roussy and Lhermitte state that this relatively common condition is diagnosticated readily enough but that pyloric ulcer and other organic causes must be eliminated. They remark that there is no tendency to spontaneous cure of neuropathic vomiting, and commend strict dietetic régime and psychotherapy. They ally the condition in its nature and genesis with so-called false or hysterical incontinence of urine in soldiers. Wiltshire’s case early received the diagnosis “gastritis.” It is remarkable how little emaciation need follow such vomiting.
Shell-shock: Amnesia; dreams of falling. POST-ONIRIC suggestion—surprise produced fear of falling.
A man was subjected to shell-shock August 11, 1916, at the Somme. He lost consciousness for five hours and was picked up stuporous with verbal amnesia, which soon passed leaving only a difficulty in getting the right word promptly. He began to have frightful dreams of falling into a hole and of exertions to avoid falling, whereupon he would awake with a feeling of anxiety that would last some time. Treatment caused the dreams to disappear.
There remained, however, a powerful post-oniric suggestion. Any slight surprise would cause the fear of falling to reappear. There was a sort of derived phobia, against any military act that would need to be performed upon sudden order. He developed a blind anger against any commanding officer who gave a brusque order. After the crisis of anger he would fall into tears and a feeling of profound depression coupled with precordial anxiety. There was also a chronic aortitis physically determined. The man himself had a vague idea of the relationship of his fear of surprise to the old nightmares.
Re persistence of fear and its relationship to nightmares, see remarks under Case 342 (Rows).
Four months’ SERVICE IN THE REAR: Depression; war HALLUCINATIONS (not based upon actual experiences); psychasthenic symptoms.
A Russian lieutenant, 32, arrived at the front in November, 1914, but never served on the front line, or had occasion to visit the line or the trenches. Toward the close of February, mental symptoms appeared, which caused the man’s evacuation to the interior.
He was a tall, well-built, well-nourished man, who was physically normal except for sharp twitching movements of the tongue, eyelids, and face; tremors of extended hands, occasionally spreading to the whole body; well-defined dermatographia (in places, stereodermatographia); exaggerated tendon reflexes; tenderness of skull and spine; hyperesthesia of chest; pulse 120.
Mentally, the patient was markedly depressed, irritable, at times lacrimose. His complaints were of a psychasthenic tinge. He feared incurable disease. He feared to go to the front, and was terrified at what he might do there. He feared crowds of soldiers; he was afraid of forests and mountains; the Germans were going to break through and capture him; shells were about to burst over his head. He was also disturbed about his family, regarding his wife and son as helpless, sometimes even as dead. Suicidal thoughts at times.
At night, though he had never been at the front, he had hallucinations of shots and the voices of soldiers, as well as those of his wife and son. He smelt an unpleasant corpse-like odor. He was unable to distinguish these hallucinations in any respect from reality. He complained of general weakness, headaches, palpitation of the heart, vertigo, and insomnia, and of a variety of pains.
He was non-alcoholic and non-syphilitic, and had been in perfect health before the war.
Re war hallucinations with service back of the line, compare remarks of Régis (see under Case 333).
A case of hysterical astasia-abasia develops “big belly” (“catiemophrenosis”), perhaps by hetero-suggestion from a ward neighbor.
A farmer, 22, of the foot chasseurs, who had been in various hospitals with a variety of diseases before his injury, was evacuated June 2, 1916, for “contusion of back,” to the temporary hospital at Bussant, from which he was evacuated to Pontarlier for “contusion of back and cerebellar shock” and thence, July 21, to Besançon for “internal contusion and cerebellar shock”; thence to four other hospitals from July 31 to February 17, 1917; finally to the Hospital at Veilpicard with “functional disorders, paraplegia, trepidant astasia-abasia.”
It seems that he had lost consciousness for fifteen days and had thereafter been paraplegic with retention of urine. The abdomen had then increased in size in such wise as to be termed a nervous pregnancy, grossesse nerveuse. The evolution of this pseudotympanites was probably related to the presence of the same so-called “big belly” of a patient who had been in a neighboring bed from May, 1916, onwards. The feet were in equine position with toes flexed, suggestive in all ways of hysterical paraplegia. The abdomen looked like that of a woman six months pregnant and measured 78 centimeters in a plane passing through the anterosuperior iliac spines and the umbilicus. The abdomen was hard, tense, swollen, and on palpation, gave out a low, tympanic note. When the diaphragm was mobilized progressively and slowly, the tympanites could be made to disappear. Slow pressure on the abdomen with flat hands effaced the swelling for the time being; but upon release of the hands the abdomen would swell up again as before. Pressure on the abdomen produced a contracture of the recti. Forced flexion of thighs on pelvis (as suggested by Denéchau and Matrais) also caused the swelling to go down. Faradization of the phrenic nerves in the neck caused respiratory movements with a slight diminution in the volume of the abdomen. There was an obstinate[480] constipation requiring daily lavage. Respiratory movements were short and rapid and of the thoracic type. Abdominal compression caused the respiration to assume almost a normal rhythm. X-ray examination of the abdomen, after 50 grams of bismuth carbonate had been taken in three spaced doses the evening before, showed the intestine to be distended by gas in such wise that the lower border of the liver became clearly visible, as after insufflation of the stomach. The bismuth was found in the large intestine. The splenic angle filled with bismuth was low. On compression the splenic angle was raised with the diaphragm.
The main features of this disease are the large abdomen, simulating what has hitherto been found chiefly in females under the name of nervous pregnancy, but also suggesting a tuberculous peritonitis (one patient was actually evacuated to a hospital for tuberculosis with this disease); gastro-intestinal disorder with aerophagy, aerocoly, and obstinate constipation (one case also showed almost daily vomiting). The genesis of the condition appears to be a contracture of the diaphragm in a low position of forced inspiration. The condition may be termed a diaphragmatic neurosis.
Psychotherapy was applied, the patient was requested to walk, and the movements made in walking required such an intense respiration that the diaphragm was forced to function, whereupon the “big belly” disappeared. The digestive disorders then rapidly disappeared. These authors suggest the name of catiemophrenosis.
War stress; collapse going over the top: Neurasthenia (hereditary taint; alcoholism).
A German soldier, 35, of a nervous make-up (his mother was nervous, and he had been nervous and tremulous and easily excitable, and alcoholic to the extent of at least 5 glasses of beer every night), was called to the colors in September, 1914. He got through his training well; in May, 1915, was on very strenuous duty in a very exposed position, had frequently to stand up under heavy shelling, had a number of frightful experiences, was surrounded by corpses and mutilated bodies, and frequently took part in storming attacks. His nervousness came to a head with some suddenness; just as he was about to “go over the top,” he had no strength for the effort and collapsed. Thereafter he could no longer stand shelling, could not speak, and was inattentive to surroundings. When he was examined by a physician he fell asleep in his presence, although sleep had latterly been almost impossible on account of the shelling. He was immediately put on the hospital train and taken to the reserve hospital in Nuremberg, where he presented an appearance of extreme exhaustion, wept, seemed much fatigued, and trembled all over whenever he started to do anything. He was very easily excited and especially sensitive to noise. There was a fine tremor of the whole body and especially of the head; the knee-jerks were increased; there was a moderate vasomotor reddening of the skin after stroking; his tongue was heavily coated; but there was no other evidence of internal disorder. His pulse was strong and not rapid.
The patient got well gradually, complained at first of bad dreams, and was given to weeping. The tremors slowly improved. The patient grew better in a hospital at home.
As to the diagnosis of this case, Jolly regards it as one of nervous exhaustion. The remarkable feature is the tardiness with which the symptoms developed under the stress of war. Such a patient would probably never develop a neurasthenia[482] under normal peace conditions. After recovery these patients may be sent back for garrison duty or for other work not directly connected with the firing line. As for the tendency to desire a pension, this wish, according to Jolly, must be strenuously opposed, both in the interest of the state and that of the patient. If there is no will to get well, some of these patients are found vibrating from garrison service to furlough and to hospital.
The above case is one of the simplest observed; yet there is evidence both of hereditary taint and of alcoholism. According to Jolly, the majority of the severe exhaustion states of a neurasthenic nature have been, in his experience, distinctly nervous before the war, and frequently show hereditary taint as well.
Re neurasthenia, see views of Babinski relative to differentiation from hysteria (under Case 340).
Series of battles: Sudden mania followed by confusion with fixation of mind upon war experiences, possibly hallucinatory; general analgesia.
A Russian private, looking much older than his years (35), had been in a number of battles without mental disorder. Where he was posted, however, there was a heavy artillery fire in the last of the battles. Suddenly the man became excited and leaped upon his comrades’ shoulders crying, “The devil is here! This is hell and murder, and here are the devil’s imps!” The commanding officer accordingly ordered him to the rear. His regiment had suffered severe losses in a succession of attacks upon a certain strategic height.
Upon evacuation to the field hospital and thence to the interior, his excitement did not lessen. He went about with a lost look, trembling, talking a great deal and gesticulating. His talk was incoherent and pointless. After every few phrases, he would repeat, “Don’t ride there! That’s hell! Murder is being done. Devils and unholy powers are beating and killing people.” As he said this, he would tremble, and hands and feet would stiffen with a suggestion of catalepsy. There was general anesthesia to pain; no response was made to deep pin-pricks. The pupils were dilated and failed to react, either to light or to pain. The tendon reflexes were exaggerated. No contraction of visual fields. The man was disoriented for time and place and much confused. No paralysis. No wound or contusion.
Re analgesia, we may only say that hysterical anesthesia appears in a variety of forms; sometimes (a) in the form of a classical stigma of hemi-anesthesia; (b) in a segmentary form; again (c) in isolated patches; (d) in a very rough way approximating the peripheral nerve distributions. Babinski gives an unpublished note by Lasègue, in which he states that hysterical patients not enlightened by the doctor’s investigations do not make mention of anesthesia. But in case 350 a psychotic factor may have entered.
Ten months of military service (several battles) without reaction; then, hot machine gun battle: Mania with disorientation and war hallucinations.
A Russian private, 24, in a scout company, entered the war on mobilization and took part in several battles without reaction. May 11, 1915, he was sent with the scout party into a hot encounter, hand to hand with machine-guns. After the battle, the man began to yell incoherent phrases at the men around him, started to climb over the top, and shot off his gun without permission. He was accordingly sent to hospital, where he was under observation for a week, during which he had occasional flashes of excitement, jumping out of bed and making movements of cutting or shooting, and then in a few minutes subsiding into inactivity.
He was a short but well-built and well-nourished man; the pupils responded rather weakly in accommodation; there was a small fibrillar tremor of the face, eyes, and tongue. The skin reflexes were diminished and there was a general hypalgesia; considerable mechanical overexcitability of muscles; no other neurological disorders. The mental state was one of confusion. Although he was in one of the corps hospitals, he said he was in a dug-out; the doctors were lieutenants; the attendants were privates in his company. Answers to questions were irrelevant or incoherent; there were a number of delusional expressions. He was to be shot because he had not himself shot enough Germans. If he were not to be shot, anyhow the soldiers would poison him. Rather than this he should be allowed to go into an attack. He would take a German fort and the Czar would name him a colonel. His regimental commander was saying to him, “You will be a hero, you will soon get a company.” His hallucinations sometimes included the voices of Germans saying, in broken Russian, “We will hang you and cut your belly open!” There was considerable amnesia for dates and even his last battle.
Numerous attacks and counter attacks in one day: Sudden incoherence with disorientation and the rapid development of war hallucinations of a scenic type. Suggestion of catatonic phenomena.
A Russian lieutenant, 28 (no mental disease, non-alcoholic), was in battle August 14, 1914, on which day his company attacked and was itself attacked several times. An officer who observed the lieutenant said that he came to him and informed him that the Germans must first be burned and then fought with. Thereafter the lieutenant began to speak loudly and incoherently, sometimes yelling incoherent orders. He was accordingly removed from the battle-field to the hospital back of the line. Upon examination, he was found to be of middle height, with dilated pupils, responding weakly to light and not at all to accommodation; twitchings of face, eyelids, and tongue, digital tremor, marked dermatographia, general analgesia, tendon reflexes somewhat exaggerated, cataleptic tendency in feet and hands.
Mentally, the patient was in a stupor, sitting or standing in one place, without initiative; uncomplaining but occasionally uttering deep sighs or occasional isolated phrases. He answered no questions or only after a long pause. He was disoriented for time and place, but gave evidence of delusions and hallucinations. He thought, for example, that he was the chief of staff and had brought with him a squad of captured Germans who were standing nearby. Some wanted to be fed and let go; others were yelling and saying they would burn down the house. Sometimes the patient would hear shots and shells bursting, at which he would shudder and turn away. Apparently he would see his comrades falling under the shrapnel hail. However, he stood his ground and commanded the rest of the soldiers to go forward to the attack. Now and then he was negativistic, flexing the hands upon request to extend them, refusing food and drink. He was still apathetic on evacuation to the interior.
Shell-shock after two days in trenches: Hysterical STUPOR seven days. Cure in three weeks, barring amnesia for stuporous period.
F. S., in civil life a wreath-binder in a flower shop, and from childhood very nervous and excited, subject to frequent nosebleeds and fainting spells (e.g., at sight of blood), enlisted at 22, November 3, 1914, as a reservist. January 18 he went into the field.
The wreath-binder was only two days in the trenches before going unconscious under the whistling and exploding shells. Physically uninjured, he was received in reserve hospital C in a deep stupor, January 22. He was unresponsive at first, once however saying, lost in a dream, “When will mother come?” His gait was unsteady and he had to be led and held. He slept a good deal in the daytime.
He became somewhat more active mentally, January 24 (remarking that he had slept well), and made his toilet, but he did not yet have bearings and wanted to go to his place of business. The next day his condition was similar. Asked what troop he was with, he said, “In the flower business.” January 26 he was much better, telling of the army training and a little about the war, and wrote a postcard to his parents. The stupor disappeared after January 27 and the patient became mentally normal. Amnesia persisted for the time, January 20 to 26. Headaches. February 9 he was well, except for the limited amnesia still persisting. He was eventually sent back to garrison duty, cured.
Re stupor, Grandclaude remarks that stupor is probably the most frequent of the mental symptoms of Shell-shock, and that it may last from a few moments to a week. During the stupor the patient is asthenic, stertorous, and staring. Upon recovery from the stupor, a condition of dulness with amnesia and disorientation ensues. There may be a third phase of a more hyperkinetic character, with hallucinations and delusions concerning the war. These stuporous cases[487] are among the most serious of the conditions found, as some of the victims may even suggest dementia praecox from the persistence of childishness and silliness. As in Gaupp’s case, Grandclaude finds that headaches and amnesia persist. Relapses are frequent on the basis of a kind of sensitization.
Re amnesia and Shell-shock, Roussy and Lhermitte speak of amnesia as ordinarily a phenomenon of confusion. Amongst the mental disorders of the Shell-shock psychoses, these authors describe a group due to inhibition or diminution of mental activity, including the rare narcolepsy, or pathological sleep, and the confusional states proper. Simple confusion involves slowness in thinking, and amnesia often anterograde from the moment of the shock. Simple confusion ought to be distinguished from so-called “obtusion” or torpor, in which there is a disorientation for time and space, such as was shown in Mallet’s case. Chavigny has described an aprosexic form (with “birdlike” movements). More common is the amnestic form of torpor. The amnesia may not merely be anterograde from the moment of shock, but may extend to a prolonged period prior to the accident. Sometimes the amnesias are selective, producing phenomena of pseudo aphasia.
Amnesia, monosymptomatic. Progressive recovery.
An infantryman, 36, arrived without information at a psychiatric center, March 15, 1916, looking confused and knowing little more than his name, believing himself in a distant town. The disorientation lasted to March 21, on which day the man recognized the doctor as such, knew that he was at a hospital, but felt that he had just left home and wife. From this time on, he began to pick up his surroundings, evidently not knowing that there was a war or that he was a soldier. He did not recognize one of his own company. It was not until March 31 that the first memory of the war reappeared, namely, a memory of the call to the colors, drums, bells, and crowds. April 11 he recollected that he was a soldier and that his wife was in the country, where he had left her on the eleventh day of the mobilization. In the next few days, memories came back bit by bit. He had been at first a little thin and showed a slight fever, oliguria, and poor digestion. All these symptoms now lapsed, and the man became apparently perfectly well.
Such states, according to Mallet, are relatively frequent in soldiers, both in epilepsy, and in infectious deliria,—more than in the deliria of exhaustion.
Aviator shot down: Organic mental symptoms.
A Canadian, 20, of normal makeup, in 1915 lost part of his left foot in a railway accident, but, notwithstanding, was finally commissioned in the Royal Flying Corps. He enjoyed the nine months of English training greatly. In France he made several successful flights over the lines, but was shot down and crashed to the ground within the British lines after two weeks of service. He got black eyes and bruises and lost consciousness for about four days, though a week later he was still hazy about recent events and was not quite sure in what hospital he lay. After another week he arrived in a London hospital.
Here he would not answer questions, but stared at the examiner, finally shouting: “I want to get up.” He said he was in a certain suburb of Toronto, which, however, he insisted was a part of London not far away. He wanted a taxicab to go thither. He pondered, but seemed content when told that Rosedale was across the ocean. A superficial machine gun wound of the hip the patient said must be the mark of a hospital in France; it was a secret mark, meaning that he could return to the line and fight whenever he wanted to and that he could use the lavatory whenever he wanted to. He sometimes uttered brief phrases after questioning. Asked if he dreamed, he looked up cunningly and said, e.g., “I down the Boche. I am a live wire.”
Next day it was clear that he had gained a good deal of information from the nurses, and the day after he had become oriented for time and able to recognize the physician, though still confused about hospital names and his recent movements. The 7 from 100 test he did slowly and made several bad unrecognized mistakes. He was over-fatigueable, complained of foggy eyesight, showed haziness and redness and obscure margins in the optic discs, with the remains of one hemorrhage, and presented nystagmus on looking to the extreme left. Two weeks later he complained less of his memory and said that he was beginning to remember what[490] had happened during the last day of his fighting; the chase by the German airplane and the maneuvers. He worried about being sent back to France by a medical board, which would not realize that he was incompetent to fly again. The left pupil was slightly larger than the right.
In this case there were no neurotic symptoms and according to MacCurdy the difficulties here are strictly those of organic type.
Re organic cases of traumatic psychosis, Lépine sums up the subjective phenomena as follows: There is (a) a cephalea, often a feeling of weight, varying at different times of the day; often frontal; often subject to marked alteration on movement. There may be (b) a number of visual phenomena like those mentioned under Case 355, part and parcel of a sort of absence, suggesting an epileptoid effect. Sometimes (c) there is vertigo, but this is rare. There are also congestive attacks. The patients are unable to work, and have strange head sensations when they attempt to work. The memory disorder is not as a rule markedly accentuated. This amnesia is usually a disordered fixation of current events, but there is also a retrograde amnesia. Insomnia and impulsiveness are also found, and more rarely is a depressed and melancholy state suggesting that which Case 355 exhibited. Lépine has tried to define the traumatic psychoses (not neuroses) on the basis of phenomena found in trephined cases. He remarks upon the extreme analogy, not to say identity, between the late sequelae of trephining and the syndrome of commotio cerebri.
Daze with relapses; mutism—following shell fire and corpse work.
A soldier lost his voice apparently from two factors: shell fire and the emotional shock of helping to fill the big common graves. The man could never tell for certain (retrograde amnesia) whether he went from corpses to shell fire or from shell fire to corpses.
Several weeks of daze followed in which he hardly reacted to outward stimuli, but occasionally said “It smells!” “Leave me still!”
He recovered gradually from the daze. But merely hinting at his experiences, especially the smells, sufficed to throw him into another daze.
The loss of voice lasted for some time after he had wholly stopped lapsing into the dazed states.
There was some alcohol in the previous history of this case, which is the only case among twenty-three Shell-shock cases reported by Mann which had a psychiatric disorder of any lasting nature due to shell fire.
Re mutism and the two factors of shell fire and emotion spoken of by Mann, compare the views of Babinski to the effect that emotion alone is unable to cause such a hysterical manifestation as mutism.
Re the corpse work, see remarks under Case 342.
Mine explosion: Mental confusion. Amnesia effected through Y. M. C. A.
A sapper, 21, was admitted to a base hospital semi-stuporous, unable to answer questions and mistaking the identity of persons about him. At first he slept, but next day found he was in hospital. His mind was “all of a blur.” He did not remember coming to France; “It all seems a mist.” He felt he was ill and was afraid of becoming insane. There was no physical sign of disease except coarse tremor of hands.
At intervals over a period of about half an hour, helped by questions, he was able to get out the following with much emotion:
“Joe, don’t go—Give me my rifle, Joe—Ten killed. Poor old Taffy—Dreamed last night—Saw Harry Edmands with all his ribs broken—when we had the explosion—5000 bombs or two and a half tons of explosives blew up.—Joe—Clay said he would never live three weeks,—Glasses blown in.—Taffy killed by shell in stomach—S— L— All privates blown off him—Just after leaving workshop.”
Between the above statements, the patient might go off into short trance states, staring and pointing out of the tent.
Next day he was found in a condition of cheerful emotion, saying that he was ever so much better; an orderly had “saved him!” This orderly had taken him to the Y. M. C. A. recreation tent, played the piano to him, and made him play himself. His whole emotional state suddenly changed over. He now had a good memory for everything previous to his reaching France, and remembered simply that there had been an explosion. He remembered two names that he had mentioned, but he could remember nothing about their fate in France. He did not know where they were but he was not anxious about them.
Shell-shock: Hallucinations; alternations of personality.
A soldier, 29, a helper in a wholesale house, came to a hospital by hospital train, uninjured, directly from the field, having become completely deranged under shell fire. He arrived at the clinic January 11, 1915, in deep emotion, anxiously excited, and looking tensely and suspiciously at the bystanders. He seemed to hear very badly and shouted his statements like a deaf person. Led to the sick section, he shouted out of the window, “Frenchmen!”; then he went willingly to the bath and was put to bed, unresisting. He lay in bed on his elbow, listening in the direction of the window or the wall, answering loud questions with a quick, yelling voice after a pause. He gave his name correctly. He seemed to think he was in the trenches and to see hallucinatory pictures of battle.
In the examining room he immediately sat down, back to the wall, taking the chair at the desk and leaning it against the wall. Asked why he did so, he said with a horrified expression, “The shells, they are coming over! Whew! they are shooting all the time.” He ducked, imitating the hissing and whistling of the shells. Asked if he had been struck, he said, “There are two dead and one’s head is off.” He declined to be told where he was, and when he was told that he was no longer in the enemy’s country, but in Württemberg, he said, “No, no; they don’t come so far. No, the Frenchmen don’t come so far.” He was very easily frightened and started at every touch as if wakened from a dream. Sometimes his whole body would tremble with anxiety. He would not allow his pulse to be taken, at first. He would suddenly shout, “That’s the Krupp now flying by. Now it has struck.” He cast his eyes along the ceiling as if to follow the course of the shell. Asked what he was doing, he said he was in the trench on the mountain.
He was able to tell about his family, his marriage in Berlin,[494] and his child, and he could tell time by the clock. Then he would suddenly shout: “The shells, they are shooting everything; they are shooting like another earthquake.” Gaupp stepped up to him, in uniform, and asked if the patient knew him. He examined Gaupp suspiciously from top to toe, looked at the shoulder-straps, and then quickly cried loudly, “Physician.”
At another time he described the shell havoc with evidence of extreme anxiety. He would take food only when one broke off a piece and ate of it before him. He would not drink out of ordinary drinking-glasses but only out of his field cup, examining it carefully. He denied he was on patrol duty at Soupis. His comrade was merely asleep just now. A civilian physician in his long coat was termed by the patient “a baker” after careful examination. There seemed to be no pause in the man’s behavior, which looked absolutely genuine and dominated by strong emotion. He had the look of a man in immediate danger of death, exerting himself to escape shell fire.
This dream-like disorder of consciousness with war delirium persisted for a number of days. There was no marked motor excitement. He would remain for the most part quietly in bed, absorbed in his thoughts, watching and listening, sometimes looking about in astonishment but not getting his bearings. Gradually his emotions declined and he developed a certain confidence in the nurse. She was able to convince him that he might be in a hospital, although he objected that there were no wounded there. (He was in a mental section where there were no bandaged men.) All the while he was very hard of hearing and shouted loudly in speech. For twelve days he could not be convinced that he was in Germany. The fact that the Sister was speaking German was met promptly by the fact that in France the physicians and Sisters spoke German too.
An extraordinary change came over him January 27 (sixteen days after admission). He went into the garden, apparently deaf and shouting his answers, accompanied by Sister Margarethe, whom he always called “Sister Anna” and whom he thought came from Lichterfelde. While walking[495] with the Sister, his condition suddenly disappeared. He began to hear; he spoke in a normal tone, in fact, rather low, and began to address the Sister by her right name, Margarethe. He was astonished at the snow in the garden, and asked the Sister whether she noticed that the artillery had just stopped firing. Gradually getting his bearings, he wondered whether he had been in the hospital since the day before. He certainly was not ill, he thought.
This normal state lasted for a half hour. The patient then relapsed into anxious semi-consciousness, becoming deaf again and shouting his words. During the next few days and weeks he had frequent changes of state like the above described. The changes to a normal state would take place spontaneously in the absence of apparent occasion, but the relapses into semi-consciousness took place when there was some outer irritation, especially some noise. Every fright would cause a relapse. Once a small cannon fired at a great distance off caused such a relapse; again, a sudden shouting at the patient.
During the clear state there was a complete amnesia for the period of illness. He did not want to believe that he had been in the hospital for weeks, declaring that he must have been in the trenches two days before.
Gradually the semi-conscious states decreased in length; the deafness and loud speech returned with the semi-consciousness. With the return of orientation, the man looked entirely normal, speaking in a low voice somewhat shyly. He was rather suspicious and could find his way about with difficulty. His memory broke off with the last days of December, 1914, at which time he was in the trenches under intense shell fire. His wife had received no word from him since December 26. Even at the beginning of February he grew anxiously tense when the word shell was mentioned.
February 4, Gaupp presented him in clinic as entirely clear. He mentioned that his relapses to semi-consciousness occurred on the occasion of a loud noise or word spoken. His face was contorted at Gaupp’s remark but there was no other change in him. The next day, however, he told the Sister that Gaupp had shouted out once to[496] “get him away.” He said he had then heard artillery fire for a moment, but pulled himself together though he had almost gone off, and had a violent headache afterward.
These states of alternating normality and semi-consciousness continued until about February 10. During a clear spell, the patient was quiet, reserved, taciturn, a little ill-tempered and seclusive, occasionally writing his wife a rather empty letter. In the semi-conscious state he was emotional and restless, seeking cover from the enemy. These states stopped altogether about the middle of February. He then became somewhat more open, though he had no idea of the gravity of his condition. He was angered by the window-bars, and offended by the opening of a letter to his wife, declaring that he would never write a word again, as it was just like a prison. These outbursts passed quickly by. He wanted to go home and believed he would soon be able to go to his comrades in the field.
At the time of the report, Gaupp felt that he could not be discharged for a number of weeks. He was pallid, gave the impression of being exhausted mentally, complained of restlessness and internal irritation. His memory gap covered at the end of March a period of about five weeks: from the end of December, 1914, to the beginning of February, 1915.
Frostbite; thrown into water by horse; horse shot under its rider who becomes: A HORSE IN THE UNCONSCIOUS.
A private in the Royal Engineers, 25, went through Gallipoli without injury and without fears. He was sent to the hospital in Malta, December 18. When observed by Eder, February 7, the frostbitten finger of the right hand was well although there was some loss of grip. He was suffering from insomnia, terrifying dreams, shaky hands. It seems that December 6, a horse started and he was thrown into the water from a bridge. The next day his horse was shot under him. A few days later, a finger was frostbitten. Then his hands began to tremble and the insomnia set in, with severe headaches.
This patient was a jovial, thickset, farmer’s son, with a diffuse enlargement of the thyroid gland, a high blood pressure, lymphocytosis, a fine tremor of the hands, irregular and rapid pulse, and anginal attacks. Extremities were cold and blue; the palms perspired markedly; there was hypersensitiveness to sound; there were occasional attacks of dizziness, with a feeling of suffocation; there was frequent desire to micturate.
The patient’s dream was always the same: He saw a Frenchman digging a knife into his horse, getting off a cart to do this somewhere in Serbia. Occasionally he had this dream in the form of a vision in the daytime. It seems that he had actually seen a French soldier plunge a knife into a mule to make it go. He had been busy with horses since childhood: as stableboy and groom. He thought that the sufferings of the mules in Gallipoli were worse than those of human beings. According to Eder, this farmer’s son was the horse of his dreams; instinctive fear had to emerge; he was pitying himself. According to Eder,[498] “That the person should become a horse in the unconscious would not startle one who has dipped into the totems and taboos of the lower races.”
Shell-shock; gassing; fatigue: Anesthesias.
A stretcher-bearer, 44, eleven years in the service and two months on French service, was seen by Lt. Col. Myers eight days after reporting sick and admission to a base hospital.
While he was under cover in a cellar, three days before reporting sick, a shell had jammed the door and the fumes came in. Later in the day, in another cellar, he had been blown off his seat by a shell and six other men had been laid out. The shelling continued that day and two following days. He had worked on the wounded without any rest.
On lying down he found his left arm numb and cold. The numbness then spread to the legs, especially to the left leg. There was continual tingling in terminal joints of fingers of left hand; hypalgesia over both forearms and hands, especially on left side; total analgesia over left dorsum.
Two days later, the patient could feel articles and reported that the numbness occurred only in the early morning and was followed by a tingling as the numbness passed off. On the same day, the hands and forearms showed a total loss of sensibility to pain, except for a small area on the flexor surface below the elbow joint.
Re spread of anesthesia and alternation of sensory symptoms in this case. Babinski, of course, believes, that the majority of these conditions are the product of medical suggestion, but Babinski meets any critique by pointing out that any other sort of suggestion may produce such results. The heterosuggestion need not be medical. Thus, the sight of a comrade with paralysis or anesthesia, organic or hysterical, may suggest such to the soldier. Léri remarks that these may also be produced by autosuggestion alone. “From a tired feeling in a limb to a loss of power in it, there is but a small step. Another step leads to paralysis and anesthesia. The neuropathic temperament takes these small steps in perfectly good faith.” Léri has found no case in which he could exclude the influence of auto- or heterosuggestion.
Shell-shock; burial; somnambulistic state: Amnesia. Recovery of memory in hypnosis.
A healthy-looking man, with flushed face and large dark eyes with wide pupils, complained of pains in abdomen, back, and limbs, chiefly in knees and ankles, and of visual impairment. This corporal said that his sight had been very indistinct since he was buried, and that if he looked at an electric light, he could see nothing for five minutes afterwards. He was admitted to the Duchess of Westminster’s War Hospital at Touquet, December 11, 1914, having been buried for 48 hours, December 8, when a shell blew in the trench where he lay. He said he could remember nothing until he found himself in a dressing station, lying on straw, in a barn. He was at that time unable to see and fell over something when he tried to walk.
He had gone out August 13, and had been in the last two days at Mons and then at La Bassée. He had slept badly and had taken a good deal of whiskey. He had led a fast life and had had domestic worries recently.
It appeared that his vision had improved since the day of the explosion; though he could read for a short time only when things became blurred, and only with the type close to the eyes. Bowels had not opened for five days. Vision in right eye was 5/60; left eye, 2/60.
Tested for smell, he failed to smell peppermint, ether, iodin tincture, and carbolic acid 1-40. Sugar was tasted only after tongue movements were permitted, as was also a strong solution of salt. Acid tasted salty like alum. The patient complained that he did not sleep, though in point of fact he slept well.
The patient was treated by suggestion, both in hypnosis and without, when he was transferred on the 31st of December, to the London Temperance Hospital, whence he was discharged. The treatment by suggestion occurred daily. At the second trial and thereafter, light hypnosis was easily[500] induced, but the deeper stages, with hallucinations, anesthesia, and post-hypnotic anesthesia, could not be reached. The lighter stages brought about sleep, a gradual restoration of memory, and later an improvement in visual and olfactory acuity; in near vision, in visual fields, and in color sensibility.
The stages in the restoration of memory are as follows: December 22, he was able to describe how he was buried, how Sergeant L. dug him out, how men of another regiment than his own took him to a dressing station, whence he was packed off by the M. O. to the dressing station of his own regiment. Capt. S. had spoken to him and given him a drink. Post-hypnotic suggestion caused him to remember this latter fact after he had come out from hypnosis.
December 23, even before hypnosis, he could remember a big hospital with a stove in the center of a big square room, and gave a fragmentary account of struggling in the trench after being buried, and of going to sleep and enjoying himself at home, when somebody started messing him about. In hypnosis, he gave further details of his dreams after falling asleep in the buried state.
December 26, further details were remembered before hypnosis, such as a ride in the motor ambulance, offers of tea, cocoa, sweets, and cigarettes, a bad headache, and the like.
December 27, in hypnosis, he was able to describe with apparent accuracy the position of the trenches and their appearance. He said:
“The explosion lifted us up and dropped us again. It seemed as if the ground underneath had been taken away. I was lying on my right side, resting on my right hand, when the shell came. I got my right hand loose but my wrist was fixed behind a piece of fallen timber. At last I dropped off to sleep and had funny dreams of things at home. One thing in particular I have thought of many times since, I have not been able to make out why I should dream of the young lady playing the piano. I don’t know her name and I don’t think I have seen her above twice.”
According to Myers, it is questionable how far the patient’s memory can be trusted; and there is considerable doubt[501] whether the man had remained in the trench for more than an hour after the shell had burst. A comrade said that the doctors at the barn thought the man off his head. Another soldier, familiar with the positions of the regiments in question, gave information suggesting that the patient had wandered in a somnambulistic state from the trench, past his own dressing station to that of another regiment.
Re Shell-shock and burial cases, compare remarks of Grasset and of Foucault concerning the feeling as if dead on the part of certain buried persons. Somnambulism is a natural sequel to such feelings. For somnambulism, compare cases of Milian (364, 365, and 366).
Shell-shock; minor injuries: Somnambulistic “carrying on”; fatigueability, physical and mental.
A lieutenant of infantry, 31, threw himself down on the earth September 9, 1914, as a shell was passing over him. The shell exploded and seriously injured a soldier one meter away. The lieutenant got up and ran for cover about twenty meters distant. Only six and a half hours later did he perceive that there was a small skin lesion between his thumb and index finger, caused by a shell fragment, as well as a superficial burn on his right temple. Neither wound bled or had to be dressed. He carried on, aware that they were marching toward the River D.; but only two or three days later did he find they had already marched to the other side of K., had rested there and spent the night in various places in between. During this whole period the lieutenant led his battalion and held a piece of woods without anyone’s noticing anything striking about him. These dazed states were twice repeated, for periods of ten and twenty-four hours respectively, and finally he was brought behind the firing lines unconscious.
The physician found him to be in a state of exhaustion, pulse 108, and had him brought to the nearest station. There Donath found increased tendon reflexes, some dermatographia and increased fatigueability of mind and body. He was especially fatigued by walking, though he had always been a good mountain climber. He was now unable to concentrate on reading, writing or calculating, though he had been accustomed to dictate letters and calculations in his official work in peace times. He had seizures of crying and trembling on September 10 and October 27, both quieted by bromides. There was diminution of sexual power.
Rest, lukewarm baths, cold compresses to the head, and psychotherapy improved his status rapidly.
This patient had never been epileptic or hysterical, subject to dazed states of any sort, was weak, delicate and anemic (three sisters leukemic), but had before the war been well.
Emotion of captain who saw men burned by bomb: Stupor “as if dead”; awakening “as if a German prisoner.” Recovery.
A captain, one day seeing some of his men hit by incendiary bombs, felt the deepest kind of emotion. He threw his coat over one of his men and succeeded in smothering the fire. Of a sudden, he completely lost consciousness, only regaining contact with the outer world two days later, in the sanitary train. He did not know where he was, but thought himself a prisoner surrounded by Germans. The disorder of consciousness lasted three days, and the memory of what happened during those days never returned. In fact, the captain declared that he felt as if he had been dead during that time. His dreamlike state lasted for some time, and for several weeks he did not sleep without disturbing nightmares. It was always the same night attack, with the burned men and the anguish of feeling that his men were not about him and that he was alone in the skirmish. He later recovered entirely and made preparations to start for the front.
Re feelings “as if dead,” see remarks of Régis under Case 293.
Emotions over battle scenes: Spontaneous hypnosis or SOMNAMBULISM lasting twenty-four days.
Upon recovery from a state of apparent hypnosis described below, the victim wrote, in part, as follows:
“After marching two days we reached a Breton village near Virtou. Next day we were in a battle that lasted from seven in the morning to eight in the evening. I was somewhat troubled by the first balls and bullets that whistled by, but felt I had to get used to them and we marched on, under our brave captain’s orders. Then we really got under fire. It was sad to see my comrades falling under the murderous bullets, and the captain was soon mortally wounded; but we had reinforcements and went on and chased the enemy from his positions. During the battle I kept thinking of my old mother and father and I felt that I should die without seeing them again. Little things about the family came to my mind. I saw my father’s roof, and his favorite garden seat, and I saw my mother weeping over her only son, her only ambition in old age. The return from the battle was very sad for me. Night began to fall on the frightful field. I saw on the bare earth the bodies of poor comrades whose joys and sorrows I had shared. There they were, cut down in all the strength of youth, leaving their parents in trouble, their widows in despair, and their poor orphans. I wanted to carry them off and I could not. We had to march over their glorious remains. I was able to give a word of encouragement to one of my comrades who now probably is no more. We then retired. Although I was very weary, I was unable to get any rest. My mind was occupied with the frightful things I had seen. I thought of the comrades over there and that no one could help them. I remember I drank coffee the next morning and talked with my relative. Then that is all. From that time I do not know what happened.”
The writer was an infantryman, 20, who had been employed in civil life in the Crédit Lyonnais, and was brought August 24, 1914, to the Saint Nicolas Hospital in a state of hypnosis.
Once placed in the standing position he kept balancing back and forth, with head motionless, eyes fixed and directed to the left side. He did not speak in reply to a request for his name or facts about his life, but as soon as the battle was talked of he began an expressive pantomime, speaking in a very low voice a few words interrupted by sighs. “What were you doing in the fight?” He extended his arms, described a half circle with his hand, as if to show the extent of the field, thrust his hands forward with a finger outstretched, saying, “Zi, zi,” as if to indicate whistling bullets; plunged forward with hands in front of his chest, as if holding a gun in charge bayonet position, saying “Prussians, Prussians,” and threw himself down in a kneeling posture, saying, “Trenches, trenches.” “Do you remember the battle?” “Belgium, Belgium. Germans pushed back,” making a sign as if chasing them. “Captain dead. Two hundred men dead.” With a suitable gesture he sighed, and tears ran down his face.
August 28 the mutism was still almost complete, but he could say his name and lay stretched out on the bed.
September 4 the hypnosis was less, but the delirious state was more active. He got up in the night and tried to escape to help the wounded. In the daytime, if he saw a man lying down resting he went to him and unbuttoned his coat to see whether he was wounded. Upon seeing the physician he would cry, “Major! Wounded! wounded!” and then pull the physician by his coat. He could hardly be stopped from these maneuvers. He had to be fed like a child, but went alone to stool.
He began to be employed about the hospital a little September 14, in sweeping the room and in guarding another patient in complete somnambulism, over whom he watched as over a child, leading him by the hand and keeping him from bumping into objects.
September 16 he awoke suddenly. Some one had talked to him about his own village and his relatives. He was astonished to find himself in a hospital. He wrote out, on request, the above account of his recollections. The man was 177 cm. tall, well proportioned; showed a slight facial asymmetry and a few other facial features of a dystrophic nature, such as an adenoid appearance. There was no stigma of hysteria.
Putative loss of brother nearby in battle: Spontaneous hypnosis or somnambulism; mutism, except “Mamma, Mamma.” Sudden awakening after twenty-seven days.
A man, 22, was brought to the Saint Nicolas Hospital in a sort of coma August 24, 1914. He lay on the bed, eyes closed as if asleep, insensible to excitation, irresponsive. Flies crawled upon him with impunity. He did not wink. The arms raised fell back inert. The corneal reflex was absent on the left side, diminished on the right. The knee-jerks and the skin reflexes were normal.
Next day he had to be fed like a child and looked after. Lifted from bed, once on the ground he stood up with flexed legs, as if to crouch. It seemed as if he was about to fall, but he did not.
The next day he was in the same immobile state. Upon removal from bed he again made as if to fall, but got his balance. He kept his legs flexed, his head lowered in a fixed posture, with his eyes on the ground. He would walk quickly without falling, if taken by the hand, feet dragging, and even holding back with a certain amount of force. His walk suggested that of a somnambulist. He was left in a standing posture by his bed throughout the medical visit. After a few minutes he began to flex his legs progressively and slowly. The attendant cried out, “He is going to fall.” Instead of falling, he sat down upon the floor near the bed. He was in the same immobile, somnolent state September 1, eyes half open, hidden under long lashes. Flies walked over his eyes and lids, but he did not wink. He would rise only when pushed and walk only when pulled, but had begun to eat a little better. To all questions he replied, from between his teeth, “Mamma. Mamma.”
The next day there was a bit more spontaneity in his walking.
Lumbar puncture showed a slight hypertension. There were traces of albumin and very few lymphocytes.
September 6, he was able to eat soup alone, but kept the same immobile posture, with eyes fixed on the ground, eyelids not winking, in a posture suggesting Parkinson’s disease, but without rigidity. He still replied only, “Mamma. Mamma.”
September 19 the patient suddenly waked up completely. Douches and external irritations had not served to wake him up, but a soldier told him upon this day that his brother was not dead, as he believed, but was alive and he then began to speak, opened his eyes, and began to talk. He told how he had been by the side of his brother in battle. Germans had taken them in the flank and opened machine guns upon them. Two men had fallen by his side, and, catching at his garments, kept him from retiring when the order was given. He got loose, looked for his brother among the corpses, could not find him, thought him dead, and from that point forward had been without memory. He shortly became perfectly normal.
Shell-shock; slight trauma; windage felt; fall; loss of consciousness; wandering, conscious, over night; shrapnel burst: Spontaneous hypnosis or somnambulism, lasting four days. Return to the corps.
An infantryman, 20, boxer by profession, was brought with other wounded, in the night, to Saint Nicolas Hospital and was seen next morning, August 24, in bed, lying motionless on his back, eyes open, fixed, eyelids not winking. No reply was got to questions. The arm lifted fell back upon the bed, although slowly and not heavily as in apoplexy. There was no catalepsy. The patient was taken from his bed and put upright. In this position he remained immobile, hands at side, head bent forward, eyes fixed on the ground. The eyelids did not move upon approach of the finger or a lighted candle, unless there was a fine beginning of movement. If he was pushed, he made two or three steps forward, with eyes fixed on the ground and head bent forward. The only spontaneous movement was carrying the left hand back to the side as if to take the bayonet. He got into bed alone.
Next day the patient could walk better and began to talk, but preserved the same absorbed attitude. He told, in monotonous voice, of the shells that his squad had received and of the dead that he saw about him. August 27 he woke up and was unable to tell how he had come to the hospital. He told how the regiment had been bombarded for a time and how a shell burst near him; how he got a splinter in the buttock (of which the contusion was still visible); and how he had been thrown down by the windage of the shell. His sack had been torn from his shoulders. He had lost consciousness, he thought, for a short time, anyhow he could not find his regiment. He passed the night near Longuyon and next day looked for his regiment again. Shrapnel burst near him, and from that time forward he had lost memory. August 27, at his express request, he started back for his corps. There was no stigma of degeneration or hysteria.
Burial; struck in head by beam; overcome by gas: Tremors, convulsive movements, confusion, flight toward enemy.
An Italian private, 28, of meager build (infantile eclampsia; brother epileptic) was buried by a shell explosion and overcome by gas. After a month’s leave he went back to the trenches.
But now, whenever a shell burst, he fell into irresistible terror and made convulsive movements which he forgot afterwards. He could not sleep. The mere memory of the scene would throw him into terror. He was tremulous, developed asymmetrical innervation of his face, was generally hypesthetic and mentally blocked.
In the midst of convulsive tremors he fled towards the enemy. He was stopped and brought back, and remained for two days confused and hallucinated.
In the original accident he had been struck in the head by a beam.
Re this Italian’s flight toward the enemy, see various cases of fugue. Clinically and medico-legally, Roussy and Lhermitte remark that these confusional escapades are of great interest, and that many cases are encountered near the front line, put under trial by court-martial, and handed over to specialists. The dream is being lived through. Such a case as this of Consiglio recalls the hystero-emotional psychoses of Claude, Dide, and Lejonne. The relation of oniric delirium to mental confusion is still a matter of polemic. According to Régis, however, the common oniric delirium of toxic or infectious origin is nothing more than a sort of somnambulism. The retrograde amnesia which follows toxic delirium is the same in principle as that which follows hysterical delirium. Régis pointed out that suggestive hypnosis could bring back the memories in both types of disease, as well as from the toxic delirium as from the hysterical somnambulism. However, the differential diagnosis between onirism and hysteria is not easy. Alcoholism and actual brain trauma need to be excluded.
Shell-shock; windage; unconsciousness: Carried on with fugue tendencies. Variety of hysterical symptoms. Fit for garrison duty four months from explosion.
A non-commissioned officer, 22, entered service at 20, went into the artillery and had been advanced repeatedly. There was no heredity; the man had been a moderately good scholar. It appears that he had had at 17 a febrile angina with delirium.
September 25, 1914, a big shell load for a cannon was exploded by the enemy. All the men about the cannon were thrown to the ground by air pressure, and the officer became unconscious. On awaking, he had headache, dizziness, and vomiting. There were many corpses lying about him.
He resumed work at once, but in the evening his headache and dizziness increased and there was “a feeling inside as if he had to run away.” This feeling appeared to come from the heart; it was an oppressive feeling, running to the head. On the next day he did gun duty, noticing, however, that every shot he fired caused him a sharp pain. He was relieved from work at 11 A.M., and was declared ill by the physician. His comrades told him that he had often been noticed trying to run away, but about this he himself declared he knew nothing.
He was received at the Jena Hospital, October 9, 1914, a very strongly built and well-nourished man. Neurologically, he showed a marked dermatographia; knee-jerks were obtainable only on reinforcement; Achilles jerks somewhat more marked; there was a weakly positive Oppenheim reflex. The abdominal reflex on the left side was greater than that on the right; and this was also true of the cremaster reflex. Percussion of the head was extremely painful; and there were painful points on pressure of the spine and head.
Touch was poor on the entire left side of the body; but there was no diminution of sensibility to pain. There was[511] a fine static tremor of the hands. The strength of both hands appeared to be decreased (dynamometer). Gait was unsteady and stiff; Romberg sign was positive; the patient fell over backward. Hearing was greatly diminished, ordinary speech being heard only close to the ear.
Toward evening of the second day after admission, there was a marked attack of dizziness while the patient was lying on his back in bed. During this attack the face was very red. It lasted two or three minutes. Hearing was remarkably improved on the left side for some time after the attack. The ear clinic examination, October 19, showed much disturbance of hearing on the right side (direct injury of the vestibular apparatus in both ears).
Headaches continued, radiating from the orbit to the top of the head, and sensitiveness to pressure at the exit point of the upper branch of the right trigeminal. The whole of the forehead was somewhat red and swollen (neuralgia of the frontalis). The patient wore dark goggles on account of his marked photophobia.
Improvement was gradual; there was a transient slight swelling and a venous hyperemia of the nasal mucosa, which was treated in the nose clinic. The impairment of hearing was quite gone in two months’ time, though buzzing was now and then heard in the right ear. The supersensitiveness in the right upper trigeminal region vanished also. The patient was discharged January 21, 1915, fit for garrison duty. Later he went into the field again.
Burial: Dissociation of personality.
The following are some stories told by a “lost personality” under hypnosis.
The patient, aged 24, was a bandsman in the Second Battalion Wiltshire Regiment, who sometime near the end of October 1914, was buried in a trench near Ypres. This is his account:
“I was dug out at night and taken to a dressing station; it was cold and dark. Then I went on to a hospital at Ypres; it was really a convent, and there were a lot of nuns about, dressed in dark robes with white hats; some of them spoke English. I stopped there for a night and a day. There were a lot of wounded there. Then I was sent on by train; I lay down all the way on a seat in the carriage; we took the whole day to get to ——, and kept on stopping at stations. I was at —— about ten days; I don’t know what hospital it was, but there were English doctors and nurses. It was near the harbor. We came over to England in a hospital ship, the Arethusa; I went straight on to Manchester by train. The hospital there was really a school turned into a hospital.”
Here is a brief account of a scrap with some Uhlans.
Q. Did you see any Uhlans? Yes.
Q. What are they like? They’ve got no guts. One time 30 of them were against 8 of us infantry, and they “done a bunk.” Their horses were not bad. They wore helmets with a double eagle on the front.
He was asked to describe the country round the trenches and to give some account of the fighting there:
“It’s agricultural land, ploughed fields. There were two farms in front of us. One day we saw an old cow between our trenches and the Germans, and we all had pot shots at it. Once the Germans rushed our trenches; we killed hundreds, bayoneted them mostly, and hit them over the heads with the butts of our rifles. It was hellish. The British were all shouting. I saw a German officer behind with a sword and a revolver. I saw a lot of French soldiers, too; they wore long coats with the corners turned back; some had blue and some had red trousers. The French dragoons are like Life Guards, with big steel breastplates and brass helmets with a long plume; they carried swords and rifles and a few had lances.”
He was asked to mention some of his impressions in Belgium and what he thought of the manners and customs of the French and Belgians.
“We cut off all our buttons and gave them to the French girls. The French cigarettes are muck; you buy them in little blue packets; the tobacco is rather dark and strong. When we bivouacked on the march at night we were not allowed any lights, but you could smoke by digging a hole in the ground with your bayonet and smoking into that.”
The following are some of his remarks about his stay at Gibraltar.
“Gibraltar’s like a great big rock; the steep side looks toward Spain. I was in barracks there, and used to spend a lot of time in the band-room practicing. Sometimes we bathed in the sea. I went to Spain two or three times and saw some bull-fights; they were very exciting, but rather too cruel for my taste. They used to kill six or seven bulls a day. The horses got fearfully cut about.”
This bandsman showed what Feiling calls dissociation of personality. There was an amnesia of such degree that all conscious memories of the patient’s life, as well as all memory of letters, objects, and life in general, were suppressed. The patient was brought, after the burial above noted, to the hospital for epilepsy and paralysis at Maida Vale, January 21, 1915. After his experience, he had been transferred to the Second Western General Hospital, Manchester, where he spoke sensibly, understood and was able to remember things since the burial. His mind was a complete blank for all previous experience. He was unable to recognize his own father or relatives. He was slightly deaf for a time but this defect disappeared.
At Maida Vale he showed a nervous twitching of eyelids and facial muscles; otherwise he was neurologically and[514] physically normal, dreamless, without complaints, and straightforward about all experiences since coming to himself in the hospital at Manchester. He took his parents on trust. “I don’t know if I ever went to school.” “A bayonet is like a knife; you see soldiers with them on their rifles. I have never seen a bullet.” His memory for recent events was also not good. He once recognized a single tune played at a concert.
Suspected of malingering, he was tried out in various ways. He was told that an elephant was a little furry animal and shown a little 6 inch toy sample. On going to the zoo he was greatly astonished at seeing a real elephant. He did not know what the war was about and he had no interest therein.
March 10 he was hypnotized and proved an easy subject. Powerful suggestions that lost memories would return were unavailing. The next day, during hypnosis, it was found that his previous experience could be readily tapped, and a history of his family, schooling, running away, and eventual enlistment was told. He had been at Gibraltar when war broke out. He was at the first battle at Ypres, and was for ten days in severe trench fighting, and was finally buried in the mud and débris of a trench blown in by a high explosive shell. He had been buried for about 12 hours, was dug out at night, and (according to his father) remained unconscious 24 hours, and deaf and dumb three days. He was transferred to another hospital and then to Manchester, where he came to himself.
Only during the first few sittings did the patient lie with eyes closed. Later, during hypnosis, he behaved exactly like a normal person. The fact came to light that when hypnotized the patient returned to the personality that possessed him just before awakening in Manchester, and accordingly during hypnosis, he had to become acquainted again with his hypnotizer. Maida Vale astonished him, as it should have been Manchester. Thus there were two personalities: No. 1: The personality since the date of the Manchester awakening; No. 2: The personality containing all the memories of the past life as well as the more recent Flanders memories. In State No. 1, the manner was jaunty and cocksure. In State[515] No. 2, the man was more modest and less loud. Moreover, though in State No. 1 he spoke with a Lancashire accent, in State No. 2 his speech was in the West Country dialect—a strange observation, confirmed by several observers. He was asked to write down the answers to questions, and on awakening from hypnosis was shown the things written; whereupon he laughed and said, “Why, that’s not my writing.” On writing out the same sentences again, various minor points of difference were apparent. Hypnotized in the presence of his father, in whom in State No. 1 he took no great interest, he showed every sign of joy, causing his father to think that in State No. 2, his son had “come all right again.” In State No. 2 he could play a euphonium better than in State No. 1; but after practicing in State No. 1 he rapidly became as expert as in the hypnotic state.
If the patient were left for some time before being awaked by a previously-arranged method of counting three, he would experience disturbed dreams, with clenched hands, snarling lips, and muttered phrases, “Give it them,” etc.
Twenty-five hypnotic sittings were given but no improvement took place and the patient was discharged May 5. May 25 there had been no further change and he remained in State No. 1, in which state he was invalided from the service by a medical board, May 28.
Ear complications and hysteria.
An infantryman, 22 (father and mother quite normal; patient showed slight convulsions, attributed to worms, from which he actually suffered; was malarial from 9 to 15; had otitis media and lost hearing completely at 11; had suffered from 9 onwards with joint pains; as an adult had no convulsions), was called to arms August, 1914, and sent to the front May 2, 1915. About the end of August, in a water-filled trench by Monte San Michele, he was covered with mud from a shell explosion, lost consciousness, and in some way got back to the second line. He was told that blood had flowed from the right ear, and on recovery he found himself unable to hear with that ear, although it was the left in which he had had otitis. There were continual noises in the ear. He was, however, sent back to the front line. By mistake, one day, he got with companions in the midst of the enemy’s barbed wire, saw sparks from the guns, heard no shots, saw comrades fall, and threw himself instinctively into the wire network. Leaving the food kettles, he finally got back to the trenches. He was sent to the hospital at Legnano for his ear pains, and was treated by leeches, which he could not feel. He began to hear a little more. Flies walked on the left cheek without being felt. This anesthesia had begun a few days after the shell explosion. He was transferred to a military hospital at Florence.
One day he wedged a toothpick in cotton into his left ear and was charged with simulation, though he had been absolutely deaf in his left ear since childhood. From the moment the military surgeon told him he would be denounced for simulation, he lost his memory. Reports indicate that he had headache and delirious dreams (October 30), and suddenly he became furious (October 31), about three hours later going into severe collapse, for which camphor injections were given.
November 1 he had battle dreams and lumbar puncture had to be given up as he was in the midst of an attack. A[517] hypodermic injection was interpreted by the patient as a wound, and he cried as if he were being abandoned on the battle-field. At one point he woke up from his hallucination and asked where he was and shortly relapsed into stupor. November 2, the patient was slightly bewildered and felt pains where the lumbar puncture needle had been tried the previous day. November 5, he was disoriented, thinking himself still at Legnano. The pupils were throughout dilated. November 6, confused and dreamy; November 7, he soiled his bed, was somewhat disoriented, immediately corrected himself; oculo-cardiac reflex 64 full compression, 62 during compression. November 11, headache; November 12, a slight bewilderment reappeared; November 13, remembered for the first time having been stunned by shell explosion, and this day got up and wrote home. November 14, complained of pains in muscles and weariness. Pupils still dilated. November 16, pulse 86; a gradual increase from 50 to 60 during previous days. November 17, patient had begun to remember facts that preceded the dream syndrome. November 18, pulse standing 88; November 20, pulse standing 120. This day cried when he remembered having been suspected of simulation. November 22 and 23, aches in joints and intense otalgia; pulse 86. November 24, diarrhea; deafness somewhat diminished; 26, diarrhea; looked as if he were about to have a new hallucinatory episode. This, however, did not come about until December 1, when he heard cannonading and knew the regiment was near. Next day he had forgotten the cannonading. December 14, the patient had become entirely tranquil and lucid and was able to give his entire history. December 16 and 17 he was given a systematic neurological examination, which showed on the left side complete anesthesia, hyperesthesia to pressure, thermanesthesia, analgesia, loss of bone, tendon, and muscle sensation. Vision was diminished more on the right side than on the left, and the visual fields on this side were more contracted. During examination, the fields became still more tubular. There was complete deafness, anosmia, and ageusia on the left side. On the right side there was a slight diminution of hearing. The pharyngeal[518] reflex was abolished; the cremasteric reflex was somewhat less on the left than the right; and the defensor reflexes of the left leg were less marked than those of the right. There was no clonus or Babinski. The dynamometer grasp on the right was 37; on the left 18; and on this side there was a limitation of voluntary movements.
| WOUNDS | 14 of 150 |
| PHYSICAL | |
| Exhaustion From Exposure, Hardship (all neuropaths) | 3 of 142 |
| Concussion | 52 of 142 |
| CHEMICAL—Shell Gas | 3 of 150 |
| PSYCHIC | |
| Gradual Exhaustion, Predisposing (43 neuropaths) | 51 of 132 |
| Same, Acting Per Se (patients chiefly neuropaths) | |
| Sudden Shock | |
| Horrible Sights | 51 of 142 |
| Losses of Companions | |
| Fright Near Explosion (one neuropath) | |
| Sounds (a few neuropaths) | |
| RELAPSES (41 of 150 observed, three-quarters neuropaths) |
After Wiltshire
In the course of our study of psychoses incidental in the war (Section A) and especially of Shell-shock’s nature and causes (Section B), we have naturally met most if not all of the major diagnostic difficulties. In the present Section we shall study cases for the light they may throw on the more technical troubles of the diagnostician. Who would à priori have felt that such diseases as tetanus, rabies, malaria, would produce practical difficulties in clinical diagnosis in the field of Shell-shock?
Mayhap there was no need to emphasize further the values of lumbar puncture fluid examination. Yet the admixture of “functional” and “organic” symptoms in numerous puzzling cases can hardly be over-emphasized.
But the interpolation, through the ingenious inquiries of Babinski, of a new or but vaguely suspected series of “reflex” (“physiopathic”) troubles between the organic neuropathic disorders on the one hand and the hysterical psychopathic disorders on the other—the result of these observations, sampled only in Section B, is given more in detail in the present Section. What a split in therapeutic method a recognition of this new group of “physiopathic” disorders might entail is seen also in further cases in the Section that follows this (Section D on Treatment and Results).
A number of simulation cases has been added.
| I. | NEUROSO-ORGANIC ASSOCIATION (NO CAUSAL NEXUS) |
| II. | REFLEX NEUROSES (LESION DISPROPORTIONATELY SLIGHT BY COMPARISON WITH PSYCHONEUROSIS) |
| III. | NEUROSO-SOMATIC ASSOCIATION (Trench Foot, Neuritis, Radiculitis) |
| IV. | FATIGUE OR EMOTIONAL PSYCHONEUROSES (CONSIDER EFFECTS OF PSYCHIC CONTAGION, EDUCATION) |
| V. | PSYCHONEUROSES ON ANTEBELLUM BASIS |
After Grasset
| I. | EMOTIONAL (Hyper- Hypo- Para-) |
| II. | CONFUSIONAL (Attention and Memory Disorder, Dream States; Deliria) |
| III. | CONVULSIVE AND PITHIATIC (Hysterical) |
| IV. | NEURASTHENIC AND PSYCHASTHENIC |
| V. | SENSITIVOMOTOR AND SENSORIMOTOR—e.g., Limited Paralyses, Contractures, Deaf-mutism |
| VI. | COMPLEX |
| VII. | PHYSIOPATHIC (Babinski) |
After Grasset
Value of lumbar puncture.
A colonial soldier arrived at Paul-Brousse Hospital with a hospital ticket showing that ten days before he had had commotio cerebri. He was dull, had a fixed stare, held his head in his hands, was disoriented for time and place, and had lost memory for everything that had happened for eighteen months. There was no sign of wound. There was no motor disorder save that walking was a bit slow and uncertain. Perhaps the right knee-jerk was stronger than the left. Percussion of the right Achilles tendon produced tremor. The plantar reflexes were flexor on both sides; flexion lasted longer right than left. The cremasteric and abdominal reflexes were a little weaker on the right. Arm reflexes were lively. Sensations proved normal. Complaint of headache, frontal and vertical.
Lumbar puncture October 7, that is, on the thirteenth day after the shell-shock, yielded a transparent, slightly greenish fluid, with 92 cells per cm. (lymphocytes with one or two large mononuclear cells and a few sometimes degenerated endothelial cells) and hyperalbuminosis.
October 9, the clouding of consciousness was less marked. The headaches and amnesia were constantly complained of; the reflexes were normal. October 12, there was less headache. October 25, another lumbar puncture showed but 14 or 15 lymphocytes per cm. and hyperalbuminosis. There was now no longer any clouding of consciousness. The amnesia, retrograde and anterograde back to May 9, 1914 (date of his daughter’s birth), and up to September 25, 1915, persisted. The man did not remember the declaration of war, or the mobilization, or his regiment, and the like. Meantime, the man’s judgment and reasoning powers were normal.
If there had been no early spinal fluid examination of this patient, he might well have been considered an hysteric or even a simulator.
Meningeal and intraspinal hemorrhage: Lumbar puncture.
A gunner from Morocco, who lost consciousness for an hour March 28, 1915, upon the explosion of a large-calibre shell in his trench, was carried to the ambulance. He complained of headache and generalized pains. His status was scarcely modified during five weeks, and a generalized contracture of the body developed whenever movements were attempted. In horizontal decubitus, the muscles of the limbs and neck were of a normal tonicity, but the head went into hyperflexion if the patient was asked to sit. The eyes turned upward, and Kernig’s sign developed. The patient could walk only with short steps, with legs apart and arms held away from the body, the head in a sort of tetanoid dorsal hyperflexion. There was a right-sided hemiparesis with trepidation and the Babinski sign.
Lumbar puncture assured the diagnosis of something organic. The fluid contained blood cells and a marked lymphocytosis. The symptoms evidently depended upon hemorrhages in the meninges and the nervous system, affecting particularly the right pyramidal tract.
Re hypothesis of organic changes in hysterical cases, Roussy and Lhermitte remark in comment upon albuminosis in the cerebrospinal fluid that the albumin is perhaps due (in cases of camptocormia) to the effect upon venous and lymphatic circulation of the spinal curvature. It was Sicard’s claim that camptocormia, or bent back, was due possibly to anatomical changes in the spinal column, that is, that camptocormia was in one sense a spondylitis. In other cases the camptocormia might be due to a ligamentous or muscular change; that is, to a syndesmitis or a psoitis. His idea was that the curvature was in a sense antalgic; that is, a response having the purpose of avoiding pain.
Slight hyperalbuminosis.
A farmer, 32, in the 66th Infantry, was lying in a dug-out March 5, 1915, when a bomb threw him on the ground and covered him with earth. He was picked up unconscious, and remained so for an hour. In the ambulance it was found that he could hardly stand, could not speak, and appeared to be completely confused. There was no sign of wound. The next day he recovered consciousness and complained of a violent headache. He was completely deaf in the left ear, and vision was also a little impaired on that side. The puncture fluid was clear, and there was a very slight excess of albumin by the heat test. The next day the headache had entirely disappeared, the left ear was absolutely deaf, but the patient complained of buzzing. Lumbar puncture the following day showed a normal amount of albumin.
March 16 the patient was evacuated to the rear presenting no abnormal symptom except deafness.
Re the spinal fluid, Armstrong-Jones considers that a shock directly sustained by the spinal apparatus through sudden impact to the surrounding cerebrospinal fluid, ought to be felt more by the anterior horn cells than by the spinal root ganglia, since the latter are shielded by the sheath in the intervertebral spaces. Motor symptoms would, naturally, then be more frequent than sensory symptoms. He also believes that the controlling neurones in the intermedio-lateral tracts that have to do with the sympathetic system, would be affected just as anterior horn cells are. Accordingly, the dilated pupils, rapid heart, dyspnoea, and a variety of precordial pains and disorder of the viscera would ensue. The jar would thus be communicated to the neuronic cells of origin of two types: spinomuscular and preganglionic, leaving the gangliospinal neurones relatively intact.
Paraplegia, organic: Lumbar puncture.
A gunner, 23, was thrown to the ground, according to his story, by the explosion of a large-calibre shell, at eight o’clock in the morning of September 10, 1914. He could not get up but thought he had not lost consciousness. September 13, he arrived at hospital, looking like a man with dorsolumbar fracture of the spine. There was, however, no external injury. There was a marked paresis of the right upper extremity, with diminished sensibility, weakened reflexes, numbness, formication. The right lower extremity was subject to complete flaccid paralysis, with lost reflexes, and anesthesia in all respects reached to the belt level, and stopped sharply at the median line of the abdomen. The left leg, also, was paretic but the muscles could be contracted weakly; the knee-jerk was exaggerated; there was a tendency to epileptoid trepidation, and the sensations were only slightly diminished. There was a Babinski reflex on the right side; the abdominal reflex was absent on the left side; both cremasteric reflexes were present. The feet at times gave formication. Rectal, bladder, and sphincter paralysis. Dark albuminous urine, with a few blood cells, was obtained on catheterization. There was an early sacral decubitus; consciousness was somewhat clouded. The man made no requests except for something to drink, and seemed apathetic.
Lumbar puncture, September 14, yielded hemorrhagic fluid. Three days later, the upper extremity regained its powers and sensations, but the paraplegia had become complete, with abolition of reflexes on both sides, and absolute anesthesia. The feet yielded formication at times, however. Sacral decubitus increased and healed not. The temperature varied between 38 and 39. The patient died September 24, in coma, with anuria and Cheyne-Stokes breathing.
Gunshot wound of spinal column; no penetration or injury of dura mater: At first quadriplegia; later cerebellospasmodic type of disorder.
A soldier, 22, sustained a gunshot wound in the neck about the level of the fourth cervical vertebra. He immediately became quadriplegic. He recovered arm motion in two months and some weeks later ability to stand and walk.
Three months after the injury, station was difficult, better on a broad base. Rombergism, even with eyes open. Cerebellospasmodic gait. There was no weakness of leg muscles, but there was a certain degree of weakness of the upper extremities, especially in finger flexion. There was hypertonia of the muscles of all the extremities and the hands showed the signs of Raimiste, of Klippel and Weil, and of Dejerine. Static equilibrium was preserved to the will, but the kinetic balance was affected, and as much in the upper as in the lower extremities. Ataxia, tremors, dysmetria, adiadocho-kinesia, and disorder of combined movements in thigh and trunk flexion were all in evidence. Meantime, there was no disorder of sensation whatever except that the ulnar border of the right hand showed a hypobaresthesia, and there was a disturbance of tactile discrimination and absolute astereognosis in the hands. The deep reflexes were everywhere increased, and ankle and patellar clonus were easy to excite, especially on the right side. Bilateral defense reflexes. Bilateral Babinski sign. The hypertonia and ataxia ebbed away during the following three months. Walking became normal, and there was little sign of difficulty except astereognosis of both hands, combined with slight disturbance of deep sensibility and poor response to compass test in palm.
We here deal with a case of spinal column injury without injury to the dura mater. This cerebellospasmodic form of the superior cervical type of spinal concussion is less frequent than a quadriplegic form with Brown-Séquard syndrome. It is striking that both types of concussion may recover.
Spinal column trauma, with local signs: Later, hysterical anesthesia and contracture of back muscles homolateral with the trauma.
A musketeer, wounded August 20, 1914, by a shell splinter in right side of vertebral column, fell unconscious, but was able afterward to crawl on all-fours out of the firing line. Severe vomiting and epistaxis followed. August 23, there was pain in the small of the back; the last two ribs were painful on right side; and the muscles were slightly swollen up to the iliac crest. August 30, a slight rise of temperature (at first it had been above 38) still persisted, but the muscular swelling was diminished. Treatment by aspirin and baths. No further rise of temperature after early in September.
On October 9, patient was permitted to get up, whereupon he showed a peculiar curved attitude of the body, reduced almost completely by passive straightening. Swelling of the longitudinal muscles. Radiograph negative, except that one picture showed a change in left twelfth rib, near the transverse process. Pains in left lumbar region.
November 19, on examination, pulse 112. November 23, after massage, vomiting. Temporary use of plaster corset.
On admission to the nerve hospital December 22, the musketeer was unable to extend the trunk, and the long muscles of the back were on the stretch, often as hard as wood, especially those of the left (longissimus dorsi). Patient lay on right half of pelvis. Hemianesthesia and hemianalgesia, left side. Tachycardia. Formerly the patient had done hard work, especially carrying heavy bags. He declined to be examined under general anesthesia. He seemed to be of unreliable character, and his trouble did not prevent him from returning from leave of absence, on one occasion, drunk.
Mine explosion: Combined hysterical and lesional effects.
A lieutenant, 23, was in a mine explosion June 23, coming out in complete torpor, with mutism and retention of urine. He was brought to hospital June 26, with jactitation, irregular pulse, markedly exaggerated tendon reflexes, absent skin reflexes, sluggish, dilated pupils, especially right, and general anesthesia. The spinal fluid contained an excess of albumin, altered blood cells and many lymphocytes.
Several hours after puncture he suddenly demanded where he was, thought it was the year 1911 when he was in the Dragoons, talked about his camp, and was confused, irritable and stereotyped in questions. There was no verbal amnesia. Speech was hesitant, explosive and scanning, suggestive of multiple sclerosis. Next day there was still retrograde amnesia. He clung to the belief that it was July, 1911, and asked wearisome, stereotyped questions. The words, “German house” caused a jactitation, stiffening and relapse into a second état, out of which he came with hiccoughs and sighs, and amnestic for this conversation. There was general hypesthesia and muscular weakness especially of legs. The reflexes were as before.
The morning of June 28, he heard the hum of an airplane, whereupon his memory returned. It seems that he had himself once ascended. The memory gap was now limited to the time immediately preceding the mine explosion and the days following, up to the time of hearing the airplane. He told about his military life and also about incidents immediately preceding his blowing up. He complained of malaise and of pains in the vertebral column and limbs.
There was a quadriparesis, more marked, however, on the left; walking with falls to the left; astasia with left foot; double facial paresis; inability to whistle and to close eyes completely; intestinal and bladder paralysis; nocturnal emissions non-pleasurable; partial anesthesia of right leg, of[531] arm and of hand, with hyperesthesia of thigh, of forearm and of the posterior aspect of the upper arm; anesthesia of the left side, including thorax and abdomen, excepting that the arm was hypesthetic only. Face hyperesthetic. Complete anesthesia of nipple and testis; hypesthesia of neck; anesthesia of tongue, nose and vertex; plantar, cremasteric, abdominal reflexes absent; exaggerated tendon reflexes; pupil reflexes normal; painful heat flashes and profuse sweating on the slightest movement; vertigo and tendencies to syncope after effort; explosive, scanning speech; intermittent convulsive movements of the arms. Palpation and X-ray show separation of the spinous processes of the third cervical vertebra.
Improvement was marked and progressive in motor, sensory and reflex fields. At the time of report three months later, there was a definite paresis of the left leg, with anesthesia and absent plantar reflexes, and slight paresis of the orbicularis palpebrarum, scanning speech and syncopal tendencies. Here, then, due to diffuse, non-systematic lesions, with superadded hysterical manifestations, were probably some effects of a permanent nature due to destructive processes.
Re combination of functional and lesional effects, Sollier and Chartier state that in Shell-shock hysteria, physical causes and conditions are the chief factors; that in the so-called hystero-traumatism of Charcot, the psychic and physical factors are of virtually equal importance, and that in ordinary cases of hysteria, the psychic is the chief genetic factor.
Shell explosion: Hysterical and organic symptoms.
A champion heavy-weight boxer, 29, was unconscious for two days after being knocked over by the explosion of a shell in December, 1914. He found at first that he could not move the right arm or left leg; and after power had returned to the limbs, he had forcible involuntary movements in the left leg whenever he tried to stand. Examined, April 1, 1915, he answered questions slowly and with slow words; the right arm was weak. When the left hand was clenched, an associated movement took place in the right hand, but not vice versa. There was, however, no diminution in the girth of the muscles. The man was unable to localize light tactile stimuli accurately. Movements of the left leg were somewhat weak, the left knee-jerk was slightly brisker than the right; ankle clonus could be obtained on the left side and Babinski second sign (paralyzed leg rising higher than the normal leg in combined flexion of thigh and pelvis). When the man tried to walk, the left leg moved rapidly from side to side round the point of contact of the toes. When the right leg moved forward, the left dragged behind in irregular movement.
Every effort to cure the patient by means of suggestion during hospital care for a month entirely failed. Although the man was easily hypnotizable, he could not be made to move his leg under the deepest hypnosis. The first whiff of ether hypnotized him, so that the method of etherization could not be used in the endeavor to control the leg movements. Over a year later, July, 1916, the patient had greatly improved mentally but was otherwise in precisely the condition that is above described.
Gunshot wound of buttocks with injury to cauda equina: Urinary disturbance; decubitus; anesthesia. Superimposed paraplegia, regarded as functional and cured by psychotherapy.
A German grenadier, October 11, 1914, was wounded in the left buttock by a missile that passed out through the right buttock. Pains in the abdomen and legs followed. The man had to be catheterized on the battle-field.
October 23, he suddenly fell down with total paralysis of both legs.
November 3, numerous small furuncles appeared on the buttocks, and bedsores developed. The patient lay helpless in bed, was unable to sit up without support, or to turn from one side to the other, and had areas of anesthesia.
During November and December, there was persistent high temperature, between 38 and 40; but January 3 the temperature stood at 36.6.
January 7 the patient was admitted to a nerve hospital. At this time he was able to pass urine unaided, though with tenesmus and pain, sometimes nausea and a tendency to vomit. He complained of pain in the back and pelvic region; the legs lay as if paralyzed. No active movement whatever was performed. There was a marked increase of tendon reflexes (even including the semi-membranosus). The muscles were relaxed through disuse but there was no atrophy. The patient moved his legs about with his hands. Sensibility was preserved except in the region of the pubis. The plantar reflexes were absent. Electrical reactions normal.
The diagnosis was functional paralysis of the legs (previous gunshot injury of cauda equina).
Treatment with psychotherapy met with prompt results; within a few days, the patient learned to move his legs and to walk with support, though making enormous efforts which threw the pulse up to about 160 and made the face congested. The bladder disturbance and the sacral anesthesia persisted.
Spinal concussion with spinal cord lesion: Thermanesthesia and analgesia of right leg and side.
An officer was hit in the back by a shrapnel fragment, fell paralyzed, but after a few minutes was able to walk more than a mile to the dressing station. Eventually arriving in London, he had nothing to complain of except the wound, as the foreign body had been removed in France. The wound healed and the patient went to a convalescent home.
However, when taking a bath he could not feel the temperature of the water with the right leg. Muscular power was perfect; reflexes normal; but the heat, cold and pain sense was lacking in the right leg and the right side of the body from the seventh costal cartilage downwards.
One may make a wrong diagnosis of “Shell-shock.”
In August, 1915, an officer was blown many yards by a shell, lay unconscious a while, could find no bruises, and carried on for twenty-four hours. Then, finding legs unreliable, he reported sick and was sent home as “Shell-shock.” He remained “Shell-shock” until February, 1916, then being able to walk five or six miles on smooth ground. Going downstairs he took the step with left foot rather than with right, and the right was apt to turn in. The sense of position and movement in regard to the right foot proved to be faulty. He could not balance himself on the right foot, nor could he appreciate tuning fork vibrations as well on this foot as on the other.
An X-ray examination showed a slight fracture, without deformity, in the left post-Rolandic region near the median line. His helmet had been bashed in at this point, and the bruised brain yielded symptoms even eight months later.
Retention of urine after shell-shock.
An infantryman underwent shell-shock December 19, 1915, from the explosion of a torpedo nearby. He arrived at the ambulance, unable to speak, and next day had a confusional crisis of convulsions with contractures. He had not urinated since the accident, and two liters of clear urine were withdrawn by catheter; after which, the patient rested quietly and gradually regained consciousness. He was catheterized again in the evening and clear urine withdrawn. He remained unable to urinate spontaneously until December 25, and was catheterized accordingly.
There was no motor, sensory, or reflex disorder in this patient. Lumbar puncture yielded a normal fluid; the pupils were normal, and the only appearance was that of a marked asthenia.
Three months after his shell-shock, in March, 1916, the soldier was once more examined and still complained of headache, weakness, and inability to walk more than four or five hundred meters without a certain trembling of the legs. The reflexes remained normal and no further bladder trouble had supervened.
Re anuria, Babinski remarks that, in days of yore, hysteria was supposed to be able to produce anuria as well as albuminuria, and even such organic changes as vesicles of the skin, ulceration, hemorrhages in the skin or of the viscera, fever, and even gangrene. He remarks that of late years no single identifiable case of this sort proved to be hysterical, has been reported. This is aside, of course, from such superficial and quickly passing vasomotor disorders as erythema and dermatographia. Anuria and albuminuria have consequently passed from the textbooks on hysteria, just as Babinski believes that hysterical edema and hysterical exaggeration of the reflexes are bound to pass. Hysteria cannot imitate everything; it cannot reproduce the characteristic phenomena of organic paralysis.
Retention of urine after shell-shock.
An infantryman, 27, underwent shell-shock August 16, 1916, at four o’clock, from the nearby explosion of a big shell. He lost consciousness for a period of ten minutes, was sent to the regimental aid post, and twelve hours later brought to a hospital center, in a state of profound muscular weakness. He could not walk although he could make every movement of the legs. There was a marked diffuse cutaneous hyperesthesia. The reflexes were normal; the pupils were unequal, the right myotic. The lumbar puncture yielded a clear fluid under normal pressure, but with an excess of albumin. For three days, retention of urine was absolute, requiring the catheter. There was neither sugar nor albumin in the urine withdrawn. On the fourth day he was able to urinate spontaneously; the asthenia and other symptoms had disappeared in two or three weeks.
Incontinence of urine after shell-shock and burial.
An infantryman was subject to shell explosion and burial May 10, 1917. He lost consciousness for a few hours and spat blood for two days. He was carried to an evacuation hospital and thence to the neurological center at Amiens. Incontinence day and night lasted from the period of shock up to May 29, when the patient was transferred again, to another hospital. The man had never, either in childhood or adult life, had incontinence. He showed a slight tendency to latero-pulsion toward the left. Puncture fluid normal.
Guillain and Barré report but 12 cases of sphincter disorder following shell-shock without external wound among hundreds of cases, and among 12 instances of sphincter disorder there were but three of incontinence, of which the above is one example. Incontinence lasted longer in these cases than retention. Guillain and Barré are unable to assign a cause for the findings.
Struck in back by shell splinter: Crural monoplegia; absence of plantar reflex.
An infantryman, 20, was struck by a shell fragment in the small of the back while lying in the firing position, about 2 P.M. August 22, 1914, at Eth in Belgium. He felt as if he had been struck by the butt of a gun in the lumbar region. He was unable to get back with his comrades. His sack had been cut. He was without ammunition, and getting to a bridge he was able to jump a distance of about 8 meters. He fell and fainted. On coming to himself, his left side felt bad and he could not move his left leg. He dragged himself to the relief post which was being bombarded just as he arrived, and he got a bullet in the left frontal region.
He was evacuated to another ambulance and decided to go back to France. Supported by his Lieutenant, he walked all night making about 35 kilometers on foot. He arrived at Charancy and got by train to Mont-Midi. On alighting, he could not walk. He said he was bent in two, and shuffled on in this position.
The “bent-back” lasted about a month, when he began to stand up again. He passed through various hospitals and was evacuated to the Salpêtrière. He then walked with the left leg in extension on the thigh and the foot in external rotation. He was hardly able to stand on either foot, and especially fell if he tried to stand on the left foot. He made no resistance to passive movements of the left lower extremity. The reflexes were normal except that the left plantar reflex was abolished. On the right, the plantar reflex was normal, and an attempt to elicit this reflex was followed by strong defensive movements. There was a tactile, thermic, and pain anesthesia of the foot and leg as far up as the lower third of the thigh. Above this anesthesia, there was a zone of hypesthesia. Position sense was also abolished in this region, and there was a bony hypesthesia likewise. A slight muscular atrophy (2 cm.) affected the lower leg and thigh.
There were no hereditary or acquired features of importance in the case except that there had been at 14 a chorea for a year. In particular this man appears not to have been an emotional person.
The point in the case is the abolition of the plantar reflex on the left side, in association with a functional paraplegia and hemianesthesia.
Re plantar reflex modification in hysteria, Babinski believes that the same law which holds that hysteria is not in line to alter either the tendon reflexes or the pupil reflexes, is true for the skin reflexes. Dejerine brought forward three cases which appeared to him, however, to demonstrate absolutely that functional anesthesia might abolish or greatly diminish the skin reactions of the sole of the foot, that is, the plantar reflexes and movements of defense. Case 385 was alleged in support of Dejerine, as also were cases of Jeanselme and Huet, and of Sollier. Babinski’s critique of Dejerine’s cases ran to the effect that two of them showed contractures, and accordingly were not pure cases in which to demonstrate plantar reflexes or movements of defense. In the third case, Babinski at a meeting of the Neurological Society, himself obtained definite flexion of the little toes by stimulating the planta. According to Babinski, therefore, Dejerine’s cases, far from proving that hysterical anesthesia could abolish the plantar cutaneous reflexes, proved that hysterical contracture might mask reflex movements. Hysterical contracture, therefore, may be as important a factor to consider re reflexes as voluntary muscular contracture itself. As Babinski pointed out, many normal persons can keep the leg immobile when the sole is stimulated. Moreover, Babinski pointed out, many cases regarded as hysterical were actually cases of a physiopathic or reflex nature which had actually undergone trauma. It will be noted that the above case of Paulian is just such a case of trauma.
Shell-shock; unconsciousness: Crural monoplegia; sciatica (neural changes).
A reserve lieutenant, September, 1914, was blown up by a shell and lost consciousness for an hour. On coming to, he felt pains in the loins, right thigh, knee and heel, and found himself unable to move the right leg at all. Urinary incontinence lasted three or four days. Violent pains lasted weeks, now and then actual crises (sleep only with hypnotics).
The pains then passed off. The flaccid crural monoplegia lasted. There was a hydrarthrosis of the right knee and a sciatica (physical nerve changes?) and a crural monoplegia without trophic, electrical, reflex or vesico-rectal trouble. Lumbar puncture showed no lymphocytes or excess of albumin. It would, of course, be difficult to tell whether this case was hysteria or simulation.
Re hysterical monoplegia, Babinski inquires whether a hysterical monoplegia can automatically appear as a result of emotion without any intellectual element whatever. Emotion produces sweat, diarrhea or erythema, without any intellectual intermediate. Can emotion—that is, emotional shock—produce a monoplegia in the same way as it produces an erythema? The narratives of patients might indicate that emotion can do such things. But according to Babinski there is no genuine case of monoplegia or paraplegia directly produced by emotional shock. One must be careful in this discussion not to confuse emotional shock and emotion of a gradual nature. Babinski wishes to define emotion as a violent affective change as a result of a sudden mental shock upsetting physiologic or psychic balance during a usually brief period. As for the more gradual affective states or emotions, there is obviously so much of the imaginative and intellectual compounded therewith, that plenty of opportunity exists for the production by suggestion of such phenomena as monoplegia, paraplegia, hemi-anesthesia.
Re sciatica, see remarks above under Case 329.
Functional paraplegia and internal popliteal neuritis.
A Zouave was taken out from under a trench shelter beam, the night of December 21, 1914, at Tracy-le-Mont. The beam had fallen upon eight men, killing one, and striking the Zouave in the hypogastrium. He was pulled out two hours later, unable to take a step. He was evacuated on his back, to Paris; stayed a month in the hospital at Croix-Rouge, bedfast. According to the patient, he was entirely anesthetic in the legs. He went to Villejuif, January 22, with the diagnosis of spinal contusion and hemiplegia. He could then walk on crutches, leaning on the left leg. He felt a sharp pain at the level of the spinous process of the first lumbar vertebra and all along the sacrum. Spontaneous movements of the left leg were possible, but they were slow and weak. The hypesthesia rose to the navel. There was a suggestion of a cauda syndrome. The knee-jerks were normal, but on the left side the Achilles jerk was absent. There was a partial R. D. in the posterior muscles of the left leg.
The diagnosis was functional paraplegia plus left internal popliteal neuritis. The crutches were removed, he was isolated, and given motor reëducation. In a week he was able to walk alone with ease.
Re popliteal nerve lesions, Athanassio-Benisty remarks that the external popliteal nerve of the leg resembles pathologically the musculospiral nerve of the arm, whereas the internal popliteal behaves like the median. The musculospiral nerve of the arm shows very variable and usually slight sensory changes. The median nerve more than any other nerve in the arm yields painful sensations during its recovery from section.
Re differentiation of peripheral neuritis and hysterical paralysis, Babinski gives as signs peculiar to neuritis, and never found in hysterical paralysis, the following: (a) diminution or loss of bone and tendon reflexes; (b) muscular[541] atrophy (except for slight amyotrophy exceptionally found in hysteria); (c) the reaction of degeneration (only of value after eight or ten days); (d) hypotonus; (e) distribution characteristic of peripheral motor sensory and trophic disorder.
Re diagnosis of organic paraplegia as against hysterical paraplegia, the latter is to be recognized chiefly by the absence of the organic signs, as (a) alteration of tendon reflexes, (b) the Babinski sign (toe phenomenon), (c) exaggeration of defense reflexes (dorsal flexion of foot on sharp pinching of dorsum of foot or leg), (d) muscular atrophy with R. D., (e) sphincter disorder, (f) skin changes, such as decubitus.
Bullet in hip: Local “stupor” of leg.
A Moroccan sharpshooter, 20, was wounded September 27, at Soissons. One bullet scratched the left thigh. A second entered below the anterosuperior iliac spine at least 6 cm. outside the femoral artery and emerged above the ischiotrochanteric line, 2 cm. above and 4 cm. behind the upper extremity of the great trochanter, thus passing through the tensor of the fascia lata and without breaking a bone.
There was a complete paralysis of the left leg. The man had to walk with a crutch and a cane, dragging the leg like a weight. There was no active or passive movement of thigh, lower leg and foot muscles, except that there was a slight tendency to abduction of the toes, from innervation of the dorsal interossei of the foot. The iliopsoas was also involved, as well as the gluteal and pelvic trochanteric muscles. There was a certain amount of muscular tone preserved, so that the bony elements of the skeleton were held together. The foot did not fall and the leg did not elongate, as it might have in a case of paralysis of the sciatic nerve. Electro-diagnosis showed an early reaction of degeneration according to one examiner, but Sebileau believes that there was no R. D. There was anesthesia of a large part of the leg, which stretched over the anterior and internal aspects of the thigh, covered the entire territory of obturator and crural nerves but did not stretch above the fold of the groin. The region of the femorocutaneous nerve was slightly sensitive and the posterior aspect of the thigh and buttock was sensitive. There was a slight sensation on the external aspect of the lower leg. Foot and toes were entirely insensitive. The anesthesia was for all forms of common sensation. No vasomotor, thermic or trophic disorder. The reflexes were all abolished, except for a tendency to cremasteric reflex. It is clear that these conditions cannot be simulated. Possibly they are hysteric and to be explained on the basis of a kind of autosuggestion or perhaps, according to Sebileau, the local and nervous[543] apparatus under the mechanical and caloric effects of the fragment had undergone a sort of local stupor. No large nerve could have been affected by the injury, according to the analysis made by Sebileau.
Re stupor, see Case 253 of Tinel. Re such local “stupor” it may be noted that this case was published in 1914, before Babinski’s larger publications on reflex disorders. As for the loss of cutaneous reflexes, Babinski remarks that immersion in hot water may cause the cutaneous reflexes in the so-called physiopathic cases to reappear for a time. He regards the loss of cutaneous reflexes in the physiopathic cases as due to a circulatory disturbance, and recalls the fact that compression by an Esmarch bandage can cause the tendon reflexes to vanish for a time, and can even cause pathologically excessive reflexes to disappear. The cutaneous reflexes have also been caused to disappear by compression.
According to Babinski, Sebileau’s explanation that such matters as loss of reflexes could be explained by autosuggestion is erroneous.
Re muscular hypertonus in reflex cases, Babinski remarks that though it may be very pronounced, it is as a rule restricted in area. Re sensory disorders in reflex cases, pains are found (they were very slight ones in the present case); hypesthesia has also been found by Babinski.
Localized catalepsy: Hysterotraumatic.
An invalided soldier had been suffering for a year with marked atrophies and the right knee in extension. There had been a bullet wound of the upper third of the tibia, which did not affect the joint. There was a total anesthesia, both superficial and deep, which stopped sharply at the upper part of the thigh. At the time of the very first examination, this apparent ankylosis was reduced, to the great stupefaction of the patient. There was, however, a peculiar phenomenon in this subject. There was a localized catalepsy of the limb, which was able to preserve any desired attitude in which it was placed; and this attitude could be indefinitely prolonged, just as in cataleptic hysterics. Here, then, was a case of localized hystero-traumatism precisely imitating the classical hysteria of Charcot except for its localization.
Re hysterotraumatism, Charcot developed ideas concerning trauma and localized hysteria in 1886, thereby overthrowing the ideas of Erichsen concerning the organic nature of “railway spine” and “railway brain” as developed twenty years before. In a case of local trauma such as the bullet-wound of Case 388, Babinski’s explanation would be that the pain and inhibition of movement resulting from the bullet wound at the time of injury, formed the focus of a process of autosuggestion. According to Babinski’s figure, the organic factor acts as a bait for the hysterical symptoms. According to the Salpêtrière experience, hysteria is incapable of producing a real superficial and deep anesthesia such as is mentioned for this case. For example, no hysterical patient in the Charcot clinic, according to Sicard, could undergo a scalpel operation without some general or local anesthetic. When, therefore, a true deep anesthesia occurs, Sicard’s conception would be that the anesthesia is not a truly hysterical one but belongs to the group of physiopathic phenomena.
Contracture: Hysterotraumatic.
A sailor, 41, got hygroma of the right knee in 1915, was operated on in July, returned to his dépôt a month later, and thence to Vizille Urage by reason of contracture in extension of the right leg. It was thought he was simulating (since there was no muscular atrophy), and he was sent to the neurological center, where under anesthesia the joint was found free. This man developed, when the knee was bent, extraordinary cracklings in the joint, and he showed pain unequivocally, making a defensive movement, partly reflex, partly voluntary, when the leg was flexed beyond a certain point. There was 3.5 cm. atrophy in the thigh, a reflex atrophy due to the joint disorder. There were no other signs of hysterotraumatic contracture.
According to Sollier, the diagnosis of hysterotraumatic contractures depends upon: first, a characteristic special attitude of the contractured limb; secondly, the participation of the antagonists as a group (global); thirdly, the superposition of sensory disorder upon motor disorder (Charcot’s law); fourthly, the segmentary topography of sensory disorder; fifthly, the extension of the contractured joint; sixthly, the persistence of the contracture in the same form, whether at rest or in attempted movements; seventhly, muscular rigidity; eighthly, normal tendon reflexes; ninthly, normal electrical reactions (though R. D. is hard to determine in muscles contracted to the maximum); tenthly, special reactions during attempts to reduce, such as pains, and equal and regular resistance to changed attitude, pseudoclonus in cases of foot contracture; eleventhly, immediate reproduction of the contracture after reduction under chloroform; twelfthly, co-existence of various hysterical stigmata.
Crural monoplegia, tetanic. Recovery.
An ensign was wounded by a shell splinter in the right scapular region September 25, 1915. A large hematoma was drawn off and drains inserted. Antitetanic serum was given 24 hours after the trauma. The wound looked well. The patient complained merely of the heaviness of his arm, and after September 27, the temperature fell to normal. Magnesium chloride solution was applied every other day, and progress was so good that evacuation was ordered.
However, October 8, the patient suddenly began to complain of a sharp pain in the right thigh, which next day became intolerable and threw the muscles into a slight contracture, the adductors being extremely stiff. Headache developed in the course of the day, with slight stiffness of neck, exaggeration of reflexes in the right leg, and ankle clonus. Temperature: 37.6 morning, 38.5 evening. The patient was isolated and given chloral.
October 10, paroxysmal crises of pain, more marked stiff neck, and lumbar stiffness appeared, with nervousness, photophobia, and hyperesthesia to noise. The wound seemed to be doing well. Chloral was given.
Slight trismus developed October 11. The tongue became dry and the patient drank little. The condition held and the same treatments were repeated up to October 15, when the temperature fell and the contractures and pains were diminished. The chloral was continued. There were still a few cramps in the neck. October 22, however, the patient was practically well.
We are here dealing with an instance of local tetanus of monoplegic form, developing a fortnight after the wound (there is an early group developing, as a rule, from the fifth to the tenth day, and a group of later development, after the twentieth day; the interval in this case was of intermediate duration). According to Courtois-Suffit and Giroux, the differential diagnosis is not easy, since, besides[547] tetanus, must be considered tetany, spastic monoplegia of cerebral or spinal origin, partial hemiplegia, peripheral neuritis, contractures due to bone, joint, muscle or tendon lesions, strychnine intoxication and hysterical contractures. Three cases out of six described by Routier were fatal.
Re differential diagnosis of tetanic conditions, see Courtois-Suffit and Giroux in the Collection Horizon. The cases as a rule appear in subjects that have had serum treatment, and may occur in subjects in whom no trismus ever develops (the above case showed slight trismus).
The recognition of localized tetanic contracture is based upon (a) the intensity of the contracture, which causes the limb to feel wooden (in one case the foot, leg, and thigh were welded to the pelvis like an iron bar); (b) paroxysmal contractions resembling those of tetanus, confined to one limb, and started by a variety of external causes, forming the principal symptom in the disease; (c) contracture of comparatively brief duration (hardly ever over two or three weeks). A slight fever may help in the differential diagnosis.
Wound of left leg: Local spasms, later contracture, and painful crises (these associated with suppuration), the whole treated as tetanic.
An infantryman was wounded by shell fragments September 28, 1915, at Virginy and was given a first dressing an hour later and a second at the ambulance, where antitetanic injection was also made. October 3, the patient arrived at Foix, showing a superficial wound of the left frontal region, a penetrating wound of the upper third of the left thigh, and another in the lower third of the left lower leg.
The evening of October 8, the man began to feel pain in the left leg, though the wounds looked well and there was no fever. October 9, sudden involuntary contractions of the left leg developed, and these increased in amplitude if the limb was touched. The other extremities were normal. Temperature 38.2; pulse 102. Restlessness at night.
Next day 10 c.c. of antitetanic serum was administered and more on the 11th, with chloral and isolation; but on the evening of the 11th, with the contractions still completely localized to the left lower extremity, came an extremely painful crisis interfering with sleep and at last requiring morphine. Up to the 15th the antitetanic injections, chloral and morphine were continued, but on the 15th the contractions were replaced in part by a contracture affecting the muscles of the posterior aspect of the thigh. In the meantime, the patient howled with pain, especially in the night. Chloral and morphine were given.
During the next five days the contractures and pains became still more violent, and on the 21st the antitetanic injections were begun once more and kept up through the 26th in 5 c.c. doses.
The patient began to urinate in bed and to be delirious. The contractions now disappeared, but the contracture persisted. Antitetanic serum was given every other day from October 28 to November 2; every third day from November[549] 4 to November 19; every fourth day from November 22 to December 3; and every fifth day from December 3 to December 17. The chloral was diminished from 15 to 5 grams per diem and by the 20th of December all administration of chloral had ceased. The morphine was given up December 25.
The tetanic symptoms of the left leg now gradually diminished. The leg, which had been flexed at a right angle, began to extend little by little, and the toes, which had been strongly flexed, reassumed their normal position. The wounds suppurated freely during the tetanic crises, but then healed. In January the man could get up and walk, dragging his leg somewhat, and January 20 a complete recovery had been obtained. There was no hysteria in the history of this patient, although the man was subject to “professional” alcoholism, being carter for a wholesale wine dealer, drinking 5 liters of wine a day.
Shell-shock by windage: Hysterical paraplegia, flaccid type, develops 10 days later, after strain, capture, privation, recapture. Paraplegia at first complete. Recovery by suggestion (one séance).
A corporal, 21, told how at Goselmind, during the Sarrebourg retreat, August 20, 1914, a shell burst a meter behind him, flattening his knapsack, throwing him to the ground, blowing him forward (as he said, by the pressure of the air) seven or eight meters, leaving him stunned though conscious for about twenty minutes. Uhlans fell upon him but did not trouble themselves further with him as he could not walk. He crawled along on elbows and knees about a kilometer and a half to some Frenchmen in a wood. He now found himself able to walk a whole day supported by two comrades, making about 12 kilometers. He got by carriage to Gerbéviller, but here fell again into the hands of Germans, who left him nine days in the corner of a barn without care. Gerbéviller was retaken, and he was evacuated to Bayon.
He had now had for some time pains in the kidney region below the point struck, some difficulty in turning his head, and some numbness and jerkings in the legs; and the legs that had carried him 14 kilometers were unable to move at all, even in bed. It was only 8 days later that he could perform the slightest movement, and two months followed before he could go a few steps on crutches. December 14, three months and a half after his accident,—he was demonstrated as “spinal contusion.” Upon examination, however, there were no reflex disorders, no sensory disorders, and the muscular weakness was equal in all parts of the lower extremities and trunk. On crutches, he lunged the trunk forward, painfully dragging his legs one after the other, the right foot in external rotation, never passing the left foot, toes scraping ground,—a functional flaccid paraplegia, completely dissolved by suggestion at a single sitting.
Scalp wound; probably no loss of consciousness: Quadriparesis, later paraplegia; tremors; profound sensory disorders, some apparently hysterical; cataleptic rigidity of (anesthetic) legs on passive movement. Diagnosis?
A soldier, 40, got a scalp wound but probably did not lose consciousness. However, when observed three months after the injury, though fat and well-looking, the patient could not stand or walk, and his hands and arms were feeble. He complained of headache, insomnia and anorexia, and remained in a state of mental inertia. All efforts to read and write produced fatigue. Memory was bad both for remote and for recent events. He was able to feed himself slowly, execute a few movements of arms and hands, and raise his feet from the bed. Upon passive movement, there was a sort of spastic state, which did not amount to a true rigidity. Now and then a clonic spasm was induced by such passive movements. After the repetition of those few voluntary movements which were possible, the muscles passed into a flaccid condition. There was a tremor of a type called swooping; the tremor resembled that of Friedreich’s disease, such as is thought to occur in cases of marked loss of muscular sense. The deep reflexes were exaggerated. Concentric narrowing of the visual fields was easily induced by testing them. There was a general slight dulness of perception on sensory tests. There was astereognosis, and apparently an absolute loss of position sense. Movements of the large joints through an angle of 90 degrees were, however, vaguely recognized. Although the patient could not touch, for example, his left forefinger with his right, yet, if he had once seen the position of a limb and it was not moved, he could remember its position and touch it after some time. His localizing sense was from two to four inches out in the hands, the localization being generally of points proximal to the point tested.
Two months later the patient was somewhat less dull and apathetic. His memory had improved. He was able to read, and he was successfully making a rug; but the legs were worse, having become anesthetic to touch and pain. When the legs were placed in any position, they would assume a cataleptic rigidity, and remain rigidly fixed in any position for some time. The patient could sit up in bed. The muscles were well nourished and the electric reactions were normal.
Re catatonic rigidity, see Case 389 (Sollier).
Shell explosion; pitched in air: Spasmodic contractions of sartorii, persistent in sleep.
A private, 23, was admitted to a casualty clearing station and the next day told the examiner, Major Myers, that the Germans had been sending whizz-bangs and coal-boxes over, and the last he remembered was being on guard and then digging himself out of fallen sandbags. His comrades told him that he had been pitched in the air, but this he did not remember. He remembered running to the shell trench, but finding this “too hot,” he returned to the firing trench, noticing on the way that he could not see well. He lay in the dug-out, flinching at each shell, and “trying to get into the smallest possible corner.” He tried to do guard duty that night, but, when some one noticed involuntary spasmodic movements, he was ordered to go back to the dug-out, was helped to the regimental aid post by two men, and was sent to hospital. He had been in France eight months and had been shaken up somewhat four months before, when bombs threw dirt in his face. At that time, his hands and handwriting had become tremulous, but he had not reported sick. He was depressed and wanted Major Myers to make him well. It seems that he had shrugged his shoulders and made leg movements, diving beneath the bedclothes, and bringing his knees to his chin. When Major Myers examined him, the leg movements were due solely “to strong periodic simultaneous contractions of the two sartorius muscles, the rate of contraction of which varied from 60 to 70 per minute, increasing to 90 during the excitement of examination.” There were special changes of sensibility in the right leg and arm and right side of the face and chest, not involving the abdomen. The patellar reflex was exaggerated; plantar reflexes could not be obtained. The legs were tremulous, especially when the patient lifted them, whereas the hands and tongue were only faintly tremulous.
Under light hypnosis, events in the amnestic period were recalled, and details as to the shell’s direction, process of lifting up, and fall. Under deeper hypnosis, the sartorius contractions diminished but did not disappear. Appropriate suggestion was made, and upon arousal from hypnosis, the movements ceased, the headache disappeared, memory was recovered, and the unilateral disturbances of sensibility had vanished.
As to the possibility of malingering in this case, Major Myers calls attention to the disorders of sensibility which he believes could hardly have been simulated, to the persistence of spasmodic movements during sleep, to their confinement to the sartorii, and to the spastic condition of legs, such that when the thighs were passively raised the knees remained extended.
Re persistence of hysterical phenomena in sleep, Ballet felt that he could prove that some hysterical contractures persisted during sleep, and Sollier has written a special article to the same effect. Ballet’s case had a contracture developing after an operation on the first metacarpal bone. The contracture which followed would be then probably, upon Babinski’s analysis, a reflex contracture and not a hysterical one. Duvernay, Sicard, and Babinski himself have noted the persistence of reflex contractures during sleep, to say nothing of their persistence under an advanced stage of chloroform narcosis. In fact, these reflex contractures are exactly as fixed and persistent as contractures of clearly organic origin. It is probable that Babinski would define Myers’ case (395) as a physiopathic one; yet against this diagnosis would be the disappearance of the movements after hypnosis. As against hysteria, it will be noted that the patellar reflex was exaggerated, and that the plantar reflexes could not be obtained.
Shell-shock: Brown-Séquard syndrome, hematomyelic?
A soldier, 24, went to the front November 12, 1914, and June 1, 1915, had a shell burst near him in the trench, on the occasion of which he felt a violent shock, as if a blow in the kidneys. He felt suddenly paralyzed in both legs. He was crouching at the time of the shell burst. His legs felt dead, and he had such violent pain in the thorax as to make breathing difficult. He was carried to a shelter. After a few hours, the left leg began to move again.
He was carried to the ambulance, remaining there five days, unable to walk, though able to move and turn in bed, slightly constipated, with persistent pains in back. He was then carried to Auxiliary Hospital 231, at Paris, and a bullet (!) was found superficially lodged in the region of the left scapula. Neither patient nor physicians had hitherto observed the bullet, which could have had nothing to do with any spinal lesion.
The pains, in the course of a month, grew less, and at the end of two or three weeks he began to walk and was sent to the psychoneurosis service at Ville-Évrard, July 10. He then complained of pain in the right thorax, especially on movement or after sitting up some time. He could hardly bring himself to the sitting posture from the bed, and found difficulty in raising the right leg therefrom. In walking, the right leg was dragged behind. The reflexes were increased on the right side. There was ankle clonus without Babinski sign. Anesthesia to touch over the whole of the left leg. Anesthesia to pin prick and temperature as far as the umbilicus. Cold was not felt on the left side.
The water of a bath seemed lukewarm on the left side and warm on the right. The left side of the scrotum and the left half of the penis showed the same disorder of sensibility. There was a zone of hypesthesia on the right side of the thorax in the region of the lower ribs. The patient compared his[556] sensations while at rest and without contact to a sensation of painful pressure occurring intermittently, or rather in paroxysms, not advancing beyond the median line of the back. Here was a question of Brown-Séquard syndrome, probably due to a slight hematomyelia, but associated with no external lesion or any injury to the vertebral column.
Re Brown-Séquard’s syndrome, see Athanassio-Benisty with respect to spinal cord symptoms associated with lesions of the brachial plexus. It appears that the combination of spinal cord and brachial plexus injury is not uncommon. Note in this case that a bullet was found in the left scapula region. According to Ballet, this bullet could have had nothing to do with a spinal lesion.
Violence to back: Dysbasia. Antebellum injury.
A man (also injured in 1906 by the fall of a heavy weight on his back) went to France in 1914 as a soldier, and eight months later was hurled into a shell hole so that his back struck the edge. He was rendered unconscious. Upon recovery of consciousness, the right leg was found to be swollen, and there were severe pains in the legs and back.
Upon return home the patient went from one hospital to another, for the most part unable to walk, suffering from agonizing pain in head and eyes. Insomnia and waking dreams.
He was able to bring himself to an upright position and to rush a few steps. He has now acquired considerable control of the feet by the aid of crutches. Insomnia persisted.
Dysbasia: Psychogenic (cerebellar nucleus (?))
On March 9, 1915, a shell wounded a man slightly, and burned off some of the hair of his head. He was unconscious two days, and on waking vomited for a time. Shortly after the injury difficulties in standing and walking set in, with headache, noises in the left ear, difficulty in the intake of ideas, excitability, and poor memory. Then, slight improvement. About the middle of June he was no longer closely confined to bed and could take a few steps with two canes; but the gait was still unsteady and the left leg tended to make abnormal-looking movements. There was nystagmus, rapid, though constant, on looking to the left,—more in the left eye; and nystagmus on looking to the right,—more in the right eye. Adiadochokinesis absent. Vestibular nerve somewhat excitable. Deviation outward in finger-pointing test.
According to Cassirer, this case is one largely of psychogenic origin, with possibly an organic cerebellar nucleus. The knee-jerks absent (even up to March 31). W. R. negative.
Shell-shock; unconsciousness: Dysbasia, in part hysterical, in part organic (?).
A private, 29, was knocked over by a shell explosion December, 1914. He was unconscious two days, found that he could not move either right arm or left leg, got some power back shortly, but, if he tried to stand, experienced involuntary violent movements in the left leg.
April 1, 1915, response to questions was slow and speech slow. The right arm and grip were weak. If the left hand was clenched, there was an associated movement of the right hand; but on clenching the right hand, no associated movement was produced in the left. The musculature was equal on the two sides, and the tendon reflexes of the arms were brisk and equal. Light tactile stimuli were hard to localize. Movements of the left leg were somewhat weak, though the musculature was equal on the two sides. The knee-jerks were brisk, the left slightly brisker. Sometimes a well-marked ankle clonus could be obtained on the left side, but sometimes not. The plantar reflex was constantly flexor. Babinski’s second sign (combined flexion of thigh and pelvis) was well marked on the left side.
On attempts to walk, the left leg would move rapidly from side to side, round the point of contact of toes with ground. When a step forward was taken with the right leg, the left one dragged, and made irregular movements.
This gait seemed obviously hysterical. The patient was kept in hospital for a month. He was very easily hypnotizable, but even in deep hypnosis leg movements could not be controlled when he was told to walk. The first whiff of ether hypnotized but did not cure him.
On the whole, upon review, Hurst believes that there may have been organic brain changes, which (a) the associated movement of the paralyzed hand when the normal hand was contracting, (b) the slightly increased left knee-jerk, (c) tendency to ankle-clonus, and (d) Babinski’s second sign, may show.
Peculiar walking tic.
A soldier was found with a peculiar walking tic. He would rest a good deal longer on the left leg than on the right. He would make a sudden movement of the right leg forward, as if on a spring. At the same time, the man’s head would give a violent movement to the right just as the right leg was receiving the weight of the body. The idea of this movement seemed to be that the center of gravity would be shifted and the work of the right leg would be relieved. This peculiar walk was naturally very slow. If the walk was slowed down, it became quite normal. There was no pain at the basis of this walk. If the man hopped, he hopped no more painfully on the right leg, nor with greater difficulty, than upon the left.
This man was guilty of desertion in the face of the enemy, and of desertion in the interior in time of war. He said he could not walk well and that he needed to take care of himself at his mother’s house, as he was not considered sick in his regiment. He had been wounded with two bullets, September 28, 1914, which struck him on the internal aspects of the knees. He was treated in hospital from October to the end of November, 1914; was held at the dépôt of his regiment from December to August, 1915. He was then put in hospital a month, and returned to his dépôt for three more months. He was examined by three physicians in August, 1915, and the commission decided that he was fit for service, and a simulator.
Thorough examination, including electrical and X-ray examinations, showed no lesion. Chavigny observed the patient for a long time, from the 21st of November, 1916, to January 5, 1917. Shells dropped near the hospital, December 2, and, following orders, the patients were taken into a vaulted cellar, and they ran thither very rapidly; but this patient could not hurry. He walked slowly, with the same tic. Surely the tic would be rather a difficult one to imagine,[560] and a somewhat more probable set of symptoms would ordinarily be chosen. The man has not the unstable nature of the ordinary victim of tic. On the contrary, he has rather the invincible obstinacy of a hysterotraumatic. On being shown that he could walk properly without these “para” movements, he would reply, “I can’t do anything else,” and he shook his head upon being told that he could be cured.
Reëducation of his anesthetic areas (there was a zone of diminution in sensibility to pin-prick in the knee region, and a complete anesthesia of the sole of the foot, with abolition of the plantar reflex), reëducation by appropriate gymnastics, and mental reëducation, might be attempted in a special neurological hospital.
Re disorders of gait, Laignel-Lavastine and Courbon divide functional gait disorders into three groups: (a) A group called dynamogenic; (b) an inhibitory group; and (c) a group showing both forms of disorder.
Roussy and Lhermitte have attempted to divide the gait disorders into two groups: (a) A group termed by them basophobic, in which there is a marked psychogenic and emotional basis; and (b) a dysbasic group, the basis of which is suggestion rather than emotion. Following is a skeleton of their classification:
1. Astasia-abasia and dysbasia group.
2. Stasobasophobia group.
3. Habit limping.
Mine explosion; unconsciousness: Camptocormia. Hospital rounder twenty months (bedfast five months) without complete neurological examination. Cure by persuasive electrotherapy in one hour.
A man became a hospital rounder to all points of the compass in France during a period of twenty months, with such diagnoses as myelopathic disorder, complex spinal trouble, ataxic phenomena.
As a matter of fact he was a camptocormic: trunk bent, knees semi-flexed, legs in external rotation. He used two canes in locomotion, made a bowing movement with each 20 cm. step, then another bowing movement, and another little step with the other foot. Made to lie down, his legs would elongate, the right completely but the left with some difficulty, the feet going into hyperextension, with the big toe raised, others flexed; the feet externally rotating, plantae turned in. In horizontal decubitus, there was only slight lumbar discomfort, but the legs stiffened and gave quick convulsive jerks. Taking the posture several times in succession would diminish these phenomena. Kneeling, he could bring his heels within 10 cm. of the buttock, whereas in spontaneous flexion of the leg on the thigh, the knee remained a distance of 40 cm. from the buttock.
A complete examination showed no joint disorder or any diminution in muscular strength, or any reflex disorder except that all the tendon reflexes were rather powerful. There was a question of possible X-ray demonstration of lesions and ankylosis of the fourth and fifth lumbar vertebrae, and there was a question of some incontinence of urine. On the basis of these phenomena apparently, this camptocormic patient had been saddled with the diagnosis of myelopathic and ataxic disorder for a period of 16 months. A neurologist was at last consulted, and on his advice, it proved possible to get the patient evacuated to a neurological center in a period of[562] four months. Facts of this species are unfortunately still too common, state Marie, Meige and Béhagne, February 1, 1917, despite the remarkable and rapid cures obtained in camptocormia by Souques. In point of fact, no complete neurological examination had been performed upon this man during a period of 20 months.
This particular patient was given to Souques for treatment (Souques and Mégevand). His cure was completed by persuasive electrotherapy, in an hour.
It appears that the man was buried in a mine explosion, June 5, 1915, lost consciousness and came to twenty hours later, able to rise and take a few steps, but bent in two with a sharp dorsolumbar pain. The pain grew more violent and generalized during the next few days, and he began to lose all power in his legs, so that he could walk with the greatest difficulty. He was practically bedfast for five months. He then tried to rise and walk, but suffered so much that he could not get up except in a camptocormic position. It was in fact only January 23, 1917, at the Salpêtrière, that the diagnosis of camptocormia was made. The man complained of pains at the lower dorsal and lumbar regions of the spinal column with slight irradiation sidewise. The following diagnoses had been made:
June 8, 1915. Severe contusion of chest and back.
July 9, 1915. Multiple contusions, commotio spinalis; lesions and ankylosis of the 4th and 5th lumbar vertebrae (X-ray examination).
Sept. 3, 1916. Lumbar intervertebral arthritis with compression of roots.
Nov. 4, 1916. Myelopathic disorder.
Dec. 5, 1916. Old complex spinal disorder.
Souques remarks that these diagnoses show that knowledge about camptocormia has not penetrated into most of the sanitary formations (1917).
Astasia-Abasia.
A soldier was evacuated to the 6th Army neurological center for paraplegia with tremor. He had been in various hospitals for a period of a year. The tendon reflexes of the arms appeared increased; there was a suspicion of patellar clonus and of foot clonus, and it had been proposed to invalid the man for spastic paralysis. In point of fact, the man was suffering from an epileptoid trepidation of the foot and of the patella. When he was lying down, his motor disorders practically passed away, though they had been very marked when he tried to stand upright or to walk. He had much trouble in walking, but could readily stand for some time on one leg.
The man was forthwith treated by persuasive methods. It is important to find out the organic lesion which in all probability served as a starting point for the functional disease, and important to remove or abolish this lesion however minute if a complete and lasting cure is to be obtained.
Re astasia-abasia, writers have remarked that it is one of the commonest hysterical syndromes in the war, though somewhat rare in its complete form. Roussy and Lhermitte state that it usually follows the explosion of a large calibre projectile and has a rapid onset. It is often an isolated phenomenon, without emotional or other Shell-shock complications. The victim has been thrown to the ground and rolled into a trench or hollow. Sometimes the victim gets back to the first-aid post, only to find himself on arrival at the ambulance wholly unable to walk. The legs, however, are drawn along inertly, as in paraplegia, or a pronounced contracture interferes with walking.
Astasia-abasia is classified with hysteria major, hysterical hemiplegia, hysterotraumatic brachial monoplegia, glossolabial hemispasm, hysterical mutism, and rhythmic chorea, as so characteristic that differential diagnosis is superfluous. According to Babinski, no functional spasm and no organic disease can reproduce hysterical astasia-abasia.
Multiple shell wounds, with persistent slight suppuration of thigh: Abdominothoracic contracture, tetanic, four months after original injury.
A soldier, 31, was wounded in the left arm January, 1915, and received 10 c.c. antitetanic serum; was wounded again July 10 in the face, scalp, upper part of the thorax, left arm and left leg by shell fragments, and again received, two days later, 10 c.c. antitetanic serum. July 13, at the ophthalmological center at Rouen the left eye was enucleated on account of a shell wound, and four days later a fragment was removed from a phlegmon of the forearm. Later a number of operations were made for blepharoplasty. The wounds all healed well except for an apparently insignificant, small suppuration of the thigh. November 10, four months after the shell wounds, while apparently in perfect health, the man began to complain of lancinating, intermittent pains in the abdomen, thorax and lumbar region. With these pains was associated a persistent abdominolumbar contracture.
On the suspicion of an abdominal form of local tetanus, chloral was given; but the condition grew worse. The sudden contractions spread from the waist to the feet, from November 20 onward, and were felt by the patient as electric shocks. The arms were not affected. Trouble with breathing supervened on the night of December 3. Sometimes there were respiratory pauses for as long as 15 seconds, followed by a slight polypnea. December 6 the man presented an intense contracture of the lower part of the trunk. The slightly retracted abdominal wall was of marbly hardness, but quite painless. Analgesic muscular rigidity took the place of the former crises of pain. The dorsolumbar contracture was so marked as to make an appreciable hollow in the back. The patient could pick up an object from the ground only by flexing his knees to the maximum, as the trunk could not be flexed. There was a very slight trismus, but he could open his mouth, drink, eat and talk without difficulty. There was[565] no trace of neck stiffness or of Kernig’s sign. The tendon reflexes, normal in the arms, were exaggerated in the lower extremities, especially on the left (wounded) side. The skin reflexes were also more marked on the left side, especially the reflex of the tensor of the fascia lata. There was no longer any evidence of suppuration of the wound of the left thigh, which had been dried up for a fortnight. The pulse was somewhat exaggerated (92) and there was a general hyperidrosis, especially of the face.
Forty c.c. antitetanic serum were given without reaction, and 4 grams of chloral; five days later, 30 c.c. more serum. After ten days the abdomen remained hard, though there was a trifling improvement of the lumbar contracture. There were no longer any spasmodic crises or respiratory disturbances. There was a slight serous exudation from the wound. X-ray showed a small shell fragment 6 cm. below the orifice of the wound.
The third injection was given December 27 to prevent mobilization of the bacilli at operation, and on the 28th, the projectile was removed under local anesthesia from a small, walled-off, old pus pocket, from which were cultivated bacillus perfringens and other organisms.
December 31 a distinct improvement set in and January 13 there was little or no trace of previous disease, except that testing the plantar cutaneous reflex on the left side produced an exaggerated contraction of the tensor of the fascia lata. February 15 he was reëxamined and found quite normal.
This case of tetanus limited to the abdominothoracic muscles (except for a very mild contracture of the masticators) had as its locus of origin, doubtless, a wound of the thigh from which the toxin rose along branches of the lumbar plexus to impregnate the corresponding level of the spinal cord. Although there was no stiffness of the wounded leg, yet there was an exaggeration of the tendon reflexes thereof. The first phase of painful contractures and spasms with respiratory disorder was succeeded by an analgesic phase of characteristically tetanic rigidity. The nonfebrile nature of the disease and the preservation of good general health are worth noting.
Shoulder blade unslung in knock-down by shell splinter: Hysterical (!) paralysis of arm with anesthesia. Recovery by electricity, massage, and reëducation (dislocation remaining).
A soldier was struck September 27, near Berry au Bac, by a shell fragment in the right scapular region and was thrown, according to his story, 15 meters. Upon entrance at Val-de-Grâce, October 13, the shoulder-girdle was found intact. There was a very painful point in the spinous process of the scapula, suggesting a fracture; but the bone was proved intact on X-ray. The scapula was very mobile, as if unslung from the thorax. The arm was paralyzed. On raising the arm the scapula followed its movements and detached itself completely from the thorax, dislocating upwards with lively pain. The fingers could be pushed under the anterior surface of the scapula, and its internal border proved to be entirely free of attachment. Pressure along this internal border was very painful. It seems as if there had been a tearing of the rhomboid and serratus magnus muscles and probably a part of the latissimus dorsi under the influence of the violent shock conveyed by the shell fragment, which had pushed the scapula forward and upward without injuring the skin.
There was also a complete paralysis of sensation. Paralysis of motion was complete except for the extensor longus of the thumb. This motor paralysis had come on progressively three days after the accident. A radicular paralysis from an evulsion of the plexus was suspected.
Babinski, however, made the diagnosis of psychic paralysis, finding the muscles reacting perfectly to percussion. After a few electric tests with the faradic current voluntary movements were obtained in all the muscles of the arm and hand.
Treatment was then continued by electricity, massage and reëducation, so that all movements soon regained strength. The patient can now himself, by raising his arm, still produce his dislocation, which still provokes a lively pain.
Gunshot wound of left forearm: PARALYSIS of the arm gradually INCREASING IN DEGREE and extent and associated with pains and anesthesias.
A reservist sustained, October 2, 1914, a gunshot wound of the left forearm from a distance of about 1400 meters. He fainted, lost much blood, and was treated surgically, October 7, in hospital (at this time no complete paralysis of the arm).
In November, however, an incomplete paralysis at first developed. November 12, the patient was able to flex his thumb but showed some anesthesia.
Transferred to nerve hospital in December, the patient said that at the first change of dressings, October 10, he had not been able to move his arm, and said that pains and paresthesia had existed in the arm ever since the injury. There was still some evidence of suppuration at the exit orifice of the bullet. The left arm was now completely paralyzed and atonic, and hung down in walking, without swinging. The supinator phenomenon, though present on the right side, was absent on the left. The triceps reflex was present. The shoulder acted like a flail joint. On passive elevation of the left arm, the deltoid seemed to contract slightly at first; later it failed to contract. Fibrillary tremor of the left thumb.
Suggestive therapy was unsuccessful. There was an anesthesia of the left arm and the left trunk. The disorder diminished proximally, being most severe in the hand and the arm. The legs were normal. The electrical irritability of the left arm was only slightly diminished. There was a well-marked hypertrichosis of the left forearm, the skin of which was slightly purple and discolored. The patient himself made an attempt to burn his arm with a lighted cigar, to see if he could feel the pain. He showed the scar but had felt nothing. The pectoralis major muscle did not contract. If the left arm was started actively swinging, it kept on swinging inertly. The left hand showed hyperidrosis. The small hand muscles were emaciated but electrically normal.
Glass wound of wrist: Differential glove anesthesias (cold to mid forearm, pain somewhat higher, touch as far as elbow).
A German soldier, 37, wounded his right wrist in the glass of a door. The hand was put up six weeks long with very few changes of the bandage on account of suppuration, and he noticed that the arm was getting weaker and weaker, that he was losing feeling in it, and that it was beginning to sweat a good deal, so that now and then drops of sweat would stream off. The right hand was found markedly congested and 1.5 cm. larger in circumference. The fingers and hand were especially weak. There was a marked tremor of the arm. Electric excitability normal. The sensory disorder was in glove form. Hypesthesia to touch reached the elbow, analgesia to a point three fingers’ breadth below the elbow, and anesthesia to cold to a point two fingers’ breadth still lower, a sort of stepwise dissociation of sensibility resembling what is found in spinal lesions. The case was presented as one of local traumatic hysteria.
Re hysterical anesthesia, the rule is that it obeys no definite rule; that is, it may be a hemianesthesia, a segmentary, an isolated, or even a pseudo-peripheral anesthesia. It is a question whether Babinski would attempt to explain Romner’s case on the basis of medical suggestion, hetero-suggestion, or autosuggestion.
Myers has had a few instances in which anesthesia spread gradually, and in which analgesia increased after its onset.
Re reëducation of cutaneous sensations, Chavigny recommends the faradic current in successive applications, marking the extent of the zone of anesthesia with ink upon the skin. Each time the current is applied, the inked limits of the area are lessened. By this form of suggestion, not only does the anesthesia disappear, but very often the accompanying paralysis also.
Hysterical contracture, edema and vasomotor disorder.
For some unknown reason, a soldier developed a contracture of the right upper and lower extremities at a time when a basin of water was offered to him for toilet purposes. Three days later, this contracture disappeared in the leg but persisted in the arm at the radiocarpal joint and in the finger joints. There was also an anesthesia to touch and pain and temperature which ran up the arm to the shoulder. The tendon reflexes were normal. On the whole, there seemed to be no doubt that the case was one of hysterical arm contracture. Associated with this contracture was a white edema of the hand. On account of the chances of simulation, the hand was done up and sealed in such wise that the seals would have been broken if the splint had been lifted down during the night. The bandage was in place from June 25 to June 29. Upon its removal, there was no edema, but the contracture was still there. The arm was put up upon a cushion so that the hand would drain to the forearm. The edema was found capable of returning when the hand was placed below the level of the shoulder, disappearing when the hand was raised. The contractured hand was warmer than its fellow. According to Ballet, we here have an anesthetic instance of contracture associated with edema and vasomotor disorder.
Re edema, Babinski states that no case of hysterical edema has stood the test of scientific critique. Sometimes a case turns out one of tuberculous synovitis. Sometimes the patient is shown artificially to have brought about the edema. The hysterical “blue edema” of Charcot has not been proved to exist. Some during the war have been found due to voluntary constriction. Some of these constriction edemas even become relatively permanent. Babinski regards the above case of Ballet, as well as cases of Lebar and of Raynaud, as not true cases. Raynaud’s case was probably vascular.
Re vasomotor disorders in Ballet’s case, the Babinski school, of course, holds that hysteria cannot cause such disorders.
Hemiparesis with syringomyelic dissociation of sensations.
A road-laborer, 42, in the 268th Infantry, had a bomb burst about a meter away, March 4, 1915. Three men nearby were killed, and two wounded. The laborer himself was turned over, covered with earth, and stunned. He could hardly get up. He was carried to shelter and found paralyzed on the left side, and unable to speak.
Next day, he was carried to the ambulance, and hemianesthesia was found to exist in addition to the hemiplegia. He could now speak with some difficulty and stammered. Vision and hearing were also impaired on the left side. Reflexes weak; no sign of wound. There was a convulsive crisis of some sort during the day, and afterwards the man complained of a violent headache, whereupon a lumbar puncture showed a clear fluid and a marked excess of albumin by the heat test.
The following day, March 6, the patient had much improved; his hemiplegia was less marked and the arm paralysis had almost entirely disappeared. He still stammered.
Upon the next day, vision and hearing were normal, and the sensation was practically normal. A second lumbar puncture, March 8, showed a diminution in the amount of albumin, although it was still supernormal.
March 9, leg contractured in extension; stammering.
March 12, there was no evidence of disease. March 13, albumin was very slightly increased over the normal in the puncture fluid. March 16, there was a slight trace only of weakness in the left leg. The urine was throughout normal. The patient wrote Bavo April 12, and May 7 he was well but still felt heaviness and pulling sensations.
July 15 it was reported at Tours that he was not yet well, presenting a left-sided hemiparesis, especially in the leg, with a syringomyelic dissociation of sensations, with atrophy of the quadriceps and diminution of reflexes on the left side. The patient had had a hematomyelia (Laignel-Lavastine).
Brachial monoplegia, tetanic.
A soldier sustained a penetrating wound of the back of the thorax on the left side and received an injection of antitetanic serum. A few days later, May 18, 1915, he came on hospital service very sick, with high temperature and marked suppuration. The next day he had an anxious facies, temperature of 40 degrees, and sharp pains in the left arm. This arm May 21 was still very painful and then began to make involuntary movements in the shape of incessant clonic contractions. The forearm would suddenly flex upon the upper arm, and the upper arm itself would violently push itself forward and outward. Meantime, the wrist and fingers were not involved in the contractions. The movements were continuous, but paroxysmally increased in extent.
Babinski, called in consultation, confirmed the diagnosis of an anomalous form of tetanus. Next day trismus, pleurosthotonos, and stiff neck developed. Antitetanic serum and chloral had been given from the beginning, with morphine at night. The patient, however, died with asphyxia June 3.
Re brachial monoplegia, the hysterotraumatic form first observed by Charcot has an anesthesia with the shoulder of mutton distribution, slightly affecting the thorax in front and behind, in addition to the paralysis.
Paralysis of right leg: Hysterical? Organic? “Micro-organic?”
A Lieutenant, aged 28, lost consciousness September 6, 1914, as the result of a shell explosion. When consciousness returned in the hospital, he could not remember what had happened. The last he remembered was that he had been pushing forward with his troop. There had been no psychic shock whatever. Examined September 15, he showed a right-sided hemiplegia with stiffness of the right lower extremity so that it could not be even passively flexed. It was with difficulty he could walk and he dragged his right foot. Patellar reflex could not be elicited on the right. Oppenheim and Babinski were absent. There was a slight nystagmus on looking to the right. Pupils normal. Tongue deviated to the left. Speech was slow and the man had to think a little over some expressions. He could not feel touch so well on the right as on the left and this hypesthesia grew more marked distally. He was greatly bothered because certain words did not come to him readily, especially names.
The absence of the Babinski and Oppenheim reflexes was against an organic hypothesis and the absence of hysterical stigmata and the non-characteristic sensory disorder, as well as the absence of any psychic shock in the history, spoke against hysteria. The hypoglossus paralysis spoke in favor of the organic nature of the disease.
According to von Sarbo we must look for the background of so-called functional nervous disorders, hysteria and neurasthenia, in structural changes of the nervous system, the changes that Charcot called molecular. But the lesions, he believes, do not lead to a degeneration of neurons. Accordingly we get only the external form of organic paralysis without concomitant symptoms, such as Oppenheim and Babinski reflexes. Von Sarbo terms his hypothesis that of “microörganic” changes. To prove the hysterical nature of a condition we must show first that the symptoms have taken their rise on a mental or moral basis.
Shell-shock and momentary burial: Muscular weakness, followed (third day) by complete paralysis (save neck and head). Diagnostic hypotheses.
A big shell burst October 3, 1914, a little over 3 meters from a soldier crouching in a shallow Saint Mihiel trench. The shell made a hole two meters in diameter and 1.5 meters deep, and covered the man with loose earth, from which he was readily released. During the next few days, the man found difficulty in following his comrades on short marches (1 to 4 kilometers). He was unable to buckle on his knapsack. The patient was himself not alarmed at his condition.
Up to the time of his accident, this man, a farmer, had never had any motor trouble, nor was there any nervous disorder in any of his relatives. He had been in several conflicts, August 24-25, September 4-6, in the Argonne and in the Haute Meuse, and he had never found it hard to keep up with his comrades. In fact, once in the Haute Meuse, he took part in an exceedingly difficult and hasty retreat, and only a week before the shell-shock above described he had put in a very long march. Thus a man, perfectly normal before the shock, had fallen into a general state of slight muscular paralysis.
On the third day very suddenly this paralysis became complete. The wounded man, while sitting in the trench, found that he could not stand up either with or without the use of his hands. Now, that very morning he had marched three kilometers from his cantonment to the trench. He was supported on the way to the relief post, hardly 200 meters away, and was then sent to the hospital at Bar-le-Duc. At this time he was so weak that he had to be fed like a child.
For a period of three weeks he lay, unable to rise or sit up. There was one exception to the generalization of the paresis: the movements of the head and neck were normal. A general muscular atrophy set in during the three months, but gradually diminished in amount. The diagnosis of myopathy was made, based upon the evident degree of lumbar wasting,[574] kyphosis, the man’s attitude, gait, manner of rising, galvanotonic contractions.
The history was, of course, rather against the diagnosis of myopathy, as well as the marked atrophy of the hands and the existence of an incomplete R. D. Moreover the fact that he improved may be regarded as rendering the diagnosis of myopathy doubtful.
Other diagnoses, less likely than that of myopathy, may be considered,—hematomyelia, recurrent traumatic poliomyelitis affecting the anterior horns, polyneuritis.
Without making decision as to the nature of this case, Léri proposes the question whether there is a shell-shock myopathy and whether there is a myopathy due to gas or to hemorrhage?
Shell-shock: Right hemiplegia with contracture and mutism. Cure by isolation and suggestion. Question of the relation between plantar areflexia and (a) anesthesia (hysterical) or (b) contracture.
A territorial infantryman, 36, of a nervous and impressionable temperament (father alcoholic), was blown up by a bomb October 3, 1914, between Bapaume and Arras. He was evacuated forthwith to the relief post. According to his own story, he spat blood, could not talk, and felt his right side weak. He was three weeks at a hospital in Paimpol, with the diagnosis of right hemiplegia with contracture and mutism. At Guingamp, an electrical treatment was followed by a gradual disappearance of the arm contracture.
Examined by Dejerine, January 2, 1915, he was found to be a tall, stalwart man with right leg contractured in extension, foot in equinovarus, heel raised. He walked, dragging the leg, which trembled; the trembling then extended to the rest of the body. In dorsal decubitus, the leg lay in adduction and internal rotation. He could lift the leg only 5 cm. above the bed, could only slightly flex leg on thigh, and could not at all flex thigh on hip. The leg could not be bent at all if he was requested to hold it stiff. Ankle joint movements were impossible from contracture. The equinovarus was in contracture which could not be corrected. Right hip movements were limited and painful. Muscular atrophy absent.
Whereas on the left side plantar stimulation produced not only the normal flexor reflex but also the classical defense movements of flexion of leg on thigh and thigh on hip,—on the right side neither a needle nor a match, nor any other form of stimulation of the sole, produced any kind of reaction on the part of the toes, the fascia lata, or any leg muscles. Tested every day for some weeks, the result was always the same. The cremasteric reflex was weak on the affected side. Abolition of the plantar reflex and of the defense movements[576] on the right side was associated with an anesthesia and a hypesthesia of the right side of the body, involving complete anesthesia below the knee and hypesthesia of superficial and deep sensation above the knee. The buccal and lingual mucous membranes were also hypesthetic. The bony sensibility was lost in the foot and lower leg, and was diminished in all of the bones of the right side of the body. There was no contraction of the visual fields. The right corneal reflex was diminished. There were no other sensory defects.
The man was also aphonic, being unable to utter a word or a sound except a jerky whistling sound like the letting off of steam. He was able to write out his history intelligently. He was very emotional, wept, and trembled all over when talking of wife and children. The spinal puncture fluid was in all respects normal. A laryngoscopic examination showed that the vocal cords were functioning normally. The long a could be pronounced distinctly, at the expense of great effort so that the larynx would finally be blocked. The laryngeal reflex was abolished. The laryngeal mucosa could be touched with a probe without producing the slightest pain or coughing reflex. By way of treatment, this case of hysterotraumatism was given isolation and psychotherapy for two months without effect. But about the middle of March he began to get better, the symptoms rapidly faded, cure was effected at the end of March, and the man was evacuated to his dépôt.
Re reflexes and contracture, see the views of Babinski reproduced under Case 385 of Paulian.
Shell-shock: Tic VERSUS spasm.
A soldier was bowled over in a trench by a big shell that burst nearby. He lost consciousness and was carried to the ambulance. But he came to, and was so absolutely well with a few hours’ rest that he took part in a lively attack shortly thereafter and got a wound in the left arm, affecting slightly the ulnar nerve. He was sent to the Salpêtrière for this ulnar nerve affection, when certain movements of his scalp were incidentally noted.
The scalp movements were quick, affecting the fronto-occipitalis muscles as well as the auricular muscles. The displacement was from behind forward, and then from before backward, with slight oscillations of the ear; and at the same time, the forehead wrinkled or became smooth. The movement was involuntary and more convulsive than the somewhat similar movements that many persons can execute with scalp and ears. The phenomenon appeared after the shock for the first time. He had not noticed it himself but the physician at the ambulance had called his attention to it. The soldier was not disturbed by the matter, either at that time or later.
The diagnostician would consider, on the one hand, tic, and on the other, spasm. According to Meige, the man was a victim of tic. No case of such limited spasm appears to have been observed previously. However, the sudden development of these movements without previous history of tic renders the diagnosis somewhat doubtful. There was also a complete anesthesia to pin-prick in the present case over the whole right side of the scalp, face, and neck, even passing below to involve the chest, shoulder, back, and upper part of the right arm, with hypesthesia decreasing toward the nipple and the elbow. The soldier was quite ignorant of this sensory disorder and had never before been examined for sensations. The examination was made with due precautions to avoid suggestion. The question of anastomosis[578] between the facial nerve and the auriculo-temporal branch of the trigeminus and the auricular branch of the cervical plexus, and of their relations to the anesthesia and tic of this case, is raised.
Re pathological movements such as tremors, tics, and choreiform movements, Roussy and Lhermitte divide the tremors (see also under Case 337) into typical and atypical.
The atypical ones are either limited, or more usually generalized when they are merely parts of the Shell-shock syndrome. Sometimes the tremors are paroxysmal, aggravated by noises. Now and then, a condition of tremophobia appears (see Case 225). As for the typical tremors, see classifications under Case 337.
Re tics, the tonic or postural tic is, according to Roussy and Lhermitte, much less common than clonic or spasmodic movements, which are Shell-shock phenomena like tremors and usually yield to psychotherapy if treated early. These tics are usually observed in and about the head, involving the sternomastoid, trapezius, and platysma muscles to produce clonic contractions of the neck. Other tics involve coarser head movements, nodding, eyelid and facial spasms, bilateral or unilateral, and shoulder movements. Babinski has suggested that some of the tremors are possibly due to organic disease, in view of the fact that they are not readily influenced by psychotherapy. Meige has suggested that some of the tics may also be in some sense organic. As for the differential diagnosis of tremor and tic, according to Roussy and Lhermitte, the Shell-shock onset may be an indicator. The non-rhythmic and irregular nature of the tic movements, and their exaggeration on voluntary movement, may be of some importance. Most of the tremors appear to be attended by a certain degree of permanent contraction of the muscle groups concerned. Tremors cease when these contractions disappear.
A point in treatment is that complete muscular relaxation should be obtained by having the patient open his mouth and breathe deeply.
Re diagnosis of neurasthenia in this case, it may be inquired whether the term is properly used, and whether[579] there is not some confusion here betwixt neurasthenia and hysteria.
Re hyperalgesia, Myers states that about 25 per cent of his Shell-shock cases have shown a variety of disorders of the skin sense. Hyperesthesia and over-reaction is one phenomenon in the list, but is far less common than hyperesthesia. According to Myers, the hyperesthesia was more relative than absolute, and was probably due to increased affective response.
Shell-shock; unconsciousness: Tremors, anesthesias. Recovery by suggestion.
August, 1915, between Ypres and Flamentières, a Jack Johnson exploded one day about three o’clock in the morning near an experienced gunner, who had been on service in the R. F. A. for 15 years, and in France during the present war 10 months. He came to in the military hospital at Chatham, two weeks later, and was told he was lucky to be there at all as the shell had killed many comrades. He was transferred to Colchester, and thence to the Fourth London General Hospital.
Sitting in a chair, the man showed continuous rhythmic movements of legs, hands, and jaw, exaggerated when he was spoken to. The tremor was almost a clonic spasm. Every now and then, the patient would start and look sidewise and upwards, as if a shell were about to drop. Hyperacusis was such that the firing of the guns as far off as Woolwich alarmed him. In telling his story, he would repeat the same words over and over. He dreamt of shells bursting. His sleep was disturbed with groaning and moaning. The face was flushed, and the palms sweating. Because of the constant tremor, he could not stand or walk without assistance, and it was difficult to test reflexes. The tremor somewhat resembled the intention tremor of multiple sclerosis. He was unable to feel the prick of the needle on legs, left arm, or hand. He could not feel vibrations of the tuning-fork on feet, legs, or hands, though he could on the forehead. The fork was heard quite well six inches from the ears. There was some difficulty in recognizing colors. Bitter fluids could be tasted, but vinegar, salt, and various fluids, could not be recognized. He could not recognize tincture of assafetida, attar of roses, or oil of cloves, though nitrite of amyl, ammonia and glacial acetic acid were recognized.
Major Mott felt that, though this prolonged severe disease in a long-service man might possibly be related to some organic[581] change in the brain, he might well treat him by suggestion. Major Mott told him that the careful examination just made showed that there was no organic disease, and made it certain that he would recover. In a fortnight, he sat in a chair without tremors and with a profound belief in Major Mott.
Hysteria as appendix to traumata.
A private, 25, something of a liar and of rather a low personality, had enlisted in the regular army in 1911, but deserted to become a football player. He reënlisted, and went to France in September, 1914, enjoying the first six months. He broke his ankles by falling into a deep dug-out, and got frost-bite. After three or four months in England, he found that he did not wish to go back to France. He was two months in barracks, and then went up the line in a good deal of a panic. Soon after, he was wounded in the thigh and was able to remain in hospital a fortnight, exposed, however, to shell-fire and given to starting at noise and occasional war dreams. Sent to his base, he remained jumpy and was now permanently afraid of the line. After three weeks in the trenches, he again got wounds, spent five months in England, came back to France in May, and fought till September, 1916. He tried to convince the medical officer that he had appendicitis and trench fever.
About the middle of September he saw with horror a man crushed by a tank, and thereafter was markedly affected by the sight of blood. Another slight wound sent him to a rest camp for two weeks, whence he was again thrown into the line, suffering acutely from fear and horror of blood. In three days he fractured his left collarbone and wrist. He gave a pint and a half of blood for transfusion purposes, and in turn was shipped to England. On removal of the splint, he found “probably not without satisfaction” that the arm was paralyzed. It remained paralyzed for five months, until treatment in a special hospital eventually cured the arm; but upon cure of the arm, nightmares developed,—an indication, according to MacCurdy, of the strong resistance he felt to the idea of returning to the front.
Neurasthenic hyperalgesia after peripheral nerve injury.
A German volunteer, a sportsman, was under heavy shell fire after the middle of October, 1914, and was wounded in the upper arm in November, with an injury to the median nerve that occasioned severe pain. These strictly localized pains increased upon any sort of physical or mental strain. If he walked down steps he kept thinking he might have an accident, and then the pains set in with greater force. He became apathetic so that he did not eat, drink or urinate. If his head were touched he felt pain as if from an electric shock. He also felt the pain when he saw anybody approaching a door to close it, through apprehension of the noise. Meantime, the wound was well healed. The pulse was accelerated. The visual fields were only slightly contracted. The patient wanted to get well and go back to the service.
Weygandt regards this hyperalgesia after peripheral nerve injuries as neurasthenic.
Military training: Peripheral neuritis in lead workers.
Among fourteen cases of lead poisoning, members of the territorial forces, largely from North Staffordshire, was a patient suffering from peripheral neuritis. He had been in the dipping-house. Two years before going into the service he had been suspended for lead poisoning by the factory surgeon. Giving up his work at the pottery, he became a general laborer in a non-lead process factory.
Three weeks after enlistment, the man began to complain of pains, tenderness in the arms, weakness of the wrists, headache, giddiness, nausea, and constipation. The bowels were opened by a large dose of epsom salts. On blood examination the hemoglobin was found diminished 40 per cent; cells with basophilic granules were found to the number of 500 per cu. mm. The face was characteristically pasty. There was albuminuria. Alcohol could be excluded. The man had to be discharged.
All Shufflebotham’s cases occurred from three to seven weeks after mobilization, nor have any cases ever been reported in territorials after their annual training. Constipation was invariable. In two cases returned to service, there was a recurrent attack. An epidemic could be excluded. Shufflebotham suggests that the altered conditions of life, especially the marching and drilling, caused increased metabolism, setting free lead compounds from the muscles and organs of the body. It is true that a glost placer always works very hard with his muscles, but not with the muscles used by the soldier.
“Peripheral neuritis” cured by faradism.
A Naval Service man, 20, was thought to have peripheral neuritis. A long history of pain and numbness in arms and legs, a well-marked analgesia and anesthesia over the anterior aspects of forearms and legs, and an anesthetic band across the front of the chest, seemed consistent with the diagnosis. The calf muscles tightly squeezed yielded no pain. Pins could be thrust without pain into the anesthetic areas. When told to say yes when the pin was felt, and no when it was not felt, the man persistently said no when the areas noted above were touched. The deep reflexes were normal. Faradism by wire brush at two sittings yielded a complete cure. It seems that once this man, after seeing his sister fall in a fit on returning from a funeral, retired to the garden and had a similar fit himself.
Cargill found in 1052 sailors fifteen cases of total absence of one or both ankle-jerks; seven of the fifteen were probably cases of tabes.
Re peripheral neuritis and hysteria (see under Case 387).
Re differential diagnosis between peripheral neuritis and reflex (physiopathic) paralysis, Babinski and Froment offer the following table:
| Peripheral Neuritis. | Reflex Paralysis and Contracture. |
|---|---|
| 1. Motor disorder, degenerative amyotrophy, and sensory disorder corresponding topographically to anatomical distribution of nerve (neuritic) topography. | 1. More or less segmentary topography. |
| 2. Amyotrophy very pronounced, regardless of localization. | 2. Amyotrophy variable; ordinarily well-marked but not so severe as that of neuritis. |
| 3. Reaction of degeneration, especially weakening or abolition of faradic excitability of muscles. | 3. Reaction of degeneration absent, never marked weakening of faradic excitability, which is often normal and may even be exaggerated. |
| 4. Tendon reflexes, corresponding to the muscular territory of the nerve, weakened or abolished. | 4. If reflexes are altered, they are as a rule exaggerated and never abolished. |
Multiple wounds; signs of late tetanus 7-8 weeks later: Pain and contracture of neck, tetanic, 14 weeks after trauma. Dysentery. Recovery.
A soldier invalided for endocarditis July 8, 1908, went back to the colors on his own request August 8, 1914. He was wounded at noon September 6, 1914, in the attack at Abbaye Woods. He lay in the woods, with several comrades as badly wounded as himself, until September 10, eating berries and drinking rain water. He had five wounds in all; in left lower leg, thigh, left external malleolus, right calf, and left forearm. Moreover, he had dysentery.
He was picked up by the Germans September 10 and carried by them to the ambulance at Saint André, where he was given belated first dressing. When the enemy retreated September 12 he was left behind and finally carried back September 13 into the French lines by a French physician who had been a prisoner likewise. A second dressing was given September 14 at Rambluzin. He was then carried in a sanitary train to Bar-sur-Aube, where, September 15, injection of antitetanic serum was given. He left Bar-sur-Aube on December 18, 1914, practically cured, though one of the wounds still needed care. The dysentery was still present and walking was difficult. He was then cared for at Auxiliary Hospital No. 102 in Paris.
It seems that about six weeks after his entrance in the hospital at Bar-sur-Aube he had had some difficulty in opening his jaws, with acute pains at the temporomaxillary joint. Similar pains appeared a few days later in the neck, with a sensation of stiffening. The jaws still opened easily enough December 18, yet the man got pains in his jaws as soon as he began to speak. The pain and contracture in the neck region were sharp and permanent. Sometimes the contracture got more marked, and the board-like muscles could be felt stiffening under the examining finger. During such crises the patient had to lie or sit down. Sometimes the[587] pains descended below the shoulders along the vertebral column. The crises occurred more often in the night, in bed.
The diagnosis of late tetanus was made, and alcohol rubs were given. The phenomena gradually disappeared. The dysentery also had not yielded to therapeutics until eight or ten days before the patient left the hospital. There was still, at the time of report, a certain difficulty in walking, with a tendency to use the external border of the left foot rather than the sole.
Shell-shock: Spasmodic neurosis and neurasthenia. Treatment without great success.
August 19, 1914, a shell exploded very close to a soldier, whose bread bag, cartridge container, and field flask were pulled away from him, but who was not himself wounded. He fell down. Shortly developed headache, vertigo, palpitation. In running he fell down repeatedly. Spasms soon appeared in the legs. He had previously suffered from gastric disturbances, and heavy food did not agree with him.
At the time of admission to hospital he complained of great irritability, nervous twitching, formication in his limbs, war dreams, tachycardia. The heart boundaries were normal. The muscles of lower extremities were attacked by tonic spasms, and felt board-like. This tonic spasm occurred on each attempt at motion, very gradually disappearing when at rest. Passive movements also had the same effect. Fibrillary tremor affected the left quadriceps. On each attempt at motion, pains were felt in the legs. At first the cramps were so severe that all locomotion or even standing was impossible.
Treatment: Cold-water pack (Priessnitz), hyoscin injections, magnesium sulphate injections (5 to 10 c.c. of ten per cent solution), perineural injections, lumbar spinal analgesia,—all without success. Fibrillary tremors persisted in the quadriceps and in the extensors of the toes. The tonic spasms on increased attempts at motion became combined with clonic twitchings. From the end of November on the patient made attempts to walk with straddling legs, and under considerable vibratory tremor. Picture of severe crampus-neurosis, combined with neurasthenia gravis.
SHELL CONCUSSION
Cause physical from explosives—amnesia for shell episode and for a subsequent period—followed by traumatic neurosis
SHELL HYSTERIA
Shell heard—victims already unstable—rum issue preparatory?—overemotionalism—sensory and motor disorder
SHELL NEURASTHENIA
Headache, dizziness, insomnia, anorexia, visceral pain—victims, older men
After H. P. Wright
(a) Bullet-wound of forearm: Combination of hysterical (brachial) monoplegia, and reflex (physiopathic) disorders. (b) Refrigeration: Combination of hysterical paraplegia and reflex (physiopathic) disorders.
The forearm of a soldier was pierced in its lower part by a bullet, which produced no lesion of large nerve trunks or blood vessels. A complete brachial monoplegia followed. Every movement of the different segments of the arm was abolished. The hand and forearm were slightly atrophied, and were of a reddish salmon color. The temperature of the affected hand and forearm was about three or four degrees lower than that on the other side. The sphygmometric oscillations of the forearm were twice as small in the paralyzed limb as in the healthy limb, but the systolic blood pressure was normal. There was a mechanical over-excitability of the muscles, and a slight exaggeration of the bone and tendon reflexes. The paralysis was in part of reflex (physiopathic) nature. On account however, of the completeness of the monoplegia, and the fact that the reflex paralyses as a rule affect only the distal portion of the limb, the diagnosis of hysteria had to be made in addition to the diagnosis of reflex disorder.
As a result of freezing, this patient had also a complete crural paraplegia. He showed vasomotor disorders and hypothermia of both feet, together with mechanical over-excitability of the muscles; and these latter disorders appeared to be of a reflex nature. The paraplegia, however, was of a hysterical nature.
Re refrigeration, see Case 309 (Binswanger) of glossolabial spasm.
Differential diagnosis of organic (central) monoplegia and reflex (physiopathic) contracture and paralysis. (Babinski-Froment.)
| Organic Monoplegia | Reflex Contracture and Paralysis |
|---|---|
| 1. Paralysis often affects the whole extremity, either arm or leg. | 1. Paralysis almost always partial. In arm paralysis, affects as a rule fingers and hand. The leg is often affected at its origin, and then only partially. |
| 2. After several weeks of flaccid paralysis, as a rule contracture occurs. | 2. Paralysis may remain flaccid for a long time, and frequently coexists with contracture, hypertonicity and hypotonicity of different muscular groups. |
| 3. The upper extremity shows flexion with clawhand. The lower extremity shows contracture of extensors. The patient walks throwing his leg sidewise (Démarche helicopode). | 3. The upper extremity in hypertonic cases often shows the main d’accoucheur, the main en bénitier (holy-water vessel hand), the doigts en tuile (crowded fingers). The lower extremity does not exhibit the sidewise movements. |
| 4. Tendon reflexes, a few weeks after paralysis begins, exaggerated. | 4. Reflex status variable. Hyperreflexia often absent even in hypertonic forms. |
| 5. Babinski sign in crural monoplegia. | 5. Babinski sign absent. The skin reflex may be abolished but may be reproduced on warming the foot. |
Slight bullet wound of hand: Flaccid paralysis with vasomotor and thermic disorder. A case “non-organic” in the ordinary sense and non-hysterical, i.e., reflex or physiopathic.
Struck by his observations upon the persistence of tendon reflexes in narcosis in a wounded soldier, Babinski continued observations in the same general direction in a case which may be termed briefly one of hypotonia of the extensors of the hand following the passage of a bullet through the arm without nerve trunk lesion.
This patient had flaccid paralysis of hand and fingers following wound in second dorsal interosseous space and vasomotor disorder and local hypothermia in the hand. There was a slight diffuse atrophy of the muscles of the hand, forearm, and arm; but this atrophy was not systematized, and there was no R. D. The tendon reflexes of the extremity were preserved. There were no signs of organic disease of the central or peripheral nervous system; that is, in the ordinary sense of these terms.
Was it a question of hysteria or of simulation?
Babinski was struck by the following symptoms:
First, the remarkably intense hypotonia, especially noteworthy in the thumb, a hypotonia quite equal if not superior to that observed in paralysis following marked nerve lesions;
Second, mechanical over-excitability of high degree in the muscles of the hand and forearm, with retardation of the muscular response; and
Third, electric over-excitability of the muscles, with what Babinski calls “anticipated fusion” of the faradic reactions.
It appears that this patient had been wounded in September, 1914, and that the paralysis had developed five months later. Before the development of this paralysis, there had been simply a meiopragic state.
Without perforating the hand, the bullet had remained[593] in the wound, being excised therefrom three months after the trauma.
In January, 1916,—that is, some sixteen months after the injury and eleven months after the recovery of the paralysis,—the vasomotor disorder and the hypothermia, and the faradic, voltaic and mechanical over-excitability of the hand and forearm muscles, were in evidence. Hypotonia was marked, permitting an overflexion of the hand upon the forearm. If the patient moved his forearm, the affected hand would hang and oscillate inertly; likewise in walking, seeming to obey only the laws of physics.
In May, 1916, the patient was invalided and found to be still in possession of the above-mentioned signs. Similar phenomena have been found in the main figée acrocontracture, and main d’accoucheur, and belong, in the opinion of Babinski, to a group which is neither hysterical nor organic in the ordinary sense of the terms. Vasomotor and thermic phenomena are in the foreground of the picture, and are, in fact, practically constant, though they vary somewhat in degree. They react abnormally to the temperature of the surrounding medium; there is undoubtedly a local perturbation of the vasomotor and heat-regulating mechanism. There is also certain evidence of vascular spasm. The vasomotor and thermic disorders run parallel with the mechanical over-excitability of the muscles and the slowness of the response.
Chloroform to demonstrate asymmetry of reflexes.
A soldier, 26, sustained, September 22, 1914, a bullet injury of the right calf. There was no fracture, as X-ray showed, but healing was slow, taking no less than three months. The right knee-jerk was a little stronger and a little sharper than the left, but the difference was controversial; and the difference between the two Achilles reflexes was still more doubtful.
Chloroformed October 10, 1915: As the patient was going to sleep, even before the phase of excitation and motor agitation had passed, the two knee-jerks and left Achilles jerk had disappeared. They grew rapidly less marked before disappearing, and none of the tendon reflexes presented any phase of exaggeration while the patient was going under. At this point anesthesia was arrested. The right Achilles reflex, which had not disappeared, was sharply defined. It was even stronger than in the normal state and polykinetic. During the whole phase of awaking from the chloroform, the right Achilles reflex remained strong and polykinetic, without, however, any ankle clonus. Thus, the difference between the two Achilles reflexes became indisputable; also the right knee-jerk reappeared before the left, and became stronger without any patellar clonus. At this time, the difference between the two knee-jerks was sharp and beyond cavil. This status, in which the knee-jerk and Achilles reflexes were asymmetrical, lasted about ten minutes after anesthesia ceased and lasted a little longer for the knee-jerks than for the Achilles jerks.
Reflexes under chloroform.
A soldier sustained a clean-cut wound of the supero-external aspect of the right thigh without much destruction of tissue or any adherent scar. He showed marked lameness, September 15, 1915, walking with his right leg extended and the foot in external rotation. There was a slight limitation of the movements of the hip joint in respect to internal rotation and flexion of thigh. The right knee-jerk was a little stronger than the left, and this condition persisted several days. After a few tests, the knee-jerk became even slightly polykinetic. The Achilles jerks were normal and equal. There was no epileptoid trepidation of the foot, and no patella clonus. There was a slight hypothermia of right leg, with ill-defined muscular atrophy. Walking caused pain.
Chloroform anesthesia, September 20, 1915, yielded an exaggeration of the knee-jerks with a suggestion of patella clonus even before the phase in anesthesia of motor excitation had set in. As anesthesia proceeded the exaggeration was rapidly lost on the left side but progressively increased on the right. In the phase of complete muscular resolution, when all the other tendon reflexes (such as the knee-jerk, Achilles jerk on the left side, the radial and olecranon reflexes on the left side) were abolished, the patella clonus on the right side was perfectly distinct and could be elicited either by the usual method or by raising the thigh and letting it fall. On percussion of the patella tendon, a strong polykinetic reflex was obtained; right Achilles jerk preserved; right leg in external rotation. Internal rotation could be passively performed better than in the waking state, but this movement was still limited. As the man was waking from anesthesia, when reflexes were reappearing, there was a suggestion of left patella clonus—right clonus as strong as before. At no time any trepidation of the foot. The patella clonus on the right side lasted an hour after waking, at which time all the reflexes returned to their previous state.
Reflexes under chloroform.
A soldier sustained a bullet wound, September 22, 1914, in the right calf. There was no fracture, as X-ray showed. Cicatrization was slow and took at least three months. He was examined October 2, 1915, at the Pitié,—not complaining of pains, but lame. There were no pains, limitation of movement, or joint sounds in the hip joint, and X-ray was negative. There was a slight atrophy of the limb, 1.5 c.m. less in circumference on the right. There was a sharply defined local hypothermia of the right leg up to the knee. The right knee-jerk was a little stronger and brisker than the left, yet it was difficult to be sure of this, and there was a still more doubtful difference between the Achilles reflexes.
The man was anesthetized with chloroform, October 10. As he was going to sleep, before the phase of excitement and agitation had ceased, the two knee-jerks had disappeared. At the same time, the left Achilles jerk vanished, followed by the plantar cutaneous reflexes. Anesthesia was then stopped. The right Achilles jerk, which had not disappeared at any time, remained distinct. It was stronger than in the waking state, and polykinetic. During the waking phase, this reflex remained strong and polykinetic, but there was no epileptoid trepidation of the foot. Accordingly, under chloroform, the difference of the two Achilles reflexes had become very sharp. The right knee-jerk reappeared before the left and became stronger, though without patella clonus. This difference was much more striking than in the waking state. This asymmetry of the patella and Achilles reflexes lasted about 10 minutes after anesthesia was stopped, and lasted a little longer for the patella reflexes than for the Achilles reflexes.
Shrapnel wound above clavicle: Brachial monoplegia, partly hysterical, partly organic.
Babinski speaks of certain symptomatic incompatibilities which emerged in the study of cases of combinations of hysteria, organic nervous disease, and the so-called physiopathic disorders. An example of such an incompatibility might be that of a patient who should, three months after a sudden hemiplegia, show complete or almost complete flaccid paralysis and but slight exaggeration of tendon reflexes—yet the Babinski reflex. Of course, the Babinski reflex would permit a diagnosis of pyramidal tract disease. Yet a sudden intense hemiplegia lasting three months, if it were merely a matter of pyramidal tract disorder, ought to show hyperreflexia of a pronounced degree as well as contracture. An example from the arm is as follows:
A soldier got a shrapnel wound in the left supraclavicular region, and had a complete paralysis of the arm, which had lasted more than a month. Electrical examination showed marked reaction of degeneration in the muscles controlled by the musculo-cutaneous nerve, as well as a diminution of electrical excitability in the muscles innervated by radial branches. On the contrary, in the circumflex territory, ulnar and median, electrical excitability was normal. There were no vasomotor disorders. The diagnosis of an association of hysteria and organic disease was made. Babinski affirmed that electrification would effect a partial cure; and in point of fact, the patient, after having submitted to the current for several minutes, was able to use all the muscles whose faradic contractility was normal or almost normal. Thus, he could raise his arm, flex the thumb, flex the fingers, close the hand, and extend the hand and fingers. Flexion of the forearm on the arm was still difficult, since there was, in fact, a reaction of degeneration in the muscles of the anterior region of the arm. The fact that the movements could be partially executed was dependent upon action of the supinator longus.
Gunshot fracture of upper arm; recovery with motor power in five weeks: Six weeks later, Erb’s palsy (plus). Hypothesis: “Reflex paralysis” preferred.
A reservist, 26, was shot through the middle of the left upper arm, sustaining an oblique fracture of the humerus, August 26. The external wounds healed in a month; the fracture somewhat later. The left arm was at first stiff and motionless, but in five weeks it could again be moved. Pains disappeared with return of motility.
About the middle of November the arm began to lose power to move again, especially the muscles of the upper arm. November 20, the patient showed atrophic paralysis (left deltoid, biceps, brachialis internus, and supinator longus) suggesting at first glance the appearance of an Erb’s palsy; but the triceps and the adductor of the upper arm were also unable to move and there was a slight paresis in the distal muscles of the extremity. There were no pains or other objective disorders.
The diagnosis of subacute poliomyelitis was considered. Electric excitability, however, was found to be normal, both faradically and galvanically.
When patient walked, the left arm swung helpless without sign of innervation or any tonus. Abduction of the shoulder could also not be performed, though a slight flexion of the forearm shortly began to be demonstrable. If the patient inclined his head to the right, extended his hand at the wrist, and flexed the fingers forcibly, he could then flex the forearm somewhat, and a slight tension of the biceps and supinator longus developed. Sometimes fibrillary tremors developed in deltoid and biceps.
Of course a transient peripheral palsy can be produced by pressure of the radial nerve without any change of electrical excitability, but such a change is not associated with atrophy.
Neuritis and poliomyelitis producing an Erb’s palsy without[599] any effect upon the electrical reactions is an hypothesis not to be entertained.
Accordingly, the hypothesis of psychogenic or hysterical palsy may be set up. Yet an atonic atrophic palsy with loss of tendon reflexes (supinator) is inappropriate. According to Oppenheim, this case falls into the category of the arthrogenic atrophies. A simple muscular atrophy may follow disease of joints and bones. However, such cases have rarely shown a complete palsy, as in Oppenheim’s case.
In short, we return to the old doctrine of reflex paralysis, conceiving that a stimulus passing from the periphery influences the gray matter in its trophic functions.
How much effect had the psyche upon this condition? The patient had stuttered from childhood and had sustained a fracture of the skull at 9, following which his school work, especially mental arithmetic, had been poor. The lack of psychic inhibitions may play some part in the situation, but on the whole, the reflex hypothesis is preferred by Oppenheim, the nerve conceived to be dynamically affected, the muscles organically.
Paralysis: Hysterical? organic?
A soldier, 20, was wounded May 15, 1915, by a large number of shell fragments, 15 of which struck the right leg, two producing serious injuries,—the one, a penetrating wound of the popliteal space followed by stiffness of the knee, later cured by extraction of the fragments; the other, causing a deep wound at the internal malleolus. The fragment was extracted June 3, but osteomyelitis persisted and a fistulous contraction was developed in January, 1916. There was a slight equinism.
By contrast with these deep bony lesions of the right leg, on the left side a fragment had struck the dorsum of the left foot at about its middle point, along the extensors of the fourth and fifth toes. The fragment was removed toward the end of June, 1915. The wound closed in a fortnight, leaving a loose 20 mm. scar. The man complained of pains, which he called electrical, in the third and fourth toes, if one bore down on this scar, a symptom suggesting that the dorsal nerves had been injured. Immediately after the wound both legs had been paralyzed, according to the soldier. He had been able only to drag himself along on his shoulders. This indeterminate paralysis lasted three days. It may have been hystero-traumatic, or it may have been a sort of diffuse inhibition. Just after the injury, the left foot was in contracture, which gave place a month later to paralysis. Only the great toe was still able to move a little. In December, 1915, the patient still could extend and flex the toes on the left side very badly, though he could execute movements easily on the right side. There was no stiffness of joints; there were no tendon reflex disorders. There were no trophic vasomotor or secretory disturbances.
The diagnosis of hysterical paresis seemed warranted, but electrical examination showed that the troubles were organic. There was an increase in the faradic and galvanic excitability of the external popliteal nerve. The response was more[601] sudden than normal, and there was an increase in faradic and galvanic excitability in the tibialis anticus. There was a decrease of faradic and galvanic excitability in the extensor communis of the toes and in the external peroneus.
Thus, this patient after being wounded in both feet May 15, 1915, paralyzed in both feet for a period of three days, undergoing a contracture of the left foot for a month, giving place to paralysis of foot and toes, with slow improvement from the end of July, 1915, was still in this latter state in March, 1916; though without trophic disorder, he showed faradic and galvanic over-excitability of the external popliteal nerve and of the tibialis anticus, pari passu with diminished electrical excitability for other muscles.
Paralysis: Hysterical? organic?
A man was wounded Oct. 11, 1914, on the back of the right hand. Two hours later, he was attended at the relief post. At this time, his hand was straight, with fingers extended. He said that he could not move his fingers, although there was no pain in them. Three hours after the wound, the hands swelled and the edema spread as far as the middle of the forearm. There was a long suppuration, complicated by lymphangitis. All of the fragments were removed October 26, 1914; healing was complete in three months. The swelling, however, persisted to June, 1915, and when the swelling disappeared, the hand began to show drop-wrist. The wound was sutured between the second and third metacarpals, and the X-ray showed that the bones had not been injured, nor had the nerves of the forearm muscles been touched. The situation was such that the case was catalogued “functional paralysis.”
October 5, 1915, the hand was still drooping, fingers extended, and middle finger and ring finger trembling. A slight stiffness of wrist and fingers did not interfere with movements. Extension of the wrist could be made very slightly above horizontal. Flexion was not quite complete, nor were adduction or abduction. Extension of the fingers could be performed normally, as well as that of the thumb, but flexion was not quite complete. There was a slight palmar retraction. Such were the movements that could be produced electrically. Voluntarily, flexion of the wrist was good, abduction and adduction incomplete; extension could not be executed to the horizontal position. There was a tendency to flexion of the ring finger. When the patient tried to flex the middle and index fingers, these fingers trembled but did not flex. Weak extension and abduction of the thumb but without opposition could be voluntarily performed; adduction good; flexion of the first phalanx, weak; of second phalanx, better. Slight muscular atrophy of the forearm,[603] which was one centimeter less in circumference than the left. The hand was subject to a general atrophy; the skin reddish and moist. The X-ray showed a decalcification of all the bones of the hand and wrist; trophic disturbance of the small carpal bones although the trauma had affected only the second interosseous space. No joint lesions or periosteal thicknesses were found by X-ray. There was a slight hypesthesia of the palmar surface of the middle finger and of the index finger. The patient complained of sharp transient pains in hand and fingers.
In this case, therefore, a wound of the back of the hand produced an immediate inhibition of muscular action in the forearm, a rapid edema of the hand and arm, lasting for eight months and followed by reflex disorders.
There was a considerable diminution in faradic excitability of the flexor brevis of the thumb, the anterior cubital, the flexor brevis minimi digiti, and of the dorsal interossei, and slighter evidence of diminution of galvanic excitability in some of the muscles.
Sollier is said to have been the first to remark trophic bone disorders in cases of neuropathic contracture.
Re bone changes, Babinski enumerates trophic changes in the tissue of bones and joints amongst objective signs that permit us to distinguish the reflex or physiopathic disorders from the hysterical or pithiatic disorders. Objective signs of this group (indicators of reflex or physiopathic disorders) are: (a) Well-marked and persistent vasomotor and thermic disorder; (b) alterations of muscular tone (either hypotonus, hypertonus, or a combination of the two); (c) increase in the mechanical excitability of the muscles and sometimes nerves; (d) quantitative changes in the electrical excitability of the muscles, but without R. D.; (e) muscular atrophy and atrophy of skin, bones, and joints. For cases of this nature, see especially Cases 431 and 432 of Delherm.
Paralysis: Hysterical? organic?
A man, 22, was wounded September 17, 1914, in the left hand, the bullet passing from the lower part of the fourth interosseous space out through the palmar face. The bones were not injured, and it was evident that only a few nerve filaments could have been injured; but he had a paralysis extending far beyond this region, which increased little by little from November, 1914, to August, 1915. Babinski, examining him in November, 1914, had made the diagnosis of psychic paresis of the extensors with diminution of electric excitability, with a very slight slowing of the contraction of the last two interossei and the hypothenar eminence, connected with lesion of the branches of the ulnar nerve. The disorder spread to the flexors of the fingers and the thumb muscles. The fifth finger was flexed at rest; there was no stiffness of joint or tendon retraction. The extensors and flexors of all the fingers and the thumb, and the abductor of the thumb showed paresis. The thumb was able to oppose; the hands were cyanotic. Augmentation of these phenomena in a period of months, their bizarre distribution, and the preservation of the opposing power of the thumb suggested a hystero-organic disease, and Babinski’s notes read, “Partial and incomplete paralysis of the ulnar nerve, attacking slightly the hypothenar eminence and the last two interossei; psychic paresis of the extensors and flexors of the fingers and thumb and of the abductors of the thumb.” Electrical examination showed, however, that there was not only electrical disorder of the common extensors of the fingers, the extensor proprius of the index and of the ring fingers, of the long and short extensors of the thumb, but also there was a considerable diminution to faradic and galvanic reaction in extensor ossis metacarpi pollicis, the radials, the supinator longus, the pronator teres, the large and small palmar, the common and superficial flexors of the fingers, the muscles of the thenar eminence, the anterior ulnar, and the[605] anterior biceps and brachial. In short, there was an irradiation of seemingly organic phenomena in the domain of the radial, median, and the non-injured part of the cubital distribution, as well as in the distribution of the musculo-cutaneous. Apparently, organic paralytic disorder had spread even to the biceps and had increased over a period of many months after the wound had healed.
Re what he terms organo-hysterical association, Babinski proposes to distinguish it from hystero-organic association. In Babinski’s organo-hysterical association, the organic symptoms are preceded by hysterical symptoms. These cases of organo-hysterical association,—e.g., a case in which a hysterical monoplegia is followed by a musculospiral crutch paralysis,—are one of the mainstays of the proof that hysteria and simulation cannot be confounded. Babinski concedes that he has sometimes said that hysteria was a sort of semi-simulation; yet a semi-simulation is not a simulation.
As for Babinski’s hystero-organic association, we here deal with cases of organic paralysis or contracture in which the fundamental disorder is organic, and the psychic disorder is grafted upon it. Both the fundamentally organic and the fundamentally hysterical associations are instances, according to Babinski’s phrase, of symptomatic incompatibilities. In such instances, the hysterical part of the disorder, whether grafted or original, is dissolved by psychotherapy. There is a third group of symptomatic incompatibilities, namely, the hystero-reflex associations, in which, e.g., a hysterical gait is combined with vasomotor and thermal disturbances. There may even be combinations of all three types of disease, namely, the type of structural disease, of vasomotor disorder, and of hysteria, in what would then be termed a hystero-reflex-organic association.
A soldier was wounded in the soft parts of the last two toes and in the furrow between toes on the left side, September 15, 1914, arriving in the Central Physiotherapeutic Service of the 17th Army Region, December 27, 1915, left foot in varus, with marked contracture of tibialis anticus, though passive movements of flexion, extension, adduction and abduction were well performed. There was a slight atrophy of the leg (33 cm. left to 34 cm. right). The scar was a little painful, and there was a slight degree of hypesthesia of foot and lower leg. The foot was cold and cyanotic; the reflexes were normal. An electric examination in the region of the external popliteal branch of the sciatic nerve showed that there was no electrical disorder either faradic or voltaic.
Another case was wounded in the right arm by a shell fragment September 7, 1914, and showed two scars above the epitrochlea and along the internal border of the triceps. Examination December 30 showed a normal elbow movement, pronation and supination, with slight flexion in repose of the palm of the hand and the fingers. Active flexion movements of the fingers could be performed only imperfectly, and the finger pad could only be brought within three fingers breadths of the palm, despite the greatest effort on the part of the patient. Minute passive movements were entirely possible. The fifth finger could not be abducted and both abduction and adduction of the third and fourth finger could not be made on account of the nerve lesion. The thumb was in a condition of contracture which placed it in abduction in front of the index finger, and the thumb could not oppose. Passive movements, on the other hand, were entirely possible. The hand was flexed upon the forearm through hypertonia of the flexors, which could be easily overcome with slight but distinct resistance. The hand was in the position of a radial paralysis. There was a slight degree[607] of muscular atrophy. Tendon reflexes were normal. Electric examination showed that stimulation of the ulnar nerve at the elbow was unable to produce flexion of the last two fingers or any movement in the hypothenar eminence, of which the muscles were also not excitable. The interossei could, however, be made to contract. The median and radial nerves were normal electrically. The above examinations were with the faradic current.
With the galvanic current the ulnar nerve proved unexcitable at the elbow, and the muscles of the hypothenar eminence contracted more slowly. The median and radial nerves and their muscles were electrically normal.
In short, there was a complete R. D. of the hypothenar and partial R. D. of the interossei as a result of the lesion of the ulnar nerve. There was nothing abnormal in the other nerves or muscles of the arm. The attitude of radial pseudoparalysis is due to the contracture of the muscles of the thenar eminence.
As to therapy, the general movements of flexion of the fingers, thumb and hand yielded a marked improvement, but such results cannot be expected in like cases unless a physician or experienced masseur treats the case. Babinski and Froment have tried thermotherapy and diathermy in these cases, finding that the paralysis diminishes and becomes partial if the limb is warm, although it is important that it should not become too warm. Sometimes a few treatments with diathermy will produce movements in a case of long standing paralysis. Babinski and Froment counsel not only diathermy, but a general motor reëducation. The idea of the diathermy is that the deeply penetrating heat affects blood vessels and muscles, bringing about a vasodilatation or even a direct addition of needed calories. In like manner, galvanism, light baths, or simple baths in combination, and with diathermy, especially with the diathermy, act favorably. Casts and apparatus have also proved without avail, as well as faradic or galvanic reëducation.
The above two cases show how in one instance there may be no electrical change and in another instance a slight one. In these cases, reflex hypertonic contracture, hypotonic paralysis,[608] vasomotor disorder, decalcification of the skeleton (X-ray), mechanical overexcitability of muscles, unmodified tendon reflexes (except elective exaggeration of reflex under anesthesia, e.g., a persistent unilateral patellar clonus when all other reflexes have been abolished), and disorders of electrical excitation are enumerated by Babinski and Froment.
Delherm sums up the electrical disorders as follows: Muscle faradized:
(a) No change.
(b) Subexcitability.
(c) Overexcitability.
(d) Diminished contractility to faradism, associated with increased contractility by galvanism (Charpentier).
(e) Anticipated fusion of shocks (Babinski and Froment).
(f) Slow contraction and decontraction on faradism (Charpentier).
(g) Rapid exhaustion of rhythmic faradic contraction with metronome.
Muscle galvanized:
(a) No change.
(b) Subexcitability.
(c) Overexcitability.
(d) Suddenness of galvanic contraction with subexcitability.
Re decalcification and osteo-articular changes, Babinski points out that the reflex or physiopathic phenomena run historically back to John Hunter, Charcot, and Vulpian. Charcot and Vulpian called especial attention to the peculiar amyotrophy and paralysis which occurred in joint disease, and upon the lack of parallelism betwixt the intensity of the joint disease and the severity of the paralysis or atrophy. The atrophy was without R. D.
Shell-shock: Functional blindness (monosymptomatic).
A shell burst above the head of a sergeant in a battle near Neuf château, August 22, 1914. The man was kneeling at the time; felt a terrible shock, slipped prone, lost consciousness and woke in the evening blind. Next day he could hardly distinguish light from dark. Yet the light reflexes were normal; the fundus was normal.
This Crouzon calls the symptomatic triad for functional nerve blindness of Dieulafoy. There have been similar cases following eclipse of the sun and nervous shock. The eclipse cases suggest that the bright flash might have something to do with the sudden blindness (yet blindness has appeared in cases in which the shell burst behind the patient).
The diagnosis of temporary blindness, with a prognosis of early recovery, was made. The neurological examination was normal.
For its suggestive effect, glycerophosphate injections and progressive reëducative measures were adopted. The patient was shown that he could see, first, the contour of objects, then details and colors, then large letters and later small letters. In a month the blindness was almost well. Five months afterwards there was still a certain haze over the field of vision and a slight difficulty in distinguishing certain colors.
Jousset states that aside from visual alterations as the result of cranial trauma, and aside from various transitory amblyopias such as scintillating scotoma, the main varieties of amblyopia are:
First, Congenital amblyopia.
Second, Amblyopia due to cerebral intoxication.
Third, Retrobulbar neuritis and toxic amblyopia.
Fourth, Amblyopia ex anopsia.
Fifth, Hysterical amblyopia.
The most frequent amblyopias among the soldiers are[610] exanopsia. Aside from a few amblyopias caused by prolonged occlusion of the eyelids, ptosis, or blepharospasm, the most frequent are due to opacities, ametropia, and strabismus. The hysterical amblyopias are, as a rule, associated with blepharospasm due to intense photophobia, and are sometimes associated with constant lacrimation. Vision at a distance is poor. The patient succeeds in reading but shows an asthenopia of fatigue. The cornea and the conjunctiva are anesthetic, and sometimes the eyelids also,—the so-called anesthesia en lunettes. The pupils are large but react properly. The patient complains of many species of disorder; loss of the sense of the third proportion, micropsia, megalopsia, diplopia, erythropsia, diplopia in two colors, inverted image, hemierythropsia, rotatory amblyopia. There is concentrated limitation of visual fields, exaggerated by fatigue and by intense light; reduced in dim light or when the patient is provided with smoked glasses; enlarged upon the instillation of atropin or with convex glasses. As a rule, with unilateral amblyopia, the functional disorders start in binocular vision. Practically the most important diagnostic feature is the anesthesia, since this cannot be readily simulated. Sometimes corneal anesthesia is found in non-hysterical persons, who may perhaps be regarded as potential hysterics.
Retrobulbar neuritis (nitrophenol).
A soldier of the 54th Artillery entered hospital 45, November 4, 1916. He had had a slight paralysis of the left brachial plexus in 1913, following a shoulder dislocation, but the only relic of this when the war began was a deltoid paresis. He had been working from August 13, 1915, at the factory in Saint-Fons, and was as yellow as the majority of the workers there. He had never shown xanthopsia.
The first symptoms of his left brachial plexus neuritis had begun six months before, after 9 months’ work in the factory, and showed themselves in an increase of the deltoid paresis, with pains in the hand and forearm, and cramps of the hand, interfering with work, formication in the right hand and in the feet, diminution of visual peculiarity (objects forgotten and reading difficult). It was only in November that he got perturbed about these difficulties, which had begun in May. There was a paralysis of the levators and rotators of the left shoulder, with a slight atrophy of the deltoid and of the supra- and infraspinatus muscles. The arm could be extended almost to the horizontal with difficulty. There was one centimeter atrophy. The forearm and hand were not atrophic but slightly weak. There was an anesthesia of the shoulder-joint region, and of the outer surface of the arm; a hypesthesia of the posterior surface of the forearm and dorsal surface of the hand and fingers; tendon and periosteal reflexes normal. Sometimes the hand would contract firmly and could be opened only by the aid of the other hand. The nerve trunks of the axilla, upper arm, and forearm, were painful on pressure, especially on the left side, and the ulnar nerve was thickened and rolled under the finger. The knee-jerk and Achilles jerk were abolished on the right; plantar reflex diminished; right posterior tibial nerve painful on pressure, and its territory was hypesthetic. There were cramps in the feet.
Gymnastics and electrotherapy and rest reduced these phenomena. The eye grounds were normal; there was a[612] paresis of accommodation, and an absolute blindness to green, with retraction of fields to 15 degrees in the right eye, and 20 on the left. There later developed a slight edematous neuritis of the nerve, corresponding to the evolution of a chronic retrobulbar neuritis of toxic origin.
It is the chronic retrobulbar neuritis which is typical of the so-called nitrophenol neuritis, developing in soldiers employed in making explosives. The above case is accordingly exceptional in its association of a severe peripheral neuritis with the optic neuritis. Typically, after six months to a year in the factory, the cramps and formication of the legs are felt, and the gradual diminution of vision with transient blindness, finally leading to inability to read, sets in. The green blindness, the accommodative paresis, and diminution of central vision, the concentric contraction of the visual fields, are the usual story. At first the eye grounds are normal; there is then an edematous neuritis, and finally a white atrophy. According to Sollier, the accommodative paresis is like that in post-diphtheritic paralysis—a disease due to cerebral cortex intoxication. In fact, the photomotor reflex is normal, and what we have is an inversion of the Argyll-Robertson sign. These symptoms are those of retrobulbar neuritis, of nicotino-ethylic origin, and it may be thought that the melinite was simply acting by creating a soil for alcoholic intoxication, but none of the patients examined has been alcoholic, nor has any been permitted to smoke in the factory. The injurious agent is probably a body in the nitrophenol series, perhaps dinitrochlorobenzol, but whether this substance is absorbed through the skin, inhaled, ingested from the hands, or by all three routes, is doubtful. These workers are often cyanotic while at work because the nitre products produce vasodilatation. Possibly this dilatation of vessels has something to do with the neuritis. The workmen will not use the spectacles and antitoxic masks given them, and even do not use the rubber gloves constantly. In some factories only, a liter of milk is given as counterpoison, every day.
Slight wound of occiput: Ophthalmoplegia externa, influencible, however, by tests and replaced by spasmodic convergence of globes with myosis; hysterical stigmata and convulsions.
A German volunteer, 20, was slightly wounded in the occiput by revolver-shot at Ypres. Then followed headaches, vertigo, and complaints of pains in the eyes such that he could not open them or see sidewise. May 5, 1915, he showed a picture of an ophthalmoplegia externa: complete immobility of the two bulbi, lively blepharoclonus, rapidly passing into blepharospasm, photophobia. The visual field for white was practically limited to the fixation point. Central scotoma for all colors. Otherwise normal.
On further examination, the apparently immobile bulbi were found to pass into convergence upon request to look to the right or left. Thereafter, this position of convergence was assumed if any test made by a strong light, such as that of a pocket flash, was used. The pupils contracted to the maximum during this assumption of the convergent position of the globes, and no further light reaction could be observed. The convergence gradually passed off when the light was removed. The appearance of bilateral external ophthalmoplegia had disappeared.
If the patient was requested to follow a finger moved to one side, the globe of that side to which the finger was being moved, stood unmoved in its central position, but the other globe followed the eye and placed itself in the convergent position. The patient complained of diplopia. Even after the closure of one eye a double vision appeared (monocular diplopia). There was achromatopsia. The cornea failed to react to stimulation.
There was an analgesia of the skin of the whole body, with a hypesthesia for tactile stimuli on the left side. Smell and taste absent. The convergent position of the globes with myosis was preserved in the midst of convulsive seizures,[614] which could be produced by exciting the patient. When it was attempted to dissolve the eye troubles by hypnosis, convulsive attacks occurred. The patient was pronouncedly hysterical.
The case is beyond question hysterical,—the phenomena consisting of an ophthalmoplegia externa, alternating with spasmodic contracture of the internal recti, associated with myosis and loss of light reaction. The influencibility of this situation during the process of tests, to say nothing of the other stigmata, clinches the diagnosis—an important one, since the development of an external ophthalmoplegia after occipital trauma might possibly be regarded as an organic disease due to hemorrhage in the region of the eye-muscle nuclei.
Sandbag drops on head: Internal strabismus and diplopia. Various diagnoses. Cure by lenses.
A four-pound wet sandbag fell eight feet on the head of a sergeant-major, 28, lying in a Gallipoli dug-out, November 24, 1915. The sergeant-major was removed to Lemnos with headache and giddiness, and a week later developed bilateral internal strabismus with double vision and head noises. The diagnosis was “brain tumor” or “syphilitic meningitis of the base.” On the voyage home, the diagnosis was altered to “multiple neuritis or neurasthenia.”
He was admitted to the King George Hospital, January 1, 1916, unable to move the eyes outwards; they moved rather poorly up and down. There was a slight lateral nystagmus. The patient had been unable to read or stand since the accident. The visual acuity of each eye was less than 6/60, but with an arrangement of lenses he could get 6/5 with either eye. He had perfect binocular vision and could read ordinary type comfortably. In a week’s time he was able to stand without support and walk with a stick. Whenever he took off the glasses, the strabismus and diplopia immediately returned. Other combinations were tried but failed to relieve symptoms. The lenses given were +0.375 c. Vert. and L. +0.25 S. +0.25 C. 75 do.
Hemianopsia: organic or functional?
A 19-year old volunteer, never ill (no nervous disease in the family), after a period of training went into the field, October 3, 1914. November 5, a shell struck the trench nearby but failed to explode. Up to that time everything had been quiet. The soldier had been looking out of the loophole, surveying the terrain. He felt a great fear, got a blow in the neck, fell down unconscious, remained unconscious for an unknown time, and later walked back with his comrades. About an hour later, this volunteer,—who was a very intelligent young man, possessing much knowledge of biology, including the nature of visual fields,—noticed a black spot in the field of vision, which came and went, but after a few hours remained continually without disappearing. Otherwise, there was no complaint except a feeling of dizziness when stooping.
Upon examination there could be found no disorder of the internal organs. Neurologically there was blinking, vasomotor excitability, slight reddening of the face, and dermatographia. An expert in ophthalmology confirmed the existence of a homonymous defect in the fields of vision. This defect could not be influenced by suggestion or by any other treatment, nor did any other change whatever occur in the condition.
Steiner inquires whether this hemianopsia is to be taken as organic or functional. The air-pressure of the shell hissing past might have produced a concussion, or the falling unconscious might have produced a commotio cerebri or a slight hemorrhage. The tic-like blinking and vasomotor excitability, however, suggest functionality.
Hysterical pseudoptosis.
Laignel-Lavastine and Ballet present a case of what they term hysterical pseudoptosis in a patient who showed no signs of organic disease of the nervous system, and moreover no special mental disorder. This soldier, 30 years of age, working in the auxiliary service, suffered from a troublesome lowering of his left upper eyelid. He went to the front in February, 1915. Aside from suffering a few mild and temporary blindnesses (éblouissements), he was entirely well up to the time of being wounded, March 18, 1915, by a bullet in the arm, and a bullet occasioning a superficial and slight wound 2½ centimeters above the middle of the left eyebrow. About three years later, a shell burst near him and made a large contusion about the right eye, without hurting the globus. He was then evacuated to Châlons-sur-Marne, and there remained for 48 hours, totally blind, probably on account of spasmodic closure of his eyelids. He then began to be able to use the left eye, which remained, however, very photophobic. A fortnight later, the wounds were healed, but the patient found himself unable to open his right eye. Three months later he returned to his dépôt, and left for the front October 24.
He was reëvacuated November 4, as unsuitable for service. He was then examined by an ophthalmologist at Chartres, who found a very mobile right pupil and a slightly atrophic right papilla; vision ½; left eye normal; vision ⅔; total paralysis of right levator palpebrae superioris without contracture of orbicularis. There was also paresis of the left upper lid, which ceased when the right eye was closed. The right half of the face was anesthetic, but there was no corneal anesthesia.
November 15: Right eyebrow lower than left; if the head was moved backward, the right eyelid followed the movements, and in this position there was no ptosis.
November 16: Analgesia in the super- and sub-orbicular region. November 17: frontalis and orbicularis functions normal.
At time of examination, patient complained of not being able to open his right eye, and that he could only partly open the left eye. To catch a view of his examiner, he had to throw his head back and to the right. He could not open his eyelids, and in the effort to do so, the forehead muscles contracted; and whereas the left eyebrow was properly elevated, the right eyebrow was only partially elevated. Associated movements could be noted in the musculature of the lower part of the face. In looking to the right, the eyelids, especially the left, were elevated slightly. The patient complained of photophobia. From time to time, he felt completely blind, and at the end of these spells of blindness, he had a severe headache. His head felt heavy. Sometimes on looking to the left, he saw objects double, although this diplopia had grown less marked of late. All the muscles of both eyes appeared to work normally. Upon pressure on the right globus, especially pressure directed from above and behind on the internal part, the patient would raise his left eyelid, but the paresis reappeared the moment the pressure was released; a fact which the patient himself noted while a tampon was being placed upon his eye.
It seems there had been a wound at the external angle of the eye, some nine or ten years before, as a consequence of which the eyelid of this side could never be parted as well as before. The accident in question had happened in 1905, and there had been a slight suppuration of a wound 2½ centimeters from the external angle of the palpable fissure.
The patient then went through a period of reëducation. It seemed that when he was trying to raise his eyelids, there was a mental inhibition which could be overcome only by effort. An attempt may be made to resolve the phenomena into three groups:
First, enophthalmia of the right side (post-traumatic, antebellum, a predisposing cause).
Secondly, a situation corresponding to so-called hysterical pseudoptosis of Charcot and Parinaud (eyelid falling without[619] wrinkles, head thrown back, frontalis contraction on effort to open eyes, eyelid lowered). The diagnosis of hysteria was supported by the transient opening of both eyelids when a sudden sharp order was given to move the eye-balls, and further supported by synergic automatic lid-movements when the patient voluntarily raised his eyes. He could not raise his eyelids to order.
Thirdly, functional ocular palpable synergy (left eye opening upon compressing the right eye).
Shell-shock Rombergism.
A soldier, 24, had sundry signs of traumatic neurosis. A curious and unexplained feature is the fact that in the course of testing for Rombergism he would fall forward like a log if his head were held in the vertical position, but if it were turned to the right he fell to the right; if it were turned to the left, he fell backward. Tests showed that he had no disease of the vestibular apparatus and no sign either of cerebral or of cerebellar disease.
The question is raised whether shell-shock can produce a differential Rombergism such as hitherto would have been explained on the basis of some organic vestibular disease.
Re Rombergism, see especially Bourgeois and Sourdille’s (edited by Dundas Grant) remarks on disturbances of balance which, if of labyrinthine origin, obey Romberg’s law, namely, are greatly increased with the eyes closed. Upon test, however, normal equilibrium, tottering, or a tendency to fall will be usually found. The tendency to fall is, as a rule, toward the side of the affected labyrinth, yet it varies according to the position of the head; that is to say, actually upon the position of the labyrinth with relation to the body. If there is a lesion of the right labyrinth, for example, and the head is turned to the right, falling is to the right; but if the head is turned 90 degrees toward the right, the patient tends to fall backward because in fact the injured right labyrinth has now become posterior in position. But if the head with the injured right labyrinth is displaced 90 degrees to the left, the tendency would be to fall forwards.
According to Beck, there was in his case of Shell-shock Rombergism no ear disease or any evidence of cerebellar or cerebral disease.
Walking with the eyes open yields in marked instances a sidewise bending or even the classical staggering called the duck’s walk and drunken gait upon a broad base. The most delicate test, according to Bourgeois and Sourdille, is[621] the Babinski-Weil test of walking with the eyes shut. A man with labyrinthine disease deviates from the straight path (he is made to walk forwards and backwards ten times in a clear space); bends pretty constantly to one side when walking forward, and pretty constantly to the other side when walking backwards. Spontaneous and Babinski’s induced nystagmus (rotation; caloric) and Babinski’s voltaic vertigo test are the other tests commonly employed in equilibrium investigation.
Otology and neuropsychiatry should go hand in hand.
A soldier in the engineers, 29, entered the neuropsychiatric center at Scey-sur-Saône, August 23, 1916. His diagnosis was: organic shock syndrome with right-side deafness and tremors. He carried a ticket showing an otological examination: tympanum normal; Rombergism absent; walks with eyes closed swerving to right; tends to fall, eyes closed, on standing on one foot; vertigo produced by rotation in either direction; no nystagmus either spontaneous or by test; deafness especially on the right side; equilibrium function insufficient.
The patient had undergone shock in April, 1915, being buried and then losing consciousness for twenty-four hours. The tremors appeared next day, and also deafness but without speech disorder. Nine comrades are said to have been killed beside him. The hospital ticket, April 13, said: deafness and multiple contusions from shell explosion. The patient was evacuated to Clarmont-Ferrand and went back to service with the same tremor and auditory disorder. He was shortly sent back to the interior for six months and returned improved to the front August, 1915. But he heard the cannon in the distance, and, under the influence of emotion and the fatigue of the journey, the tremors and deafness reappeared.
The tremor was generalized, involving both arms and legs and a slight lateral movement of negation of the head every ten or twelve seconds. Occasionally tonic contracture of the face, lips, cheeks, forehead; tremors of tongue; winking. The tremors were somewhat suggestive of toxic tremors.
The deafness was evidently exaggerated. Voltaic vertigo tested normal. Reflexes normal.
The diagnosis psychoneurosis was made and the patient was rigorously isolated, given a long psychotherapeutic talk concerning the nonreality of his deafness and his vertigo and[623] the possibility of cure by means of a very disagreeable electrical treatment. He made improvement upon psycho-electrical treatment and the next day both tremors and deafness had greatly diminished. September 4, the patient was considered completely well. There was a slight diminution of hearing in the right ear, the whispered voice was heard at 50 centimeters on the right side, the watch at 25 centimeters on the right and 60 on the left.
October 5 the patient was sent back to his corps. On the evening of his departure, angry at not having received leave, he boasted to his comrades of having passed but three days at the front since his injury.
It is remarkable, according to Roussy and Boisseau that this patient had passed sixteen months without ever having been taken for a neuropath or treated as one. The otologists gave the diagnosis of labyrinthine shock, but did not attend to the tremors. The pseudo-symptoms disappeared in six days at the neurological center and the cure had lasted six weeks at the time of report.
Re otology in these cases, see Bourgeois and Sourdille’s book mentioned under Case No. 439, particularly Chapter III, upon the functional examination of hearing. In the present instance, it will be noted that voltaic vertigo tested out normal. According to Bourgeois and Sourdille, the Babinski electrical test is the most convenient one to begin with, to learn in a few moments whether the vestibular system is working normally or not. These authors found amongst twelve patients, three normal reactions and one instance of hypo-excitability amongst four subjects who, by other tests, failed to show vestibular disturbance. Inexcitability as to voltaic vertigo was found in one man with a destroyed labyrinth. There were four instances of hyperexcitability in Babinski’s cases with marked equilibrium disorder. A case of Ménière’s disease yielded the same results. According to the intensity of the current, the following phenomena (in addition to the pricking sensation) are noted; (a) salty taste; (b) sidewise swaying with slight vertigo; (c) nystagmus with more pronounced vertigo; (d) sensations of sound. In short, nerve branches that go through[624] the petrous bone, namely, the chorda tympani, the vestibular nerve, and the cochlear nerve, have been successively stimulated. Babinski’s test was published before the Barany work on induced nystagmus, but Barany’s rotation test for the physiological excitation of the semi-circular canals, and his caloric test for the investigation of the ears and canals separately are to be utilized in addition to the Babinski voltaic test. Babinski’s law of voltaic vertigo is that a normal subject inclines to the side of the positive pole; a pathologic subject falls to the side to which he tends to incline spontaneously. If the labyrinth has been destroyed, there has been no reaction.
Re Case 440, Roussy and Boisseau in their capacity as neuropsychiatrists, point out the inadequacy of an otological examination taken by itself. They insist that neuropsychiatrists should be called in. It is probably equally true that neuropsychiatric work upon deaf cases is often inadequate on account of the lack of otological examinations. According to Bourgeois and Sourdille, the expert otologist’s problems are as follows: (a) Deafmutism; here Gault’s cochleopalpebral reflex is of value. The hearing of a sudden noise causes contraction of the orbicularis palpebrarum on the side upon which the noise is suddenly and unexpectedly made. Eyelash tips are particularly watched.
(b) Complete bilateral deafness. This is practically never organic; complete bilateral deafness is a phenomenon either of traumatic hysteria or of simulation. Sundry methods of surprising the patient into hearing have been adopted. The practice of teaching lip-reading to simulators and hysterics has led to some difficulties in diagnosis, but tests have been produced by Gosset (of one sound with the lips set to form another, and the like) which are of service.
(c) Extreme bilateral dulness of hearing.
(d) Total unilateral deafness. For the minutiae of tests for these types of hearing disorder and their simulation and exaggeration, see the War Manual of Bourgeois and Sourdille.
Jacksonian syndrome: Hysterical.
A Lieutenant of Infantry, 32, was struck by a bullet September 6, 1914, in the upper part of the left temporal fossa 4 cm. above the external auditory meatus. He did not lose consciousness, but had the sensation as if his head had been shot off, and about three minutes later he turned about, fell down, and lost consciousness. However, he regained consciousness a few minutes later and walked with support for about an hour. At the ambulance, he lost consciousness again, for half an hour. He was then carried to Amalie-les-Bains. The trip lasted 108 hours. The left side of the face was now swollen so that he could not open the eye nor could he chew from swollen mucosa folded between the jaws. The bullet was removed Sept. 12, from just below the scalp outside the bone, the point being slightly bent back. The bone had been depressed slightly for an area the size of a franc piece, and pressure at this point yielded a feeling of pain and discomfort. There was no suppuration. After a week, the man got up. He returned to his dépôt October 3 or 4 and was about to rejoin his corps when he had a sensation of pressure in the head and fell. When he came to himself he found that there was a frothy saliva at the left side of the mouth and that the whole left side of the body felt weak. The tongue had not been bitten nor had urine been passed, and twenty minutes later he felt as well as ever. He returned to the front in the Argonne, having from time to time similar crises,—at least once a week. Ordered to take a trench the night of January 17, he failed the first time, about midnight, but succeeded at four in the morning,—just afterward falling exhausted in another crisis, with unconsciousness. The stretcher bearers took him back and he was evacuated to Perpignan. He had two convulsions.
While with his family the crises grew in number to three or four a week, and sometimes twice a day. Upon request, he was sent to hospital in the Pantheon May 5.
There was always a sensory aura, consisting in a violent shock felt in the left side of the cranium like a blow of a club. There immediately followed a crawling sensation in the fingers and hand of the left side, running up the arm, with loss of consciousness coming on before the crawling reached the elbow. The seizure would last two or three minutes. There was no initial cry. The face grew pale. There was apnea, and frothy fluid running out of the left side of the mouth. There was no jerking of face or limbs; at the end of the seizure there were no deep inspirations. The extremities of the left side were rather flaccid during the attack.
A hemianesthesia was found affecting both skin and mucosae of the left side, and a slight retraction of the visual field on the left side was found. There were no other sensory disorders; the knee-jerks were lively on both sides but not actually exaggerated. Plantar stimulation was not perceived on the left side. The toes, except the great toe, were slightly extended. The fascia lata reflex failed to demonstrate itself. On the right side the great toe went into flexion on forcibly stimulating the sole. Sometimes the abdominal reflex on the left side was weak or even absent. The patient, who had never been nervous, had now become so since his attacks. He had had nocturia up to 12. There was no evidence of neurosis or psychosis in the family. Bromides diminished the crises a little in number. Static electricity was given from January 8,—no attacks for 8 to 10 days.
According to Jeanselme and Huet, this is a case of Jacksonian syndrome of an hysterical nature, about which it may be noted that the bullet struck the left side of the skull and the hemianesthesia and muscular resolution appeared on the same side as the injury.
Leg tic: Phobia against crabs.
A man, shell-shocked in 1916 (with loss of consciousness, disorientation and confusion followed by nightmares, memory disorder, attention disorder, irritability, mental instability and over-emotionalism) later still showed a choreiform tic. He had a knife-grinding movement of the left leg which made standing and walking difficult. There were no signs in the reflexes or reactions of organic disease. The man himself said that he felt a sensation like little electric shocks when his foot touched the ground, a sensation like pinching. He also had certain hysteriform crises. He was able to remember nightmares in which he felt as if he had fallen into a hole where there were crabs. In point of fact, he had a true phobia against crabs, crayfish, lobsters and the like; if he saw one, he always felt as if he were going to have a new crisis. The defense movement of the leg and foot was against a supposed pinch of the crab. At rest, there was no trace of the choreiform movement. The tic was especially marked when the man was suddenly asked to get up and walk. In a few days, when he had become more clearly conscious of his phobia and had slept better, the tic grew appreciably less.
Convulsions reminiscent of fright.
A soldier, 28, was blown up February 8, 1915, by a shell burst. He sustained no contusions but became completely mute. On July 3, he began to speak in a low voice. The torpillage treatment was unsuccessful because the man felt a morbid apprehension that the vibration of a loud voice or even of a rapid walk would resound in his brain. He had a sort of noise phobia, probably maintained by nightmares which frequently woke him up with a jerk though he could not remember their content. On the way back to his dépôt this man got off the train at the first station and went to a hospital complaining that the vibration of the train was going to be transmitted to his brain. Hysteriform crises developed in a few days.
According to Duprat these crises are nothing but a psychomotor development of the initial complex. The clonic and tonic convulsions are reminders of his states of extreme fright, a phenomenon of revival of the ideo-affective process, aggravated however by the oniric or post-oniric images.
Re diagnosis of hysterical fits, the absence of facial cyanosis, sub-conjunctival hemorrhages, petechiae of skin, and the Babinski reflex are suggestive for hysteria. Babinski points out that the initial cry, the fall, the loss of consciousness, the tongue-biting, the bloody frothing at the mouth, the urinary incontinence, and the post-convulsive prostration can all be consciously or unconsciously imitated. Hysterical convulsive movements are apt to be of wide range, gesticulatory, and opisthotonic.
Babinski announces to the supposed hysteric that he is going to reproduce the attack, as he is perfectly able to do by electricity. A mild current or mere electrode application suggests a fit in a hysteric, often very quickly. Babinski now announces that he can arrest the fit; carries out some selected procedure, and stops the fit. During the hysterical fit, the patient of course hears what is being said and during this time wrong suggestions must not be offered.
Fugue in a motor cyclist, with prodromal fatigue and subsequent delusions—recovery in six weeks.
A motor-cyclist, 36, with the colors from the outbreak of the war, about April, 1916, grew very weary, suffering from headache and seizures without loss of consciousness. Finally there was a voice: “Sleep, you must sleep.” Then other voices; then ideas of thought transference with people around him.
Observed in the psychiatric center, May 12, 1916, he had the same ideas of thought transference, and he made as if to talk with the attendants by responsive-looking gestures. Sometimes, he said, fluid struck his forehead, calling on his thought. Whereupon he listened. The man made no complaints about his plight, was not astonished in any wise at what was happening, nor did he seek to explain it. There was nothing in his history to suggest psychopathy except perhaps that his father was unknown.
The diagnosis of a chronic hallucinatory psychosis was made, but the outcome promptly overset the diagnosis. The man talked with ward-mates, and particularly with another patient who also talked about thought transference. This shook the man in his convictions, and he decided that it was but imagination and delirium.
He now told his story: How it seemed that he had in his thoughts the phrase, “Sleep, you must sleep;” how he had gotten up, saying, “No;” had noticed the others paying no attention to him; had gone back to his work and from that moment had begun to go into delirium. During this delirium or delusional state, his whole life from birth up, came back to him, as if some one were telling him. The headaches, which he at first felt due to Hertzian waves, suddenly ceased.
Shortly, however, a new phase had set in, in which he felt himself surrounded by spies and that others had control of his thoughts and were reading them. In fact, he grew a[630] little proud of the fact that people reading newspapers all around him were actually reading his own thoughts. The letters he wrote were being dictated. May 9, he spent a night with a succession of nightmares, and woke up with the firm purpose of going back to Paris by motor cycle to find the spies. He described his fugue and the thousand ideas he had on the way, his arrest, his imprisonment in a cell of Hertzian waves with a smell of sulphur and poisoned bread—a necessary fate on account of the spies.
On arrival at hospital, he had not known what was going forward. The nurses were giving him milk to destroy the taste of sulphur; the delirium then grew less and less. The room-mates were neutrals, war-weary; he seemed to be reading the newspapers before his mates, and they seemed to be talking of thought transference. May 20, the ward was changed. The new ward-mates did not believe in thought transference and laughed, causing the man to doubt.
June 2, the cure was in full process, and the ward was changed again; but in the new ward was a patient who had the same ideas of thought transference as the patient. At this time, the man’s autocritique saw through the delusion. He talked with his telepathic comrade and pretended to engage in a fake conversation about it. The delusions shortly disappeared, having lasted about six weeks.
Ordinary gunner’s life; a few days’ feeling of moral and physical discomfort: Obsession leading to fugue.
An artilleryman, 32, gave himself up a few kilometers back of the lines, three days after deserting his post. The man was a very good gunner and had never been punished once. Moreover, the battery was not under any special bombardment, and he had been in the same place a number of weeks.
He explained that he had gotten tired during the last few days. Everything was well at home and in the regiment, but he felt sad, his head felt bad, and he couldn’t sleep. Something drew him to leave, but then “sang froid came back to me, and I gave myself up.” He had lived the three days without eating and without sleeping. He was very emotional over what he had done, but he began to work and asked that he be sent back.
His mother had been very nervous. There was a marked facial asymmetry and faulty arrangement of teeth. The man was not alcoholic.
According to Mallet, in these cases of fugue, and in other cases of absolute delirium of apparently sudden onset, there is a feeling of moral and physical discomfort for some days before the outbreak. The outbreak itself is sudden on the occasion of some idea, either an obsession or a hallucination. Of all the prodromal signs, headache is the most striking. According to Mallet, such fugues are the expression of a mental imbalance allied to the onirism of Régis.
Aprosexia and bird-like movements.
A soldier of the dragoons, 25, entered Chavigny’s service May 30, 1915. He acted like a mechanical figure, requiring guidance. The face was without expression except for the mobile eyes, and sudden bird-like movements of the head, continually attracted to new noises and objects. An interlocutor was glanced at but not responded to. If an intense electrical shock was passed through his abdomen, for example, the man would look for a moment in that direction, but only the most fugitive defence reaction would be made, and the stimulus could be repeated with the same result, a moment later.
After three days, this aprosexia began to clear, and in four or five days, answers to questions and ordinary associations set in. Memory reappeared. It seems that he had been in concealment in the loft of a barn, when he saw his commanding officer carried by, having lost an arm and a leg. He lost consciousness and fell three meters, through the trapdoor of the loft. There was thus a combination of trauma and emotional shock. No external lesion was produced in the fall. His memory showed a very sharply defined gap for the period of his aprosexia with the bird-like movements, of eight days, and his memory was perfectly good up to the time of the fall. This is one of five cases observed by Chavigny, who remarks that there is something in the attitude of the young child which recalls the aprosexia of these patients. (Perhaps the phrase of James, “buzzing, blooming confusion” might be used.) One must go back to a period in the child’s development when he is not yet able to smile or keep his glance fixed on a shining object. On the whole, the resemblance is closer to the attitude of certain caged birds.
Re aprosexia and bird-like movements, see discussion under Case 353. See also Case 334.
Shell-shock; unconsciousness (45 days): Mutism (monosymptomatic).
A soldier, 32, had a large caliber shell burst one meter from him September 26, 1915, lost consciousness and remained comatose 45 days. He then got progressively better but did not recover speech. He was neither blind nor deaf. He was examined at the neurological center at Nantes and there Mirallié called him a case of hysterical mutism, finding no paralytic disorder of any sort and finding the patient able to write his story, to read and to understand what he read, but without much power of retention. He was placed in the phonetic reëducation service March 30, but made no progress. In the effort to speak the patient made strong generalized contractions, including contractions of his face and winking of his eyes, contractions of the jaw, and movements of the neck muscles. In fact, he seemed to be agitated by a sort of cervico-facial tic, and sometimes, although not always, he succeeded in getting out a loud voice sound, in which one could imagine the syllable that he was trying to utter.
In this case the mutism was evidently secondary to motor disorder. It is an example of functional dyskinesia (Benon). As long as this functional dyskinesia remains, the patient will not speak. The respiratory muscles are disordered, since the respiratory capacity does not go over 3 liters. This approaches the normal, however, and if the subject cannot speak it is because his diaphragm is subject to jerky or cramplike movements and because the lips and tongue do not execute the proper movements either for sounds, syllables or words. Such a patient cannot protrude the tongue or even bring it beyond the teeth.
Shell-explosion: Recurrent amnesia.
A shock case of Mairet and Piéron had a disorder of memory. Association paths were open one day and closed the next. Subjected to shell-shock, September 18, 1915, he was found wandering in the woods a few days later, having completely lost his memory, even for his name. In November he recovered his surname but not his given name. On stimulation he was gotten to remember his city, his father, the street, and the like. Shortly he could get back his memories more quickly; after a week it took only 35 seconds to remember that he was born at Paris. However, his recollection of the Trocadero and of the Eiffel Tower, which had come back to him in November, 1915, was lost again in April, 1916, to return once more in August. December, 1915, he could not write to dictation, but copied writing as he would a design. He suddenly felt himself able to write in the Morse code (he was a telegrapher); then ordinary writing returned. February, 1916, however, he had forgotten what the Morse code was. In April, he was taught numbers. One day he would know left from right, but had forgotten it by evening.
Shell-explosion: Comrade killed: Amnesia.
F. K., a 23-year old soldier, in civil life a turner, of Polish descent, and of a somewhat nervous and easily excitable disposition, early in August went from Strassburg into the Vosges and Lorraine. On the 26th a number of shells exploded near him. The troop was excited and took refuge in a cellar. K.’s best friend was torn to pieces by a shell. When his body was removed, K. felt sick and lost consciousness. He arrived at the clinic in Tübingen in a stuporous condition, by hospital train, on August 31, 1914. He walked weakly to his bed, supported by two men, and lay in the bed, apathetic and reacting to questions only with a stare. Things put in his mouth were swallowed. He remained motionless.
Next evening he answered a low Yes to a nurse’s question about eating. A little afterwards he said he supposed he was a prisoner in the enemy’s country. A little later he got properly oriented but still did not know how he had come. September 2, however, he was much clearer and said he had awakened out of a long dream. There was a complete amnesia, however, from the moment when he went to help remove the torn body of his friend up to September 1. Memories became clearer for the period before the shell explosion. The patient became very lively, talking vividly of war experiences, imitating shell hissing with an expression of intense anxiety, getting accustomed to battle scenes, saying that he was now seeing everything again as if real. He remained anxious for some days, complaining of weight on his chest and of feelings of internal restlessness and tension.
Amnesia for the period of August 26 to September 1 remained; all that K. could add to the story of those days was that he had been thrown sidewise for some distance by the air pressure of the shell.
From September 6 onwards, he grew calmer but he was still very labile, given to lively imaginings and emotion. By the middle of September he was well and discharged for garrison duty.
Shell-explosion: Recurrent amnesia.
A man, 33, had suffered shell-shock early in December, 1914. His intervening history is not reported, but he showed on admission to the service of Mairet and Piéron, May 5, 1915, a remarkable amnesia. There was a complete cutaneous anesthesia, anosmia, and ageusia, and he was mute. He lived only in the specious present. His previous life was completely abolished for him. He could dress himself, eat, use a fork and spoon, and a glass. He understood ordinary words; such words as man, woman, day and night, however had no meaning. He was observed for 15 months and presented four phases.
In phase one, there was a measure of success in reëducation, such that he grew able to recognize a few persons, to find his bed, and name objects. He was got to copy writing, to learn the alphabet, and to say a few words. He could not write from dictation, however. Less than two seconds after looking at an A, he had forgotten how it looked and could not trace it. This first phase lasted about two months.
The second phase began with fatigue, headaches, and the rather quick effacement of all he had relearned. If an errand was given him to do, he would run to do it before he should forget it; but if the trip required more than 4 or 5 seconds, he had to stop, not knowing what to do with the thing in his hands. He was still able to recognize 4 or 5 persons, but could add no more to his repertoire; and when one of them had been absent for a fortnight, he did not recognize him on his return. He could not remember the time for his meals.
The third phase was ushered in by improvement after vomiting; his speech came back in a feeble voice, November 16, 11 months after the shock. Reëducation could now be undertaken again. He easily relearned a number of things, feeling the greatest astonishment at his new acquirements as to the sun and the moon, the trees and the flowers, and the like. He expressed a curiosity to see his own home,[637] but when he went thither, he could recognize nothing. He wanted to get back home, namely to the hospital where he had lived all his life; where, in fact, he had been born from the psychic point of view.
At this time began the fourth phase, April, 1916—a phase of decline once more, in which a large portion of his acquisitions were again lost and he fell back to his condition in the second phase.
See discussion under Case 353 and under Case 367. Re confusional mental states, Roussy and Lhermitte, after distinguishing stuporous confusion from simple confusion, go on to differentiate what they call obtusion (see also discussion under Case 353). These authors say that Régis, in common with most psychiatrists, fails to distinguish the slow thinking and amnesia of true mental confusion from the temporal and the spatial disorientation that characterize the so-called obtusion. Of course, in all attacks of confusion, both attention and memory are affected, but there are special types in which attention defects and memory defects stand out in relief. The first of these types is the aprosexic type with birdlike movements, described by Chavigny (see for an example, Case 446). This aprosexia may be combined with mutism, deafness, or convulsions. The form of confusional disease in which amnesia is the out-standing feature is due to toxic or infectious disease, or is a Korsakow phenomenon, i.e., in the psychiatry of peace times; but the war has brought out amnestic confusion in other states than the toxic, infectious, and alcoholic states (Régis, Chavigny, Dumas, Roussy and Lhermitte). The amnesia may be incomplete, a sort of dysmnesia, or twilight memory, but as a rule, the amnesia is lacunar. The toxic and infectious amnestic confusions have a loss of memory for events following the onset, but these war cases of amnestic confusion have the loss of memory running back far into the patient’s past, slipping from the mind his name, his parentage, age, and vocation. Instead of being like the toxic confusional amnesia, an anterograde amnesia of fixation, the Shell-shock amnesia is apt to be antero-retrograde. These antero-retrograde amnesias, whether due to emotion or to[638] strong physical shock, may sometimes leave in sharp relief the recollection of the shock or event itself which initiated the amnesia. Meanwhile the patient does not forget automatic actions of dressing, reading, writing, and the like. The amnesia may be very selective, imitating aphasia, word blindness, letter blindness, agraphia, and the like. All this is part of the hallucinatory form of mental confusion which Régis describes as oniric delirium (see for oniric delirium, discussion under Case 333).
Lépine distinguishes amongst the confusions, five forms as follows: Simple confusion, hallucinatory confusion, acute delirium, stuporous confusion (under which Lépine also considers the battle hypnosis of Milian, see Case 365, and Roussy’s narcolepsy), and amnestic confusion. All these phenomena from the clinical point of view are connected with an acute and fleeting insufficiency of the most delicate or, as it were, psychic portions of the cerebral cortex, the delirium, so to speak, being activity of the unconscious, whereas a confusion is due to a clouding of the centre O of Grasset’s polygon.
Soldier’s heart, both neurotic and organic.
A territorial, 19, who had enlisted in January 1914, reached France in September, 1916. He was of neurotic make-up (night terrors, fear of dark, giddiness in high places, fear of tunnels, enuresis until 10 years, worry about seminal emissions), and had always had a tendency to short wind. Enlisting at 16, he found it hard carrying his pack at first but soon grew stronger. The trench life was distasteful. He began to wish that he might be killed, or at all events removed from the trenches. Pains developed under the heart, with shortness of breath, palpitation, dizziness, and faint feelings. The man connected these heart symptoms with what he called his weakness of gall bladder (namely, enuresis). He was several times sent off duty for heart treatment. After three months in and out of hospital, he got trench foot, was sent to England, and transferred to a special heart hospital. Here the pulse test was positive, in that the rate did not diminish as it normally does after two minutes’ rest. After graduated exercises for several months, the pulse test had become negative and the heart had gradually improved from the organic standpoint. The patient, however, insisted that his heart trouble was as bad as ever, and was probably consciously hoping that his symptoms might persist.
Re soldier’s heart, Abrahams classifies cases that come to the military surgeon for heart symptoms as (a) functional fatigue cases; (b) nicotine and drug cases; (c) organic heart disease and Graves’ disease; (d) the true soldier’s heart, occurring in men with a neurasthenic soil that lose control of the vasomotors and inhibitors of the heart.
Soldiers heart, neurotic.
An Australian gunner, 35, of a neurotic make-up (night terrors; horror of blood; fear of thunderstorms, high places, tunnels, horses; shy with both sexes), benefited by military training physically, but remained as neurotic as ever. On the way to his first service in Egypt, he feared shipwreck, and in Egypt was troubled by the weather and occasional palpitations and sinking feelings. He was transferred to the French front, May, 1916. He was terrified and depressed under shell fire, and horrified by blood. Peculiar sinking sensations or feelings that the soul was leaving the body came to him as he was going off to sleep; from which he woke at times with sudden starts. Later he had nightmares of things, mainly shells, falling on him. He worried, wanted death, and thought of suicide. In May, 1917, he was blown off his feet by a shell. Thereafter he began to feel that shells were being especially aimed at him, and four days later got a pain in the side, and began to tremble and breathe with difficulty, as if his throat were swelled up and he were going to choke. He ascribed this to gas. The bombardier finally sent him back to a hospital, where he grew weaker and screamed aloud on being awakened by his dreams. After six weeks in a special heart hospital, all the symptoms cleared up except the choking feelings and fear of instant death. Organically the man appeared normal. An initial pulse of 96 ran up to 168 after exercise, and down to 84 after two minutes’ rest.
Re soldier’s heart, Abrahams speaks of sundry hypotheses that he regards as erroneous. Soldier’s heart has been thought to be (a) athlete’s heart; others regard it as (b) a toxemic condition, possibly of bacterial origin; (c) hyperthyroidism (a larval form of Graves’ disease has been incriminated); (d) excessive cigarette smoking; and (e) deficiency of buffer salts in the blood, have been proposed by other authors.
Gallavardin has especially studied the tachycardial cases revealed by the war, cases in which auscultation is frequently unable to detect aught. These tachycardiacs are often hypertensive. Sedentary service should be found for them.
Re pulse 168 after exercise, Gallavardin found 8 per cent of 500 non-organic and non-tuberculous cases to run up from 150 to 175 (125 to 150 in 27 per cent; 100 to 125 in 37 per cent; 75 to 100 in 26 per cent; 50 to 75 in 2 per cent).
Re cardiac neuroses, Brasch points out that cardiac neuroses in the male in war time have found a strange new association with hyperesthesia of the skin. The patients showed dermatographia and hyperreflexia. The hyperesthetic zones of Head and Mackenzie were found by Brasch in all cases of organic cardiac disease, but also in two cases of cardiac neurosis in hysterics.
Moore calls attention to somewhat similar phenomena in the somatic group of nervous and depressed cases found in the war. These patients are fatigued, exhausted, sleepless, tremulous, vascular, and cardiac cases, with dermatographia, areas of paresthesia, and pains in the neighborhood of wound scars.
War Strain; Shell-shock: Hysteria (question of malingering).
A sergeant, 32, with 11 years’ service and eight months’ service in France, was admitted to a base hospital for inquiry as to possible malingering. It seems that he had taught in an army school for seven years before the war. He found heavy marches in France too much for him and fainted in the retreat from Mons and during the fighting on the Aisne, where he had reported sick for dysentery. The field ambulance where he was treated was near the shell fire, and a shell knocked him into a ditch. The ambulance had to move to a cave. Thereafter the patient suffered from tremor when spoken to or when watched. After discharge, he was employed as a dispatch rider on a motor cycle, but after three months lost his nerve for this work and took charge of fatigue parties. He found the work too much for him. He had been a total abstainer. Finally the malingering charge was brought up.
The patient was nervous, delicate-looking, with widely dilated pupils, prominent eyeballs, tremor of right arm, and pulse of 102. The tremor was markedly lessened when he was alone, and was somewhat under control. He felt that his memory was defective, and tests demonstrated the defect.
In hospital patient slept better, the pupils grew smaller, the pulse rate diminished. There was a reduction in sensibility to pain over the right side of the head and body and over the right limbs. A prick of the right arm or leg was described as a finger touch. There was also almost complete hemi-anosmia and complete hemi-ageusia on the right side. Visual acuity was diminished on the right, and there was general limitation of right field; left-sided vision and field normal.
After a month in hospital at home and two months’ leave, the patient was discharged no longer physically fit for service. He is now weak physically and mentally, subject to[643] severe headaches, and tremulous, especially in the right arm, when tired.
Re malingering, Sicard denies the existence of unconscious malingerers (presumably regarding this phrase as a figure of speech in relation to hysteria), and divides malingering into a creative and an acquired form. The simulateur de création assumes attitudes and symptoms to attract attention or pity; the simulateurs de fixation having been sick in the beginning, perpetuate their disease, in brief, crystallize their neuroses. The fixateur may be very realistic in all this, seeing that he has known from his own experience what a real disease is. The formula runs: The simulateur de création improvises; the simulateur de fixation repeats.
According to Mott, malingering in the form of an assumed Shell-shock is not uncommon amongst soldiers, and is rather hard to distinguish from a neurosis developing on the basis of an idée fixe.
Ballet’s definition of simulation is “a subjective or objective disorder which the patient invents with the idea of voluntarily and consciously misleading the observer.” Closely related to simulation is exaggeration or prolongation, conscious or intentional, of a real disorder. Babinski states that cases of genuine simulation are very rare, and that the subject under suspicion should be given the benefit of the doubt. Especially the word simulation, or similar words, should not be uttered in the presence of the patient. Practically speaking, psychotherapy applied as in cases of hysteria may often cure the simulator and the exaggerator.
The officer who could not kick.
An officer had had a bullet in the right calf, of which nothing was evident months later but small scars of entrance and exit. Nevertheless he complained of pain, especially after walking, and of inability to dorsiflex the foot beyond a certain point. No wasting could be found and no impairment of sensation. The muscles were faradically normal. Mills thought the symptoms were exaggerated and so remarked to the officer.
Under anesthesia, however, the dorsiflexion also proved to be impossible, and after exerting considerable force, Dr. Dunhill was able to rupture a massive fibrous band of adhesions that had prevented extension. The officer made a good recovery.
Dr. Mills confessed his error to the officer who had naturally resented the suggestion of malingering. The officer forgave him.
Re malingering, Moore states that no diagnosis of malingering should be made without the most careful examination and consideration of the individual as such, on account of the fact that the erroneous diagnosis dejects the patient and postpones recovery. It is particularly unwise to term the trouble “imaginary,” or to talk about “suggestion” or use similar terms in the presence of the patient.
Craig has found very few cases of actual malingering and states that tremors and paroxysms are often mistaken therefor. Bispham remarks that few malingerers are found among the patients of a doctor who is known to be a thorough examiner.
Re orthopedic cases like Case 454, Gleboff remarks upon the simulation of joint affections and upon methods of surprising the malingerers into sudden movements made in obedience to request in the course of medical examination.
Doubtful accounts by patient concerning arm palsy: Incorrect diagnosis of simulation.
A volunteer, 18, just before the war had a fall in which apparently he injured his skull. In December, 1914, he hurt his left forearm. About this injury he sometimes said he fell in a storming attack in a trench and broke his arm, and again he said his arm had been smashed by stones from a falling house. From that time forward there was paralysis of the left forearm with flexor contracture. May, 1915, slight hypesthesia could be demonstrated on the ulnar side of the arm, suggesting ulnaris injury. There were, however, no considerable electrical changes.
Six months later the man was sent up with a suspicion of simulation. In the meantime the contracture had resolved and there was a typical hysterical paralysis with all signs of neurosis. Six months later he was well enough to be examined for military service.
Here was a case in which the incorrect data offered by the patient himself as to the origin of his paralysis gave rise to the suspicion of simulation, whereas, as a matter of fact, the man was clearly hysterical.
Re incorrect data supplied by the patient to his own disadvantage, Lumsden remarks on the great difficulty of diagnosis in cases where hysteria and malingering have been combined, and Morselli states that, if the doctor has really made up his mind that the man is shamming, he should send him back to the fighting line at once.
Forearm wound: Hysterical edema?
A corporal, 26, formerly a farmer, was struck in the forearm by a shell fragment on the mid-portion of the radial border. The wound was slight (the fragment entering and emerging hardly 2 cm. apart) but bled profusely, according to the patient, who was evacuated next day but one to a hospital in the interior. By this time the right hand was swollen, nor could any movement of hand or fingers be made. Massage, mechanotherapy, passive movements did no good.
The man entered the neurological center of the Eighth Region, July 7, 1915, when there were already a few skin changes with dorsal thinning and palmar thickening. There was cutaneous anesthesia not only of hand and fingers but of the forearm to the elbow, and this anesthesia included heat and cold. Position sense was preserved. There was no evidence of atrophy except for the skin changes. An electrical examination showed normal conditions.
July 13, a sealed bandage was put on, but at the end of five days the hand looked as before. July 19, a new treatment was announced to the patient. With a hot needle a number of pricks were made on the dorsal surface of the hand and a few c.c. of fluid were withdrawn (containing a slight amount of albumin and a few lymphocytes), whereupon a dry bandage was put on. The next day a few finger and thumb flexion movements could be made and sensation had returned. Sensation completely returned July 21. The flexion movements were still incomplete, by reason of the edema and dryness of the skin. However, July 22, flexion was better and the swelling had gone down sixty per cent. Jacquet’s biokinetic treatment (active gymnastics of the hand and fingers) was given for four hours. July 25, the edema had greatly diminished and normal motion had returned.
Examination excluded renal disease. There was no sign indicating phlegmon. Quincke’s disease had other features.[647] Fraudulent application of a bandage might be considered, but the course of the disease under sealed conditions seems to exclude this hypothesis also. May it, therefore, not be a case of hysterical edema?
Re hysterical edema, see remarks under Case 407. In the case above, of Lebar, Babinski calls attention to the fact that the edema and the contracture diminished though they did not entirely disappear after the scarifications. This physical treatment did not act, according to Babinski, wholly as a matter of suggestion, and he fears that some cases of so-called hysterical edema are really cases of physiopathic vasomotor disorder; in fact, three of the cases published (and amongst them, the present case of Lebar), were cases of edema associated with contracture and developing in an injured limb. To prove a case of anything to be hysterical is, of course, according to the Babinski school, to submit it to a therapeutic test and cure it by suggestion.
Shell splinters in head: Suspicion of (a) simulation, (b) hysteria. Case actually surgical.
A man, injured by shell fragments in the head and sustaining fracture of both arms and a thigh, got well of his wounds, but fell into a nervous state with headache and dizziness. He was given prolonged observation psychiatrically and then sent back to the front as fit for service, but was shortly returned to hospital and sent to Cologne under the suspicion of simulation.
The picture was of unilateral increase of tendon reflexes, accelerated pulse, disorder in the intake of ideas, difficulty in finding words and delayed associations. His gait suggested a psychogenic disorder. X-ray showed two shell fragments in the vault of the skull.
According to Voss, it is a sad fact that victims of skull injuries are frequently charged with simulation or exaggeration. In the above instance, moreover, this charge was undoubtedly inaccurate.
Re simulation, see remarks under Case 453. Re neurological cases, the Neurological Society of Paris sent to the War Ministry a special note pointing out how tardy was the reference of sundry neurological cases to the special neurological service. They pointed out how important it was to send to these special services all cases of bullet and shrapnel lesions.
Re the malingering question, there is a wide divergence of opinion, even amongst experienced workers in the same city. The late Professor Dejerine said he had not seen a single case of malingering. In fact, he thought that malingering amongst soldiers and amongst injured industrial workers had been much exaggerated. Marie, however, working in the examination of many surgical cases, found malingering relatively common. Amongst forty of his cases, he regarded at least nine as malingerers or exaggerators.
“Sciatica,” torticollis, stiff arm: The desire to avoid active service plus functional disease.
A man enlisted September, 1914, went to France after six months’ training, immediately put himself on sick list, and was admitted to a base hospital: Diagnosis, sciatica. Later, he ceased complaining of sciatica and developed spastic torticollis. He was sent back to England, was treated with radiant heat and so on, and was eventually sent to the Royal Bath Hospital at Harrowgate.
He recovered from torticollis after six weeks’ treatment; but then developed a spasmodic contracture of the right shoulder and forearm. He was massaged for this and also given high frequency treatment. Then came two transfers (massage).
Early in December, 1915, he came under Collie’s observation. He then showed right wrist bent at right angles to the forearm; hand tightly clenched, so firmly that it seemed as if the wrist were ankylosed. The case was obviously a functional one. The man refused to enter hospital at Collie’s suggestion. He was sent to the Maida Vale Hospital. Previously he tried to persuade the medical officer that further hospital treatment was unnecessary, stating that he was now able to straighten his arm and that he was applying a splint to keep it straight. He progressed slowly in the institution. Told, if he would recover within fourteen days, he would be classified “for home service only”—before the fourteen days were up, he had suspended his weight on a trapeze and pulled himself up to his chin on it; had also lifted a 28-lb. weight with his paralyzed hand. In short, he wholly recovered. He is now doing duty with his unit.
Collie says this is not deliberate malingering but a mixture of functional disease and an obvious desire to avoid active service. When he appeared before the board for a final decision, there was a tendency to assume the old[650] paralyzed position until he was sharply called to order, when his arm assumed normal position.
Conclusion: The direct personal treatment of his mental condition and an appeal to his lower instincts were immediately curative and of much more value than the radiant heat or high frequency treatment.
Re Collie’s case, Russel finds surprisingly large numbers of malingerers; he found many at the time of the battles at Loos. It was particularly easy in cases of epilepsy to demonstrate a close relation between hysteria and malingering. In the psychogenesis of these conditions, Russel emphasizes the initial element of deception, which soon enormously increases either through the patient’s convictions of his ability to deceive or through a process of autosuggestion. Cases of semi-malingering are not uncommon. In England, Russel found more cases of a clearly psychogenic nature; yet in these, also, there was always primarily an element of deception.
Yes-No test of value re anesthesia.
The “Yes-No” test proved of special value in the case of an Australian private. Shortly after landing at Gallipoli this man had a bullet graze his ankle and fell some thirty feet over the bow of a ridge. He was picked up unable to move his legs and insensitive therein.
The paraplegia and anesthesia lasted three months. “Fracture dislocation of the dorsal spine” was the diagnosis made, and laminectomy was even contemplated. The sphincter reflex was normal and there was no atrophy, no rigidity and no reflex disorder. Asked to say “no” when he could not feel a pin-prick and “yes” when he did feel it, he replied “no” to each prick to the anesthetic area and changed his reply to “yes” when the sensitive parts of the body were examined. At another time the answers were found not to correspond with those given before.
The soldier was assured that he would get well and that as soon as he could walk he would be boarded and returned to Australia.
After a number of weeks he became able to walk.
Arabian fever.
An Arab fell on his knee, one day in the trenches. A contracture of the left arm, with great pain, and a temperature of 38 to 40 degrees, with hemoptysis, developed. This man had been considered tuberculous. One day, however, the thermometer went up to 41 degrees. It was discovered that he took artificial means to push the mercury up, and that the spitting of blood was voluntary. All these phenomena disappeared after he was put in the guardhouse for 24 hours.
Shrapnel scratch of head: Hysterical amaurosis “?” On isolation in a dark room, the patient began to see light!
A man may seek to exaggerate an anomaly of his eye which had existed before the war, in order to live comfortably far from the front.
A soldier sustained a slight scratch from a shrapnel bullet in front of the left ear, which scarred over in a few days. The soldier said, however, that the bullet had gone through his skull and a few hours after his wound said he could not see. Sent to the hospital he continued to say he was blind and finally brought up in an asylum for the blind near Lyons where he was taught to cane chairs and to write in Braille. This happened in July, 1915.
In October he was sent to the Hospital at Quinze-Vingt where a diagnosis of hysterical amaurosis was made with a large interrogation point. He was then sent to Brequet where there was a section reserved for disciplinary cases and very nervous cases not wanting to get well, a service under the charge of Roubinowitch.
The soldier escaped with a comrade and eventually reached Val-de-Grâce where the diagnosis of hysterical amaurosis was again made. Examinations several times showed that there was nothing abnormal about the eyes except that the eyelids presented habitual fibrillary movements (antebellum).
The eyelids passively opened, would remain open for a few minutes and then close. There was no winking of the eye to a light, yet the pupil preserved its reflex power.
Vision was abolished, however, the soldier said. He was without any other motor or sensory disorder. Much sympathy was given to the poor blind soldier. People were much astonished when the chief of the ophthalmological service had the man isolated in a dark room. Three weeks later the man had begun to see the light a little. A week later[653] the eyes remained open without the necessity of having the lids raised by the fingers, and vision returned.
Re amaurosis, Parsons explains the blindness which may remain after consciousness returns following Shell-shock, as a condition in which the lower visual paths are carrying on their functions normally. For example, the pupillary reactions are preserved. The condition is not unlike that found in amaurosis of uremia, and Parsons has found it in children with posterior basic meningitis. For Parsons, therefore, the block occurs in the higher centers above the thalamus, possibly in the synapses of the optic radiation fibers. Ormond states that the true cases of concussion blindness invariably pass through phases of great discomfort; whereas the malingerers are without such discomfort. Medical suggestion, also, has a powerful effect here, and may actually retard recovery.
A newspaper cure.
Sicard read in a French newspaper a story to the effect that, at two o’clock in the afternoon, a soldier had fallen on the sidewalk between Nos. 40 and 42 Boulevard de Liberté, in a nervous crisis. The people ran and picked him up. When he came to, he was very joyful, perceiving that the shock had given him back his speech, which he had lost the August previous. This soldier, the newspaper continued, became deafmute through the explosion of a bomb in a fight in Upper Alsace. “The brave soldier is most happy over the unexpected result.” The newspaper went on, “We congratulate him sincerely, as well as the people who assisted him.” He was the more contented that he had gotten well because, the soldier said, he would now be able to go back among his comrades to fight with the Boches!
Now, in point of fact, Sicard had dealt with this soldier the morning of the day in question. He had been simulating mutism for ten months, and finally told Sicard that he would like to leave that afternoon as he felt cure coming. Sometime after, he wrote a letter of profuse thanks for the benefits received, and said he did not deserve to avoid court-martial. He also said that he was going to do everything he could to justify himself. Incidentally, he kept his word and an officer in his regiment later gave him an enthusiastic recommendation.
Re malingering, see discussion concerning simulateurs de création and simulateurs de fixation under Case 453.
Deafmutism: Explained by patient as malingering.
A pure malingerer, of set purpose, initiates a quasipathological condition which he will discard when he has gained his end or when he is assured that he is unobserved. Malingering in the field of speech is rare. A private, 26, one year in service, three months in France, entered a base hospital, deafmute for nine weeks. He wrote: “I should be very happy if you can do anything for me. I cannot give a very clear account of what happened, as it is sometime since. I remember retiring from Hill —— with some more to some trenches, and in the open we were shelled and I lost touch with our chaps or else they were killed. I remember a great concussion and finding myself on the ground, and a soldier dragged me up and we ran for the trench. I was very thirsty and I ran down the trench to get some water. I met one of our chaps and tried to ask him for some, and I could not make him understand. He only smiled at me. The man who picked me up took me to an officer who was sitting on the edge of the trench and tried to make me understand, and then he sent me with this man to a dressing station, and from there I have been to different places, the names of which I do not know, except the last place, No. — Convalescent Camp. I have been there about two months——”
He seemed anxious to get well. He could not understand what was said. Induced anesthesia caused no phase of excitement, and the patient failed to regain his speech. He was evacuated to England. Three months later the patient thence wrote the following confidential letter from a Convalescent Home.[656] “Sir,—I regret very much to inform you that I was imposing upon you.——I may state that I was physically unfit for the Front.——During the whole time of training my pay was chiefly spent in tonics and drugs, but I kept going as I was determined to see what it was like at the Front.——I have written this——that your ‘notes’ on cases will not suffer any detrimental effect through my imposture.——I have not got my discharge yet, but shall stick out for it. I ‘speak’ but do not ‘hear’ very well.—” He was in two hospitals for functional nervous disorders in England, but in neither institution was he regarded as a malingerer.
Re hysteria explained by the patient as malingering, Chavigny discusses what he calls sursimulation. The physician must not fall into a permanent state of suspicion, and especially must not reveal his suspicions to the accused or to the bystanders. Chavigny quotes a French soldier whose letter to his wife was intercepted, stating that he was going to feign deafmutism to secure his discharge. Before he had succeeded in doing so, however, he suffered Shell-shock, and got a true hysterical deafmutism, which showed no signs of malingering whatever.
Deafmutism: Appearance of malingering.
A stretcher bearer was seen by Lt.-Col. Myers two days after admission to a base hospital. Stolid looking and mute, he had nevertheless talked in his sleep, had written a few words about “shells coming over,” and understood what was said to him. Lt.-Col. Myers’ notes run, “He puts out his tongue and closes his eyes and holds out one hand when I ask him to do so, but gets stupid (as if sulky) when I ask for the other hand. He will not hear any more. Next day quite deaf, and the following day light anesthesia with ether caused a return of hearing and of speech, with repetition of syllables to request on the way to deeper anesthesia. On awaking he cried as he was induced to resume his speech, and complained of pains in the head.
“Two days later, he seemed normal and said that he could have spoken on the second day, but that his eyes and ears had begun to swim, that he had felt dizzy, and was afraid to talk. He did not want to be sent back to the trenches. There had been severe shelling. He had lost consciousness until he awoke in a hospital at Y—. He recalled, little by little, how he had been taken back by a corporal to a cellar. He said he wanted to go back, but wanted a rest first. He went back to his unit and was reported as having done well for four months.”
There was a certain suggestion of malingering about the admission of the lad that he could have spoken before he was induced to do so. According to Lt.-Col. Myers, a number of patients upon recovery of speech are apt falsely to believe that they have been malingering. Functional disorders may simulate malingering.
Lannois and Chavanne warn against the suggestions given to malingerers and to hysterics by the statements on the tickets of admission borne by the patients for transfer, e.g. “incurable deafness.” These authors found 11 per cent malingerers amongst 262 cases of labyrinthine shock.
Simulation of deafmutism.
A soldier in the mountain artillery acted like a deafmute. He was unable to read or write. It was reported that he had been wounded, but no evidence of wound could be found. The man had a low forehead and a furtive glance, his whole impression being that of a criminal.
The only evidence of disease found was inflammation with perforation of the tympanic membrane of the left ear. Deep in the left auditory meatus was found a grain of crushed oats! The man’s speech difficulty was of a stuttering nature, but he stuttered in a different way at every test. He was unwilling to be narcotized. Finally by a process of scolding and cajoling, the man was made to confess that he could both hear and speak well. The peculiar stuttering early led to the diagnosis of simulation, but the fact that the tympanic membrane was not anesthetic, and that there was no anesthetic zone in the body strengthened the suspicion—to say nothing of the refusal of narcosis and the general behavior of the somewhat criminal-looking soldier.
A lame rascal.
An infantryman, 28, had an equinovarus, for which he was evacuated, hospitalized, given treatment, sent home for convalescence, and declared unfit for service. He was, however, sent back to the front, and on arrival, went lame; whereupon the regimental surgeon sent him to a nerve center. The equinovarus was there but it was nothing but a simple contracture without pain, atrophy, sensory, reflex, electrical, or X-ray disorders.
The abductor muscles were stimulated by electricity and the foot straightened. He was kept under observation for a time, was lame no longer, and was sent back to his regiment.
However, sometime later he was evacuated again to the same neurological center, stating that he did not know why. There was no longer any varus or anything abnormal. The rascal had enjoyed the game of going lame and had prevailed upon his officers to evacuate him. He then saw that he was found out and pretended that he had been forcibly evacuated.
Mother love and jaundice.
A soldier, 19½, entered the central psychiatric service at Val-de-Grâce, having been evacuated from a hospital in Paris, suspect of having brought about a picric acid jaundice. He had been undergoing treatment in this hospital, when the physician who had isolated him found that he was getting picric acid in packages secreted in his képi.
It seems that the soldier lived with his mother, and enlisted when he was not yet 18. He proved to be as good a soldier as he was workman, and came through the campaign without wound or disease. Accordingly, in December, 1915, he got a six-day leave. His mother, who loved him well, and of whom he was the sole support, had much regretted his enlisting. She was sick with some stomach disease and, after he enlisted, she told everybody that she was going to die and that it was his fault. So, when he came on leave the next day, she asked him to take a powder so he might stay a fortnight. She did not tell him the name of the drug; only told him how to take it in a small paper, swallowing it with a little water. She said he would become yellow and that he would get a supplementary leave. Three days after his return to the front, the boy took three of the ten powders; took the same number three or four days later; and the others five or six days later. He soon had jaundice with colic and diarrhea, and apparently was exempted from service for a few days. He had returned to the front hardly a month when his mother died and the boy got another six-day leave for the funeral. He took ten fresh doses of picric acid while at Paris, and was put into hospital by a physician without suspicion. His relatives thought he was suffering from a recurrent jaundice. When the story was told, the boy confessed to the family, and said that he had taken the drug in the first place only to please his mother. It is harder to explain the second trial, since he talked about the compassion and sense of obedience he felt to his dead mother. It is probable that he simply wanted a prolonged leave at Paris.
Re malingering, Blum speaks of fictitious jaundice as having received the name of La Carotte (the carrot) from the soldiers. Blum gives a partial list of instances of simulation as follows:
SIMULATION
(Blum, December, 1916)
False angina, from irritating solution.
Gastric disorder. Oil and tobacco (with tachycardia or jaundice) (use ipecac).
Diarrhea. (Isolate.)
Diarrheal stools imitated by a mixture of urine and water.
Dysenteric stools imitated by the addition of fat pork and bits of raw meat.
Appendicitis. Complaint of pain at the well-known McBurney point.
Tape worm. Carriers supply others.
Jaundice. (Smoke mixture of antipyrin and tobacco; drink tobacco juice. Ingest picric acid.)
Hemoptysis. Irritation of throat surfaces with a needle.
Albuminuria. Eat kitchen salt to excess in a bowl of milk. Edema and albumin disappear on surveillance. Albumin injected into bladder.
Diabetes. Phloridzin, or oxalate of ammonia. Glucose added to urine.
Incontinence. (Difficult to prove fraudulent. True incontinence in middle of night. Simulated, just before waking.)
Skin diseases:
Erythema. Herbs.
Eruptions. Mercury, arsenic, iodine, bromide.
Herpes. Euphorbiacae.
Eczema. Rubbing with slightly warmed thapsia. Rubbing excoriated skin with acids, Croton oil, bark of garou, sulphur, oil of cade, mercurial pomade.
Impetigo. With cantharides plaster and pomade stibiée.
Intertrigo. (In the infantry.)
Hyperidrosis of feet. Prolonged hot baths. Hot foot baths with excoriation, followed by scratching and covering with linen soaked in urine.
Edema of legs. Constriction.
(In Lombardy, cases due to introduction of equisetum arvense, an astringent herb, by fingers and toes, followed by energetic rubbing.)
Recurrent wounds. (Cover with wax sealed bandages.)
Abscesses. Introduction of septic material. A thread soiled with tartar from teeth is drawn through the skin. Characteristic odor of resulting abscess.
Phlegmons. Subcutaneous introduction of turpentine or petrol.
Paraffine tumors. (Apply heat.)
Sprain. A stopper is put under the heel; or compress the leg with bandages to stop circulation and knock below repeatedly and forcibly. Edema and ecchymosis follow.
Conjunctivitis. Ipecac, pepper, septic or fecal materials. Pupillary dilatation has been produced by introduction of a belladonna grain under the eyelid daily.
Ears. Running at the ears produced by placing urine or chemical product in the ear.
Emaciation and pallor. Ingestion of a large amount of vinegar. Abuse of strong tobacco.
Muscular weakness. Arsenious acid in eggs. Voluntary lead and mercurial intoxications.
Epilepsy. Absence of pupillary reflex to light and pupillary dilatation, insensibility of nasal mucosa and modifications of pulse persistent after the attack is over cannot be imitated.
Fever. Striking elbows against walls to elevate the mercury in the thermometer. Take temperature by rectum.
Bites. One simulator had a fork with twisted teeth to produce the effect.
Intra-abdominal projectiles. Bullet swallowed.
Swelling of hand and forearm, seven months.
A soldier was wounded September 22, 1914, at Charleroi by a bullet in the forearm. He came under observation May 14, 1915, with a huge edema of forearm and hand, suddenly stopping at the elbow, an elastic edema, especially marked in the palm, which was restored to its smooth contour very quickly after being compressed by the fingers, and very like an elephantiasis. The hand was in a position of moderate extension on the forearm, with fist clenched. There was a linear ecchymotic line at the upper edge of the zone of edema, especially on the antero-internal face.
According to the soldier’s own story, the swelling had begun a fortnight after the injury. He said that a very tight moist dressing had been applied during the first few days.
The patient was cared for by massage, and then by local baths. He was anesthetized in December and several drains were inserted; no result. In January he was chloroformed again and two long incisions were made along the internal border of the supinator longus and along the ulnar border of the forearm. He was better for two weeks after this second operation, but then grew worse.
The diagnosis of syringomyelia was now made, based upon the appearance of the arm and upon some ill-defined hypesthesia. This diagnosis was not entertained by Léri and Roger who, when they obtained the patient, put him into a plaster cast up to the shoulder. The edema went down rapidly to normal. In short, it was here a question of a simulator, who was even willing to undergo surgical operations with general anesthesia.
Re evading service, Gleboff’s classification is as follows: 1. False assertion of disease of (a) internal organs, (b) vision, (c) hearing, (d) joints. 2. Simulation of temporary disease of organs. 3. Mutilation of limbs.
Re swelling of hand and forearm, see remarks on hysterical edema under Cases 407 and 456.
A German shell-shy.
Gaupp’s simulator had not been under shell fire. He said to his captain that he wanted to see his badly wounded brother (he had in fact no brother), and got a furlough on this ground. He then fled as far as possible from the front, into the interior, roved about for some days, falsely asserting that he was under dentist’s treatment.
He was brought to Tübingen on the ground of mental derangement, on a hospital train, and was delivered to the clinic as a case of Shell-shock. This man’s state of excitement soon ended. As Gaupp could not make out his case clinically, he applied to the regiment and received in return court-martial papers. The man confessed that he had made false statements and fled because he was afraid of shells. Reproached with simulation, he preserved a shameful silence.
A fair exchange no robbery: France gets a simulator in an exchange with Germany of prisoners “unfit for service.”
A French soldier arrived in France from Germany in a reciprocal exchange of prisoners supposed to be incapable of bearing arms. The man showed a paraplegia with clonic movements of exaggerated degree. He was rapidly “cured” after being placed in a military hospital, and disciplined. He proved to be a vulgar simulator.
It was clear that the German physicians had made a gross error in diagnosis; but what, asks Marie, should be done with such a man, since he evidently should not be given a convalescent leave or a retirement? Should he be sent back to his dépôt?
If a year’s treatment yields no results, Grasset suggests discharge with suitable gratuity.
SIMULATION: Question of Quincke’s disease.
An infantryman was brought to the eye department of the Wieden Hospital early in May, 1915, with a diagnosis (from the internists) of Quincke’s disease.
Under the conjunctiva of each globus oculi were countless small air vesicles. There was not the slightest emphysema of the eyelids or of the skin about the eyes. The skin in the neighborhood of the zygoma was thick, red and swollen; but no air could be demonstrated in the subcutaneous tissues on palpation. Next day the skin swelling and the conjunctival emphysema had disappeared. No communication of the orbits with the air spaces of the skull could be demonstrated nor was it possible to push air into the conjunctiva by nose-blowing. The fundi were both normal and vision was normal. Special rhinological examination showed the nose to be normal. It was the skin swelling of the orbital region that had given rise to the diagnosis of Quincke’s disease. The man had been then referred to the internists who could, however, find no evidence of disease whatever.
During the three months’ stay of the patient in the eye department, once more swelling of the left orbital region and air under the conjunctiva of the left globus oculi suddenly appeared one day, but disappeared over night. At this time small subconjunctival ecchymoses were found.
This case must be regarded as one of simulation but produced in a manner unknown.
Bruises of head and back, not severe: “A case of pensionitis, a self-made neurasthenic for medicolegal purposes.”
Sir John Collie remarks that sometimes one has to recommend a pension knowing that what amounts to a fraud is being perpetrated. A seaman, 25, got newspaper notoriety after receiving some not very serious bruises of head and back. Two months later, when seen by Sir John Collie, he was a victim of bent back. He was finally able to remove his clothes and put them on with some alacrity, although at first he declared he could not. Woebegone during examination, he was noted to laugh and gossip with strangers outside. A physician had diagnosticated it as an obscure spinal lesion, but as he was fit to work, he was sent back.
Forty-one days later he put himself on the sick-list again. Pluck and nerve were gone beyond recall, according to his physician. In hospital his appetite was good, he slept well, and he had no troubles except an hysterical loss of sensation. There followed 33 days in hospital, three weeks in a convalescent home, and return to work for a month. Unable to stoop or kneel for pain, he was thought organic.
Sir John found him without desire to get well, hysterical, and suffering “from pensionitis, a self-made neurasthenic for medico-legal purposes.” He was placed for four months in a nerve hospital. On leaving this hospital he was still in the bent-back position, and went into a pantomime display when asked to touch his toes. Four weeks in the convalescent home found the following: The attending physician now suggested locomotor ataxia as the correct diagnosis! Sir John Collie was asked to report finally as to the fitness for work. Well assured that the patient was really a malingerer, Sir John nevertheless certified him as permanently unfit for further service as a case of traumatic neurasthenia, venturing to predict that after receiving the pension, he would be at work within six months. He received the pension (25 s. a[667] week for life), and Sir John Collie’s ability at prediction was justified by his return to work, at the end of exactly six months.
Re malingerers, Glueck remarks that a malingerer, besides being a malingerer, is a worthless sort of person in any event, and calls attention to the fact that special stresses may reduce men to lower cultural levels, to which lying and deceit may be more appropriate. Glueck remarks that the lay mind does not readily appreciate that a man with mental disease may at the same time be a malingerer of additional mental symptoms. It may be added that the professional mind is sometimes equally slow to appreciate the fact.
After Farquhar Buzzard
After A. W. Campbell
In previous sections we have already become acquainted with many therapeutic successes and failures: indeed it was almost necessary to detail treatment in certain cases to show the nature of the disease in hand or the correctness of a given diagnosis. In the present Section we approach the question more systematically.
After presenting a few examples of various spontaneous and non-medical recoveries, we bring into contrast the types of medical recovery that may be termed rapid (or miracle) cures and those that fall under the general head of reëducation. Admixed are cases of failure as well as of success: if it be remarked that the case method puts forward the best foot, it is probable that the same is true of almost any therapeutics as reported in early articles. As we go to press, trench reports indicate that at least one part of the profession is far more hopeful of successful psychotherapy even in the physiopathic group of disorders than their expounder, Babinski, could concede. The true statistical evaluation of the results must come years later.
Some neuropsychiatrists have been fond of saying that there is nothing new in Shell-shock, that specialists have long been familiar with the psychoneuroses, etc. Yet in the past, specialists have not learned overmuch about the true inwardness of the psychoneuroses. Even a casual inspection of the various therapeutic efforts here described shows how much novelty of observation and ingenuity of plan must eternally be shown in these ever-so-simple psychoneuroses!
Shell-shock: Deafmutism. Spontaneous cure.
A British soldier, 25, a coal miner, had had a bicycle accident five years before, after which he was unconscious for 2½ hours, and gave up work for five weeks, with headaches, fainting-fits, and nervousness ever after and with a tendency to imagine he could see things when there was nothing to be seen.
September 19, 1915, he was under shell fire in trench and dugout. A sergeant and three men working with him were killed by an explosion, and he remembers his cap being lifted off his head. He came to in 46 Rest Camp, some time later, unable to see clearly, or to hear or speak, and with headache and insomnia. He brought a paper from a hospital in France, saying, “Doctor, I had an awful dream last night again; I was dreaming that I was in the trenches; I could see the men falling and the great big shells exploding. I could see the light from the bursting of the shells very plain. They fairly lighted all the place up. I woke up very anxious I can tell you. I wish I could give over dreaming, and I keep having pains in my head right across my eyes.”
October 15, while sitting by himself outdoors, he felt a slight crackling in his head, noticed that he could hear sounds faintly, and in a few minutes he could hear fairly well.
October 17, he was heard making inarticulate noises in his sleep. The corporal next him told him about the noises in his half drowsy state; he tried to speak and said, “Mother.” He then felt queer all over, with pain in his head, and afterward became able to talk very well with slight hesitation.
Re spontaneous cures, Elliot Smith and Pear cite the cure of two mutes on hearing that Roumania had entered the war, and the cure of another by seeing Charlie Chaplin’s antics. Some workers (for example, Aimé), treat the functional mutes by simply leaving them to themselves, and maintain that they secure numerous spontaneous recoveries, regarding these as superior to cures by isolation, psychotherapeutic treatment, and the like.
Re mutism spontaneously or non-medically cured, see also cases 476, 480, 481, 482. For various medical methods of treatment, see, e.g., cases 516, 518, 520, 526, 544, 579.
Mott had a case which had been mute more than six months, unable to whistle, phonate in coughing, or blow out a candle, though heard to shout in his sleep: This patient recovered his speech when pitched out of a punt on New Year’s Eve. The condition was in one sense physical enough, as the X-ray showed that the man’s diaphragm hardly moved even with the greatest effort. Mott regarded the inhibition of the breathing movements, especially the phonation, as caused by fear. Mott speaks of a case that recovered on being told by a comrade that he had talked in his sleep. The man was so astonished by this statement that he said, “I don’t believe it.” Other instances of cure under quasi natural conditions are related by Mott: In the presence of a functional mute, Mott speaks loudly to the patient’s sister so that the patient may hear: “This man must be kept on a No. 1 diet, and when he can ask loud enough for you to hear, he can have a bottle of stout and a mutton-chop.” Several mutes are reported to have gotten well the next day under this treatment.
These effects shade imperceptibly over into the manifestly suggestive, and probably no sharp line can be drawn between the effects of medical suggestion, non-medical heterosuggestion, and even autosuggestion. Adrian and Yealland rather decry the Micawber line of waiting for something to turn up. Zeehandelaar, a Dutch professor, studied Berlin methods (Lewandowsky), and found numerous cases (both of mutism and of deafness, paralyses, contractures, and tremors) lying about without special treatment. According to this observer, the expectant treatment was sometimes successful, and sometimes not; if unsuccessful, the soldier was sent home, and re-examined a year later; whereupon he might be found to have profited by this long waiting and to have gotten well enough to return to army duty.
A decorated officer, evacuated for Shell-shock on the third day of the Aisne, after four days returns to the front. Evacuated a second time, after weeks returns to the front without relapse.
A young officer, with many decorations for brilliant Colonial service, was in the battle of the Marne, under six consecutive days’ shell fire, smoked phlegmatically a cigarette no matter whether walls were crashing or horses disemboweled beside him, and was uniformly able to stimulate his men to the heavy work by humor or heroic phrases.
A week later, on the third day of the Aisne, he had to be evacuated. He was another man—wild-eyed, shivering, jumping at the least noise, unable to eat or sleep, given to battle dreams. He had to be carried away from the battle zone and put in a bed in a town in the rear and given chloral. The nightmares continued. On being awakened he would ask where he was. He was kept in bed, given strychnine cacodylate, and dieted. He went back to the front in four days. Two days later he had to be evacuated a second time. After some weeks more in the rear, however, he went back to the front, and thereafter had not relapsed (April, 1916.)
Re relapses, Wiltshire thinks their causes and frequency prove the psychogenic nature of Shell-shock. Ballard states that a severe case lasting six months does not recover in the army. Many that are said to recover in hospital break down at dépôts, often with symptoms quite unlike those which they originally presented, and it will be remembered that Ballard has an epileptic theory of the nature of Shell-shock. See Cases 82, 83, and 84 in Section A, III, Epileptoses. But another portion of Ballard’s contentions relates to a causation through fear suppressions released by perturbing events. According to Ballard, if the man endeavors to re-suppress the released fear, the fits occur. Ballet and DeFursac note the frequency of relapses—fewer after treatment at the front.
Vicissitudes in fifteen months of a Shell-shock case with mutism and amnesia. Attacks of mania. Hyperthyroidism?
An Englishman, 21, in a rifle regiment, arrived in May, 1915, at the Dublin University V. A. D. Hospital, being dumb, impaired as to vision and hearing, having dilated pupils, tremors, restlessness and weakness, and giving the impression of visual hallucinations. Although suspicious, he was treated kindly for a few days, recovered his hearing, and wrote the few things that he remembered about home and the war, now and then tremulously and perspiringly writing down, “Asylum; do not lock up; I am not mad.”
With the idea of hypnosis, his bed was surrounded by screens, whereupon he grew so perturbed that the attempted hypnosis could not be executed. He learned the letters PP, TT, SSS, A-OOO, and finally AA-SS, AA-TT, T-OO, and after many weeks SS-SST-R and B-TT-R. His father visited him and probably was recognized.
At the end of September another dumb Shell-shock case recovered speech upon being given ether. Maj. Purser asked the sister to arrange for a like treatment for the first case, explaining that an examination of his throat might be painful. The cure of the second case by anesthesia got into the papers and before he was treated the account was possibly seen by the hitherto gentle rifleman. At any rate, he was seized with a sort of spasm, became furious and could only see Germans coming and carrying off his machine gun. He shouted for help. A half grain of morphine was given him and when it began to take effect the fighting spirit gave way to despair. He trembled over the loss of the gun, and remained in this state of despair for three days, remembering his regiment number and the like, but amnestic for his life during the past few months. He could not read now because print was indistinct. Words, when he had spelled them out, conveyed no meaning. He had a functional alexia.[677] When he saw a picture of a bunch of flowers in a notebook of his, he had another spell of excitement and regained his power of speech, remembering about his experiences only that he had been locked up. He had now completely forgotten his father, who came to call.
By the end of October he was stronger, but his horizon was still limited to the hospital surroundings and a little newspaper reading. Headaches and impaired vision persisted. Sight temporarily left him early in November, and there was a suggestion of an epileptic fit one day early in that month. Tonic and sedative drugs and suggestive remedies were of no avail. Hypnotism made him worse, and psychanalysis was, perforce, ineffective through the amnesia. At the end of November depression and suicidal thoughts set in, with an elevation of blood pressure to 178 m.m., pulse 80 to 90. Maj. Dawson then thought he was a suicidal melancholic. Rest in bed and thyroid extract were given, but the latter threw up his pulse on the fifth day to 140. He grew better mentally on the treatment, however, and his blood pressure fell to 140 in three weeks. He was now over-emotional, unable to stand or walk or feed himself or to pull on his socks.
For change of scene he was transferred to Mercer’s Hospital in February, 1916. He suffered from astasia-abasia. The tremor became jerky, coarse and persistent. The thyroid gland grew a good deal in size during the spring and the pulse went up to 120 per minute. There was also well-marked dermographia and there was a suggestion of the clinical picture of Graves’ disease. Even a quarter grain of morphine had little or no effect upon an ineradicable insomnia.
Maj. Purser gave the case up as a bad job and the man was discharged and sent home September 2, 1916. During the next two months at home he improved in steadiness, though he flushed if dealing with strangers, and improved as to memory. He began to be able to read better. He had begun to be able to get about on his feet without so much support. The ultimate outcome could not be reported by Maj. Purser.
Shell-shock: Mutism. Cure after killing a snake.
An Australian soldier of 20 went to Egypt, thence to Gallipoli where, on July 29, 1915, he was almost completely buried by earth from the bursting of a high explosive shell. He was admitted to hospital August 5 and transferred to Malta, where he did not speak, stared into space and sometimes made, impulsively, attempts to get away. About September 17 he began to assist the orderlies and played draughts.
The diagnosis there was cerebral concussion. He was sent back to Australia by transport and had to be put in a padded cell on November 1, having become violent, noisy and destructive. He would assault anyone who beat him at the game of draughts and threw anything he could lay his hands on out of the porthole. Hyoscine he resented and threatened the givers by signs. He was at times restrained. He threatened to throw himself overboard. Diagnosis: Melancholia.
At Melbourne he was found in good physical shape, but dazed, mute, apparently deaf, indicating his wants by signs. With pencil and paper he would draw a ship or a gun and would copy any question put to him in writing. He played draughts intelligently and made friends with one of his shipmates. In four days’ time he began to communicate in writing, answering simple questions correctly. Asked to put a question, he wrote “Do you think I am mad?” On the appropriate answer he shook hands with the physician heartily.
He was then sent to a military convalescent home at Highton. Here he communicated often in writing, and had an appreciation of sounds without distinguishing words. At a picnic on December 4 he killed a snake. While returning in the dark he began to whistle a song the rest of the party were singing. At the end of the song he clapped his hands and said, “What is the next item on the program?” Thereafter he was able to hear and speak. Seen four days later he asked to join the officers’ training school. However, he was discharged as permanently unfit for the service.
Course in hospital of an oniric delirium.
An Italian gun-maker, 27 (father neurotic; grandmother and mother, alcoholic; patient excessive onanist), was called to arms June 14, 1915, and went into artillery service in the Tolmino, early in September. Some time later, a shell burst about 30 meters away and killed his lieutenant. The patient, however, was not hurt and did not even fall. He became mute and inaccessible, and was sent to a military hospital, and thence to an asylum in Udine, where he was restless and hallucinatory. October 2, he was sent to Florence on two months’ leave for convalescence. He was still hallucinated, always seeing his dead lieutenant. He spoke rarely, slept little, and his conduct became more and more queer. Now and again, he would act exactly as if he were at the front. November 5, he started off to find his brother, but was met by a hospital attendant, who promptly took him to a clinic. Here he was inaccessible and lived in a hallucinatory way a soldier’s life at the front: in continual movement, shielding his eyes with his hands as if looking far into the distance, bending down to turn an imaginary lever, apparently taking part of his aim, crouching in a corner, clapping his ears with his palms, and obeying hallucinatory commands: “Ready,” “Fire,” and the like. As to his interpretation of the actual surroundings, he would give a military salute at the entrance of the physician, as if he were the lieutenant. Another patient near by was interpreted as a spy. Hypodermic injections, November 6, were interpreted as military antityphoid injections. On succeeding days he piled dry horse-chestnut leaves for a parapet, which became the scene of battle. November 12 he had become a little more lucid. November 14, he evidently heard whistling and made the leaves ready as a bed for horses. November 15, he rolled up his blanket in a military fashion and hid in a cell corner. He explained, November 16, that he was a sentinel and had not been relieved by the corporal. He had saved everybody’s lives by signaling from a tree the presence[680] of four airplanes. He could not be convinced he was in an institution for the insane. November 20, he was virtually recovered but amnestic for what he had done since commitment. Headaches and dizziness. November 21, he remembered some of his dreams, especially one of being blinded and another of being tied by a German to a tree. By November 29 he had become lucid and oriented, but there was an amnestic gap for his stay at the clinic. Early in December the fields of vision were contracted; polyopia and a glaring and burning sensation before the eyes (after each test conjunctival and tear duct inflammation).
December 21, discharged well.
Re the nature of oniric delirium, see discussion under Cases 333 and 450, Chavigny had but two cases out of 260 in which a rapid curability was noted (90 per cent finally curable). Chavigny’s treatment consists of rest in bed, quiet, purgation if necessary, and warm or cold shower baths. Chavigny remarks upon the extraordinary transformation from apathy to lucidity in the course of a few minutes, brought about by arranging a slight but definite emotional shock to the patient, namely, by mentioning in his presence something about home or family. One bit of technic was to get the patient to write or dictate a letter home.
Régis remarks that battle dreams of this nature occasionally affect alcoholics in garrison or at home. The victim ought not to be hastily committed to an asylum, but should be treated in a military neuropsychiatric service with isolation chambers and open wards. Régis organized early in the war at Bordeaux a central psychiatric service along these modern lines. He remarks that the central service ought to receive not only patients from the military hospitals, but also patients from the temporary auxiliary hospitals of the city and district round about. A pooling of the military and civilian issue upon rational lines is here indicated.
Régis and others have remarked upon the necessity of differentiating these battle deliria from toxic and infectious psychoses.
Shell explosion: Deafmutism, recovery of speech with electrical treatment; deafness cured by suggestion in writing.
A fusileer, 20 (mother neurotic, brother hemiparetic from infantile disease; patient had extreme otorrhea from an early otitis media), entered the army January 15, 1915. He was sent to the Isonzo in May and was slightly injured in the nape of the neck and the left calf by fragments of a shell that exploded near by. He was picked up unconscious and taken to the hospital at Servignano. There he was given electric treatment, and in a period of 18 days recovered his speech, passing through a phase of stammering. He was sent to a special hospital in Florence, still deaf, and passed into a state of mental excitement with visual hallucinations of soldiers. He was given chloral and bromide. He insisted that he was incurably deaf. August 22, he was admitted to Buscaino’s clinic, completely deaf, slightly stuporous, somewhat indifferent, and innocent of any effort to make himself understood (contrary to the habits of an organically deaf person). Simulation could be excluded. It was possible to awaken the patient during sleep by auditory stimuli, whereupon he opened his eyes but could not hear. He talked well and spontaneously, telling about his accident, reading and answering by signs. He was assured,—always in writing,—that upon the following Sunday his hearing would be restored. Upon that day, during the visit of a lady,—one of the patient’s friends,—hearing was suddenly and almost completely restored in the left ear. The patient was so moved by this that he cried when the physician came. Upon the following day, he gradually began to hear with his right ear. A slight diminution of hearing in the right ear persisted, however, until September 24, and was associated with headache and pains in the left ear—pains which the patient compared to his ear pains in childhood (remains of otitis with retraction of the tympanic membrane).
Paraplegia: Cured by administration of Iron Cross.
After heavy shelling a soldier fell for two days into a clouded state from which he waked with complete paraplegia of the lower extremities, and total anesthesia from the pelvis downward (reflexes and electric excitability normal).
On the third day after his reception in Nonne’s wards, he was about to be hypnotized when news came that he had been promoted to a lieutenantcy and had received the Iron Cross. He fell forthwith into hysterical convulsions, in the midst of which the hitherto paralyzed legs worked perfectly well! Even after the hysterical attack was over, the man could still move his legs in bed normally, but had absolute astasia-abasia. Next day, with deep hypnosis, markedly improved. After eight more days of hypnosis the new lieutenant got back his normal gait.
Shell-shock, burial: Mutism. Cure by getting drunk.
A patient, 25, nine years in the service, was buried in a dugout by an explosive shell at Ypres, June 17, was taken out unconscious, and eventually reached the hospital at Versailles. Consciousness had returned a few days after the injury. There was ringing in the ears, difficulty in hearing, and inability to speak. He arrived at the Duchess of Connaught’s Hospital at Taplow, July 12, when, aside from the above-mentioned symptoms and a rapid heart action (108 at rest), he seemed perfectly well. About August 14, he began occasionally to refuse solid nourishment and remained in bed, eyelids closed but twitching at times, especially when spoken to. He resisted having his eyelids opened.
August 27, he was allowed to go to the village with companions, and got drunk, found his voice, for two days talked and sang incessantly. Discharged September 9, cured.
Shell-shock and burial: Mutism. Cure by work in a vineyard with wine to drink.
A correspondent of the British Medical Journal reports a case of cure of emotional mutism. This robust young soldier at Verdun was buried by the explosion of a shell and was thereafter found unable to speak. A week later he arrived at the ambulance in the interior, and was still mute. He could understand what was said to him without difficulty, and was able to reply by signs. He did not even move the lips when requested to pronounce such words as mamma and papa, but was eventually induced to whisper these words.
The laryngoscope showed complete paralysis of the vocal cords, which were in extreme abduction (it was possible to see several tracheal rings). There was no reaction on the part of the pharyngeal mucosa upon stimulation.
A fortnight passed without restoration of speech, though at one time, not having bolted the closet door, the patient was startled when a nurse rushed in, and he said, “Oh, pardon, Madam.” The mutism persisted. He was then given work in the vineyard, plenty of wine to drink, and hard work. After a time (not specified) speech suddenly returned. According to this correspondent, “this indeed is a universal experience, namely, that hard manual work is the best remedy for such functional incapacities of traumatic origin.”
Re Cases 480 and 481, compare cures by anesthesia with chloroform, nitrous oxide, and the like.
Re gradual cures as opposed to sudden ones, Dundas Grant deprecates violent measures in the treatment of mutism during the period of exhaustion after Shell-shock. However, Dundas Grant does not advocate an expectant treatment, but employs a gradual reëducation of the voice through imitation of the teacher. The voice is sometimes restored at a sitting, sometimes gradually; see, for example, Case 578 of Briand and Philippe, and Case 586 of MacCurdy.
Shell-shock, unconsciousness: Deafmutism: Spontaneous recovery of speech and gradual recovery (several months’ isolation) of hearing.
A musketeer was deafened and stunned by a near-by shell explosion. On coming to, he found no wound, but was deaf and dumb.
Speech returned after ten days, and hearing partially, but there was a tonic stuttering. He had to hunt anxiously for words, talked like a child in infinitives and telegram style, although he could express himself in writing perfectly well.
Hearing improved on the right side very quickly, but on the left side conditions varied from total deafness to subtotal deafness. There was a general hyperesthesia of the skin, pain on pressure on the temples, exaggeration of skin and tendon reflexes, marked tremor in both hands. The man was anxious, depressed, and irritable. During caloric tests of the vestibular apparatus in the course of the next few weeks, the man had an hysterical attack of crying twice, following which all the phenomena got worse.
Rest and isolation from all such influences procured an almost complete recovery in several months.
Re differential recoveries, see also Case 585 of Liébault, in which speech was recovered by suggestion and reëducation, and hearing by a process of reëducation alone.
Re isolation, Roussy and Lhermitte remark that in all the psychoneuroses of war, isolation is a valuable and indeed an indispensable aid to psychotherapy. The application of this old classical method of Weir Mitchell reinforces the persuasive talk of the doctor on the day of admission, allows the man to think over the promises made to the doctor, and permits longer observation. It depends on the case, whether rigorous isolation on limited diet shall be employed. See below a general discussion of the psycho-electric and reëducative method employed in French centres.
Marches; battles; slight shell wound of left upper arm: Hysterical anesthesia of the arm and tremors (NO paresis). Causes slight—disease obstinate (partly explained by furloughs among sympathetic friends).
A soldier, 26, without heredity, always well, in long marches and several battles early in the war, August 23 sustained slight shell wounds of thighs and left upper arm. He was unconscious about five minutes. In eight days, the wounds were healed, and all movements were free.
Immediately after the trauma the arms trembled, and at times the legs. Treatment was instituted (baths, drugs, massage, electricity), but without result. After a month’s treatment and a furlough at home, the patient was sent, January 3, 1915, to the Jena Nerve Hospital. He was a powerful man of middle size, with some small movable scars on the left upper arm, remains of the shell injury; two similar scars of the gluteus maximus. The deep reflexes were slightly exaggerated, as were the skin reflexes. The touch and pain sense in the left arm was absent as far as the shoulder in typical segmental fashion. Arm movements were free; there was an occasional tremor in both arms, especially the left. This tremor would pronouncedly increase upon intentional movements and with emotion.
He said that about two weeks before, at home, he had waked up in the night and lain down on the floor beside his bed, feeling giddy in his head. In a week the tremors had diminished, leaving only a very slight tremor of the left hand. The patient went to considerable pains to conceal his tremor, holding his hand in a military position at the seam of the trousers, on the medical visit. Sometimes he would succeed in making the tremor quite disappear. February 5, he was busy about the ward work, going errands and carrying trays. He would intentionally spare his left hand in this work. Upon trying gymnastic exercises, the[686] tremors of the left hand and also of the right reappeared. After a few days these tremors again disappeared, only to come back on the 12th, when there was a constant tremor also when the patient was at rest. He had been affected when observing another patient (8[7]). Accordingly, he was separated from this patient and put in a psychiatric ward. The tremor remained of varying intensity, sometimes being absent for hours together.
Request for furlough at the beginning of March was refused with the statement that it would be granted when cure was complete. The patient was inaccessible to psychotherapeutic influence. He was always of a friendly, modest demeanor, sleeping well, and performing all bodily functions properly. On any exertion the pulse ran to 134. The heart was normal. There were outbreaks of perspiration.
March 26, he renewed his request for leave, desiring his Easter furlough. He was told he might expect it. March 31, the tremor was found to have quite disappeared. Upon his return, April 12, there was a marked tremor of the left arm, especially of the wrist joint, which again disappeared after some days. The middle of June he was released as capable of garrison duty with the recruits.
If there was a mechanical factor in this case, it must have been the shaking-up of the body by the shell explosion. His skin lesions were slight. The main factor was doubtless the emotional shock. The tremor supervened upon a very brief period of unconsciousness. It is hard, according to Binswanger, to explain the localization of the cutaneous anesthesia without the development of a corresponding paresis. May it be, inquires Binswanger, that the wound of the left upper arm at the moment of the setting-in of unconsciousness, or perhaps at the moment of waking from unconsciousness, directed the mind forthwith upon the left arm and in this way produced localized disorder of sensation? If so, why did the wound of the gluteal region not produce corresponding disorders of feeling and sensation of an hysterical nature? The obstinacy of the disease stands in striking disproportion[687] to the slightness of the causative factors at work.
According to Binswanger, this is perhaps due to the long furlough which the patient had. According to Binswanger’s experience, as that of many others, home works badly for these hysterical patients; their friends sympathize with them too much.
Re furloughs, Ballard states that severe Shell-shock cases should get analogous treatment to that of civilian psychoneurotics, namely, a complete removal from the environment in which the illness began. He advocates three months’ leave, after which the man is to be sent to a convalescent home, and thence to a command dépôt. He states that if a relapse then occurs, such a patient will never be a soldier. Ballard would allow the men to walk about with their “pals (not with escorts).” Cimbal remarks that German data show that home furloughs should be avoided in every instance where possible. Fiessinger remarks, on the basis of English experience, that a Shell-shock patient treated by rest, suggestion, and manual occupation may go back to the line “and on a subsequent occasion prove a hero.” (See Case 474 of Gilles.) But Forsyth remarks that it is probably injudicious to send any cases of Shell-shock, with few exceptions, back to the firing line, because their fighting value has been permanently deteriorated, and because, if the fear of return to the trenches is removed, recovery is more rapid. The experience here is not unlike that of industrial accident board cases with rapid recovery after the decree of compensation.
War stress in a volunteer banker: Hysterical seizures. Treatment by hydrotherapy.
A banker, a volunteer (articular rheumatism at three years; at 18, some form of lung and tracheal inflammation; tendency to fainting spells on cold days—heart disease was said to have been found), as a result of the strain and excitement of the war had hysterical attacks during a fortnight before observation in hospital, consisting of sensations suddenly developing in the region of the heart, stiffness of the whole body, disorders of movement, without loss of consciousness.
November 23, 1914, he was examined in bed in the dorsal position, with the muscles of the legs, back, and neck in a state of tonic contraction. He was unable to answer questions. The pupil reactions were normal in the seizure. The attack ceased in two minutes, as the result of hitting heavy blows on the chest with a moist handkerchief and the threat of a strong and painful application of the electric current. The patient then got out of bed at request, walked about a little incoördinately for a time, but after a few minutes was able to walk perfectly and to talk once more.
Examined, November 25, he was found to be pale, fairly well nourished, with a somewhat accelerated pulse, and a melancholy, slightly apathetic expression. A systolic murmur at the right apex; accentuation of secondary pulmonary sound; increased knee-jerks; trembling of the lids (Rosenbach).
By December 12, the patient was completely well. The seizures had not recurred. The treatment was by hydrotherapy. A preliminary treatment is advocated by Hirschfeld, to insure peripheral circulation, either by light baths, hot douches, or packs. More important than this preliminary treatment is the cooling off process by means of tepid douches or partial baths. These partial baths are given at 28°C. for the intense effect of the cold. Sometimes[689] this treatment can be concluded with a dry pack. The patients are treated by Hirschfeld three times a week with both the warming and the cooling procedure.
Re hydrotherapy, Mott has found the continuous warm bath of great value in Shell-shock cases coming back from France. He keeps the patient in the water from a quarter to three-quarters of an hour, or longer. A warm bath and a drink of warm milk at bedtime may permit a man to get on without hypnotics, or to get on with lesser amounts of hypnotics. The effect of these baths is doubtless largely somatic. Some writers stress the suggestive value of hydrotherapy as well as of electricity, radiant heat baths, and the like (Ballard). A neuropsychiatric center properly equipped with a hydrotherapeutic plant can do therapeutic work by means of the suggestion afforded by a cold shower, which may act quasi miraculously, like electricity (Roussy and Boisseau). In fatigue and exhaustion cases, along with adrenalin and strychnin, Aimé gives mild hydrotherapy without other sedatives. Laehr’s free sanatorium at Schönow treats the arrhythmia and tachycardia cases with rest and hydrotherapy.
Brasch reports rather poor results with hydrotherapy in the cardiac neuroses. Weichardt has used the continuous bath as a form of psychotherapy and permits the symptoms of psychoneurosis to subside therein.
Shell-shock: low blood pressure: Pituitrin.
A lance corporal of the Expeditionary Force, 26, went to France feeling very fit, February, 1916. He was blown up by a shell July 1, and faintly remembered crawling out of some water. He came to in a dugout, dumb and partially deaf, and was blind for a few minutes. August 17, he was admitted to Mott’s wards at Maudsley, mute but with hearing normal. The hands were dusky, sweating, cold, and slightly tremulous. He was given to battle dreams and used to wake in a sweat and terror after a pantomime of bomb-throwing. He had headache and was depressed. He complained of feeling cold and the surface temperature was subnormal. The blood pressure was also subnormal (according to Green, nightmares are most marked in cases with low blood pressure; these are, in fact, severer cases of Shell-shock than cases with high blood pressure; only 10 of 27 cases with blood pressure above 120 showed nightmares).
September 25, he was able to speak in a whisper. The dreams had become less terrifying. The other symptoms had been slowly improving.
November 25-28, all of the symptoms returned upon hearing the death of his brother in action.
The man was now put on extract of pituitrin gr. 2, t.d.s. (better results are claimed by Green from pituitrin extract than from pituitary fluid injections, as these sometimes cause dizziness, of which no case treated with extract complained). As in other cases, the extract was immediately followed by an increase in blood pressure, a general improvement and a diminution of headache and depression. The bomb-throwing pantomimes still persisted, but the patient was less weak on waking. The treatment was continued for seven days, whereupon the surface temperature began to rise and the patient himself felt that he was much warmer. The pituitrin was discontinued after a month’s treatment, yet the improvement persisted. The man was boarded out of the army and in March, 1917, wrote that he was still feeling better.
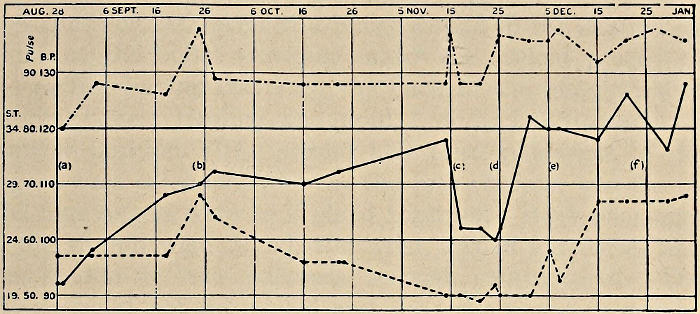
Blood pressure, surface temperature, and pulse in a case of functional mutism. (a) On admission, troubled by nightmare. (b) Able to speak in a whisper. (c) Much depressed after bad news. (d) Put on pituitrin. (e) Marked general improvement. (f) Taken off pituitrin.
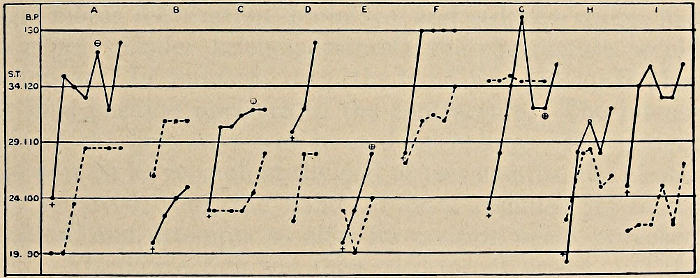
A-1 Showing the effect of pituitrin on the blood pressure and surface temperature. Each dot is one week’s interval. + is the pressure when the first dose was given. 𐌈 is the point at which the pituitrin was discontinued.
Various treatments of a contracture of hand.
A chasseur, 22, received a bullet wound in the anatomical snuffbox, the bullet emerging under the styloid process of the radius, having traversed the back of the hand without striking bone. Healing was rapid, but the hand assumed a peculiar position. The second and third phalanges of the fingers were extended, whereas the first phalanx was flexed. The four fingers were as if glued together. Both phalanges of the thumb were flexed, the wrist was in extension, and the tendon of the palmaris seemed contractured. The fingers could not be moved and the wrist was very mobile. There was pain on attempts to move the hand passively, and small clonic contractions were made by the fingers. There were no sensory disorders, but there was a maceration of the interdigital spaces.
Mechanotherapy accelerated the contracture, and massage, motor reëducation, bromides, and sedative drugs, had no effect. Under kelene-anesthesia the contracture would disappear. In January, 1915, the hand was put up in plaster in a position opposite to the contracture. The intense pain of the first days was treated by opium. The patient was sent on leave, and, at the end of two months, the plaster was removed; but the hand at once resumed its faulty position, and attempts to alter its position again provoked pain. Elastic traction was then tried for six weeks, and the bad position was somewhat modified but not improved by hyperextending the second phalanx on the first, and putting the third in slight flexion on the second. Hot compresses were unsuccessful also. May 14, 1915, the position was still irreducible; there was no R. D. or electrical hyperexcitability. This was not a question of radial paralysis, since finger extension was distinct; nor a paralysis of the median, since the thumb was flexed. The contracture, in fact, does not affect a special nerve territory, and the disorder is in the ulnar, radial, and median territories.
Orthopedic case.
A patient suffered from a rupture of the peroneal nerve in its lower part, September, 1915, and had operation scars before and behind the external malleolus. He was immobilized for 45 days at first, and then for 30 days, with the foot in extension on account of the pain produced in the endeavor to put it into normal position. A 6 cm. atrophy was then found to affect the calf, and there was a fibrous retraction of the tendo Achillis and of the calf muscles. There was no anesthesia, the toes moved easily, the foot was fixed in equinus, with about 7 cm. of the heel above the ground. He was placed in various orthopedic institutions and was treated with mechanotherapy, but without result.
At the neurological center, however, in six weeks, he was got to walk, with his heel on the ground, by means of massage and manual mobilization. The atrophy diminished a centimeter and the foot became mobile in all directions.
According to Sollier, mechanotherapy by means of apparatus is apt to be ineffective, especially in contractures, because its action ceases the moment it ought to commence, namely, when the patient is beginning to react a little painfully after recovery from anesthesia. In cases of retraction, mechanotherapy with apparatus does not allow the proper combination of massage with progressive mobilization.
Re orthopedic cases, Jones classes the conditions that create an orthopedic case under four heads (note especially the fourth):
1. Mechanical injury to bone, joint, muscle, or nerve.
2. Atrophy and disease of these structures primarily due to the injury.
3. Incoördination of movement due to disease of the brain—a result of atrophy and disease of peripheral structures.
4. Psychological conditions which can be overcome by reëducational processes.
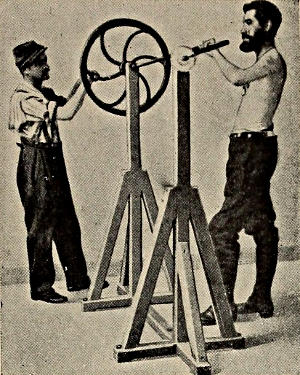
ROTATION OF SHOULDER
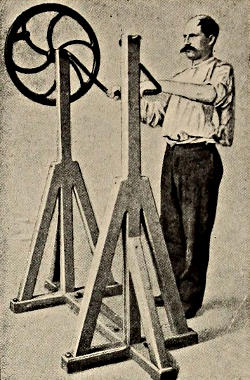
ROTATION OF SHOULDER
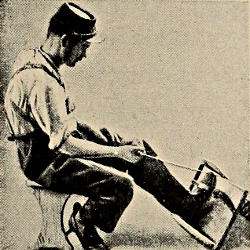
ANKLE EXTENSION

ANKLE EXTENSION
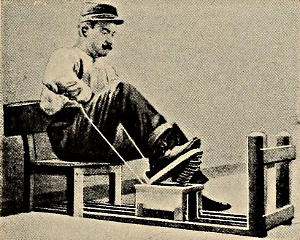
FLEXION AND EXTENSION

ROTATION OF HIP
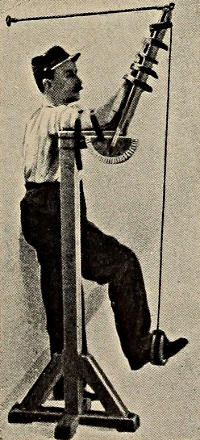
ELBOW FLEXION AND EXTENSION
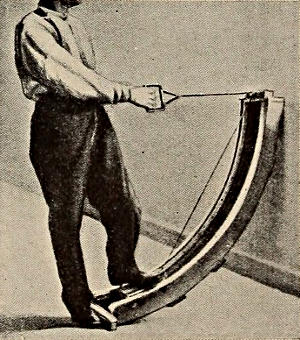
CIRCUMDUCTION OF THIGH
Favorable effects of lumbar puncture.
An accountant, 20, in the 135th infantry sustained shock from mine explosion near his trench, March 6. He was kept two days at the relief station. March 8, at the ambulance, he did not appear to understand questions and had a fixed stare. He complained of a violent headache and kept pressing his head between his hands. He kept looking about him anxiously, and the slightest noise made him jump. He would mutter a few incomprehensible words, and in reply to a question would give only the last phrase which he happened to have been saying. Lumbar puncture showed a very slight excess of albumin. Next day, he answered his name. March 12, he could speak in monosyllables, and he began to understand what was said. After the lumbar puncture, the headache disappeared and did not set in again. March 13, he began to be able to write and say short phrases. March 16, expression was good though hesitant, and the patient wrote a letter to his parents, telling about his shock. Lumbar puncture showed that the albumin was now normal. From the rear, April 5, the patient sent Ravaut a postcard in perfect form, telling how he was ready to go back to the front.
Re lumbar puncture, Imboden quotes Podmanizky as having used lumbar puncture as a method of suggestion for the cure of abasia. See also cases 560 and 561, in which Claude cured two cases of dysbasia by the device of stovaine anesthesia of the spinal cord. Pastine also has a case in which a slight improvement was produced on removal of cerebrospinal fluid, and a sudden and complete cure was brought about by the second puncture, a very painful tap. Pastine’s case is thought by him (1916) to be in part at least organic.
Bullet wound of forearm: Hysterical clenching of fist. Recovery by fatiguing the flexors.
A soldier, 28, was thrice wounded between August 18, 1914, and July 14, 1916. The third time, a bullet passed through the fleshy part of the forearm, whereupon the hand became clenched and remained so after the wound was surgically healed. As a case of war neurosis, the man was treated by electricity, massage, passive movements, and fixation in a straight splint during a period of nine months, without result. He was admitted to Maghull Military Hospital, April 18, 1917.
Two days after admission a treatment was given whose principle consists in producing a condition of fatigue in the muscles responsible for contracture. This fatigue is produced by continuous passive movements in a direction opposed to the normal action of the muscles in question. Many hours of forcible movement are sometimes necessary in the case of the more powerful muscles before the limp, toneless fatigue condition is brought about. Relays of men are told off for this purpose. Patients are got to assist in the work, particularly such as have been cured by the treatment. Also, the patient is himself told about the nature of spasms and the relief which the method will bring. This patient was told that after the flexor muscles were fatigued they would no longer be able to pull the fingers into the clenched position, whereupon the antagonistic muscles on the back of the forearm would begin to work.
The fingers were forcibly opened without interruption for six hours, in each case as soon as the fingers closed into the palm. In a few hours they began to return more slowly, and at the end of the six hours remained extended. The extended position was still found the following morning. The extensor muscles were feeble in action, but improved day by day. The spasm did not return. The patient was discharged July 2, 1917, about two and a half months after admission to Maghull. The hand was now strong and useful.
Bullet through shoulder girdle: Hysterical adduction of arm. Treatment by induced fatigue.
A man, 29, was in hospital more than two years before the Reeve fatigue treatment was applied to a functional contracture. This man had a bullet pass through the right scapula and out the pectoralis major, June 4, 1915, was (according to patient’s story) operated two months later, then further operated for drainage of septic wounds, and from August, 1915, had his arm fixed to the side, going into spasm at any attempt to move it passively. The elbow was extended and at first the fingers were tightly flexed and wrist extended. The finger flexion and wrist flexion cleared in March, 1917, and recurred in May. Electrical massage in June, 1917, yielded free movement, but the spasm returned.
The man was admitted to Maghull, June 12, 1917, that is, a little over two years after his injury. The arm sprang back to the side like a clasp knife on being released. The wrist and fingers were moved freely. Three days after admission the elbow was forcibly flexed for some hours, whereupon the spasm disappeared. Next day the arm was forcibly abducted and reabducted: for four or five hours the arm could be voluntarily abducted. Two assistants were necessary, such was the force of the adductor contraction. At the end of a week the patient was found able to lift his hand to the back of his head. There was no longer spasm.
Re abrupt treatments, amongst which Reeve’s treatment by induced fatigue may be counted, Babinski and Froment consider that abrupt treatment is far superior to slower psychotherapy combined with isolation, whether or not we are dealing with a recent or an old disease. So far as psychotherapy goes, Babinski wants to obtain a definite improvement, if not a cure, on the first application of treatment. According to Babinski, the patient’s faith in his physician’s power to cure him is most active at this first meeting, whose emotionality favors the cure.
Burial and bruises of back: Hysterical cross-legs. Treatment by induced fatigue of contractured muscles.
A man, 32, was buried by a shell and bruised about the back, August 2, 1916. He was bedfast until February, 1917. Every attempt to move the legs brought on tremors. He was then allowed up; but the attempt to walk caused one foot to knock the other, and his ankles became bruised, necessitating cotton wool pads for feet.
He was admitted to Maghull, June 12, with one leg crossed over the other and the thigh adductors spastic, especially on the right.
The fatigue treatment was carried out in dorsal decubitus, each leg being pulled by a man, and the separation repeated when necessary. Four hours a day for three days of this work finally reduced the spasm so that the patient was able to walk with assistance. On the sixth day he walked a mile without assistance. The spasm has not returned.
Re leg contractures, Bérard got successful results by continuous extension combined with injections of 1 per cent novocain into the sciatic nerve trunk and the contractured muscles. According to Babinski and Froment, there ought to be an almost certain cure of any genuine hysterical state. They quote the observations of Souques, Meige, Albert Charpentier, Clovis Vincent, Roussy, and Léri as proving this claim.
The Reeve method, so far as it is psychotherapeutic, bears a resemblance to Clovis Vincent’s first stage of what the poilu calls torpillage, namely, the stage of crisis and of intensive reëducation. But Clovis Vincent uses in his direct and forcible reëducation the galvanic current.
Bullet wound of neck: Hysterical torticollis. Treatment by induced fatigue.
A soldier, 20, had a bullet pass through the back of the neck, July 10, 1916, and returned to his dépôt surgically well October 1. A fortnight later a Zeppelin raid turned his troop out in the middle of the night, and on the morrow the man’s neck was twisted around and inclined upon the left shoulder.
Treatment followed in various hospitals, with fixation in the corrected position by plaster of Paris but without result. The patient was admitted to Maghull, April 18, 1917, with spasm of left trapezius and right sternomastoid muscles. Under hypnosis the deformity could be easily corrected. Unfortunately, it returned.
The fatigue treatment described by Reeve was started a week after admission to Maghull. The neck was forcibly straightened and restraightened upon return to its twist. In a few hours the contracting muscles had become fatigued; the neck was straight.
The next day the deformity returned slightly. The fatigue treatment was repeated. The patient was discharged well, July 2.
Burial by shell explosion: Abasia, tremors. Claw foot persistent two years cured by induced fatigue.
A man, 24, buried by a shell, February, 1915, had had a functional “claw foot” for more than two years, cured by the Reeve fatigue treatment in less than a week. According to Reeve, claw foot is perhaps the most common of the war contractures, particularly intractable, and often seen out of hospital with an “inside splint.”
After his burial this man could not walk, had tremors, was in bed for four months and on getting up showed strongly inverted foot. Three months’ splint treatment, strong faradic currents, massage, passive movements, special boots with leather wedges to tilt the foot over, were methods of treatment tried, but unsuccessful. At Maghull from November 18, 1916, he was treated by exercises, passive movements, suggestive and reëducative measures, and after a few months got about without sticks.
The claw foot continued. Toward the end of June, 1917, the feet were forcibly flexed and everted for eight hours. The deformity disappeared, but returned slightly next day. Further fatigue treatment for eight hours caused the spasm to cease permanently. He was discharged quite normal, July 20, 1917. Reeve remarks that this fatigue method might be applicable to certain hysterical contractures in civil practice.
Skull trauma over right eye: Delirium, febrile? post-traumatic? exhaustive? Operation: Epileptiform excitement. Later, explosive diathesis: Operation: Euphoria. Seizures and slight mental change.
A soldier (brother choreic, sister infantile palsy) had had measles at 13 and in his fever climbed out of bed upon a couch, fell from the couch and was found by his mother lying on the floor. He was of moderate intellectual grade, of an emotional, passionate Saxon nature and had now and then been intoxicated.
In September, 1914, he was wounded over the right eye. He did not lose consciousness but concluded that he could not get back to his own lines on account of the enemy fire. Using a knapsack to cover his head, he lay down for twenty-four hours, until rescued by a passing body of the sanitary corps who were about to leave him for dead when he called loudly to them.
He was very weak in hospital and, towards the evening of the day after receiving his injury, he must have fallen into some sort of psychotic state lasting ten days. For this he remained quite amnestic, although he was told by comrades that he had hallucinations and had scolded and yelled, hearing voices. Apparently there were situation-deliria—the call to go over the top. Temperature, which had run to 38.8, after ten days sank to normal, and consciousness cleared up.
Was this a case of protracted febrile delirium? Or of psychosis due to commotio cerebri, that is, an effect of heightened intracranial pressure? Or was it exhaustion-delirium following loss of blood, sleep and food?
But this was not the end. The wound suppurated, and in May, 1915, eight months after the injury, operation was performed to relieve this abscess. Temperature immediately rose to from 38.4 to 38.6, the fever lasting three days, and a second psychotic phase with complete amnesia entered.[700] He went into this phase immediately after recovering from the operative narcosis, looking wildly about and cursing the sister. The patient was violently excited and was put in a straight jacket on the second day. This phase may be regarded as one of epileptiform excitement with delirium. The operation may have played a part in the psychosis.
There were no further psychotic phenomena which could be attributed in any way to commotio. There were, however, attacks of cortical origin and emotional seizures. The patient became emotionally excitable and lost all inhibitions against expression of emotion, such as crying. Once he actually tried to suppress his emotion with a noose about his throat. He became seclusive and withdrew within himself—a victim of Kaplan’s explosive diathesis, or of Bonhoeffer’s emotional hyperesthetic defect condition.
A second operation was performed in September, 1916, to loosen the brain scar, and a large splinter of bone was removed. During the operation, under local anesthesia, there was a severe cortical seizure with complete disappearance of the reflexes. Ether was then administered. Later, in the same day, there were several minor cortical attacks.
After this operation the man’s emotional status changed; he was no longer irritable or exclusive, but became slightly euphoric and contented. He received during the next two weeks four tablets of Sedobrol and for a long time thereafter two tablets daily. There were never any phenomena of bromidism or any suggestive effects of the bromides.
The first attack after the second operation came in November, 1916, and was followed by slight dysarthria. Repeated attacks followed which were attributed to contractions in the scar. Accordingly, a third operation was performed and an attempt was made to bridge over a defect in the right frontal bone. The man’s emotional status remained good after the operation, but further attacks appeared six weeks later and there were spells of dizziness. Occasionally, in process of thinking, he said something stuck in between his thoughts. Sometimes thinking broke off sharply as if he had cut through a wire with an electrical current in it. There was a slight reduction in attention and a slightly increased fatiguability.
Hard service; shell explosion with loss of teeth: Vomiting. Cure by restoration of self-confidence.
A married reservist was called up at the outbreak of the war and went through Mons, the Marne, and the Aisne and was finally blown up by a shell at Ypres. Early in November, 1914, he lost his speech but got it back in time to get home for Christmas. A number of teeth had been lost in the injury. Vomiting began first in England. While on leave at home he vomited at every meal. Asked whether it was his food or his thoughts, he said, “You are quite correct, Sir, you know I have always been with thinking.”
Under medical care, June, 1915, he was found suffering from hesitating speech, general tremulousness and emotionality. He worried a great deal on account of money matters at home. He lay awake thinking. A child became ill and died, and all the while he got worse, “thinking all the time.”
It was explained to him that the vomiting was a matter of emotions. The lost teeth were replaced by false ones. As he began to get control of his emotions, he vomited less and increased in weight. Finally he was boarded for discharge and was sick again on the day of the meeting. A fortnight later when sent to sign discharge papers he vomited once more.
According to McDowell, the vagus may possibly be incriminated as a cause of these gastric disturbances. Practically, the vomiting is a result of emotional stress. The cure is to produce insight on the part of the patient, the removal of worry and the restoration of self-confidence.
Michell Clarke cured such cases with milk diet.
Roussy and Lhermitte find hysterical vomiting to be relatively common and as a rule without difficulty in diagnosis; but they remark that there is often some underlying organic condition to be sought for and treated after the neuropathic element has vanished. They remark, also, that there is no tendency to spontaneous cure of the disease. They advocate a strict dietetic régime and psychotherapy.
Cure of self-accusatory (“started retreat from Mons”) and other delusions by “autognosis.”
Capt. William Brown, in the discussion at the Section of Psychiatry of the Royal Society of Medicine, January 25, 1916, speaks of a method of treatment which he calls autognosis—a method of giving the patient self-knowledge, by revealing to the patient through his own confessions the cause of mental change leading to his symptoms. One of Brown’s examples is that of a sergeant in the firing-line during the retreat from Mons. He was admitted to Maghull with the delusion that people thought he had given the signal for the retreat from Mons on a silver whistle, a shooting prize of his. German officers used silver whistles that made a note like his own. In fact, he had other like delusions, such as that people thought him responsible for an Edinburgh railroad accident in connection with his troop-train. A German spy might have heard this.
In the process of procuring autognosis, Capt. Brown found that at the age of 12 this man had been falsely accused of stealing pork pies from a shop, and had been brought before a magistrate. In point of fact, he proved an alibi, but he was greatly worried by the charge. According to Capt. Brown, this incident of the insistence of the false accusation was the beginning of his tendency to delusions. In two months’ time there was a remarkable improvement.
Re psychoanalysis, autognosis and various modifications, Forsyth remarks that when the acute stage is passed, the Shell-shock case becomes an everyday neurosis in which war experiences are merely the latest phases in the patient’s life, and that psychoanalysis may then become necessary. Eder regards the “mechanisms” of what he terms “war shock” as the Freudian mechanisms of hysteria, and has commended psychoanalysis for a few cases, preferring hypnotism for acute cases. Adrian and Yealland decry psychoanalysis on the score of time limitations.
There were three Zouaves in a first-line trench north of Arras, January 14, 1915, who were blown up by a bomb thrown from the enemy trench some hundreds of meters away, by a mortar, a crapouillaud. This projectile burst with a great noise, louder than that of a bomb, and made a very strong windage. A dozen men were blown under the trench wall, just after entering the trench; two were killed; and the others, most of whom had been buried to the neck, were pulled out and carried, trembling, to the nearest relief post. Two of the three Zouaves were bleeding at nose and ears, and all three were absolutely deaf and mute. Evacuated to an ambulance, and thence to Paris, they arrived at Val-de-Grâce, January 17, that is to say, three days after the shell burst. They communicated with the attendants by signs; one got hold of paper and wrote several hours in the day rapid notes about the accident. However, hysteria or pure simulation was suspected in these three Zouaves, and they were placed in small separate rooms. They were informed through the physician’s remarks to his staff that these were cases of nothing but simple nervous shock such as we had often observed, and the claim was made that they would be completely well either on the morrow or the day after.
On the morrow, two of them partially recovered hearing and got back their voices. They became loquacious and began to tell about the battle. The day after, the third patient began to speak. Two of them showed traces of auricular hemorrhage, and in fact, actual ear lesions were found in all three. One had a suppurative right middle ear, with perforation; another had both drums perforated and a suppurative middle ear, also on both sides. The third, who recovered his speech after the others, had perforation of the left tympanum with a little suppuration of the right ear tympanum and a slight tear of the right tympanum. In April, 1915, the hearing was cured.
These men had been under fire several months, and had taken part in the battle of the Marne. It was not a question of their first baptism of fire, and in fact, each of them had been previously wounded. According to Roussy, the story is, that the shell-burst produces by displacement of air tympanic perforation, and at the same time a violent nerve shock with loss of consciousness for a few minutes. The men come to, but the ear lesion, probably exaggerated by the nervous status of its bearer, creates a complete bilateral deafness. This deafness produces an absolute hysterical mutism.
Re case groups of war neurosis, several writers speak of dangers of contagion, but also emphasize the values of contact of patients with one another in the securing of therapeutic results. What Mott has termed the atmosphere of cure was no doubt present in the three instances of Roussy just cited. The cure of one may act heterosuggestively to produce the cure of a second, and so on. Functional deafmutes are somewhat refractory as a rule. H. Campbell states that there is some danger attached to allowing large numbers of functional cases to consort together too closely. He suggests making use of small wards and screens, and a process of sorting out patients so that they shall not affect one another injuriously. Steiner especially stresses the value of individual rooms in preventing psychic infection, of which, he says, the danger is large in open dormitories. The psychic contagion is as a rule that of hysterical seizures and tremors; but complaints about faulty hospital arrangements are also readily spread. Steiner advocates never questioning a nervous patient concerning his troubles in the presence of other soldiers. To reach 60 to 70 patients, Steiner had one examining and treatment room. Roussy’s institution at Salins in 1917 had a service limited to traumatic hysteria, from which, in three months’ time, 200 subjects had been discharged cured (see Boschi).
Dysentery: Milk diet persisted in: Vomiting, incontinence, inability to walk. Cure by persuasion.
A soldier, 25, a low menial when war broke out, developed “dysentery and gastritis” at the Dardanelles, although even before the dysentery his nerves had gone bad. He had diarrhoea and vomiting, was sick every day, found himself unable to walk, and found himself always wet with urine dribbling day and night. Arriving in England and treated in a hospital, he still had vomiting. He had lived on milk and custard and been kept in bed.
Capt. McDowell convinced the patient that his legs were not as weak as he supposed. He was encouraged to walk, put upon light diet and then upon ordinary diet. He became an active worker in the ward, later going for five-mile route marches. Two months later he went back to duty in good health, weighing seven pounds more than before. This man was weakminded and, when his dysentery was cured, did not dare to start eating ordinary food. He was a victim of hospital régime. Individual attention would have obviated much of the subsequent state.
Re vomiting, see remarks under another case of McDowell (Case 495).
Re incontinence, see Case 384, of Guillain and Barré.
Officer dies in convulsions: Servant develops hysterical convulsions, which vanish on being explained as such.
An officer and his servant were blown up by a shell. The servant ran to fetch a stretcher for the officer, to whom he was much attached, but on his return the officer made a few convulsive movements and died. Immediately after, the servant had a fit. During the next two months he had eleven more. Hurst made a diagnosis of hysterical fits resulting from emotion, explained his idea of their origin and nature to the servant, and the convulsions then ceased completely.
Re hysterical convulsions, see remarks under Case 443.
Course of a case with crises of trembling.
A soldier in the artillery, who had been in the lines from August as a kitchenman, looking after the food of the first line trenches, with which his shelter was connected by communication trenches, 800 meters away, was on January 17, 1915, with three other men placed in the shelter kitchen of the trenches but a short distance away from the French artillery. The firing passed over the heads of these men but they could feel the windage, which obliged them to lie down each time. The evening of that day, several hours after firing had ceased, the kitchenman had a shivering spell, with trembling that lasted all night; after which these crises came on every day. He had finally to be evacuated to the rear.
According to Roussy, such patients always have neuropathic taint and a history of previous crises. Such a patient ought to be handled with rather severe discipline. In this way, according to Roussy, the reappearance of a severe attack of convulsions can be prevented. But these patients cannot go back to the front.
Re tremors, see Cases 224 and 225.
Two cases of lameness cured by persuasion: Russel.
A man on crutches, paralyzed completely in the right leg, partially in the left, developed paralysis in the right arm from the use of the crutch. There were marked vasomotor changes in the right leg and arm together with anesthesia to pinprick. Assured that he could move the legs perfectly he said that he had tried and failed. After a persuasive talk in private he began to use the arm, and to walk perfectly. It seems that in the trenches he had a sharp pain in the right knee, after which he did not use the leg and it gradually became more and more useless. It had been paralyzed for three months. The reason he did not use this leg was not on his own account, but on account of his mother at home. He seemed really grateful for the cure.
A sergeant in hospital for a year for shell-shock still had a marked shaking of the right leg whenever he raised it from the ground. He walked in leaning on a silver headed cane. The functional nature of his shaking was explained to him by Russel, whereupon he walked out normally saying he could do without his cane. Russel suggested that crutches and sticks thus given up were often donated to the shrine. The sergeant whose cane must have cost at least three pounds beat a hasty retreat carrying the cane in front of him.
Re Russel’s general point of view concerning malingerers and psychogenic cases, see under Case 458.
Hard patrol work: Delirium; head tremor augmented by excitement: Virtual recovery on bandaging neck, isolation, open air, to-and-fro transfers to mental and nervous wards.
A metal moulder in civil life, 29, in military service 1907 to 1909 (no hereditary taint, moderately good scholar), became unconscious for a half hour after taking a cold drink following a somewhat long practice march, at some time during his first year of military service.
He was in several skirmishes in Belgium and Northern France early in the war, being once surrounded in patrol work (November 11) by Turcoes and Zouaves. There was a lively exchange of shots, in the course of which five of the eight men on patrol fell. The three survivors hid themselves for three days in a quarry, and on the fourth were found by the advancing troops, and immediately went into battle.
But during a pause while on the point of taking coffee, the man suddenly fell sick, tried to carry on, but lost consciousness and apparently remained unconscious for about three-quarters of an hour. It seems that he raved and shouted and tried to bite his fingers, being held with great difficulty by several comrades. He was removed to a dressing-station three km. distant.
At the dressing-station, his head began to shake, although he was unaware of this until his attention was called to it by his comrades. He said that he felt restless and that his head ached almost continually. He was carried to the reserve hospital, and from thence, December 9, 1914, to the nerve hospital at Jena, where he was unaware of the shaking of his head (which had now lasted for three weeks), and said that he felt a thick fog in his head (to say nothing of headaches), and was only free and clear in his head while standing in the open air.
His sleep was restless and poor; there were war dreams almost every night. In the process of getting to sleep, his arms and legs frequently twitched. He would soon tire and feel weak. Also since his dangerous experience, he had noticed a change in his speech: always fluent before, it was now hard for him to speak because one had to exert one’s head so much in speaking.
This head tremor was in fact the most marked symptom of his illness. It would increase on every active motion of the head, but ceased almost entirely when attention was diverted. The head would then be held bent to the right.
During emotional excitement, the shaking spasm would spread over the entire upper part of the body, but would remain more severe upon the right than upon the left side. The forearms would fall into a lively shaking movement of pronation and supination. The hands and fingers would be attacked by a less marked tremor. After calm had set in, a fine tremor of the right hand would remain plainly noticeable. The musculature of facial expression would frequently fall into spasmodic movement, the left corner of the mouth twitching, the lips set for whistling, or the upper lip making movements as if snuffing spasmodically.
Physically the man was of medium height, strongly built, with adherent lobules, and a somewhat pointed skull. The teeth were defective and irregularly placed. Both deep and skin reflexes were increased. Marked dermatographia and mechanical excitability of the muscles: periosteal reflexes strongly developed; numerous pressure points in the head. The right temple and back of the head were painful on percussion. The patient showed no disturbance in touch and pain sensibility. Outstretched tongue showed marked fibrillary twitching; speech was difficult, being slow, awkward, stumbling, and sometimes hesitating (suggesting the speech of general paresis). At other times, the speech was of a peculiar sighing, tremulous nature, reminding one of the speech of children complaining or asking for pity. Rest was secured by injections of salt solution. A few days later, the treatment was continued by a bandage about the neck. After this the tremor grew slighter and would even remain[710] absent for some hours. The patient was told to rest in bed and not to speak much; being “seriously ill,” he was kept alone. He was often irritated, querulous, and subject to outbursts of profanity. He took food well and slept well, receiving sodium bicarbonate.
The bandage was changed after five days. The tremor was very marked. The patient was furious because visitors were refused to him. He was especially angry with his nearest relatives and his betrothed, and wrote defiant letters to all of them. He became one of the most troublesome patients in the psychiatric division of the hospital. He complained sometimes of anxiety and feelings of unrest. He received treatment by pantopon. He continued to be a very disagreeable patient, feeling himself opposed and not properly considered. He thought himself seriously ill, behaved much like a spoiled child, and was of the opinion that he would not get well in the hospital because they were grieving him so. His appetite became bad; he complained of pains in the loins and of rheumatism in the legs. A cord was found hidden in the bed. The patient expressed suicidal thoughts at various times.
At the beginning of January there was marked improvement. The headshaking ceased almost entirely; the patient walked in the garden some hours daily. However, in the middle of January, on refusal of furlough, the head-shaking began again markedly. At his request a bandage was placed on the head again for a few days. He seemed emotionally very tender; his head would shake at the sight of a dead rabbit.
He was transferred to the nerve division of the psychiatric clinic at the end of January. He had recently begun to complain of flickering before the eyes. The ophthalmologists established an existence of a choroiditis disseminata. The eye examination had a markedly depressing effect upon the patient, and the shaking spasm of the head appeared again. Upon being told that he would have to be sent back to the psychiatric section of the clinic, the shaking immediately disappeared (24 hours after it had begun).
Thereafter slow improvement followed. He stayed in the open a great deal and walked. March 2, he showed a vehement[711] outburst of anger, quarreling and using violence with a comrade. He was brought back to the psychiatric section, and in transit had a severe hysterical attack with unconsciousness, crying fits, and stepping movements of the extremities. He was promptly taken to a section for those seriously ill. The next day, upon his assurance that he could control himself, he was put in a more quiet division. He began to take part in gymnastic exercises, worked as a coachman, and then as an experiment was sent to a gentleman’s estate for recreation. At last accounts he was feeling well except that he occasionally had headaches during work. He could not work so hard as before on account of the rapid onset of fatigue, especially when working in the sun. The head-shaking recurred but seldom and lasted for a few hours only when the patient became angry or when there was much noise about.
Rationalization of war memories: Returned to duty.
A young English officer was wounded just as he was extricating himself from burial in a mass of earth. He became nervous and sleepless and lost his appetite. After the wound had healed, he was sent home on leave, which had to be extended as he got worse. An out-patient in London for a time, he was finally sent to a convalescent home, still troubled with insomnia, battle dreams and concern about his recovery. He made light of his condition and was on the point of being returned to duty by the medical board, when his sleeplessness led to his being sent to Craighlochart War Hospital.
He could not sleep without a light in the room, else every sound attracted his attention. He tried hard all day long to banish all unpleasant and disturbing thoughts, but at night it took him a long time to get to sleep and then came vivid dreams of warfare. He did not, himself, feel that he could ever forget the war scenes.
Rivers, in general believing that the attempt to banish such experiences absolutely from the mind is poor psychotherapy, narrated his views to the patient. Rivers advised him no longer to try to banish the memories, but to try to transform them into tolerable, if not pleasant, companions. The war experiences and anxieties were talked over. That night the man had the best night he had had for five months, and during the following week the sleeplessness was no longer so painful and distressing. If unpleasant thoughts came, they had to do rather with home life than with the war. General health improved; insomnia diminished. He was at last able to return to duty.
Rationalization of war memories.
An English officer was buried by shell explosion and developed severe headache, vomiting and disorder of micturition, yet remained on duty for more than two months. Collapse came when he went out to seek a fellow officer and found the body blown to pieces, with head and limbs severed from the trunk. This vision haunted him in dreams. Sometimes the officer appeared as on the battlefield; again as leprous. The officer would come nearer and nearer in the dream, until the patient woke pouring with sweat and in utmost terror. Accordingly, he was afraid to go to sleep, and spent all day thinking painfully about the night to come. Advice to keep all thoughts of war out of mind merely brought the memories in sleep upon him with redoubled force and horror.
Rivers’ therapy was to draw attention to the fact that the terrible mangling proved conclusively that the officer had been killed outright and without pain. The officer said he would now no longer attempt to banish the thoughts and memories of his friend, but would concentrate on the pain and suffering his friend had been spared. No dreams at all came for several nights, but one night in his dream he went out into No-Man’s-Land and saw the mangled body, but without horror. He knelt down, as he had in the original experience, and woke as he was taking off the Sam Browne belt to send to the relatives. A few nights later came another dream in which he talked with his friend. There was but one more dream in which horror occurred.
Rationalization of war memories: Eventually unfitted for military service.
A young English officer, after doing well for a period, was rendered unconscious by shell explosion. The first thing he remembered was being led by his servant towards his base, thoroughly broken down. He had headaches, sleeplessness, war dreams and spells of terrible depression appearing with absolute suddenness, unlike ordinary “blues.” For ten days in hospital no such attack appeared, but one evening he came to Rivers pale and anxious. A few minutes before, he had been writing a letter in his usual mood, when this causeless depression came on. In the afternoon he had walked about on some neighboring hills. The letter dealt with no depressing matter. In ten minutes the depression vanished. Nine days later another came as he was standing idly looking out of a window. The attack lasted for several hours, as no physician was present to meet the issue. If he had had a revolver he would have shot himself.
Rivers was inclined to interpret these gusts of depression as due to a forgotten but active experience. As there was no definite tendency to dissociation, Rivers hesitated to plunge in with the hypnotic method, nothing short of which, however, served to recall the incident. The man was gravely apprehensive about fitness for further service, and was repressing his fear, as he thought it either was cowardice or would be called cowardice. The patient, by his discussions with Rivers, had already become familiar with the idea that the gusts of depression might be due to a submerged experience. Perhaps, however, there had been no experience, and the patient was advised that possibly the thing repressed was the idea about fitness for service. Accordingly, the patient agreed to face the situation. One transient attack of morbid depression occurred, after an operation. Then the man fell into a state of anxiety neurosis such that he was passed by a medical board as unfit for military service.
Rationalization of war memories: Commission relinquished.
An oldish English officer lost consciousness while looking at the havoc wrought by shell explosion. Probably there was a second shell that sent him off. He was eventually admitted to an English hospital with paresis and anesthesia of legs, severe headache, sleeplessness and terrifying dreams. Hypnotic drugs and advice neither to read nor to talk about the war were the measures adopted and after two months in hospital he was given three months leave. He buried himself in the heart of the country, away from relatives, with aspirin and bromides. He began to sleep better and had less headache. When the president of the medical board asked a question about trenches at the end of his period of leave, however, he broke down and wept. He again repaired to the country for two months’ leave, for the chosen treatment by isolation and repression.
An order was then given that all officers must be either in hospital or on duty. He was sent to an inland watering place and treated by baths, electricity and massage, whereupon he rapidly became worse, especially as to sleep. He was transferred to Craiglochart in an emaciated state, with an expression of anxiety and dread, paresis of legs, sleeplessness and war dreams.
He was now advised to give up repressing, to read and talk a little about the war, and to accustom himself to thinking about war experiences. He did this but half-heartedly, as he thought the ideal treatment was what he had so long followed. Nevertheless, he got distinctly better and the content of the war dreams was altered to home scenes. He was still loath to acknowledge his improvement and thought that he would have recovered if he had not been taken from his retreat and sent to hospital. As it was obvious that he would be of no further use in the army, he was allowed to relinquish his commission.
Rationalization of war memories, without redeeming feature as nucleus.
An English officer was flung by shell explosion so that his face struck the ruptured and distended abdomen of a dead German. The officer did not immediately lose consciousness and got distinct impressions of taste and smell and an idea of their source. After a period of unconsciousness he came to, vomiting and much shaken. He carried on several days, still troubled by vomiting and haunted by taste and smell images. Several months later he was observed by Rivers suffering from horrible dreams, in which the battle experience was faithfully reproduced. He got no relief except when he went into the country, far from every suggestion of war. Rivers’ psychotherapeutic plan of finding a redeeming feature in the experience, upon which the patient might concentrate, failed because there was no redeeming feature. Accordingly, it was thought best that the man should leave the army and seek the conditions that had given him slight relief.
Re psychoanalysis and its modifications, see remarks under Case 496, under which several favorable opinions were mentioned. Boschi in his report on French conditions gives no reference concerning psychoanalysis or hypnosis. Bruce has found blended with the war dreams many episodes quite alien to the war, and considers that the patient’s ante-bellum history is of importance, since ante-bellum emotions may be revivified by the war. Craig states that he has not been impressed favorably by the results of psychoanalytic treatment. Arinstein from Russian experience gives preference to Dubois’ psychotherapy over hypnosis and psychoanalysis. Nonne states that the data of the war prove that hysteria is neither a degenerative disease according to classical theory, nor a disease based upon Freudian principles.
Post rheumatic “paraplegia” (or abulia?) cured by removal of crutches, after question of discharge “unfit” had been raised.
A soldier, 23, had fever with swelling of several joints and temperature in 1915, and was furloughed to England. He complained of pains in the limbs and shortness of breath, and was put in hospital. As he did not improve, he was sent to a special hospital for baths and electricity. There he remained from August, 1915, to March, 1916, with D’Arsonval baths, cataphoresis, electric treatment and massage.
He was now sent to the second Northern General Hospital to see whether he should be discharged permanently unfit. Here he shuffled along on two crutches, very tremulous, and sweating, and suffering from palpitation on exertion. He wanted to take poison if he could not be cured.
The crutches were taken away. He was asked to walk up and down. He had to be supported at first and fell several times. The exercises were continued. Massage and drugging were stopped. The next day he was able to stand alone. In twenty-four hours he walked by himself. The other patients in the ward encouraged him on account of the genuine exertions he was making to get well. April 7, he returned to duty, smart and well set up.
Babinski and Froment always give the suspected subject the benefit of the doubt, never uttering the word simulation in the presence of the soldier, and proceed to psychotherapy; for psychotherapy will act to cure simulation or exaggeration just as it acts to cure hysteria. They say that in their experience, all these disorders of doubtful nature—that is, that lie diagnostically between hysteria, exaggeration, and simulation—are as a rule cured by resort to psychotherapy provided that the due amount of energy, tact, and perseverance is employed. See also remarks under Case 453. Veale’s case (511) never showed mauvaise volonté, and nothing more than aboulia.
“Trench foot,” “neuritis,” a year of astasia-abasia or at least of complaint of inability to stand or walk. Treatment by a “cruel though justifiable” process.
A regular army man, 38, well built and muscular, in Flanders the first winter, returned to England in January, 1915, with “trench foot.” “Neuritis” then developed, with loss of power to walk. Baths, electricity, massage, sympathetic wheeling about in a chair by women, all failed.
January 11, 1916, he still complained of inability to walk or stand. The reflexes were exaggerated. He was able to get into a wheel chair from bed by jerks, associated with palpitation, tremors, flushing and sweating.
He was told that he had now recovered from the neuritis. Crutches, sticks and wheelchair were removed. He flopped about and then lay on the bed exhausted. In a few days he began to shuffle about and was put on the stationary bicycle. January 29, he left the hospital well, remarking that though the treatment at first seemed cruel, it was fully justified.
Re genuine polyneuritis, Mann gives German experience regarding neuritis as somewhat frequent and affecting a special form which he terms polyneuritis neurasthenica. He states that the commonest instances of mononeuritis developing in the war are the sciatic and trigeminal. The neuritis often outlasts the other symptoms. The treatment was rest, tepid baths, and electricity. Naturally, alcohol and syphilis must be excluded in the diagnosis.
Nonne also described non-alcoholic, non-syphilitic, and non-infectious polyneuritis in neurasthenics, which he, however, finds most common in the ulnar, median, radial, anterior crural and posterior tibial nerves.
Re “spa” treatment, Turner thinks there may be easily too much massage, electricity, bathing. He prefers segregation in special hospitals to “spa” measures in general hospitals, prefers occupation to rest, and calls attention to the stimulating value of the gratuity to be paid on leaving the hospital.
Shell-shock paraplegia: Treatment by bed, cigarettes and chocolates altered to isolation, no tobacco, no visitors, faradization. Recovery.
Early in the war, a lad, 19, was blown up by a shell. He was sent home paralyzed from waist down, and was seen by Capt. Buzzard after he had spent ten months in various hospitals, “carefully nursed, on the water bed, constantly using a bed urinal, smoking innumerable cigarettes, and eating countless chocolates.” He could not move his legs. They were wasted and flaccid. The knee-jerks could be got with difficulty. Plantar reflexes flexor. Complete anesthesia from umbilicus downwards, but preservation of abdominal reflexes. The navel did not shift downwards when the patient attempted to sit up. The incontinence was not real; urine was passed into the urinal at appropriate intervals.
Buzzard directed treatment “not to his spinal cord but to his mind; isolation; the stoppage of tobacco and all visits; the assurance that he would rapidly get well, together with some suggestive faradization of his legs.” This brought about a cure in a very short period. The atrophied legs eventually grew strong enough to walk.
Re cigarettes in Shell-shock, Mott decries the over-liberal gifts of cigarettes that induced cigarette habits in both officers and men. Of course, the cigarettes are still more detrimental to cases of soldier’s heart than to other cases of neurosis. Mott remarks how over-frequent are the social tea-parties, joy rides and drives given by well-meaning ladies for the “poor dears,” actually perpetuating neuroses.
Re atrophy, Babinski and Froment again bring up the question whether muscular atrophy can be brought about by a hysterical motor disorder. In point of fact, Charcot and Babinski were the first to describe the true hysterical amyotrophy, but this hysterical amyotrophy is exceptional in hysterical paralysis, and is slight when it occurs.
Shell-shock blindness, mutism, deafness: Blindness spontaneously vanished, 24 hours. Mutism, 2-3 months. Deafness cured by “small operation.”
A lance corporal, 26, became blind, deaf and dumb, though without losing consciousness, when blown up by a shell, August 29, 1916. His sight returned next day. On reaching England he talked in his sleep. Encouragement, electricity, etherization failed to effect improvement. One night in November he woke up and asked the sister for a drink; thereafter he talked normally.
Seven months after the shell explosion he was transferred to the neurological section at Netley, March 21, 1917. Deaf to air and bone conduction, a loud noise behind him caused a slight tremor of hands, with blinking and dilatation of pupils; but further stimuli of the same sort failed to produce such reactions. Normal nystagmus and giddiness on functional tests of vestibular nerve and canals. The internal ear was then probably free from organic changes. Since shell-shock mutism is always hysterical, it was probable that the deafness was hysterical. Under hypnosis (staring at lines for fifteen seconds) he showed no change. During natural sleep, also, a shout of “Fire” and metallic noises failed to wake the patient or to produce contraction of eyelids. Electric suggestion (despite the patient’s belief in electricity) and reëducation failed.
April 16, he was told that a small operation would have to be done April 20. To this he readily consented. Two small incisions were made behind the ear under light ether and suture was inserted. A loud noise was made during the “operation”; he heard this noise and jumped from the table. To his intense delight normal hearing returned in a few minutes. Next day hearing was tested and found normal to air and bone conduction. He was discharged to duty three weeks later and on his way to France, June 29, demonstrated his normal hearing to the physicians.
Deafness: cure by stimulating vestibular apparatus.
A private, 20 years of age, lost speech and hearing after the battle of Neuve Chapelle. Eight days later he came under the care of the laryngologist in a very excited state, pointing to lips and ears and carrying a note with information concerning his deafmutism.
Dr. O’Malley wrote on a piece of paper that he would restore the patient’s speech and hearing. Dr. O’Malley then used the mirror until the point of retching, and wrote, “You can speak now; count up to ten loudly.” He did.
Dr. O’Malley next used the cold water douche to the right ear to the point of giddiness, then shouting through a speaking-tube (see description below). The patient then found he could hear and the tears streamed down his face. Thereafter he was able to converse freely. Dr. O’Malley writes:
The treatment of functional deafness consists in exciting the vestibular apparatus as follows. Cold or hot water is allowed to flow in a steady stream into and out of the external auditory meatus by means of a tube attached to a receptacle placed about one and a half to two feet above the patient’s head and continued until he becomes very giddy and an active nystagmus is produced. A speaking-tube three feet long is then used by placing the ear-piece in the ear so treated, and the surgeon shouts into the mouth-piece the assertion, “You hear now,” and the answer, “Yes” comes promptly. The tube is now dropped and a conversation held as if no deafness ever existed. So far I have found the treatment of one ear sufficient. The patient is usually very emotional, as the disturbed vestibular function, which in these cases responds easily and markedly, causes him to feel as uncomfortable as a bad sailor on a stormy voyage. This feeling, however, rapidly gives way to one of pleasure at the return of his hearing. Where functional deafness and mutism co-exist it does not appear to be material which is treated first. In two cases of this kind under my care I treated the loss of voice first.
Bullet through mouth; Hysterical mutism. Treatment by operative manipulation.
A Colonial infantryman, 32, was wounded December 17, 1914, at the Boisselle, being struck by a bullet which entered on the right side in the upper part of the neck and came out behind the left side of the mouth, having traversed the tongue, broken two teeth, and caused a good deal of hemorrhage by mouth. The patient felt his tongue swell, and from this time on he could not pronounce a word. He was sent to the ambulance, then to Mien, then to Saint Germain, and finally to Morestin’s surgical service. With wounds by this time healed, the patient found it hard to open his mouth. There was no trace of fracture of the lower jaw. The tongue could be only incompletely examined. The man swallowed liquids easily but could take no solid food. He tried hard to speak, made pantomime movements, grew emotional and lachrymose.
On the whole, however, it seemed that his inability to articulate sound could not be due directly to the lesion. There must be either simulation or hysteria. For four days he was attentively watched, and not once did he pronounce a word. He grew more and more stricken and humiliated by his plight. Rigorous diet did not cause his mutism to cease. Isolation and ennui did not decide him to talk. Accordingly, it was announced, in the man’s hearing, that an operation was to be done to restore speech. January 9, 1915, his face was copiously washed with alcohol and ether. Cocaine was injected to secure anesthesia and resolution of the muscles of mastication. Six c.c. of a 1-100 solution on each side. Shortly the surgeon began to open the jaws, against decreasing resistance. The tongue, which was not spastic, was seized with a tractor and rhythmic movements were executed with it. After a few of these movements, joy was painted on the features of the patient. He said that he wanted to speak and that he was about to speak. He shook[723] the surgeon’s hands effusively and said, “Merci.” Although the first words came hard, little by little speech became free and a perfectly sincere elation at having recovered speech set in.
This man was neuropathic, having always been a rather strange, irritable and restless person, and given to nervous crises in anger, in which he lost consciousness entirely.
Re pseudo operations as forms of disguised persuasion, almost countless methods have been used. See Cases 514, 515, 518, 519, especially 521, 560, 561. Sham injections under ethyl chloride have been made (Goldstein). See also under Case 484, re continuous bath, and under Case 488, re lumbar puncture. Very close to these methods are the methods of torpillage of Vincent and the methods employed by Yealland in England and Kaufmann in Germany. See under Cases 574, 563, and 564, and 570.
Léri quotes Babinski as saying, “We cannot fight hysteria in trench warfare; manoeuvres are necessary.”
Re treatment of mutism, Chavigny remarks that the principle of treatment for mutism is quite different from the principles of treatment of paralysis. The reëducation of mutism is psychic. Chavigny claims probably absolute success in the treatment of mutism through faradism to the larynx region simultaneously with a signal given to the patient to make an effort to pronounce the letter A. Garel modifies the treatment (in case the faradic apparatus is not at hand), by a vigorous and sudden blow to the patient’s epigastrium simultaneously with the patient’s endeavor to imitate the movement of the doctor’s lips.
Shell-shock: Impairment of vision (even commanded men to fire on kindred troops!) Improvement by verbal suggestion, faradization, injections.
A sergeant-major, 29, in private life a bookkeeper, said that shrapnel struck the ground in front of him and burst as it struck. Unconscious for a moment, the sergeant-major thereafter saw everything imperfectly, led his men in the wrong direction, and even commanded them to fire in the direction of his own troops.
Seven days afterwards the eyes looked normal, fundi were normal, vision was reduced to the perception of hand movements; with a plus 10 sphere the right eye could count fingers at 5 c.m. and with a plus 8 sphere the left eye could count fingers at 3 c.m. There was a right frontal analgesia.
Treatment: Sweating; rest in bed for several weeks; assurance of complete recovery. There was a slow but constant improvement, aided by faradization and injections of strychnine sulphate into the temporal region, but the prospect of a return to the front retarded the improvement.
Re injections into the temple, see also Case 521 of Bruce. Re cure of blindness, Grasset has a case of a blind deafmute who was cured by a nurse. She put a pencil in his hand and guided the pencil while she wrote a question. The patient replied in very good MSS. In blind deafmutes sight is described as returning first, hearing next, and speech last.
For other cases of blindness, see especially under Section C, Cases 433 to 438, with discussions thereunder.
Re retardation of improvement by the prospect of further military service, Lewandowski has insisted upon the strong factor of the wish in all such functional conditions. Lewandowski wants all functional cases, however, to be sent to duty in the rear or to be discharged as unfit.
Aphonia: manipulation in larynx.
A corporal, 28, had a bullet pass through his neck from a point in the middle line at the upper border of the thyroid cartilage to a point behind the right sternomastoid muscle, two inches below the point of entry. The corporal lost his voice at the time of injury, spat up a teaspoonful of blood, and thereafter was able to whisper only. The laryngoscopic examination betrayed no intralaryngeal lesion. Treatment as described below enabled the patient to speak. O’Malley describes his technique as follows:
The patient is placed in the common position for the examination of the larynx, the tip of the tongue being seized in a piece of linen by the left hand fingers and the laryngeal mirror introduced with the right hand. The patient is then requested to say “e” or cough, and if the cords do not approximate, they can be made to do so by using moderate friction on the fauces and pharynx with the mirror to excite secretion. The latter begins to drop into the larynx, and acting as a foreign body, a protective reflex is at once excited which adducts the cords to prevent the secretion from entering the trachea. At the same time an involuntary cough is produced to expel the mucus, and if the friction and flow of secretion are maintained and the patient is urged to cough vigorously, voluntary coughing and a tendency to retching with forced laryngeal notes will rapidly follow. It is usually best to persist until retching occurs, as the cords are then forced together to protect the larynx and trachea from the possible entrance of regurgitated stomach contents. Involuntary laryngeal sounds are thus produced and the patient is conscious of laryngeal effort. Some of these cases are at the moment very shallow breathers, which can be demonstrated by X-ray screening, but the act of retching causes a wide excursion of the diaphragm with a more pronounced expiratory blast, to be rapidly followed by deeper inspirations. This method of treatment is best carried out just before a meal, as the stomach is then practically empty and the unpleasant effects of the sudden regurgitation of food are avoided. When the[726] explosive sounds accompanying retching have occurred two or three times the mirror is withdrawn, the tongue released, and the patient is requested to swallow, take a deep breath, and cough, and then urged to count up to ten, directing his voice to a certain point on the ceiling. This method has given me uniformly good results, and was rapidly effective in all cases coming under treatment soon after the onset of the neurosis.
Re methods for curing aphonia, Muck has a method called the “ball” method. A ball is put into the larynx to cause a temporary suffocation, which produces a reflex that starts the adductors. He would apply the method as soon as the man was well over the shock that produced aphonia. Muck states that he has applied the ball method, not only to cases of aphonia, but to cases of mutism and deafness, with success.
Tilly mentions a case in which the patient refused to open his mouth, so the device was adopted of passing an electrode through the left nostril so that it finally reached the larynx. A spasm was produced, which was carried to the point of considerable cyanosis, but the aphonia was relieved and for the first time in three months the man spoke. Incidentally he began to hear also.
Re treatment of aphonia, Schultz has used the electric current externally over the larynx, all the while carrying on a laryngoscopy. Schultz remarks upon the fatigue that may come during the first few sittings. Roussy and Lhermitte remark that, although aphonia sometimes exists from the outset of shock, it is often a phase in recovery from mutism.
Liébault notes that, not only cases of true nervous aphonia but cases of laryngitis, apparently of infectious origin, and cases of true voice strain, may also turn up for treatment. Some men have been improperly discharged from the army for aphonia actually due to voice strain.
Hysterical aphonia in a mechanician (war time contributory?). Cure by suggestive manipulation of larynx.
A mechanician was refitting an engine valve, when steam was suddenly put on and the drains were opened out. Some of the steam entered the throat of the mechanician, who rushed up, gasping, unable to speak. Oedema of the larynx was thought of; but there was no complaint except the inability to speak.
A month later he was discharged to the hospital ship at Plassy, where he got faradic treatment, the effect of which was to cause him pain without recovery of voice. The man could whisper well enough and cough fairly loudly. The vocal cords of the larynx appeared normal on laryngoscopic examination, but adduction of the cords was not be properly effected. He was now given rest and constant assurances that he would get well.
Ten days later, another laryngoscopic examination was made, with mild mechanical stimulation of the air passage. The patient remarked that he had never been so near being able to speak since his dumbness came on. The patient was now informed that his muscle of talking was going to be replaced and that the success of the operation depended upon his help, so that he was to shout out as soon as he became conscious of the physician’s working inside his throat. The patient was given ether lightly, into the second stage. When consciousness was about to return, the laryngeal mirror was placed lightly on the larynx. The patient was commanded and encouraged to count out loud and shout. Speech returned permanently.
It is to be noted that there was no specific war effect underlying the phenomena, unless we regard the fact of its being war time as contributory to the shock produced by an incident in every day engine room duties.
Gradual onset of mutism and amnesia without special occasion. Faradism. Dream.
A soldier was slightly wounded in the arm and returned to the trenches. Later he found himself in hospital at Boulogne, unable to speak and unable to remember what had happened to him from the time he was in the trenches. It appears that his voice and memory had gradually disappeared, according to what was told him by his comrades.
A month afterward, in a London hospital, the patient was roused suddenly from sleep, and then proved able to speak, although there was great difficulty in getting each word out. Two months later, he went to bed, feeling indisposed, in the night had a kind of fit, and remained unconscious until the following night; the next morning, his voice was again lost. The aphonia persisted for a fortnight, and the patient could hear only loud shouting when close to his ear. He was anxious to get well and requested electricity from the physician, Dr. Smyly, having heard probably of another case cured thereby. Dr. Smyly applied faradic current to the larynx externally, instructing the patient to blow at the same time. At first the patient spoke so low that he could not hear himself speak, but on suggestion succeeded in speaking up loudly enough. He was shortly able to speak and hearing improved. The climax arrived with a bad dream one night, from which the patient awoke in a fright and found himself able to hear and speak perfectly.
Re nocturnal spontaneous cures, see observations by Mott under Case 473. Note also in this case the presence of what Mott has termed “the atmosphere of cure.”
Re relapses, see Case 476 as well as remarks under Case 474. Re special cases of mutism, Goldstein has insisted upon a greater individualization of treatment for functional mutes than even for other neurotics, and advocates the establishment of schools within the hospitals and aftercare institutions. He thinks the problem very serious.
Shell-shock blindness: Cure by a course of injections in the temple.
A soldier from Gallipoli was admitted to the Royal Victoria Hospital at Edinburgh, blind. He had been at Gallipoli from May 1, 1915, until August 12, when a shell explosion blew in his trench and buried him. He was dug out nervous and tremulous. Shortly afterwards there was the bright flash of a second shell, and amnesia set in until he found himself in hospital. He could not see at all with the left eye and the sight of the other was poor. He arrived in Scotland, October 9. He was nervous, excitable and now somewhat depressed, complaining of blindness and pain in the left eye, and headache. The left eyelid drooped. The fundus was normal. He had not been given an anesthetic.
It was explained to him that the eye had not been injured; that it had become weak from the explosion; that he would be given a series of injections into the left temple of a strong drug which would restore the sight of the eye.
Gradually increasing quantities of normal saline solution were given every morning. After four days he said that the treatment was doing him good. A week later he said that the eye was much stronger. After the fifteenth injection he could not sleep. The headache was worse, and there was “moving about inside his head.” Early in the morning he went to sleep after a period of restlessness. He awoke at eight o’clock able to see perfectly, and was overjoyed at the result. There was some blurring and four days later he said he was becoming blind again. More normal saline was injected, causing pain. After that there was no relapse, and the man was sent back to his unit.
Re Shell-shock blindness, Ormond and Hurst recommend a light hypnosis; taking the functionally blind man into a dark room and requesting him to make his mind a blank. Some cases are refractory. An anesthetic may be used with suggestion in the semi-conscious stage.
Deafness, cured by suggestion in writing.
L. G., 20 years old; fusileer. (Mother of neuropathic constitution. Father died in 50th year of heart disease. One brother had hemiparesis from infantile cerebropathia.) The patient suffered from infantile otitis media bilateralis, which was followed by abundant chronic otorrhea from his fifteenth year. He relates that for a long time he was obliged to wear a very large handkerchief on his shoulders to receive the pus, which came from an ear. No sex disease. Nothing of importance in the physical anamnesis.
Patient entered the army, Jan. 15, 1915. In May, he was sent to the front (Basso Isonzo). Towards the end of July, while he was in the trench, a grenade exploded a short distance from him, causing slight abrasions at the nape of the neck and in the fleshy part of the left calf. He was picked up in an unconscious state, and taken to the hospital at Cervignano, where he was admitted as a deafmute and was given electric treatments. After 18 days or so, first stammering and then pronouncing with difficulty a few words, he finally regained his speech entirely. Deafness continued, however.
Being transported to a special hospital in Florence, he was in a state of psychic excitement for several days, showing also visual hallucinations—saw “many soldiers,” saw “many soldiers all about him.” He was treated with chloral and bromide. The suspicions of several physicians were aroused by the obstinate declaration by the patient that he was incurably deaf.
On being admitted to the clinic on August 22, he showed complete deafness in addition to a slight degree of stupor; he remained impassive to the glance of his questioner without showing signs of worry about his condition, nor did he make any effort to make himself understood by making lip-movements (which is in contrast to another patient affected by organic deafness, who on the contrary made great efforts to[731] understand anything said to him, clearly showing his great grief over his incapacity).
He failed to respond to auditory stimuli either by air or by bone conduction. It was possible from the beginning to exclude suspicion of simulation; during the day, indeed, it was not possible by any of the repeated attempts to awaken surprise in the patient by means of an acoustic stimulus. At night, while the patient slept, it was possible, however, to awaken him by calling his name, or by making a fairly loud sound; the patient would then open his eyes but was quite unable to hear. Neither confusion nor hallucinations were in evidence.
He was able to converse very well and spontaneously (he remembers having lost consciousness at the explosion of the grenade and not coming to until after his arrival at the hospital at Cervignano); he read correctly both mentally and aloud, and answered by signs the questions put to him in writing. Being face to face with hysterical traumatic deafness, notwithstanding no other hysterical phenomena were noticed, a successful attempt was made with suggestive therapy, the patient being emphatically assured (always in writing) that the following Sunday his hearing would be restored without doubt. The following Sunday, in fact, during the visit of a lady (one of his friends), hearing in his left ear was suddenly and almost completely restored to the patient. He was in profound emotion on account of this, and upon the appearance of the physician he had a hard weeping spell. During the following day, he began slowly to hear with the right ear.
During the latter part of his stay at the clinic, however (until September 24, 1915), a slight hypo-acusia in the right ear persisted, along with severe headaches and pains in the left ear (which the patient compared to the suffering as a child with otitis).
At the otoscopic examination by a specialist, only residuals of the old catarrhal otitis with retraction of the tympanic membrane were found.
Shell-shock story reproduced in hypnosis. Recovery.
A private had been found wandering in a village, in shirt and socks, unable to give name, regiment, or number. He was admitted at a field ambulance, and seen by Major Myers three days later. No Christian name seemed familiar to him. The past was a blank. He was depressed. There was numbness over the occiput. The legs, hands and tongue were tremulous. The left arm and leg and the left side of the face, chest and abdomen were hypalgesic. The knee-jerks were exaggerated; pseudo-clonus of left knee and right ankle. There had been a nightmare of bombs thrown into trenches—one thrown by a German hit him in the neck and woke him up in a cold sweat.
In hypnosis the dream was repeated, and points about his previous life were dragged out piecemeal. Next, the names of village and near-by town, and finally his own name, regiment and number were elicited. After the bomb-throwing, he said, “I must have gone off my head and run away. I must have taken off my clothes in a field. I spent the first night under a hedge. I spent the next two nights in a wood. I ate nothing. The next night I was walking along a road on the outskirts of a village and I was taken to a house by two men.” On waking, he proved unable to remember these things and was promptly rehypnotized, whereupon the memories became clearer and more ample. More powerful suggestion was given, and complete recovery of memory followed the second period of hypnotism. The pupils became larger. The despondency disappeared, together with the occipital numbness and the left-sided hypalgesia. He was transferred to a base hospital, and thence after three weeks to a hospital in England, made an uninterrupted recovery, and rejoined his regiment.
Shell-shock story reproduced in hypnosis. Recovery.
Private, 29, seen by Major Myers in a base hospital the day after entrance, was in a stupor from which he had to be repeatedly roused to answer questions. He could recall neither name, regiment nor age, and was unable to write or read except a few letters in very large type. Twice he said the words war and comrade, and made a gesture as if following. He agreed that a shell came and intimated that he had pains in the forehead. He could not hold his hands out for many seconds without dropping them. Knee-jerks brisk.
Four days later he was very little better, never having spoken voluntarily, but replying yes to the utterance of his name, and was able with great effort to write his name. He still intimated his severe headache. The next day the names of his two children were given. He could not read aloud the figure 2 but held up two fingers. Next day, he gave syllable by syllable his wife’s name from her photograph.
A week from admission he was hypnotized and persuaded to talk about the events that preceded his disorder, breathing excitedly, gesturing, and evidently visualizing the scenes. He had been in the trenches, had been sent to draw water at a camp, and had been knocked down when two or three shells burst over him. He carried out post-hypnotic suggestions.
He was hypnotized again, two days later, and now described how, after shelling, he had lain on the ground, dazed; had risen, picked up the water bottle, returned to the trenches, and then lost all sense and reason. He recalled how his mates had told him he was silly, but had lost all intervening memories. But the full details were elicited by persuasion. Next day he complained that he still wrote with difficulty. Under hypnosis, his speech and writing were restored to normal. He was discharged two days later to an English hospital.
He was then passed for foreign service, being prevented from active service in the field by occasional severe headaches.
Burial after explosion of a “coal box”: Automatism, amnesia, deafmutism: Recovery by hypnosis.
A sergeant, 18, with nineteen months service in the army, 11 months in France, was seen by Lt. Col. Myers at a clearing station to which he had been transferred after three days in another clearing station, with a note “Found in the streets of B——, asking his way to the fire trench; could not be got to speak on admission nor since; seems deaf, but now writes rationally.”
Mute and very deaf at the second C. C. S., he regained a good deal of his hearing with encouraging talk and also became able to cough and utter P, B, F and S, finally whispering name, regimental number, and the like. At the same time he could write fluently. After being buried he had lost himself until he had asked his way of a military policeman at the crossroads in B——. There was amnesia again until he had been 48 hours in the clearing station at B——. The throat hurt as if it were pulled down when he tried to speak, and his head ached when he tried to remember. There was much tremor, especially of right arm. In a quiet room adjoining, the tremors increased and there was much agitation. Lt. Col. Myers suggested cure and encouraged the man, finally inducing a mild hypnotic state in which he spoke aloud, at first hesitatingly, later fluently.
The man eventually remembered what had happened after he had extricated himself. He had run, as he thought, towards the fire trench, taken a wrong direction, and met a Frenchman who gave him eggs and bread, allowed him to sleep on a couch, put him on a cart and drove him to B——. He was then very giddy and asked his way of the policeman. The shell by which he was “terribly shaken” was a “coal box.” Posthypnotic suggestion that the headache would not recur and that he would shake hands with the orderly was successful. He now talked in a proper voice, at first hesitatingly. He looked another man as his clay-colored face resumed a[735] normal aspect. After a good night’s sleep he was evacuated to a base hospital, thence to an English hospital, whence he wrote six days later in gratitude for the successful treatment, stating that he was now nearly well and hoped to be fit for light duty.
Six weeks later he wrote that he was still dizzy. He also remembered certain further details of his experience; how he had wandered into a listening sap in front of the Huns’ barbed wire and had had a tussle with three Huns, after which he was buried during the heavy shelling.
This case belongs in the group termed by Myers “A Group,” namely, the physical group, in which the patient has been lifted, buried or knocked over by a shell or otherwise felt physical or chemical effects of an explosion (in contrast with the B Group, or psychical group, in which fear of the noise or emotional response to the mutilation of companions is the exciting cause). Predisposing affections occur as often in the physical group as in the psychical group. The average age of mutism cases seen by Lt. Col. Myers is twenty-five. Mutism is rare among commissioned officers. Lt. Col. Myers has heard of but one or two cases.
With respect to the technique of getting these men to utter sounds, Lt. Col. Myers states that he first assures the patient that he has already cured many cases of loss of speech by the method about to be employed. The patient is next asked to copy his teacher as the sounds (not the vowels) B, D, finally V, S and K are made. The patient is, as a rule, shortly induced to make the necessary movements of lips, tongue or throat. “You see you are beginning to talk. Now let me hear you cough.” The patient coughs. “You see you are able to make a noise. I want you next to cough out an A (Continental pronunciation).” After a time the patient adds this vowel to the cough. Other vowels are now taught him. Eventually a consonant is prefixed to the vowel instead of the cough. The patient is now delighted with his progress and can shortly repeat surname and regimental number.
Mutism: Recovery by hypnosis.
A transport driver, 31, was run over by a loaded wagon at Gallipoli in May, 1915, and fractured his pelvis. He remained perfectly conscious but unable to speak for three days. At the beginning of August, when he was admitted to the war hospital, he still spoke with great difficulty and with contortions of his face. Even when he did not speak, he had facial contortions and that mental condition characteristic of tic, namely: although he was able to control the contortions by will, he felt uncomfortable during the control and finally gave way to the irresistible impulse.
Under hypnotism, it was suggested to him that he would be able to speak without difficulty and would no longer have the contractions of the face. When he came out of hypnosis he was able to talk quite normally, sang next evening at a concert, and a few days later he took part in a play. The facial contortions persisted in hypnosis and even afterwards, but vanished after a second hypnosis.
Re hypnosis as treatment of mutism, Ballard remarks that a genuine return of speech and a merely hypnotic speech must be distinguished.
Nonne is the great exponent of the use of hypnotism in treatment of the war hysterias. He got as good results from high as from lower classes of men. He remarks that the hypnosis does not protect against recurrence if the patient again falls under the original conditions that brought about the first attack. Hypnosis may be used also as a diagnostic measure between functional and organic cases. Even tics and tremors have been at times cured.
Re employment of hypnotism, Hurst suggests that it may well be used, not only in mutism, but in hysterical deafness, blindness, and occasionally in psychasthenia. It is not a cure-all for the war hysterias, but is to be used as a not infrequent form of treatment. Nonne claims cures of 51 out of 63 cases of hysteria major (28 rapidly, 23 more gradually). Ten of his 63 proved refractory to hypnosis altogether.
Stammering: Cured by hypnosis.
An Australian, 22, wrote the following, August 21, 1916:
“You may be a little surprised to hear that I am in the Hos. suffering from shell-shock, which has taken away my speech and hearing. It is some sixteen days now since it happened.… We were in the trenches and going for dear life, when two of us spotted a German machine gunner in a hole, so we made up our minds to have him. We made a charge at him, and I just remember getting to him when a high-explosive shell burst at my head; it seemed as if it burst inside my head; everything went black. I tried to call out and couldn’t, and I could not hear my mates—only just a terrible bursting in my head all the time. I never remembered anything more until I came to on the boat. The Drs. have told me that I will get alright in time. I saw a good deal of France.… There is not a young man there who is not in the Army. The girls and women work in the fie——”
The abrupt ending of the letter was due to the entrance of Major Hurst. The patient had been hypnotized but his deafness had persisted during the hypnotic sleep, so that suggestions could not be effectively taken. He heard nothing whatever during a very heavy thunderstorm, was unable to make any sign whatever, and could not even cough.
He was now told in writing that his speech and hearing would be restored when ether was given. After a few whiffs, he struggled and before he was under began to repeat the word “Mother.” Etherization was discontinued before his limbs had even become relaxed. As he was coming to, he was requested to repeat various words, and when the anesthetic had passed, he was talking normally and had completely recovered hearing.
Now, however, his memory had become a complete blank. From a short time before his shell-shock up to the moment of his regaining consciousness after etherization, he remembered nothing of his loss of speech or hearing, nothing about the events in his letter, and nothing about Major Hurst, whom he[738] felt he had not previously seen. According to Hurst, this patient had become (a) speechless from fright at the time of the shell explosion, (b) deaf from the noise of the explosion, and (c) unconscious from the windage. After he came to at the time of the explosion, an autosuggestion to the effect that he had lost his power of speech and hearing occurred. Ether broke down this inhibition of speech and hearing by interfering with the control of the high over lower cerebral centers.
Re emotional stammering, Chavigny treats by voice gymnastics, rhythmical breathing movements, sounds spoken by metronome with simultaneous movements of arms or trunk, and by singing. Re hysterical stuttering, Roussy and Lhermitte remark that the symptoms are always very pronounced, come on suddenly, and cease just as suddenly under the influence of electrical treatment. The history will differentiate hysterical stuttering. The effects of treatment will also help. Genuine non-hysterical stammering may, of course, be increased through emotion or shock. Dundas Grant aids the stutterer by having him twist a button or carry out some other muscular movement simultaneously with the attempt to speak. He also has the patient endeavor to expand the lower part of his chest during the effort.
MacMahon notes that Shell-shock stammering is chiefly a difficulty with vowel sounds and voiced consonants, and amounts to a speech inhibition, accompanied sometimes by amnesia for words and suggesting a form of aphasia. Mild cases of such stammering are cured simultaneously. MacMahon relies in part upon especially regulated breathing movements and the attendant sense of repose. The cases of old cured stammering that have come back under Shell-shock are harder to treat.
Two burials; shell-shock: Mutism and amnesia. Recovery aided by hypnosis.
Major C. S. Myers recites hypnotic cure in a case of mutism. He remarks that malingering is sometimes suspected in these cases. There was, however, in this case a severe constipation which lasted five days from the shock, and a retention of urine with catheterization during the same period. This private, 32 years, came to a base hospital, mute but able to read and write as follows:
“I was buried alive on —— and again on —— [5 months and 4½ months respectively before admission], and then I had the misfortune to have two shells burst over me on —— [four days before admission]. There was shelling for about 20 minutes and then two bursted over my head. I did not remember any more until you came to see me, but I am still living in hopes to regain my speech back.”
It seems that he had wandered off with a lance-corporal for three days after the first burial, and neither he nor his comrade were able to find their regiment.
Understanding was slow and look vacant. There were jerky movements of the arms and a snoring sound from the nasopharynx. Voluntary movements were restricted, weak, slowly executed, jerky, and incoördinated, but not tremulous. Station was unsteady; failure in finger-to-nose test. He could imitate the sound ah, and the consonants s and p.
Knee-jerks exaggerated; plantars flexor; abdominal reflexes absent; pupils reacted; eye movements normal; moderate restriction of visual fields on temporal side; watch not heard even in contact with ear; heard better by air than by bone conduction.
In the next two days, the patient became brighter and movements became better. On the seventh day stupor and ataxia had disappeared. Familiar names could be repeated and the next day could be given on request. The patient would sweat profusely in giving replies. There was no spontaneous speech. A week later speech had improved.
Under hypnosis he spoke more fluently though feebly, and became emotional upon being questioned as to trench life, waking up suddenly from hypnosis and wiping the sweat from his chest.
The next day, forgotten events of the second burial were recalled together with what followed. Post-hypnotic suggestion of the performance of eccentric actions was successful.
Next day his memory had returned save in reference to the two days’ wandering after the first burial; and under hypnosis the events of those two days were recalled. He was then transferred to an English hospital.
Re hypnosis for “war shock,” Eder remarks that the usual objections to hypnosis cannot apply because the majority of cases have no neuropathic antecedents. Eder, as psychoanalyst, endeavors to level hypnotic suggestion against the so-called “complexes.” Elliot Smith and Pear commend Lt.-Col. Myers’ results, but regard the results of hypnotic treatment as brilliant but erratic. Colin Russel, regarding hypnotism as an induced hysteria, remarks that a true hysteria can hardly be cured by adding more, although he has sometimes used the treatment with apparent success. Podiapolsky notes that some 17 per cent of his functional cases will, at a word, drop off into an artificial deep slumber. He thinks chloroform should not be given to these subjects without an attempt to secure this artificial deep slumber first. Chavigny, highly commending suggestion, notes that the use of hypnotism is prohibited in military hospitals in France. A remark of Smirnow indicates that the Russian authorities also look with disfavor upon hypnosis, but he notes certain patients whom he cured by hypnosis, so that apparently Russia did not absolutely forbid the use of hypnosis in war cases. Another Russian, Arinstein, prefers the Dubois method to hypnosis.
Roussy and Lhermitte definitely state that the psychotherapy of Dejerine, Dubois, and Babinski beneficially replaces hypnotic suggestion, “which ought definitely to be rejected.” However, if the conclusions of Bernheim are sound, there can be no theoretical claim of distinction between hypnosis and other forms of suggestion.
Fifteen bayonet wounds; recommendation for Victoria Cross: Hysterical contracture of hand, revealed by hypnosis as the bayonet clutch.
A left-handed Irishman, 23, on December 22, 1915, got 15 bayonet wounds, 14 of which were on the right side of the body. He was in the trenches with 23 men, when they were attacked by about 200 Turks. He and a sergeant leaped out of the trench into a bayonet attack with Turks.
He was admitted to the hospital January 26, 1916, for a hysterical contracture of the right hand. The fingers were semi-flexed and could not be passively extended. Col. Purves Stewart noted that there was an anesthesia and analgesia to pin-pricks and cotton wool on the whole of the right arm. “At the beginning of the examination, the patient felt pin-pricks at the wrist; as examination continued, the boundary of anesthesia steadily increased until it reached the shoulder, by which time the previously sensitive spots were now anesthetic.” Later there was a complete right hemianesthesia.
In telling his story, this soldier repeatedly emphasized that “You must clutch your rifle very firmly and never let it up, guarding yourself all the time.” This was the explanation of the contracture. According to Eder, in the unconscious, he was still clutching the rifle, fighting the good fight, and symbolizing the desire by the grasping hand. In hypnosis, suggestion was made that the fight was over and the rifle could be let go, whereupon the hand was immediately relaxed.
The analgesia, thinks Eder, was present during the fight and passed away subsequently. In fact, the soldier said that he felt no pain during the fight and did not know that he was wounded until his attention was called to the fact that blood was flowing from him. According to Eder, the unconscious mind refused to feel pain. At Col. Stewart’s first prick or two “the unconscious took no notice, but as the pricks continued, the former memory was revived and the unconscious became on guard.” He had been recommended for the V. C.
Gunshot of forearm: Hysterical contracture, wrist and fingers: Cure by hypnosis, “indecently quick.”
An infantryman, without special hereditary taint and previously well, was shot September, 1914, in the right forearm. A paralysis of the hand and fingers persisted after the wound had healed. Several reserve hospitals failed to cure the paralysis.
Eight months after the injury he arrived at Nonne’s clinic at Eppendorf, with a flexor contracture of the right wrist joint as well as of the fingers (exclusive of thumb). The finger tips were deeply sunk in the flesh of the palm. Extension could only be brought about against strong resistance. There was a total anesthesia for all sensations in the hand and fingers. No contraction of visual fields.
The patient, upon suggestion, fell immediately into hypnosis. At first the contracture was released with some difficulty; then, with greater ease, and then without any resistance whatever. During the same hypnotic séance the patient finally became able to extend actively both fingers and wrist; and next day, after the patient had convinced himself of his cure, he was able voluntarily to stretch the hand and fingers with normal amplitude and power. The disturbance of sensibility had spontaneously disappeared.
This cure was, from the patient’s point of view, indecently quick. He said everybody must feel he was a malingerer, and in fact he felt so himself. He went back into service, where he had been for several months at the date of Nonne’s report.
Re Nonne’s enthusiasm for hypnosis, see under Case 526. Nonne, contrary to Babinski and Froment, would regard even the severe and obstinate vasomotor disturbances as purely functional and as not even “sub-organic.” The basis of this belief is that hypnosis cures these phenomena as well as various tics and pertinacious tremors. French observers consider that these tics and tremors may even be organic in their nature, basing their ideas upon the non-success of[743] suggestion. (It may be noted [see under Case 528] that the French military authorities do not allow the use of hypnotism in the army.) With respect to the present case (530), of course, the French observers would not deny the power of hypnotism to produce the cure. Babinski and Froment’s Postscript to the English edition of their work on hysteria, remarks that, though Roussy and Lhermitte state that vasomotor symptoms may disappear along with the psychotherapeutic cure of paralyses and contractures, yet Roussy and Boisseau later admitted that improvement in thermal and vasomotor control is at best an exceedingly slow one.
More recent personal communications indicate that there is still room for some question as to the curability by suggestion of such disorders as tic, tremor, vasomotor imbalance, and the like. In short, the true scope of the “pithiatic” or suggestion-curable diseases is still somewhat a matter of controversy.
Shell-shock: “Doll’s head” anesthesia, mutism: Hypnosis.
An officer, mute for five months following shell-shock, had been for four months treated in a succession of hospitals—field hospital, war hospital, two reserve hospitals.
He had no acquired or hereditary neuropathic taint, but even in the period before the critical shock he had been under tremendous physical and mental strain. The explosion produced a total anesthesia of the skin of the head, face, neck and shoulder region—in short, what Charcot called the “doll’s head” form of sensory disorder. Moreover, there was a marked contraction of the visual fields.
The patient, when treatment was given, fell at once into a deep hypnosis and began to intone, and then to speak isolated words, and finally to speak complete sentences. All that was left of his mutism was a slight over-fatiguability of the speech organs. This also cleared up in the next few days. He was discharged well, and had already been—December, 1915—some months in the field.
Case 531, though an officer, responded to hypnosis well, and Nonne remarks that hypnotizability is independent of the presence of any neuropathic tendencies, or of any loss of resistance through exhaustion. One trouble with the hypnotic method, according to Nonne, is the fatigue of the hypnotizer and his inability to rely upon assistants.
Re Charcot, Nonne remarks that the work of Charcot on hysteria is not sufficiently well-known, especially as civilian practitioners in peace times had few cases. Re taint, Nonne found such tendencies absent in more than half of his cases with careful anamneses. The absence of adequate psychogenic cause is a not uncommon experience according to Nonne. Nonne, finding 26 cases of pure neurosis amongst 1800 cases of war injury, had a considerable number of odd erroneous diagnoses in the group. Not only were cerebrospinal paralyses wrongly diagnosticated, but ischemic paralysis, plexus paralysis, arthritis deformans and synovitis.
A soldier is put in the Landsturm at 22 and later called “unfit” by reason of tremors after mine-explosion (history of tremors at 14 after a fall), but is cured by hypnosis.
A Landsturm soldier, 22 (father excitable, family otherwise normal), had a history of being the best scholar in the class and well up to his fourteenth year. At 16 he fell from a tree and though he apparently sustained no injury his head and arm began to tremble. He became unable to learn and gave up his preparations to be a teacher. The tremor, however, disappeared in six months and he went into some technical work. At 16½ years he went as cabin-boy, but in a fortnight he was sent home by the physician. He then began to breed carrier pigeons and got first prizes at international exhibitions. He also went into foundry work and did well as an apprentice. He worked well at home and busied himself with setting up small electrical and other machines. He had never been interested in women and loved his pigeons best, and therefore was regarded by people who knew him as not quite right. He was also non-alcoholic.
After mobilization he was sent back twice but finally was put into a Jäger Battalion. After reaching the front he had to have a hernia operation and on getting well went back to his place and a few days later a mine exploded near him. He was much frightened and fell down unconscious. On regaining consciousness he felt a “running” in the legs and tremors in the hands. The latter grew stronger and began to affect the arms.
After two months in hospital he went to garrison unrecovered, was placed in the Landsturm and did four months station duty in Russia. The tremors persisted and when his comrades played a bad practical joke on him the tremors got so bad that he was sent back home as unfit for service.
He was a stocky looking, well-nourished man of middle height, without visceral disease or sign of organic nervous disorder.[746] The shaking tremor grew much more powerful in any state of excitement but always paused sufficiently to permit the execution of any particular movement. The head movements were continuous, slight rotations. There were a few regions of anesthesia to touch, but these areas differed at different examinations. There was a general hyperesthesia. Conjunctival, corneal and pharyngeal reflexes were absent. The man was slightly excitable, apprehensive, depressed, complained of sleeping badly, did not want to sit or stand and felt as if he wanted to run away, no matter where. In dropping off to sleep he would fall out of bed and talked aloud in his sleep. He thought he was incurably sick. Intelligence and school knowledge were very good.
He was hypnotized eight times for periods of about five minutes each. Hypnosis was extremely easy to accomplish. At the second trial the manual tremor disappeared. After the third trial there was an essential improvement in the shaking tremor. Moreover, his emotional state had become happier. He began to sleep well. He was now free from disease and regained confidence and looked upon himself as well and fit for work. Undoubtedly without hypnotism this man would have been released from service after a few months of inconsequential hospital care without pension.
Re tremors, see remarks under Case 308, concerning the possibly organic nature of many of the so-called Shell-shock tremors; an opinion apparently shared in by Meige and by Guillain. Babinski also found that these tremors were not influencible by psychotherapy. Yet here is an instance in which tremors are reported cured by hypnosis, and moreover, tremors that were recurrent from an ante-bellum attack at 14. See remarks under Case 530.
Shell-shock, slight injury, unconsciousness: Astasia-abasia: Recovery under hypnosis, two séances.
A musketeer, without neuropathic taint and without nervous symptoms before the war (parents both dead of tuberculosis, eleven brothers and sisters died young), saw four comrades killed by a shell October 27, 1914. The musketeer himself was slightly injured superficially in the back. He remained unconscious for three hours and on coming out showed general tremor of the body, felt pressure in the head, was lachrymose and unable to walk or stand. He was subject to insomnia. He was in four different hospitals, finally reaching Eppendorf. Diagnosis rendered at the first hospital and carried on through the others was hemorrhage into the spinal canal.
For two months at Eppendorf he lay in extension. He was then examined by Nonne, who found general neuropathic habitus, pronounced “cramp neurosis” in the lower extremities, psychogenic astasia-abasia, hyperidrosis of the lower extremities, marked cyanosis of feet and lower legs, increased tendon and skin reflexes, pseudoclonus, no Babinski or Oppenheim reflexes. The man complained of pressure in the head, sleeplessness, a feeling of depression and hopelessness. Pulse 120-130.
Hypnosis proved easy. After the first treatment the man stood and walked and showed no tremor. The next day the hypnosis was repeated and the cyanosis of the legs disappeared. Sleep on the second night was good. Appetite returned and the man fell into a good emotional state. Thereafter the patient was intentionally ignored by the physicians and could soon not be distinguished in any respect from the other non-nervous convalescents.
This case is expressly stated by Nonne to resemble in all respects those formerly described by Oppenheim as[748] “traumatic neurosis.”
Crural monoplegia: Cured by hypnosis.
A Belgian soldier fell into mud on the collapse of a roof from which he was observing the enemy. It was an hour before he got his left leg out of the mud, and found it fixed in extension. He was sent to England, where for three months the leg remained stiff. The spastic paralysis did not seem organic as the leg was dragged behind. The knee and ankle could be bent only by using much force. The entire leg was in all ways anesthetic. Babinski sign gave additional proof that the condition was hysterical: when the patient lay with arms folded and legs apart and then tried to sit up, the normal leg was lifted and the paralyzed leg remained flat.
According to Hurst, the paralysis and stiffness were due to an autosuggestion from the legs being embedded in mud. The anesthesia was probably a matter of medical suggestion produced in the course of examination during the three months of disability. According to Hurst, Babinski is right in supposing that hysterical anesthesia is almost invariably produced by the observer.
Accordingly a strong faradic current was passed through the leg, and he was assured that sensation and power would be restored. However, he could still walk only with difficulty.
Hypnosis was therefore resorted to and repeated on several occasions. He went back to duty in three weeks, although he still held the leg somewhat stiff when he walked.
Re recurrences after hypnotism, see remarks of Nonne under Case 530. Howland also notes that cases treated by hypnotism must be followed up to prevent relapse. In the above case of Hurst’s, it will be noted that the hypnotic treatment was several times repeated.
Shell-shock, emotional (slight trauma): Tremors and sensory impairment: Cure by hypnosis, thrice repeated.
A reservist, always well, not neuropathic (mother had had seizures, possibly epileptic, for many years) was wounded in the left calf by a shell fragment, about the middle of December, 1914. He was at the same time, as a result of the shell explosions near by, afflicted with a tremor of the whole body; this tremor gradually increased and proved refractory to all treatment for nine months.
At the beginning of September, 1915, the patient reached Nonne’s wards, showing tremor of head, arms and legs, with pronounced hypalgesia of the whole body, abolition of frontal and conjunctival reflexes, and contraction of the visual fields.
The tremor of the head was completely removed at the first hypnotic treatment. There was a slight recurrence of this tremor two days later, and traces of it could be observed for nine days. A third hypnotic treatment swept away this tremor, which did not return.
The patient was discharged after about four weeks, suitable for garrison duty.
Re traumatic neurosis, Nonne dislikes this term of Oppenheim, because such a term rather tends to connote unfavorable prognosis. As quoted under Case 530, Nonne holds that the war data show that hysteria is neither a form of degeneration nor an affair built on the Freudian schema.
Nonne in fact maintains that the hysterical syndrome may occasionally occur with much greater ease in a normal person than ever has been known before. It is precisely in these cases of normals getting hysterical that Nonne gets especially good results with hypnosis. If the development of the hysterical syndrome had extended over days or weeks, then the hypnotic cure was a slower one. The above reservist developed his Shell-shock gradually and required three[750] hypnotic treatments. But although the number of doses of hypnotism required may be said roughly to depend upon the time which the condition took to come to a head, yet there is no similar rule re duration. A miracle cure may be brought about even in cases that have lasted over a year. This result, if confirmed, would signify that the hysterical condition once fixated did not especially increase in its tenacity.
Re hypnosis in Germany, it should be noted that Nonne is the chief protagonist for hypnosis, at least among the well-known neurologists. Psychoelectric cures, which the Germans term Kaufmann’s cure, are also greatly in vogue in German clinics. Despite the well-based claims of Lt.-Col. Myers and of Eder, some English observers appear to condemn hypnosis as inadequate, or even as dangerous.
A series of relatively successful cases like those here mentioned might yield a wrong impression of the value of hypnosis (see Feiling’s unsuccessful case 369).
Hysterical paraplegia of gradual development: recovery only under repeated hypnosis.
A volunteer, of nervous parents, had for four years suffered from attacks of uncertain (hysterical or epileptic) nature. These attacks came on again after strenuous marching in the campaign in Belgium and France. Released from service at the front and detailed for guide duty, he proved unsuitable for this work, too, and was sent back to a hospital at home. Here there gradually developed a paralysis of the lower extremities. Treatment proved ineffective.
At the end of January, 1915, he came to Nonne’s wards at Eppendorf with a paralysis that had lasted six months. There was a total paraplegia inferior, with anesthesia for all sensation from the knees downward. The lower legs and feet were cyanotic and cold. The tendon and skin reflexes were lively. There was a moderate contraction of the visual fields on both sides.
Under hypnosis, the patient proved able to move both joints somewhat, but very weakly and slowly. The patient was hypnotized daily for a week, and made slow progress. Only after another week did it prove possible to get him to stand. After four weeks, his gait had so improved as to look like that of a tired old man. Three weeks more of treatment permitted the patient to walk, run and hop normally. Repeated waking suggestion had failed to accomplish anything in this case. The improvement followed only hypnosis. It seems to be a general principle that in cases of gradual development, the recovery by hypnosis will also be gradual.
Re repeated hypnosis for cases of gradual development, see remarks under the preceding case (535).
Struck by rifle butt: blindness of an eye already poor. Shell-shock: dysbasia. Hypnosis.
A lieutenant, 20 years, managed to get into the army despite the fact that he had never been able to use his left eye, owing to hypermetropia and amblyopia. He was hit on the left side of the head by a rifle butt, and knocked unconscious, in June. On recovering, he found he could not see at all with his left eye, which he had never been in the habit of using. August 10, he was wounded slightly in the left thigh. August 23, while still on duty, with the wound not completely healed, he was blown up by a shell. He regained consciousness on a stretcher. Feeling the pain in his old wound, he thought he should be unable to walk.
On shipboard, he found that he actually could not walk. He kept his left eye covered by a shade on account of headache that would follow exposure to light. He was much excited and had bad nightmares.
After the journey home from the Dardanelles, it was found that the left eye was normal except for the hypermetropia, despite the fact that he was quite unable to see with the eye.
He was hypnotized four times, losing the nightmares and much of the headache after the first treatment; the eye pain on exposure to light, after the second treatment; and the blindness, after the third treatment. He was now able to see with his left eye as well as before he was struck. He was still unable to walk without crutches. Hypnotized the fourth time, he was told he could walk, and did so.
For hypnotic treatment of blindness, see under Case 521. Re blindness of eye already poor, see Cases 294-301 (296 and 297 eye cases). Ormond states that in the treatment of Shell-shock blindness, he first tried rest, tonics, cutting off tobacco, confinement in bed, isolation, persuasion, encouragement, counter-irritation; but that all these measures failed. Suggestion and hypnosis succeeded.
Shell explosion; concussion; retinal hemorrhage: Blindness. Cure by hypnosis.
An English private, 22, was looking over a parapet, July 18, 1915. He afterward remembered sand thrown in his eyes and a fall backward, hitting his head, after a shell had struck the sandbags in front of him. He was unconscious 24 hours. Upon recovery, he found himself completely blind, save that he could just tell light from darkness with the left eye. His eyes were sore and eyelids blackened; there was also severe headache and partial deafness.
Hearing returned and the headache improved shortly; but the condition of the eye seemed more permanent. On forcibly opening the eyes, September 14, they were turned far upwards so that the iris could scarcely be seen. Some sand grains were buried in the conjunctiva, not in the cornea. There was no inflammation about the sand grains.
In hypnosis, he was told that he would see on waking. The moment he woke, this suggestion was repeated forcibly and his eyes were held open. He cried out that he could see; tears ran down his cheeks; he fell on his knees in gratitude. Three days later, he said he was able to see as well as he had ever seen. There was, however, an opacity of the vitreous of the left eye, the result of a retinal hemorrhage: doubtless the result of injury at the time of the explosion. September 30, he had perfect vision in the right eye and 6/36 in his left.
Re results of hypnotic treatment, Lt.-Col. Myers, summarizing 23 cases of Shell-shock, got apparently complete cures in 26 per cent, and distinct improvement in another 26 per cent. He failed to hypnotize 35 per cent, and got no improvement after hypnosis in 13 per cent. Is the recovery after hypnosis complete and permanent? Lt.-Col. Myers believes that it may be, but others remark the tendency to relapse (see Case 534). Similar objections may be made to the psychoelectric treatment as used by Vincent, Yealland, or Kaufmann. See under Case 535.
Appendix operation: Post-operative retention of urine. Relief by hypnosis.
A soldier, 32, operated for appendicitis, had a post-operative retention of urine. Hypnotic suggestion was requested to reëstablish excretion of urine before resort should be had to the catheter.
Somnambulistic amnesia was obtained at once and without questioning him P. suggested to him directly that he must feel the need of micturition. The suggestion was unsuccessful. However, bearing in mind psychogenic obstacles of an unknown nature, P. questioned the patient as to sensations and learned that in the operation the skin had been burned about the urinary passage and that the patient feared micturition. Besides this, micturition was painful on account of the wound above the appendix. The patient also feared that the sutures would yield.
Accordingly assurance was given that the burned parts would be insensible and that the bladder could be emptied without effort and without endangering the sutures. Analgesia was produced by a few passages of the hand upon the bed clothes. Complying with post-hypnotic suggestion the patient urinated after a quarter of an hour of sleep, and in thirty-six hours retention was relieved.
With respect to frequency of immediate somnambulism for the first trial, P. states that, although authorities set the percentage of successful immediate somnambulisms at 17-20 per cent, war conditions yield three or four times as high a percentage. The war has produced a suitable soil for hypnotism. Hypnosis is impossible in from 1½ to 2 per cent of cases.
Wound of sciatic nerve: Pains after operation. Relief by hypnosis.
A German prisoner, 33, was admitted to a Russian Hospital, November 11, 1916, with “a bad wound of upper right thigh, marked pains in right sciatic nerve especially affecting feet.” Morphine and pantopon did not abolish the pain. Insomnia. November 13, the sciatic nerve was surgically freed from a scar and laid in the midst of the femoral biceps. Every evening pantopon was injected; but the pains and insomnia persisted nevertheless.
November 19, he was hypnotized. The pain stopped. He had an excellent night, and the next day felt only a slight pain in the toes.
Curiously enough, while giving him suggestion in the German language, P. had said fingers instead of toes (inadvertently, since the Russian language uses the same term for both). He slept well to November 29 but still felt a slight pain in the toes. On November 29 another hypnotic sitting was given, and the toes this time were named correctly. The next day the patient said, “You have relieved me of all the rest of my pain.” He had no pain thereafter and the morphine and pantopon were dispensed with. Sleep returned.
Incidentally, this patient had his hair grow white in a few months of war.
Ship blown up by mine: Stereotyped explosion dream by survivor: Cure by hypnosis (also of antebellum habitual headache).
A survivor of H.M.S. T.B. II, blown up by a mine off Harwich, was admitted to the naval hospital at Chatham, March 3, 1916, a well-nourished, nervous looking lad, aged 20. After the accident, he began to dream, always the same dream, of the explosion, waking up with the cry of the ship mates, and then unable to sleep the rest of the night. The knee and ankle-jerks were somewhat exaggerated.
April 15, when there had been no improvement, he was hypnotized. The patient was told to lie back in an arm chair, make himself comfortable and allow muscles to relax. He was told to fix his eyes and concentrate his attention on an electric lamp. The suggestion of sleep was made, and he was repeatedly told in a monotonous voice that he was becoming more and more sleepy. Then in an emphatic voice he was told that the treatment would completely cure him. He had no more dreams after this first sitting.
Hypnosis was continued every other day until April 20, when he was discharged cured. After the first sitting hypnosis was induced by simply telling the patient to go to sleep, which he would immediately do on entering the room, while still standing up. At subsequent sittings, he was made to write twenty times such phrases as: “I feel much better”; “I shall have no more bad dreams.”
Once when a tooth was to be pulled a post-hypnotic suggestion that no more pain would be felt was given, nor was any pain felt. Headache persisted after the first two or three sittings. Accordingly, during hypnosis a pencil was pressed to the forehead with the suggestion that it would burn and that after waking there would be an itching pain for half an hour, followed by recovery from headache. Curiously enough, a distinct erythema of the skin was observed over the point of pressure. Toothache and headache vanished.
Shell-shock from air-craft bomb: Amnesia: Recovery under hypnosis (also removal of a headache dating from childhood).
May 22, 1916, a stoker, 26, was found on shipboard in a workshop behind oil drums, refusing to come out, looking dazed, not recognizing messmates, suspicious and complaining of headache. He reached the Royal Naval Hospital at St. Malo, May 24, answering questions “Don’t know,” and physically normal except for diminished knee-jerks. At the end of two or three weeks he would answer questions about his stay at the hospital, but complained of headache or weight in the head. Wassermann reaction, negative.
Special examination on May 26, showed an amnesia for everything up to his arrival at St. Malo. For example, he did not know the name or use of a hammer or a pressure gauge, though he knew the pressure gauge was made of brass and glass, having seen brass and glass in the hospital wards. He had no idea of the nature of a ship. He was sent to the sick bay at the Royal Naval Barracks at Chatham, July 7, carrying a recommendation that he be retrained as a stoker.
He was put under hypnosis, induced by gazing at the brass knob of a paper weight. He went off easily, was told there was nothing to worry about, taken back to the beginning of his illness, and asked what happened. He told about a bomb explosion from aircraft, and how he had lost his memory after a nearby explosion. He told how he was married and had a child 21 months old. During the narrative about bombs falling, his worry was such that he was put in a deeper hypnotic sleep, and was told that he would remember all that had happened. Upon being ordered to wake up, he remained dazed for a few moments, and then said that he was all right. Asked about his marriage, he replied that of course he was married and had a child.
After four days leave, he returned, July 13, without trouble except a headache, from which it appeared that he had suffered[758] ever since a fall when a child. He was again put into a hypnotic state and asked to remember the accident that caused the headache. He was conducted back through the years, and finally described a white house in India, his fall in the area, the black people in white clothes, the cut bleeding head. He was told that he would have no more of such headaches. On being wakened, he said that his headache was gone, and retold the story of the accident. August 2, he said he had never felt better in his life. September 1, he was drafted to a seagoing ship.
Shell-shock, unconsciousness: Convulsions (recollection of childhood convulsions): Cure by hypnosis.
A New Zealander was rendered unconscious for a few minutes following concussion from a high explosive shell. Convulsions developed, occurring at least once and often several times a day.
As to the origin of these convulsions, it appeared that the soldier had had a few convulsions after falling on his head at the age of 8. According to Hurst, recollection of these childhood convulsions probably led by a process of autosuggestion to the Shell-shock convulsions.
Captain Crabtree hypnotized the man, suggesting recovery. The fits immediately ceased and did not recur.
Recurrent hysterical mutism. Spontaneous recovery in (a) 18 months (antebellum incident). (b) Hypnotic recovery in a few minutes.
A soldier in a mine accident eight years before the war, lost his speech when his brother was killed, and then recovered his speech spontaneously after 18 months.
After a shell explosion in Gallipoli, he was again struck speechless and also deaf.
Six weeks later, he came to Dr. Eder and objected in writing to treatment, saying that he believed in nature’s methods. God had taken his voice away before and had restored it. Eder replied in writing “rather irreverently” that God had taken 18 months, but he could do it in a few minutes. The patient afterward consented to treatment, and speech and hearing were duly restored in the time promised, whereupon Dr. Eder told him that in point of fact his physician was merely the instrument of Providence.
Neurasthenic symptoms: Cured by repeated hypnosis.
A private, 24, was admitted to hospital with diagnosis neurasthenia, March 11, 1916. He suffered from vertical headache; general analgesia, more definite on the right side (patient left-handed); loss of smell and taste, also more definite on the right side; paresis of right leg, with dragging of foot (old trench foot); and sleeplessness.
The next day Tombleson put him in a hypnotic state, third stage, and again, March 13, but without results.
March 14, the somnambulistic stage was reached in hypnosis, and next day the man’s headache was much relieved as a result of the suggestion offered. He was again hypnotized and the following day, March 16, the headache had vanished and the man was in general much improved. In somnambulism the disappearance of the analgesia was suggested, and it proved possible to make the man walk about without limp and without dragging the right foot. Next day the analgesia was much relieved. In somnambulism the suggestions were repeated.
March 18, the man said he was quite well, and proved to be so on examination, except that he could not yet taste with absolute normality on the right side. In somnambulism it was further suggested that the cure was a perfect one and included the sense of taste. However, March 25, the expected improvement had not yet occurred in the taste, whereupon further suggestions were given in hypnotic somnambulism, re taste. Next day taste had become normal.
Re hypnosis, Tombleson says that the most successful cases of hypnosis are those of Shell-shock psychasthenia, but that he gets very good results with hyperthyroidism and with neurasthenia also. He goes so far as to say that practically all cases of war neurasthenia and psychasthenia can be cured and sent back to work if treatment by hypnotic suggestion is used in a reasonable time.
Neurotic symptoms: Improvement under repeated hypnosis.
A private, 32, was admitted, April 15, 1916, to Tombleson’s ward from the Cottonera Mental Ward with the diagnosis: psychasthenia with paresis of right arm. The man was very suspicious of the medical profession, melancholy, morose and prone to tears. He had been kicked by a horse four years before and showed a depressed and very tender scar in the right parietal region. The right side of the body since that injury had been getting weaker, but the arm was much weaker than the leg. Anesthesia was practically complete on the right side. There was a wasting of the muscles of the right arm and the skin of the hand and fingers was thin and shiny.
Before his transfer the man was placed in the somnambulistic state, with suggestions of happiness and confidence in the coming cure. He arrived at Valletta, April 16, in a cheerful frame of mind, stating that there was nothing now the matter but weakness. Under somnambulism the loss of symptoms was suggested and, April 17, the patient was well except for the loss of power in the arm and leg. Daily training under somnambulism was given for a period of seven days, with suggestions especially leveled at the paretic muscles. He was then so far recovered that hypnotic treatment was stopped. The patient went to England, May 12, 1916, well.
Convulsions, “Jacksonian,” and dysbasia: Cure by hypnosis.
A private, 18, was admitted to hospital, March 22, 1916, with the diagnosis Jacksonian epilepsy, with marked functional gait. He had just had several fits—two March 20, two March 21, and several earlier. He was tremulous and could not stand. Much pain. Knee-jerks brisk.
There was a history of a fall into a harbor at seven, followed by bleeding from nose and ears and unconsciousness for a week. Convulsions, involving the face, arm and leg, and attended by unconsciousness, kept recurring until twelve. Five months before admission there had been cerebrospinal meningitis. In February at Salonica he had had pneumonia.
March 23-24 the soldier was hypnotized to the third stage, but he had two fits. A “funny feeling in the right big toe” was brought out and suggested away. March 26-27 the patient was able to walk with a typical functional disorder. Under somnambulism the suggestions were repeated, but on the evening of March 27 two more convulsions appeared. In somnambulism he explained that he “had got round” the inhibition of the aura.
The night of April 2 occurred two convulsions. April 5, the man was placed in the somnambulistic stage to last three days. During the night of April 6 he was observed to be restless for an hour, with some twitching of the right face, yet no fit followed. The morning of April 8 the patient woke feeling well. He was again placed in somnambulism to last two days. Two hours later, however, a fit started. It was stopped at once by suggestion, but the patient woke. He was left awake the rest of the day. April 9, somnambulism: suggestions repeated; sleep to last for two days. That evening there was a slight beginning of a fit, which was stopped at once by suggestion, the patient waking April 11 in another beginning of a fit, stopped by suggestion.
Thereafter no more fits recurred at all. May 12, 1916, well.
Agoraphobia: Cure by hypnosis.
A captain was (with one lieutenant) the sole survivor among his battalion officers at Ypres. The captain received the D. S. O. for his gallant conduct in saving the remnant of his battalion. He now felt he could never face responsibility again and that he would disgrace himself if he ever got into danger. He developed a terrible dread of open places and became more and more depressed. When he heard that there was going to be an attack at Neuve Chapelle, he broke down but managed to get through the first day of the battle. He was worse off than ever in the evening, felt that he could not face another day’s fighting, was invalided home, and arrived in a condition of exhaustion and feeling of disgrace. He had bad dreams at night. Rest was insufficient to restore confidence. Hypnosis was followed by rapid improvement, and the man was soon able to get back to duty.
Re agoraphobia, see Section A, XI, Psychopathoses, and also Steiner’s case (182) of claustrophobia, in which shells were preferred to safety in a tunnel.
Stress on Eastern front; cardiac seizures; cellulitis: In convalescence, manual tremors. Treatment eventually by forcing and isolation.
A subaltern officer, 24, in civil life a student of mathematics, had serious hereditary taint on both sides (father, alcoholic; maternal grandfather, victim of “severe nervous disease”). As a boy he developed normally, and was a good student. He served as volunteer in 1911 to 1912, but in drill in 1913 he had had to be released from service on account of nervous heart and difficulty with respiration.
However, he was called to the colors at the outbreak of the war, and was subjected to tremendous strain in the eastern campaign; and he was put in the pack train at the end of November for cardiac seizures. He had a cellulitis with furunculosis following, and at the beginning of December there was suppuration of the whole right tibia. He was treated in hospital and slowly recovered.
At the beginning of March, 1915, without obvious external cause, while sitting in a café, the convalescent officer felt a cramp in his right hand, and strong movements of the hand to right and left followed. He was treated with bromides, but unsuccessfully. The tremors became more marked and then again from time to time grew weaker. Electric treatment increased the shaking to a maximal degree. April 27, the patient was brought to the nerve hospital at Jena.
The patient was a fat and muscular man, of average size, with very small ears and poorly-developed, adherent lobules, and syndactylism of the second and third toes of both feet; reflexes increased; marked dermatographia; a static fine tremor with rapid oscillations. The tremor became a positive tonus if the arm and hand were stretched out horizontally. Face and chest reddened easily.
Whenever any other voluntary movement was carried out (even slight finger movements of the left hand or of the right or left foot while lying in bed) this right-sided convulsive[765] tremor immediately disappeared. The movements could also be made to disappear by slight turning movements of the head or of the tongue. Moreover, when the mind was diverted, as in reading, the tremors ceased. When the patient thought intensely of some mathematical problem, he could bring his shaking to a stop. The left grip was stronger than the right. In the Romberg position there was a marked swaying to the left and backwards.
Subjectively, the patient complained of nothing but a circumscribed headache in the left parietal region and of sleep interrupted by frightful dreams. At first the condition remained unchanged. There was much insomnia, and the slightest noise caused fright. Headaches in the daytime also were produced by any noise, and these headaches were localized in the left parietal region. The tremors of the right hand persisted except as he caused them to stop as above mentioned. He could write well with his left hand. He would drum with his left hand on the table until the tremor of his right hand disappeared. He could play on the piano, playing first with the left hand until the right had become quiet. He was a very irritable man, passing into anger and extreme profanity at the slightest occasion, and it was very difficult to bring him to any kind of orderly activity or persistence in therapeutic measures. These consisted of baths, massage, and gymnastics, but they proved quite unavailing.
As the fellow got more and more intolerable, and as upon May 27 at about 9 o’clock in the evening, he disturbed the quiet of the entire hospital by a severe paroxysm of scolding, he was placed in a single room in the psychiatric department. He was placed in bed, cut off from all communication with others, and forced to carry out his exercises.
For two days he was surly, crabbed and obstinate, but then changed his demeanor completely; he became friendly and obedient. The tremor completely disappeared.
Five days later he was able to carry out all active gymnastic exercises with great energy and without the slightest disturbance in the right arm. At date of report he was busy in the garden.
Five weeks’ field service: Loss of speech. Cure by verbal and electric suggestion in three weeks.
A grenadier, 21, of healthy stock, physique, and habits, lost his speech, April 15, 1916, five weeks after going into the field. May 5, examination showed him a well-nourished healthy man (lively reflexes and slight dermatographia), able to communicate only by signs and writing. The laryngoscope showed almost complete immobility of the two vocal cords, which lay in the cadaveric position, as in paralysis of the recurrent nerves. In endeavoring to pronounce the vowels ā and ee the cords trembled but failed to move toward each other. The patient’s effort to speak was such that his head soon got deep red and sweat streamed from the forehead.
Speech exercises were started by passing the electric current through the larynx during the processes of laryngoscopy. The patient was meantime assured that his larynx was healthy and that he would soon learn to speak again. At the first sitting, the patient felt himself able to cough aloud.
After a few days, the patient was able to speak the separate vowels tolerably well, and was then made to go on with such words as Anna, Otto, Hurrah. The vocal cords began to move better. Fatigue was a feature of the first treatments, of such a degree that words that could be pronounced during the first part of the sitting were lost toward the close.
The grenadier assiduously set himself to say over and over again the words that he had learned, and would come to the sister radiant with joy at his success. In ten days he was able to speak again perfectly, though giving the impression of a slight stuttering. After three weeks hospital stay he was discharged cured and fit for service.
Struck by a rifle butt on right side of head; old wound of right thigh: Hysterical right hemiplegia and deafmutism. Treatment by faradization: Return of speech and improvement of hearing. Full recovery by suggestion. Hysterical CONVULSIONS developed BY HETEROSUGGESTION from convulsive neighbor.
A Russian corporal, 21, was knocked unconscious, September 13, 1915, by a butt of a rifle which struck the right side of his head. He came to in a short time. He was examined in hospital, early in October, and besides a small skin wound of the head, there was evidence of a wound on the anterior aspect of the thigh. There was paralysis of both right arm and right leg, and anesthesia of the entire right side of the body, face and even of the tongue. There were also pains over the whole right side of the body. The abdominal reflexes were present on both sides; the tendon reflexes were in excess on the hemiplegic side; there were no pathological reflexes of any sort. The patient’s hearing was diminished, and he could not speak at all although he could understand the speech of others perfectly.
Speech returned after a single séance of suggestion with faradism to the throat. Hearing began to improve. The patient’s suggestibility was a favorable factor in his cure, but there were some unfavorable features. One day, he saw a neighbor go into convulsions and proceeded to develop convulsions himself. These hysterical convulsions continued. According to Arinstein, such undesirable complications appear under conditions of extreme crowding of hospital patients suffering from shell-shock. Progressive séances of psychotherapy caused the disappearance of all the signs of paralysis, and at the time of the report, there was no disability, except that the full use of the hand had not yet been regained.
Shell-shock and burial; labyrinthine disease on one side: DEAFMUTISM. Cures, relapses and eventual cure by general anesthesia, more than four months after shock.
A private, 30, had been 12 years in the service. July 8, 1915, he was partially buried by a shell which killed two companions.
On admission to hospital he spoke a few sentences but was deaf, and next morning could neither speak nor read, nor did he take food for 36 hours thereafter.
Admitted to the King George Hospital, July 18, he was found stuporous, but started violently if touched, made signs indicating his wants, took no interest in surroundings, and resisted efforts to arouse him. He was without signs of organic disease. It seems that he had been a nervous child, with nightmares and fits.
July 24, he was given gas for dental extraction, partly in the hope that he would recover speech; but though he struggled violently, he made no sound. He had by this time become rather intelligent in a childlike manner, being pleased to see his small boy, but taking no notice of his wife. It transpired afterward that he did not recognize her.
Phonation in whisper now began. There was then a relapse, and for a week or more no food was taken. Such relapses with irritation and hypobulia and an obstinate constipation recurred; but improvement came on slowly. He became able to read short printed words, and later handwriting.
For another month there was no improvement and he lost heart and the will to get well, brightening up only when offered a motor drive or something else pleasant. He was transferred to an auxiliary hospital, against his will, September 18.
November 1, he was brought back to the King George Hospital, excited, shouting, struggling and evidently drunk. On[769] a day’s leave from the convalescent hospital he had come up to London, and in alcoholic elation began to laugh and talk. Morphia did not reduce his violence. He insisted on seeing the physician, to tell him the good news. Hearing was still diminished, though if attention were diverted, direct answers were given to some questions. Sleep followed.
The next day he spoke perfectly but could hear nothing. There was no further progress for three weeks, though he occasionally caught sounds. He now became bright and pleasant and had lost all irritability and sulkiness. Galvanic and faradic current had no effect on the ears.
November 27, after elaborate preparation to heighten the suggestive effect, the patient was kept in bed and given gas and ether up to the abolition of the corneal reflex. As he was coming round, the doctor shouted that he could now hear well. He was overcome with joy and had hysterical convulsions. He could hear, but with the right ear only. In point of fact, the left ear on examination showed signs of labyrinthine deafness. He was placed on home service.
Re etherization for functional deafness and mutism, Ninian Bruce maintains that ether is more satisfactory than chloroform. The loss of consciousness in cases of deafness and mutism ought to be a relatively slight one, and the patient should be suddenly roused to the realization that he is speaking. Recovery from chloroform anesthesia is, according to Ninian Bruce, too slow to allow the patient to catch the point that he is now speaking and hearing when he was formerly dumb or deaf. A failure with the method is a bad thing for the patient, as he loses confidence in the method, whereupon some other method must be resorted to.
Re etherization for deafmutism, see technic of Ninian Bruce under Case 553. Penhallow has a case in which during primary etherization the patient reviewed in a loud voice the whole story of his speech loss. He was found to have recovered speech and hearing after coming out of ether.
Re anesthesia by gas, Abrahams has used nitrous oxide for cure of hysterical paraplegia. Proctor also reports the use of light ether anesthesia for bringing out the voice of functional mutes.
Shell-shock functional deafness (five months). Yes-No test. Cure by suggestion on emerging from ether anesthesia.
A soldier was admitted to the Royal Victoria Hospital, Edinburgh, completely deaf in the left ear. He had been under shell fire a number of times in France and was eventually thrown down and made unconscious by a shell explosion on his left. He did not remember the noise of the explosion or anything until he found himself in hospital. After the explosion he had begun to stutter, and the stuttering had grown worse. Examination of the ear indicated that the deafness was functional. He was given ether and when just under was asked if he could hear anything spoken in his right ear. He said, “Yes.” With the right ear closed he was asked if he could hear when his left ear was spoken into. He said, “No.” This test was repeated several times. After covering his right ear, he gave his name, regiment, etc., in reply to questions whispered into his left (previously deaf) ear. The incongruity was pointed out. He was now suddenly wakened. He laughed hysterically with joy over his recovery.
But the next morning he was again stone deaf in the left ear. Blistering and electricity failed to produce benefit. He was, however, puzzled about himself.
After a fortnight he was again given ether and a little chloroform was added. The yes-no test was again positive. He was allowed to recover gradually from the chloroform, but he had now lost recollection of what had happened. The left ear remained deaf. Ether was again given. He was asked to close his right ear with his finger. While answering questions addressed to his left ear, he was suddenly awakened and immediately said that his hearing had come back. This return proved permanent. He returned to his dépôt. In the conversations under ether there was no stuttering. He had been totally deaf in the left ear for five months.
Blow in neck by rifle butt: aphasia, right hemiplegia and hemianesthesia, and especially (here MEDICAL suggestion) trismus: Recovery by anesthetic and suggestion.
A Russian soldier was struck in the head and neck by a rifle butt, and developed paralysis of right arm and leg with loss of speech. After the excitement experienced by the patient when exhibited to the students by the late Prof. M. N. Szukowsky in the neurological clinic of the Military Medical Academy, trismus developed.
The patient spent a year in various hospitals, the most diverse methods of treatment by drug therapy, electricity, and suggestion yielding no results. The patient had to be fed chiefly by nose and rectum, though small quantities of fluids were fed through the mouth through an opening formed by the falling out of one tooth in the upper jaw. The patient became greatly emaciated and weak and was, October 29, 1915, brought into the nervous wards of the hospital.
He showed flaccid paralysis of left arm and leg, together with anesthesia, analgesia and thermanesthesia over the whole left side of the head, extreme general atrophy of muscles, somewhat more marked on the palsied side. The temperature of the paralyzed half of the body was not lowered. No knee or Achilles reflex obtained upon either the affected or the healthy side (general exhaustion?). Abdominal and testicular reflexes lively. The pupils responded well to light. Corneal reflexes lively. The neck was held awry to the left, and the head was inclined somewhat downwards and leftwards; hearing on left side impaired. The jaws could not be opened even with the greatest effort. Wassermann reaction negative.
Patient thought himself incurable. Purves Stewart’s case, in which chloroform and oxide of nitrogen were used, was the basis of Arinstein’s treatment. It was suggested to the patient that he submit to narcosis with the proviso that he[772] would not be operated upon. His consent was secured; with the coöperation of others, the chloroform was administered November 6. The stage of excitability was not well marked. 8 gr. of chloroform was used altogether, by the drop system. Nevertheless, even with the weak initial excitability, the patient became capable of some movements with paralyzed hand and foot. On opening mouth, the patient yawned yet uttered no sound. Between the jaws was put a rubber insertion and upon awakening the patient was let see with his own eyes that his jaws were open and that therefore food might be introduced through the mouth. Upon repetition of the narcosis, 5 gr. of chloroform was used altogether, and the stage of excitability was this time better marked. To strengthen movements in the paralyzed extremities, the device of pricking the patient with a pin on the unaffected half of the body, with the unaffected hand and leg held horizontal by assistants, was adopted. The patient then made reflex defensive movements in the paralyzed extremities, especially the hand. At this point the narcosis was suspended, and the irritation with the pin was continued until consciousness returned. At this moment, the patient’s attention was called to the disappearance of the paralysis and his restored ability to move the paralyzed extremities.
From that time on, the patient’s condition underwent a sharp transition. Artificial feeding became unnecessary. The patient ate by mouth; the mouth was opened by the leverage of a small stick held by the patient between his teeth. Speech returned gradually. In reading aloud the patient aided the movements of his lips with his hands. At the time of report the patient spoke well, ate normally, had gained in weight, and with some effort could sit down and even stand and walk. All this was attained in a relatively short time after a whole year of paralysis.
The author felt that the success attained in this case gave him the right to use the same method where the cause was not a contusion.
Ten months’ field service; severe FEBRILE DISEASE: Afterward hysterical TRIPLEGIA, MUTISM, “JUMPING-JACK” reactions to stimulation of feet. Cure by anesthesia, verbal suggestion, faradism to palate.
A Russian private, 30, brought to a field reserve hospital, June 20, 1915, was in a grave condition diagnosed typhoid. By the end of June the general condition had improved and the temperature had fallen.
July 9, worse; happening to be in the company of a sanitary in a privy, he was observed suddenly to fall unconscious, with both feet and left arm paralyzed. Soon afterward he lost the power of speech. From September 30 to October 19, he lay in field hospital; but was then transferred to the nerve hospital with diagnosis: convulsive paralysis and aphasia. At entrance, complete paralysis of both legs and left hand; loss of speech and aphonia (speech understood). Upon touching a foot, strong convulsions developed with legs rapidly drawn apart and drawn together much in the manner of dancing toys. The mouth was twisted to the left. Though he silently opened his mouth and made rapid movements with the lower jaw, he could not utter a single sound, either vowel or consonant. Left hypalgesia. Hypesthesia of skin of hand and mucosa of tongue. Knee-jerks absent because of the strain of the muscles of the legs. Wassermann negative.
The history showed that the speech of the patient had been incorrect and indistinct from childhood. Moreover, in 1908, in chopping wood in the forest he had fallen under a sleigh and hurt his left hand, which had not since fully recovered. He had volunteered for the war.
The psychogenic character of the disease seemed clear. Suggestion was followed by ether narcosis, during which, on pricks of the healthy side with a pin, the patient made defensive movements with the paralyzed hands, and also[774] moved both legs. Speech was not regained either during or immediately after the narcosis, although the patient gave forth indefinite sounds. Speech was restored on the same day, September 7, with verbal suggestion and faradic brush applied to palate. The patient at once began to speak clearly and distinctly, read his prayer book, and described distinctly and in detail how he went to war. From that moment the convulsive movements in the feet disappeared, the region of anesthesia on the left side narrowed, speech was permanently reëstablished, and the patient began to move with his feet and finally began to walk after six months of paralysis. Before that time no medical treatment had had the slightest effect. The effort to stop mechanically the jerks even temporarily by means of plaster casts had been unsuccessful. In sleep the twitches ceased, but upon reawakening, even before full consciousness returned, the jerkings would resume. It is curious to note that upon falling asleep under the anesthetic the patient would issue always one and same kind of yells—“Help, there goes the German! They are shooting! Russians, do not yield!”
Re chloroform anesthesia, Milligan remarks that the treatment should be carried out in a quiet, single room, with the chloroform slowly administered and the suggestions made by the anesthetist during the optimal phase for suggestion,—just before the stage of involuntary struggling.
Shell-shock; unconsciousness: Mutism and musical alexia. Cure by anesthesia.
A private, 23, was admitted to the Duchess of Connaught’s Hospital at Taplow from Gallipoli, September 10, 1915. A shell had exploded behind this man. He had been picked up, unconscious, and remained so about a day. He recovered without the power of speech. Cerebration was slow at first but improved steadily.
The man had been a professional musician. Curiously enough, though his ability to read ordinary print was as good as ever, his reading of music was lost with the speech.
September 20, he was etherized, but being of a phlegmatic type, he was not readily excited and took the anesthesia very quietly. After perseverance, however, he was induced to talk. The ability to read music returned with the voice. He was discharged, October 4, 1915.
Re the use of anesthetics for curing deafmutism, Colin Russel rather disapproves of this method on the ground that no attempt is made to get at the genuine pathogenesis of the case and that accordingly there may be a tendency to recurrence.
Re the peculiar musical alexia, see discussion under Cases 353 and 450 of confusion and amnesia. The most highly selective amnesias have been found in confusional cases. However, Case 556 had been a professional musician and the effect may have been a highly specialized suggestion. See also Case 369 of Feiling for differentiated musical disorder. Mott has used the retained knowledge of tones as an avenue of approach in certain mute cases.
Shell-shock; burial (24 hours?); unconsciousness, 13 days: Deafmutism. Chloroform narcosis cured the deafness (!), not the mutism.
An Italian infantryman was buried under Mt. Zebio after shell explosion. After 24 hours he was found and dug out. He remained unconscious for 13 days and came out absolutely deaf and mute.
At hospital he was markedly depressed and cried very readily on being spoken to. The tympanic membrane had lost its sensitiveness to pain. As for the speech mechanism, the larynx proved negative. All the movements of the soft palate, tongue and vocal cords could be normally performed. The tongue was anesthetic to touch, but the taste function was perfectly preserved. The cheeks and various parts of the face were also anesthetic to touch, and the lobules of the ears could even be pierced with large pins without reaction by the patient.
He tried to pronounce labials, opening and closing the lips rapidly; but the expiratory movement was too weak, and not a single sound was made.
At the patient’s request, he was chloroformed. During a very violent excited phase, he did emit groaning sounds. The narcosis, however, did not put an entire stop to the mutism, since only a few inarticulate sounds could be emitted, and those only after great efforts. Curiously enough, however, the chloroform narcosis had caused the deafness to disappear entirely. Another narcosis upon the patient’s insistent request was given but remained without results, and at the time of report, the patient though cheerful and intelligent-looking, was still mute.
A soldier was out with a bombing party when a shell burst. He came to in a casualty clearing station, and was sent on to Salonica, deaf, dumb and jumpy. Two months later, an attempt at hypnosis failed; faradism of vocal cords failed.
The patient dreamed one night that if he vomited he could speak. Ipecac produced vomiting without speech. The patient, however, wanted a second dose, and while waiting for it, uttered an exclamation, which he did not himself hear, however. In the meantime, Dr. Smyly had been trying to hypnotize a second soldier, dumb but not deaf. This man’s dug-out had been blown in on him seven months before, whereupon the patient became very shaky, but did not become sick for a week. He was then sent to hospital, and his voice gradually disappeared. He suffered from violent headache and spasmodic movements of the arms and legs. Suggestion seemed powerless, and ether was unexpectedly given to the patient. While going under the ether, he said, “Oh dear, oh dear” several times indistinctly. It seems that another physician had already tried to cure the patient of dumbness by removing teeth without an anesthetic.
While this therapy was proceeding with the dumb man, the deaf-and-dumb man disappeared. It seems that the smell of the gas had caused him to take refuge on an outhouse-roof. The next day he had recovered voice and hearing completely, partly from shock and partly through suggestion.
The etherized patient did not recover voice but lost the spasmodic movements and his insomnia. A week later ether was again administered, and the patient was strapped down; as he was coming to, faradism was applied to the head and face. The patient then quickly recovered his voice and still retains it.
Shell wound: Hysterical dysbasia from contracture. Many methods of treatment fail. Success with “a new measure,” e.g. stovaine.
A sergeant was struck in the suprapubic region, December 15, 1915, by a shell fragment and got a large hematoma in the perineal region (shell fragment visible on X-ray). The man was treated a year in a center for physiotherapy and was then treated in a neurological center, where a faulty position of the right thigh maintained in extensor rotation and abduction was found. The patient walked on crutches, legs wide apart, balancing with body.
Upon transfer to Bourges, an intraspinal injection of stovaine (after withdrawal of 2-3 cc. fluid, 1 cc. stovaine, 0.07 to the cc., mixed with cerebrospinal fluid) was made. This reduced the contracture and permitted the patient to place his legs parallel. They were then bandaged in the parallel position. The bandages were removed two days later and the limbs did not reassume their faulty position. The man was shortly able to walk with a cane; progress was rapid. This man was very desirous of cure and refused to be invalided, believing he was to be cured, and had received medal and war cross. Simple motor reëducation in competent hands had been without effect. A new kind of measure, such as stovaine, proved successful.
Re “new measures” for hysteria, see items under Case 516. See also remarks upon cures by lumbar puncture under Case 488.
Burial: Hysterical dysbasia. Treatment by stovaine anesthesia.
A chasseur, buried June 24, 1916, had a number of general symptoms, apparently got well and was given seven days’ leave at home. On the way he felt abdominal pain which he thought due to the jolting of the car. Suddenly he felt his legs trembling on extension. He left the train and went into a hospital where a diagnosis of radicular and spinal lesions was made. Two months later he was sent to Claude who found that he could walk only with knees flexed. If he was requested to stand up and extend his legs on the thigh, a trembling set in suggestive of an epileptoid trepidation. Even in the horizontal position the same clonic trepidation occurred which only stopped if the patient flexed his legs on the thighs.
However, no sign of organic lesion could be found. There was an analgesia limited to the ankles. Psycho-physiotherapeutic treatment was unavailing. January 28, 1917, the stovaine injection method was tried. After anesthesia had set in, it was found possible still to produce the spastic state by extending the legs; but a half hour after injection the spastic state could no longer be produced. The patient was shown that the trepidation was abolished. During the period of return of sensibility, the legs were constantly moved and the patient constantly told to make movements himself. He was convinced of his power. There was no longer any clonus. The patient remained all day in bed without epileptiform movements. Next day he complained merely of weakness in the legs and was got to walk without having convulsive tremors. During the next few days he began to walk with a cane, later without support, and there were no more contractions except transiently in the left leg if the patient walked a little too long. He left the hospital cured.
Shell-shock deafmutism: Psychic treatment.
A soldier in a colonial regiment was sent, August 14, 1916, to an evacuation post with a diagnosis “deafness following shell-shock, unfit for service.” The patient asked that he be spoken to very loud because he could not hear, and he himself spoke in whispers. He kept watching his interlocutors’ lips and moved his own as if to pronounce the words.
A shell had burst nearby fourteen months before in June, 1915. After being in several hospitals, he was sent to an oto-rhino-laryngological service where he had his hearing reëducated and was taught lip reading. It was soon perceived that he could hear without lip reading and he was assured that he could be cured at once, but naturally he was not convinced. He produced a carefully filed paper stating “atrophic ozenous rhinitis, deafness from labyrinthine shock following shell explosion, hearing diminished 60 per cent right, 30 per cent left.”
However, energetic psychotherapy was started and in the absence of electricity, subcutaneous injections of ether were given. Such patients had always been cured, and a drug injected under the skin, not dangerous but extremely painful would cure him! This treatment was carried out in a dugout near enough to the lines to be daily “potted.” The patient was left for a space to reflect, and he finally accepted the chance of cure. He was exhorted to stand courageously the pain and to breathe deeply and to repeat a word more and more loudly. Finally he was made to speak normally and eventually to cry out loudly. He now felt much astonished, and in his astonishment forgot his deafness. He said that he had never spoken or heard since the accident, that he had been a deafmute from the first month of his illness, and that for the last three months he had been able to speak only in a whispered voice.
He should have been watched a few days to confirm the cure. This was impossible in the crowded dugout and no[781] risk could be run of his escaping. Kept over night he was found next day unable to hear and talking in the same voice as before.
He was now found to be either an exaggerator or a simulator. He was given a half hour to exercise his voice in and told that he must succeed unless he was a simulator. At the end of half an hour it was found that he had skipped. He was sent back by the division surgeon with orders to send him to the otological service for inquiry. The otological service found an atrophic ozenous rhinitis, a normal larynx, perfect audition. He was given a psychic X-raying and a few electric sparks were also drawn from his neck. He then began to talk in a loud voice and to hear normally. August 30, he was sent out completely cured and rejoined his regiment.
Re treatment of deafmutism by other means than pseudo operations and anesthesia, see remarks under Case 556 concerning Colin Russel’s opinion that anesthesia does not get at the true genesis of cases. Re the teaching of lip reading to Shell-shock deafmutes, see discussion under Case 580.
Brachial monoplegia. Cure by electrical suggestion (physician bored-looking, brief, and authoritative).
Adrian and Yealland had occasion to treat an officer with a persistent functional paralysis of the arm, which had successfully withstood hypnotism, psychoanalysis, rest, massage, anesthesia with ether, and painful electrical treatment.
This patient knew something of the functions of the brain and was prepared to discuss his condition exhaustively. He was told, however, that he had come to be cured and that the nature of his cure would be explained to him afterwards. Without further discussion, the motor areas of the cortex were mapped out rapidly. The measurements were repeated aloud to impress and mystify the patient. He was assured that as soon as the shoulder area of the cortex was stimulated faradically, he would be able to raise his shoulder, and that then the rest of his arm would recover. An exceedingly mild faradic current was then applied to the scalp for a few moments and he was then ordered to move his shoulder. He did so at once. In a few minutes, all of the paralysis had vanished and the patient could raise 30 pounds. Adrian and Yealland believe that the success here was largely due to the fact that the patient was not allowed to discuss the case or criticize the treatment beforehand.
It is essential that the patient should be convinced that the physicians understand the case and can cure him. No physical sign should be examined as if it were interesting or obscure. An attitude of “mild boredom bred of perfect familiarity with the patient’s disorder” is cultivated. If the case is exhibited it should be exhibited “as a perfect example” of the type of case that is cured in five minutes by appropriate treatment. “Rapidity and an authoritative manner are the chief factors in the reëducative process.”
Re psychoelectric treatment, see Yealland’s book, published while this compilation was going to press, Hysterical Disorders of Warfare, 1918.
Brachial monoplegia following use of sling after bruise or wound. Technique of electrical suggestion and rapid reëducation.
Adrian and Yealland give the following typical case of paralysis of the arm as a very frequent and very curable form of war neurosis, occurring as a rule after a slight wound or bruise necessitating the use of a sling. The patient, having received a slight wound of the forearm, for months had a useless arm, which he could move but slightly at the shoulder on exerting a superhuman effort. Occasionally he could flex the fingers through a small angle. There was complete anesthesia of the hand and arm of long-glove type. This anesthesia was not complained of, and might not be noticed until suggested to the patient by the physician. It is well to elicit the anesthesia, however, in view of the treatment to be applied. There was no wasting of muscles; the sensory loss was typical of hysterical anesthesia; nor could the whole arm have been involved by an injury that did not affect the upper arm and shoulder.
The patient was told that he was very lucky to have come off with such a slight injury; his arm was to be set right in five minutes by the application of a special form of electricity. He was then made to sit on a large pad electrode connected with an induction coil; the other terminal is connected with a wire brush. The first effect, he was told, would be the return of feeling in the forearm; power would return with the feeling. The wire brush with a fairly strong current was drawn downwards over the forearm from elbow to wrist. He was told that he could now feel as far as the wrist, and a pin was used to convince him that he could thus feel. If he had not felt the pinprick, the current would have been increased in strength until he could feel. The hand was now treated in the same way.
He was now told that, as feeling had returned to the arm, the power of movement would be restored shortly. Adrian[784] and Yealland remark that laymen seem to consider that loss of power and loss of feeling are inseparably connected. The electrode was now used to produce contraction in the muscles. Under these circumstances, the arm will be used hesitatingly, with an appearance of great effort; but the patient is nevertheless convinced that power is returning.
“Rapid reëducation follows at once. He is given no time to think, but urged to move the arm more and more strongly, to grip the physician’s hand, to flex and extend the elbow, etc., and the pressure is not relaxed until the whole arm has returned to its normal vigor. If recovery is stationary, faradization is repeated with stronger and stronger currents. If it seems as though he might relapse on leaving the hospital, he is told that this is very unlikely, but that if it should occur, he should report sick at once and come back for treatment with a current far stronger than that already used.”
Adrian and Yealland claim that they have applied their combination of suggestion and reëducation in more than 250 cases (including 82 cases of mutism, 34 of deafness, 18 of aphonia, 37 brachial or crural monoplegia, 46 paraplegia, 16 hemiplegia, and 18 of non-organic gait disturbance), and that although a majority of the cases have been of several months’ standing, treatment has been almost immediately successful in at least 95 per cent of the cases.
Exposure in the retreat from Mons: Persistent hysterical sciatica. Treatment by faradism and verbal suggestion.
A soldier developed pains about the hips and down the right thigh after getting wet through in the retreat from Mons, August, 1914. He was treated for a period of nine months in various convalescent homes and military hospitals, incidentally receiving forty baths at Droitwich. He hobbled on a stick, leaning upon the left leg and dragging the right stiffly. The thigh was tender and hyperesthetic.
The proper treatment of cases of hysteria, according to Harris, is strong faradism, applied by a small electrode or wire brush to the moistened skin. The stimulus is made powerful enough to force the patient to admit that he feels. The theory is that the powerful stimulation “breaks down the psychical auto-inhibition which produces the hysterical anesthesia.”
Faradism is only the first phase of the treatment. Verbal suggestion follows. Building on the basis of the feeling produced by the faradism or on the basis of the ocular evidence of motion in the hitherto paralyzed muscles, the patient is informed that the electricity will now be more and more strongly felt and that he will be cured in a few minutes.
The two elements in the therapy, then, are: encouraging verbal suggestion and the suggestion afforded by the paraphernalia of a complex looking, noisy machine. The knowledge on the part of the patient that a powerful and mysterious stimulus, namely, electricity, is being employed is a third element of suggestion.
Persistent hysterical sciatica, such as that of the present case, may require prolonged treatment. In this instance, the man was completely cured in five minutes, so that he was made able to run across the room. He said he would now be able to go back to the front, and wondered why he could not have been cured before.
Prognosis of intensive reëducation in reflex (physiopathic) disorder—complete recovery (except for the hysterical fraction of the disease) not expected.
A young soldier was superficially wounded in the left knee, in August, 1914. A year later, he showed amyotrophy of the left calf, which measured 2.5 cm. less than the right, a weak slow Achilles reflex on the left side, cyanosis and hypothermia of the left foot, weakness and limitation of movements in the left foot, with slight contracture in flexion of leg upon thigh.
Thenceforward and for eight months, this soldier was submitted at the Tours Centre to intensive reëducation. For two hours every day upon prescription he walked, ran, and hopped upon the left leg. In September, 1916, after twelve month’s training, there was a certain improvement in his disorder. The leg was now completely extended upon the thigh, and the amplitude in the movement of the foot was almost normal; but the amyotrophy, vasomotor disorder and certain electrical disturbances remained quite unchanged. The man himself recognized that his status was greatly improved, but he could not walk more than four or five kilometers without great fatigue.
In view of the inferior results of reëducation in some of these cases, should any attempt at all be made to reëducate? Vincent thinks that that should be; but that it should be borne in mind that sometimes no results may be obtained. If the reflex disorder (in the Babinski sense) is minimal and the chief difficulty is hysterical, then sometimes the man may go back to service after reëducation; but in intense examples of reflex (physiopathic) disorder, invaliding has often proved necessary.
Re values of intensive reëducation, Vincent’s technique and results have logical resemblances to those of Yealland and of Kaufmann. Vincent established in the 9th district neurological center a method of intensive reëducation which[787] is particularly suited to old hysterical cases. He divides the treatment into three stages: First, the stage called by the poilu by the picturesque name of torpillage; secondly, the stage of fixation; thirdly, the stage of training. According to Roussy and Lhermitte, there are few cases at the front suitable for the treatment of Clovis Vincent, which is especially devised for the old cases. See under Case 574 for further details of Vincent’s treatment.
Re prognosis of the physiopathic disorder, there has been some controversy in France. See discussion under Case 530. Re suitable treatment for physiopathic disorders, Babinski and Froment suggested the application of heat. The warm bath test is also of value in diagnosis. Babinski and Froment claim progressive improvements with hot baths, hot air douches, and light baths—but counsel great prudence. The improvement is never rapid.
Wound of calf; operations: hysterical contracture with “physiopathic” features. “Brutally conquered” by reëducation.
A French infantryman, class of 1912, was wounded, May 12, 1915, in the upper third of the right calf. His posterior tibial artery had to be ligated. In a few weeks the wound was healed, but he began to walk badly, presenting a contracture of the calf with retraction of the tendo Achillis.
Toward the last of 1915 a surgeon under the impression that the disease was organic cut the tendo Achillis but the soldier could not walk any better. As he could not take the position of equinism, he semiflexed his knee and walked upon a crutch.
Another surgeon was now found to perform a tenotomy on the flexors of the leg and put the patient in a plaster cast to correct the flexion and immobilize in extension. This second operation was in July, 1916. The patient now walked without a crutch.
He was then sent to a neurological center, Dec. 8, 1916, walking on two canes, right leg in forced extension on thigh, in permanent and absolute contracture. All movements except leg flexion could be executed, though slowly and weakly; but positive movements were impossible, except flexion of the knees. There was no sensory disorder. Reflexes were normal save that the leg reflexes were a little stronger on the affected side, and the patellar reflex on that side was nullified by the contracture. Electrical reactions proved normal. There were marked trophic disturbances of the right foot and of the lower third of the lower leg. There was a certain amount of edema, cyanosis, coldness and thickening of skin; marked muscular over-excitability of the distal extremity of the leg. In short, Ferrand was here dealing with a case of Babinski’s group of the so-called physiopathic cases. The[789] man was somewhat feeble-minded, and anxious and a trembling suppliant for cure.
He was put, December 15, in a reëducation room and by means of fatigue, induced by violent physical exercises, was (Ferrand states) “brutally conquered.” The contracture after a half hour of physical movement of flexion and extension of the leg ceased. The patient was shown how he could himself both flex and extend the limb himself; he was then caused to do this spontaneously. These active movements were aided and at times provoked by somewhat painful galvanic discharges. The patient then walked slowly, and flexed both knees to the maximum. He was cured after a treatment of 2½ hours. There were, of course, some (surgical) intra-articular adhesions in the knee and it was necessary for the patient to break these adhesions. An X-ray had shown the bone to be intact. A slight hydrarthrosis developed the next day, but a few days later he was able to walk as well as anyone. For five weeks he followed a training platoon in the reëducation work and was evacuated, January 23, 1917, to his station, though he had entered the neurological center with the idea that he was to be invalided with a pension.
He had a few relics of physiomotor disorder when he left, including the abnormal delicacy of skin and muscular over-excitability above mentioned. On the basis of this and similar cases Ferrand believes that, although the physiopathic group of Babinski exists, it does not signify a separate clinical syndrome and the occurrence of physiopathic symptoms does not contraindicate psychotherapy.
Re this controversy, see remarks under Case 530.
Shell-shock: Paraparesis. Cure by electricity.
Turrell, in a paper on electrotherapy at a base hospital, narrates a case of spinal concussion which rapidly yielded to the persuasive influence of Bergonié’s machine for electrically provoked exercises. Turrell grants that such a rapid cure would probably be attributed to suggestion, but thinks that the term demonstration might be preferred on account of the vigor and amplitude of the muscular contractions excited.
This soldier was driving an ammunition wagon at the front, when a shell exploded under the wagon, killing one horse and severely wounding the other. The patient himself was blown into the air, fell, dragged himself to a trench where he lay all night, and found himself in the morning unable to walk or stand. He recalls that pins were stuck into his legs by the examining medical officer and that they produced no sensation. When he was finally brought to the Third Southern Medical Hospital, he was unable to draw up or move his legs, or to stand up (yet neurologically normal).
After a few days’ rest in bed, he found himself able to walk a few steps with assistance, and was then transferred to the Radcliffe Infirmary for electrical treatment. This treatment consisted in electrically provoked exercises to the back (positive) and seat and thighs (negative). He was able to walk back to his ward, leaning on a wheelchair. Next day he walked to the electrical department with sticks, and after the exercises were repeated, he was found able to walk without assistance. On the third day, the Morton wave current was applied to the back, to clear up any persistent stiffness. The patient was then discharged on sick furlough.
Re the Morton wave and similar applications of electricity, Zeehandelaar speaks of a high frequency hall fitted up at Berlin. Touching the walls of the hall with the finger elicited a powerful spark. The scheme appeared to be on a commercial basis, and it was proposed to start similar institutions for poor metabolism and neuroses in other cities.
A year’s field service, gunshot; typhoid fever: Astasia-abasia: Lourdes-like cure: Residual amnesia.
A soldier in service from the outbreak of war, shot in September, 1915, afterward suffering from fainting spells, was treated in several hospitals. He developed a typhoid fever at Lindau, which was at first taken for hysterical fever. Eventually he came to the observation of Voss, unable to stand and falling hysteria-wise if compelled to walk.
Thorough examination was made. It was emphatically explained to him that there could be no reason why he should not stand or walk.
A miracle occurred. From the second day of his hospital stay he not only walked about but began to polish doors and windows with inexhaustible strength.
But when he was about to be told that he must now be looked upon as well, the miracle was not so manifest. It now transpired that he had serious gaps of memory and disorders in recognition, a sphincter disorder and ever since his typhoid incontinence with fluid feces.
In short, waking suggestion had caused a very prominent symptom to disappear, but the total personality remained sick. According to Voss, the procedures of Kaufmann are dubious just because they cannot stand the test of time. Yet so far as the cure of this man’s astasia-abasia was concerned, it was not at all unlike the cures wrought at Lourdes.
Re miracles of this sort, see cases of Colin Russel (503 and 504) as well as those of Veale (511 and 512). Voss’ arguments run parallel with the contentions of various persons that the miracle cures (such as those by anesthesia, electric suggestion, and hypnosis), do not get sufficiently to the bottom of the affections in question. Buzzard, in the preface to Yealland’s book on the Hysterical Disorders of Warfare, remarks that the question of the ultimate prognosis in cases thus suddenly cured must be left unanswered.
Dysbasia after a fall: “Kaufmann” cure in six weeks.
Severe dysbasia, due to monoplegia of the right leg of sudden origin (a fall), was variously treated 64 weeks without effect.
July 15, 1916, the patient walked in on a stick, and fell down on trying to walk without. August 1, 1916, at 9 o’clock, he was rapidly examined: Anesthesia to pain and temperature; inability to lift right foot; the right knee could be lifted about a hand-breadth above the body if the foot was supported.
At 9:10, a small electrode was applied: sensibility became normal at once. Second application: leg raised much better. The man was told that he was better and that his hand could be put under the heel. Third application: Leg raised 8 cm. The patient showed pleasure at the advance. Fourth application (slightly increased strength): Patient able to stand and to lift knee with flexion at 135° while standing. Walking exercises under direction. At 9:30, five minutes recess was given for fatigue, whereupon the exercises were taken up again and transition made from stationary running to walking without aid as well as a variety of other associated acts (grasping handkerchief instead of physician’s hand, and the like). The patient became exhausted after 8 or 9 minutes running about, and another pause was given.
The large brush electrode with stronger current was now given to the back and to the back of the right leg. Practice in slow walking, lifting knee, and holding hip joint firm. The patient became tired, but remained very willing. Exercises in pulling on stockings, in climbing stairs—the whole concluded at 10 o’clock, whereupon it was found that the patient could walk alone for a distance of 50 meters. The patient was a very suggestible one. It was striking that the patient in the time between 9:35 and 9:40 minutes could[793] walk better on the right (that is, the previously affected leg) than upon the left. Rest in bed and phenacetine were ordered, with the suggestion that in the morning he would walk much better. He became irritated after the treatment but grew quieter in the afternoon.
On August 3, he was found able to walk well, better when not observed than when observed. August 5, he complained that his leg was worse and used a cane, without permission. He was roundly scolded by the physician and threatened with being sent to bed if he did not practice earnestly. August 7, he was better, and confessed that he could not walk as well on command as he could alone; the exercises were nothing but a fraud and he could go out and beat everything up (alles zerschlagen) if he did not have to carry out such exercises.
August 15, he was much better, quiet, and satisfied. The lameness was practically gone. August 30, there was no sign of lameness, even when he was observed. According to Schultze, the Kaufmann method is not merely an Erb tradition, and rather special measures need to be taken in executing it.
Re Kaufmann’s cure, Imboden sums up this “highly logical and brutal method” as a method in which powerful electric shocks and loud military orders to perform certain exercises secure results. Imboden suggests that relapses may follow, sometimes on the slightest provocation. Mann states that Kaufmann’s method of suggestion and electric shock forms very good treatment; yet Mann states there have been two deaths under this treatment: in both instances there was an enlarged thymus at autopsy. A better technique, especially the use of the faradic current alone, might have avoided these deaths. Mann himself prefers to Kaufmann’s Ueberrumpelung milder methods, such as rest. Kaufmann keeps up the sitting until the man is cured, even if it takes two hours of electricity and staccato commands. For similar persistance, see the treatment by induced fatigue of Reeve (Cases 489-493).
Wound of shoulder: Heterosuggestion of BRACHIAL paresis. Electrical suggestion of muscular power. Recovery in five days.
A reënlisted soldier arrived at the Royal Victoria Hospital, as a case of ulnar paralysis. He had been wounded in France six months before by a bullet which passed through the fleshy part of the shoulder, above the middle third of the clavicle. Power in the right arm gradually diminished; yet two months after the wound he seemed fit enough to be sent to Egypt. The paresis developed, and in a month’s time he was invalided home. He had been unable to use a rifle for months.
The healed bullet wounds were found about the region of the brachial plexus. The patient was sure the bullet had damaged the nerves in that region. The right arm and hand were limp and over-inclined to blueness, and the muscles were flabby. Active movements of all sorts could be carried out with the arm but not against resistance. There was a definite anesthesia and analgesia throughout, and responses to touch and pain stimuli were irregular.
By way of treatment, the patient had the muscles of the paretic arm stimulated electrically, and at the same time he was told that no nerve of the neck had been injured. He was greatly surprised to see his palsied arm move vigorously.
A milk isolation treatment in bed behind screens was adopted, whereat the patient was angry, looking upon the Weir-Mitchell treatment as punishment.
On the next day, another electrical application secured complete power in the arm and abolished sensory disturbance. Three days later the man went back to full duty. According to Fergus Hewat, someone doubtless had suggested to this patient that he had received a nerve injury. He had become obsessed thereby and developed a typical functional paralysis. This was a “cortical misinterpretation,” which disappeared upon forcible demonstration of the error.
Exposure; intestinal disorder in weakminded neuropath: Camptocormia and hysterical paraplegia: Cure by psycho-electric treatment.
A French territorial, 45, was observed at the Centre Neurologique, August 28, 1916. He was a victim of hysterical paraplegia with tripod gait. There was a stiffness of the lumbar vertebral column which had lasted six months. This paraplegia had begun spontaneously after cold and an attack of diarrhoea followed by constipation. The camptocormia and disorder of gait had come on gradually in the ambulance. He came on a stretcher. He was found to be able to walk with great difficulty by leaning both hands on a cane. The two legs were tremulous in a pseudospastic gait. The next day, after a single psycho-electric treatment, cure was complete. This patient was mentally somewhat weak and a constitutional neuropath. He was discharged, cured, October 20, 1916.
Brachial monoplegia, hysterical (or feigned?). Found able to descend ladder with arms only.
Claude had a case of a soldier with right-sided brachial monoplegia, which had lasted for 18 months and defied efforts to cure. There was a question of simulation, and Claude handed the case over to Vincent.
The case came on service, June 20, and was seen June 21. He was then treated and found able to descend a ladder applied to a wall with the help of his arms only. On June 24, he was found able to lift a weight of 10 kilos, and could now write with the right hand, although he had been writing only with his left. This man had looked like a simulator to many physicians. He may have been a simulator or an hysteric. In any case, he was cured.
Vicissitudes of treatment of hysterical brachial monoparesis (shell burial).
A French private was buried in a trench upon the explosion of a large shell, November, 1914. He said he had had a “fracture of the occiput” and had fainted away without regaining consciousness for several hours.
He was evacuated to Dunkirk, then Saint Nasire, and then to Sables-d’Olonne. He showed no paralysis or paresis of limbs. During the first month, he had violent pains in the head, spells and vomiting. There was a slight aphasic disorder. He was treated by cupping upon the head and by applications of ice.
After the visit of the inspector general, he was sent to Nantes to be trephined. Dr. Mathieu regarded an operation as useless. He was treated with bromides and the faradic current by Miraillé, applied to the right arm, which had become paretic.
June, 1915, he started on a three-months convalescent leave in Paris.
From October to December, he had electric treatment at the Grand-Palais.
December, 1915, he went to the Salpêtrière under P. Marie, where he was given electric treatment.
January 1916, he went to Maison-Blanche under Laignel-Lavastine, where he was given electricity 4½ months.
April 4 he went back to his dépôt.
Presented to the invaliding board, May 11, at Decize, he was sent to the neurological center at Bourges. He was there given massage and movements. Upon entrance he had a functional inactivity of the right arm. He should have been cured a long time before by the therapeutics employed. He was then sent to Vincent at the neurological center at Tours for special motor reëducation. Vincent found almost complete functional incapacity of the right arm, without atrophy, with normal reactions, no R. D., and normal arterial[797] pressure. June 26, 1916, the patient was able to write, although slowly. He could sign a letter, and could lift a weight of 10 kilos.
The details of Vincent’s method mentioned under Case 566 are pursued, to use his own words, with methodical ruthlessness. This form of reëducation consists in manoeuvres that make the patients yield despite themselves. The galvanic current is used to force a man to react voluntarily or automatically. See, for example, Claude’s case of a hysterical brachial monoplegic (Case 574) found able to descend a ladder with the use of his arms only. After the physician’s victory is secured, then a sort of consolidation must be obtained by means of the execution of certain movements on the part of the patient for an hour or two. As another factor in the situation set up by Clovis Vincent, is the enthusiasm generated in the moral atmosphere in which the cure takes place. Mott has also insisted upon this atmosphere of cure, which Mott believes is in part responsible for the good results of Adrian and Yealland. Roussy and Boisseau, at Salins, started out with a process similar to that of Vincent, with a preliminary period of isolation. Roussy also uses the faradic current instead of the galvanic (see remarks of Mann concerning deaths with the Kaufmann method in Germany, under Case 570). Vincent’s three stages are given in Chart 19, page 897.
Struck by shell fragment; run over by shell; paresis and regionary sense disorder. Treatment by reëducation.
A German subaltern officer, 27, was wounded September 25, 1914, in a battle in France. He gave the following account:
“We had been firing without interruption four days, and then were sent back. While going back from cover we were under shell fire. Three or four horses fell. I got a glancing blow from a shell fragment in the back of the head, and fell down. I was not quite unconscious. I tried several times to get up, but I could not, for I had very bad pains in the head and a confused feeling in it, too. I remember also that a wheel ran over my foot, and that I got a sharp blow in the chest. Then I was unconscious for about an hour. When I awoke, there were two comrades busy over me and they pulled me back of the firing-line. Then I got to a field hospital.”
The man arrived at the nerve hospital (Jena), October 8, 1914, with insomnia, respiratory disturbance, sudden perspiration, feelings of cold in the right foot, and poor appetite. He had had nausea for a few days. Lungs and heart proved normal. X-ray of the right foot showed normal relations. The man was a small, powerfully-built man, well nourished, with lively reflexes, especially the knee reflexes, of which the right was greater than the left; slight patellar clonus, right; left plantar reflex greater than right; segmental disorder of touch and pain sense in the right foot and lower leg, a zone of analgesia lying above the zone of total anesthesia. Gait was lame on account of inability to move the right ankle joint. In walking, the right foot was trailed.
Treatment was suggestive and supported by active gymnastic exercises, breathing exercises, exercises in moving the right leg, massage, faradism and local hydrotherapy. The gait gradually improved, the cold feeling disappeared[799] from the right leg, disturbances of pain and touch sense disappeared. The patient was released on the 2d of February, 1915, capable of garrison duty.
With respect to this man, who was married, he was from a healthy family and had healthy children. He is said, however, to have suffered from convulsions for a long time in early life, but thereafter had never been sick in any way. He was a good student and had been a post-office official since 1908. After two years’ military service, he became, in 1910, Unteroffizier-Aspirant. Later he was advanced to his subaltern position in the reserve.
This case seems to be a characteristic example of segmental disorder of sensations of both touch and pain, combined with a paresis in the same region. Mechanical and mental factors seem to have been present, and the case belongs in what Binswanger calls the “hysterosomatic” group.
Re Binswanger’s so-called hysterosomatic group, he defines the cases as having emotional, mechanical, and toxic (gas) factors. On the whole, they are best classified as a kind of psychoneurosis. Binswanger finds all physical and drug treatment without result except as supportives. He has used hydrotherapy and electrotherapy with the perfectly clear conception that the procedures were of suggestive value only. In fact, Binswanger had before defined such procedures as Realsuggestionen or material suggestions. Common verbal suggestion, says Binswanger, will work sometimes only when aided by these material suggestions. See also under Case 576.
Post-traumatic (ANTEBELLUM) seizures with unconsciousness: Further seizures, astasia-abasia, anesthesias, following no special period of stress in field service. Recovery by reëducation.
O. F., 26, healthy, of a healthy family, in military service, 1908-1910, a miner in October, 1912, had fallen into a shaft from a considerable height, and is said to have been unconscious for three days and two nights and to have had some sort of attack a short time after waking. Later he had another attack, beginning with violent headaches, running from the back to the fore part of the head, then dizziness, then a fall with unconsciousness. The whole attack lasted about four minutes and was followed by feelings of extreme fatigue.
It seems that in the spring of 1913 these attacks had begun to repeat themselves two or three times a week. In the spring of 1914 there had again been two attacks at an interval of two weeks. They had occurred on the way to work and had been introduced by the same symptoms as before. They lasted about half an hour.
He was in the war in France from August 6, 1914. While he was cooking, one day, in the middle of September, he had an attack and this without special occasion. The next attack occurred a little while afterwards, at the time of an assault. He said that he fell down and lost his senses. When he came to his senses again, he found he could not move his legs.
He was taken to a reserve hospital in Germany, and while there had several attacks with unconsciousness and spasmodic convulsions—the last on December 7, 1914. He was transferred to the Jena Hospital on the 11th.
The Jena examination had the benefit of an inquiry concerning the case. It seems that he had left the field hospital in the enemy’s country, in a half-conscious condition, and rode away therefrom aimlessly. It was only in Germany[801] that he, on his own story, found his bearings again. However, upon admission the disturbance in walking was very noticeable, since the patient came hobbling through the garden of the clinic with the upper part of his body bent forward, and with the support of two canes. The legs were moved with difficulty; he seemed to take short, tripping steps, with the toes dragging on the ground. His inability to walk he explained through the violent pains which he would feel in the joints of the legs and an extraordinary weakness in his legs.
Physically, the man was a tall, strongly built and well-nourished subject. Neurologically, the knee-jerks were somewhat decreased and weaker on the right side than on the left; the Achilles reflexes were lively. The plantar reflex was not obtainable on the left side; decreased on the right. The abdominal reflexes were absent on both sides.
Most remarkable was the general diminution in sensitiveness of the skin to touch and pain, involving the whole body, up to the neck, where the sensory impairment abruptly ceased in a sharp line. The anesthesia was not everywhere complete. In a few places pencil strokes were successfully localized and recognized. Deep pin-pricks were everywhere recognized as itching. When the trunk was everywhere examined on both sides symmetrically, a strong pressure with a pin-head was felt as a strong pressure on the right side, but was felt not at all on the left side. Anesthesia and analgesia were total in the legs. Deep folds of skin could be punctured by needles without reaction.
The legs could be moved freely upon urgent request with the patient in dorsal decubitus. Still these movements were slow and difficult, as explained by the patient, on account of violent pains in the joints. If put on his feet, he would begin to sway greatly and permit himself to slide down to the ground, stating that he was quite incapable of standing or walking without aid. With two canes, however, he could move freely about in the ward and in the garden, and even with considerable speed, in a peculiar, dragging, shuffling way; in the execution he gave no sign of pain, contentedly smoking a cigar or a pipe.
While his status was being taken on admission, he became suddenly dull and irresponsive, with a staring look. He could not state his age or his birthplace. However, he became clear shortly, upon urging, and explained the spell by saying that the blood had risen to his head. A few days later, he was transferred to the psychiatric division. He was given strict rest in bed, smoking was forbidden, prolonged baths were used, and the legs were massaged. He felt very comfortable in the prolonged baths and could then move his legs without pain.
A few days later he was taken out of bed several times a day, the canes being removed immediately, and he was led about the day-room with the light support of two nurses. Being promised a cigar as a reward, he proved able to walk through the day-room supported by but one nurse. A week later the pains in walking exercises had disappeared. He had become able to walk alone, supporting himself lightly along the wall with one hand. Walking was still uncertain and slow.
December 20, the patient could stand free without support, swaying slightly; improvement became rapid. He could shortly stand and walk without support though his walk was still awkward and on a wide base with knees pressed in and body bent forward, soles were kept applied to the ground. December 22, the patient could walk in the garden without aid.
December 23, there was a spell of great weariness and complaint of being sick. The patient lay down on the bed, cried aloud, and had rhythmic twitchings and sudden movements with arms and legs. He scratched the right half of his face with his right hand. This spell lasted about a minute. It was repeated in the same way twice within the half hour.
He had complete amnesia for these attacks. The pupillary reactions were entirely normal in the attacks. He had been in bad spirits that day because a Christmas furlough had been refused. The attacks provoked no bad consequences and his gait improved. He was on furlough from the 30th to January 3; on the 4th he was transferred to the nerve department, but on the 12th of January he was reprimanded for a breach of discipline, whereupon at 9:15 he had[803] an hysterical attack with the same coördinate rhythmic motions as before. This attack lasted about 20 minutes. Two hours before the attack he had complained of weariness and a boiling-hot feeling in the body. Long walks were taken. On February 15 he began to feel very happy. He was informed that the charge against him for leaving his troop had been dropped. He complained of sudden weariness and headache and was markedly depressed, but he had no hysterical attack.
After February 23 he took part regularly in gymnastics, executing the movements with joy and without special weariness. He wanted to be discharged. He was discharged as fit for garrison duty and he has since gone back to field service.
Re gymnastics, Binswanger holds that they have a special value in overcoming inner psychic resistances and weak-willed persons. The Realsuggestionen (see under preceding case, 575), such as hydrotherapy and electrotherapy, serve to concentrate the person’s attention on certain regions. These regional suggestions then smooth the way for the curative suggestion, namely, the constant and monotonously repeated assurance that recovery is advancing. At the next stage, according to Binswanger, gymnastic exercises may be brought in to overcome hopelessness, indifference, or exaggeration of morbid feelings. Binswanger sets methodical tasks for the attention and the will (a so-called Uebungstherapie). If these gymnastics lead to manifest improvement, then a proper educational therapy is prescribed, which is no longer a merely exercise therapy, but consists of actions of actual value in hospital routine. The convalescents are gradually led to carry on housework, food service, gardening (the latter under supervision). Hospital clerical work is a suitable occupation. Re supervision over gardening, mentioned by Binswanger, Canadian experience indicates that the idea of supervision may be greatly extended. Particularly is this true in vocational reëducation. Kidner describes the functions of a vocational counsellor, who has to have an expert knowledge of industry and methods of industrial training, as well as an acquaintance with the varying[804] demands for workers, a knowledge of the seasonal variations in employment, and a knowledge of occupational diseases. Re occupational therapy, Todd estimates that from 0.5 to 1 per cent of wounded men in France will require vocational reëducation. Occupational therapy is the proper vestibule to vocational training. He lists the following forms of treatment used in institutions for vocational reëducation:
Central specialized institutions such as those developed in France are necessary, and such centres should be large rather than small, according to Todd, and should contain not less than 200 beds. Todd insists that work is, after all, the most important measure of reëducation; and Turner, speaking of the home for neurasthenics at Golders Green, says that during a period of three months (the number of the patients is limited to 100, and three months is the limit of stay), the vast majority, even of the most obstinate cases, get well through the effects of sympathy and insistance upon work. Near Golders Green is the Maida Vale Hospital for nervous cases, so that in case of need the physicians there may treat the patients. Salmon gives a list of the occupations which are suitable for these cases.
Blown up by shell; wounds, right side, distention and bloody urine: Paresis of right foot and spasticity of hip; later rectal and bladder incontinence.
A Russian from the Ukraine was received at the nerve hospital, Jena, December 12, 1914. Through an interpreter it was established that he was a peasant, had been under shell fire in a skirmish at the beginning of November, and had been hurled (so he said) 1¼ meters into the air without loss of consciousness. There was a wound of the right shoulder and also, he thought, of the legs, from the air pressure. Becoming a German prisoner, he had been treated in various hospitals.
He was a strong man of medium height, with a healthy complexion. There were two healed wounds of the right shoulder, and near the twelfth spinous process a third similar scar. There were a number of ulcers and furuncles over the os sacrum.
Neurologically, the knee-jerks and Achilles jerks could not be obtained, and the plantar reflex, extinct on the left, was weak on the right. Sensitiveness to pain on both sides was lost from the knee downwards but there was hyperalgesia in the thigh. Inaccurate statements in response to tactile tests were made, apparently on account of lack of understanding. In lying down, there was a slight restriction in the movements of the legs, and active movements of the joints of the foot on the right side were impossible. Gait was ataxic-paretic, more markedly so right than left. He could walk only with two canes, and during walking the musculature of the thigh fell into a spastic tension. The tongue deviated to the left. There were severe rheumatic pains in the thighs.
It appears that some weeks before, this Russian soldier had suffered from severe rheumatic pains in both sides and was at that time absolutely unable to walk or stand. At that time, however, there was no question of a crural paraplegia of organic origin, since the man could move his legs[806] well enough when in dorsal decubitus. There were no signs of paralysis of the rectum or bladder at that time.
Treatment at Jena consisted in regular walking exercises with support at the shoulders. The lower legs and feet remained weak and paretic. The decubital ulcers disappeared.
About the middle of December rectal incontinence began, the stool being discharged without the patient’s noticing it while being led to the bath. Later there was incontinence of feces in bed. Pains in the legs were constantly complained of. Nevertheless improvement in walking was maintained. The toes were dragged at every step and the knee-joints were thrown outward in walking. The musculature of the lower legs was weak. Knee-jerks could not be elicited more than before. He constantly complained of pains in the knees and right hip. The rectal disorder did not again occur during January.
Toward the close of January, the patient’s right lower leg and left foot would occasionally feel asleep; both legs felt cold and itched. In a general way, however, the pains had become less marked than they were at first. It seemed that he had no sensations at stool, and consequently had to resort to the closet at a definite time. Moreover, urine was discharged irregularly and involuntarily when he coughed. It appears that a few days after receiving his wounds in battle, there had been pains on micturition as well as blood in the urine, and it appears that he had been catheterized. It is probable that he had suffered from distention, as he described his abdomen, thighs and sex organs as swollen.
In February he began to be able to move alone with two canes through the ward, but he moved his legs from the knee downward very little, and dragged them after the rest of the body. Upon galvanic examination, the peroneal and tibial nerve trunks were found normally excitable. At this time the sensibility situation had changed somewhat, since complete analgesia was present only in the foot, and hypalgesia had developed upon the anterior surfaces of the lower legs. Pin-pricks were described as touches. The posterior surface of the left lower leg was normally sensitive. There was an oblong stripe about 3 cm. long, beginning in the popliteal[807] space and stretching downward on the left side. The right lower leg was entirely insensitive. The posterior surfaces of both thighs as far as the gluteal folds were completely insensible to pain. The Wassermann reaction of the blood was negative. In this condition the patient was transferred to a prison camp hospital.
Re bloody urine, see Section B, Case 202. Re rectal incontinence, it might be inquired whether this was possibly functional. Roussy and Lhermitte devote a chapter to visceral disorders. They do not list rectal incontinence amongst the disorders noted in this war, nor have any cases of hysterical anorexia or disorders of sensation in the intestinal tract been seen during the war despite the occurrence of these latter disorders in the civilian group. The main digestive disorder that the war cases show is vomiting (see Cases 495 and 500).
Emotionality: Shell explosion; mutism. Recovery by reëducation.
A plumber, 27, went into the infantry. He was very emotional and was but a short time in the trenches when the explosion of shells threw him into a state of mutism. Deafness, rather curiously, did not manifest itself for several days. He had to go back on horseback, and, as he was a poor horseman, slipped off the horse, giving himself a bad fright. When he got up, he had lost his hearing.
He was sent to several hospitals and finally to Val-de-Grâce, in July, 1915. He recovered hearing in fifteen days, but the mutism persisted several months. According to Briand and Philippe, this is a typical case, except for the duration of the mutism. The first treatment was given this patient August 6. His respiration was examined and tracing was taken. August 15, on the morning visit, he was found able to whistle very distinctly the first bars of “Au Clair de la Lune,” and then began to sing the first verses, articulating distinctly, but stammering a little. He was now left to his own resources, without special exercises, from August 15 to September 26, and completely lost the benefit of his previous exercises. A week of special treatment allowed him to recover speech again, enough to take up every day life. The patient went out well.
The general lines of the examination in this case took up attitude in abdominal respiration and the question of respiratory pauses, especially pauses in abdominal respiration, which, in the above case, were exaggerated. Expiration was deficient and disordered. The normal adaptations that had been established during his childhood learning of speech had failed, and the patient would not have been able by himself to regain proper balance of respiration for speech.
The examination was continued to learn the difficulties of innervation of the muscles of phonation whose proper delicacy had been lost. Such a patient is a kind of bad gymnast,[809] executing an exercise known to be hard by contracting all the muscles of the region, both the antagonist and the agonist muscles. Reëducation must, therefore, endeavor to sweep away the contractions that block sound. Then the patient must be made to perform the contractions necessary in phonation and articulation unconsciously. The methods used for teaching children might here be employed, but more elaborate and designed methods can be used with the adult, e.g.,
1. Breathing exercises, especially with the idea of making respiration complete.
2. Blowing exercises.
3. Whistling.
4. Vowel sounding.
Séguin and Rouma, on the other hand, counsel beginning exercises with consonants in stammerers and dyslalics.
Re tests for functional deafness, Ranjard states that on account of the complexity of Shell-shock deafness, exact diagnosis needs to be made. Examination of the hearing by speech alone, or by the watch-tick, yielded poor results; and an accurate mathematical acoumeter (Sirène à voyelles, Marage) is recommended. See especially chapter on the functional examination of audition in Bourgeois and Sourdille’s War Otitis and War Deafness, a work translated and highly recommended by the English otologist, Dundas Grant.
Three days’ skirmish on East front: Unconsciousness, later delirium, still later (six weeks) stammering, hysterical stigmata: Recovery by isolation and reëducation.
A traveling salesman in civil life, 36, as a non-commissioned officer took part in severe fighting in the East shortly after the outbreak of the war. He was under violent shell fire at one time for five hours at a stretch. In the middle of November, after a skirmish in the woods which had lasted for three days, he was found unconscious. According to his own story, he was awakened from this unconsciousness about a week later in a hospital. He described himself as quite unable to say anything about what had gone on during that week.
The medical report on the case stated that he arrived at the hospital, November 18, in a dormant state of mind. He had appeared markedly excited and kept incessantly talking about military matters, such as the placing of machine guns, the occupation of the edge of the woods by his company, addressing the nurse as “Captain,” and the sister as “Mrs. Captain,” making as it were an official report to them. He showed shyness, and always an extreme excitement. His hands and legs were in constant motion; he complained of headaches and itching finger-tips. Sleep could be achieved only by drugs. This mental state lasted till November 26, when he became oriented. Sleep improved, but he complained of pains in the back of the head.
Upon transfer to a convalescent home, December 5, he was still occasionally excited and sometimes sleepless. On December 30, the patient began to stammer; his speech had before this been somewhat difficult, but the stammering began suddenly; speech was indistinct and slow; syllables failed to follow one another at like intervals. The headache at this time radiated from the middle of the top of the head to the side of the neck. There was a complaint of[811] vibrating pains on the two sides of the vertebral column, and a feeling of weakness and unsteadiness in walking. The patient would sway with eyes closed and turn sidewise. The heart action was tumultuous, the pulse irregular and uneven.
The patient was transferred back to the reserve hospital on January 2, 1915, whereupon the stammering became worse, sleep restless, and arms and legs subject to spasmodic pains and twitching. On January 25, he was removed to the Jena Hospital. He remarked that at the convalescent home he became very much excited at the Christmas celebration and had to cry, whereupon his speech became more and more difficult; he could not find the beginnings of words and had to stammer. Upon admission he also complained of sharp pains in the soles of the feet and in the finger-tips.
Neurologically, there was marked dermatographia, the deep reflexes were increased, abdominal reflexes were absent; there were points of pain on pressure in both supra-orbital regions, and there was a general hypalgesia with the exception of the head, the lower legs, the feet, the scrotum, the penis and the anal region. Pin-pricks were recognized on the right side only, when the patient was tested bilaterally. They could be recognized on both sides when the patient was examined on one side at a time. There was a static tremor on both sides (?). He could move his arms, but in dorsal decubitus he could move his legs only jerkily and uncertainly. His gait was waddling with dragging of toes.
There was a marked photophobia. The palatal and swallowing reflexes were in excess; speech was hesitant and stammering. The first letters of words, especially initial consonants, could be pronounced with difficulty, explosively with cheeks blown up, after several attempts. The consonant would be repeated several times before the vowel could be added. The patient’s name was Singer, and he would pronounce it: S … S … S … Si … n … n … ger; the last syllable (ger) being brought out with a strong accentuation. The whole process took five seconds. The word Flanelllatten took 14 seconds. It seems that the patient had already suffered (in 1907) from nasal catarrh and disturbance of hearing from stoppage of the Eustachian tubes. Another[812] attack in 1908 had been accompanied by an irritating cough, and there seems to have been catarrh on the right in 1913, as well as cerumen on the left side.
Treatment: The patient was isolated; in the next few days there was improvement in the headache. The patient complained of muscular twitchings, which would occur suddenly in different parts of the body. On February 1 there was a subjective feeling of happiness since all pains had disappeared.
The patient was given regular exercises in speaking and there was gradual improvement in speech. Body-weight increased, regular walks were taken, and the patient occupied himself with garden work.
By June, 1915, he had still further remarkably improved, working now all day long, partly in the garden, partly in the hospital office. Disturbance of speech was not noticed except for hesitation before the last syllables of long words during comparatively long conversations. All trace of difficulty in walking had disappeared. In this patient no hereditary taint could be proved. He appears to have been of normal development, serving in the army from 1901 to 1903. In his life as a traveling salesman, there was frequently catarrh of the throat, and in 1912 there was a marked swelling of the vocal cords with extreme hoarseness and inability to speak, which condition was cured after local treatment.
Re hysterical speech and voice disorders, Binswanger has found them amongst the most obstinate conditions, often persisting when all other hysterical phenomena have dropped away. He states that apparently the cure of some of these cases must be postponed until the end of the war.
Re general results of the therapeutic treatment of the war hysterias, Binswanger states that he has been able to send some cases back to the front that have successfully stayed there. He has had failures, however, even amongst men who have had no mauvaise volonté and have themselves desired to be sent back to the front.
Gordon Wilson observed 250 cases of Shell-shock at the Ypres salient and on the Somme. Fifty of these cases complained of deafness, and 17 of the 50 were found to have[813] actual nerve deafness. Wilson treated “fixed idea” cases by hypnotism, and sometimes by cold water run into the ear. He, in general, divides the cases in to (a) cases of nerve deafness, (b) fixed idea cases, and (c) malingerers.
Marage states that frequent exposure to the noise of shells for long periods may produce a permanent deafness, as has long been known in naval gun-makers and boiler-makers in peace times. He advocates obturators, a good form being plasticine wrapped in gauze moulded to the shape of the internal meatus. Celluloid plugs, sometimes used, have been known to be set afire by the flash of a shell. Cerumen sometimes protects against deafness, but Mott speaks of the driving of the wax into the tympanum as a dangerous effect in certain shock cases.
BURIAL by shell explosion: DEAFMUTISM. Treatment: phonetic reëducation.
A machine gunner, 26, was buried at Rheims, January 5, 1915, by the explosion of a large shell bursting over the dugout. He was unconscious three days and deafmute on coming to, without amnesia but with a feeling of constriction in the throat.
After fifteen days in the ambulance he was sent for four months to the Maritime Hospital at Brest, and treated by hypnotism. Seven or eight sittings had no other result than to fatigue him. There were then three months of convalescence. Returned to Vannes, September 20, 1915, he was put into the auxiliaries. As he could not work much he was sent, December, 1915, to the Hôtel-Dieu at Nantes. Here electric vibratory massage was given, which secured a few hoarse sounds.
Phonetic reëducation was then undertaken at Prés-à-goutrière, May 10, and his respiratory capacity increased from 170 the first week to 250 and 300 the following weeks. His blowing strength was raised from 15 to 20 to 25 at the same time. In a few weeks he was much improved and June 27 passed on to his auditory reëducation. The respiratory capacity in this man was insufficient. He could not speak, but his respiratory movements were good and he learned again to speak in a voice as good as ever.
According to Liébault, it is a general principle that, if the respiratory capacity is increased, the voice will clear or become better; but, if the respiratory capacity remains stationary, the voice will not improve. It is the same with normal persons. A subject with a very subnormal respiratory capacity cannot speak loudly, but, if his respiratory capacity approaches normal, he can speak normally. According to Liébault, all cases of this sort have had some respiratory anomaly and each case must be systematically examined with the aid of anthropometric tables, including[815] weight, height and chest capacity. The vocal disorder is proportionate to the degree of functioning of the phonating apparatus taken as a whole. It is not merely that the larynx should be examined, but the motor side of the apparatus, the respiratory muscles, the resonating apparatus, the lips, the mouth, the nasal fossæ and the pharynx.
Re curability of different types of war deafmute, Roussy and Boisseau maintain that the type (a) that comes gesticulating, pointing to the ears, and desirous of writing, is the type that responds most rapidly to psychotherapy. There are two other types less responsive: (b) is an apathetic type, with impassive and stupid facies, lies immobile in bed, or sits in a chair in mental confusion; type (c) shows a facies of terror, looks haggard and anxious, confused, disoriented, and possibly delirious.
Re general treatment of deaf cases, Zange suggests that emotion should not be aroused by intense auditory impressions, that he should not be reminded of his shock, and should be kept as cheerful as possible. Zange states that he found the static electric current of service, and got good results in hysterical deafness of sudden development by applying a strong faradic current.
A year’s service; leave: Hysterical aphonia developed at home. Respiratory gymnastics.
A soldier, 35, went on leave August, 1915. Arriving at his farm, he had a violent feeling of moral perturbation and suddenly lost his voice. When he returned from leave he seemed stupid, spoke very few words and seemed to look about in a vague and undecided way. He was several months in this state and sent January, 1916, to Saint-Luc.
The vocal cords were there found of a normal color and without paralysis. “It was, therefore,” remarks Garel, “a nervous aphonia susceptible of instantaneous cure.” The patient was made to make a sound in the lowest tone possible. While he was making this attempt, sharp pressure was exerted upon the lower part of the sternum, to provoke expiratory reinforcement. The sound emitted was loud, to the great astonishment of the patient, who, thus aided by suggestion, shortly began to talk aloud.
In this particular patient a temporary return of voice was readily obtained, but not maintained. Special exercises had to be instituted, whereupon the patient immediately fell back into a complete aphonia. He was then made to scan words, syllable by syllable, executing with his arms classical movements of respiratory gymnastics, or sometimes with the utterance of every syllable the epigastrium was manually compressed or the shoulders suddenly lowered. The patient could now read a book in a jerky manner, and after a few lines he could read without his shoulders being pressed.
Another plan was to have the man read or talk while walking. As soon as he was stopped and accosted, however, he lost his voice again. Up to the time of report it was impossible to secure a definite return of voice, as the patient was not willing to associate words with peculiar movements. It might make him ridiculous. Accordingly, the nurses were requested not to fulfil requests unless they were made aloud. Recovery was to be hoped for from this measure.
Wounded: Recurrent stammering: Reëducation.
A young English officer, previously cured of stammering while a boy, fell to stammering again after being twice wounded. The impediment was of the laryngeal type. When spoken to he was often quite speechless. In Shell-shock stammering, the chief difficulty according to MacMahon is in the production of voice consonants and vowel sounds. In mild cases the trouble is best left alone.
This officer was anxious to pass into the regular army from the reserve to which he was attached. The stammering prevented this. He was treated nine months and improved rapidly. He passed through the trying ordeal of the medical board successfully and went to his regiment.
In severe cases the patient is taught how to fill his lungs properly. He is taught to acquire an inferior lateral costal expansion in inspiration. During expiration the abdominal muscles are trained to contract slowly and strongly, pressing the diaphragm upwards and drawing the lower ribs downwards and inwards. This steady breathing produces a sensation of repose in the stammerer. He is not to raise the upper chest and not to tense the throat, tongue or jaws.
The main vowel sounds are now taught. The main vowel sounds are oo, oh, au, ah, a and ee. They combine in six ways, oh and oo in the word wound, ah and ee make the long i, au and ee in boy, oh and oo in road, a and ee in rain and fair, ee and oo in new and you. There are also words in which no main vowel or compound sounds appear, which may be placed either on the open ah position or the closed ee position. Such words as long, abbot, among, which are on the position of ah and such words as it, sister, minister which are in the position of ee. The voice consonants are b, d, g, j, l, m, n, r, v, w, y, z, w being oo sound and y the ee sound. The breathed consonants are c, f, h, k, p, q, s, t.
The treatment of stammering intensified by Shell-shock is more difficult than that of Shell-shock stammering de novo.
Wound of face: Speech disorder. Recovery by reëducation in two months.
An officer was wounded under his left eye, October 7, 1916. His speech was affected only five days later in a casualty clearing station. Observed by MacMahon, November 5, he was found to speak with great difficulty and became exhausted after a few words. He was tensing all the muscles in attempting to speak. Breathing advice was given and counsel how to relax in the abnormal efforts.
November 12, the officer, who was at Number One London General Hospital, began to speak with more freedom. “I am getting a bit better. I feel I must keep quiet, and it comes after a bit. I think far quicker than I speak.” He said that the breathing exercises had helped him most.
November 15, he still spoke in a rather staccato way; but the words did not check as they had. In a week further there had been so much improvement that he was discharged with a prognosis of complete recovery.
January, 1917, he had recovered.
Shell wound and burial: Camptocormia (psychoelectric treatment successful in one séance) and lameness (long reëducative treatment successful).
At a Neuropsychiatric Center, September 2, 1916, arrived a chasseur, 29, showing lameness of a pseudocoxalgic type on the left side, combined with an anterior camptocormia. The whole situation had lasted a year. The chasseur had been wounded by shell explosion on the left side and was buried on July 29, 1915. He lost consciousness and had respiratory trouble and mutism. His arched walk and lameness began August 20, 1915.
He had a number of terms in hospital and six months at the dépôt. He was sent back to the front, June 20, 1916, being proposed for auxiliary work. There was some mental weakness. After one séance of electric treatment, the improper attitude of the trunk was corrected. The lameness, however, persisted and required long daily reëducation.
The patient was discharged cured, October 20, 1916, without lameness or camptocormia. There were a few persistent lumbar pains.
Re treatment of war psychoneuroses, Roussy and Lhermitte recommend rational and persuasive psychotherapy after the manner of Dejerine, Dubois, Babinski, and others. Hypnosis, they say, should definitely be rejected. Mental contagion must be staved off, and Roussy and Lhermitte believe that almost all cases are curable and should be sent back as competents.
They maintain that the medical officer himself plays the leading part. Many patients are “cured” when they find “good masters”; this mastery of the combined confessor and educator is greatly aided by prestige. He must speak with authority, with “iron in the velvet glove”; but with patience and persistence. If a long sitting fails, postpone work on the pretext of resting the patient. The patient must not be early threatened with discipline. Even exaggerators[820] and malingerers must be talked to as if neuropathic.
A careful medical examination, besides correcting false diagnoses and demonstrating hystero-organic associations, will give the patient confidence in his physician.
A new patient is more easily cured than an old one. In general, patients should be treated as soon as possible after the shock. Contractures are habitually more persistent than paralysis; tremors and tic are more pertinacious than deafmutism; ante-bellum psychoneuroses are less easy to treat than cases developed by the war alone.
The neurological centers near the front, with their discipline, inaccessibility to friends, and nearness to the front, present a situation which yields easier and quicker cures than the interior; but after the two-years’ experience which proved this fact, according to Roussy and Lhermitte, many cases still get sent back into the interior for many months,—cases that ought to be cured near the front. Cases having convulsive attacks get confinement in separate rooms; chronic neuropaths are kept in bed on a milk diet.
The general features of the treatment of psychoneuroses commended by Roussy and Lhermitte are summed up in what they call the psychoelectric and reëducative method, divided into four stages: A stage (a) of persuasive conversation; (b) isolation; (c) faradization; and (d) physical and psychical reëducation. Roussy and Lhermitte got during six months in one of the army neurological centers, 98 to 99 per cent of recoveries. Clovis Vincent, in a special interior hospital (see for Clovis Vincent’s treatment, a summary under Case 575). Re the first stage of persuasive conversations, Roussy and Lhermitte discuss on the day of admission the general nature of the patient’s condition, and place him in the atmosphere of cure, in contact with recovered patients. The conversation takes place in the physician’s consulting room. The patient is gotten to promise on oath that he will submit to any methods of treatment. Although one may pass from the first stage to the third or electrical stage, forthwith, Roussy and Lhermitte recommend several days of isolation. The patient is placed in a separate room, and[821] kept in bed on a milk diet. This isolation treatment of Weir Mitchell allows reinforcement of the suggestion by talks on the medical rounds, allows the patient, perhaps, to beg for the electrical treatment, which he may have refused at first, and lengthens the period of observation. According to Roussy and Lhermitte, spontaneous recovery not infrequently takes place during this phase of isolation. Lameness of long standing, tremors, and deafmutism disappear.
The third stage is that of faradization, executed by the physician with only such attendants as may be necessary to support the patient. At first, the man lies nude upon the bed, but later may be treated while sitting, standing, walking, or running. Feeble currents are used at first; later stronger ones. The poles are applied to the affected parts, and sometimes to especially sensitive parts of the skin, such as the ears, neck, lips, soles, perineum, and scrotum. Energetic treatment by the rapid method is indicated in the vast majority of cases, especially at the front. If a case is seen early, the rapid energetic treatment almost always cures at once. The success of the method depends upon the production of a crisis, which ought to be produced at the first sitting. Sometimes this sitting has to be continued for hours. Some patients require two or three sittings; some, still more. Instead of faradism, a cold jet of water, or even painful subcutaneous injections of ether, may be used.
The fourth stage is that of physical and psychical reëducation, important in long-standing cases. The various forms of physiotherapy are carried out by special assistants or head nurses, accompanied by psychotherapy, and if necessary by electricity. According to Roussy and Lhermitte, these reëducative methods used alone, without previous faradic treatment, are not successful. Relapse follows premature transference from the front to hospitals in the interior, and too early sick leave.
Shell-shock deafmutism. Speech recovered by suggestion and reëducation; hearing by reëducation.
A corporal, 20, was exposed to the shock of an aerial torpedo, January 18, 1916, at Souchez. The torpedo fell a meter away. There was no loss of consciousness, but the patient was agitated for several hours, not knowing what he was doing. Evacuated to hospital, he remained several days in a stupid state. He was completely deaf and remembered poorly what had happened. He made every effort to speak, but could not. His head felt on fire. He could not open his mouth well and his lower jaw was almost in a state of contracture. He felt that his tongue could not move easily. In this status he remained until February, always trying to talk, but not succeeding.
He then arrived at Hôtel-Dieu. The mouth was now opening better and he was in a better general status, though always feeling fatigued. Vibratory massage was given to the laryngeal region. He was gradually got to emit a few sounds in a low voice. He was sent, April 26, to Prés-à-goutrière. He was now somewhat vocal, but at times would become completely aphonic once more. The voice during the first few weeks of treatment became better, and the respiratory capacity was increased from 450 the first week to 460 and 500 in the next two weeks.
May 12, he suddenly lost his voice again and wanted to commit suicide. However, in three more days he was able to speak normally again and has had no relapse. He was then put under auditory reëducation and at the time of report his hearing had slightly improved.
Liébault remarks that during the time when the patient could not speak his jaw muscles were contracted and his tongue could not mobilize well. He could think words but could not articulate them. It was accordingly important to cultivate the normal functioning of these muscles.
Gassing; tracheitis; crash from airplane; unconsciousness: mutism; stammering. Reëducation; hypnosis.
A lieutenant in the Royal Flying Corps, 23, described as “unusually normal,” a successful business man, athletic, socially popular, had been for a year in the Infantry. He was caught suddenly in a gas attack, and, though he recovered after a few days in bed, had a severe tracheitis and laryngitis. The lieutenant had been very proud of his voice and its carrying power. He went to a laryngologist in London, who said that he would never be able to sing again—a matter of some worry.
He soon became an expert airman. In the spring of 1917 he was shot at by antiaircraft guns in a trip over the enemy’s lines. One of the wings was hit and so weakened that in landing the lieutenant crashed to the ground. He was unconscious for three hours and on coming to tried to shout to his servant in the distance, who, on arrival, found the lieutenant quite unable to speak.
According to MacCurdy, there was here a conversion hysteria with regression to the tracheitis that followed the gassing. The mutism MacCurdy regards as a pathological degree of an effort of protection for his voice. In hospital three weeks later he learned to whisper a few words, though with great mental effort. He regained the voiced sounds by coughing and then saying “ah.” Stammering now developed. Not more than one or two words could be said at a breath. Training to say two, three, four and then five letters in one expiration yielded improvement in the stammering. Under mild hypnosis, to the degree merely of distraction, normal speech was re-attained. There was no relapse. Singing was then practiced and in a period of six weeks the singing voice was virtually as good as it ever had been.
Shell-shock: Loss of consciousness, possibly hemorrhage from head: Spontaneous gradual recovery from anesthesias in three months: Recovery from paralysis by reëducation in a few more weeks.
A German youth of 19 volunteered at the outset of the war as a motor cycle rider. About the end of October, he was hurled from his wheel by a shell which struck close beside him and exploded, knocking his back against a pile of beams. He lost consciousness. There may have been hemorrhage.
He came to, two hours later, in the dressing station, hardly able to move his limbs. Such movements as he could make were painful. There was an evident contusion of the back. He had a fainting fit after his bath in the field hospital and then could get to bed only with support. Severe pains in the legs, especially in the knee.
In the reserve hospital, there was a second similar fainting spell, followed by buzzing in the head, feelings of pressure in the chest and an irregular pulse; all of which phenomena disappeared the morning after the fit.
A careful examination about the middle of November showed the persistence of a severe paresis of the left arm, and a less marked motor weakness of the right arm. Both legs were paretic, and there were no spontaneous movements of the leg. This paresis of the legs was combined with complete anesthesia and analgesia. Sensory impairment was found only in the right arm and trunk, and there was no evidence of sensory impairment in the left arm. Both motor and sensory disturbances of the arm disappeared rapidly.
However, at the beginning of December, 1914, the complete insensibility of the lower extremities up to the groin still persisted. The anesthesia then began to retreat, so that four days later, the upper limit of anesthesia was somewhat below the groin. There could be found a circumscribed area of anesthetic skin over the os sacrum up as far as the second[825] vertebra of the os sacrum; but the skin around this area, as well as over each tuber ischii, gave normal sensation.
The anesthesia continued to retreat: to the middle of the thigh at the middle of December; to a level 3 cm. above the knee-cap at the end of December; to the upper end of the knee-cap on the right side and the middle of the left knee-cap, January 1. January 11, the anesthesia had retreated to a level 10 cm. below both right and left patella. February 8, sensibility in the legs had entirely returned.
While the anesthesia was pursuing this favorable course, the motor symptoms failed to improve to any marked extent, although active motion of the legs with the patient in dorsal decubitus had gradually returned to a limited degree.
The diagnosis upon arrival at the Jena Nerve Hospital was “rheumatism of the left side of the body and dislocation of the spine.”
The treatment consisted at first of rest in bed and moist dressings of the legs, but the treatment had to depend greatly upon the diagnosis. The patient complained of difficult micturition; yet there were no other positive signs of organic disease, of spine or cord.
Hysteria was the diagnosis preferred to rheumatism, despite the fact that examination at the Jena Hospital failed to show any disorder in pain or tactile sense.
The patient was a rather tall man of slender build, with a slightly accentuated second pulmonic sound, decidedly increased tendon reflexes, weak plantar reflexes, and many points painful on pressure in various parts of the head, over the spine, and in the sciatic regions. The vertebral sensibility to pressure was most acute in the region of the third, fourth, and fifth thoracic vertebrae. There was a marked dermatographia. There was no other sensory disorder and no motor disorder of the arms, though the left hand-grasp was weak. All passive movements could be successfully carried out with the legs. Upon bending at the hip, there were subjective feelings of tension in the posterior parts of the thighs. In active motion there was a marked limitation in leg movements, which appeared to be executed with great difficulty with but small excursion and with considerable[826] trembling. The knee-joint could be flexed only when the sole of the foot had support. The lower leg could not be extended. The excursion in the joints of the feet and toes was slight. Muscular strength was in general decreased. There were no feelings of pain in muscular action but merely feelings of great effort. Gait was slow, shuffling, unsteady, hesitating and only possible with support. Fatigue set in after a few steps. In walking, the legs could hardly be bent at the knee. The soles of the feet dragged on the ground. The patient was unable to stand upright, and when placed upon his feet, anxiously and stiffly clung to some support. Without support, he fell over backwards. When supported he could move his legs at the hip and lift the feet from their base by bending the knee-joints. The patient could not sit in a chair or in bed except with support; otherwise he would fall to the right side. In dorsal decubitus he complained of pain in the loins.
With this hysterical picture, treatment of a psychotherapeutic nature was carried out. The patient was given methodical exercises in walking and standing, during which affirmative suggestions about his new capacity to walk and stand were given with monotonous repetition.
For the first fortnight he walked with the support of two nurses for a half hour every day. He was very industrious and willing to execute this treatment; and later began to exercise with a cane. Two days later, he omitted the cane and found himself able to walk about without support. He was shortly able to stand without swaying, although for some time the walk was upon a rather wide base and somewhat slow and suggestive of spastic paresis.
The general condition of this patient remained good. His appetite and sleep were good. After the middle of March, 1915, there were no more peculiarities in walking, and the patient was able to take somewhat long walks in the city and vicinity. He applied for work in the airship division, for which he already possessed some experience.
The youth appears to have been of a normal mental and bodily development, though his mother is said to have been nervous and a sister died of convulsions in childhood.
Shell-shock with loss of consciousness: Deafmutism, rhythmic head movements, anesthesia, asymmetrical areflexia. Recovery by suggestion with faradism, massage and reëducation.
A Russian private, 30, literate, lost consciousness upon the explosion of a large shell, November 10, 1915. He was brought to hospital, November 14, completely deaf and dumb, and with his head rhythmically swaying sidewise 60 to 70 times per minute. The swaying ceased during sleep. The head was carried inclined to the right; there was complaint of headache. The left leg, the trunk and the hairy part of the head were anesthetic. The knee-jerks were obtained with difficulty, the Achilles jerks were lively; the throat and conjunctival reflexes were absent; the abdominal and cremasteric reflexes were lively. The right plantar reflex was absent; the left normal. The vision of the right eye was impaired, and there was a monocular diplopia of this eye. The drum membranes were pulled in, and the disorder of hearing was explained on the basis of labyrinthine shock.
After a séance of written suggestion with faradism to neck and small palate and vibratory massage to throat, speech returned. November 26, the patient read in a loud voice a written phrase. He did not speak again independently until early in December, when he read aloud written matter. The return of spontaneous speech was gradual. Hearing returned December 5, when he was able to hear in the right ear by means of a tube. In the sitting posture there was less swaying of the head. If the patient lay down, rhythmic movements of the head became stronger and more rapid (120).
Shell explosion; unconsciousness: Amnesia; paralyses. Reëducation.
A corporal in the Belgian army was mobilized when the war broke out, and was in action continuously in the retreat from Liège, in the siege of Antwerp, and finally on the Yser until October 27, 1914, when the explosion of large shells rendered him unconscious. He recovered consciousness only in hospital at Calais. Though he was able to see and hear well, he was dazed and remembered nothing of what had happened. In fact, he did not understand what was said to him.
In a week’s time, his memory and intelligence returned, save for periodic attacks in which he was dazed. From the very beginning he had been quite unable to move his legs, and at first the arms were weak. He had a series of attacks of violent struggling in November and December, 1914, which the corporal himself called fainting attacks, claiming that he did not move his legs in the attacks but only his arms. In fact, he claimed that he could move neither head, body, nor legs, but only the arms. He said, “Sometimes I try hard and set my teeth, but I do not know how to move my head and my legs; I try but they do not move.” Sphincter control was maintained. Although he could see, when he attempted to read, everything went black.
He was finally admitted to the National Hospital for the Paralyzed and Epileptic on July 8, 1915, on the service of Major Walshe. He was thin and wasted. He was firmly convinced, according to the notes of Major Walshe, that he was seriously paralyzed. He said he could not lift his head; when his body was lifted, his head fell back, or rather perhaps was definitely thrown back, lolling about alarmingly. However as he lay in bed he frequently lifted his head unconsciously and placed his hands under it. When asked to lift his head, the sternomastoids were strongly contracted, but at the same time the neck extensors also, so that the head was[829] stiffly and strongly held in an extended position. Despite the patient’s statement that he could not move the trunk muscles, he could turn over readily in bed, and when trying to move the head the trunk was fixed in a strong opisthotonos, and the abdominal walls were rigid. When requested to move his legs, he made no movement whatever, though during head movements the legs were strongly fixed in extension. On passive movements, there was no active muscular resistance. There was an indefinite blunting of all kinds of sensations. Reflexes were normal.
Major Walshe worked hard with the patient, inducing him first to lift his head from the pillow, and finally to move the legs. In three weeks’ time, the corporal could just sit up, and at the end of another month, he was able to stand in the walking machine. At the end of a third month, he was walking upon crutches, and at the end of another, he could walk upon two sticks with his feet wide apart, moving as if glued to the floor. To quote Batten,[830] “The corporal will eventually get well but not, I think, before the end of the war.”
[8] Material is here drawn passim from the compiler’s Shattuck Lecture on Shell-shock and After, read before the Massachusetts Medical Society, Boston, June 18, 1918.
1. Shell-shock, a lay term, usually refers to the medical entity or disease-group: functional neurosis, or more briefly, neurosis.
The history of the term Shell-shock will repeat that of Railway Spine in the last century; the term will fall into disuse when the cases subsumed thereunder get their exact medical diagnoses—which, statistically speaking, will prove to be as a rule psychoneuroses, either hysteria (pithiatism), neurasthenia (nervous exhaustion, “prostration”), or psychasthenia (obsessive neurosis).
2. But the laity cannot be got to use the term Shell-shock in this exact sense, because the laity cannot make exact diagnoses.
In the post-bellum and reconstruction period the physician will need to guard against regarding all cases called Shell-shock as really neuroses, merely on the ground that Shell-shock is probably neurosis. Laymen will in the reconstruction period succumb to the lure of the 100 per cent and gossip about cures and failures in the same loose manner that is but too familiar in discussions of Lourdes, Christian Science, the Emmanuel Movement. It will be worth while to preserve a certain generality and comprehensiveness for the term Shell-shock, which will stand to medicine as the term weeds stands to botany.
3. In short, keep the connotation but try not for any denotation of this lay term Shell-shock in the lay mind!
The dangerous history of the term dementia praecox may be recalled. Neither dementia nor praecox is an exact term[832] except for the statistical majority of cases of schizophrenia. Yet does not the layman hearing the term dementia feel entitled to assume that a victim must be demented or become so?
4. The term Shell-shock appears to be a perfect term for the ordinary man, as it means much and little, connotes enormously and denotes a minimum and casts the lay hearer back upon the expert.
But confronted by the term Shell-shock, the ardent social worker or the ordinary man fails to get any incorrect notion about the nature, and especially about the prognosis, of the condition. If there is any suggestion of prognosis, it is the correct suggestion of curability possibly conveyed by the suddenness implied in the term shock; but I defy the ordinary man to get from the ordinary term Shell-shock very much that denotes anything in particular. All he gets is an enormous connotation. This connotation may run back for the race into tree stumps, savages brandishing spears, palatial decorations, the protrusion of animal spirits, the Leyden jar (sometimes familiarly known as the “shock bottle”), and the aspen shaking of the man in fear or its interior equivalent. But whether the slang runs back so far or no, and whether the shell is a shell of powder or a shell of fear, and whether the shock is of solid particles or in a moral sense, the problem is implicitly laid down in the slang (see historical discussion, Shattuck Lecture).
5. The terminological difficulties are clarified somewhat by the French distinction of états commotionnels and états émotionnels in the Shell-shock group.
The French very neatly distinguish what they term états commotionnels from états émotionnels. They think of the états commotionnels or commotional states much as we think of commotio cerebri, that is, of a physico-chemical happening in the brain of an essentially curable (or reversible) nature; that is, of something that falls short of being, as they say, lésionnel, namely, as bringing about a structural lesion. That is, they distinguish a brain with a visible focal lesion from one which has sustained a physical jar or commotion, and they distinguish the effects of both of these from the états émotionnels[833] or emotional effects of an injury. The nomenclature here brings out one of the most fundamental difficulties in the whole field of so-called Shell-shock, namely, the distinction between structural conditions, microscopic or macroscopic, on the one hand, and functional conditions of a psychopathic nature, on the other. The commotion would affect the neurones themselves in some perhaps invisible but still genuine physico-chemical way, whereas the emotion would affect these neurones merely after the manner of the normal emotional life, except that the neurones would perhaps deliver an excessive stream of impulses.
6. Terminology, especially in the matter of explanations to laymen (Americans demand monosyllabic explanations as a preliminary to taking suggestions!), is not always assisted to clearness by physicians on account of the old ontological fallacy that Charcot insisted on.
Would that the medical profession understood neuroses at their true value! Only too frequent is the impression on the part of the profession that imaginary symptoms are by the same token non-existent! I have even heard a physician well-trained in somatic lines say that Shell-shock did not exist because Shell-shock was nothing but neurosis, and neuroses were characterized by imaginary symptoms,—accordingly neuroses, being imaginary, do not exist! All of which reminds us that many of the profession were entirely skeptical when Charcot made his original observations. Some men here in America felt that, whereas hysteria might occur in Paris, it did not occur to any extent in America. The Shell-shock data of this war will abundantly prove to the profession the existence of the neuroses, and I feel that physicians will have to brush up their ontology to the extent of conceding that a symptom may be in a sense imaginary and yet not in any sense non-existent.
7. Babinski points out a case of hysterical paralysis of a leg which led the patient to lean so heavily upon his arm as to produce an organic crutch paralysis. It would be to no point to argue that the hysterical paralysis was here non-existent. Of course we shall have to meet the false analogies drawn from methods of cure. If a paralysis can be cured in a[834] few minutes by the electric brush, or by hypnosis, or on emergence from chloroform, or by some other modern miracle.
8. Is it too much to ask the profession not ever to say that this rapid and seemingly miraculous cure was brought about because the disease was non-existent?
9. The delimitation problem, taken up in Section A, is not identical with the differentiation problem, taken up especially in Section C but passim in Sections B and D; by delimitation we may refer to the process of localizing the diagnostic battle through exclusion of the other great groups of mental diseases that à priori ought not to come in question, but do come in question sometimes, before we slice down to the question.
10. Is there or is there not evidence of destructive lesion in the nervous system of this so-called Shell-shocker? Is this man a victim of organic or of functional neurosis? This latter is what may be termed the differentiation problem.
Confining ourselves now to the delimitation problem, what are the major groups of mental diseases that might come in question?
I shall enumerate these. We think of mental diseases as I, syphilitic; II, hypophrenic (that is, feeble-minded in some of its phases, including even slight degrees of subnormality not entitled to be called feeble-minded in the ordinary sense); III, epileptic; IV, alcoholic (or due perhaps to some drug or poison); V, encephalopathic (in the sense of some focal brain disease); VI, symptomatic (in the sense of some somatic disease); VII, senile (or presenile). The seven groups so far enumerated, I believe, the general profession is pretty well equipped to consider, at least roughly to diagnosticate and to handle with due respect to the interests of the patient and of the community. I am bound to say that some of my colleagues would not go so far as to the competence of physicians in general in these fields, and one is aware that a plenty of mistakes have occurred even in these groups through the bad judgment of practitioners. Nevertheless, I hold to the conception that our profession is reasonably well equipped to[835] handle these greater groups, having in mind all the while the appropriate temporary calling-in of the specialist. But there are two more groups, in addition to these seven, in which I am not so sure that the general profession knows as much as it should. I refer to VIII, the schizophrenic group, commonly known as the dementia praecox group; and IX, the cyclothymic group, sometimes termed the manic-depressive group. It is the victims of the diseases that constitute these latter groups that ought unconditionally to be excluded with few exceptions from the army; and it is the study of these conditions which ought to be carried out as a part of every man’s post-graduate training, not merely for his work on draft boards, but for his work in civilian and reconstruction practice. There is another group of, X, psychoneuroses, with which the profession regards itself as familiar, and with which it doubtless is familiar, in what might be called blooming examples of hysteria, neurasthenia, and psychasthenia. But the nub of the situation lies in the fact that the diagnosis of instances which are not such blooming examples is difficult, and hence it was that I qualified my statement as to the competence of the practitioner in this tenth group. It is, of course, the tenth group, of psychoneuroses, into which the majority of the Shell-shock cases fall.
11. Now a study of the literature of the belligerents having Shell-shock in mind as its special topic and aim proves to require a study of war literature in all of these groups. There are cases of so-called Shell-shock which even well-prepared medical men have placed in the neurosis group, when they should have been placed in one or other of the groups mentioned.
12. In short, whereas the Shell-shock delimitation problem deals with groups, I, II, III, IV, VI, VIII, IX and (as our compilation shows) especially with groups I, III and VI, on the other hand the shell-shock differentiation problem deals primarily with groups V and X.
To clear the decks for action re the differentiation problem, let us dismiss the major troubles of the delimitation problem as shown in groups I (syphilitic), III (epileptic), VI (somatic) and thereafter very briefly refer to the residue of the delimitation[836] problem. For convenience of reference, a few out-standing remarks concerning the general relations of these divisions to war and peace conditions are inserted here. We dealt in the diagnostic order of exclusion with 190 cases, distributed as in the table below (bear in mind that the method of this book precludes attaching great statistical weight to the comparative figures, since the various authors published their cases for their special rather than their typical interest).
| I. | Syphilopsychoses | 34 | |
| II. | Hypophrenoses (feeble-mindedness and imbecility) | 18 | |
| III. | Epileptoses | 33 | |
| VI. | Pharmacopsychoses (alcohol; morphine) | 17 | |
| V. | Encephalopsychoses (focal brain lesion cases) | 15 | [9] |
| VI. | Somatopsychoses | 29 | |
| VII. | Geriopsychoses (senile—a null class) | 0 | |
| VIII. | Schizophrenoses | 16 | |
| IX. | Cyclothymoses | 7 | |
| X. | Psychoneuroses | 12 | [9] |
| XI. | Psychopathoses | 15 | |
| 196 |
13. The neuropsychiatric side of syphilis in the war is presented in 34 cases (Cases 1 to 34). The syphilitic basis of sundry military difficulties, quite unsuspected by the laity and probably not too well understood by service men, is suggested by Case 1, a case of desertion by a French officer of high rank. Nor is Case 2, in which visions of submarines proved syphilitic, without its warning. Such cases point only too obvious a moral:
14. Neurosyphilitics have no place in the army or navy.
Eight cases (Cases 3-10) follow in which the aggravation or acceleration or liberation of neurosyphilis has come about under the conditions of war. Some of these cases suggest the gravity of the problems of compensation, allowance and pension that may arise. We might ask,
15. Should not a government which enlists a syphilitic pay full allowances to him when under war conditions he becomes a neurosyphilitic?
For the government was theoretically able to learn at the start (within a small margin of error by means of the serum test) whether the man was syphilitic. If a one-eyed man loses his remaining eye in an industrial accident in civil life, his damages are often fixed at damages for total blindness; for the industrial firm should not have employed a one-eyed man in an industry dangerous to eyes. The principle cannot differ with a man hired in a spirochete-bearing state: The company has hired a man who may under traumatic conditions become an incompetent neurosyphilitic, and should pay damages accordingly when the aggravation begins.
16. What are the responsibilities of government if the neurosyphilis is due to a syphilis acquired during the war?
Often such infection may be due to a tragical form of “negligence.” But, as pointed out in a work on Neurosyphilis, 1917, I believe that any form of licensing system, official or virtual, which would permit the purchase of syphilis in or near military zones, abolishes the argument of “negligence.” A man acquiring syphilis under the connivance of government ought to stand as well as a syphilitic hired by the government, when it shall come to the question of compensation for incapacity. Yet, it may be argued, the man might have remained continent after all. The point is left to the mercy of jurists.
17. The share of neurosyphilis in the “crimes” and disciplinary problems of the army is intimated in three cases (Cases 11 to 13).
18. The latter part of the series (Cases 14 to 31) embraces problems of a more medical nature, touching traumatic paresis and “Shell-shock paresis.” Unusual, these cases may be readily conceded to be; but their infrequency is not such as to put them out of the field of consideration in the “Shell-shock” group.
Very intriguing to the diagnostician would be the cases of pseudotabes and pseudoparesis (Cases 23 and 26 of Pitres and Marchand), were such cases at all frequent.
Case 28, in which shell-shock (the physical event) apparently caused recurrence of a syphilitic (!) hemiplegia, is particularly instructive and might better belong with the[838] series (under Section B: Nature and Causes, Cases 286-301) in which ante-bellum weak spots were picked out by shell-shock and war conditions. But Case 28 is placed here for its syphilitic interest.
Case 29 stands out as a warning example not to crowd the hypothesis and try to make syphilis sponsor for everything, even when it plainly is at work.
Cases 32-34 are cases in which syphilis played a part, though possibly a minor part, in certain peculiar mental reactions.
To sum up the part played by syphilopsychoses and syphiloneuroses in the war, we find, that
19. Syphilis may have occasionally a serious military effect, as in the case of desertion by a French officer of high rank.
20. Important problems of pension, retirement, and compensation are brought out, and as no previous war has had the benefit of the Wassermann reaction and other exact tests bearing upon the nature, progress, and curability of neurosyphilis, we may hope for a far more scientific determination of these questions by review boards during and after the war.
21. We find a few instances in which neurosyphilis has played a part in the discipline of troops. According to one author (Thibierge, 1917), syphilis has become a genuine epidemic among French soldiers and mobilized munition workers. In Germany, also, it may be remembered that Hecht has claimed that no less than an equivalent of sixty army divisions has been temporarily withdrawn from fighting on the Teutonic side for venereal diseases. In this connection, Neisser had recommended the giving of salvarsan and mercury in the trenches. According to Hecht, the appearance of syphilis should be a signal for sending a man to the front. Hecht also made the somewhat bizarre suggestion that special companies of syphilitics should be formed, for convenience of treatment, on the firing line.
22. A more solid foundation is laid for the theory that general paresis may be evoked by trauma—a conclusion already fairly well established by civilian cases, notably those of industrial accident.
23. The question whether shell-shock (the physical event) can produce general paresis is probably to be settled in the affirmative, for it may always prove difficult to show that the physical shell-shock did not actually produce mechanical molar lesions of the brain, permitting the rapid advance of spirochetes. It is perhaps easier to prove that shell explosion may precipitate neurosyphilis in the form of tabes dorsalis (take, for example, Cases 21 and 22). The cases of most importance in the question of traumatic neurosyphilis and traumatic paresis are cases 20, 21, 22, 24 and 25.
24. The picking out of preëxistent weak spots by Shell-shock is given clear illustration, as in the case of Shell-shock recurrence of an old syphilitic hemiplegia (Case 28). Only on such a basis could the syphilitic ocular palsy of Case 19 be satisfactorily explained.
25. The coexistence of functional phenomena with organic syphilitic phenomena is demonstrated by Cases 29 and 30; perhaps also in Case 16.
26. It must be said that presumably there will be, unless our authorities are more successful than in the past, a considerable increase in venereal disease as the result of army life in wartime. There will be a certain number of cases of neurosyphilis a number of years after discharge from the army caused by infection acquired during service. (Germany is said to have got its crop of neurosyphilis after the War of 1870, in the early eighties of the last century.) The names of all soldiers acquiring syphilis and not considered cured at the time of discharge should, under ideal conditions, be given to health organizations in their home states so that they may be accorded proper care and treatment.
27. Shell-shock and epilepsy. The authorities have been somewhat surprised by the number of epileptics that have gotten by the draft boards. The statistics are not yet ripe, but certainly the enlistment of an epileptic is not a rarity. There are some singular instances in the war literature showing how hard it sometimes is to bring out epilepsy. There is the English case, for example, of a man, an epileptic’s son, who had himself been epileptic from 11-18, who entered the Expeditionary Force at the outbreak of hostilities, went[840] through the retreat from Mons and through two years of active warfare without having a single epileptic convulsion. In fact, in September, 1916, he was put in charge of eight men on guard duty. Apparently the new responsibilities worried him, and two months later he had become epileptic to the extent of petit mal.
Another man who had never been epileptic (though his sisters had been) was wounded four times, was never worried by shell fire, got somewhat depressed after the death of his father and five brothers in the service, but did not become epileptic until finally he was blown up and buried three times in one day, and it was a whole month later when he became epileptic, although treatment by rest and bromides apparently resolved the affair.
Other cases seem to show that war experiences can bring out epilepsy, although in most instances it would appear that there was an epileptic or otherwise neuropathic heredity in these cases.
28. There is one author, Ballard, who has actually propounded a theory of Shell-shock as epileptic, pointing out the occurrence of epilepsy long after the early symptoms of Shell-shock have disappeared.[10] There does not appear to[841] have been any increase in epileptics as the result of the war, either from the standpoint of Shell-shock or from the standpoint of brain injury, so far as the records of the National Hospital for the Paralyzed and Epileptic in London are able to show.
[10] In one instance, fugue and other minor symptoms were later replaced by epilepsy; in another, an epileptic confusion developed eight months after an explosion, and in a third, a case of mine explosion, stammering resolved into mutism and mutism finally into epilepsy. Of course there is a so-called general resemblance among all forms of hyperkinesis or irritative discharge of the nervous system. If we term epileptic all the things that various authors have termed epileptoid, we may be doing nothing more than to say that we believe these cases all subject to epileptic hyperkinesis. In that direction, of course, it has long been said that dipsomania was really a form of epilepsy. Whether Shell-shock is ordinarily subject to recurrence in such wise as to imitate the recurrence of attacks of dipsomania, of manic-depressive psychosis or of epilepsy, is, to say the least, doubtful at this time.
29. As in all other instances of mental or nervous disease, when an epileptic returns from the war, whether or not he was potentially or actually an epileptic before the war, his relatives are bound to term him a case of Shell-shock. I am familiar with a case in a hospital in a certain Atlantic port, a case of pronounced and obvious epilepsy. In the wards he is treated as the hero of every occasion. Not only the nurses and attendants, but the other patients and often the physicians can hardly resist thinking of him as somehow a case of Shell-shock. It is a comment upon the status of mental hygiene in general that this self-same epileptic, had there been no war, would have been, as it were, a common or garden epileptic, mute and inglorious on some sunny hillside.
30. In passing I may note how many instances in the medicolegal part of the war literature there are of epileptics who come up for courtmartial or for medical examination pending courtmartial. We may suspect that many a case of epileptic fugue has been regarded as a case of desertion. There is the case of an epileptic who left camp one morning and got drunk. Investigation showed that he left camp before anything epileptoid had happened. He developed in his drunkenness a pretty clearly epileptic crisis with great violence, for which he had a complete loss of memory. The French Council condemned him to five years of labor, not admitting in this instance that responsibility was diminished by reason of the man’s being epileptic. In short, from the military point of view, he should, so to say, have known enough not to have gotten drunk, and so have avoided getting his epileptic crisis. Of course the decision was here very close, and a like decision would not always be rendered. To add to the complication of this particular case, the very first epileptoid crisis which caused it to be known that the man fell into the epileptic group was due to Shell-shock, or at least developed immediately after the bursting of a shell[842] nearby. On the whole, however, the relation between epilepsy and Shell-shock is not a close one.
31. The question of epilepsy in the war is considered in a series of 33 cases (Cases 53-85). The considerations range from banal cases developing quite incidentally, up to cases regarded by one author (Ballard) as illustrating a theory of Shell-shock as epileptic (Cases 82-84). First are considered two cases actually syphilitic. In the first (Case 53), the diagnosis had to be revised from epilepsy to neurosyphilis (the convulsions of this neurosyphilitic were brought out by alcohol, and the reporter, Hewat, remarks that the serum of any patient developing epileptiform seizures between 35 and 50 years of age should be subject to test). In Case 54, the soldier got his syphilis in wartime and the syphilis acted to bring out an epilepsy with which the patient was hereditarily tainted (epilepsy syphilogenic, i.e., reactive to syphilis).
Case 55 might perhaps better have been considered in the group of hypophrenoses, as he was epileptic and imbecile. He was at first condemned by court martial to five years’ imprisonment for leaving his post in the presence of the enemy.
Another mixed case is Case 57, in which another feeble-minded subject showed seizures of a psychogenic nature, which he was able eventually to stop by clenching his teeth.
Seven cases (Cases 58-64) are cases of a disciplinary nature, amongst which attention may be called to Case 62, the “specialist in escapes.” The medicolegal questions of responsibility in the drunken epileptic (Case 58) are particularly perplexing.
32. Case 64 is one of epilepsy following antityphoid inoculation one-half hour. There were five attacks during a fortnight and then no others. The antityphoid inoculation came eight weeks after a shell wound of the thigh, which had not served to bring out the epilepsy in this patient. Bonhoeffer had three other instances of the sort: one in a severely tainted subject, and the others in alcoholics.
33. The next group of cases, 66-77, yields a series of the most interesting medical problems, some of which scarcely[843] belong in an account of psychoses incidental in the war. Case 66 is one with recovery from Jacksonian seizures after decompression of the upper Rolandic region, which was edematous following an (apparently very slight) scalp wound and shell-shock.
34. The cure by studied neglect (in Case 67) is one of hystero-epileptic convulsions occurring in series. Case 68 demonstrates the superposition of hysterica phenomena over a genuine epilepsy, a case therefore with two diagnoses: not hystero-epilepsy, but epilepsy and hysteria.
35. The theoretical implications of Case 69 are striking: The case was one of musculo-cutaneous neuritis (gross enlargement), in association with which Brown-Séquard’s epilepsy developed, waxing and waning with the disease of the nerve. Another case of possible reactive epilepsy is Case 70, and a case of epilepsia tarda brings up the same issue (Case 71). Cases 72-74 are cases with strong psychogenic components, of which Case 74 is particularly instructive on account of the gradual building up of a remarkable visual aura of an approaching fire-wheel, this aura developing after scotoma from looking at the sun. Cases 75 and 76 are cases of somewhat doubtful epilepsy, one of fugue and the other of a solitary epileptic episode following 38 artillery battles in two months.
36. Friedmann discusses narcoleptic seizures, regarded as due to the brain fag of trench life (Case 77). Sham fits and epileptoid attacks controllable by will appear in Cases 78 and 79 respectively. Case 80 is a striking case of a man with epileptic taint, which two years’ service, four wounds, the death of a father and five brothers, and eventually Shell-shock and burial thrice in one day, served at last to bring out.
37. Shell-shock and bodily disease. In civilian psychopathic hospital practice, if a case is not syphilitic, not feeble-minded, not epileptic, not alcoholic, and without signs of intracranial pressure or disorder of reflexes, then we, as specialists, must consider whether the disease in question is not due to some form of bodily disorder outside the nervous system; for example, we think in practice of infectious psychoses, of exhaustive states such as the puerperium, of toxic states[844] such as may be found in cardiorenal cases, and of glandular phenomena such as we are familiar with in the thyroid disorders.
Under the war conditions, it might be thought that these somatic disorders yielding the so-called symptomatic mental diseases would be frequently found.
Aside from these rarities in puzzling diagnosis, we find more commonly in the literature evidence of
38. The soldier’s heart, the so-called “D.A.H.,” or disordered action of the heart, of the English army reports. This soldier’s heart is sometimes associated with hyperthyroidism, and sometimes hyperthyroidism is found alone, with symptoms suggesting those of a sort of diffuse Shell-shock.
One author claims rapid cures of hyperthyroidism by the relatively simple process of hypnosis. Perhaps this is not too unlikely in view of the still obscure relations between mind and hormones. A little more surprising, perhaps, is the assertion met with that psoriasis is sometimes a Shell-shock phenomenon.
The literature clearly shows, however, that, as in most special problems, the internist is still in demand. I recall how one internist was misled on the witness stand into stating that he was a “general specialist.” This is what we would all need to be, were we to solve the problems of Shell-shock in the time allotted to us by the war.
39. Following are special cases to show how near the somatic (“symptomatic”) may be to Shell-shock.
The somatic group of psychoses, sometimes termed symptomatic, is illustrated in 29 cases (Cases 118-146), and comprises cases ranging all the way from rabic phenomena to those of hyperthyroidism. Possibly the first two cases (Cases 118 and 119) might better be placed among the encephalopsychoses. Case 118, one of rabies, was that of a farmer without history of having been bitten by a dog, who eventually came to autopsy and received the Pasteur Institute diagnosis of rabies. A diagnosis of angina was at first made. When the symptoms became more serious and masseter spasm developed, a question of tetanus arose. Later[845] the diagnosis of meningitis was suggested. At this point, the symptoms became predominantly psychotic.
Case 119 was one of seven cases reported by Lumière and Astier, in which delirium and hallucinations appeared as a complication of tetanus. The case in question had been given anti-tetanic serum. (Another case showed identical symptoms without having been given anti-tetanic serum.)
That a local tetanus could be mistaken for hysteria might seem à priori unlikely, but Cases 120 and 121 indicate as much; and Case 121 is interesting on account of the officer’s own description of his local tetanus and its treatment. A psychosis apparently related with dysentery occurred in Case 122. Hysteria followed typhoid fever in Case 123. Another form of typhoid fever complication is perhaps shown in Case 124, wherein the diagnostic question lay between dementia praecox and a post-typhoid encephalitis.
Paratyphoid fever has diagnostic complications, as shown in Cases 125 and 126, wherein the mental symptoms outlasted the fever (Case 125), and psychopathic taint was brought out (Case 126).
Diphtheria was also represented in the matter of nervous and mental symptoms in Cases 127 and 128. In Case 127 the nervous symptoms appeared eight days after evacuation for diphtheria. There were a few sensory symptoms (hypalgesia, hypoacusia, and peculiar bone sensations) in this subject. The phenomenon in Case 128 was apparently one of hysterical paraparesis; nor does it appear in this case that the hysterical paralysis was preceded by polyneuritis.
Malarial effects are present in three cases (Cases 129-131), of which Case 129 showed an amnesia, Case 130 a Korsakow syndrome, and Case 131 anterior horn symptoms. Case 132 exemplifies 15 instances of acroparesthetic disorders in so-called trench foot. This case, like several others, is inserted in this group, not because the symptoms are psychotic, but because they might cause diagnostic difficulty as against hysterical phenomena.
Case 133 is an autopsied case of bronchopneumonia following bullet injury of the spine. Microscopic examination of the spinal cord showed small cavities in the first and fourth[846] dorsal segments. This myelomalacia was doubtless related with the bullet injury of the spine, although the spinal cord was not itself directly touched by the bullet. Case 134 might be regarded perhaps as one of Shell-shock and should be considered in relation with the cases at the head of Section B (Cases 197-209). The case might be regarded as functional, except for a decubitus that developed. Despite this decubitus, there was recovery. The case is placed in the somatic group on account of pulmonary phenomena which it seemed well to relate with those of Case 133. Compare also Case 136, in which reflex phenomena are associated with a bullet wound of the pleura. Case 135 is a many-sided case, with ante-bellum hysteria and certain Shell-shock phenomena. While under observation, the patient caught typhoid fever and then developed neuritis. This neuritis was very probably not post-typhoidal so much as hysterical. Accordingly, the case should be considered in connection with the ante-bellum weak spot series, Section B (Cases 286-301). There was in this case a cure by reëducation.
The reflex hemiplegia with double ulnar syndrome in Case 136 seemed to have followed a bullet wound of the pleura. According to the authors, Phocas and Gutmann, there is considerable literature upon nerve complications of pleura trauma, including syncope, epilepsy, and (more rarely) hemiplegia.
Heart cases are illustrated by Cases 137-139: the first one of hysterical tachypnoea, and the others of the so-called soldiers’ heart.
Diabetes mellitus seems to have followed war strain and shell wound in Case 140.
It is doubtful whether shell-shock and burial had anything to do with the appearance ten days later of lipomata, which proved to be the initial phenomenon in a pronounced Dercum’s disease. (Case 141).
Hyperthyroidism is illustrated in four cases (Cases 142-144). The first (Case 142) appears to have been cured by inducing deep somnambulism (Tombleson claims cures by suggestion in eight cases of hyperthyroidism). Neurasthenia or questionable Graves’ disease (Case 145) followed Shell-shock. That[847] of Case 144 followed 10 months’ service, at times under protracted shell fire. A forme fruste of Graves’ disease is shown in Case 145, in which the phenomena followed gassing and shelling.
A somewhat curious somatic complication in a case of Shell-shock hysteria was the finding of a needle in the left upper arm, which was then extracted. (Case 146).
40. Regarding our rough delimitation of the Shell-shock group as well in hand, having put upon one side three of the most disturbing groups (save one) in our process of demarcation, we must proceed to the Shell-shock material itself: a material now definable as assuredly non-syphilitic, non-epileptic, non-somatic,[11] as beyond question without narrow relations with feeble-mindedness, alcohol and drug states, schizophrenia and cyclothymia, and as probably of the general nature of the psychoneuroses.
[11] In the limited non-encephalic sense of the term somatic (“symptomatic”) of some writers.
Note that in this epicrisis I have designedly not followed the order of presentation of the text materials. The process of diagnosis per exclusionem in ordine which I find most serviceable in civilian psychopathic hospital practice is the elimination of possibilities in the order presented in Chart 1 or in Paragraph 10 of this epicrisis. Because this book will find its greatest use in peace times as a kind of illustrative commentary on the peace material that presents itself in general practice or in psychopathic hospital voluntary, temporary-care, and out-patient practice, I chose to arrange the delimiting material according to the order of the practical key devised for civilian practice. We may now profitably change our order of consideration and consider whether
41. The most practical key or sequence of consideration in the endeavor to delimit Shell-shock neuroses is probably: Exclude (1) syphilis, (2) epilepsy, (3) somatic disease (of a sort able to produce “symptomatic” effects somewhat like those of Shell-shock).
Below I shall still permit myself some general words concerning the other more easily excluded groups because of the light which feeble-mindedness, alcoholism, schizophrenia, cyclothymia, and even old age can theoretically throw on the nature of Shell-shock.
42. Suppose then that syphilis, epilepsy, and somatic (non-nervous) disease are out of the running, we come practically down to the psychoneuroses, knowing that knotty problems are at hand in telling them from structural traumatic effects: But, after all, what are functional neuroses? What do we really know about the neuroses other than to say that they are not distinguished by the existence of the structural lesions which characterize organic disease of the nervous system? Is not the definition of neurosis purely by negatives? However true this definition by negatives may be from the genetic and general pathological viewpoint, the work of Charcot and in particular of Babinski has yielded a number of positive features from the clinical viewpoint, which to some degree make up for the lack of anything positive in the neurones themselves as studied post-mortem. An eminent German has recently declared that the data of this war itself go far to prove some of the long dubious contentions of the Frenchman, Charcot; and the work of Babinski during the war has strengthened and developed the conceptions of his master, Charcot, as well as the ante-bellum conceptions of Babinski himself.
43. Let me insist that the problem is practical enough: Organic versus functional neurosis. The point I want to make is that, when so much theoretical doubt concerning organic and functional neuropathy holds sway, the practical doubts in the individual case under the varying conditions of civilian practice and in the upheavals of military practice, must be still more in evidence. Case after case described in the literature of every belligerent has passed from pillar to post and from post to pillar before diagnostic resolution and therapeutic success. Colleagues meeting, for example, at the Paris Neurological Society, find themselves reporting the same case from different standpoints,—the one announcing a semi-miraculous cure of a case which another had[849] months before claimed only as a diagnostic curiosity. In the midst of such discussions and controversies, there must inevitably be a renaissance in neurology.
44. In cases of alleged Shell-shock, the hypothesis of focal structural damage to the nervous system or its membranes has to be raised.
Shell bursts and other detonations can produce hemorrhage in the nervous system and in various organs without external injury. Thus a man died from having both his lungs burst from the effects of a shell exploding a meter away. Hemorrhage into the urinary bladder has been identically produced. Lumbar puncture yields blood in sundry cases of shell explosion without external wound, and Babinski has a case of hematomyelia produced while the victim was lying down, so that the factor of direct violence through fall can be excluded. In sundry cases, not only blood but also lymphocytes have been found, sometimes in a hypertensive puncture fluid.
45. Moreover, in cases of alleged Shell-shock there may be a combination of structural and functional disease.
A herpes or the graying-out of hair overnight can suggest organic changes. A case may combine lost knee-jerks (suggesting organic disease) with urinary retention (suggesting functional disorder).
46. Again, there is a group of war neuroses, especially clearly brought out in cases of ear injury, in which the functional disorder surrounds the organic as a nucleus. But these “periorganic” neuroses are no proof that the neuroses in question are organic in nature. Hysterical anesthesia, paralysis, or contracture may occur on the side of the body which has received a wound: the process of such a peritraumatic disorder is, nevertheless, a functional process.
47. But, when the problem is statistically taken, the majority of cases of alleged Shell-shock without external wound prove to be functional, as indicated by their clinical pictures. Thus, after a mine explosion, a man was hemiplegic, tremulous and mute. After sundry vicissitudes, the tremors were hypnotized away. Then the mutism vanished, to be supplanted by stuttering. Finally the hemiplegia remained. So far as[850] the mutism and the tremors went, this man might belong in the majority group of Shell-shock cases, namely, the functional group. Assuming the hemiplegia to be really organic, we should regard this man as a mixed case, organic and functional.
48. But do we not know all we need to know or all we are likely to know about the neuroses already from old civilian studies? There are some cases without very close relations to the war: Thus, we conceive of (a) psychoneuroses incidental to the war and such that they might very probably have developed without the entrance of war factors; and on the other hand, we conceive of (b) psychoneuroses (to be dealt with in extenso later) in which war factors (either physical Shell-shock or other factors) forcibly enter. There are in this group of incidental psychoneuroses 12 cases. The first, described as a constitutional intimiste, a psychasthenic en herbe, was one in which a hallucination was developed in the field, and in which three phases of a psychopathic nature—(a) over-emotionality, (b) obsessions, (c) loss of feeling of reality—developed. In this case the war work at first seemed to better the man’s general condition, and he gave two years of effective service. This officer in effect invented his own Shell-shock equivalent in a hallucination of Germans appearing in his trench. The case may be compared with one described in Section B, namely, Case 347: that of a Russian soldier who developed perfectly characteristic war dreams, though his entire service had been rendered in the rear and he had not had experiences in action.
Possibly Case 171, that of hysterical fugue, might be regarded as one of Shell-shock, since two shells burst near him prior to his fugue. The man had had analogous crises, certified by Régis, in adolescence, and had received the diagnosis hysteria. In this instance, we are dealing merely with an habitual somnambulist who has a characteristic fugue following explosion of two shells. The war is in a sense responsible for the fugue, yet not directly, and the fugue would, without the stress and strain of war, probably never have developed (see sundry cases in the group in which ante-bellum phenomena are newly evoked in war: Cases 286-301).
The hysterical psychosis of an Adventist (Case 172) might be regarded as liberated by military service; the terrible fear of the guns shown by the psychoneurotic (Case 173) proceeded to the point of fugue. A Shell-shock victim whose war bride was pregnant, developed fugue with amnesia and mutism (Case 174). Under hypnosis, it appeared that his fugue began with his running away from shells. Case 175 was that of a neurasthenic who volunteered and had to be sent back from the front after three months. In this case, war dreams were supplanted by sex dreams, and the fear of insanity became ingrained. The phenomena here were largely ante-bellum and the war brought them out once more, as might other disturbing experiences.
Case 176 is here introduced to show that neurasthenia may develop in a man without hereditary taint or acquired soil. There was a very slight shrapnel injury of the skull, which somewhat clouds the diagnosis in the case. Five months’ war experience brought out the neurasthenia. Case 177 deals with a point in the diagnosis of psychasthenia, which, according to Crouzon, shows arterial hypotension, a condition important to distinguish from that of pulmonary tuberculosis and of Addison’s disease. Compare this case with Case 169: a case of depression treated by pituitrin. Case 178 is a case of psychasthenia following several months’ service by a man who probably should never have entered military service.
Another case of ante-bellum origin is Case 179. Antityphoid inoculation appears to have been the initial factor in the case of neurasthenia No. 180. Compare Case 65, epilepsy after antityphoid inoculation. Case 181 was that of a non-commissioned reserve German officer whose neurasthenia was distinguished by sympathy with the enemy. He did not want to let his men shoot at the enemy because the idea came forcibly to him that the enemy soldiers had wives and children. This symptom of sympathy with the enemy was also shown by another German (Case 229). Compare the sentiments of a Russian under narcosis (Case 555).
To sum up concerning the small group of psychoneuroses presented in the section on Psychoses Incidental in the War,[852] we are dealing with cases in which the phenomena are either continuous with ante-bellum phenomena, or are of such a nature that they might well have been brought out by other factors than those of war. These cases by the design of their choice throw little or no light upon the relation of physical shell-shock or its equivalent to the psychoneuroses, though in a few instances the factor of shell explosion is not entirely to be excluded, and in one instance (Case 170) a hallucination may be regarded as a virtual equivalent of an emotional shock of great compelling power.
Examples are available of hysteria (Cases 171, 172, 173, 174), of neurasthenia (Cases 175, 176, 179, 180, and 181), and of psychasthenia (Cases 177, 178, and possibly 170).
49. Let us now contrast with these specified ante-bellum or non-war cases the situation which will face us in the war group.
Section B contains 174 cases (Cases 197-370). Autopsied cases (Cases 197-201) are put first and are followed by cases in which lumbar puncture data are available (Cases 202-207). A third group of cases is that in which so-called organic symptoms are much in evidence, either independently or in association with functional symptoms (Cases 208-219). There follows a small group of three cases with shrapnel wound (Cases 220-222), in which hysterical symptoms were prominent, as against the prevalent and correct conception that wounded cases are not so prone to psychoneurosis as non-wounded cases. Three cases specially marked by tremors (Cases 223-225) follow, the last of which gives the victim’s (a French artist) own account of his feelings. The next two cases (Cases 226 and 227) give respectively a German and a British soldier’s account of Shell-shock symptoms.
There then follows a great group of cases (Cases 228-273) arranged according to the part of the body chiefly affected by hysterical symptoms. The arrangement is one of toe to top, or as one might more technically say, cephalad. This cephalad arrangement naturally begins with cases with symptoms affecting one leg or foot (Cases 228-235). Then follow cases of paraplegia (Cases 236-241). As we proceed cephalad then follow four cases of the so-called hysterical[853] bent back, or camptocormia (Souques). Then come walking disorders (Cases 246-248). Still proceeding cephalad, disorders of one arm and hand are considered in a series of six cases (Cases 249-254). Bilateral phenomena, symmetrical or asymmetrical, follow in Cases 255-258. Now reaching the head, we deal with cases of deafness (Cases 259-260), of deafmutism (Cases 261-263), of speech disorder (Cases 264 and 265), with two special cases (Cases 266 and 267). Eye symptoms are dealt with in a series of cases (Cases 268-272), and Case 273 deals with cranial nerve disorder supposed to be due to shell windage without explosion.
The idea of the above arrangement of 46 cases (Cases 228-273) is that the reader dealing with cases of hysterical disorder due to physical shell-shock, or some equivalent thereof, may inspect the data in a few analogous cases described more or less fully in the literature. By reference to the index, the reader will be able to find still further cases to illustrate the symptom in question.
The next series of cases (Cases 274-281) are to illustrate the contentions of Babinski concerning the elective exaggeration of reflexes under chloroform, and the conception of reflex or physiopathic disorders based thereon—a topic to which return is made in Section C on Diagnosis, and elsewhere. A small group of cases (Cases 282-285) illustrate the delay of Shell-shock and kindred symptoms in certain instances, cases that suggest a refractory period of greater length than usual, or the interposition of some unusual factor.
The next group of cases (Cases 286-301) is of special note, bringing out what is discussed below, namely, the emphasis, reminiscence, or repetition of antebellum phenomena, and the picking out of weak spots in the organism by Shell-shock. Possibly Cases 302-303 belong in the same group of illustrations of the driving in of ante-bellum effects. Cases 304 and 305 are definitively cases in which hereditary instability is a factor, whereas Cases 306 and 307 form a foil to these, in that the phenomena develop in subjects confidently stated to be without hereditary or acquired psychopathic tendency.
The next series of cases (Cases 308-320) shows peculiar phenomena; e.g., monocular diplopia, shell-shock psoriasis,[854] synesthesia, puerilism, and the like. Shell-shock equivalents of various sorts are placed in a group of cases (Cases 321-325). The next series of cases (Cases 326 to the end of this Section: 370) show tendencies to general neurasthenic, psychasthenic, and other psychopathic phenomena, rather than the more definite phenomena discussed in the early part of this section in the series arranged “cephalad.”
50. Rehearsing more briefly these findings, what is the nature of these disorders? The literature is practically unanimous on the point: We have to do merely with the classical problem of the neuroses, and when all the data are some day united, we shall doubtless know a great deal more about the neuroses.
51. Locus minoris resistentiae. That the process, whatever else it does, is rather apt to pick out pre-existent weak spots in the patient (the habitual gastropath becoming subject to vomiting; the old stammerer stammering once more or even becoming mute; the man always “hit in the legs” by exertion, now becoming paraplegic) is obvious. The striking instances in which an old cured syphilitic monoplegia, or an old hysterical hemichorea, comes back under the influence of shell explosion in precisely the limits and with precisely the appearance of the former disease, indicate how various a factor may be the locus minoris resistentiae.
52. But, without weak spot, without acquired soil, without heredity, we must now erect the hypothesis that, the classical neuroses may in some, though certainly a minority of cases, afflict normal men. Under the war conditions of investigation touching the family and personal histories of the men, perhaps we should not be too sure of this hypothesis; but the army records will after the war allow us to make or break the point forever and thereby throw the clearest light upon the vexing problems of industrial medicine, wherein progress in general has been so slow on account of the partisanship of the corporation and plaintiff’s attorneys.
53. Purely psychogenic war cases exist: Though Shell-shock denotes, to say the least, shocks and shells—yet we know Shell-shock sans any shock and sans any shell, nay sans either shell or shock.
The fact that a soldier may get war dreams though he has never been in the fighting zone and never by any chance observed the circumstance of war, or the fact that a man can become mute on the second day after a shell explosion because the night before he had dreamed of some hysterically mute patients in his ward—these facts again, although they argue a psychogenic origin for the phenomena of so-called “Shell-shock,” do not at all mean that actual physical explosion in other cases may not be tremendously important.
54. This is shown by the exceedingly interesting phenomena of localization or determination of symptoms to a given region under the special local influence of the explosion. Thus, in the schematic case, an explosion to the left of the soldier produces anesthesia and paralysis on the left or exposed side. Now and again a case will show such anesthetic and paralytic phenomena upon the side exposed to the explosion and some hypertonic, irritative phenomena upon the other side. One gets the figure in one’s mind of an organism fixed, immobile and numb, on the spot by the explosion—and the other half of the body, as it were, attempting to run away from the situation. One side of the body, as it were, plays ’possum, the other tends to flight.
55. Of course these physical phenomena should not blind us to the emotional ones. Now and then the multiple causes of a case may be analyzed, as, for example, one of blindness in which a series of factors emerged, such as excitement, blinding flashes, fear, disgust and fatigue. I cannot here go further into these details, and I need no longer insist upon the fact that surrounding the problem of Shell-shock means surrounding the problem of nervous and mental diseases as a whole, and that thus to be a Shell-shock analyst means to be a neuropsychiatrist.
56. The organic problems of the nervous system are brought up constantly in differential diagnosis, but the functional problems divide themselves up in a perturbing manner into a fraction properly termed the “psychopathic” (that is, after the manner of hysteria), and “non-psychopathic” (that is, after the manner of reflex disorders of Charcot, newly named “physiopathic” by Babinski).
57. For the moment we are not discussing differential diagnosis, but are merely trying to circumscribe the features we wish to call Shell-shock features: We have concluded to call them functional—but what is it to be functional?
Too simple is the reply:
Functional = Non-Organic.
Inaccurate and misleading is the reply
Functional = Psychic.
We may more correctly express the situation, pathologically speaking, in the following categories (see chart, page 870):
ORGANOPATHIC (Lesional, destructive):
(a) gross, or (b) microscopic, or perhaps (c) chemical.
DYNAMOPATHIC (functional, irritative, inhibitory,—but reversible ad originem):
(a) psychopathic; (b) physiopathic (“reflex”).
58. As to the high psychic functions, we had thought of them as split in hysteria, in dissociation of personality. And we had roughly distinguished these conditions as psychopathic from conditions we called neuropathic, regarding the latter neuropathic disorders as on the model of the effects of cutting off or destroying certain necessary neurons. However clear or unclear we were as to the nature of the neuropathic, it does not here matter. Babinski’s point is that there is another kind of dynamic disease that operates, not after the manner of hysteria, but after a manner reminding one of the forgotten “reflex” disorders of Charcot—disorders that fitted the textbooks so poorly that the textbooks dropped them out. In short, what you might call the dynamopathic or functional in nervous disease has been shown to fall into two parts—a psychopathic fraction and a non-psychopathic fraction. Babinski calls this non-psychopathic fraction physiopathic or reflex. And these reflex or physiopathic disorders have a different order of curability from that of hysterical or psychopathic disorders. By what simple device did Babinski prove this? By chloroforming the patient. Under chloroform, when all the other reflexes were stilled, Babinski could bring out, in relief as it were, certain reflexes, or even hypertonuses, that were in the waking[857] life wholly concealed,—yet at the same time consciousness, in the usual sense of that term, had vanished. Accordingly, the proof of a new type of functional disease, at times concealed by the overlay of higher neurones, was now plain. Does not this offer new leads of the greatest value in that most intricate of fields, psychopathology? Is not the model here offered of diseased nervous functions, non-psychic in nature (in the ordinary sense of psychic) but of almost equally complex nature:
Whoever wins the great war from the military point of view, there can be no doubt as to what writers contributed most from the war data concerning the doctrine of hysteria, especially concerning the theoretical delimitation of hysteria from other forms of functional nervous disease: There can be no other answer than that, in theoretical neurology at least, the French have already won the war, if only by means of the remarkable concept set up by Babinski of the so-called physiopathic (that is, non-neuropathic and non-psychopathic).
But how has this splitting of functional neuroses into psychopathic and physiopathic been rendered certain? By the tremendous modern sharpening of differential diagnosis dating from, e.g., the discovery of the Babinski reflex. This brings us to the brink of considerations concerning the differential diagnostic problem.
First it may be well to regard the whole problem in the light of those mental diseases that we slid over when we were delimiting Shell-shock as against syphilis, epilepsy and somatic disease.
59. Why do some authors think of Shell-shock as an “officer’s disease”? It is clear that they cannot be thinking so much of the physiopathic cases as of the psychopathic ones. But psychopathic conditions are obviously more readily brought about in complex and labile apparatus. This point comes out strongly in relation with the comparative stability of the feeble-minded, at least of most feeble-minded, that get into war relations.
The possible relations of Shell-shock to feeble-mindedness are of some interest. We know that Shell-shock picks out[858] certain nervous and mental weaklings and indeed that one author claims as high a percentage as 74 for war neuroses having a hereditary or acquired neuropathic basis. How far does feeble-mindedness itself count among these supposedly susceptible nervous and mental weaklings? Is a feeble-minded person especially in condition for Shell-shock?
There are rumors of experiments to show that if in an aquarium containing some jelly fish alongside bony fishes, you explode a substance, the jelly fish ride through unscathed whereas the bony fishes are killed by the shock. The jelly fish presumably had too simple an organization.
There is something to be said for the idea that in man also the higher and more complex specimens are more susceptible to Shell-shock, that is, to the neuroses of war, than are the lower and more simple combatants. Some statistics indicate that officers, who are in the main of a higher and more complex organization than the private soldiers, are much more susceptible than are private soldiers to the neuroses of war. Doubtless we shall not be able to verify these statistics until long after the war and, so far as I know, no very inclusive statistics have been presented.
On the whole, I judge from the case history literature that the feeble-minded, unless they be of that very high level sometimes called subnormal, are not particularly susceptible to the neuroses. It is obvious that idiots and, for the most part, imbeciles, do not get into military service. As for what the English term the feeble-minded or what we in America are now terming morons, it may well be that our draft boards do not always exclude. High French authorities have specifically determined in certain instances that the high-grade feeble-minded would be perfectly suitable for certain branches of the service. There is the case, for example, of a sandwich man of Paris who somehow got into the French army and was being perpetually sent to look for the squad’s umbrella and the key to the drill ground, but sang and swung his gun with joy as he went to the front, and apparently did very well there. This man had been a state ward and, as you know, well-trained state wards are frequently exceedingly good at elementary forms of drill.
Then there is another case of an obvious imbecile who was quite without any idea of military rank and often got punished for treating his superiors like his comrades and was the butt of his section, but on the firing-line remained cool, careless of danger—a magnificent example to his comrades—at last surrounded and taken prisoner. Here the story might have ended and the folly of enlisting imbeciles in the army might have seemed perfectly plain, except that our imbecile forthwith escaped from the Germans, swam the Meuse and got back to his regiment!
Here then are cases in which the slight degree of hypophrenia—it seems unwise to give it the opprobrious title “feeble-mindedness”—would have been entirely inconsistent with the development of Shell-shock. Such men are, perhaps, too simple to develop neuroses. On the other hand, it would appear that certain of the slight degrees of hypophrenia, such as we might find in so-called subnormal or stupid persons, would prove capable of “catching Shell-shock” as it were, and then find themselves entirely incapable of rationalizing the situation. In short, there may be a group of psychic weaklings, just complex enough to fall into the zone of potential neurotics, but just simple enough to render the processes of rationalization (or what one author terms autognosis) and of psychotherapy in general entirely unavailing.
After the war we may be confronted with a number of persons with their edges dulled by the war experiences. One has met even brave officers who, after months of furlough, still maintain that they will never get back to their normal will and initiative. Whether these hypoboulic persons have not been reduced to subnormality so as to resemble the slighter degrees of hypophrenia or feeble-mindedness can hardly be determined now. They will form important problems in mental reconstruction, for with the best will in the world, the occupation-therapeutist with all her technic, may be unable to force or coax the will of such hypoboulics into proper action. Nor will the ordinary environment of home and neighborhood turn the trick properly. Expert social work in adjustment, both of the returned soldier to his environment and of the environment to the returned soldier,[860] may be necessary. I speak of this problem here not because these persons are hypophrenic or feeble-minded in the ordinary sense, but we must constantly bear in mind our experience in the teaching of hypophrenics (both in the schools for the feeble-minded and in the community) when we are facing problems of mental reconstruction.
60. As for alcoholism, Lépine’s figures bespeak its importance as a hospital-filler and a good deal of prime interest surrounding alcoholism has been developed in the war; but on the whole, so far as I can determine from the war case literature, there is little or no direct relation between alcoholism and Shell-shock, despite the fact that in a number of instances alcohol has complicated the issue and very possibly helped in a general demoralization of the victim. However, the alcoholic amnesias and particularly a few instances of the so-called pathological intoxication have exhibited a certain medicolegal interest, recalling what was just said above about the responsibility of a drunken epileptic. Alcohol remains, I should say, pending exact monographic work upon this topic, purely a contributory factor for the war neuroses.
It must be that the exigencies of the war have prevented full reports of alcoholic cases; or perhaps they are regarded as of such every-day occurrence as not to demand case reports. The alcohol and drug group is represented by 17 cases (Cases 86-102).
The so-called pathological intoxication is illustrated in Cases 86 and 87. Case 86 was entirely amnestic for an attack of hallucinations in which he tried to transfix comrades with a bayonet. Cases 87-97 are cases of disciplinary nature,—the majority from a German writer, Kastan. Case 88 illustrates desertion in alcoholic fugue, and Cases 90-92 are three further cases of desertion in alcoholism.
Cases 94 and 95 give a partial explanation of some German atrocities. At least, here are cases in which the atrocities, with attempted murder and rape, are described more or less fully in transcripts of medicolegal reports. Case 98 throws a curious cross-light upon the war, in that a drunken soldier got an unmerited long leave after paying 100 sous for an injection of petrol in his hand. Cases 99-102 are cases of[861] morphinism, illustrating the effects of the war upon the fate of morphinists.
61. That war makes nobody go mad in the asylum or lay sense of the term has been abundantly proved by the data of this war—and this conclusion is of value in our medical endeavors to establish a proper lay conception of the nature of Shell-shock. Consider first schizophrenia (dementia praecox).
That the causes of dementia præcox, still unknown as they are, lodge more in the interior of the body or in special individual reactions of the victim’s mind, seems to be shown by the phenomena of this war, since there seems to be no great number of dementia præcox cases therein produced. To be sure, some schizophrenic subjects do get into the service, and sometimes their delusions and hallucinations get their content and coloring from the war. Thus a Russian, wounded in the army, developed delusions concerning currents running from his arm to the German lines and felt that he was, so to say, the Jonah of the Russian front, as he could determine shell fire to the spot where he was by the arm currents.
Now and then a case shows a scientifically beautiful admixture of ordinary dementia præcox phenomena with the effects of shell wound or shock. A picturesque case from the standpoint of German psychiatric diagnosis is one of a soldier who boxed the ear of a kindly sister who tried to steer him from a room where the examination of another patient, a woman, was going on. On the whole, the eminent German psychiatrist who examined him felt that the case was really one of psychopathic constitution, as he had shown somewhat similar irascibility on a slight occasion before. However, much to the astonishment of all, the patient developed further symptoms. His ego got terribly swollen. At last he was fain to utter a denunciation of the entire Junkertum and of the Kaiser: he said in fact that he was an Inhabitant of the World and not of Prussia merely. Over here we allow such persons to edit newspapers and write books with impunity, but the eminent German psychiatrist, before mentioned, was constrained to alter his diagnosis of this cosmopolite from psychopathic constitution to dementia praecox!
The group is represented by 16 cases (Cases 147-162).
62. There are four cases (Cases 148-151) of a disciplinary nature. The first (Case 148) was actually arrested as a spy because he was making drawings near a petroleum tank. Of two cases of desertion, one was due to a fugue of catatonic nature (Case 149), and the other (Case 150) was one of desertion with behavior suggesting schizophrenia. However, this man was determined to be responsible for his act, and condemned to 20 years in prison. This latter case might be considered also in connection with Group III (the epilepsies), Group IV (the pharmacopsychoses), and possibly Group XI (the unresolved psychopathias).
Case 151 was likewise alcoholic and disciplinary: the man went so far as to keep a cigar in his mouth while the captain was rebuking him and was, in fact, an old sanatorium case, afflicted with some sort of degenerative disease, presumably dementia praecox.
63. That schizophrenic symptoms may be aggravated by service is shown likewise in the case that follows, namely, Case 152, a man who had been hearing false voices for some two years, had heard his own thoughts, and felt his personality changing. The military board decided that the mental disease had been aggravated by service. Case 153 might offhand be regarded as a malingerer, as he shot himself in the hand. Upon military review, a delusional state set in, and in the course of no very long time a state of schizophrenic apathy. In point of fact, however, this man had already been in several hospitals for previous examination, and had served in the army in relatively normal intervals. Case 154 is that of a dementia praecox who volunteered for three years in French infantry but forthwith gave indications of mental deterioration. This case of a dementia praecox volunteer may be compared with Case 36: that of a superbrave imbecile who swam the Meuse, back from a German prison; with Case 47, that of the feeble-minded person with an insubordinate desire to remain at the front; with Case 163, a maniacal volunteer; and Case 175, a neurasthenic volunteer.
64. Diagnostic questions are brought up by Cases 155-166, in the former of which Bonhoeffer made at first a[863] diagnosis of some form of psychogenic disease, possibly hysterical, but had eventually to alter the diagnosis to hebephrenia or catatonia. Case 156 was possibly one of Shell-shock, though the man remained on duty for a month with but one symptom, trembling of the arm. For nine months he showed a variety of symptoms apparently consistent with the diagnosis hysteria, but then developed catatonic and paranoic symptoms clearly warranting the diagnosis dementia praecox.
65. Schizophrenia may not only be aggravated by service, but as Case 157 shows, war experience may have a definite effect upon the content of hallucinations and delusions. Thus, a man wounded in the left shoulder built up the idea of currents running from his left arm to the Germans, such that if anything were touched by the arm, bombardment of the Russians would at once start up. The arm, in short, was charmed.
66. Psychopathic bravery is not shown in the feeble-minded only: Case 158 is that of an Iron Cross winner who, after an hysterical-looking attack with hallucinatory reminiscences of a Gurkha whom he had bayoneted, turned out to be hebephrenic. Case 159 might at first sight have been placed among the encephalopsychoses on account of the trauma to the occiput, and in fact the mystical hallucinations shown were of a visual nature (a rainbow-colored bird with the face of the Holy Virgin). In point of fact, there was probably no causal relation between the mystical delusions and the brain injury.
67. Case 156, above mentioned, might perhaps be interpreted as one of Shell-shock dementia praecox, but the interval of nine months, though filled with hysterical symptoms, is decidedly long in which to suppose that shell-shock factors could be in process of causing dementia praecox. Cases 160 and 161 are more suspicious. Six German soldiers were killed by a German shell within the zone of German fire, two steps away from the subaltern officer (Case 160), who carried on for some hours, made his report duly, but thereafter developed tremors and lost consciousness. According to Weygandt, the case is one suggestive of dementia praecox, but[864] very possibly should be regarded as one of psychoneurosis. At all events, it would be dangerous to found a doctrine to the effect that dementia praecox can be initiated by shell-shock upon such a case as 160. Case 161 is similarly doubtful. There are a number of symptoms in this man (the sole survivor of an explosion in a blockhouse) consistent with the diagnosis Shell-shock, and a number of others which hardly can be given any other interpretation than that of catatonic dementia praecox. But the available medical data do not begin until five months after the shell explosion. We must conclude here also that no definite evidence exists that dementia praecox can be initiated by the physical factor shell-shock. Case 162 is one in which there are shell-shock factors and fatigue factors in a man who had once ante-bellum shown signs of mental disorder, and who developed delusions subsequent to a fugue following shell-shock. The most one could make of this case would be to say that a latent schizophrenia had been liberated by shell-shock.
68. To sum up concerning the schizophrenias (dementia praecox group), there are cases of great disciplinary interest in which alleged espionage and desertion turn out actually to be schizophrenic phenomena. Again, there are interesting diagnostic problems in the differential diagnosis of hysteria and catatonia. There is evidence that experience in the war may be woven into the hallucinatory and delusional contents of cases of pre-existent psychosis.
69. As to the important question whether shell-shock can initiate dementia praecox, the evidence from these reported cases is against the hypothesis; but if the query be, whether Shell-shock might not aggravate dementia praecox, it may be stated that a military board has decided that dementia praecox may be aggravated by some forms of military service. There is no reason to suppose that shell-shock factors might not operate in this way. Cases 152 and 162 will be of service in the proof of this contention; and Case 162 seems to be definitely one in which a latent schizophrenia, showing itself in one ante-bellum attack, was liberated once more after shell-shock. Of course, the plan of this book and the method of choice of its cases precludes any statistical conclusions[865] of great weight from the relative number of cases found in the different groups; and it might well happen that psychiatrists would not report cases of an everyday and commonplace nature which might yet be very frequent. On the whole, however, it would not appear that dementia praecox is at all a frequent phenomenon in the war.
70. Nor can the cyclothymias (manic-depressive psychoses) be charged up to war factors to any important extent.
On account of the somewhat close resemblance between the phenomenon of manic-depressive psychosis and what we ordinarily feel ourselves—a logical situation reflecting merely the fact that the phenomena of over-activity (mania) and of under-activity (depression) are merely quantitative variations from the normal—it might be supposed that the war life and its shock and strain would start up the cyclothymias in some numbers. Why should not a shell explosion start up a mania or throw a man into a depression? In point of fact the literature somehow does not agree with this presupposition.
Some years ago in Massachusetts a brief investigation was made of the assigned causes of the successive attacks in a great number of cyclothymic (manic-depressive) cases, and it was found that each successive attack progressively had less of the physical in the previous history. Something like 45% of all the first attacks had a pretty obvious cause in the soma, such as a kidney disease, a heart disease, a puerperal condition and the like, but the second attacks failed to show even 20% of such obvious somatic causes, and the third attacks even less than 10%, and so on.
Now war conditions and even the shell explosions themselves have apparently not set up any such conditions as those of mania or of depression. Most of the instances of cyclothymia are instances of men who are cyclothymic before they enter the army. These experiences, when after the war we can sift them all out, may allow us to form better ideas as to the etiology of many of the psychoses, and the great war may thus prove a gigantic experimental reagent which will aid in solving some of the major problems of mental hygiene.
71. The cyclothymic or manic-depressive group is represented in strikingly few cases, seven in number (Cases 163-169).[866] One of the ideas in the literature concerning the manic-depressive group has been that it is very possibly remotely allied to Graves’ disease, a hypothesis upheld by Stransky in Aschaffenburg’s Handbook. Hyperthyroidism itself has been, of course, a rather striking feature in the foreground or background of many sick patients in the war. However, war factors have proved able to bring out very few instances of cyclothymic (manic-depressive) disease. Amongst our seven cases, the first (Case 163) was that of a maniacal Alsatian of 59 years, who volunteered because of his hypomania. Case 165, the case of a German who pelted French trenches with apples from an appletree in No Man’s Land, was another case in which the war had little or nothing to do with the development of the mania. One of fugue (Case 164) was a case of melancholia and anxiety not closely related with war experience. In three further cases trench life and war stress may be thought to have liberated the cyclothymic phenomena. Case 166 was that of a man of 38, previously referred to, who developed arteriosclerosis and whose depression and hallucinations had followed four months of trench life devoid of battles or injury. It is possible that this case should be regarded rather as syphilitic or of some unknown organic origin. At all events, it is not clear that it could be made to bear a heavy weight of hypothesis concerning the genesis of cyclothymic psychoses. Case 167, a naval officer who distinguished himself greatly by work on land in Belgium, was regarded by its reporter as one of manic-depressive psychosis with the fatigue of war as its base. It might be queried whether the man’s distinguished work was not due to an early phase of hypomania, after which the cyclothymic effects began. In Case 168 there was some evidence of the effect of war stress, as certain hallucinations grew more intense after the bombardment of Dunkirk; but in point of fact, this man had shown a predisposition and indeed a period of so-called neurasthenia ante-bellum. It is doubtful, therefore, whether there is any case here abstracted which can be used to support the hypothesis that the manic-depressive (cyclothymic) group of mental diseases has had or is likely to have its genesis in war stress. The remaining[867] case (Case 169) is one illustrating a method of treating low blood pressure in depression.
To sum up concerning the cyclothymias: War stress seems to have had singularly little effect in the production of fresh attacks, and so far as we are aware, no effect in starting up a manic-depressive diathesis, unless Case 167,—that of the naval officer who distinguished himself in land battles,—looks in that direction. It is, of course, to be conceded that hypomania might readily be overlooked under war conditions, and that suicidal melancholias, belonging in this group, might be interpreted as natural war-made depressions. Very possibly, therefore, this result (running to the effect that the cyclothymic forms of mental disease are rare in military life) may need revision.
72. Summary of general considerations concerning the nature of the Shell-shock neuroses (paragraphs 40-71).
Having (a) roughly delimited the Shell-shock neuroses from syphilis, epilepsy, and somatic disease, we inquired
(b) What, after all, are functional neuroses? We remained dissatisfied with a definition by negatives. But we found that
(c) practically the problem seemed to reduce to telling the organic apart from the functional and we found that
(d) in almost all cases we have to raise the hypothesis of the organic. Also that
(e) the absence of external injury is no guarantee against the existence of internal injury. Also that
(f) cases are frequent enough in which organic and functional phenomena are combined. Also that
(g) essentially functional cases may be peritraumatic or metatraumatic (in the sense of Charcot’s hysterotraumatism). But
(h) the statistical majority of cases remains essentially functional.
(i) We then looked over a series of cases developing incidentally in the war and
(j) we compared these with the war cases, the latter arranged cephalad.
Note arrow lengths: Practically we find shell-shock neuroses very different from certain functional (or but mildly organic) disorders and not so different from certain seriously organic disorders.
Note arrow lengths: Theoretically, shell-shock neuroses, being presumably in large part functional, ought to ally themselves more closely with the left-hand group than with the right-hand group. But they do not!
In short, these functional diseases are not so hard to distinguish from various other functional diseases as they are from certain organic diseases. The most serious diagnostic problem is between the war neuroses and organic brain disorders.
| e.g. neurosyphilis paretica ORGANO- PSYCHOPATHIC |
Hysteria e.g. DYNAMO- PSYCHOPATHIC |
| ORGANO- NEUROPATHIC e.g. neurosyphilis tabetica |
DYNAMO- NEUROPATHIC Babinski’s “reflex” or physiopathic disorders e.g. |
A frequent error of neurologists has been to identify “functional” with “psychic” when it came to a question of the classical functional neuroses. The above diagram indicates that “functional” contains more than “psychic.” Doubtless much that goes under the name “unconscious” belongs in the right lower quadrant of this diagram. See discussion in text.
(k) We found many war cases showing emphasis, reminiscence, or repetition of ante-bellum phenomena (weak spots, locus minoris resistentiae, imitation), but
(l) we also found that perfectly sound untainted men could succumb to Shell-shock neurosis.
(m) We found a few purely psychogenic cases without sign or suspicion of physical shock.
(n) We studied the localization (traumatotropic) group.
(o) We arrived, with the aid of Babinski, at the necessity of splitting functional cases into psychopathic and physiopathic.
73. Summary of general considerations: continued.
We found ourselves looking on the Shell-shock neuroses as, like other functional neuroses, in a sense mental diseases. Perhaps we would better say (to get rid of all suspicion of medicolegal “insanity”) that the Shell-shock neuroses seemed to us in some sense psychopathic. But, though the Shell-shock neuroses looked psychopathic and were presumably more functional than organic in nature, it was a curious thing that, practically speaking, the Shell-shock neuroses proved to be farther away from the more functional of the psychoses than from certain organic psychosis.
In particular, we found reliable authors insisting on the practical diagnostic necessity of excluding syphilis, epilepsy, somatic disease—whereas the nature and causes of the Shell-shock neurosis seemed theoretically to withdraw them most remotely from that triad of mainly organic disorders. By the same token, theoretically one might have supposed these Shell-shock neuroses to draw very near to those far less organic disorders (schizophrenia, cyclothymia, feeble-mindedness (i.e., the slighter degrees likely to be found in military service, alcoholism))—yet practically few large diagnostic problems came to light as between the Shell-shock neuroses and the tetrad of dynamic or lightly organic diseases above listed.
74. Diagrammatically this situation is presented in Chart 17.
But why should the Shell-shock neuroses seem so “organic”? Partly, it is probable, because the term[871] “organic” is too often used to mean “subcortical.” In another diagram the truer relations are depicted, with four classes of phenomena (Chart 18).
(a) Organic mental (cortical), e.g., general paresis.
(b) Functional mental (cortical), e.g., hysteria.
(c) Organic neural (subcortical), e.g., tabes dorsalis.
(d) Functional neural (subcortical), e.g., “reflex” disorders.
75. Having disposed of the problem of the rougher Delimitation of the Shell-shock neuroses, we approach the problem of their finer Differentiation. For the sake of the present argument we propose to regard the Shell-shock neuroses as essentially Dynamopathic, i.e., functional whether in the ordinary mind-born (psychogenic) sense of classical hysteria or in the modern nerve-born (neurogenic) sense of Babinski. The problem of this differentiation will accordingly be that between the dynamopathic and the organopathic.
In the orderly diagnosis of mental disease, from the standpoint of the major orders or groups, we ordinarily come at this point to the focal brain diseases. In analyzing the neuro-psychiatric problem of a so-called Shell-shocker, it is, of course, our bounden duty to exclude syphilis. Even though the percentage of syphilitic victims of Shell-shock is not high, yet these cases promise so much from treatment that they deserve to get their diagnosis as early as possible, and the English workers who have worked most in the syphilitic field insist upon this point.
We next proceed, as above indicated, to the elimination of hypophrenia with all the various grades of feeble-mindedness. Thirdly, we try to exclude the various forms of epilepsy; and fourthly, the effects of alcohol, drugs and poisons.
In ordinary civilian practice, such as that at the Psychopathic Hospital, the orderly elimination for diagnostic purposes of the great groups of the syphilitic, hypophrenic (feeble-minded), epileptic and alcoholic, leaves us with cases in which there either is or is not important evidence of organic[872] nervous-system disease, such as that shown in cases with heightened intracranial pressure or in cases with asymmetry of reflexes and other forms of parareflexia. In military practice these logical questions of prior elimination of syphilis, feeble-mindedness, epilepsy, and alcoholism must go a-glimmering at first, unless their signs are so obvious as to permit diagnosis by inspection.
76. But the nervous and mental cases almost one and all give rise to the suspicion at least of organic disease, possibly traumatic in origin. Even when a man falls to the ground without a scratch upon his skin, there is some question whether in his fall he has not sustained some slight intracranial hemorrhage which the lumbar puncture fluid might show. Add to this that the signs of hysteria are very often unilateral, and it will readily be conceived how much like an organic case an hysteric in the casualty clearing station may look. Rapid decision may be necessary in order to get immediate effects in psychotherapy a few minutes or hours after the shell explosion, and one may need to choose between applying a possibly unsuccessful psychotherapy forthwith and making a thorough neurological examination. As Babinski has pointed out, making a thorough neurological examination gives opportunity for all sorts of medical suggestion to be conveyed to the patient. It would appear that many an hysterical anesthesia has been given to a patient by the very suggestion of the physician testing sensation. Here one does not refer to malingering in the conscious and designed sense of the term, but to the operation of some genuinely psychopathic, that is to say, hysterical process.
77. In the case of head injury, naturally the majority of nerve phenomena will ordinarily be upon the opposite side of the body to the side of the head that is injured. The reverse situation holds for hysterical cases, wherein it would appear that the bursting of a shell, let us say upon the left side of the body, seems to determine contractures, paralyses and anesthesias to that same left side of the body; now and then complicated cases appear which put the neurologist through his best paces. Such a case is that of a man who was wounded on the left side of the head and promptly developed[873] a hemiplegia on the same (left) side, with aphasia. Now aphasia ought to be the result of a lesion on the left side of the brain in the common run of cases, whereas left-sided hemiplegia ought to be the result of lesion on the right side of the brain. In point of fact, the analyst of this case felt that he was dealing with a direct injury on the left side of the brain, leading to aphasia, and a lesion by contrecoup on the right side of the brain, leading to a left-sided hemiplegia.
It is not only at the casualty clearing stations and along the lines of communication that the difficulties in telling Shell-shock in the neurotic sense from traumatic psychosis and the effects of focal brain lesions are found, since the literature amply shows that diagnostic problems remain open for weeks or months in the various institutions of the interior, to which all the belligerents have been forced to send their cases.
78. A glance at the differential tables that have been developed, for example, by the French neurologists, will show how fine the diagnosis betwixt a hysterical and an organic disease may be, especially when we consider how often there are admixtures of the two. The rule holds for the vast majority of cases that absolute bullet wounds or shrapnel wounds do not produce Shell-shock; and the statistical story is so clear that one might almost think of the wounds as in some sense protective against shock, that is, against Shell-shock, not against traumatic or surgical shock. Nevertheless, by some process whose nature is obscure, the hysteric is apt to pick up some slight wound and, as it were, surround this wound with hysterical anesthesia, hyperesthesia, paralysis or contractures.
The chances are, if we should collect all our civilian cases of Railway Spine and of industrial accident with traumatic neuroses, we should be able to prove this same strange relation between slight wound in a particular part of the body and the local determination of hysterical symptoms to that region. Of course, the determination follows no known laws of nerve distribution to skin or muscles, and the effect is apparently a psychopathic or, at all events, a dynamic process without clear relations to the accepted landmarks.
I do not mean to suggest, that aside from the hurry of war, the differential diagnoses here are more difficult than those in civilian practice; but the difficulties are at least as great as those that have faced the civilian practitioner. What needs emphasis is that just because we have concluded that the statistical majority of the cases of so-called Shell-shock belongs in the division of the neuroses, we should not feel too cock-sure that a given case of alleged Shell-shock appearing in the war zone or behind it is necessarily a case of neurosis.
After the early “period of election” for psychotherapy in the war zone has passed, there can be no excuse except general war conditions for not according to every case of alleged Shell-shock a complete neuropsychiatric examination, having due regard to the ideas of Babinski concerning medical suggestion of new increments and appendices to the original hysteria, developed in battle or shortly thereafter.
We have, however, been able to find in the literature good instances of puzzling diagnosis in which such conditions are in evidence as acute meningitis of various forms, hydrophobia, tetanus, and the like.
Especially in the diagnosis against Shell-shock hysterias we may need to think of the abnormal forms of tetanus, to which an entire book in the Collection Horizon has been devoted. The differential diagnostic tables here draw up distinctions between local tetanus, involving, let us say, the contracture of one arm, as against a hysterical monoplegia.
79. The focal brain group of psychoses here termed encephalopsychoses, is illustrated by a comparatively short series of cases, 16 in number (Cases 103-117). Many more cases of this group are presented in Section B, On the Nature and Causes of Shell-shock. The motive here is to show sundry effects of focal brain lesions produced in the war and not related with shell-shock. Case 103 was the curious case (see above) of aphasia with hemiplegia—not upon the right side, but upon the left side. There had been a wound in the left parietal region, and the aphasia was presumably consequent upon a direct affection of the left hemisphere. On the other hand, the left-sided hemiplegia may probably be regarded as due to lesions on the right side of the brain produced[875] by contrecoup. The case not only has surgical implications and suggestions of importance, but also it throws some light on the possibilities in concussion of minor degree. As the cases in Section B (On the Nature and Causes of Shell-shock) show, shell-shock, the physical factor, is apt to produce anesthesia and paralysis or contracture on the side exposed to the shell-shock. The means by which these symptoms ipsilateral with the shock are produced is commonly thought to be the “hysterical mechanism,” whatever that may be. Lhermitte, however, suggests that in some cases such phenomena might be due to an actual brain jarring with contrecoup effects. However, it must be granted that Case 103 did not come to autopsy.
80. Case 104 might perhaps better be considered in the section on alcoholism, since a gun-shot wound of the head may be regarded as having produced intolerance of alcohol in the classical manner, similar to that described in Case 97, wherein, however, the trauma was ante-bellum. Peculiar crises associated with cortical blindness, vertigo, and hallucinations, characterized a case of brain trauma by bullet (Case 105). Case 106 is that of a Tunisian, who before the war had had a number of theopathic traits with mystical hallucinations, but after a gun-shot wound of the occiput developed lilliputian hallucinations and micromegalopsia.
81. Cases 107-112 are cases of infection or probable infection. Cases 107 and 108 are instances of meningococcus meningitis, the second of which appears to have followed shell-shock (?). Case 107 led to psychosis with dementia. Case 109 developed a meningitic syndrome, which followed shell explosion a metre away, the syndrome lasting 14 months. The spinal puncture fluid was several times found to contain blood. There was apparently no infection of the fluid as in Case 112. Possibly Case 109 should be set down as an unusual example of shell-shock psychosis, chiefly dependent upon meningeal hemorrhage.
82. A syphilitic (Case 110) in which appropriate tests were made and found positive, showed at autopsy a yellowish abscess or area of softening in the right hemisphere. The curious point about this case was that the only neurological[876] phenomenon in the case was the absence of knee-jerks in the early part of the day; later in the day, they would appear once more. Possibly Case 111, a case of somewhat doubtful nature but presumably of organic hemiplegia, ought to be aligned more with the group of cases illustrating the nature and causes of Shell-shock. The case was not one with the physical factor shell-shock, since the phenomena began ten days after a serene convalescence following an operation for chronic appendicitis. Perhaps the case was one of organic lesion grafted upon a neurosis.
83. Case 112 is the one noted above of infection of the spinal fluid. It is the only case of infected meningeal hemorrhage observed by Guillain and Barré in a wide experience. As a rule, these hemorrhages remain aseptic and have a favorable prognosis. The organism cultivated from the spinal fluid proved to be the pneumococcus. Case 113 yielded a somewhat remarkable phenomenon and perhaps would be more logically considered in relation with the series of cases in Section B that show the picking up of ante-bellum weak spots (Cases 287-301); for this subject had had two serious affections of the brain ante-bellum. He had had a poliomyelitis at five, affecting the left leg, and he had had a right hemiplegia with aphasia following pneumonia, at 20. He was struck (but apparently not wounded) by shrapnel on the right shoulder, and developed athetotic movements of the right hand, as well as a general weakness of the left leg. In this case, according to Batten, the stress had been sufficient to bring into prominence symptoms due to an old cerebral lesion. Whether the mechanism in this case is hysterical is doubtful.
84. That not every case of hemianesthesia is hysterical is suggested by Case 114, in which the diagnosis of hysteria was actually made; but the diagnosis was soon rendered doubtful by the fact that there was no evidence of autosuggestion or heterosuggestion. Other phenomena make a diagnosis of thalamic hemianesthesia more likely.
85. Although Shell-shock is not the subject of this section, yet a case of syndrome strongly suggesting multiple sclerosis is here inserted, following shell-shock (Case 115). The[877] co-existence of hysterical and organic symptoms is illustrated in Case 116, one of mine explosion, and Case 117, one of injury to back. Case 116 somewhat resembled another case of Smyly (Case 219).
86. Differential Diagnosis between Organic and Hysteric Hemiplegia. Babinski, 1900.
| Organic Hemiplegia | Hysterical Hemiplegia |
|---|---|
| 1. Paralysis unilateral. | 1. Paralysis not always unilateral; especially facial paralysis, usually bilateral. |
| 2. Paralysis not symptomatic., e.g., in unilateral facial paresis, the paresis occurs also when bilateral synergic movements are being performed. | 2. Paralysis sometimes symptomatic; facial paralysis almost always symptomatic. With complete unilateral paralysis, the muscles of the paralyzed side may function normally during the performance of bilateral synergic movements. |
| 3. Paralysis affects voluntary, conscious, and unconscious or sub-conscious movements; hence, (a) platysma sign,[12] (b) sign of combined flexion of thigh and trunk, and (c) absence of active balancing arm movements in walking contrasted with exaggeration of passive balancing movements (limb inert on sudden turn of body). | 3. Voluntary, unconscious, or sub-conscious movements not disordered. Absence of platysma sign and combined flexion of thigh and trunk. The active balance movements of arm may be lacking but there is no exaggeration of passive balance movements. |
| 4. Tongue usually slightly deviated to the paralyzed side. | 4. Tongue sometimes slightly deviated to the paralyzed side; but sometimes contralateral deviation. |
| 5. Hypertonicity of muscles, especially at first. The buccal commissure may be lowered, the eyebrow lowered; there may be exaggerated flexion of the forearm, and the sign of pronation may occur (hand left to itself lies in pronation). | 5. No hypertonicity of muscles. If facial asymmetry exists, it is due to spasm. No exaggerated flexion of forearm, and no pronation sign. |
| 6. Tendon and bone reflexes often disturbed at the beginning, either absent, weakened, or exaggerated (almost always exaggerated.) In many cases, there is epileptoid trepidation of the foot. | 6. No alteration of tendon or bone reflexes. No trepidation of the foot.[878] |
| 7. Skin reflexes usually disordered. Abdominal and cremasteric reflexes, especially at first, weakened or abolished. On stimulation of sole, toes, and especially the great toe, are extended on the metatarsals. Babinski toe reflex. Extension of great toe often associated with abduction of other toes (fan sign). Sometimes exaggeration of reflexes of defence. | 7. No disturbance of skin reflexes. Abdominal and cremasteric reflexes normal. Babinski toe reflex and fan sign absent. Defense reflexes not exaggerated. |
| 8. Contracture characteristic and non-reproducible by voluntary contractions. The hand-grip yields a sensation of elastic resistance, automatically accentuated on passive extension of the hand. | 8. The contracture can be reproduced by voluntary contractions. |
| 9. Evolution of diseased regular contracture follows flaccidity. When regression of disorder occurs, it is progressive. Paralysis not subject to ups and downs (motor defect fixed). |
9. Evolution of disease capricious. Paralysis may remain indefinitely flaccid or may be spastic from the beginning.
Spastic phenomena may sometimes be associated (particularly in the face) with characteristic phenomena. The disorder may get better and worse alternately several times, alter rapidly in intensity, and present transitory remissions which may last even but a few moments (motor defect variable). |
[12] More energetic contraction of platysma on healthy side when mouth is opened or when head is flexed against resistance.
87. Differential between Reflex (Physiopathic) Contracture and Paralysis, and Hysterical Contracture and Paralysis. Babinski, 1917.
| Reflex | Hysterical |
|---|---|
| 1. Paralysis usually limited but severe and obstinate even when methodically treated. | 1. Paralysis usually extensive but superficial and transient if treated. |
| 2. In the hypertonic forms attitude of the limb does not correspond to any natural attitude. | 2. The hysterical contracture as a rule resembles a natural attitude fixed. |
| 3. Amyotrophy marked and of rapid development. | 3. Amyotrophy, as a rule, absent, even when the paralysis is of long standing. If existent, it is not marked. |
| 4. Vasomotor and thermic disorder often very marked, accompanied by an often very pronounced reduction in amplitude of oscillations measured by oscillometer. | 4. There may be thermo-asymmetry but it is slight. There are no very characteristic vasomotor disorders nor modifications in amplitude of oscillations.[879] |
| 5. Sometimes very marked hyperidrosis. | 5. No sharply defined hyperidrosis. |
| 6. Tendon reflexes often exaggerated. | 6. No modifications of tendon reflexes. |
| 7. Hypotonia sometimes very well marked, and in arm paralysis main ballante. | 7. Hypotonia absent. |
| 8. Mechanical over excitability of muscles, often accompanied by slow response (?). | 8. Over-excitability of muscles absent. |
| 9. Fibrotendinous retractions of rapid development except in the rare completely flaccid forms. | 9. No retractions even if paralysis is of long duration. |
| 10. Trophic disorders of bone, decalcification of the hairs and of the phanères. | 10. No trophic disorders. |
88. The section on Shell-shock diagnosis contains 102 cases (Cases 371-472). These cases differ in no respect from those of Section B except that many of them are more puzzling and dubious and have been presented by their reporters more from the standpoint of diagnosis than from that of etiology or therapeutics. In general arrangement, the cases roughly correspond to those of Section B. First are four cases illustrating the value of lumbar puncture data (Cases 371-374). There follow cases with either a mixture of organic and functional symptoms, or such a constellation of symptoms as might readily lead to erroneous diagnosis (Cases 375-381). Retention and incontinence of urine after shell-shock are illustrated in Cases 382-384. Crural monoplegia, monocontractures, and other affections of one leg are shown in Cases 385-392; but these monocrural cases are in many respects peculiar or even unique as compared with the monocrural cases of Section B. Peculiar paraplegias or spasms affecting both legs are found in the series 393-395. Then follow (Cases 396-400) other cases of doubtful spinal cord lesion or shock, including several with dysbasia. Camptocormia, astasia-abasia and abdominothoracic contracture are found respectively in 401, 402, and 403. Affections of one arm follow (Cases 404-409). An assortment of peculiar cases in which the differentiation between hysteria and[880] structural disease is in question, is found in Cases 410-415. Peripheral nerve injuries of a sort which might be confused with Shell-shock phenomena, including one of light tetanus, are considered in Cases 416-419. A variety of cases bearing upon the question of the reflex or physiopathic disorders of Babinski is found in the series of Cases 420-432. Peculiar eye phenomena are presented by Cases 433-438; and cases of otological interest are 439 and 440. Epileptoid, obsessive, fugue, and amnestic phenomena follow in Cases 441-450; 451 and 452 are cases of soldier’s heart. The simulation question is presented in a series of 20 cases (Cases 453-472).
89. We are now ready to consider in how far Shell-shock[13] is a distinctive disease. The physical event, shell-shock[13] we have seen at work in most of the major groups of mental disease and in some groups of nervous disease. Shell-shock, the physical event, has started up a “Shell-shock” paresis, a “Shell-shock” epilepsy, a “Shell-shock” Graves’ disease, a “Shell-shock” dementia praecox, wherein the term “Shell-shock” is merely a more specific term than the term “traumatic.” The physical event, shell-shock, has in special ways also changed the responses of the feeble-minded, the alcoholic, the cyclothymic, and the psychopathic person of whatever ill-defined sort may get into military service.
[13] I capitalize Shell-shock here (as elsewhere) to indicate the name of a supposed disease entity and leave shell-shock without an initial capital to indicate the physical event.
The physical event, shell-shock, has likewise caused focal irritative and destructive brain disease, spinal cord disease, peripheral nerve disease; and many well-recognized species of the so-called “organic” diseases of the nervous system have been produced. Shell-shock “organic” diseases have proved as difficult to tell from all sorts of Shell-shock “functional” diseases as ever have been the organic and functional analogues of these diseases in peace practice.
But, besides (a) sharing in the cause of mental and nervous disease (in the sense of “Shell-shock” general paresis and “Shell-shock” tabes, wherein at least one other factor, viz. the spirochete, is known to be at work) and (b) producing mental and nervous disease by killing or weakening or sensitizing neurones in the classical manner of the “focal” lesion, the physical event, Shell-shock, (c) appears able to bring out the subtler diseases and dispositions of mind which we term psychoneuroses, that is, hysteria, neurasthenia, psychasthenia. Just as we have for years spoken of “traumatic” psychoneuroses, so we may now speak of “Shell-shock” psychoneuroses—nor should anyone believe we cheat ourselves with the idea that the adjective “Shell-shock” has helped us more re genesis than the adjective “traumatic.” “Shell-shock hysteria” and “traumatic hysteria” are on precisely the same—slippery—footing in the matter of their origin. The physics and chemistry of the psychoneuroses remain in Egyptian darkness.
The physical event, shell-shock, then, as the common man might say, affects body, brain, and mind in a great number of familiar ways; and these familiar ways remain as plain or as blind as the neuropathology and the psychopathology of today leave them. If thunderstorms and earthquakes got suddenly more frequent, we should have numbers of “lightning neuroses” and “earthquake hysterias,” neither of which would render the physics and chemistry of the psychoneuroses immediately a whit clearer.
When the common man speaks of some one as suffering from lightning stroke or earthquake, he is entitled to be met halfway by his hearer, who readily understands that the victim is suffering some sort of transient or permanent effects of the stroke or quake. In a like common sense should the term shell-shock be taken. Stroke, quake, or shock, each physical event is recognized as a factor in the situation. An event has become a factor. A condition for which the noun “shell-shock” was descriptive, in the present tense of some event, has passed into history; and the adjective “shell-shock” is now explanatory of the past cause, or one of the past causes, of a new situation. Shell-shock, the physical[882] event, takes part in a great number of pathological events and as such lapses from noun to adjective.
But what are these pathological events, viz., the conditions of disease, that supervene? So far, in our consideration of psychoses incidental in the war, we have found Shell-shock varieties, perhaps, of mental disease; again, possibly a few Shell-shock species, using both these terms, variety and species, in a quasi botanical or zoölogical sense. But in either instance we do not rise, under the ordinary principles of nomenclature, beyond the adjective: Is there any evidence that shell-shock, the physical happening, has issued in a pathological event of greater dignity, namely, a genus of disease? Can shell-shock rise to the dignity of a proper noun, Shell-shock, so that we might think of e.g., a new genus of the psychoneuroses, something coördinate with hysteria, neurasthenia, psychasthenia? None, I believe, has the hardihood to propose a new genus of mental or nervous disease for Shell-shock regarded as a pathological event. A fortiori, it is unheard-of to think of Shell-shock, the pathological event, as representing a new order of such events, coördinate with the psychoneuroses or the epilepsies, for example.
Shell-shock, the pathological event, we conclude, is a variety or a species, hardly a genus or an order of mental or nervous diseases. If we can keep in mind the obvious distinction between shell-shock, the physical event, and Shell-shock, the pathological event, we shall save ourselves much trouble. And if we can apply the ordinary criteria for the differentiation of the great groups (or orders) and the lesser groups (or genera) of mental and nervous disease to the given concrete case, we shall not go far wrong therapeutically in any case of so-called Shell-shock. For Shell-shock, the pathological event, becomes a humble variety or species of disease whose therapeutic indications are in larger part those of higher and comparatively well-recognized genera of disease, e.g., hysteria, neurasthenia, psychasthenia.
A shock is not a smash, a crush, a breach. A shock literally shakes. The shaken thing stays, for a time at least. Shaken up or down, the victim of shock is not at first thought[883] of as done for. The spirit of the language is against the thought of shock as destruction or even as permanent irritation. Shock ought to be a “functional” rather than an “organic” thing, as medicine bandies these terms about. Shell-shock or Surgical Shock, it is all one to the logic of shock, which is thought of as a physical or chemical disturbance of mechanisms and arrangements that are, or ought to be readjustable. The one character which the late Professor Royce told me (in conversation) he could find in the term “functional” was the idea “reversible.” Shock is or ought to be, as a pathological event, reversible.
If this thought is in the backs of our minds as we think of Shell-shock, it can readily be seen why the “organic,” that is, non-reversible diseases, do not take kindly to the term Shell-shock. Shell-shock, the pathological event, prefers to be an item in the pathology of function. Can we further specify? The pathology of function, neuropsychically taken, considers such great groups as the psychoneuroses; (so far as we know) the cyclothymias; some of the symptomatic psychoses; a portion of the alcohol and drug group; some of the epilepsies; perhaps the dementia præcox group; not to mention various unresolved psychopathias. The psychoneuroses are the group most innocent of every “organic” taint: the machinery is assumed to be most normal in them and presumably the effects of disorder most reversible.
Shall we not therefore accept the psychoneuroses as the group in which to place those pathological happenings called Shell-shock? It will do no harm to make this choice if we do it humbly in the spirit of acknowledgment that we know next to nothing about the psychoneuroses. The psychoneuroses should fall on their knees to Shell-shock rather than that Shell-shock make obeisance to the psychoneuroses. For what is a psychoneurosis? It is a functional disease of the nervous system in which the mind plays an important part—it is also probably much else. But the “much else” is as likely to be found in Shell-shock as anywhere else during these particular years.
Thus, rehearsing in a broad way the case arrangement of Section B, we find, first, autopsied cases and cases with lumbar[884] puncture data; then cases with prominent admixture of organic phenomena; a few cases to illustrate the victims’ own impressions of their disease; the long toe to top, or “cephalad” series (crural monoplegias and paraplegias, campto-cormias, astasia-abasias, brachial monoplegias, brachial paraplegias, deafmutism, blindness); the series to illustrate the idea of reflex or physiopathic disorders; the series of delayed Shell-shock phenomena; the series to show the picking out by Shell-shock of ante-bellum weak spots and tendencies in the organism; cases touching the hereditary question; peculiar and unique cases; examples of Shell-shock equivalents; and cases of a psychopathic rather than local hystero-traumatic trend.
90. At the outset of Section B (Shell-shock: Nature and Causes), we face the question of the possibly organic nature of Shell-shock. It is safe to say that the vast majority of cases of Shell-shock do not die of Shell-shock, and the collection of material from true Shell-shock cases that are killed by accident or intercurrent disease has proved a matter of great difficulty under military conditions. Of course, it is possible to answer the question à priori, by agreeing that any case with structural lesion of whatever sort, is by the same token not a case of Shell-shock.
91. Apparently the most informatory case yet presented is that of Mott (Case 197). In this case, death came in 24 hours, and the immediate cause of death was doubtless a small hemorrhage of the spinal bulb. There was a congestion of veins in the bulb, as well as a congestion of the pia mater over all other parts of the brain. Nor was the bulbar hemorrhage unique, for there were a number of superficial punctate hemorrhages. In short, the brain was not even grossly normal, such as one might desire in a case of true Shell-shock as conceived by à priori workers. Yet, according to Mott, there are microscopic changes of an intimate nature that lie nearer to the microscopic possibilities in true Shell-shock. For example, in the bulb itself there was a distinct and photographable change of nerve cells: the vago-accessorius nucleus had cells in a state of chromatolysis. The internal alterations of these cells, with dissolution of chromatic material, may[885] possibly indeed have been the direct cause of death or an indicator of its direct cause. Here again, to accord full justice to Mott’s contention, we are dealing perhaps more with a phenomenon of the cause of death than with a Shell-shock phenomenon. According to Mott, the Shell-shock symptoms themselves are due to capillary anemia and to nerve cell changes such as he found in various regions. These nerve cell lesions were of the nature of chromatolysis and identical with those of the vago-accessorius nucleus. In this connection, one thinks of the ideas of Crile concerning exhaustion and its effect upon certain nerve cells and other cells, and indeed the whole conception runs back to the early years of discussion of the meaning of chromatin deposits in nerve cells, and to the work on fatigue of such cells. It may well be that Mott’s suggestion is sound, and that changes of the order of chromatolysis are what subtend some, if not most, of the phenomena of Shell-shock. On account of the myriad interconnections of neurones and the remote effects upon normal neurones of disturbances of a microchemical or microphysical nature in a few neurones, it would not do to throw out of court forthwith such a contention as that of Mott by triumphantly pointing to the miracle cures of certain Shell-shock phenomena; for it will not necessarily be the chromatolytic (or otherwise microchemically or physically altered) cells that will be directly responsible for the symptoms in question. Cells whose activity is but temporarily in abeyance (perhaps by phenomena akin to diaschisis) might be reached from an unusual source in the process of “miracle cure,” whereupon the newly opened paths of energy might conceivably remain open. Nevertheless, it cannot be denied that there are considerable stretches of speculation in the thread of this hypothesis.
92. Particularly important is the question, how frequently such hemorrhages as those found by Mott in Case 197 occur. Cases are given in the text which show such hemorrhages.
Rather often quoted in this relation is Case 201, a case of Sencert, in which a shell exploded one metre away from a soldier and injured him so that he died that night through the bursting of the pleura of both lungs within a thoracic[886] cage which was quite intact. This sort of finding reminds one of cases in which the inner partitions of houses are burst by explosion when the outer walls remain intact. In particular, one thinks of the physical changes within an aneroid barometer, which have been shown to come about when something is exploded near by. If such an event may happen as the bursting of the lungs within an otherwise intact body, so also is there evidence that a similar event occurs in the nervous system. Clinical evidence of this is obtained in the hemorrhage and pleocytosis of spinal fluid obtained early in the clinical examination of certain cases. In fact, in Case 205 (one of Souques), there is a pleocytosis of the fluid as late as a month after shell-shock. When there is no pleocytosis or hemorrhage, there may be a hypertension of the fluid,—a finding sometimes attributed to Dejerine (see, for example, Case 207, of Leriche). It might be inquired whether the fall sustained by the patient as a result of the shell explosion could not be responsible for the hemorrhage, and this may indeed be the fact in certain instances. Babinski has offered in Case 209, an instance in which hematomyelia (with later partial recovery) was produced in a subject who was lying prone in the performance of machine-gun duty (the phenomena in this case were well described by the victim himself, a veterinary student who was six months a captive in Germany). Doubtless, it would not be difficult to produce a complete series of cases with and without trauma to the tissues investing the nervous system, with definite clinical or autopsy evidence of organic lesions of the nervous system, whether by mechanical impact, by the concussion (windage) of the air, or even by the effects of muscular contractions.
93. A case of Chavigny’s (Case 198), in which there was an extremely careful autopsy, showed a strongly blood-stained cerebrospinal fluid; in fact, there was an intradural hemorrhage, though of minor degree and possibly not the cause of death; and throughout the brain substance there were slight hemorrhagic points. But there was no sign whatever of fracture of the cranial vault or base. Another case of similar meningeal hemorrhage but sharply localized, was Case 199, an instance of minor explosion in which neither skin nor muscles,[887] bone or viscera showed any lesion; and the death, which occurred in seven days, seemed hardly explicable on the basis of hemorrhage itself. In fact, this case would require the sort of microscopic examination performed by Mott in Case 197 for a proof of the cause of death, which was thought by the reporters themselves (Roussy and Boisseau) to be within the field of histology.
94. Case 200 seems to bring proof that there may be areas of gross softening within the spinal cord produced by the concussion of the cord from shell-burst, although there had been no fracture of the spine itself and no penetration of splinters of shell or of bone into the spinal canal or the substance of the cord itself. The argument here is that the tissues that lie between the agent of violence and the interior of the spinal cord are affected en bloc by the impact, the resultant gross or molar lesions being several millimetres or centimetres from the point reached by the impinging body or force. How complicated such a situation might be, we may recall from a case previously studied, namely, Case 103 (Lhermitte), wherein a missile struck the left side of the skull and produced lesions beneath its point of impact, but at the same time apparently caused a contre-coup effect upon the opposite hemisphere. That particular case did not come to autopsy, but Lhermitte’s explanation of its queer association of aphasia with ipsilateral hemiplegia seems sound enough. In fine, what with the mechanical trauma to which many victims of shell explosion are subject, what with the findings in sundry autopsies, and what with the determination of hemorrhage in the spinal fluid early after the shock, it might be conceived that the majority of cases of Shell-shock are actually cases of mechanical injury to the brain or spinal cord in which hemorrhage or laceration and overriding of neuronic tissues would be found. Nor would such a hypothesis be prima facie absurd with the evidence afforded by certain cases of Shell-shock having an admixture of reflex phenomena and other symptoms proved by the older neurologists to be beyond peradventure organic. (Compare, for example, such a case as that of Case 210, with herpes zoster and segmentary symptoms.) It should be remembered, however,[888] that Mott in the case cited above (Case 197) sharply distinguishes between the hemorrhages (especially the bulbar hemorrhage which caused death) and the nerve cell chromatolysis which he regarded as possibly at the basis of Shell-shock symptoms. It is decidedly doubtful whether the hypothesis of microscopic or larger hemorrhages, or of local areas of destruction of neurones will suffice for the explanation of true Shell-shock. This is not to say that in the diagnosis of true Shell-shock (that is, roughly speaking, the psychoneurosis), we shall not need to concede and consider in every case the possibility of traumatic focal brain disease. This will always need to be faithfully excluded in all cases unless the initial set-up of symptoms is so suggestive of immediately curable psychoneurosis that without further ado miracle-therapy is undertaken and executed. But in virtually all the slower cases, an exclusion of organic brain and cord disease is undertaken. Admixtures of organic and focal phenomena are quite in the order of everyday occurrence.
95. Especially good instances of this co-existence of functional and organic symptoms are found in ear cases; and it may be suspected that when, after the war, all these data can be suitably gathered and compared, it will be from the field of otology that some of the most fruitful hypotheses will be developed. In the cases of Shell-shock deafness, mechanical peripheral factors are admixed with central factors in phenomena admitting in some ways more exact diagnosis than in other fields. We may await the correlation of these data by some worker, equally skilled in otology and neurology, with the profoundest interest. Analogous results may be hoped from a correlation of neurological and ophthalmological conceptions.
96. Suffice it to say that the differentiation of organic and functional phenomena has long been possible on the basis of what we know concerning various reflexes (e.g., the Babinski reflex and its congeners); and the net result of this work is that the majority of Shell-shock cases,—that is, cases in which the physical factor shell-shock has entered,—are probably not cases in which a coarse organic disease could be[889] proved to exist, or assumed with any color of likelihood to exist. Even limiting ourselves to cases in which the physical factor shell-shock or some sort of impact with or without an external wound occurred, we shall find cases enough of a truly functional nature, as indicated by their reflexes, to render it quite impossible to assert that they are in the classical sense “organic” cases. Putting these cases with the physical shell-shock factors together with the other large series of cases in which precisely similar symptoms occur without the presence of the physical shell-shock factor, we shall find ourselves convinced that classical Shell-shock phenomena are by and large what is called functional. We shall arrive at the hypothesis that they are cases of hysteria or other form of psychoneurosis, entitled to the diagnosis of traumatic hysteria (or hysterotraumatism, in the sense of Charcot), or not, according to whether the physical factor shell-shock was in evidence. What now underlies the concept functional, as we use it in Charcot’s sense of hysterotraumatism, or in the more modern phrase traumatic hysteria? Do we perhaps mean some microchemical or microphysical change of a reversible nature, similar to that described by Mott, e.g., in Case 197? It is not possible to answer this question at this time.
97. But if we give up the hypothesis of organic disease of the nervous system (that is, the hypothesis of coarse lesions, small or large, conceived to be the direct effect of mechanical impact), can we incriminate any other factor? Chemical factors from the gas of bursting shells may be thought of; yet in abundant cases there is no evidence that these have been in play. They and a variety of other special causes may be found working in a few instances but have nothing to do with the moot question.
98. Upon giving up the organic hypothesis, the modern functionalist is very apt to run directly into the embrace of hysteria. If a thing is not physical, it must be psychical in its genesis, so runs the argument. What, after all, is a neurosis? We mean ordinarily by neurosis, something functional rather than structural. We often mean something psychical rather than peripheral. Accordingly, as we have seen, many[890] writers rush to the hypothesis that Shell-shock effects, except in a few unusual instances of organic disease, are functional; and not only are they functional but psychic, and maintained by some of the so-called “mechanisms” which abound in modern speculative writing.
99. Case 253, a case of Tinel, may serve to illustrate this point. Tinel’s patient was not subject to shell-shock at all, but was wounded in the arm. Three weeks later, he was able to flex his forearm only by means of the supinator longus. It was found that the biceps was soft and flaccid, though the electrical reactions of the biceps were normal. Now, since flexion of the forearm is normally produced by a synergic contraction of the biceps and supinator longus, the situation in Tinel’s case was striking in that the functions of the biceps and supinator longus had been separated out by a process which could not be hysterica. The hypothesis is that in hysteria it has always been found impossible to split the synergic action of these two muscles. What has happened? In Tinel’s picturesque phrase, the biceps muscle has been stupefied by a process which involved no destruction of a nerve trunk or any important nerve elements. This process of stupefaction passed away with a few weeks’ massage and rhythmic faradism. But what is this process of stupefaction, as Tinel calls it? No definite answer can be given. But is not the process analogous to what may happen in a variety of cases of shell explosion in which, for one reason or another, sundry neurones are, as it were, stupefied, stunned, anesthetized, or thrown out of gear by some internal physico-chemical readjustment of unknown nature? Perhaps that readjustment, though in Tinel’s case it probably took place within the tissues of the arm itself, is analogous to the chromatolytic process in nerve-cell bodies suspected by Mott to be at the bottom of certain Shell-shock symptoms as in Case 197.
100. Are there, then, phenomena of peripheral nerve shock analogous to the phenomena of spinal cord and brain shock which we find in so many cases? But if so, it is clearly unnecessary, and indeed injurious for us to conceive that cases proved not to be organic must necessarily be hysterical.[891] Several authors have called a halt upon this undue extension of the concept of hysteria to include all the non-organic phenomena. Take, for example, the case of the Victoria Cross winner (Case 529), reported by Eder, in which a contracture was shown by hypnosis to be a representation of the patient’s clutch upon his bayonet (he had been at Gallipoli and was wounded in fourteen places during a bayonet fight with Turks). It would not be possible—in fact, it would seem almost impolite—to refuse to entertain the hypothesis of a kind of symbolism in the bayonet-clutch contracture of Eder’s case; but it would, on the contrary, be far from exact to consider all cases of contracture to be even probably or possibly symbolic in the manner of the bayonet-clutch. There are, many workers feel, many functional phenomena that are non-hysterical, and as it were infra-hysterical in the sense that the “mechanisms” (to use that over-worked term) are in neurones below the level of complexity required by hysteria. This theoretical possibility (that the functional should be divided into the psychical and the infrapsychical) has been given a new status by the work of Babinski and his associates. That work seems to show that the older doctrines of Charcot concerning the existence of “reflex” disorders, are perfectly sound.
101. Babinski has been able to bring into the light of observation the morbid operation of certain of these reflex arcs. Even in cases where in the waking life the central nervous system is able to overpower the reflex arcs in question and permit the limb or limbs to work reasonably well and smoothly, the process of chloroform anesthesia will quickly bring out an odd and unsuspected interior situation. The chloroform suspends the operation of numerous neurones, including those that have to do with the downflow of cerebral inhibitions, those silent streams of impulse that serve to keep the knee-jerks, for example, in leash. Now at a time when all the other muscles of the body are relaxed, the withdrawal of the cerebral inhibitions by chloroform anesthesia may cause a phenomenon to appear in certain reflex arcs that argues an excess of activity; thus in the leg, for example, an ankle-clonus, or a patella-clonus, or a degree of contracture,[892] may be brought about early in chloroform anesthesia, though there had been little or no suspicion of such a tendency in the waking life. The cerebral inhibitions in the waking life have been enough to dampen the ardor of the reflex arc in question. It must be remarked that these cases of reflex, or, as Babinski termed them, physiopathic disorders, as a rule occur in cases locally wounded. It is the locally wounded limb that develops functional excess of contained reflex arcs. Does this occur by a process of neuritis, or by some other unknown process? Whatever the answer to this question, Babinski and his associates appear to have shown the existence of a group of physiopathic or reflex disorders; disorders below the level of the psyche and below the theatre of operations of hysteria.
102. Practically speaking, also, it is important not to consider every functional situation hysterical, since the non-hysterical functional changes may be extremely obstinate to treatment. Both physician and patient suffer if the patient is treated along psychotherapeutic lines for hysterical symptoms, some of which turn out on investigation to be functional enough but non-psychic. The peculiar configuration of symptoms shown in cases with the physical shell-shock or its equivalent, is perhaps dependent upon what neurones are locally affected. If there has been good evidence of near-by explosion or of wound, it will be especially important to learn just what parts of the nervous system and just what synergic neurones and other structures were affected. Whether the process within these neurones be one analogous to the dissolution of chromatin, or whether the process is more like one of narcosis, or narcosis and stupefaction, or whether the process is more like that of a stun, or like the plight of the nerves in a foot for a long time “asleep,” it may be impossible to say; but it is entirely unnecessary to soar directly to the higher mental process, unnecessary in short, to assume a hysterical dissociation when the dissociation may be far lower down in the nervous system.
103. We have pictured the practical situation in which the neuroses of the war find themselves—a situation bristling with diagnostic difficulties. The great proposition deducible therefrom is,
The diagnostic problem in Shell-shock is the diagnostic problem of neuropsychiatry at large.
The neuroses of war have this in common with the neuroses of peace—that they need to be distinguished from all other nervous and mental diseases. One cannot be a specialist in Shell-shock unless one is a neuropsychiatric specialist; even the neuropsychiatrist has much to learn from the internist, the orthopedist, the neurosurgeon, as well as from the psychologist.
But however wide the diagnostic field for Shell-shock, the therapeutic field is wider still. For the neuropsychiatric reconstructionist has to face the peculiarities of the military status of his ward, the difficulties of demobilization into civilian life (a canal system with very precise technic for the opening and closing of locks), the choice and timing of the proper measures of bedside occupation, of occupation therapy in a broader sense, of prevocational and vocational training—the whole complicated by the character changes that may have set in to bowl over all one’s preconceptions. The nub of the matter, after the era of the manière forte, the brusque psychotherapy, the rough jarring of the man back into approximate normality is, perhaps, this potentiality of subtle character changes defying possibly anybody’s analysis, but stimulating us all to our best endeavor, whether we are physicians, psychologists, occupation-workers, social workers, or nurses. Now that all sorts of reconstruction programs are in the air, each claiming its share, or more than its share, of attention, let us not forget that no one can stake out in any small plot the measures of refitting, readjustment, readaptation, rehabilitation—all these terms with slightly differing denotation have been used—especially when we take into account that not only must the patient be refitted to his entourage,[894] but also not seldom the entourage to its returned Shell-shocker.
104. It is proper to place these general considerations first because the slow, patient, prosaic measures of reëducation are apt to be forgotten in our enthusiasm for the lightning-like cures of the hypnotic, the psychoelectric, the pseudo-operative, and other psychotherapeutic forms. Psychotherapy in all its forms has come into its own in Shell-shock. Miracles or their equivalents are daily wrought by men who are not prophets. Lourdes and Christian Science have their unassuming rivals. Let us remember, however, that even Lourdes and Christian Science never solved 100% of the problems placed before them, even though the votaries have the best will in the world to be cured. If the will itself is disordered, what can be done save investigate? And the mauvaise volonté is by no means absent from some of our prospective patients; witness one man, a Frenchman, who so resented being cured by torpillage, i.e., by the electric brush, that he carried his case against Clovis Vincent, who cured him of his hysteria, clear to the Academy! And, even after we have cured our cases by these modern miracles, let us not be too proud of ourselves! One soldier sent back to Australia, hysterically mute for months, got his voice back after killing a snake—a peculiar instance of occupation-therapy, not enumerated in courses on reconstruction. And remember the man who jumped the wall and got drunk, breaking back into the hospital to show his doctor how his refractory voice had at last come back. Thus there are cures and cures (even a newspaper cure of mutism by a moving picture vision of the antics of Charlie Chaplin), and spontaneous non-medical cures as well as medical ones, and slow cures due to vis medicatrix, as well as to shrewd reëducation measures.
105. I shall not attempt to cover systematically the topic of Shell-shock therapy in this epicrisis. The reader must go through the treated cases, especially in Section D but passim elsewhere, if he is to obtain a proper conception of all the methods so far employed—and at the end he cannot know the ultimate outcome of the cases. Patrons of the miracle[895] cures and the manière forte are having their day: on the whole, the law of sudden onset, sudden ending has much to say for itself in the hysterical (pithiatic) group. Forebodings of relapse in these torpedoed cases may indeed have some foundation: but figures are yet lacking, and relapses may be as expectantly predicted in the slow-onset, slow-cure group. The decision must be post-bellum. Nor must the fact that a few absolutely normal subjects have succumbed de novo to Shell-shock blind us to the fact that, statistically speaking, most cases are ab ovo psychopaths in whom relapses, recurrences, or new instances of neurosis may be confidently expected. For these ab ovo psychopaths, what can suffice but (a) removal of the disease by the vis medicatrix naturae; or (b) reëducation, intellectual or (c) moral (as the case may be); or else (d) some plan of environmental shielding from new occasions of disease?
106. I shall content myself with a brief survey (insisting that the details be read of at least the leading cases in each treatment subgroup) of the cases offered in Section D (Shell-shock: Treatment and Results), consisting of 117 cases (Cases 473-589). The cases are in general arranged with the spontaneous and quasi-natural cures at the outset,—a series of 11 cases (Cases 473-483). The remainder of the section deals with cures under medical conditions, although many cases naturally show an interplay of non-medical factors in the cure or persistence of one or more symptoms.
A few cases illustrative of the physical value of hydrotherapy, mechanical therapy, and drugs are given in a short series (Cases 484-489). A treatment of hysterical contractures by induced fatigue is dealt with in Cases 489-493; and the occasional value of surgery is shown by Case 494.
The simpler methods of persuasion and explanation follow in a series of 19 cases (Cases 495-513).
Pseudo-operations and suggestive operative manipulation of avail in the treatment of certain local hysterical phenomena are considered in a series of eight cases (Cases 514-521). The comparatively long hypnotic series follows: 27 cases (Cases 522-548). The above-mentioned cures by pseudo-operation and by hypnosis may be classified with those that follow, i.e.,[896] mainly rapid cures by psychoelectric methods and by suggestion on emergence from anesthesia (Cases 549-574), as modern miracles. These cases of modern miracle are followed by a briefer set of reëducative cases (Cases 575-589).
Throughout the treatment section are scattered instances in which, not a cure, but merely a modification or even a persistence of symptoms was the outcome. It is useful to bear in mind, while reading cases in the etiological and diagnostic sections, these main divisions of treatment into what might be called (1) spontaneous, (2) rapid (or “miraculous”) and (3) slow or reëducative.
107. It is beyond the scope of this book to deal systematically with the hospital and administrative side of these questions. Especially the zone question is of practical importance, that is, the question of arrangements at the front, on evacuation lines, and in the interior. Roussy and Lhermitte have particularly discussed these matters.
After thirty months’ experience in the psychiatric centers of two armies, Damaye suggested an organization of psychiatric centers in two parts,—First, a service draining patients from the firing line, rapidly give them first care and evacuate them, in charge of special attendants, to: Second, a psychiatric or neurological center in the communication zone (étapes) without danger of bombardment and at a distance from the guns. The more serious cases will then be evacuated, thirdly, into the interior from these centers along communication lines. But most will have gotten well at the front.
108. By orthopedists and mechanotherapeutists too much stress may indeed be laid on non-psychiatric measures, as Duprat hints. Yet perhaps neuropsychiatrists may need as much coaching in the opposite direction. One must remember the non-psychopathic fraction of these Shell-shock disorders and their need of diathermy (Babinski). Duprat says that the centers for physiotherapy cannot effectively do the work of all Shell-shock therapy, as the physiotherapists have their aims fixed on nerves and muscles rather than the mind. Each case requiring psychotherapy ought to be studied in an experimental psychological laboratory from a number of points of view such as mechano-motor capacity, the sensibility, emotional and intellectual sides, memory, impulses and the like. Testing apparatus should be available together with dynamometers, sphygmometers, chronoscopes, ergographs, pneumographs, cardiographs and recording apparatus.
| Phase | I. | PERSUASIVE TALK IN CONSULTING ROOM |
| Phase | II. | ISOLATION, REST IN BED, MILK DIET (a few days) |
| Phase | III. | FARADIZATION |
| Phase | IV. | REËDUCATION (Physiotherapy and Psychotherapy) |
| Phase | V. | AFTER-CARE |
Curing a psychoneuropath means victory in a moral battle!
After Roussy and Lhermitte
| Phase | I. | “TORPILLAGE” AND INTENSIVE REËDUCATION |
| Phase | II. | FIXATION OF PROGRESS BY EXERCISES |
| Phase | III. | PROLONGED SPECIAL TRAINING |
After Clovis Vincent
Specialists for consultation should be available, including ophthalmologists, otologists, laryngologists and electrical specialists. The tests over, the patient should be examined as it were, in a free state and his habits and character noted. Hypnosis may be tried but it should not be prolonged. Psychic contagion is to be avoided especially in the case of subjects with epileptoid crises.
It would be well to establish for the cases regarded as susceptible to psychotherapy, reëducation centers like those for the re-adaptation of the tuberculous. The improved tuberculous are sent to health centers under the Ministry of the Interior for three months at the maximum and emerge much better able to support the exigencies of life. According to Duprat, there ought to be psychotherapy centers which should not in any sense recall asylums for the insane. Set in the country but not far from the city, managed by the psychological physicians and “médecins psychologues, plus éducateurs que médecins.” The personnel should consist of students going into psychiatry and of teachers whose pedagogical practice ought to enable them to second the efforts of the psychiatrists. In this way we might avoid the perpetuation of some of the psychopathies of war.
109. Possibly “putting forward the best foot” may yield a wrong impression of the proportion of what I have termed “miracle cures.” Other devices of a slower nature are mentioned throughout the book. Perhaps much depends on the temperament of the psychotherapeutist, as e.g., Laignel-Lavastine has remarked about the method of psychotherapy by means of conversation: that one might easily remain in a honeymoon state in military psychotherapy. When hundreds and thousands of functional nervous cases pass through one’s hands it is necessary to remember that behind the conversation there stands the imposing finger of material force.
Compare the work of Clovis Vincent, Yealland, Kaufmann.
110. On the other hand, Rows points out that shock is a term that does not explain at all adequately the great variety of mental illnesses occurring in the soldiers at the front. The term is popularly used for cases which recover quickly, but in the majority of cases there is a residuum after the shock has disappeared. Accordingly Rows’ work has dealt chiefly with underlying causes, conditions, and factors. Here we may consider
(a) The war strain before breakdown;
(b) Special causes of shock, such as death of comrades near by, near-by shell explosions and blowing up of trenches;
(c) Fatigue and exhaustion with lowered capacity of resistance.
The men themselves find that they have
(d) undergone a change of character, having become irascible, unable to sustain interest and attention; solitary and morose, and less capable of self-control. Anxiety, worry and a state of morbid expectancy set in. Everyday trifles are exaggerated.
But below these cases are still deeper ones, such as
(e) revival of horrible memories and terrifying dreams of war scenes, together with memories of incidents of past life.
(Rows attributes to Dejerine the idea that the cause of all cases of hysteria and neurasthenia must be sought in antecedent emotion.)
Emotion compels attention, and to such a degree in some cases that the memories and attendant fears and anxieties cannot be expelled. Hallucinations and delusions may then develop. The patient is largely incapable of reasoning about his status; he lacks[901] “insight into the nature and mode of origin of his mental illness. This insight can be provided by explaining to him in plain language the mechanism of simple mental processes, by enabling him to understand that every incident is accompanied by its own special emotional state, and that this emotional state can be re-awakened by the revival of the incident in memory.” The patient and the physician now “begin to realize that they have some ground in common.… The mystery of the illness will be swept away and the physician will be able to … show him how he can educate himself to regain that which was lost.” “The patient can be induced to face the trouble.” “The excessive emotional tone will thus be stripped away and the patient will thus become able to appreciate the real value of the incident.” “The reëducation must vary with each case in order to overcome the difficulties connected with the specific cause which has been discovered.”
Rows’ work has been done at the Red Cross Hospital at Maghull, and several of the Maghull cases have been reported in Elliot Smith and T. H. Pear’s book on Shell-shock. A somewhat similar point of view has been maintained by Wm. Brown, who has suggested the neat term autognosis for psychoanalysis. W. A. Turner speaks of the Maghull point of view as one of modified psychoanalysis.
111. Or again a species of combination of the manière forte and the manière douce (operations, shall we say with William James, of the “tough-minded” and the “tender-minded” respectively?) may be used as in the formula
SYMPATHY + FIRMNESS (Mott).
112. More special devices, suggesting faintly the methods of animal training, may be used, as described in the following account of a new isolation and psychotherapeutic service established in May, 1915, at the Salpêtrière for soldiers with functional nervous diseases. The basic idea has long been held by Dejerine,—the avoidance of heterosuggestion by other patients, imitation, ill effects of visits from members of the family. The functional additions that come from near-by organic patients are among the disadvantages of the ordinary treatment. The isolation service of the neurological center is composed of 34 beds, arranged in two halls, with three extra rooms. Each bed is isolated. The régime in one of the rooms is more rigorous than in the other, and it is an advance for a patient to be moved from the first to the second room. The patient on wakening has no right to leave his box or communicate[902] with his neighbors. He leaves only to be treated by hydrotherapy or electrotherapy. He takes his meals in isolation, receives no calls, and has no leave to go out. The physician sees the patient twice a day and carries on psychotherapy and motor reëducation, as well as special treatments.
Women nurses care for the patients. A system of control and of progressive rewards has been installed, being a sort of metric evaluation of the process of cure. As the cure proceeds the patient’s lot is progressively mitigated, or if he gets worse the regime is clamped down. Suppose a man a victim of paralysis of leg—the height to which he can lift his leg is measured in centimeters daily as well as the time during which he can hold the leg in air; or, the progress of an ankle, or of the forearm or the arm in a case of arm contracture, is measured. The grade obtained by our scholar in psychotherapy is inscribed upon a slate. Finally, walks, concerts, visits and eventually permission to go out into the town are granted.
113. Can Shell-shock neuroses be prevented, other than by stopping or modifying the war or by weeding out Shell-shock candidates as they volunteer or are drafted? Morton Prince offers points of some suggestive value. The very various proportions of neurosis observed in different units and arms of the service suggest that various degrees of preparedness may have played a part. Bernheim says suggestion is an idea accepted. Aside from a possible increase of simulation, much might depend on what idea administered really got accepted! Morton Prince’s plan is that the prevention must be based upon the education of the mind. This therapeutic education should be based, however, on a preliminary systematic study by a board of specialists in the psychoneuroses of (a) the mental attitude of minds generally toward shell fire, and (b) clinical varieties of this “shock” neurosis as it occurs in trench warfare, (c) its frequency and disabling incidence, and (d) the state of mind previous to the trauma of those suffering from it.
On the basis of the findings of such a study, first, the regimental surgeon through lectures and clinical demonstrations would be instructed systematically in the symptoms and[903] pathology of the disease and the methods of psychotherapy for its prevention.
Second, soldiers, including officers, could then, in units of say 100, in turn be instructed in the nature of the disease through lectures by regimental surgeons. Shell-shock, they should be told, is a form of hysteria caused by mental factors. The work of the instruction should be done in France in the atmosphere of the war, wherein would be formed an attitude of healthy mental preparedness instead of an attitude of fear and mystery. Has mental hygiene this great scope? Is morale merely education?
114. What after all, is Morale? We hope to learn a little about it from this war for use hereafter, when we can say with the Florentine
These references were collected in the main by Sergeant Norman Fenton both before and after his entering the army, in connection with preparations for the work of one of the Neuropsychiatric Training Schools (that at Boston), established by the Division of Neurology and Psychiatry of the Surgeon-General’s Office, U. S. Army. The work, through the year 1917, at least, is not a mere vernis de bibliographe, but is based on a first-hand search through journals available in the Boston Medical Library and the New York Academy of Medicine (to whose officers thanks are due for very special privileges accorded). After Sergeant Fenton’s departure for service in the war neurosis hospital, 117, American E. F., France, the work was finished by the writer in considerable haste by skimming the current indexes and gathering the more prominent titles for 1918 (some for 1919). The titles, be it noted, go beyond the scope of the case-material in the body of the book and cover also a variety of reconstructional, reëducational, clinical-neurological, neurosurgical, and other topics bearing indirectly on neuropsychiatry. These auxiliary subjects are by no means completely covered, but it was thought the titles might help other inquirers. Under the war conditions numerous errors have no doubt crept into the references, which errors we hope will not, by reason of the short space of time covered by the bibliography, prove particularly misleading. The auxiliary topics can be referred to in the Index under page-numbers after the word “Bib.”
E. E. S.
Abadie. La neuro-psychiatrie d’urgence aux armées. Presse Méd., Par., 1915, v. 23, p. 46.
Abrahams, Adolphe. A case of hysterical paraplegia. Lancet, Lond., 1915, v. ii, p. 178.
Abrahams, A. “Soldier’s Heart.” Lancet, Lond., 1917, i, 442.
Absence of neuroses in war. N. York M. J., 1916, v. 103, p. 1178.
Ackerley, R. Treatment by physical methods of mental disabilities induced by the war. Proc. Roy. Soc. Med., Lond., 1917-1918, v. 10 (sect. Balneol.), pp. 37-38.
Aconi, A. Le nevrosi di cuore e la guerra. Riforma med., Napoli, 1916, v. 32, pp. 501-505.
Addinsell, A. W. Head injuries in war. Brit. Med. Jour., 1916, ii, 99.
Adler, H. M. The broader psychiatry and the war. Mental Hyg., Concord, N. H., 1917, v. 1, pp. 364-370.
Adrian, E. D. and Yealland, L. R. The treatment of some common war neuroses. Lancet, Lond., 1917, i, 667.
Adrian and Yealland. The treatment of some common war neuroses. Lancet, Lond., 1917, i, pp. 867-872.
After care of nerve injuries. Rev. of War Surg. & Med., 1918, i, no. 3, 49.
Agostini, C. Sulla utilizazione degli epilettici in zona di guerra. Gior. di med. mil., Roma, 1918, lxvi, 24-33.
Agnus, A. Le cloquement de la balle et de l’obus. Rev. Scient., Paris, 1915, li, pp. 358-363.
Agudo Avilla, A. La guerra y las enfermedades mentales. Prensa med. argentina, Buenos Aires, 1916-1917, v. 3, pp. 129-131.
Aimé, Henri. De la variété et de l’évolution des troubles nerveux et psychiques d’origine commotionnelle pendant la guerre. Presse Méd., Par., 1917, v. 25, pp. 113-114.
Aimé, H. et Perrin, E. Considerations sur un cas d’épilepsie partielle guérie après extraction du projectile intra-cérébral. Progrès Méd., Par., 1916, v. 3, pp. 187-189.
Aitkin, D. M. Orthopaedic methods in military surgery. Lancet, Lond., 1917, v. 1, pp. 10-16.
Albert-Weil, E. Physiothérapie et blessés de guerre. Paris Méd., 1914-1915, (Part. Méd.), v. 15, p. 405.
Alberti, A. I servizi psichiatrici di guerra. Riv. ospedal., Roma, 1917, v. 7, pp. 233-245.
Alienée arrosé des passants avec de l’esprit de sel. Ann. méd.-psychol., Par., 1914-1915, v. 6, p. 524.
Allbutt, T. C. Investigation of the significance of disorders and diseases of the heart in soldiers. Brit. Med. Jour., 1917, ii, 139.
Alquier, L. Sur les troubles nerveux par engorgements lymphatiques. Rev. neurol., Par., 1917, v. 24, pp. 8-13.
Alquier, Paul and Tanton, J. L’appareillage dans les fractures de guerre. Collection Horizon, Masson et Cie, Paris, 1916; also trans. Engl. in Military Medical Manuals, Univ. Lond. Press, and in Medical and Surgical Therapy, D. Appleton, N. Y.
Alt, Konrad. Psychische Störungen im Kriege. (D. Oester. Sanat., Wien, 1915, v. 12, p. 2). Aerztl. Central Ztschr., Wien, 1915, also v. 10, pp. 1-2; and 1915, v. 9, p. 2.
Alt, Konrad. Im Deutschen Heere während des Krieges aufgetretende psychische Störungen und ihre Behandlung. Ztschr. f. ärztl. Fortbild., Jena, 1915, No. 11, pp. 331-333.
Alt, Konrad. Ueber die Kur- u. Badefürsorge f. nervenkranken Krieger, mit besonderer Berücksichtigung der sogen. Kriegsneurotiker. Wien. Klin. Wchnschr. Nr. 18, 1918.
Alter, W. Zur Erkenntnis abwegger und krankhafter Geisteszustände bei Schulrekruten. Psychiat.-neurol. Wchnschr., Halle a. S., 1914-1915, v. 16, pp. 327-330; 339-341; 351-356.
Amar, Jules. Le moteur humain. Dunod et Piénat, Paris, 1914.
Amar, J. Principes de rééducation professionnelle. Compt. rend. acad. d. sc., Par., 1915, v. 160, pp. 559-562.
Amar, J. La rééducation des blessés et mutilés de la guerre. Rev. scient., 1915, v. 53, pp. 363-367.
Amar, J. La rééducation professionnelle des blessés et des mutilés de la guerre. J. de physiol. et de path. gen., 1915, p. 820; p. 837; p. 855.
Amar, J. Technique d’éducation sensitive pour amputés et aveugles. Compt. rend. Acad. d. sc., Par., 1916, v. 163, pp. 335-338.
Amar, J. Organization of vocational training for war cripples. Am. J. Care Cripples, N. Y., 1916, v. 3, pp. 176-183, 12 pl.
Amar, J. La rééducation professionnelle des mutilés de guerre. Paris, 1917, P. Renouard, 33 p., 8o.
Amélie, A. C. L. Contribution à l’étude des complications cardiovasculaires mentales de la méningite cérébrospinal de l’adulte. Thèses de Paris, 1915-1916, v. 13.
Amenitski, D. A. The insane at the front. Sovrem. Psikhiat., Mosk., 1915, v. 9, pp. 325-333.
Ancherson, Maria. (Psychosis following gunshot wound of the brain.) Ugeskr. f. Laeger, Kbenh., 1917, v. 79, pp. 1039-1046.
Anderson, H. M. and Noel, H. L. C. Case of shrapnel injury to right parietal cortex, showing paresis of left lower extremity, together with cortical sensory loss and thalamic over-response. Lancet, Lon., 1916, i, 79.
André-Thomas. Discussion de la conduite à tenir vis-à-vis des blessures du crâne—par P. Marie. Rev. neurol., Par., 1916, v. 29, p. 473.
André-Thomas. Le tonus du poignet dans la paralysie du nerf cubital. Paris méd., 1917, No. 49, pp. 473-476.
Angelucci, A. La protezione degli occhi dei soldati e la rieducazione dei ciechi di guerra. Arch. di ottal., Napoli, 1916, v. 23, pp. 177-205.
Anglade. Discussion de la conduite à tenir vis-à-vis des blessures du crâne—par P. Marie. Rev. neurol., Par., 1916, v. 29, p. 471.
Ankle-jerk. Brit. M. J., Lond., 1917, i, p. 556.
Anton, G. Über psychische Folgen von Kopfverletzungen mit und ohne Gehirnerschütterung. Psychiat.-neurol. Wchnschr., Halle a. S., 1914-1915, v. 16, pp. 365-370.
Anton, G. Geistige Wechselwirkung im menschlichen Verkehr und Psychologie der Masse. Neurol. Centralbl., 37, Nr. 12, 1918.
Antonini, G. (Mental symptoms of returning disabled soldiers.) Pensiero med., Milano, 1915, v. 5, No. 50.
À propos d’alcoolisme. J. de méd. et chir. prat., Par., 1916, v. 87, pp. 149-153.
Arinstein, L. S. (Neuropathological observations on those suffering from wind contusion.) Psikhiat. Gaz., Petrogr., 1915, v. 2, pp. 85-88.
Arinstein, L. S. (Hysteria and organic troubles of commotional origin.) Novoye v. Med., Petrog., 1915, v. 9, No. 9 and 10.
Arinstein, L. S. (War and psychiatry.) Russk. Vrach, Petrogr., 1916, v. 15, p. 950.
Armstrong-Jones, R. Psychology of fear. Effects of panic fear in wartime. Hospital, Lon., 1917, lxi, 493.
Armstrong-Jones, R. Relation of alcohol to mental states, particularly in regard to the war. Practitioner, 1918, c, 201.
Armstrong-Jones, R. Mental states and the war; in particular the psychological effect of fear. St. Barth. Hosp. J., Lond., 1916-1917, v. 24, pp. 95-103.
Arnoux. La mort par décompression. La Nature, 18 Dec., 1915.
Ascarelli, A. Una nuova forma di autolesione (noduli sclerotici sottocutanei da iniezione di sostanze inassorbibili). Policlin., Roma, 1917, xxiv, sez. prat., 1407-1410.
Aschaffenburg, G. Über das Zusammenvorkommen organischer und nicht organischer Nervenstörungen. Neurol. Central bl., Leipz., 1915, v. 34, pp. 926-928.
Aschaffenburg, G. Winke zur Beurteilung von nerven- und psychisch-nervösen Erkrankungen. München. Med. Wchnschr., 1915, v. 622, pp. 931-932.
Aschaffenburg, G. Lokalisierte und allgemeine Ausfallserscheinungen nach Hirnverletzung. Die Methode zur Feststellung und ihre Bedeutung für die soziale Brauchbarkeit der Geschädigten. Berl. klin. Wchnschr., 1916, v. 53, p. 127.
Ash, Edwin Lancelot. Nerves in war-time. Lond., 1914, Mills and Boon. 126 p., 8o.
Astvatsturoff, M. L. (Critique of the study of reflex epilepsy, based on observations on wounded.) Psikhiat. Gaz., Petrogr., 1916, v. 3, pp. 185-190.
Athanassio-Benisty, Mme. Formes cliniques des nerfs. Paris, 1917, Masson and Cie, 12o; also transl. Engl. in Medical and Surgical Therapy, D. Appleton, 1918; and in Military Med. Manuals, Univ. Lond. Press, 1918.[14]
[14] These translations from Masson’s Collection Horizon are appearing from time to time and not always mentioned in the body of the bibliography.
Aubaret. L’héméralopie des tranchées. Bull. Acad, de méd., Par., 1917, v. 77, p. 552.
Aubertin. Les tachycardies de guerre. Presse méd., 24 Jan., 1918.
Audibert, Victor. La simulation dans l’armée. Paris méd., 1916, v. 19, pp. 103-106.
Auer, E. M. Phenomena resultant upon fatigue and shock of the central nervous system observed at the front in France. Med. Rec., N. Y., 1916, v. 89, pp. 641-644.
Auer, E. M. Some of the nervous and mental conditions arising in the present war. Mental Hyg., Concord, N. H., 1917, i. 383-388.
Auerbach, F. Der Nachweis der Simulation von Schwerhörigkeit mittels einfacher Gehörprüfung. Deutsche med. Wchnschr., 1916, v. 52, pp. 1600-1601.
Auerbach, F. Zur Erkennung der Simulation von Schwerhörigkeit und Taubheit. Deutsche mil. ärztl. Ztschr., Berl., 1917, 46, 412-17.
Axenfeld, T. Hemianopische Gesichtsfeldstörungen nach Schädelschüssen. Klin. Monatsbl. Augenh., Stuttg., 1915, n. F., v. 20, pp. 126-143.
Axhausen. Die Behandlung der Schädelschüsse. Die Behandlung von Kriegsverletzungen und Kriegskrankheiten in den Heimatlazaretten. Erster Teil, p. 128. Jena, Fischer, 1915.
Babcock, H. L. Bárány tests as applied to aviators. Bos. M. and S. J., 1917, clxxvii, 840.
Babinoff, Y. K. (Characteristics of diseases of the nervous system during the present war.) Mosk. Vrech., Petrogr., 1915, pp. 503-514.
Babinski, J. De la paralysie radiale due à la compression du nerf par des béquilles (Association organo-hystérique.) Rev. neurol., 1914-15, v. 22, pp. 408-409.
Babinski, J. Lésion spinale par éclatement d’obus à proximité sans blessure ni contusion. Rev. neurol., Par., 1914-15, v. 22, pp. 581-583.
Babinski, J. Les caractères des troubles moteurs (paralysies, contractures, etc.), dits “fonctionnels” et la conduite à tenir à leur égard. Rev. neurol., Par., 1916, v. 23, pp. 404; 521-534.
Babinski, J. Réformes, incapacités, gratifications dans les névroses. Rev. neurol., Par., 1916, v. 23, pp. 753-756.
Babinski, J. Discussion de la conduite à tenir vis-à-vis des blessures du crâne—par P. Marie. Rev. neurol., Par., 1916, v. 29, p. 464.
Babinski, J. et Froment, J. Contributions à l’étude des troubles nerveux d’ordre réflexe. Examen pendant l’anesthésie chloroformique. Rev. neurol., Par., 1914-15, v. 22, pp. 925-933.
Babinski, J. et Froment, J. Sur une forme de contracture organique d’origine périphérique et sans exaggération des réflexes. Rev. neurol., Par., 1914-15, v. 222, p. 1276.
Babinski, J. et Froment, J. Les modifications des réflexes tendineux pendant le sommeil chloroformique et leur valeur en sémiologie. Lyon Méd., 1915, v. 124, pp. 347-361. Also, Bull. Acad, de Méd., Par., 1915, v. 74, pp. 439-452.
Babinski, J. and Froment, J. Hysteria or Pithiatism and Reflex Nervous Disorders. Military Medical Manuals, Univ. of London Press, 1918.
Babinski, J. and Froment, J. Service de neurologie militarisé de la Pitié. Rev. neurol., Par., 1916, v. 23, pp. 638-645.
Babinski, J. et Froment, J. Troubles nerveux d’ordre réflexe ou syndrome d’immobilisation. Rev. neurol., Par., 1916, v. 29, pp. 914-918.
Babinski, J. et Froment, J. Abolition du réflexe cutané plantaire, anesthésie, associées à des troubles vaso moteurs et à l’hypothermie d’ordre réflexe. Rev. neurol., Par., 1916, v. 29, pp. 918-921.
Babinski, J. et Froment, J. Paralysie et hypotonie réflexes avec surexcitabilité mécanique, voltaique et faradique des muscles. Bull. Acad, de méd., Par., 1916, p. 40.
Babinski, J. et Froment, J. Contractures et paralysies traumatiques d’ordre réflexe. Presse méd., Par., 1916, v. 24, pp. 81-83.
Babinski, J. et Froment, J. Troubles physiopathiques d’ordre réflexe. Association avec l’hysterie. Evolution de mesures médico-militaires. Presse Méd., Par., 1917, v. 25, pp. 385-386.
Babinski, J. et Froment, J. Hystérie, pithiatisme et troubles nerveux d’ordre réflexe en neurologie de guerre. Paris, 1916, Masson and Cie., 12o; also transl. Engl. in Medical and Surgical Therapy, D. Appleton, 1918, and in Military Med. Manuals, Univ. London Press, 1917.
Babinski, J. et Froment, J. A propos de la communication de Roussy et Boisseau sur le pronostic et le traitement des troubles physiopathiques. Rev. neurol., Par., 1917, v. 24, pp. 527-537.
Babinski, J., Froment, J., et Heitz, J. Des troubles vasomoteurs et thermiques dans les paralysies et les contractures d’ordre réflexe. Ann. de Méd., Par., 1916, v. 3, pp. 461-497.
Babonneix et Célos. Deux cas de goitre exophtalmique survenus à la suite d’une commotion nerveuse. Bull. et mém. Soc. méd. d. hôp. de Par., 1917, v. 33, pp. 738-739.
Babonneix, L. et David, H. Traumatismes cérébraux et syphilis. Rev. neurol., Par., 1917, v. 23, pp. 277-281.
Babonneix et David. Monoplégie hystérique de membre supérieur gauche durant depuis deux ans et guéri en deux jours par la suggestion. J. de méd. et de chir. prat., Par., 1917, v. 88, Oct. 10.
Bailey, Pearce. Neuropsychiatry and the mobilization. N. Y. Med. Jour., 1918, cvii, 794.
Bailey, Pearce. The care of disabled returned soldiers. Pacific M. J., San Francisco, 1917, lx, 608-615.
Bailey, Pearce. The care of disabled returned soldiers. Mental Hyg., Concord, N. H., 1917, v. 1, pp. 345-353.
Bailey, Pearce. Psychiatry and the army. Harper’s monthly mag., 1917, v. 135, pp. 251-257.
Bailey, Pearce. War and mental diseases. Am. Jour. Pub. Health, 1918, viii, 1.
Baldi, Felice. Le subconscient dans la génèse des phénomènes traumato-névrosiques. Contribution à la connaissance de la névrose traumatique. Annali di Neurologia, an XXXII, fasc. 4, pp. 147-178, 1914.
Ballard, E. Fryer. An epitome of mental disorders. 1917, Blakiston, pp. 145-165.
Ballet, Gilbert. Oedème blanc associé aux contractures d’origine psychique. Rev. neurol., Par., 1914-15, v. 222, pp. 705-707.
Ballet, G. Bourdonnements et sifflements d’oreille dus à un trouble du représentation mentale. Rev. neurol., Par., 1914-15, v. 222, pp. 707-708.
Ballet, G. Syndrome de Brown-Séquard par suite de commotion par éclatement d’obus, sans plaie extérieure (hématomyélie vraisemblable). Rev. neurol., Par., 1914-15, v. 222, pp. 768-769.
Ballet, G. Note sur la relation des tremblements et des états émotionnels. Rev. neurol., Par. 1914-15, v. 221, pp. 934-936.
Ballet, G. L’insomnie à crises intermittentes. Presse méd. Par., 1916, v. 24, pp. 73-74.
Ballet, G. Persistance des contractures d’origine psychique pendant le sommeil. Société de Neurol. 29 juillet 1915.
Ballet, G. et Rogues de Fursac, J. Les psychoses “commotionnelles.” Paris méd., 1916, v. 19, pp. 2-8.
Ballet, Sicard, Dejerine, etc. Examens où l’on peut suspecter simulation chez les “blessés nerveux.” Rev. neurol., Par., 1914-15, v. 22, pp. 1245-1247.
Bannard, W. The mechanics of convalescence: methods of hastening the cure of German wounded soldiers. Scient. Am., N. Y., 1915, v. 112, p. 404.
Barat, L. Une fugue confusionnelle en temps de guerre. J. de psychol., norm. et path., Par., 1914, v. 2, pp. 455-463.
Barker, L. F. War and the nervous system. J. Nerv. and Ment. Dis., N. Y., 1916, v. 44, pp. 1-10.
Barr, J., Sir. The “Soldier’s Heart” and its relation to thyroidism. Brit. Med. Jour., 1916, i, 544.
Barron, Netterville. Physical training with especial reference to the training of convalescents. J. Roy. Army Med. Corps, Lond., 1916, v. 27, pp. 460-476.
Barth, E. Ueber organische und funktionelle Kehlkopfstörungen bei Kriegsverletzungen. Berl. klin. Wchschr., 1916, No. 5, pp. 120-121.
Basset, A. Plaies des nerfs des membres par projectiles de guerre. Rev. de Chir., 1916, li, 609.
Batten, F. E. Some functional nervous affections produced by the war. Quart. J. Med., Oxford, 1915-1916, ii, pp. 13-38.
Batten, F. E. Two cases of post-central injury of cortex shown for the purpose of eliciting evidence on—(i) the appreciation of vibration, (ii) Recovery, (iii) Segmental Representation of the Cortex. Proc. Roy. Soc. Med., Lond., 1915-16, v. 9 (neurol. sect.), pp. 67-68.
Baudisson and Marie (A.). Sur la spondylothérapie des troubles asthéniques et vasomoteurs post-traumatiques ou commotionnels. Comp. rend. Acad. d. sc., Par., 1917, clxv, 479.
Bauer, J. Kombinationen organischer mit funktionellen Nervenstörungen. Neurol. Centralbl., Leipz., 1915, v. 34, pp. 175-176.
Bauer, J. Einige Bemerkungen über die Beurteilung und Behandlung der Kriegsneurosen. Wien. klin. Wchschr., 1916, v. 29, pp. 951-953.
Bauer, J. Der Báránysche Zeigeversuch und andere zerebellare Symptome bei traumatischen Neurosen. Wien. klin. Wchschr., 1916, v. 29, pp. 1136-1144.
Baumel, J. La ponction lombaire dans les commotions nerveuses et les traumatismes du crâne par projectiles de guerre. Lyon chirurg., 1915, v. 12, pp. 271-292.
Baumel, J. et Lardennois, G. Diplégie faciale. N. iconog. de la Salpêtrière, Par., 1916-17, No. 4, pp. 272-381.
Bayliss, Wm. M. Intravenous injection in wound shock. Longmans, Green & Co., 1918.
Bayliss, W. M. On the origin of electro-currents led off from the human body, especially in relation to “Nerve-leaks.” Proc. Roy. Soc. Med., Lond., 1917 (sect. of electro-therap.), v. 10, No. 7, p. 11.
Beaton, T. Some Observations on Mental Conditions among a Ship’s Company in War-time. J. Roy. Nav. M. Serv., Lond., 1916, No. 1; pp. 447-452.
Beauchant, R. Morichau. Le signe de l’atrophie musculaire et de l’hyperesthésie profonde dans la tuberculose fibreuse du sommet. Paris Méd., 1916 (Part. Méd.), v. 19, pp. 589-592.
Bechterew, W. M. (War and psychoses.) Novoye v. Med., Petrogr., 1915, v. 9, No. 7, No. 8.
Beck, O. Das Romberg-Phänomen bei traumatischer Neurose (Schrapnellneurose). Monatschr f. Ohrenhk., Berl. u. Wien., 1915, v. 49, pp. 209-210.
Becker, Wern. H. Kriegspsychosen. Psychiat.-neurol. Wchschr., 1914-15, v. 16, pp. 295-298.
Belenki. Les symptomes sensitifs dans les sections anatomiques et physiologiques des nerfs périphériques. Presse Méd. Feb. 17, 1916.
Bellin et Vernet. Sur une forme nouvelle de syndrome bulbaire inférieur avec ataxie du larynx. Bull. et mém. Soc. méd. d’. hôp. de Par., 1917, v. 33, pp. 83-89.
Benassi, G. Malattie vere e malattie simulate in rapporto al servizio militaire. Quaderni di med. leg., Milano, 1917, i. 196; 217-252.
Benedikt. Der Epileptiker bei der Musterung. Wien. klin. Wchschr., 1915, v. 28, pp. 592-593.
Benedikt. Der Epileptiker bei der Musterung. Med. klin., Berl. u. Wien., 1915, v. 22, p. 762.
Benisty-Athanassio. Clinical Forms of Nerve Lesions. Military Medical Manuals, Univ. of London Press, 1918.
Benisty-Athanassio. The Treatment and Repair of Nerve Lesions. Military Medical Manuals, Univ. of London Press, 1918.
Benisty-Athanassio. Traitement et restoration de lésions des nerfs. Collection Horizon, Masson et Cie, Paris, 1917.
Bennati, Nando. La etiologia determinante nella nevrosi traumatica di guerra. Rev. sper. di freniat., Reggio-Emilia, 1916, v. 42, pp. 49-84.
Bennett, Wm. L. Psychasthenia. J. Roy Army Med. Corps, Lond., 1917, v. 28, p. 614.
Benon, R. Au sujet des névroses traumatiques, Réunion de la IIe armée 17 juillet, 1915.
Benon, R. Les maladies mentales et nerveuses et la guerre. Rev. neurol., Par., 1916, 4. 23, pp. 210-215.
Benon, R. Les maladies mentales et nerveuses et la pratique des réformes No. 1. Rev. neurol., Par., 1917, v. 24, pp. 306-309.
Benon, R. La guerre et les pensions pour maladies mentales et nerveuse. Rev. neurol., Par., 1916, v. 24, pp. 320-323.
Bérard. Alcoolisme et anesthésie. Lyon Méd., 1917, v. 126, pp. 282-285.
Bergonzoli, G. Stati ansiosi nelle malattie mentali. Voghers: Art Grafiche, 1915, pp. 186.
Berlung, Richard. Organische Erkrankungen mit hysterische Pseudodemenz. Monatschr. f. Psychiat. u. Neurol., Berl., 1916, v. 39, No. 5; p. 268.
Bernhard, L. I. Business organization of the workshops connected with the Royal Orthopedic Reserve Hospital at Nürnberg. Am. J. Care Cripples, N. Y., 1917, v. 4, pp. 197-200.
Bernheim. Le courage. Rev. gén. de clin. et de thérap., Par., 1915, v. 29, pp. 495-498.
Bernheim. Amaurose simulée et amaurose psychique. Simulation et autosuggestion. Rev. gén. de clin. et de thérap., Par., 1916, v. 30, pp. 609-610.
Bernheim. Psychonévroses, psychothérapie. Rev. gén. de clin. et de thérap., Par., 1916, v. 30, pp. 739-741.
Bernheim. Psychonévroses rebelles. Procédés divers associés à la suggestion. Rev. gén. de clin. et de thérap., Par., 1916, v. 30, pp. 820-823.
Bernheim. Névroses, psychonévroses, hystérie. Progrès méd., Par., 1917, v. 43, pp. 355-357.
Bernheim. Y-a-t-il des aphasies sensorielles?—Surdité et cécité verbales. Rev. gén. de clin. et de thérap., Par., 1917, v. 31, pp. 518-520.
Berruyer. Un cas de surdi-mutité simulée datant de cinq mois. Caducée, Par., 1916, v. 16, pp. 129-130.
Berruyer. Surdité de guerre. Rééducation de l’ouïe. Caducée, Par., 1917, v. 17, pp. 17-21; also pp. 1-3.
Berruyer. Un cas de surdi-mutité simulée datant de cinq mois. J. de Méd. de Par., 1917, v. 36, p. 34.
Bertein et Nimmer. Les premières heures du blessé de guerre du trou d’obus au poste de secours. Collection Horizon, Masson et Cie., 1918.
Besson. Au sujet des névroses traumatiques. Rev. gén. de clin. et de thérap., Par., 1915, v. 29, p. 527.
Besson. Au sujet des névroses traumatiques. Presse Méd., Par., 1915, v. 23, p. 316.
Best, F. Über Nachtblindheit im Felde. München Med. Wchschr., 1915, v. 622, pp. 1121-1124.
Beutenmüller. Über Nachtblindheit im Felde. München med. Wchnschr., 1915, v. 622, p. 1207.
Beyer, Ernest. Über die Bedeutung der Rentenhöhe bei der Entstehung der Rentenneurose. Aerztl. Sachverst. Ztg., 1915, v. 21, pp. 242-244.
Bianchi, V. Le nevrosi nell’ esercito in rapporto alla guerra. Med. e chir. d. med. prat., Napoli, 1917, v. 1, No. 5, pp. 1-16.
Bianchi, V. Le nevrosi nell’ esercito in rapporto alla guerra. Ann. di. nevrol., Napoli, 1917, v. 34, pp. 1-20.
Bianchi, V. Neuropsichiatria di guerra. Ann. di nevrol., Napoli, 1917, v. 34, pp. 21-38.
Bickel, Heinrich. Zur pathogenese der im Krieg auftretenden psychischen Störungen. Neurol. Centralbl., Leipz., 1915, v. 34, pp. 117-121.
Bielschowsky, A. Sehstörungen im Kriege ohne objektiven Augenbefund, München med. Wchnschr., 1914, v. 61, pp. 2443-2445.
Bielschowsky, A. Die Forderung des akademischen Blindenbildungswesens im Kriege. Stuttgart, Enke, 1917.
Bikhovski, S. (Diagnosis of epilepsy in the clinic and in army medical practice.) Psikhiat. Gaz., Petrogr., 1916, v. 3, pp. 300-306.
Bilancioni, G. Di un metodo sicuro per svelare la simulazione della sordita bilaterale. Arch. ital. di otol. (etc.), Torino, 1916, xxvii, 516-524. Also: Policlin, Roma, 1917, xxiv, sez. prat., 743-745.
Bing, Robert. Pathogenese, Prophylaxe und Begutachtung psychoneurotischer Unfallfolgen. Deutsche med. Wchnschr., Berl. u. Leipz., 1915, v. 412, pp. 903.
Binswanger, Otto. Kriegsneurologische Krankenvorstellungen. München med. Wchnschr., 1915, v. 631, p. 1651.
Binswanger, Otto. Hystero-somatische Krankheitsserscheinungen bei der Kriegshysterie. Monatschr. f. Psychiat. u. Neurol., Berl., 1915, v. 38, pp. 1-60.
Binswanger, Otto. Über Kommotionspsychosen und Verwandtes. Cor. Bl. f. Schweiz. Aerzte., 1917, v. 47, pp. 1401-1412.
Bird, Charles. From home to the charge; a psychological study of the soldier. Am. J. Psychol., 1917, v. 28, pp. 315-348.
Birkett. Special discussion on warfare injuries and neuroses. Proc. Roy. Soc. Med., Lond., 1917, v. 10 (sec. Otol.), p. 90.
Birnbaum, Karl. Geistesstörungen im Kriege. Umschau, 1914, No. 43.
Birnbaum, Karl. Kriegsneurosen und psychosen auf Grund der gegenwärtigen Kriegsbeobachtungen. Ztschr. f. d. ges. neurol. u. psychiat., Berl. u. Leipz., 1914-1915, v. 11 (Ref.), pp. 321-369.
Birch-Hirschfeld. Ueber Nachtblindheit im Kriege. Deutsche med. Wchnschr., Leipz. u. Berl., 1916, v. 42, p. 1306.
Bittorf, A. Zur Behandlung der nach Granatexplosionen auftretenden Neurosen. Med. klin., Berl. u. Wien, 1915, v. 112, pp. 897-898.
Bittorf, A. Zur Behandlung der nach Granatexplosionen auftretenden Neurosen. München med. Woch., 1915, v. 62, pp. 1029-1031.
Black. Treatment by physical methods of mental disabilities induced by the war. Proc. Roy. Soc. Med., Lond., 1917-1918, v. 10 (sect. Balneol.), pp. 24-30.
Blanc, Jean. La dysthyroïdie, facteur de névroses. Le réflexe oculocardiaque régulateur de l’opotherapie thyroïdienne. Progrès méd., Par., 1917, No. 12, pp. 95-98.
Blässig. Funktionelle Stimmbandlähmung. München med. Wchnschr., 1915, v. 62, p. 835.
Blin and Kernéis. Un cas de paralysie générale spinale antérieure. Caducée, Par., 1916, v. 16, pp. 111-113.
Blum, E. De la simulation: Étude des qualités que doit posséder le médecin militaire expert. Gaz. hebd. d. sc. méd. de Bordeaux, 1916, 27 août, pp. 124-125, also 1916, 10 Sept., pp. 129-132.
Blum, E. De la simulation “La carotte.” J. de méd. de Bordeaux, 1915-16, v. 45, pp. 274-280.
Blum, E. and Dimier, G. De la simulation; ses causes, son traitement. Gaz. hebd. d. sc. méd. d. Bordeaux, 1916, xxxvii, 76; 84; 93.
Blum, E. La dissimulation. Gaz. hebd. d. sc. med. de Bordeaux, 1917, v. 38, pp. 57-61, and pp. 67-68.
Blumenau, L. V. (Organization of medical aid to neurotic soldiers at the front.) Psikhiat. Gaz., Petrogr., 1915, v. 2, p. 5.
Boeckel, J. À quels accidents tardifs sont exposés les blessés du crâne? Bull. et mém. Soc. de chir. de Par., 1916, v. 42, pp. 1575-1593.
Boeckel, J. Les blessures du crâne. Lyon chir., 1916, 13, pp. 903-911.
Boisseau, J. Quelques exemples de différents modes de suggestion déterminant des accidents hystériques. Presse méd., Par., 1915, v. 23, pp. 47-48.
Bonhoeffer, K. Die Dienstbeschädigungsfrage in der Psychopathologie. Die militärärztliche Sachsverständigentätigkeit auf dem Gebiete des Ersatzwesens und der militärischen Versorgung. Erste Teil, pp. 86-115. Jena, Fischer, 1917.
Bonhoeffer, K. Psychiatrisches zum Kriege. Monatschr. f. Psychiat. un Neurol., Berl., 1914, v. 36, pp. 435-448.
Bonhoeffer, K. Psychiatrie und Krieg. Deutsche med. Wchnschr., 1914, v. 40, pp. 1777-1779.
Bonhoeffer, K. Die Dienstbeschädigungsfrage in der Psychopathologie. Mil. ärtzl. Sachvest-Tatigk., Jena, 1917, i, 86-114.
Bonhoeffer, K. Ueber Fälle von hysterischer Granatexplosionslahmung. Berl. klin. Wchnschr., 1915, lii, 166-168.
Bonhoeffer, K. Über die Abnahme des Alkoholismus während des Krieges. Monatschr. f. Psychiat. u. Neurolog., 1917, 41, 382-5.
Bonhoeffer, K. Die Differentialdiagnose der Hysterie und psychopathischen Konstitution gegenüber der Hebephrenie im Felde. Med. Klin., Berl. u. Wien, 1915, v. 11, pp. 877-881.
Bonhoeffer, K. Erfahrungen über Epilepsie und Verwandtes im Feldzüge. Monatschr. f. Psychiat. u. Neurol., Berl., 1915, v. 38, p. 61.
Bonhoeffer, K. Hysterischer Granatexplosionslähmung. Berl. klin. Wchnschr., 1915, v. 521, pp. 166-168.
Bonhoeffer, K. Über meningeale Scheincysten am Rückenmark. Berl. klin. Wchnschr., 1915, v. 522, pp. 1015-1018.
Bonhoeffer, K. Psychiatrisches zum Krieg. Ztschr. f. Ärtzl. Fortbild., Jena, 1915, c. 12, pp. 1-9.
Bonhoeffer, K. Fälle von sogenannter Granatexplosionslähmung. Neurol. Centralbl., Leipz., 1915, v. 34, pp. 73-74.
Bonhoeffer, K. Die Bedeutung der Kriegsbeschädigungen in der Psychopathologie unter besonderer Berücksichtigung der D.-B.-Frage. Med. Klin., Berl., 1916, v. 12, pp. 1301; also Deutsche med. Wchnschr., Berl. u. Leipz., 1916, v. 42, pp. 1466.
Bonhoeffer, K. Erfahrungen aus dem Kriege über die Aetiologie psychopathischer Zustände. München med. Wchnschr., 1916, v. 63, pp. 1557-1558.
Bonhoeffer, K. Fälle von hysterischer Granatexplosionslähmung. Arch. f. Psychiat., Berl., 1916, v. 56, pp. 701-702.
Bonhomme. Un cas de puérilisme mental post commotionnel. Ann. méd. psychol., Par., 1917, v. 73, pp. 384-390.
Bonhomme et Nordmann. Caractères essentiels de la commotion cérébrospinale. Progrès méd., Par., 1916, pp. 194-196.
Bonhomme et Nordmann. Caractères essentiels de la commotion cérébrospinale. Ann. méd. psychol., Par., 1916-17, v. 7, pp. 530-540.
Bonhomme et Nordmann. Note sur deux cas de déments précoces à l’armée. Ann. méd. psychol., Par., 1916-17, v. 7, pp. 546-549.
Bonhomme et Nordmann. Un cas d’hallucinose. Ann. méd. psychol., Par., 1916-17, v. 7, pp. 549-554.
Bonnier, P. L’état de guerre et les pannes nerveuses. Compt. rend. Soc. de Biol., Par., 1916, v. 75, pp. 216-218; Presse méd., Par., 1916, v. 24, p. 140.
Bonnier, P. Discussion de la conduite à tenir vis-à-vis des blessures du crâne—par P. Marie. Rev. neurol., Par., 1916, v. 29, pp. 5-6.
Bonnus, G. La radiothérapie dans les affections spasmodiques de la moelle par blessures de guerre. Paris méd., 1916, (Part. Méd.), v. 19, pp. 32-35.
Bonnus, Chartier et Rose. Résultats de la radiothérapie dans les traumatisme cranio-cérébraux. Lyon méd., 1917, v. 126, pp. 233-234.
Bonola, F. La sindrome commozionale da scoppio di projettile. Bull. d. sc. med. di Bologna, 1917, 9. s., v. 282-288. Also: Gazz. med. lomb., Milano, 1917, lxxiv, 189-192.
Bonola, F. I disturbi psico-nervosi dei combattenti. Quaderni di psichiat., Genova, 1917, v. 4, pp. 141-156.
Bonola, F. Contributo allo studio delle psiconevrosi di guerra. Gior. di med. mil., Roma, 1915, lxiii, 837-841.
Bonola, F. (Psychoneuroses of War. A case of psychic deafness.) Gior. di med., Mil., 1915, v. 63 (Nov.).
Borchard, A. Spätapoplexien nach Gehirnschüssen und Schadelplastiken. Centralbl. f. Chir., Leipz., 1917, 44, 650.
Bordier, H., et Gérard, M. Ce que peut donner la radiothérapie dans les lésions nerveuses par blessures de guerre. Presse méd., Par., 1917, v. 25, pp. 453-455.
Borishpolski, Ye. S. (Role of the motor area of the brain cortex in the development of epileptic attacks, based on observations on wounded.) Psikhiat. Gaz., Petrogr., 1916, v. 3, p. 119.
Borne. De la rééducation et de la réadaptation au travail des blessés et des mutilés de la guerre. Rev. d’hyg., Par., 1915, v. 37, p. 81; p. 159.
Borne. De l’assistance et de la réadaptation des malades de la guerre. Rev. d’hyg., Par., 1915, v. 37, pp. 833-849.
Borne. De la réadaptation et de la rééducation au travail des blessés et des mutilés de la guerre. Paris méd., 1915-16, v. 17, pp. 293-298.
Borovikoff, I. V. (Prisoners and those under test for insanity, and insane, in the psychiatric ward of the Riga military hospital.) Voyenno-Med. J., St. Petersb., 1914, ccxxxix, med.-spec. pt., 221-240.
Boschi, G. La neuropsychiatrie et la guerre. Rev. neurol., Par., 1917, v. 24, p. 474.
Boschi, G. L’assistenza feminile nei reparti maschili dei manicomi durante la guerra. Atti Accad. d. sc. med. e nat. di Ferrara (1914-15), 1915-16, lxxxix, No. 2, 3-7.
Boschi, G. (Provision for the Care of War Neuroses and Psychoses in France.) Gior. di med., Mil., 1917, v. 65, Nov. 30.
Bossi, P. Il padiglione di meccanoterapia F. Ponti. Osp. Maggiore, Milano, 1916, 2 s., v. 4, pp. 144-153.
Bostroem, A. Zur Psychologie u. Klinik der psychogenen Hörstörungen. Ztschr. f. d. ges. Neurol. u. Psychiat., 40, 1918.
Bott, E. A. Rehabilitation of wounded Canadian soldiers. Mod. Hosp., 1917, ix, 365.
Boucherot, F. M. A. Maladies mentales dans l’armée en temps de guerre. Thèses de Paris., 1915-16, No. 37, v. 2.
Bouquet, Henri. La rééducation des mutilés de la guerre. Bull. gén. de thérap., Par., 1916, v. 85, pp. 156-181; pp. 193-213.
Bouquet. Deux cas de tétanos localisé tardif. Bull. gén. de thérap., Par., 1916, v. 168, pp. 814-817.
Bourgeois, H. and Sourdille. Otites et surdités de guerre. Collection Horizon, Masson et Cie., Paris, 1917.
Bourgeois, H. and Sourdille. War Otitis and War Deafness. Military Medical Manuals, Univ. of London Press, 1918.
Bourgeois, A. Traumatismes graves de l’oeil par blessures de guerre dans lésions immédiatement apparentes. Arch. d’ophth., Par., 1914-15, v. 34, pp. 766-769.
Bourillon. Comment rééduquer nos invalides de la guerre: l’assistance aux estropiés et aux inutilés en Danemark, Suède, et Norvège. Collection Horizon, Masson et Cie, 1916.
Bourillon. Functional readaptation and professional reëducation of the disabled victims of the war. Amer. Jour. Care for Crip., 1916, iii, 23.
Bourillon. The vocational re-education of disabled soldiers. Mil. Hosp. Com. Canada, Spec. Bull., Ottawa, 1916, pp. 77-89.
Boven. Discussion de la conduite à tenir vis-à-vis des blessures du crâne—par P. Marie. Rev. neurol., Par., 1916, v. 29, pp. 4-5.
Boveri, P. Di alcune questioni medico-legali in rapporto alla guerra; le nevrosi. Riv. crit. in materia di infortuni (etc.), Roma, 1916, v. 5, pp. 33-35.
Brackenbury, H. B. Discharged disabled soldiers and sailors. Brit. M. J., Lond., 1917, v. 2, p. 437.
Braquehaye. Section du nerf médian droit. Suture immédiate du nerf. Retour partiel des fonctions. Reunion med. de la VI armée, Nov.-Dec. 1915.
Brasch. Herzneurosen mit Hauthyperästhesie. Med. klin., Berl. u. Wien., 1915, v. 111, pp. 627.
Braunschweig. Kurze Mitteilungen über die epidemische Hemeralopie im Felde. Med. Klin., Berl. u. Wien., 1915, v. 111, pp. 313-314.
Bresler. Schädel- und Gehirnverletzungen (Bib.) C. Marhold, Halle, 1917.
Briand, Marcel. Les toxicomanes et la mobilisation. Presse méd., Par., 1914, v. 22, pp. 751-752.
Briand, Marcel. Les fugueurs à l’armée. Soc. de méd. lég. de France, Bull., Par., 1915, v. 12, pp. 42-63.
Briand, Marcel. Les comitiaux à l’armée. Soc. de méd. lég. de France, Bull., Par., 1915, v. 12, pp. 196-202.
Briand, Marcel. Discussion de la conduite à tenir vis-à-vis des blessures du crâne—par P. Marie. Rev. neurol., Par., 1916, v. 29, p. 470.
Briand, Marcel. Troubles organiques d’origine fonctionnelle chez les militaires commotionnés. Ann. méd.-psychol., Par., 1917, v. 73, pp. 577-582.
Briand, Marcel et Delmas. Sur la liquidation des indemnités aux militaires “persévérateurs” atteints de troubles fonctionnels hystériques. Soc. méd. lég. de France, Par., 1917, v. 14, pp. 223-233.
Briand et Haury. Rôle de la complicité dans la simulation ou la provocation des maladies. Soc. de méd. lég. de France, Bull., Par., 1916, v. 13, pp. 51-59.
Briand et Kalt. Maladies simulées et maladies provoquées dans l’armée. Soc. de méd. lég. de France, Bull., Par., 1917, v. 14, pp. 42-48.
Briand, Marcel et Philippe, Jean. L’audi-mutité rebelle, d’origine émotionelle. Progrès Méd., Par., 1916, No. 17, pp. 145-148.
Brickley, C. W. Treatment by physical methods of mental disabilities induced by the war. Proc. Roy. Soc. Med., Lond., 1917-1918, v. 10 (sect. Balneol.), pp. 36-37.
Briggs, L. V. A plea for more psychiatrists and neurologists for war service. Proc. Alienists and Neurol. Am., Chicago, 1917, v. 6, p. 31.
Broca, Aug. Troubles locomoteurs consécutifs aux plaies de guerre. Collection Horizon, Masson et Cie, Paris, 1918.
Broca, A. et Ducsoquet. La prothèse des amputés en chirurgie de guerre. 1917, Paris, Masson and Cie.
Brock, A. J. The war neurasthenic. Lancet, Lon., 1918, i, 436.
Brock, L. G. Reëducation of the disabled. Amer. Jour. Care for Crip., 1917, iv, 19.
Brocq. Influence de la guerre sur les affections cutanées. Bull. méd., 1916, No. 3.
Brodman, K. Zur Neurologie der Stirnhirnschüsse. München med. Wchnschr., 1915, v. 622, p. 1120.
Brousses, J. Une mécanothérapie de fortune à l’hôpital complémentaire No. 31 de Toulouse. Arch. de méd. et pharm. mil., Par., 1914-15, v. 64, pp. 177-185.
Brovchinski, A. V. (Case of nervous symptom complex due to wind contusion.) Psikhiat. Gaz., Petrogr., 1916, pp. 237-240.
Brovchinski, A. V. (Paraplegia in atmospheric contusion.) Psikhiat. Gaz., Petrogr., 1916, v. 3, pp. 394-398.
Brown, H. E. Head, abdominal and joint injuries; notes on cases. Lancet, Lon., 1916, i, 1082.
Brown, Mabel W. and Williams, Frankwood E. Neuropsychiatry and the War, 1918.
Brown, Mabel W. and Williams, F. E. Neuropsychiatry and the War; a bibliography with abstracts. Mental Hyg., Concord, N. H., 1917, v. 1, pp. 409-474.
Brown, William. Shell shock without visible signs of injury. Proc. Roy. Soc. Med., Lond., 1915-1916 (sect. Psychiat.), pp. 301-32.
Bruce, Ninian. The Treatment of Functional Blindness and Functional Loss of Voice. Rev. Neurol. and Psychiat., Edinb., 1916, v. 14, pp. 195-198.
Brunig, F. Ueber grosse lufthaltige Gehirncyste nach Schussverletzung. Bruns’ Kriegschir. Hefte d. Beitr. z. klin. Chir., Tübing., 1917, 107, 432.
Bruns, L. Kriegsneurologische Beobachtungen und Betrachtungen. Neurol. Centralbl., Leipz., 1915, v. 34, pp. 12-15.
Bucky. Diathermia in den Lazaretten. Deut. Med. Woch., 1915, xli, 467.
Bulletins. Federal Board for Vocational Education. Nos. 1-10, 1917-1918. Washington Government Printing Office.
Bunnemann. Zur traumatische Neurose im Kriege. Neurol. Centralbl., Leipz., 1915, v. 34, pp. 888-898.
Bunnemann. Die Neurosenfrage und das biologische Grundgesetz. Neurol. Centralbl., Leipz., 1916, v. 35, pp. 178-187.
Bunse, P. Die reaktiven Dämmerzustände u. verwandte Störungen in ihrer Bedeutung als Kriegspsychosen. Ztschr. f. d. ges. Neurol. u. Psych., 40, 1918.
Burke, Noel H. M. Electrotherapy in Military Hospitals. Arch. Radial. and Elec., Lond., 1917, Oct., pp. 130-135.
Burniston, Hugh S. Notes on a successful case of treatment by suggestion. J. Roy. Nav. M. Serv., Lond., 1917, v. 3, pp. 116-117.
Burton-Fanning, F. W. Neurasthenia in soldiers of the home forces. Lancet, Lond., 1917, v. 1, pp. 907-911.
Burton-Fanning, F. W. Neurasthenia in soldiers of the home forces. Lancet, Lon., 1917, i, 907.
Bury, J. S. Distant effects of rifle bullets, with special reference to the spinal cord. Brit. Med. Jour., 1916, ii, 212.
Busacchi, A. Edemi pseudo-traumatici della man. Bull. d. sc. med. di Bologna, 1917, 9. s., v. 345-355.
Buscaino, V. M. and Coppola, A. Disturbi mentale in tempo di guerra. Riv. di patol. nerv., Firenze, 1916, v. 21, pp. 1-103; also pp. 135-182.
Buschan, Georg. Über Kriegspsychosen. Med. Klin., Berl. u. Wien, 1914, v. 102, pp. 1588-1591.
Butenko, A. A. (The War and Mental Diseases in Women.) Obozr. Psikhiat., Neurol. (etc.), Petrogr., 1914-1915, v. 19, pp. 521-542.
Butt, A. P. Destruction of the spinal cord by molecular vibration. Surg., Gynec. and Obst., Chicago, 1915, xx, 486.
Buttersack. Zur Casuistik der Kriegsneurosen. Med. Cor.-Bl. d. würtemb. ärztl. Landesver., Stuttg., 1916, v. 86, pp. 1-5.
Buzzard, E. Farquhar. “Warfare on the Brain.” Lancet, Lond., 1916, ii, pp. 1095-1099.
Call, Annie P. Nerves and the war. 1918.
Calot, F. Orthopédie de guerre; appareil pour fractures, etc. Paris, 1916, A. Maloine et fils, p. 100, 8o.
Cadenat, F. M. Le pronostic des fractures du crâne par projectiles. Paris méd., 1915 (Part. Méd.), v. 17, pp. 437-44.
Campbell, A. W. Remarks on some neuroses and psychoses in war. M. J. Australia, Sydney, 1916, i, pp. 319-323.
Campbell, Harry. War neuroses. Practitioner, Lond., 1916, v. 96, pp. 501-509.
Camus, J. L’évaluation des incapacités fonctionnelles. Paris méd., 1916-17, (Part. Méd.), v. 21, pp. 289-297.
Camus, J. Le corps de rééducation physique du Grand-palais. (Dépot de physiothérapie). Arch. de méd. et pharm., mil., Par., 1916, v. 65, pp. 365-410.
Camus, J. Les sourds, leur placement, leurs intérèts economiques et sociaux. Presse méd., Par., 1917, v. 25, pp. 309.
Camus, J. La rééducation des aveugles de guerre. Presse méd., Par., 1917, v. 25, p. 309.
Camus, J. Placement et rééducation des grands infirmes par lésions des centres nerveux. Paris méd., 1917, No. 27, pp. 1-5.
Camus, J. et Nepper. Recherches sur les réactions psychomotrices et émotives des anciens trépanés. Rev. neurol., Par., 1916, v. 29, pp. 923-924.
Capelle, W. Über Prognose und Therapie der Schädelchüsse. München. Med. Wchnschr., 1917, 64, Nr. 8.
Capgras, Juquelier et Bonhomme. La confusion mentale de guerre. J. de méd. de Bordeaux, 1917, v. 88, pp. 164-165. Rev. Progrès méd., Par., 1917, v. 43, p. 355.
Cardgill, L. V. Recent work on ophthalmology. Practitioner, Lond., 1916, v. 97, p. 44.
Carle, M. Vocational schools for war cripples in France. Amer. Jour., Care for Crip., 1917, v, 165.
Carle, M. Les écoles professionnelles de blessés à Lyon. Par., 1915, p. 132, 8o.
Carlill, Hildred. The diagnostic importance of ankle-jerk. J. Roy. Nav. Med. Serv., Lond., 1916, ii, pp. 180-190.
Carlill, Hildred. Korsakow’s psychosis in association with malaria. Lancet, Lond., 1917, i, v. 192, pp. 648-650.
Carlill, Fildes and Baker. A report on cases of syphilis of the central nervous system observed in the Neurological Department of Royal Naval Hospital, Haslar, during twelve months. J. Roy. Nav. Med. Serv., Lond., 1917, v. 3, pp. 397-427.
Cas remarquable de protection crânienne par le casque. Lyon méd., 1916, v. 125, pp. 259-261.
Case of Emotional Mutism. Brit. M. J., Lond., 1916, i, p. 769.
Cases of neurasthenia and mental shock. Mod. Hosp., St. Louis, 1917, ix, 368.
Caspari, J. Klinische Beiträge zur Differentialdiagnose zwischen Epilepsie und Hysterie aus den Erfahrungen des gegenwärtigen Krieges. Inaug-Dissert., Berlin, 1916.
Cassirer. Demonstration eines Falles von Erythromelalgie. Berl. klin. Wchnschr., 1915, v. 421, p. 168.
Cassirer. Demonstration von Verwundeten mit erfolgreicher Nervennaht. Neurol. Centralbl., Leipz., 1915, v. 34, pp. 284-287.
Cassirer. Über Kombination funktioneller und organischer Symptome bei Kriegsverletzungen. Ztschr. f. d. ges. Neurol. Psychiat., Berl. u. Leipz., 1916, v. 30, p. 229.
Castex, André. Surdités de guerre. Bull. acad. de méd., Par., 1915, v. 74, pp. 547-548.
Castex, André. La rééducation des sourds de guerre. (Présentation de militaires rééduqués.) Bull. Acad, de méd., Par., 1917, v. 77, p. 817.
Catalepsie “post mortem.” Caducée, Par., 1916, v. 16, p. 101.
Cathelin, F. Classifications des troubles sphinctériens avec les blessures ou commotions de la région lombo-sacrée. Paris méd., 1917, No. 42, pp. 319-323.
Catola, G. Neuropatologia di guerra; le ferite dei nervi periferici. Riv. di patol. nerv., Firenze, 1915, v. 20, pp. 533-554.
Catola, G. A proposito di alcune sindromi nervose funzionali di guerra con considerazioni in rapporti alla simulazione nelle sue varie forme. Riv. di patol. nerv., Firenze, 1916, v. 21, pp. 662-675.
Cestan. Discussion de la conduite à tenir vis-à-vis des blessures du crâne—par P. Marie. Rev. neurol., Par., 1916, v. 29, pp. 465-466.
Cestan; Descomps, Paul; et Sauvage, Roger. Les troubles de l’équilibre dans les commotions crâniennes. Paris méd., 1916 (Part. Méd.), v. 19, pp. 518-525.
Cestan, R.; Descomps, Paul; Euzière, J. Les empreintes digitales dans les lésions nerveuses du membre supérieur. Leur application au diagnostic des névrites traumatiques. Presse méd., Par., 1916, v. 24, pp. 258-262.
Cestan, Descomps, P., et al. “La marche sous courant galvanique” chez les commotionnés et les traumatismes du crâne. Bull. et mém. Soc. méd. d’hôp. de Par., 1916, v. 32, pp. 1730-1747.
Cestan, Descomps P., Euzière, J. et Sauvage, R. Troubles de la sensibilité d’origine corticale à disposition pseudo-radiculaire en épilepsie Jacksonnienne. Rev. neurol., Par., 1917, v. 24, pp. 235-242.
Cestan, Descomps, P., et Sauvage, R. Sur une nouvelle méthode d’exploration du sens de l’orientation et de l’équilibre chez les traumatismes du crâne. La[917] sensibilisation à l’épreuve de Babinski-Weill. (Rev. Neurol., Par., 1917, p. 368) Bull. et mém. Soc. méd. d’hôp. de Par., 1916, v. 32, pp. 1381-1403.
Chalier, A. et Chalier, J. Des phlegmons provoqués chez les soldats. Rev. internat. de méd. et de chir., Par., 1914-16, v. 25, pp. 277-281.
Chalier, A. and Glénard, R. Grandes blessures de guerre. Rev. de Chir., 1916, li, 210.
Chamberlin, J. W. Injuries in modern warfare. Boston M. and S. J., 1917, i, p. 113; also p. 116.
Chapin, F. Stuart. The training school of psychiatric social work at Smith College. IV. A scientific basis for training social workers. Mental Hygiene, II, October, 1918.
Charon, R. Psychopathologie de guerre. Progrès méd., Par., 1914, v. 30, pp. 425-428.
Charon, R. et Halberstadt, G. Puérilisme mental au cours d’une psychose postcommotionnelle. Rev. neurol., Par., 1916, v. 24, pp. 316-319.
Charon, R. et Halberstadt, G. Les troubles psychiques des commotionnés. Paris méd., 1917, No. 27, pp. 23-32.
Charpentier, R. Un cas de puérilisme mental au cours des opérations de guerre. Rev. neurol., Par., 1917, v. 24, pp. 296-306.
Chartier, M. Un cas de paralysie hystérique persistant chez un sujet en danger de mort par immersion. Rev. neurol., Par., 1914-15, v. 222, pp. 1241-1245.
Chatelin and de Martel. Blessures du crâne et du cerveau. (Collection Horizon), Paris, 1917.
Chatelin, C. and De Martel, T. Wounds of the Skull and Brain. Military Medical Manuals, Univ. of London Press, 1918.
Chauvin, H. et Heiser. À propos d’un cas de tétanos monoplégique. Rev. neurol., Par., 1917, v. 24, p. 445.
Chavanne, F. Les sourds, leur placement, leurs intérêts économiques et sociaux. Presse méd., Par., 1917, v. 25, p. 309.
Chavigny, P. Étude médico-légale sur les mutilations volontaires par coup de feu. Soc. de méd. légal de France, Bull., Par., 1915, v. 12, pp. 209-222.
Chavigny, P. Les réformes et l’aptitude au service militaire. Soc. de méd. lég. de France, Bull., Par., 1915, v. 12, pp. 253-260.
Chavigny, P. Phlegmons provoqués par injection sous-cutanée d’essence de térébenthine, de pétrole ou d’essence de pétrole. Soc. de méd. lég. de France, Bull., Par., 1915, v. 12, pp. 274-284.
Chavigny, P. Psychiatrie et médecine légale aux armées. Paris méd., 1915, (part. méd.), v. 17, pp. 184-189.
Chavigny, P. À propos des mutilations volontaires doit-on le dire? Paris méd., 1915 (part. méd.), v. 17, pp. 384-387.
Chavigny, P. Psychiatrie des armées. Paris méd., 1915 (part. méd.) v. 17, pp. 415-423.
Chavigny, P. Étude médico-légale sur les mutilations volontaires par coup de feu. Ann. d’hyg., Par., 1915, v. 24, pp. 5-21.
Chavigny, P. Psychiatrie aux armées. Thérapeutique et médecine légale. Paris méd., 1916 (part. méd.), v. 19, pp. 8-13.
Chavigny, P. Les maladies méconnues. Anesthésies et analgésies hystériques. Paris méd., 1916 (part. méd.), v. 19, pp. 214-215.
Chavigny, P. Maladies provoquées ou simulées en temps de guerre. Paris méd., 1916 (part. méd.), v. 21, pp. 150-153.
Chavigny, P. Les explosions des champs de bataille. Ann. d’hyg., Par., 1916, v. 25, pp. 5-25.
Chavigny, P. La complicité dans la simulation et la provocation des maladies. Soc. de méd. lég. de France, Bull., Par., 1916, v. 13, pp. 74-76.
Chavigny, P. Présentation d’un blessé atteint de monoplégie hystérique. Presse méd., Par., 1917, v. 25, p. 193.
Chavigny, P. Un fugueur pendant la guerre. Presse méd., Par., 1917, No. 31, P 326.
Chavigny, P. Un cas de dipsomanie. Presse méd., Par., 1917, v. 25, p. 502.
Chavigny, P. Les maladies rares et le diagnostic de la simulation. Un cas de “tic de la marche.” Caducée, Par., 1917, v. 17, pp. 45-49.
Chavigny et Laurens. Un fugueur pendant la guerre. Rev. neurol., Par., 1917, v. 24, p. 486.
Chavigny et Spillman, L. Un cas de hystéro-traumatisme revu 15 ans après les accidents initiaux. Paris méd., 1916 (part. méd.) v. 19, pp. 525-527.
Chevallier. Installation et résultats du service de rééducation physique et massage au cantonnement de Villetaneuse occupé par le Ne régiment de Zouaves. Arch, de méd. et pharm. mil., Par., 1916, v. 65, pp. 411-433.
Chevallier, Paul. Traitement pratique de la blennorragie chez l’homme. Presse méd., Par., 1917, v. 25, pp. 573-574.
Chevalier-Lavaure. A propos de la réforme des militaires aliénés. Montpel. méd., 1916, n.s., v. 39, pp. 418-427.
Chevassu, M. Les traumatismes cranio-cérébraux dans la zone de l’avant. Montpel. méd., 1916, v. 39, p. 29.
Cheyrou. Réactions immédiates observées à la suite d’éclatements à proximité de projectiles de guerre. Caducée. Par., 1917, xvii, 31-33.
Chiari, H. Zur Pathogenese der Meningitis bei Schussverletzungen des Gehirns. Münch. med. Wchnschr., 1915, v. 621, pp. 596-598.
Chiray. Centre neurologique de la 10e région (Rennes). Rev. neurol., Par., 1916, v. 23, pp. 672-686.
Chiray. Discussion de la conduite à tenir vis-à-vis des blessures du crâne—par P. Marie. Rev. neurol., Par., 1916, v. 29, p. 472.
Chiray, J., Bourguignon, G. et Dagnan-Bouvert. Interprétation des discordances entre les réactions électriques et les signes cliniques, dans les lésions nerveuses périphériques. Paris méd., 1916 (part. méd.) v. 21, pp. 220-224.
Cimbal. Psychosen und Psychoneurosen im IX. Armeekorps seit der Mobilmachung. Berl. klin. Wchnschr., 1915, v. 52, p. 304.
Cimbal. Die seelischen und nervosen Erkrankungen, seit der Mobilmachung. Neurol. Centralbl., Leipz., 1915, v. 34, pp. 411-415.
Clarke, C. K. Psychiatric treatment. Mil. Hosp. Com. Canada, Spec. Bull., Ottawa, 1916, p. 101.
Clark, D. A. Treatment by physical methods of mental disabilities induced by the war. Proc. Roy. Soc. Med., Lond., 1917-18, v. 10 (sect. Balneol.), pp. 12-18.
Clark, E. Eyesight and the war. Med. Press and Circ., Lond., 1916, ii, pp. 72-74. Also: Nature, Lond., 1916, v. 96, pp. 552-555.
Clark, E. Clinical lecture on eyesight and the war. Med. Press and Circ., Lond., 1916, v. 102, p. 72.
Clarke, J. Mitchel. Some neuroses of the war. Bristol. M. Chir. J., 1916, v. 34, p. 130. Rev. J. Nerv. and Ment. Dis., N. Y., 1917, i, p. 119.
Claude, Henri. Les états névropathiques (Rev. neurol., Par., 1914-15), v. 222, p. 1162.
Claude, H. L’organisation et le fonctionnement des centres neurologiques régionaux. Paris méd., 1915 (part. méd.), v. 17, pp. 61-65.
Claude, H. Discussion de accidents nerveux par la déflagration des explosifs. Rev. neurol., Par., 1916, v. 23, pp. 587-590.
Claude, H. Discussion de la conduite à tenir vis-à-vis des blessures du crâne—par P. Marie. Rev. neurol., Par., 1916, v. 29, pp. 460-462.
Claude, H. Discussion de Vincent. Rev. neurol., Par., 1916, v. 29, p. 587.
Claude, H. De l’évolution des incapacités dans les attitudes vicieuses sans rapport avec des lésions organiques appréciables. Paris Medical, octobre 1916.
Claude, H. War neurology; traumatic lesions of nerves by projectiles. Med. Press, and Circ., Lond., 1916, v. 102, p. 72, and p. 469.
Claude, H. L’évaluation des incapacités dans les attitudes vicieuses sans rapport avec des lésions organiques appréciables. Paris méd., 1916-17, v. 21, pp. 300-305.
Claude, H. L’anesthésie régionale associée aux méthodes psychophysiothérapiques dans le traitement des attitudes vicieuses et des tremblements des membres inférieurs d’ordre fonctionnel. Bull. et. Soc. méd. d’hôp. de Par., 1917, v. 33, pp. 424-430.
Claude et Chauvet. Sémiologie réelle des sections totales des nerfs mixtes périphériques. Paris, 1901.
Claude, H., Dide, M., et Lejonne, P. Psychoses hystéro-émotives de la guerre. Paris méd., 1916, v. 21, pp. 181-185.
Claude, Henri, et Lhermitte, J. Étude clinique et anatomo-pathologique de la commotion médullaire directe par projectiles de guerre. Ann. de méd., Par., 1914-15, v. 2, pp. 479-506.
Claude, Henri, et Lhermitte, J. Le tétanos fruste à évolution lente et incubation prolongée. Étude des réactions électriques. Presse méd., 1915, 14 oct., p. 406.
Claude, Henri, et Lhermitte, J. Les réflexes tendineux et cutanés, les mouvements de défense et d’automatisme dans la section totale de la moelle d’après une observation anatomo-clinique. Ann. de méd., Par., 1916, v. 3, pp. 407-430.
Claude, Henri, et Lhermitte, J. Les paraplégies cérébello-spasmodiques et ataxo-cérébello-spasmodiques consécutives aux lésions bilatérales des lobules paracentraux par projectiles de guerre. Soc. méd. d’hôp. de Par., 1916, 26 mai.
Claude, Henri, et Lhermitte, J. La glycosurie dans les lésions traumatiques du cerveau. Soc. méd. d. hôp. de Par., 1916, 26 mai.
Claude, Henri, et Lhermitte, J. Les contractures du tétanos tardif à évolution prolongée et leur diagnostic avec les contractures organiques ou “fonctionnelles.” Progrès méd., Par., 1916, pp. 185-187.
Claude, Henri, et Lhermitte, J. Troubles médullaires dans les commotions directes mais à distance de la colonne vertébrale. Paris méd., 1917, No. 27, pp. 11-14.
Claude, H., et Lhermitte, J. Formes cliniques de la commotion de la moelle cervicale par projectiles de guerre. Rev. de méd. Par., 1916, 35, 535-554.
Claude, Henri, et Lhermitte, J. Le syndrome infundibulaire dans un cas de tumeur du troisième ventricule. Presse méd., Par., 1917, v. 25, pp. 417-418.
Claude, H., et Lhermitte, J. Les modifications dynamogéniques des centres nerveux inférieurs dans les paralysies ou dans les contractures fonctionnels. Presse méd., 1918, No. 1.
Claude, Henri, et Porak, R. De la décalcification osseuse dans les paralysies des membres organiques ou névropathiques. Paris méd., 1915, v. 17 (part. méd.), pp. 321-328.
Claude, Henri, et Porak, R. Les troubles de la motilité dans les psychonévroses du type hystérique. Progrès méd., Par., 1914-15, v. 23, p. 486 and p. 512. Rev. Paris méd., 1915, v. 17 (part. méd.), p. 540.
Claude, Henri, et Lhermitte, J. et Loyes, Mlle. M. Étude histologique d’un cas de commotion médullaire par éclatement d’obus. Bull. et mém. Soc. méd. d’hôp. de Par., 1915, v. 39, pp. 680-687.
Claude, Henri, Lhermitte, J., et Vigouroux, A. Délire mystique chez un blessé de l’encéphale. Ann. méd.-psychol., Par., 1917, v. 73, pp. 560-568.
Claude, Henri, Loyes, Mlle. M., et Lhermitte, J. Étude clinique et anatomique de la commotion médullaire par éclatement d’obus. Rev. Paris Méd., 1915, v. 17 (part. méd.), p. 370.
Claude, Vigouroux, et Dumas. Étude anatomique de cent cas de lésions traumatiques des nerfs des membres. Presse Méd., March 4, 1915.
Clerici, A. Disturbi psichici nei soldati combattenti. Riv. di. psicol. applic., Bologna, 1915, v. 11, pp. 112-117.
Clinical aspects of hemilesions of the cord. N. Y. Med. Jour., 1917, cvi, 1189.
Clunet, Jean. Les effets immédiats de l’émotion sur le système nerveux, en dehors de toute commotion. Rev. neurol., Par., 1917, v. 24, pp. 48-51.
Cluzet. Paralysie du plexus brachial avec troubles trophiques de la main, sans blessure ni contusion apparente, provoquée par l’explosion d’un obus. Lyon méd., 1916, v. 125, p. 20.
Cohn, Toby. (Discussing Lewandowsky)—“Kriegsverletzungen des Nervensystems.” Deutsche med. Wchnschr., Berl. u. Leipz., 1915, v. 41, p. 89 and p. 149.
Cohn, Toby. Zur Frage der psychogenen Komponente bei Motilitätdefekten infolge von Schussverletzungen. Neurol. Zbl., Leipz., 1916, v. 35, No. 6.
Cohn, Toby, Kron, H., and Hansemann, etc. Ueber Kriegsverletzungen des Nervensystems. Discussion before Referat of Lewandowsky. Berl. klin. Wchnschr., 1915, v. 521, pp. 88-91.
Colella, R. Arteriosclerosi e neurosi posttraumatiche. Gazz. med. sicil. Catania, 1916, xix, 121-128.
Colin, H. De l’envoi en congé de convalescence des alienés militaires guéris et fortunés en cas de refus du certificat d’hébergement. Soc. de méd. lég. de France, Bull., Par., 1916, v. 13, pp. 136-146.
Colin, H. et Lautier, J. De la valeur émotionnelle des maladies vénériennes dans l’étiologie et l’évolution des psychoses. Ann. méd.-psychol., Par., 1917, v. 73, pp. 357-373.
Colin, H., Lautier, et Magnac. Les imbéciles à l’armée. Ann. méd.-psychol., Par., 1916-17, v. 7, pp. 540-546.
Collie, Sir John. Fraudulent and neurasthenic cases. Tr. Med.-Leg. Soc., Lond., 1914-15, v. 12, pp. 25-67.
Collie, Sir John. Fraudulent and neurasthenic cases. J. Roy. Army Med. Corps, Lond., 1915, v. 24, pp. 653-682; also Practitioner, Lond., 1915, v. 44, pp. 653-682.
Collie, Sir John. Fraud and skin eruptions. Lancet, Lond., 1916, ii, pp. 1007-1010.
Collie, Sir John. Neurasthenia; what it costs the State. J. Roy. Army Med. Corps, Lond., 1916, v. 26, pp. 525-544.
Collie, Sir John. Tests for simulated defective vision or for blindness of one eye. J. Roy. Army Med. Corps, Lond., 1916, v. 26, pp. 800-812.
Collie, Sir John. Jaundice and malingering. Birmingh. M. Rev., 1916, v. 80, pp. 93-94.
Collie, Sir John. Malingering: examination of the upper extremities. J. Roy. Army Med. Corps, Lond., 1916, v. 27, pp. 85-91.
Collie, Sir John. Malingering and feigned sickness. 2nd. ed., 1917.
Collie, Sir John. La simulazione dei dolori di schiena. Gazz. med. lomb., Milano, 1917, xxiv, 129-132.
Collie, Sir John. Treatment by physical methods of mental disabilities induced by the war. Proc. Roy. Soc. Med., Lond., 1917-18 (sect. Balneol.), v. 10, pp. 21-24.
Collie, Sir John. The management of neurasthenia and allied disorders contracted in the Army. With report of remarks made by Lt. Col. Aldren Turner. “Recalled to Life,” 1917, Sept., No. 2, pp. 234-250.
Collier, James. Shell shock without visible signs of injury. Proc. Roy. Soc. Med., 1915-16, v. 9 (sect. Psychiat.), pp. 34-35.
Collier, James. Gunshot wounds and injuries of the spinal cord. Lancet, Lond., 1916, i, pp. 711-716. Also Tr. M. Soc., Lond., 1915-16, v. 39, pp. 227-256.
Collins, J. and Craig, C. B. Injuries to spinal cord produced by modern warfare. J. Nerv. and Ment. Dis., N. Y., 1916, v. 44, pp. 527-528.
Colmers, F. Ueber Schädelschüsse. Deutsche med. Wchnschr., 1917, 43, 741.
Cololian. La mécanothérapie de guerre avec les appareils de fortune. Arch. de méd. et pharm. mil., Par., 1914-15, v. 64, pp. 155-176; also pp. 658-695.
Commotion des centres nerveux par explosion. Lyon méd., 1916, v. 125, pp. 181-182.
Commotionnés vrais. Caducée, Par., 1916, v. 16, p. 172.
Condorelli-Francaviglia, M. Congiuntivite catarrhale acuta in un militare, provocata mediante l’uso di semi di ricino. Policlin., Roma, 1917, xxiv, sez. prat., 735-739.
Conférence interalliée pour l’étude de la rééducation professionelle et des questions qui intéressent les invalides de la guerre. Grand-Palais, Paris, May 8-12, 1917. Proc. Roy. Soc. Méd., Lond., 1917-1918 (Sect. Balneul. and Climatol.), v. 10, pp. 81-95.
Cone, S. M. Pathological findings in nerves in following war injuries; preliminary report. Brit. Med. Jour., 1917, ii, 615.
Cone, Sydney M. Some of the results of work on the pathology of peripheral nerve injuries. Amer. Jour. Orthop. Surg., 1918, xvi, 319.
Cone, Sydney M. Surgical pathology of the peripheral nerves. Brit. Jour. of Surg., 1918, vi, 524.
Congrès interallié de rééducation des mutilés. Presse méd. Par., 1917, v. 25, pp. 301-303.
Consiglio, P. Studii di psichiatria militare. Riv. sper. di freniat., Reggio-Emilia, 1912, v. 38, p. 370; 1913, v. 39, p. 792; 1914, v. 40, p. 881; 1915, v. 41, p. 35.
Consiglio, P. Delle psicosi e delle nevrosi e specialmente della criminalità in guerra. Ann. di med., nav., Roma, 1915, ii, pp. 408-417.
Consiglio, P. Psicosi, nevrosi e criminalita nell’ ambiente militare in tempo di pace. Ann. di med., nav., Roma, 1915, ii, pp. 418-422.
Consiglio, P. Nevrosi e psicosi in guerra. (Nota 2) Gior. di med. mil., Roma, 1915, v. 63, pp. 665-703.
Consiglio, P. Studien über Militär-psychiatrie und Kriminologie. Ztschr. f. d. Ges. Neurol. u. Psychiat., Berl. u. Leipz., 1915, v. 128, pp. 384-444.
Consiglio, P. Psicosi nevrosi e criminalita nei militari in guerra. Arch. di antrop. crim., etc., Torino, 1916, v. 8, pp. 258-268.
Consiglio, P. L’Anomalie de carattere dei militari in guerra. Riv. sper. di freniat., Reggio-Emilia, 1916, v. 42, pp. 131-172.
Consiglio, P. Disturbi nervosi e mentale nei militari in guerre. Gior. di méd. mil., 1917, v. 65, pp. 607-616.
Cooper, George. Contractures and allied disorders: their cause and treatment. Brit. M. J., Lond., 1917, i, pp. 109-114.
Cooper, P. R. (Discussion of Milligan’s paper.) Brit. M. J., Lond., 1916, ii, p. 73; also p. 201.
Cooper, J. W. A. Use of alcohol on the battlefield and elsewhere. Lancet, Lon., 1914, ii, 1168.
Cooper, P. R. Treatment of “shell shock,” Brit. M. J., Lond., 1916, ii, 201.
Cordier, Charles Albert. Les états psychasthéniques frustes et la guerre. Thèse de Lyon, 1916. Rev. neurol., Par., 1917, v. 22, p. 471.
Core, Donald E. The “Instinct-distortion,” or “war neurosis.” Bos. M. and S. J., 1918, clxxix, 448.
Core, Donald E. “Instinct-distortion,” or “war-neurosis.” Lancet, Lon., 1918, ii, 168.
Cornet. L’auto-mutilation. Rev. gén. de clin. et de thérap., Par., 1915, v. 29, pp. 649-653; and pp. 683-686.
Costello, C. A. Principal defects found in persons examined for service in the United States Navy. Amer. Jour. Pub. Health, 1917, vii, 489.
Cottet, J. Troubles objectifs de la sensibilité cutanée dans les gelures des pieds: l’acrotrophodynie paresthésique des tranchées. Paris méd., 1917, No. 11, pp. 222-27.
Cottet, J. Syndrome d’aéro-paresthésie a frigore et gelures des pieds. Presse méd., Par., 1917, v. 25, pp. 517-518.
Courtois, Suffit M. et Giroux, R. Les formes anormales du tétanos. 1916, Paris, Masson et Cie.
Craig, C. B. Injuries to the peripheral nerves produced by modern warfare. Am. Jour. Med. Jour., 1916, clii, 368.
Craig, Maurice. Psychological medicine. 1917, 3rd ed., Blakiston, pp. 300-311.
Crile, G. W. The Kinetic Drive. W. B. Saunders, 1916.
Crile, G. W. A mechanistic view of war and peace. Macmillan, 1916.
Crile, G. W. Man: An adaptive mechanism. Macmillan, 1916.
Crile, G. W. Notes on Base Hospital No. 4, U. S. A., on Active Service. J. Am. M. Asso., Chicago, 1917, v. lxix, p. 206.
Crile, G. W. The Fallacy of the German State Philosophy. Doubleday, Page, 1918.
Crinon, J. Les éclopés psychiques. (Méd. légale.) Caducée, Par., 1916, v. 16, pp. 115-116.
Crinon, J. Les centres psychiatriques de l’avant. Progrès méd., Par., 1917, v. 43, pp. 364-365.
Cristiani, A. Note practiche (psichiatriche militari). Riv. ital. di neuropat. (etc.), Catania, 1917. x 265-272.
Crouzon, O. Cécité temporaire provoquée par l’éclatement d’obus à proximité. Bull. et mém. soc. d’hôp. de Par., 1915, v. 39.
Crouzon, O. Les pseudo-maux de Pott au conseil de révision. La spondylite traumatique. Bull. et mém. soc. méd. de Par., 1915, v. 39, pp. 111-113.
Crouzon, O. Hémorrhagies naso-pharyngiennes profuse et répétées après commotion par éclatement d’obus chez un sujet atteint d’hypertension artérielle. Bull. et mém. Soc. méd. d’hôp. de Par., 1916, 3. s. xl, 1376-1378.
Crouzon, O. De la valeur de l’hypotension artérielle comme signe objectif de la psychasthénie. Bull. et mém. soc. méd. d’hôp. de Par., 1915, v. 39, pp. 234-237.
Cruchet, R. Calmettes et Bertrand. Épilepsie Jacksonienne grave. Trépanation et application de sac herniaire. Cessation des crises. Disparition des troubles subjectifs. Rev. neurol., Par., 1917, v. 24, pp. 510-511.
Cruchet, R. Calmettes et Bertrand. Fracture du crâne méconnue. Commotion cérébrale. Crises d’hystéro-epilepsie avec état obsenant. Trépanation tardive. Guérison. Rev. neurol., Par., 1917, v. 24, pp. 511-513.
Culpin, M. Practical hints on functional disorders. Brit. M. J., Lond., ii, pp. 548-549.
Cumberbatch, E. P. A criticism on the reaction testing of muscles and the interpretation of the results with reference to electrical examination of nerve injury in war. Proc. Roy. Soc. Med., Lond., 1915-16, v. 9 (Electro.-therap. sect.), pp. 23-38.
Curschmann. Bemerkungen zur Behandlung hysterischer Stimmstörungen. München med. Wohnschr., 1916, v. 63, pp. 1644-1645.
Cutler, E. C. Neurological surgery in a war hospital. Boston M. and S. J., 1916, v. 174, pp. 305-309.
Cygielstrejch, Adam. La psychologie de la panique pendant le guerre. Ann. med.-psychol., Par., 1916-17, v. 7, pp. 172-192.
D’Abundo, G. Alterazioni nel sistema nervoso centrale consecutive a particolari commozioni traumatiche. Riv. ital. di neuropat., Catania, 1916, v. 9, pp. 145-171.
D’Abundo, G. Considerazioni cliniche sui traumi di guerra a capo. Riv. ital. di neuropat. psichiatr., ed elettroter., 1917, v. 10, 357-76.
D’Abundo, G. Reparto neuropatologico militarizzato della clinica delle malattie nervose e mentale della R. Universita di Catania. Riv. ital. di neuropat., Catania, 1917, v. 10, pp. 22-24.
Dacco, E. Autolesioni cutanee nei militari. Gior. ital. d. mal. ven., Milano, 1917, lii, 340, 370.
Dal Collo, M. E. Contributo casuistico alle dermatosi simulate di guerra. Quaderni di med. leg., Milano, 1917, i, 24-29.
Damaye, H. Organisation et fonctionnement d’un service de neuropsychiatrie, d’armée. Presse méd., Par., 1916, v. 24, p. 24.
Damaye, H. Étude sur les affections mentales et neuropathiques occasionnées par les commotions de la guerre. Progrès méd., Par., 1917, 3. s., xxxii, 441-443.
Damaye, H. Organisation des centres psychiatriques. Caducée, Par., 1917, v. 126, p. 147.
Damaye, H. Considérations cliniques sur les commotions de la guerre. Progrès méd., Par., 1917, 3. s., xxxii, 332-334.
Damaye, H. Aperçu général sur les fonctions d’un service de psychiatrie d’armée. Progrès méd., Par., 1917, v. 43, pp. 362-364.
Dames de la Croix-Rouge et la simulation. Caducée, Par., 1916, v. 16, p. 94.
Darkshevich, L. O. (Nomenclature of disturbances in the region of the nervous system, following traumatism.) Russk. Vrach., Petrogr., 1916, v. 15, p. 97.
Daude. Contribution a l’étude de la psychopathologie de guerre. Fonctionnement d’un centre psychiatrique de l’avant. Thèse de Bordeaux, 1916.
Daussant. L’assistance aux invalides et mutilés de la guerre (appareillage, rééducation professionelle, placement). Arch. de méd. et pharm. mil., Par., 1916, v. 65, pp. 733-759.
Davidenkoff, S. N. (Acute psychoses in time of war.) Psikhiat. Gaz., Petrogr., 1915, v. 2, pp. 321-325.
Davidenkoff, S. N. (Dysarthria and mutism following wind contusions.) Psikhiat. Gaz., Petrogr., 1916, v. 3, pp. 190-194.
Davidenkoff, S. N. Acute traumatic psychoses; retroanterograde amnesia after traumatism of the skull. Ibid., 341-347.
Davidenkoff, S. N. (Case of hysterical psychosis developed during battle.) Psikhiat. Gaz., Petrogr., 1916, v. 3, pp. 211-213.
Davidenkoff, S. N. (Nature of speech disturbances in the contused.) Sovrem. Psikhiat., Mosk., 1916, v. 10, pp. 292-373.
Davidson, J. M. and Lockhart-Mummery, P. Fragment of shell embedded in the internal popliteal nerve: illustrating the value of accurate localization. Lancet, Lon., 1917, i, 719.
Dawson, G. H. A case of shell concussion: treatment by general anaesthesia. Lancet, Lond., 1916, i, p. 463.
De Boer, J. Desertie en vagabondage. Mill.-geneesk. Tijdschr., Haarlem, 1917, v. 21, pp. 149-167.
De Brun, H. L’amnésie paludienne, Presse méd., Par., 1917, v. 25, pp. 625-627.
Dedor, V. P. (Skull-brain wounds, according to the data of the evacuational hospital No. 88.) Russk. Vrach., Petrogr., 1917, v. 17, pp. 429-431, and pp. 450-454.
DeFleury, Maurice. Un moyen de délassement pour les troupes en marche. Bull. de Acad, de méd., Par., 1914, v. 72, pp. 442-443.
Dejerine, J. Deux cas de paraplégie fonctionnelle d’origine émotive observée chez des militaires. Rev. neurol., Paris, 1915.
Dejerine, J. Sur l’abolition de réflexe cutané plantaire dans certains cas de paralysies fonctionnelles, accompagnées d’anesthésie (hystéro-traumatisme). Rev. neurol., Paris, 1914-15, v. 221, pp. 521-529.
Dejerine, J. Deux cas de paralysie fonctionnelle d’origine émotive observés chez les militaires. Rev. neurol., Par., 1914-15, v. 222, pp. 421-424.
Dejerine et Gascuel. Tachycardie d’origine émotive permanente. Rev. neurol., Par., 1914-15, v. 222, pp. 211-214.
Dejerine, J. et Gauckler, E. Le traitement par l’isolement et la psychothérapie des militaires atteints de troubles fonctionnels du système nerveux. Presse méd., Par., 1915, v. 23, pp. 521-522.
Dejerine, Marie, Babinski, Claude, Léri, Sollier, Sicard. Travaux des centres neurologiques. Rev. neurol., Par., 1915, p. 1136.
Dejerine et Mouzon. Deux cas de syndrôme sensitif cortical. Rev. neurol., Par., 1914-15, v. 222, p. 388.
Dejerine et Mouzon. Les lésions des gros troncs nerveux par projectiles de guerre. Les différents syndrômes cliniques et les indications opératoires, Presse méd., May 10, July 8, Aug. 30, 1915.
Dejerine et Mouzon. Un nouveau type de syndrôme sensitif cortical dans un cas de monoplégie corticale dissociée. Rev. neurol., Par., 1914-15, v. 222, pp. 1265-1273.
Dejerine et Mouzon. Le diagnostic de l’interruption complète des gros troncs nerveux de membres. Presse méd., Par., 1916, v. 24, pp. 97-101.
Dejerine, M. and Mme. and Mouzon. Troubles trophiques articulaires analogues à ceux du rhumatisme subaigu et semblant consécutif à un tiraillement des racines des plexus brachiaux chez un soldat atteint de paraplégie traumatique. Rev. neurol., Paris, 1915.
Dejerine et Schwartz. Déformations articulaires analogues à celles du rhumatisme chronique, avec troubles trophiques, cutanées et hyperidrose relevant d’une lésion irritative du nerf médian. Rev. neurol., Paris, 1915.
De la Motte. Demonstration zweier forensischer Fälle. Neurol. Centralbl., Leipz., 1915, v. 34, pp. 590-591.
De Lapersonne. La rééducation des aveugles de guerre. Presse méd., Par., 1917, v. 25, p. 309.
Del Greco, Francesco. Gli ansioso emotivi. Riv. ital. di neuropat. (Psichiat. ed elettro.) Catania, 1917, v. 10, pp. 169-183.
Delherm, L. Note sur les contractures et les paralysies traumatiques d’ordre réflexe. J. de radiol. et d’électrol., Par., 1916, v. 2, pp. 292-300.
Delherm, L. Le traitement des phénomènes hystériques par la rééducation intensive d’après Cl. Vincent. J. de radiol. et d’électrol., Par., 1917, v. 2, pp. 531-532.
Delherm and Py. De l’importance de bien différencier les manifestations organiques et les manifestations psychiques chez les blessés de guerre. J. de radiol. d’électrol., Par., 1914-15, i, 625-628.
Delinquent children and the war. Brit. M. J., Lond., 1917, i, p. 231.
Délire raisonnant d’invention. Ann. méd.-psychol., Par., 1917, v. 73, pp. 589-594.
De Lisi, L. Ricerche sperimentali sulle alterazioni nervose centrali degli annuali sottoposti a commozione cerebrale. Riv. sper. di freniat., Reggio-Emilia, 1915, v. 41, pp. 249-312.
Delorme, Edmond. Sur la fréquence des troubles des organes des sens, et en particulier de la vision, dans les blessures de la tête par les projectiles. Bull. Acad, de méd., Par., 1915, v. 73, p. 397.
DeMartel, T. Blessures du crâne. Collection Horizon, Masson et Cie, Paris, 1917.
De Massary, E., et Du Souich, P. Syndrôme choréiforme hystérique et paralysie générale incipiens. Rev. neurol., Par., 1917, v. 24, pp. 219-221.
De Massary, E., et Tockmann. Un cas de paludisme avec réaction meningée violente simulant la méningite cérébrospinale. Bull. et mem. Soc. méd. d’hôp. de Paris, 1917, 3 ser. 41, 1195-9.
Deny, G. La neuropsychopathologie française pendant une année de guerre (août 1914-août 1915). Encéphale, Par., 1914-15, ii, pp. 153-174.
Deny, G. Sur trois cas d’hystéro-traumatisme (monoplégie brachiale, contracture dorso-lumbaire, météorisme). Rev. neurol., Par., 1914-15, v. 221, pp. 559-560.
De Paeuw, Leon. The Vocational Reëducation of Maimed Soldiers. Princeton Univ. Press, 1918.
De Parrel, G. Surdité de guerre et méthode orale. Rev. de laryngol., etc., Par., 1911, v. 1, pp. 401-425.
De Sanctis, S. L’isterismo di guerra. Riv. ospedal., Roma., 1917, vii, 405-409.
De Sandro, D. Il mutismo funzionale da scoppo di granata e quello degli isterici; loro cura con l’eterizzazione. Riv. di patol. nerv., Firenze, 1917, v. 22, pp. 9-31.
Deschamps, Albert. Un symptôme fonctionnel de la fatigue. L’inversion de la sensation de fatigue. Rev. gén. de clin. et de thérap., Par., 1916, v. 30, pp. 262-264.
Déserteur ambulatoire. Ann. méd. psychol., Par., 1914-15, p. 527.
Descoust, Paul. Attitudes vicieuses du pied d’origine névropathique dans les traumatismes du membre inférieur. Presse méd., Par., 1917, v. 25, pp. 330-331.
Desplates, R., and Buquet, A. Oblitération des artères des membres et troubles circulatoires des nerfs. L’ischémie nerveuse des blessés de guerre. Rev. de méd., Par., 1916, 25, 578-619 (Published in February, 1918).
Dessoir, M. Kriegspsychologische Betrachtungen. Leipz., 1916, S. Hirzel, 47 p. 8o.
De Tarnowsky, George. Military Surgery of the Advanced Zone. No. 7, Medical Manual War Series. Lea and Febiger.
Detecting the pretense of deafness; tests adopted in France to reveal the tricks of slackers. Scient. Am. Suppl., N. Y., 1917, lxxxiii, 372.
Devaux et Logue. Les délires guerriers dans la fièvre typhoide. Presse méd., Par., 1915, v. 23, pp. 363-364.
Devaux et Logue. Les anxieux. 1917, Paris, Masson et Cie., pp. 283-300.
Dide, W. et Lhermitte, J. La diplégie brachiale spasmodique consécutive aux blessures par coup de feu de la région cervicale. Progrès méd., Par., 1917, No. 1, pp. 1-3.
Diederich-Schwalbe. Discussion, Everth, E. Von der Stelle des Soldats im Felde. Rev. in Deutsche med. Wchnschr., Berl. u. Leipz., 1915, v. 412, p. 1351.
Die behauptete Zunahme geistiger Erkrankungen bei Beginn des Krieges in der Zivilvölkerung Deutschlands. Psychiat.-neurol. Wchnschr., Halle a. S., 1915-16, v. 17, No. 29-30, 131-132.
Di Pietro, S. Pneumotorace curativo o pneumotorace practicato a scopo di simulazione per esenzione dal servisio militare. Ann. di clin. med., Palermo, 1916, vii, 43-63.
Discussion of Functional Cases. Proc. Roy. Soc. Med. Lond., 1914-15, v. 8, (sect. laryngol.), pp. 117-120.
Discussion on Shell Shock. Lancet, Lond., 1916, i, p. 306.
Discussion on the treatment by physical methods of mental disabilities induced by the war. Proc. Roy. Soc. Med., Lond., 1917-18, v. 10 (sect. Balneol.), pp. 1-44.
Discussion sur les troubles nerveux dits fonctionnels observés pendant la guerre. Rev. neurol., Par., 1914, xxii, 447-452.
Disordered action of the heart among soldiers. Jour. Lab. and Clin. Med., 1917, iii, 134.
Disqué. Behandlung der Kriegsneurosen durch Hypnose, Wachsuggestion und suggestive elektrische Anwendungen. Therapie der Gegenwart, May, 1918.
Dölger, R. Hysterische Erkrankungen des inneren Ohres neben allgem. Hysterie nach Granatenschlag u. Verschüssung. Münch. med. Wchnschr., nr. 16, 1918.
D’Oelsnitz. L’adaptation organique des territoriaux à la guerre actuelle. Bull. et mém. soc. méd. d’hôp. de Par., 1915-16, v. 40, pp. 1935-44.
D’Oelsnitz, M. et Boisseau, J. Note sur les résultats des recherches oscillo-métriques pratiquées dans 100 cas de mains figées et 27 cas de pieds bots psychonévrosiques. Bull. et mém. soc. méd. d’hôp. de Par., 1917, v. 33, pp. 1147-1149.
Donald-Smith, Helen. War distress and war help; short catalogue of the leading war help societies. Lond. 1917, John Murray, 38 p. 16o.
Donath, J. Beiträge zu den Kriegsverletzungen und Erkrankungen des Nervensystems. Wien. klin. Wchnschr., 1915, v. 28, pp. 725-730, and pp. 763-766.
Donath, J. Schwere Polyneuritis rheumatica der Plexus brachiales bei einem Kriegsteilnehmer. Wien. klin. Wchnschr., Nr. 41, S. 1291.
Droiin. Plaie du crâne par éclat d’obus. Epilepsie Jacksonnienne et hémiparésie. Cranioplastie par transplant cartilagineux. Résultats. Jour. de méd. de Bordeaux, 1915-16, v. 45, pp. 241-242.
Drouot, E. Pour les sourds de la guerre; rééducation auditive, lecture sur les lèvres, orthophonie. Rev. scient., Par., 1915, i, pp. 363-367.
Drug Habit and Mobilization in France. Lancet, Lond., 1915, i, p. 161.
Dub. Heilung psychogenen Taubheit und Stummheit. Deutsche med. Wchnschr., Berl. u. Leipz., 1916, No. 52, pp. 1601-1602.
Dubois, Laumonier, Bouquet, Fiessinger, Pardel. Sur l’angoisse de guerre. Bull. gén. de thérap., Par., 1915-16, v. 168, pp. 821-828.
Duco, A. and Blum, E. Guide pratique du médecin dans les expertises médico-légales militaires. Collection Horizon, Masson et Cie, Paris, 1917.
Ducoste. Les contractures dans les lésions nerveuses périphériques. Compt. rend. Soc. de biol., Par., 1915, No. 14, p. 435.
Ducroquet. L’ankylose tibio-tarsienne et les troubles fonctionnels consécutifs. Presse méd., Par., 1917, v. 25, pp. 561-564.
Ducroquet. Les troubles fonctionnels dans les raideurs et les ankyloses douloureuses de l’articulation tibio-tarsienne. Presse méd., Par., 1917, v. 25, pp. 597-599.
Dufour, Henri. De l’origine infectieuse de certaines hémiplégies par hémorrhagie et ramollissement cérébral. Rev. neurol., Par., 1917, v. 24, pp. 505-507.
Dufour, Henri, et Livy. Neurasthénie avec troubles de la nutrition décelée par l’examen du sang. Presse méd., Par., 1917, v. 25, p. 323.
Duken, John. Ueber zwei Fälle von intrakranieller Pneumatocele nach Schussverletzung. Münch. med. Wchnschr., 1915, v. 621, pp. 598-599.
Dumas. Sur les accidents nerveux determinés par la déflagration de fortes charges d’explosifs. Rev. neurol., Par., 1916, v. 29, pp. 593-595.
Dumas, R. Libération des nerfs et recupération fonctionnelle. Bulletins et Memoires de la Soc. de chirurgie de Paris, Feb. 8, 1916.
Dumas, G. et Aimé, H. Les troubles mentaux et nerveux dans les armées Austro-Allemandes. J. de psychol. norm. et path., Par., 1915, v. 2, pp. 329-347.
Dumas, G. and Delmas. Les confusions mentales d’origine commotionnelle chez les blessés. Arch. de méd. et pharm. mil., Par., 1917, lxvii, 69-77.
Dumesnil, Marius A. Délires de guerre. Thèses de Paris, 1915-16, v. 5, No. 62.
Dumesnil, Marius A. Délires de guerre. (Review.) Ann. d’hyg., Par., 1916, v. 26, p. 183.
Dumolard, Rebierre et Quellien. Inhibition, variabilité, instabilité des réflexes tendineux. Rev. neurol., Par., 1916, v. 23, pp. 139-142.
Dumolard, Rebierre et Quellien. Réflexes tendineux variables. Seule manifestation clinique objective d’un état asthénique grave. Paris méd., 1916, v. 21 (part. méd.), pp. 286-288.
Dumoz, A. G. The simulation of disease; drugs, chemicals, and septic materials used therefor. Pub. Health Rep., Wash., 1917, xxxii, 1887-1892.
Dunlap, Knight. Psychologic observations and methods. Jour. A. M. A., 1918, lxxi, 1392.
Dunn, Naughton. Treatment of lesions of the musculo-spiral nerve in military surgery. Amer. Jour. Orthop. Surg., 1918, xvi, 258.
Duplant, A. G. Blessure du crâne datant de vingt mois. Abcès du cerveau à méningocoques. Meningite cérébrospinale. Presse méd., Par., v. 24, p. 366.
Dupont, J. et Troisier, Jean. Plaie perforante du crâne dans la région occipitale. Polyurie, dysphagie, tachycardie et zona cervical. Guérison. Bull. et mém. Soc. méd. d’hôp. de Par., 1915, v. 39, pp. 21-28.
Dupouy, Roger. Notes statistiques et cliniques sur les troubles neuro-psychiques dans l’armée en temps de guerre. Ann. méd.-psychol., Par., 1914-15, v. 6, pp. 444-451.
Dupouy, R. Note sur les commotions cérébro-médullaires par l’explosion d’obus sans blessure extérieure. Bull. et mém. Soc. méd. d’hôp. de Par., 1915, v. 39, pp. 926-930.
Dupouy, R. Commotion cérébro-médullaire par éclatement rapproché. Presse méd., Par., 1916, v. 24, p. 52.
Dupouy et Bosc. Troubles cérébro-médullaires par explosion de mine. Presse méd., Par., 1915, v. 23, p. 330.
Duprat, G. L. La psychothérapie en temps de guerre. Progrès méd., Par., 1917, No. 13, also No. 15, pp. 123-125.
Duprat, G. L. Rôle des complexus idéo-affectifs et de l’onirisme dans les syndrômes émotionnels. Progrès méd., Par., 1917, v. 43, pp. 357-360.
Dupré. The emotions and the war. War Med., 1918, ii, 31.
Dupré, E. Recherches sur les symptômes homolatéraux dans les perforations du crâne et de l’encéphale par projectiles de guerre. Presse méd., Par., 1916, v. 24, p. 174.
Dupré, E. Réformes, incapacités, gratifications dans les états psychopathiques de guerre. Rev. neurol., Par., 1916, v. 23, pp. 790-799.
Dupré, E. Discussion de la conduite à tenir vis-à-vis des blessures du crâne—par P. Marie. Rev. neurol., Par., 1916, v. 29, p. 471.
Dupré et Grimbert. La psychonévrose émotive constitutionelle et acquise. Rev. neurol., Par., 1917, v. 24, pp. 45-48.
Dupré, E., et LeFur. Paraplégie spasmodique par traumatisme du vertex. Rev. neurol., Par., 1914-15, v. 222, p. 406.
Dupré et Rist. Hémiplégie hystérique chez un cuirassier. Rev. neurol., Par., 1914-15, v. 22, p. 200.
DuRoselle et Oberthür. Sur les accidents nerveux déterminés par la déflagration de fortes charges d’explosifs. Rev. neurol., Par., 1916, v. 23, pp. 598-605.
Duroux, E. and Couvreur, E. Résultats éloignés expérimentaux et cliniques des sutures nerveuses. Rev. de Chir., 1917, liii, 401.
Dutheillet De Lamothe, G. Étude sur les troubles laryngés moteurs dans le paludisme. Thèses de Paris, 1916-17, Nr. 87.
Dutton, A. S. Beards in warfare. Med. Press and Circ., Lond., 1915, v. 100, p. 520.
Duvernay, L. Contractures post-traumatiques en chirurgie de guerre. Paris méd., 1915, v. 17 (part. méd.), pp. 429-437.
Dyakonoff, P. P. (Cases of self-inflicted injury to avoid military service.) Vestnik Obshtsh. Hig., Sudeb. i Prakt. Med., Petrogr., 1916, v. 52, pp. 1080-1082.
Eager, E. War psychoses occurring in cases with a definite history of shell shock. Brit. Med. Jour., 1918, i, 422.
Ebel, S. Einige Bemerkungen über physikalische Therapie der Kriegskrankheiten. Ztschr. f. Phys. u. Diätet. Therapie, Leipzig. 1915, v. 19, pp. 182-190.
Ebers, E. M. Functional Reëducation and Vocational Training of Soldiers disabled in War. Canad. M. Ass. J., 1917, No. 3, pp. 193-200.
Edel. Psycho-analytische Behandlung der Hysterie im Lazarett. Psychiat.-neurol. Wchnschr., Halle a. S., 1916, v. 17, No. 2. Rev. Aerztl. Rundschau, München, 1916, v. 26, pp. 128-130.
Edel, K. Krieg und Geisteskranken. Neurol. Centralbl., Leipz., 1915, v. 34, pp. 590.
Edel, M. Neurosen und Psychosen. Deutsche med. Wchnschr., 1915, v. 411, p. 30.
Eder, M. D. The psychopathology of the war neuroses, Lancet, Lond., 1916; ii, pp. 264-268.
Eder, M. D. War Shock. Philadelphia, Blakiston Son & Co. and Wm. Heinemann, 1917.
Effects of high explosives. Jour. A. M. A., 1917, lxviii, 1182.
Effect (The) of the war upon psychiatry in England. Lancet, Lond., 1917, ii, 352.
Ehrmann. Notiz über die Herztätigkeit während Granatfeuers. Ztschr. f. Phys. u. Diätet. Therap., Leipz., 1915, v. 19, p. 52.
Elliott, T. R. Transient paraplegia from shell explosions. Brit. M. J., Lond., 1914, ii, pp. 1005-1006.
Emerson, E. B. Mental states responsible for malingering. Med. Press, Lond., 1917, n. s., civ, 433-436.
Emslie, Isabel. The war and psychiatry. Edinb. M. J., 1915, v. 14, p. 359.
Engelen. Beurteilung der Persuasion (Unter Bezugnahme auf die Kriegsneurosen und Unfallsneurosen). Aerztl. sachv. Ztg., Berl., 1915, v. 2, pp. 157-163, and pp. 171-175.
Engelen and Rangette. Nachweis von Simulation durch das Assoziations-Experiment. Aerztl. Sachverst.-Ztg., Berl., 1916, v. 22, pp. 37-40.
Epstein, L. (The war and psychoses.) Gyógyászat, Budapest, 1915, v. 55, pp. 40-43.
Erben, S. Ueber die motorischen Reizerscheinungen bei Kriegsteilnehmern. Wien. klin. Wchnschr., 1916, v. 29, pp. 1129-1134.
Erving, William G. Orthopedic treatment of nerve lesions. Amer. Jour. Orth. Surg., 1918, xvi, 346.
Escat, E. Epreuve des diapasons unisonnants appliquée, au diagnostic de la surdité unilatérale simulée. Presse Méd., Par., 1916, v. 24, pp. 562-563.
Eschbach, H. et Lacaze, H. Méningite cérébrospinale débutant par des troubles mentaux. Bull. et mém. Soc. Méd. d’Hôp. de Par., 1915, v. 39, pp. 1024-1029.
Estève. La nostalgie des militaires. Gaz. méd. de Par., 1916, v. 87, pp. 122-123.
États anxieux. Rev. gén. de clin. et de thérap., Par., 1916, v. 30, pp. 89-90.
Eugène, V. Paralysie radiale par section complète du nerf, avec perte de substance de 3 centimetres suture; guérison avec recuperation des fonctions motrices du nerf. Lyon Méd., 1916, v. 125, pp. 192-194.
Evans, J. J. Organic Lesions from Shell Concussion. Brit. M. J., Lond., 1915, ii, pp. 848.
Evans, Jameson. The Peripheral Lesions of Shell Concussion. Brit. M. J., Lond., 1916, i, pp. 721.
Everidge, John. Mental symptoms complicating a case of acute tetanus during treatment by carbolic injections. Brit. M. J., Lond., 1916, i, pp. 443-444.
Everth, E. Von der Seele des Soldaten im Felde. Jena, 1915. Rev.-Deutsche Med. Wchnschr., Berl. u. Leipz., 1915, v. 412, p. 1351.
Farrar, Clarence B. Neuroses among returned soldiers; types and indications. Bos. M. & S. J., 1918, clxxix, 583, 615.
Farrar, C. B. War and neurosis, with some observations of the Canadian Expeditionary Force. Am. J. Insan., Balt., 1917, v. 73, pp. 693-719.
Farrar, C. B. The problem of mental disease in the Canadian Army. Mental Hyg., Concord, N. H., 1917, v. 1, pp. 389-391.
Farrar, Clarence B. War neuroses and psychoses. Amer. Jour. Med. Sc., 1918, clv, 425.
Fauntleroy. Military organization and equipment in the present war. U. States Nav. M. Bull., Wash., 1916, v. 10, pp. 34-61.
Faure, J. L. Sur les tumeurs provoquées par l’huile camphorée. Bull. et mém. Soc. de chir. de Par., 1917, n. s., xliii, 525.
Faure, Maurice. La rééducation motrice des blessés et infirmes de la guerre. Bull. gén. de Thérap., Par., 1916, v. 168, pp. 40-46.
Fauser, A. Über dysglanduläre Psychosen. Deutsche med. Wchnschr., Berl. u. Leipz., 1916, No. 2, pp. 47-49.
Fazio, F. La cura del mutismo psicoisterico dei militari combattenti. Med. prat., Napoli, 1916, v. 1, pp. 371-373.
Fearnsides. Wassermann reaction in shell shock. Proc. Roy. Soc. Med., London., (Sec. of Neurol.), 1915-16, v. 9, pp. 39-41.
Feilchenfeld, Hugo. Ein objektives Symptom zur Prüfung der Nachtblindheit. Berl. Klin. Wchnschr., 1916, No. 44, pp. 1195-1196.
Feilchenfeld und Bauer. Kriegsblinden Fürsorge. Deutsche med. Wchnschr., Leipz. u. Berl., 1916, v. 42, pp. 1324.
Feiling, Anthony. Loss of personality from shell shock. Lancet, Lond., 1915, ii, pp. 63.
Fellner, B. Fall von echter Katatonie (Mähren). Wien. med. Wchnschr., 1915, No. 30, pp. 1155.
Felzmann. (War psychoses). J. Neuropath. i. Psikhiat., Korsakova, Mosk., 1915, v. 15, No. 4.
Fenwick, P. C. C. Entero-spasm following shell shock. Practitioner, Lond., 1917, s. xviii, 391.
Fernández Sanz. Contribución á la psiquiatria de la guerra; comentarios al determinismo causal y á la sintomatología de la psicosis de origen belico. Rev. clin. de Madrid, 1915, v. 13, pp. 121-131.
Fernet, Charles. De la surdité et de son traitement par l’activité fonctionelle. J. de Méd. et de chir., 1915, v. 86, Apr.
Fernet, Charles. De la gymnastique oculaire et de son application à l’éducation de la vue et au traitement de la myopie et de la presbyopie. J. de Méd. et chir. prst., Par., 1916, v. 87, pp. 153-157.
Ferrand, J. Réflexions médicochirurgicales sur la pratique neurologique en temps de guerre. J. de radiol. et d’électrol., Par., 1914-15, i, pp. 629-639.
Ferrand, Jean. Aphasie avec hémiplegie gauche par ligature de la carotide primitive droite. Paris Méd., 1916 (Part. Méd.), v. 19, pp. 537-540.
Ferrand, J. Y-a-t-il des hystéro-traumatismes différents en temps de paix et en temps de guerre? Rev. de méd., Par., 1916, v. 35, pp. 239-275; and pp. 293-313.
Ferrand, Jean. Y-a-t-il des hystéro-traumatismes différents en temps de paix et en temps de guerre? Rev. de méd., mai-juin, 1917, Rev. Progrès méd., Par., 1917, v. 43, pp. 356-357.
Ferrand, Jean. Hystéro-traumatismes avec syndrôme dit “physiopathique” guéri par la rééducation. Progrès méd., Par., 1917, No. 10, pp. 81-83.
Ferrand, Jean. De l’unité clinique et pathogénique de tous les hystéro-traumatismes. Paris méd., 1917, No. 24, pp. 509-512.
Ferrannini, L. La rieducazione professionale degli invalidi della guerra. Riforma, med., Napoli, 1917, v. 33, pp. 347-349.
Ferrie, Jean L. Contribution à l’étude des voyages pathologiques chez les alienés militaires. Thèses de Paris, 1915, v. 5.
Feuillade. Sur les accidents nerveux determinés par la déflagration de fortes charges d’explosifs. Rev. neurol. Par., 1916, v. 29, pp. 591-592.
Fiessinger, Ch. Le rôle psychologique du vin. Bull. Acad. de méd., Par., No. 8, fer. 1916. Paris Méd., 1916 (Part. Méd.), v. 19, p. 210.
Fiessinger, Noel. Choc emotionnel par explosion d’obus de gros calibre. Rev. gén. de clin. et de thérap., 1915, v. 29, pp. 99-100.
Fiessinger, Noel. Emotional Shock. Med. Press and Circ., Lond., 1915, v. 99, p. 563.
Fischer, H. Six months of war surgery in a base hospital in Germany. Am. J. Surg., N. Y., 1917, v. 31, pp. 4-10.
Fischer, H. Gunshot injuries of the peripheral nerves and their treatment. Ann. of Surg., 1917, lxv, 56.
Fischer, M. Die Erwerbsfürsorge für Kriegsinvalide an unseren Heil- und Pflegeanstalten. Psych.-neurol. Wchnschr., Halle a. S., 1915, v. 16, p. 420.
Flesch, J. Ueber sogen. funktionelle Nervenerkrankungen. Psychiatr.-neurol. Wchnschr., 20, 1918-9.
de Flines, E. W. Doofheid, simulatie en dissimulatie. Mil.-geneesk. Tijdschr., Haarlem, 1917, xxi, 124-133.
Flusser, E. Über Psychosen beim Kriegstyphus. Wien. med. Wchnschr., 1915, v. 65, No. 297.
Foix, Ch. Contribution à l’étude de l’apraxie idéo-motrice, de son anatomie pathologique et de ses rapports avec les syndrômes qui ordinairement l’accompagnent. Rev. neurol., Par., 1916, v. 29, p. 283.
Folgezustände. Über durch der Krieg bedrohte Folgezustände am Nervensystem. Berl. klin. Wchnschr., 1915, v. 42, p. 277.
Forgues. Maladies simulées. Caducée, Par., 1915, v. 15, pp. 132-133.
Forster. Der Krieg und die traumatischen Neurosen. Monatschr. f. Psychiat. u. Neurol., Berl., 1915, v. 37, pp. 72-75.
Forster, Frederick C. Management of neurasthenia, psychasthenia, shell-shock, and allied conditions. Practitioner, 1918, c. 85.
Forsyth, David. Functional nervous disease and the shock of battle: a study of the so-called traumatic neuroses arising in connection with the war. Lancet, Lond., 1915, ii, pp. 1399. (See also Mercier, Lancet, Lond., 1916, i, P. 154.)
Fortineau, Louis. Quelques cas de délire onirique observés au cours de la fièvre typhoïde. Presse Méd., Par., 1915, v. 23, p. 225.
Foucault, Prof. Expériences sur la fatigue mentale. Rev. phil., Par., 1915, v. 79. pp. 505-526.
Fox, R. Fortescue. Model hydrotherapeutic installation for soldiers with ground plan. J. Roy. Army Med. Corps, Lond., 1916, v. 26, pp. 660-664. Also, The “sedative pool bath”—Lancet, Lond., 1916, v. ii, p. 302.
Fox, R. Fortescue. Physical remedies for disabled soldiers. Lond., 1917, Bailliere, p. 287, 8o.
Frank. Krieg und ärztliche Sachverständigentätigkeit. Ärztl. Sachverst. Ztg., Berl., 1914, No. 23, pp. 434-436.
Fraser, J. S. War Injuries of the Ear. Edinb. M. J., 1917, p. 107.
Fraser, J. S. and John. The Morbid Anatomy of War Injuries of the Ear. Proc. Roy. Soc. Med., Lond., 1917-18, v. 10 (see Otol.), pp. 56-90.
French wounded from some early actions. Brit. M. J., Lond., 1914, ii, p. 853-854.
Frenkel, H. L’héméralopie chez les mobilisés de l’intérieur. Arch. d’opht., Par., 1917, v. 35, pp. 577-579.
Freud, Sigmund. Zeitgemässes über Krieg und Tod. Imago, Leipz. and Wien., 1915, v. 4, pp. 1-21.
Frey, Hugo and Selye, Hugo. Beiträge zur Chirurgie der Schussverletzungen des Gehirns. Wien. klin. Wchnschr., 1915, v. 28, pp. 722-724.
Friedländer, A. Nerven- und Geisteskrankheiten im Felde und im Lazarett. Wiesb., 1914 (J. J. Bergmann), p. 39, 8o.
Friedländer, R. Julius. Zerebellare Symptomenkomplexe nach Kriegsverletzungen. Neurol. Centralbl., Leipz., 1915, v. 34, p. 813.
Friedmann. Zur Auffassung die gehäuftigten kleinen Anfälle. Monatschr. f. Psychiat. u. Neurol., Berl., 1915, v. 38, p. 76.
Fröderström, H. (Neurological impressions (May, 1916) from a travel report to the chief of the naval medical department.) Tidskr. i mil. Hälsov., Stockholm, 1917, v. 42, pp. 137-149.
Froment, J. Paraplégie par déflagration d’obus. Rev. neurol., Par., 1914, v. 22, pp. 754-755, and pp. 1205-1214.
Froment, J. Du pronostic de l’aphasie traumatique consécutive aux plaies du crâne par armes à feu. Lyon chirurg., 1916, v. 13, pp. 434-447.
Froment. La préhension dans les paralysies du nerf cubital et le signe du pouce. Presse méd., Oct. 21, 1915.
Fuchs, W. Mobilmachungspsychosen. Aerztl. Sachverst.-Ztg., Berl., 1915, xxi, 25-29.
Functional cardiac disorders in soldiers. J. Am. M. Ass., Chicago, 1917, v. 69, p. 202.
Furbush, Edith M. Mental disease, suicides and homicides in the United States Army and Navy, 1897-1915, prepared from the Annual Reports of the Surgeons-General. Mental Hyg., Concord, N. H., 1917, i, 406-408.
Further Extension of Second Eastern General Hospital, Brighton. Brit. M. J., Lond., 1915, i, p. 908.
Gaillard. Tachypnée hystérique chez un militaire. Bulletins de la Société Médicale des Hôpitaux de Paris, 30 décembre 1915.
Garbo. A propos du choc gazeux causé par l’explosion des obus. Wien. Klin. Woch., No. 4, 1915.
Garrod, A. E. War heart, which calls for treatment by complete rest. Lancet, Lon., 1917, i, 985.
Garton, W. Shell shock and its treatment by cerebrospinal galvanism. Brit. Med. Jour., 1916, ii, 584.
Garton, Wilfrid. Shell shock and its treatment by cerebrospinal galvanism. Brit. M. J., 1916, v. ii, pp. 584-586.
Gaté, J. et M. Dechosal. Méningite cérébro-spinale à pseudoméningocoque. Lyon Méd., 1916, v. 125, pp. 349-352.
Gaucher et Renée Klein. Le psoriasis émotif et traumatique. Paris méd., 1916, (Part. Méd.), v. 18, pp. 428-430.
Gaupp, R. Granatkontusion. Bruns. Beitr. 96 H. 3. Rev. Deutsche med. Wchnschr., 1915, v. 412, pp. 811-812.
Gaupp, R. Hysterie und Kriegsdienst. Münch. med. Wchnschr., 1915, v. 62, pp. 361-363.
Gaupp, R. Ungewöhnliche Formen der Hysterie bei Soldaten. Münch. med. Wchnschr., 1915, v. 33, p. 1119.
Gaupp, R. Ungewöhnliche Formen der Hysterie bei Soldaten. Psychiat. Neurol. Wchnschr., Halle a. S., 1915-16, v. 17, p. 256.
Gaupp, R. Die Granatkontusion. Beitr. z. klin. Chir., Tübing., 1915, v. 96B, pp. 277-294.
Gaupp, R. Die Granatkontusion. Centralbl. f. Chir., Leipz., 1915, v. 421, pp. 429-430.
Gaupp, R. Die Diensbrauchbarkeit der Epileptiker und Psychopathen. Die militärärztliche Sachsverständigentatigkeit auf dem Gebiete des Ersatzwesens und der militärischen Versorgung. Erste Teil., pp. 115-139. Jean Fischer, 1917.
Gautrelet, J. Les bases scientifiques de l’éducation professionnelle des mutilés. Bull. Acad, de Méd., Par., 1915, v. 73, pp. 663-668.
Geigel. Nervöses Herz und Herzneurosen. Münch. Med. Wchnschr., 1917, No. 1, pp. 30-32.
Gennerich, W. Die Ursachen von Tabes und Paralyse. Monatschr. f. Psychiat. u. Neurol., Berl., 1916, v. 39, No. 6, p. 341.
Gerhardt. Uber Herzstörungen im Kriege. Münch. med. Wchnschr., 1915, v. 342, p. 1174.
Gerhardt. Hysterische Paraplegie. Münch. med. Wchnschr., 1915, v. 342, pp. 1763.
Gerstmann. Hemianopie durch Contrecoup nach Schussverletzung. Klin. therap. Wchnschr., Wien. u. Berl., 1916, v. 332, p. 29.
Gerver, A. V. (A study of statistics of mental diseases in the army in time of war.) Psikhiat. Gaz., Petrogr., 1916, v. 3, pp. 158-165.
Gerver, A. V. (Mental diseases in the theatre of war.) Russk. Vrach., Petrogr., 1915, v. 14, p. 793; p. 817; p. 841.
Gerver, A. V. (Traumatic neuroses among soldiers). Russk. Vrach., Petrogr., 1915, v. 14, pp. 937-944; and pp. 967-972.
Gerver, A. V. (Neurasthenia and influence of the war on its symptomatology.) Russk. Vrach., Petrogr., 1916, v. 15, p. 220; p. 241.
Giachetti, C. I caratteri e la guerra. Riv. di psicol., Bologna, 1916, v. 12, pp. 301-316.
Giannelli, A. Le malattie mentali e nervosi in guerra. Riv. ospedal., Roma, 1915, v. 5, pp. 322-331.
Giannuli, F. Le syndrome Korsakoff et la commotion cérébrale. Rivista sperimentale di Freniatria, vol. XL, fasc. 2, 30 juin 1914.
Gibt es eine “Kriegspsychose?” Psychiat. Neurol. Wchnschr., Halle a. S., 1914-1915, v. 6, pp. 356-357.
Gilbreth, F. B. The problem of the crippled soldier; how to put him on the payroll. Scient. Am. Suppl., N. Y., 1917, v. 83, p. 260.
Gilbreth, F. B. and Gilbreth, Lillian M. The conservation of the world’s teeth; a new occupation for crippled soldiers. Trained nurse (etc.), N. Y., 1917, v. 59, pp. 5-11.
Gilchrist, Norman S. Analysis of causes of breakdown in flying: with notes on the nervous mechanism of the flying man. (Ref. lost.)
Gilles, André. Étude sur certains cas de neurasthénie. Ann. méd.-psychol., Par., 1916, 1917; v. 73, pp. 209-229; and pp. 333-364.
Gilles, André. L’hystérie et la guerre troubles fonctionnels par commotion. Leur traitement par le torpillage. Ann. méd. psychol., Par., 1917, v. 73, pp. 207-227.
Gillet, H. et Boyé, G. Les insuffisants cardiaques. Paris méd., 1916, v. 21, pp. 30-33.
Gilyarovski, V. A. (The war and the care of the insane in time of peace.) Sovrem. Psikhiat., Mosk., 1915, v. 9, pp. 287-297.
Gilyarovski, V. A. (Nature of alterations in the neuropsychic sphere after war contusions.) Sovrem. Psikhiat., Mosk., 1916, v. 10, pp. 403-433.
Ginestous, E. L’indice visuel d’aptitude au service militaire. Arch. de méd. et pharm. mil., Par., 1914-15, v. 64, pp. 718-24.
Ginestous, Etienne. Blépharospasme tonique hystéro-traumatique. Gaz. méd. de Par., 1915, v. 14, pp. 61-62.
Ginestous, E. L’armée française perd 20,000 astigmates. Caducée, Par., 1915, v. 15, p. 99.
Ginestous, E. Hémianopsie en quadrant. Progrès méd., Par., 1916, v. 31, pp. 3-4.
Gino, S. and Stefano, B. Mutismo isterico consecutivo a scoppio di granata in sogetto istero-epilettico. Gazz. d. osp., Milano, 1917, v. 38, pp. 308-310.
Giroux. Hémiplégie consécutive à une intoxication par les gaz asphyxiants. Rev. Paris méd., 1916. (Part. Méd.), v. 21, p. 436.
Glaser, W. Diphtheriebazillen als Meningitiserregen. München. med. Wchnschr., 1917, 64, 856-57.
Glieboff, D. A. (Malingering by recruits.) Sibirsk. Vrach., Tomsk, 1915, i, 4, 49, 62.
Goddard, H. H. The place of intelligence in modern warfare. U. S. Nav. M. Bull., Wash., 1917, v. 9, pp. 283-289.
Goetjes. Ueber Gehirnverletzungen durch Granatsplitter. Münch. med. Wchnschr., 1915, v. 62, pp. 897-898.
Goissard, Liébault. Les aphones pendant la guerre. Archiv. de Méd. et de Pha. Mil., 1916, v. 66, No. 1 or No. 3; p. 169.
Golant, R. Ya. (Neurotic symptoms in soldiers). Obozr. Psikhiat., Nevrol., Petrogr., 1916, v. 20, pp. 63-66.
Goldscheider. Zur Frage der traumatischen Neurose. Deutsche med. Wchnschr., Berl. u. Leipz., 1916, v. 42, No. 46.
Goldsmith. Special Discussion on Warfare Injuries and Neuroses. Proc. Roy. Soc. Med., Lond., 1917, v. 10 (sec. Octol.), pp. 119-122.
Goldstein, K. Die militärische Sachsverständigentatigkeit auf dem Gebiete des Ersatzwesens und der militärischen Versorgung bei de Hirnverletzungen. Erste Teil, pp. 194-232. Jena, Fischer, 1917.
Goldstein. Beobachtungen an Schussverletzungen des Gehirns und Rückenmarks. Deutsche med. Wchnschr., Berl. u. Leipz., 1915, v. 41, pp. 215-217.
Goldstein. Die Suggestionstherapie der funktionellen neurosen im Feldlazarett. Therapie der Gegenwart, Sept., 1917.
Goldthwaite, J. E. The place of orthopedic surgery in war. Am. J. Orthop. Surg., Bost., 1917, v. 15, pp. 679-686.
Gonda, Viktor. Rasche Heilung der Symptome der im Kriege entstandenen traumatischen Neurosen. Wien. klin. Wchnschr., 1916, v. 29, No. 30.
Goodwin, T. H. No. 2, Notes for Army Medical War Officers. Medical Manual War Series. Lea and Febiger, 1917.
Gordon, W., Sunderland, S. (et al). Physical treatment for disabled soldiers. Lancet, Lond., 1917, v. 1, p. 348.
Goria, C. Alcune considerazioni attomo al mutismo psichico nei militari alla sua genesi emozionale e commozionale. Riform. med., Napoli, 1916, v. 32, pp. 725 and 756.
Gosset, H. Contribution à l’étude expérimentale du contrôle auditif. Progrès méd., Par., 1916, No. 1, pp. 21-22.
Gosset, H. Traitement des impotences consécutives aux blessures de guerre par la rééducation psycho-motrice. Progrès Méd., Par., 1916, No. 3, pp. 35-38.
Gosset, H. La rééducation de l’appareil locomoteur. Progrès Méd., Par., 1916, No. 3, pp. 65-70.
Gosset, H. Expériences relatives au contrôle auditif. Progrès Méd., Par., 1917, No. 2, pp. 9-10.
Gouget, A. La bradycardie de fatigue. Bull. Acad. de Méd., Par., 1915, v. 74, pp. 810-812.
Gouget. Un cas de neuro-fibromatose. Presse Méd., 1916, v. 24, p. 309.
Gougerot, H. and Charpentier, Albert. Paralysies réflexes troubles trophiques réflexes consécutifs aux blessures des extrémités. Ann. de méd., Par., 1916, v. 3, pp. 269-297.
Grace, J. J. A note on the electrical treatment of disabilities due to wounds. Brit. M. J., Lond., 1915, ii, p. 812.
Gradenigo, G. Esagerazione e simulazione della sordita nei militari. Arch. ital. di otol. Torino, 1916, v. 27, pp. 139-147.
Gradenigo. Mutismo, afonia, sordita nei militari: di origine psichica, de cause organiche: simulazioni e criteri differenziedi obiettive. Riv. di patol. nerv. Firenze, 1917 (March).
Graham, W. War and the incidence of insanity. Med. Officer, Lond., 1916, v. 16, p. 453.
Granjux. La faillite de l’instruction sur l’aptitude physique au service militaire. J. de méd. et chir. prat., Par., 1915, v. 86, pp. 849-853.
Granjux. De la nécessité des services de psychiatrie et de médecine légale aux armées. Caducée. Par., 1916, xvi, 43-45.
Granjux. Les conditions dans lesquelles seront pratiquées les expertises en matière d’accidents du travail dont seront victimes les mutilés de la guerre. Soc. méd. lég. de France, Bull., Par., 1917, v. 14, pp. 221-222.
Grant, Dundas. Mutism, stammering, psychical deafness. Proc. Roy. Soc. Med., Lond., 1915-16, v. 9 (sect. Psychiat.), pp. 37-38.
Grant, D. Special discussion on warfare injuries and neuroses. Proc. Roy. Soc. Med., Lond., 1917, v. 10 (sec. Otol.), pp. 93-96.
Grasset. Clinical lectures on the psychoneuroses of war. (2 papers). Med. Press and Circ., Lond., 1915, i, v. 99, pp. 560-563; and pp. 586-587.
Grasset. Le traitement des psychonévroses de guerre. Presse méd., Par., 1915, v. 23, pp. 105-108; and p. 425.
Grasset. Les psychonévroses de guerre. Presse médicale, 1 avril, 1915.
Grasset. Les névroses et psychonévroses de guerre; conduite à tenir à leur égard. Rev. neurol., Par., 1916, xxiii, 767-774. (Discussion) 774-788.
Grasset. Les symptômes atypiques à développement tardif dans les traumatismes crânio-cérébraux. Montpel. méd., 1916, v. 39, p. 19.
Grasset. Les maladies de guerre du système nerveux et les conseils de réforme. Presse méd. Par., 1916, v. 24, pp. 1-2.
Grasset. Les grandes types cliniques des psychonévroses de guerre. Rev. neurol. Par. 1917, v. 24, p. 471.
Grasset. Les grandes types cliniques de psychonévroses de guerre. Montpel. méd., 1917, n. s., v. 39, pp. 607-628.
Grasset et Maurice Villaret. À propos de pronostic tardif des traumatismes crânio-cérébraux. Rev. neurol., Par., 1916, v. 29, pp. 833-834.
Gray, H. M. W. Gunshot wounds of the head. Brit. Med. Jour., 1916, i, 261.
Green, Edith M. N. Blood pressure and surface temperature in 110 cases of shell shock. Lancet, Lond., 1917, ii, pp. 456-457.
Greenlees, T. D. The war; impressions, neuro- and psychological. Med. Press and Circ., Lond., 1916, n. s., v. 101, pp. 101-103; also Caledon., M. J., Glasg., 1915-16, No. 10, pp. 183-187.
Gregor. Granatenkontusion mit ausgedehntem amnestichen Defekt. Münch. med. Wchnschr., 1915, v. 622, p. 1055.
Grenier de Cardenal, Legrand, Benoit. Trois nouveaux cas de rage chez l’homme. Presse méd., Par., 1917, v. 25, pp. 564-566.
Griffith, A. D. Injuries of the eye and orbit. Lancet, Lon., 1916, i, 1245.
Grivot, M. Appareil auditif et traumatismes de guerre. Paris méd., 1915, v. 17, pp. 359-365.
Grober. Die Krankheiten der Kreislauforgane und der Krieg. Munch. med. Wchnschr., 1914, ii, v. 61, pp. 2388-2390.
Gross, C. Nervöse Kriegsdienstschädigungen. Wien klin. Wchnschr., 1916, xxix, 1577.
Grünbaum, F. Hysterie und Kriegsdienstbeschädigung. Deutsche med. Wchnschr., Berl. u. Leipz., 1916, v. 42, pp. 1452-1453.
Grünwald. Schussverletzungen der pneumatischen Schädelhöhlen. München [933]med. Wchnschr. 1915, v. 621, pp. 823-825.
Grutzhaendler-Indelson. Troubles sensitivo-moteurs hystérotraumatiques observés a l’occasion de la guerre 1914-1915. Thèse de Paris, 1915.
Gudden. Beginnende Behandlung psychischer Erkrankungen im Felde. München med. Wchnschr., 1915, v. 62, pp. 1730.
Guépin, A. Dix cas de chirurgie cérébrale. Caducée, Par., 1916, v. 16, pp. 74-77.
Guerre et les éclopés psychiques. Ann. d’Hyg., Par., 1917, v. 25, pp. 252-254.
Guilbert, Charles and Maucurier, G. Guide de rééducation physique en groupe. Méthode de gymnastique rééducative pour les blessés militaires. Par., 1916, J. B. Baillière et fils. 128 pp., 12o.
Guild, S. R. War deafness and its prevention; a critical review. J. Lab. and Clin. M., St. Louis, 1916-17, v. 2, pp. 849-861.
Guillain, G. Un cas de contractures généralisées avec symptômes méningés consécutive à l’éclatement d’un projectile sans plaie extérieure. Presse Méd., Par., 1915, v. 23, p. 181.
Guillain, G. Les crises épileptiques consécutives à l’explosion des projectiles sans plaie extérieure. Presse méd., Par., 1915, v. 23, pp. 181.
Guillain, G. Sur un cas de mutisme consécutif à l’éclatement d’un projectile. Presse Méd., Par., 1915, v. 23, p. 182.
Guillain, G. Un cas de tremblement pseudo-parkinsonien consécutif à l’éclatement d’un projectile sans plaie extérieure. Presse Méd., Par., 1915, v. 23, p. 182.
Guillain, G. Les syndrômes paralytiques consécutifs à l’éclatement des projectiles sans plaie extérieure. Presse méd. Par., 1915, v. 23, pp. 225-226.
Guillain, G. Le syndrôme cérébelleux à type de sclérose en placques consécutif à l’éclatement des projectiles sans plaie extérieure. Presse méd., Par., 1915, v. 23, p. 226.
Guillain, G. Sur un état de stupeur avec catatonie, hypothermie, bradycardie et hypopnée consécutif à l’éclatement d’un projectile sans plaie extérieure. Presse méd., Par., 1915, v. 23, p. 226.
Guillain, G. Les névrites irradiantes et les contractures et paralysies traumatiques d’ordre réflexe. Soc. méd. des Hôpitaux, 26 mai 1916.
Guillain, G. Sur un syndrôme choréiforme consécutif à l’éclatement d’un projectile sans plaie extérieure. Presse méd., Par., 1915, v. 23, p. 225.
Guillain, G. Hémiplegie organique consécutive à un éclatement d’obus sans plaie extérieure. Presse méd., Par., 1915, v. 23, p. 429.
Guillain, G. Influence sur le système nerveux des éclatements d’obus de gros calibre. Rev. gén. de clin. et de theráp., Par., 1915, v. 29, p. 736.
Guillain, G. Sur les accidents nerveux déterminés par la déflagration de fortes charges d’explosifs. Rev. neurol. Par., 1916, v. 29, pp. 576-577.
Guillain, G. Un syndrôme consécutif à l’éclatement des gros projectiles sans plaie extérieure. Arch. de méd. et pharm. mil., Par., 1916-17. lxvi, 542.
Guillain, G. et Barré, A. Inversion du réflexe achilléen et du réflexe médio-plantaire dans un cas de lésion du nerf sciatique poplité interne. Presse méd., Par., 1917, v. 25, p. 448.
Guillain et Barré. Hémorragie méningée consécutive à une commotion par éclatement d’obus sans plaie extérieure. Méningite à pneumocoques mortelle secondaire. Bull. et mém. soc. méd. d’hôp. de Par., 1917, v. 33, pp. 898-900.
Guillain and Barré. Les troubles sphinctériens transitoires dans les commotions par éclatement de gros projectiles sans plaies extérieures. Bull. et mém. soc. méd. d’hôp. de Par., 1917, v. 22, pp. 1114-1118.
Guillain and Barré. Les troubles des réactions pupillaires dans les commotions par éclatement de gros projectiles sans plaie extérieure. Bull. Acad. de méd., Par., 1917, v. 78, pp. 158-159.
Guillain et Barré. Troubles pyramidaux organiques consécutifs à l’éclatement d’un projectile sans plaie extérieure. Soc. méd. d’hôp. Par., 1916, 26 mai.
Guillain et Barré. Soc. méd. d’hôp. Par., 1916, 21 janvier.
Guillain et Barré. Soc. méd. d’hôp. Par., 1916, 7 avril.
Guillain et Barré. Les contractures ischémiques. Réunion Méd. de la VI armée, Jan. 12, 1916.
Guillain. Les névrites irradiantes et les contractures et paralysies traumatiques d’ordre réflexe. Soc. Méd. des Hôpitaux, May 26, 1916.
Guillain et Barré. Forme clinique de la névrite ascendante. Presse méd. 3 avril 1916.
Guillain and Barré. (Lesions with external wounds.) Bull. et mem. soc. méd. hôp. d Par., 1916, v. 40, p. 834.
Guillain and Barré. Deux cas d’astasie-abasie avec troubles du nerf vestibulaire chez les syphilitiques anciens. Ann. de méd. Par., v. 3, 1916, pp. 431-436.
Guillain and Barré. A propos d’un cas d’astasie-abasie trépidante. Presse méd., Par., 1916, v. 24, pp. 119-120.
Guillain and Barré. Apoplexie tardive consécutive à une commotion par éclatement d’obus sans plaie extérieure. Ibid., 1473-74.
Guillain et Barré. Hémiplégies par blessures de guerre. Diagnostic topographique du siège des lésions. Presse méd., Par., 1916, v. 24, pp. 121-122.
Guillain et Barré. Syndrôme d’avellis bilatéral, manifestation de syphilis nerveuse. Presse méd., Par., 1916, v. 24, p. 150.
Guillain et Barré. Deux cas d’hémiplégie organique consécutifs à la déflagration de fortes charges d’explosifs, sans plaie extérieure. Paris méd., 1916 (Part. Méd.), v. 21, p. 420.
Guillain Barré and Strohl. Étude graphique des réflexes tendineux abolis à l’examen clinique dans un cas de commotion par éclatement d’obus sans plaie extérieure. Bull. et mém. Soc. méd. d’hôp. de Par., 1917, 3. s, xii, 313-315.
Gumpertz. Beiträge z. Kenntniss d. Nervenschädigungen des Kriegs. Aus dem Kriegslazarett. Berl., J. Goldschmidt.
Gunson, E. B. Cardiac symptoms following dysentery among soldiers. Lancet, Lon., ii, 146.
Gutzmann, H. Stimm- und Sprachstörungen im Kriege und ihre Behandlung. Berl. klin. Wchnschr., 1916, v. 53, pp. 154-158.
Haas. Sur quelques blessures oculaires occasionnées par les engins à forte charge d’explosif. Presse méd., Par., 1916, v. 24, p. 52.
Haberer, H. v. Beitrag zu den Schädelverletzungen im Kriege. Wien. klin. Wchnschr., 1914, v. 27, pp. 1590-1593.
Hadfield, J. A. Influence of hypnotic suggestion on inflammatory conditions. Lancet, Lond., 1917, v. ii, p. 678.
Haddon, John. Shell-shock: its cause and proper treatment by diet. Domin. Med. Mon., 1918, i, 33.
Haddon, J. Shell shock; its cause and proper treatment by diet. Med. Press. Lond., 1917, n. s., civ, 409-411.
Hagedorn. Abnorme Selbstbeschädigungen. Deutsche Zeitschr. f. Chir., Leipz., 1916, v. 137, pp. 1-46.
Hahn. Kriegspsychosen. Med. Klin. Berl. u. Wien., 1915, v. 3, pp. 114-115.
Hahn. Uber Kriegspsychosen. München med., Wchnschr., 1915, v. 621, p. 268.
Hakkebusch, V. M. (What is caused by wind contusion: neurosis, or organic injury of the nervous system.) Sovrem, Psikhiat., Mosk., 1915, v. 9, pp. 389-405.
Hakkebusch, V. M. (Nervous diseases in connection with wind contusion.) Sovrem. Psikhiat., Mosk., 1916, v. 10, pp. 226-249.
Halipré, A. Test de guérison de la paralysie radiale (signe des fléchisseurs) Rev. neurol., Par., 1917, v. 24, pp. 87-89.
Hamburger, Franz. Uber simulierte und aggravierte Bronchitis. Militärarzt Wien. med. Wchnschr., 1915, v. 49, No. 35.
Hamilton, Allan McLane. Tests for the perception efficiency of recruits. Med. Rec., N. Y., 1918, v. 93, pp. 285-286.
Hamilton, Allan McLane. Psychopathology of the war. Med. Rec., N. Y., 1915, v. 87, p. 110.
Hammesfahr. Vorstellung zweier Patienten mit Gehirnschüssen. (Abstract.) Deutsche med. Wchnschr., 1915, Berl. u. Leipz., v. 41, p. 575.
Hammond, T. E. Involvement of the external and internal popliteal nerves in lesions of the sciatic nerve. Brit. Med. Jour., 1918, i, 397.
Harford, C. F. Visual neuroses of miners in their relation to military service. Brit. M. J., Lond., 1916, i, pp. 340-342.
Harris, W. Abnormal median and ulnar nerve-supply in the hand. Lancet, London, 1917, ii, 710.
Harris, Wilfred. Nerve Injuries and Shock. 1915, London, Henry Frowde.
Harris, Wilfred. Shell shock without visible signs of injury. Proc. Roy. Soc. Med., 1915-16 (Sec. Psychiat.), pp. 33-34.
Harrower, H. R. Shell shock and the internal secretions; with suggestions as to treatment. Prescriber, Edinb., 1916, x, 203-209.
Harwood, T. E. Nature and treatment of concussion. Lancet, Lond., 1916, i, p. 551.
Harwood, T. E. Shell shock. Lancet, Lond., 1916, i, 698.
Harwood, T. E. Three cases illustrating the functional consequences of head injuries. Lancet, Lond., 1916, ii, v. 191, p. 431.
Harwood, T. E. Functional conditions in head injuries. J. Roy. Army Med. Corps, Lond., 1917, v. 28, pp. 699-707.
Harzbecker. Ueber die Aetiologie der Granatkontusionsverletzungen. Deutsche med. Wchnschr., Berl., u. Leipz., 1914, v. 402, p. 1985.
Hauptmann, A. Kriegsneurosen und traumatische Neurose. Monatschr. f. Psychiat. u. Neurol., Berl., 1916, v. 38, pp. 20-32.
Haury. Un dément précoce engagé volontaire. Rev. de méd., Par., 1914-15, v. 24, pp. 591-593.
Haury. Un cas de “folie minime” chez un débile. Presse Méd., Par., 1915, v. 23, p. 429.
Haury. Un autre déserteur pathologique. Presse Méd., 1915, v. 23, p. 429.
Haury. Les retentissements psycho-organiques de la vie de guerre. Presse Méd., Par., 1915, v. 23, pp. 458-459.
Haury. De l’utilisation des indisciplinés en temps de guerre. Ann. méd. psychol., Par., 1916-17, v. 7, pp. 525-530.
Hayward, E. Beitrag zur Klinik der Schädelschüsse, nach den Erfahrungen im Heimatlazarett. Berl. klin. Wchnschr., 1915, v. 52, pp. 1186-1200; and pp. 1212-1218.
Hecht, V. Leitfaden den physikalisch-therapeutischer Nachbehandlung Kriegsverwundeten. W. Braumüller, Wien. u. Leipz., 1916. Rev. Deutsch. med. Wchnschr., 1916, No. 39, p. 1207.
Heilig and Sick, P. Uber Schussverletzungen des Gehirns. München med. Wchnschr., 1915, v. 621, pp. 172-173.
Heimanovich, A. I. (Public psychiatric hospitals and the war.) Kharkov. M. J., 1915, v. 20, pp. 371-376.
Heimanovich, A. I. (Mental diseases of war time.) Kharkov. M. J., 1915, v. 20, pp. 377-395.
Heimanovich, A. I. (Institutes of functional reëstablishment.) Kharkov. M. J., 1916, v. 22, pp. 243-252.
Heitz, Jean. Cinq cas de paraplégie organique consécutive à des éclatements d’obus sans plaie extérieure. Paris Méd. (Part. Méd.), 1915, v. 17, pp. 78-85.
Helys, M. The reëducation and placement of war cripples. Am. J. Care Cripples, N. Y., 1917, v. 4, pp. 168-178.
Helys, M. Reëducation and placement of war cripples. Amer. Jour., Care for Crip., 1917, iv, 168.
Henderson, D. K. A case of pathological lying occurring in a soldier. Rev. Neurol. and Psychiat., Edinb., 1917, v. 15, pp. 223-232.
Henderson, Yandell and Seibert, E. G. Organization and objects of the Medical Research Board, Air Service, U. S. Army. Jour. A. M. A., 1918, lxxi, 1398.
Hertz, A. F. (See also Hurst.) Paresis and involuntary movements following commotion produced by the bursting of a large shell. Proc. Roy. Soc., Méd., Lond., (sec. Neurol.), 1914-15, v. 8, pp. 83-84.
Hertz, A. F. Nerves and the War. Guy’s Hosp. Gaz., Lond., 1915, v. 29, pp. 169-173; and pp. 335-339.
Hertz, A. F. Concussion Blindness. Lancet, 1916, i, p. 15.
Hertz, A. F. Medical diseases of the war. Lond., 1917, G. Arnold, pp. 151, 8o.
Hertz, A. F. and Ormond, A. W. The treatment of concussion blindness. Lancet, Lond., 1916, i, 15-17.
Hesnard, A. Le traitement local et la radiothérapie locale des blessures des troncs nerveux. Arch. d’électric. méd., Bordeaux, 1916, v. 26, pp. 5-9.
Hesnard, A. Note sur la radiothérapie des blessures des troncs nerveux. Paris méd., 1916 (Par. Méd), v. 19, p. 302.
Hesnard, A. Un nouvel élément de la réaction de dégénérescence—l’hyperexcitabilité galvanotonique des muscles. Par. méd., 1917, No. 46, pp. 410-415.
Hesnard, A. Un cas d’hémiplégie glosso-pharyngo-cervico-laryngée par syndrôme des quatres dernières paires crâniennes. Arch. de méd. et pharm. nav., Par., 1917, v. 103, pp. 370-377.
Hesnard, A. Un cas de psychose post-onirique chez un aliéné militaire. Caducée, Par., 1914, xiv, 202.
Hesse, W. Ueber Spättetanus, chronischen Tetanus und Tetanusrezidiv. Deutsches Archiv. f. klin. Med., Leipz., 1917, 124, p. 284.
Hewat, A. Fergus. Clinical cases from Medical Division, Royal Victoria Hospital, Netley. Edinb. M. J., 1917, v. 18, pp. 210-215.
Hezel. Eine im Felde vorkommende Beschäftigungsneuritis. Neurol. Centralbl., 37, Nr. 15, 1918.
Hill, David Spence. Valid uses of psychology in the rehabilitation of war victims. Mental Hygiene, II, October, 1918.
Hill, L. Death from high explosives without wounds. Brit. M. J., Lond., 1917, v. 1, p. 665.
Hine, M. L. The recovery of fields of vision in concussion injuries of the occipital cortex. Brit. J. Ophth., Lond., 1918, v. 2, pp. 12-25.
Hinsdale, G. Hydrotherapeutics in the war. N. Y. Med. Jour., 1917, cvi, 893.
Hirschfeld, Arthur. Die hydrotherapeutische Behandlung der im Kriege erworbene Neurasthenie und Hysterie. Zerb. f. Phys. u. Diätet., Ther., Leipz., 1915, v. 19, pp. 59-62.
Hirtz, E. J. Le traitement des impotences fonctionnelles consecutives aux blessures de guerre. Presse Méd., Par., 1915, v. 23, pp. 139-141.
His, W. Ermüdungsherzen im Felde. Med. Klin. Berl. u. Wien., 1915, v. ii1, pp. 293-298.
Hoch, August. Recommendations for the observation of mental disorders incident to the War. Psychiat. Bull. Utica, 1917, v. 2, No. 3, pp. 377-385.
Hoche. Krieg und Seelenleben, 1915, Speyer and Kaerner, Freiburg.
Hoche. Die Versorgung der funktionellen Kriegsneurosen. Münch. med. Wchnschr., 1916, v. 63, p. 1782.
Holland, C. T. Two years’ experience of war radiography in a base hospital. Amer. Jour. Elec. and Radiol., 1917, xxvi, 448.
Hollande, Lepeytre et Gate, J. Simulation d’albuminurie par injection intravésicale d’ovalbumine. Lyon méd., 1916, v. 125, pp. 194-196.
Hollande et Marchand. A propos d’un cas de maladie de Derkum. Lyon med., 1917, v. 126, pp. 362-365.
Holmes. G. and Lister, W. T. Disturbances of vision from cerebral lesions, with special reference to the cortical representation of the macula. Proc. Roy. Soc. Med., Lond., 1915-16, v. 9 (sec. Ophth.), pp. 57-96.
Holmes, Gordon and Smith, S. Case of bilateral motor apraxia with disturbance of visual orientation. Jr. Roy. Army Med. Corps, Lond., 1917, i, pp. 78-91.
Horder, Thomas J. Cerebro-spinal fever. Lond., 1915, Henry Frowde.
Horn, P. Zur Begutachtung nervöser Unfallfolgen. München. méd. Wchnschr., 1915, v. 62, pp. 1745-48.
Horn, P. Zur Nützbarmachung erhaltener und wiedergewonnener Arbeitskraft bei Unfallsneurosen. Aerztl. sachverst. Ztg., Berl., 1915, v. 21, pp. 253-257; and pp. 279-282.
Horn, P. Uber Sonnenstich mit organische Symptomen. Zentralbl. Nervenk. u. Psychiat., Coblenz. u. Leipz., 1915, v. 51, No. 4. Berl. Klin, Wchnschr. 1916, i, No. 2, p. 44.
Horn, P. Zur Aetiologie und klinischen Stellung der Unfall- und Kriegsneurosen. Neurol. Zentralbl. Leipz., 1917, v. 36, No. 3, and No. 7.
Horsfall, W. N. Malingering in the services. Med. J. Australia, Sydney, 1916, iii, 54.
Horsley, Sir Victor. Address on gun-shot wounds of the head; Lancet, Lond., 1915, i, pp. 359-362.
Horstmann. Zur traumatischen Neurose. Arztl. Sachverst. Ztg., Berl., 1914, v. 22, Nov. 5; Rev. Psychiat. neurol. Wchnschr., Halle, a. S., 1914-15; v. 16; p. 346.
Horstmann. Traumatische Neurose. Arztl. Centr. Ztg., v. 27, p. 53, also p. 76.
Hotz. Über Kriegsverletzen des Nervensystems. München med Wchnschr., 1914, No. 45, pp. 2219-2221; and pp. 2264-2266.
Hotz. Über Kriegsverletzungen des Nervensystems. Zentralbl. f. Chir., Leipz., 1915, v. 421, pp. 6-7.
Hoven. Les maladies mentales et la guerre. Presse Méd., 1917, v. 53, p. 559.
How to Avoid Damage to Auditory Apparatus by Explosions. Monde méd., 1918, v. 28, pp. 61-63.
Howard, W. L. Psychology of War. N. Y. M. J., 1915, v. 101, p. 15.
Howland, G. W. Neurosis in returned soldiers. Med. Fortnightly, St. Louis, 1917, v. 49, pp. 97-100.
Howland, G. W. The neuroses of returned soldiers. Am. Med., Burlington, Vt., 1917, v. 23, pp. 313-319.
Hrdlicka, Ales. Suggestions relating to the new National Army by the Anthropology Committee of the National Research Council. (Wash., 1917), p. 4, 8o.
Hunt, J. R. Exhaustion pseudoparesis; a fatigue syndrome simulating early paresis, developing under intensive military training. Jour. A. M. A., lxx, 11.
Huntington, P. W. The present and proposed Roentgenologic Service of the United States Army. Am. J. Roentgenol., Detroit, 1917, v. 4, pp. 597-601.
Hurst, A. F. (See also Hertz.) Nerves and the war. Guy’s Hosp. Gaz., 1915, v. 29, pp. 169-173.
Hurst, A. F. Case of deaf-mutism followed by partial amnesia. Guy’s Hosp. Gaz., Lond., 1916, v. 30, p. 279; also pp. 410-412.
Hurst, A. F. Medical diseases of the war. Lond., 1917, Arnold, p. 151, 8o.
Hurst, A. F. Observations on the etiology and treatment of war neuroses. Brit. M. J., Lond., 1917, ii, pp. 409-414.
Hurst, A. F. (Nervous Affections.)
Hurst, A. F. War epilepsy. Guy’s Hosp. Gaz., Lond., 1917, pp. 209-213.
Hurst, A. F. Classification of war neuroses. Guy’s Hosp. Gaz., Lond., 1917, xxi, 109. Also: Alienist and Neurol., St. Louis, 1917, xxxviii, 458.
Hurst, A. F. Etiology and treatment of war neuroses. Brit. Med. Jour., 1917, ii, 409.
Hurst, A. F. Psycho-analysis and war neuroses. Guy’s Hosp. Gaz., Lond., 1917, pp. 308-309.
Hurst, A. F. Syphilis of the nervous system in soldiers. Guy’s Hosp. Gaz., Lond., 1917, pp. 365-368.
Hurst, A. F. Warfare injuries and neuroses. Proc. Roy. Soc. Med., Lond., 1917-18, v. 10 (sec. otol.), pp. 115-118.
Hurst, Arthur F. Medical diseases of the war; a record of personal experiences. Hospital, Lon., 1918, lxv, 9.
Hurst, A. F. and Peters, E. A. The pathology, diagnosis and treatment of absolute hysterical deafness in soldiers. Lancet, Lond., 1917, v. ii, pp. 517-519.
Hurst, A. F. and Peters, E. A. Pathology, diagnosis, and treatment of absolute hysterical deafness in soldiers. Lancet, Lon., 1917, ii, 517.
Hurst, A. F. and Peters, E. A. Nerve-shattered soldiers and their treatment; Dr. Lumsden’s excellent scheme. Hospital, Lon., 1917, lxii, 487.
Hurst, A. F. and Syms, J. L. M. Rapid cure of hysterical symptoms in soldiers. Lancet, Lon., 1918, ii, 139.
Hutt, C. W. Education of the left hand of disabled sailors and soldiers. Lancet, Lond., 1917, v. 1, pp. 642-646.
Hutt, C. W. The future of the disabled soldier. Wm. Wood, 1917.
Hypertension des névroses tachycardiques. Rev. gén. de clin. et de thérap., Par., 1916, v. 30, pp. 185-186.
Hyslop, T. B. The psychology of warfare. West Lond., M. J., 1917, v. 22, pp. 2-12.
Imbert, Léon. Accidents du travail et blessures de guerre. Une nouvelle loi. Presse Méd., Par., 1917, v. 25, pp. 591-592.
Imbert, Léon, et Réal, Pierre. La constriction des machoires, par blessure de guerre. Presse méd., Par., 1916, v. 24, pp. 372-373.
Imboden, K. Das Neurosenproblem im Lichte der Kriegsneurologie. Cor. Bl. f. Schweiz. Aerzte., 1917, No. 34, pp. 1098-1109.
Isolation and Psychotherapy for soldiers suffering from functional disturbances of the nervous system. Monde méd., Par., 1917, v. 27, pp. 113-115.
Isserlin. Kriegspsychiatrische Erfahrungen. Berlin. klin. Wchnschr., 1916, v. 53, p. 295.
Jackson, J. A. A report of the clinical and pathological findings in a case of hystero-epilepsia and hystero-epileptoid. Alienist and Neurol., St. Louis, 1915, xxxvi, 231-235.
Jacob, O. Tumeurs consécutives à l’injection d’huile camphorée preparée avec de l’huile de vaseline. Compt. rend. Soc. de biol., Par., 1917, lxxx, 371, 487.
Jacobson, L. Krieg und Nervensystem. Therap. d. Gegenw., Berl., 1915, v. 56, pp. 22-29.
Jacobson, L. Krieg und Nervensystem. Med. Klin., Berl. u. Wien., 1915, v. 111, p. 110.
Jacquetty, G., Bergonié, J. Le travail agricole médicalement prescrit et surveillé comme traitement des séquelles de blessures de guerre. Arch. d’elec. méd. et physiothérap., Par., 1917, No. 148, pp. 297-317.
Jahrmärker. Ueber psychische u. nervöse Störungen bei Kriegern. München med. Wchnschr., 1915, No. 33, p. 1118.
Jarrett, Mary C. The Training School of Psychiatric Social Work at Smith College. V. An Emergency Course in a New Branch of Social Work. Mental Hygiene, II, October, 1918.
Jeanselme et Huet. Syndrome jacksonien de nature hystérotraumatique. Rev. neurol., Par., 1914-15, v. 222, pp. 723-726.
Jeanselme et Huet. Myotonie acquise. Rev. neurol., Par., 1916, v. 29. pp. 414-418.
Jelliffe, Smith Ely. Nervous and mental disturbances of influenza. N. Y. Med. Jour., 1918, cviii, 725, 755, 807.
Jelliffe, S. E. War (The) and the nervous system. I. Peripheral nerve injuries. N. Y. Med. Jour., 1917, cvi, 17.
Jellinek, S. Zur militärärztlichen Konstatierung der Epilepsie. Wien. klin. Wchnschr., 1915, v. 28, pp. 1021-1025.
Jellinek, S. Zur militärärztlichen Konstatierung der Kriegsneurosen. Wien. klin. Wchnschr., 1916, v. 29, pp. 189-193.
Jendrassik, E. Einige Bemerkungen zur Kriegsneurose. Neurol. Centralbl., Leipz., 1916, v. 35, No. 12.
Jendrassik. E. Zur Discussion über die Neurosenfrage. Theorie der Hysterie und der Neurasthenie. Neurol. Centralbl., Leipz., 1917, 36, 962.
Jessop, Walter, H. H. Discussion on ophthalmic injuries in warfare. Tr. Ophth. Soc. U. Kingdom, Lond., 1914-15, v. 35, pp. 1-68.
Jessop, Walter H. Shell shock without visible signs of injury. Proc. Roy. Soc. Med., Lond., 1915-16, v. 9 (sec. Psychiat.), p. 36.
Jobson, T. B. Normal gun-deafness. Lancet, Lon., 1917, ii, 566.
Johnstone, E. K. Shell Shock; notes. Mil. Surg., 1918, xlii, 531.
Jolly. Uber die Dienstfähigkeit und Rentenfrage bei nervenkranken Soldaten. München med. Wchnschr., 1915, v. 34, pp. 1714-1719.
Jolly, Ph. Arbeitstherapie für nervenkranken Soldaten. Deutsche med. Wchnschr., 1916, v. 42, p. 1514.
Jolly, P. Uber Kriegsneurosen. Arch. f. Psychiat., Berl., 1916, v. 56, pp. 385-444.
Joltrain, E. Camptocormie et paraplégie consécutives à un ensevelissement par éclatement d’obus. Presse méd., Par., 1917, v. 25, pp. 194-195.
Joltrain, E. Camptocormie et paraplégie consécutives à un ensevelissement par éclatement d’obus; considerations sur l’action due choc émotif. Bull. et mém. soc. méd. d’hôp. de Par., 1917, v. 41, pp. 431-436.
Jones, A. B. and Llewellyn, J. L. Malingering, or the Simulation of Disease. Lond., 1917, Wm. Heinemann.
Jones, I. H. Ear (The) and aviation. Jour. M. M. A., 1917, lxix, 1607.
Jones, Robert. Notes on Military Orthopedics. Cassell and Co., 1917.
Jones, Robert. Orthopedic surgery in its relation to the war. Amer. Jour. Care for Crip., 1917, vi, 119.
Jones, Robert. The Psychology of Fear and the Effects of Panic Fear in War Times. J. Ment. Sc., Lond., 1917, v. 63, pp. 346-389.
Jones, Robert. Notes on military orthopaedics. Lond., N. Y., etc., 1917, Cassell and Co., p. 132, 8o.
Jones, Robert. The orthopaedic outlook in Military Surgery. Brit. M. J., Lond., 1918, i, pp. 41-45.
Jones, W. E. Case of Shell Shock. M. J. Australia, Sydney, 1916, v. 1, pp. 203-204.
Jones-Phillipson, C. E. Special Discussion on Warfare Injuries and Neuroses. Proc. Roy. Soc. Med., Lond., 1917, v. 10 (sec. Otol.), pp. 96-110.
Jörger, J. Mobilmachung als krankheitsauslösendes Trauma bei Dementia Praecox. Cor.-Bl. f. Schweiz., Aerzte, 1914, v. 442, No. 50, pp. 1553-1570.
Joseph, E. Einige Erfahrungen über Schädelschüsse, besonders über die Bedeutung des Röntgenbildes für die Schädelchirurgie. Münch. Med. Woch., 1915, lxii, 1197.
Joubert, Camille. Note sur un cas de paraplégie organique consécutive à la déflagration d’un obus de gros calibre sans plaie extérieure. Paris méd., 1915 (Part. Méd.), v. 17, pp. 444-446.
Jourdan. Un cas d’oedème provoqué du membre inférieur. Montpel. méd., 1916, xxxix, 446-449.
Jourdan and Sicard. Étude macroscopique et microscopique des lésions des nerfs par blessure de guerre. Presse méd., July 29, 1915.
Jourdran, Maurice-Louise-Marie. Crises nerveuses chez les blessés de guerre crâniocérébraux. (Épilepsie généralisée, hystérie, hystéro-épilepsie). Bordeaux, 1917, 88 pp., 8, + No. 1.
Jourdran et Marchand, L. De la rage chez l’homme. Presse Méd., Par., 1917, v. 25, pp. 371-373.
Juliusburger, O. Zur Kenntnis der Kriegsneurosen. Monatschr. f. Psychiat. u. Neurol., Berl., 1915, v. 38, pp. 305-318.
Jumentié. Discussion de la conduite à tenir vis-à-vis des blessures du crâne—par P. Marie. Rev. neurol., Par., 1916, v. 29, p. 463.
Jumentié. Contraction neuro-musculaire et réflexes tendineux dans certains états d’impotence dits fonctionnels et à caractères psychonévrosiques. Étude par la méthode graphique. Rev. neurol., Par., 1916, No. 6, p. 960.
Jumentié. Deux cas d’hémiatrophie linguale associée à d’autres paralysies des nerfs crâniens et rachidiens chez des commotionnés. Montpel. med., 1917, xxxix, 1006-1009.
Juquelier, P. Un cas complexe d’appréciation de la résponsabilité pénale chez un épileptique. J. de méd. de Par., 1917, v. 36, pp. 47-48.
Juquelier, P., et Quellien, P. Épilepsie larvée par traumatisme de guerre (commotion cérébrale). Ann. méd. psychol. Par., 1917, v. 73, pp. 536-546.
Kafka, V. Fortschritte der für die Psychiatrie wichtigen biologischen, insbesondere serologischen Forschungsgebiete. Jahresb. f. Ärztl. Fortbild., München, 1915, v. 5, pp. 51-54.
Kafka. Schreckneurose. (Ärztl. Verein Hamburg, 26, Jan., 1915.) München. med. Wchnschr., 1915, v. 62, p. 198.
Kahne, Max. Über die Anwendung der physikalischen Heilmethoden bei Kriegskrankheiten. Wien. med. Wchnschr., 1914, v. 64, pp. 540-547.
Kahne, Max. Vorschläge zur Organisation der spezialärztlichen Dienstleistung in Kriegszeiten. Wien. klin. Wchnschr., 1914, ii, pp. 1262-1263.
Kahne, Max. Über Hyperthyreoidismus vom Standpunkte der Kriegsmedizin. Wien. klin. Wchnschr., 1915, v. 281, pp. 148-153.
Kalhof. Operierte Schädelschüsse. Ther. Monatschr., Berl., 1915, v. 29, pp. 450-453.
Kalt. Rapport sur les maladies simulées et les maladies provoquées. Clin. Ophth., Par., 1916, v. 21, pp. 500-504.
Karplus, I. P. Ueber Erkrankungen nach Granatexplosionen. Wien. klin. Wchnschr., 1915, v. 28, pp. 145-148.
Karplus, I. P. Ueber eine ungewöhnliche zerebrale Erkrankung nach Schrapnellverletzung. Neurol. Centralbl., Leipz., 1915, v. 34, pp. 456-462.
Kashtshenko, P. P. (Statistics of the movement of insane soldiers, according to data obtained by an inquiry.) Psikhiat. Gaz., Petrogr., 1915, v. 2, pp. 199-203.
Kashtshenko, P. P. (History of development of measures for the care of insane soldiers and those participating in military events.) Psikhiat. Gaz., Petrogr., 1916, v. 3, pp. 151-156.
Kashtshenko, P. P. (À propos of M. B. Krol’s article, “Statistics of the movement of insane soldiers, etc.”) Ibid., 1916, iii, 22, 43.
Kashtshenko, P. P. (Certain data concerning insane warriors, prepared by the combined Statistico-Psychiatrical Bureau of the Unions of Zemstvos and Municipalities.) Psikhiat. Gaz., Petrogr., 1916, v. 3, pp. 353-377.
Kastan, Max. Forensisch-psychiatrische Beobachtungen an Angehörigendes Feldheeres. Deutsche med. Wchnschr., Berl. u. Leipz., 1915, v. 41, pp. 734-737.
Kastan, Max. Die strafbaren Handlungen psychischkranker Angehöriger des Feldheeres. Archiv. f. Psychiat., Berl., 1916, pp. 573-631.
Kaufmann, Fritz. Die planmässige Heilung komplizierter psychogener Bewegungsstörungen bei Soldaten in einer Sitzung. Münch. med. Wchnschr., 1916, v. 631, pp. 802-804.
Keiper, G. F. Pretended blindness and deafness and their detection. J. Indiana M. Ass., Fort Wayne, 1917, x, 422-426.
Keith, John R. Vasodilators in the treatment of hysterical aphonia. Brit. M. J., Lond., 1915, i, p. 847.
Kennedy, F. Clinical observations on shell shock. Med. Rec., N. Y., 1916, v. 89, p. 388.
Kennedy, Foster. Nature of nervousness in soldiers. Jour. A. M. A., 1918, lxxi, 17.
Kenyon, E. L. The stammerer and army service. J. Am. M. Ass., Chicago, 1917, v. 69, p. 664.
Khoroshko, V. K. (Psychiatric impressions and observations in the regions of the active army.) Psikhiat. Gaz., Petrogr., 1915, v. 2, pp. 377-383.
Khoroshko, V. K. (Mental disturbances following physical and mental shock in the war; traumatic psychoses in the active army.) Psikhiat. Gaz., Petrogr., 1916, v. 3, pp. 3-10.
Khoroshko, V. K. (Organization of aid to warriors with wounded or diseased nervous system.) Psikhiat. Gaz., Petrogr., 1916, v. 3, pp. 398-401.
Kidner, E. B. The vocational reëducation of the disabled soldier. Am. Med., Burlington, Vt., 1917, v. 23, pp. 405-408.
Kinberg, O. (Psychoneuroses in soldiers at the front.) Hygiea, Stockholm, 1916, v. 78, pp. 97-126.
Kindlmann. Entlarvung von Taubheit und Schwerhörigkeit Simulierenden. Wien. klin. Wchnschr., 1915, v. 28, p. 1069.
Kirmsze, M. Geistesschwäche als Helden. Ztschr. f. d. Behndl., Schwachsinn. u. Epilept., Dresd., 1915, No. 9, pp. 134-141.
Kleist. Schreckpsychosen. Neurol. Centralbl., 37, Nr. 16, 1918.
Kluge, O. Hysterische Seh- und Hröstörungen bei Soldaten; (Inaug. Dissert., Berl., 1914). Rev. Neurol. Centralbl., Leipz., 1915, v. 34, p. 735.
Knapp, Paul. Kriegschädigungen der Sehorgane. Cor.-Bl. f. Schweizer Aerztl., 1916, Nr. 38, pp. 1185-1201.
Koblylinsky, M. La psichiatria e la guerra. Quaderni di psichiat., Genova, 1914, i, pp. 337-341.
Kofler. Fall von hysterischer Gehstörung nach Schussverletzung des Unterschenkels. Wien. med. Wchnschr., 1915, No. 1, p. 39.
Kouindjy, P. Le massage méthodique chez les blessés de guerre. Presse méd., Par., 1914, v. 22, pp. 610-611.
Kouindjy, P. La rééducation chez les blessés de la guerre et le rôle de la suppléance. Bull. Acad. de méd., Par., 1915, 3 s., v. 74, pp. 105-108.
Kouindjy, P. La rééducation des mouvements chez les blessés de guerre. Paris méd., 1915-16, v. 17, pp. 298-302.
Kouindjy, P. La kinésithérapie de guerre. Paris, 1916, A. Maloine and Fils.
Krebs. Ohrbeschädigungen im Felde. Münch. med. Wchnschr., 1915, v. 62, pp. 347-349.
Kreuser, D. Zur Frage der Kriegspsychosen. Allg. Ztschr. Psychiat., 74, 1918.
Krieg und Wahnsinn. Psychiat. Neurol. Wchnschr., Halle a. S., 1914-15, v. 16, p. 298.
Krol, M. B. (Statistics of the movement of insane soldiers; Apropos of P. B. Kashtshenko’s article: “Statistics of the movement of insane soldiers, etc.,”) Psikhiat. Gaz., Petrogr., 1915, v. 2, pp. 287-291.
Krüche, A. Zur medico-mechanischen Nachbehandlung der verwundeten Krieger. Aerztl. Centralbl. Ztg., Wien., 1915, v. 27, pp. 43-45.
Krückmann, E. Ueber Kriegsblindenfürsorge. Deutsche med. Wchnschr., Leipz. u. Berl., 1915, v. 41, p. 725; p. 763; p. 788.
Krüll. M. Die Strafrechtliche Begutachtung der Soldaten im Felde. Berl. klin. Wchnschr., Nr. 24, 1918.
Kuehn, A. Ueber functionelle Erkrankungen des Nervensystems bei Kriegsteilnehmern. Ztschr. f. Med. Beamte, Berl., 1917, 30, 497.
Laborderie, J. La mécanothérapie dans les formations sanitaires. Rev. gén. de clin. et de thérap., Par., 1915, v. 29, p. 327.
Lagrange. Des désordres oculaires médiats ou indirects par les armes à feu. Bull. Acad. de méd., Par., 1915, v. 73, pp. 591-601.
Lagrange, Félix. Les fractures de l’orbite. Paris, 1917, Masson and Cie.
Lahy, J. M. Sur la psycho-physiologie du soldat mitrailleur. Compt. rend. Acad. d. sc., Par., 1916, v. 163, pp. 33-35.
Laignel-Lavastine. Diagnosis and treatment of war psychoneuroses, especially with reference to cases of convulsions and asthenia. War Med., 1918, ii, 44.
Laignel-Lavastine. Rapport sur le centre neurologique de la Ire région. Rev. neurol., Par., 1914-15, v. 222, p. 1165.
Laignel-Lavastine. Discussion de la conduite à tenir vis-à-vis des blessures du crâne—par P. Marie. Rev. neurol., Par., 1916, v. 29, p. 472.
Laignel-Lavastine. Sur les accidents nerveux determinés par la déflagration de fortes charges d’explosifs. Rev. neurol. Par., 1916, v. 29, pp. 595-596.
Laignel-Lavastine. Sur la relative fréquence des cas de peur invincible, chez les combattants. Ann. med.-psychol., Par., 1917, v. 73, pp. 380-384.
Laignel-Lavastine. Centre des psychonévroses du gouvernement militaire de Paris. Rev. neurol., Par., 1916, xxiii, 649-656.
Laignel-Lavastine et Ballet, V. “Pseudo-ptosis hystérique” avec synergie fonctionnelle oculo-palpébrale. Rev. neurol., Par., 1916, v. 29, pp. 179-181.
Laignel-Lavastine et Ballet, Victor. Maniérisme puéril post-confusionnel. Ann. méd.-psychol., Par., 1917, v. 23, pp. 232-240.
Laignel-Lavastine et Courbon, Paul. Camptodactylie, causalgie et inversion du reflexe tricipital par lesion de la VII paire cervicle. Rev. neurol., Par., 1916, v. 29, pp. 927-932.
Laignel-Lavastine et Courbon, Paul. Amaurose par éclatement d’obus avec meningite syphilitique. (Présentation de malade.) Rev. neurol., Par., 1916, v. 24, pp. 402-405.
Laignel-Lavastine et Courbon, Paul. Les déviations de la colonne vertébrale: le Campto-Rachis. Rev. gén. de pathol. de guerre, Par., 1916, No. 1, pp. 1-18.
Laignel-Lavastine et Courbon, Paul. Les troubles de la marche consécutives aux émotions et commotions de la guerre. Paris méd., 1916, v. 21, pp. 194-203.
Laignel-Lavastine et Courbon, P. Stéréotypies de la marche, de l’attitude et de la mimique avec représentation mentale professionnelle de l’ouie consécutives aux émotions du champ de bataille. Ann. méd.-psychol., Par., 1916-17, v. 7, pp. 498-505.
Laignel-Lavastine et Courbon, P. De la simulation des troubles fonctionnels du système nerveux par les débiles mentaux. Ann. méd.-psychol., Par., 1916-17, v. 7, pp. 512-519.
Laignel-Lavastine et Courbon, P. Trois dysbasies différentes consécutives à des blessures de la région du tenseur du fascia lata (Essai de physiologie pathologique neuro-musculaire). Rev. neurol., Par., 1917, v. 24, pp. 221-224.
Laignel-Lavastine et Courbon, P. Syndrôme sympathique cervical oculaire de paralysie avec hémianidrose cervico-faciale et aphonie hystérique par blessure cervicale droite. Rev. neurol., Par., 1917, v. 24, p. 509.
Laignel-Lavastine et Courbon, P. Féminisme post-ourlien (microrchidie et gynécomastie consécutives à une orchite double). Presse méd., Par., 1917, v. 25, p. 492.
Laignel-Lavastine et Courbon, P. Essai sur l’insincérité chez les accidentés de la guerre. Paris méd., 1917, No. 27, pp. 14-19.
Laignel-Lavastine et Courbon, P. Prophylaxie et traitement de l’insincérité chez les accidentés de la guerre. Paris méd., 1917, No. 46, pp. 407-410.
Laignel-Lavastine et Courbon, P. Syndrôme psychasthénique consécutif aux émotions de guerre. Ann. méd.-psychol., Par., 1917, v. 73, pp. 391-403.
Laignel-Lavastine et Courbon, P. États seconds cataleptiformes post-confusionnels par émotion-choc de guerre. Ann. méd.-psychol., Par., 1917, v. 73, pp. 411-422.
Laignel-Lavastine et Courbon, P. Psychasthénie acquise. Ann. méd.-psychol., Par., 1917, v. 73, pp. 582-588.
Laignel-Lavastine et Fay, H. M. Psychogénèse d’une crise hystérique. Ann. méd.-psychol., Par., 1917, v. 73, pp. 422-425.
Landau. Le principe de l’isolement psychique dans le traitement des troubles nerveux fonctionnels. Presse méd., Par., 1916, v. 25, p. 312.
Landau. Le principe de l’isolement psychique dans le traitement des “troubles nerveux fonctionnels” de guerre. Bull. Acad. de méd. de Par., 20 juin 1917, v. 31, p. 236, No. 23.
Lande, P. et Marguery, F. Contribution à l’étude expérimentale de l’ictère simulé picrique. J. de méd. de Bordeaux, 1917, v. 88, pp. 277-280.
Landolt, Marc. Les troubles de la vision nocturne chez les soldats. Arch. d’ophth., Par., 1917, v. 35, pp. 580-605.
Lannois (avec M. Chavanne). Des surdités totales par éclatement d’obus. Bull. Acad. de Méd., Par., 1915, v. 73, pp. 105-108.
Lannois et Chavanne. Des surdités totales par éclatement d’obus. J. méd. et de chir., 1915, v. 86.
Lannois et Chavanne, F. Le pronostic des surdités de guerre (d’après 1000 cas). Rev. Paris, méd. (Part. méd.), v. 19, p. 36.
Lannois, M. et Chavanne, F. Le pronostic des surdités de guerre (d’après 1000 cas.). Lyon méd., 1916, v. 125, pp. 35-40.
Lannois et Chavanne, F. La surdité de guerre bilatérale totale. Rééducation auditive ou lecture sur les lèvres? Lyon méd., 1916, v. 125, pp. 479-487.
Lannois et Chavanne. Rééducation auditive ou lecture sur les lèvres dans la surdité bilatorale totale. J. d. méd. Par., 1917, pp. 114-115.
Laquerrière, A. Notes sur l’électro-diagnostic de guerre. J. de radiol. et d’électrol., Par., 1916, v. 2, pp. 19-30.
Laquerrière, A. L’électricité dans la rééducation des troubles névropathiques des blessés de guerre. J. de radiol. et d’électrol., Par., 1917, v. 2, pp. 459-467.
Laquerrière et Peyre. La physiothérapie préventive dans les blessures de guerre. J. de méd. et de chir., 1915, v. 86. June.
Larat et Billiard. L’électrothérapie pendant la rééducation professionnelle. Arch. d’élect. méd. et de physiothérap., Par., 1917, No. 418, pp. 335-336.
Larat, J. et Billiard, A. Électricité médicale et rééducation professionnelle. Paris méd., 1917, No. 43, pp. 344-347.
Larat, J. et Lehmann, P. Traitement électrique simplifié des accidents nerveux consécutifs aux blessures de guerre. Presse méd., Par., 1915, v. 23, pp. 35-37.
Lattes, L. I semi-alienati in medicina legale militare e il concetto di pericolosità. Riv. di méd. leg., Pisa, 1917, vii, iv, 49.
Laudenheimer. Die Anamnese der sogenannten Kriegspsychoneurosen. München. med. Wchnschr., 1915, v. 62, pp. 1302-1304.
Laurent, O. Accidents nerveux produits à distance par les projectiles de guerre. Compt. rend. acad. d. sc., Par., 1914, v. 158, pp. 1211-1213.
Lautier-Jean, H. M. A. Contribution à l’étude des maladies mentales dans l’armée. Peut-on utiliser les imbéciles? Thèses de Paris, 1915-1916, v. 8.
Lautier, J. Médecine mentale de guerre. Presse méd., 1917, v. 25, p. 492.
Lautier. J. Un cas de délire mystique chez un Musulman. Ann. méd.-psychol., Par., 1917, v. 73, pp. 404-411.
Lattes, Leone, e Goria, Carlo. Alcune considerazioni attorno alle psiconeurosi d’origine bellica. Arch. di antrop. crim. (etc.), Torino, 1917, v. 38, pp. 97-117.
Laval, E. Des abcès par injection de pétrole. Bull. et mém. Soc. de chir. de Par., 1915, n. s., xli, 2378-2382. Also: Bull. méd., Par., 1916, xxx, 94-96.
Lawson, A. Blinded sailors and soldiers; remarks on the training at St. Dunstan’s. Lancet, Lond., 1917, v. 1, p. 223.
Lawson, A. How blinded soldiers are cared for. Hospital, Lon., lxi, 319.
Lawson, A. Making the unfit into serviceable recruits. Hospital, Lon., lix, 390.
Lebar. Sur un cas de canitie rapide. Bull. et mém. soc. méd. d’hôp. de Par., 1915, v. 39, pp. 439-443.
Lebar. Sur l’oedème hystérique. Bull. et mém. soc. méd. d’hôp. de Par., 1915, v. 39, pp. 757-760.
L’école de rééducation professionelle et les œuvres d’assistance pour les mutilés à Bordeaux. J. de méd. de Bordeaux, 1915-1916, v. 45, pp. 139-141.
LeClerc et Tixier. Un cas de paralysie totale du plexus brachial droit compliquée de paraplégie spasmodique produite par le même-projectile. Lyon méd., 1916, v. 125, pp. 196-199.
Le Damany, P. La paralysie du facial supérieur dans l’hémiplégie cérébrale. Presse méd. Par., 1917, v. 25, pp. 1-3.
Le Dantec. Rééducation et auto-rééducation des blessés de guerre. J. de méd. de Bordeaux, 1917, v. 88, pp. 219-224.
Ledoux-Lebard, R., Chabaneix, Dessane. L’importance des variations du squelette dans le diagnostic radiologique des blessures de guerre. J. de radiol. et électrol., 1914-15, v. 1, pp. 689-693.
Lee, John R. A case of gunshot wound of the head with a piece of shrapnel in the brain; value of the use of an electric magnet and x-ray screen for removal. J. Roy. Army Med. Corps, London, 1916, v. 26, pp. 105-106.
Leeson, C. The war and juvenile delinquency. Pub. for Howard Ass. of Lond., by P. S. King and Son, Ltd., 1917. (1 s. net.)
Le Fur, René. Abcès du cerveau (lobe temporal), consécutif à une plaie par éclat d’obus en avant de l’oreille. Paris Chirur., 1916, v. 8, pp. 276-278.
Legros. L’électrothérapie de guerre. Paris, 1916, A. Maloine et fils.
Legueu, F. Battlefield urology; urinary and vesical psychoses in the fighting line. Med. Press and Circ., Lond., 1915, n. s., v. 100, p. 11.
Legueu, F. De l’incontinence d’urine et des psychoses vésicales chez les combattants. Bull. Acad. de Méd., Par., 1915, v. 73, pp. 314-315.
Leitner, P. Wien. klin. Wchnschr., 1917, 30, 1327-28.
Lelong, Marcel. Quelques formes de la fatigue à l’avant. Paris méd., 1917, No. 3, pp. 66-68.
Lemon, Felix. Functional cases. Discussion. Proc. Roy. Soc. Med., Lond., 1914-15 (Sect. Laryncol.), v. 8, p. 117.
Lenoir, R. Contribution à l’étude des phénomènes psychologiques et physiologiques observés pendant la narcose. Rev. neurol., 1914-15, v. 2211, p. 1310.
Lents, A. (The war and hysterical stigmata.) Psikhiat. Gaz., Petrogr., 1915, v. 2, pp. 152-155.
Lenz. La guerre et les stigmates hystériques. Gazette psychiatrique (russe), 1915.
Lépine, Jean. Troubles mentaux de guerre. Collection Horizon, Masson et Cie, Paris, 1918.
Lépine, Jean. Commotions nerveuses à la suite d’explosions. Rev. Paris méd. (Part. méd.), 1916, v. 21, p. 67.
Lépine, J. Discussion de la conduite à tenir vis-à-vis des blessures du crâne—par P. Marie. Rev. neurol., Par., 1916, v. 29, p. 473.
Lépine, J. Centre de psychiatrie de la 14e région. (Lyon). Rev. neurol., Par., 1916, xxiii, 698-701.
Lépine, J. La commotion des centres nerveux par explosion. Bull. acad. de méd. de Par., 1916, v. 75, pp. 9-11.
Lépine J. La commotion des centres nerveux par explosion. Lyon méd., 1916, v. 125, pp. 181-182.
Lépine, J. Réformes, incapacités, gratifications dans les psychoses. Ibid., 803-809.
Lépine J. Troubles mentaux de guerre. Les solutions militaires. Presse méd., Par., 1917, v. 25, pp. 659-663.
Leplat, Georges. Note sur un cas de troubles oculaires produits à distance par une explosion. Arch. méd. Belges, Brux., 1917, v. 47, pp. 412-415.
Leppmann. Psychiatrische und nervenärztliche Sachverständigentatigkeit im Krieg. Deutsche med. Wchnschr., Berl. u. Leipz., 1915, v. 41, p. 209.
Lerda, G. Contributo alla conoscenza delle suppurazioni da benzina. Gior. di med. mil., Roma, 1916, lxiv, 586-590.
Lereboullet. Spasmes consécutifs à la paralysie faciale. Rev. gén. de clin. et de thérap., Par., 1917, v. 31, p. 294.
Lereboullet, P. et Mouzon, J. Hallucinations de la vue et crises jacksoniennes dans un cas de lésion du cortex visuel. Paris méd., 1917, No. 27, pp. 19-23.
Leredu. Réponse du ministre de la guerre au sujet de l’envoi en convalescence des aliénés militaires guéris et fortunes en cas de refus par leur famille de les recevoir. Soc. de méd. Lég. de France, Bull. Par., 1916, v. 13, pp. 179-180.
Léri, André. Commotions et Émotions de guerre. Collection Horizon, Masson et Cie, Paris, 1917.
Léri, André. Sur les pseudo-commotions ou contusions médullaires d’origine fonctionelle. Rev. neurol., Par., 1914-15, v. 222, pp. 433-436.
Léri, A. L’électrisation directe des troncs nerveux au cours des interventions pour blessures des nerfs, ses données pratiques. Paris méd., 1915 (Part. Méd.), v. 17, pp. 134-138.
Léri, A. Hémorragie de la couche optique par commotion pure. Hémiplégie avec hémianesthésie à type cérébral. Soc. méd. d’hôp., Par., 26 mai, 1916.
Léri, A. Hémorragie de l’épicone médullaire par commotion (éclatement d’obus à proximité). Rev. neurol., Par., 1916, v. 23, pp. 133-135.
Léri, A. Discussion de la conduite à tenir vis-à-vis des blessures du crâne—par P. Marie. Rev. neurol., Par., 1916, v. 29, pp. 466-469.
Léri, A. Sur les accidents nerveux determinés par la deflagration de fortes charges d’explosifs. Rev. neurol. Par., 1916, v. 29, pp. 586-587.
Léri, A. Réformes, incapacités, gratifications, dans les névroses de guerre. Rev. neurol., Par., 1916, xxiii, pp. 763-766.
Léri, A. A propos de l’hystérie. Sur un cas d’hémianesthesie organique presque pure. Paris méd., 1916 (Part méd.), v. 19, pp. 531-534.
Léri, A. Les commotions des centres nerveux par éclatement d’obus. Rev. gén. de. path. de guerre, 1916, No. 2, pp. 169-212.
Léri, A. Épilepsie jacksonienne par “vent d’obus” (hémorragie corticale probable). Presse méd., Par., 1916, v. 24, p. 96.
Léri, A. Traumatisme du crâne; hémiparésie droite, grosse hémiatrophie post-hémiplégique avec hémiatrophie linguale homolatérale; syndrôme protubérantiel probable. Rev. neurol., Par., 1917, v. 24, pp. 561-563.
Léri, A. Procédé bi-photographique pour mesurer l’évolution progressive ou régressive des paralysies et pour étudier les mouvements des membres. Rev. neurol., Par., 1917, v. 24, pp. 563-564.
Léri, A. Émotions et commotions de guerre. Collection Horizon, Masson et Cie, 1918.
Léri, A. and Dagnan-Bouvert. Soc. de Neurol. May 6, 1915. Rev. Neurol., July, 1915.
Léri, Froment et Mahar. Atrophie musculaire et déflagration d’obus sans traumatisme apparent. Rev. neurol., 1914-15, v. 222, p. 754.
Léri, A. et Roger, Édouard. Sur la pathogénie de certains oedèmes soi-disant traumatiques. Rev. neurol., Par., 1914-15, v. 222, pp. 756-759.
Léri, A. et Roger, É. Sur quelques variétés de contractures post-traumatiques et sur leur traitement. Bull. et mém. soc. méd. d’hôp. de Par., 1915, v. 39, pp. 885-8941.
Léri, A. et Schaeffer, H. Hématobulbie par commotion; survie; syndrôme bulbaire complexe. Soc. méd. d’hôp., Par., 1916, 26 mai.
Léri et Schaeffer. Hémorragies du nevraxe par commotion. Presse méd., Par., 1916, v. 24, p. 351.
Léri, A. et Schaeffer. Un cas de lésion bulbo-médullaire par commotion due à un éclatement d’obus hématobulbie probable survie avec syndrôme bulbaire complexe. Rev. neurol., Par., 1917, v. 24, pp. 1-8.
Lériche, René. De la causalgia envisagée comme une névrite du sympathique et de son traitement par la dénudation et l’ablation des plexus nerveux péri-artériels. Soc. de Neurol., 6 janvier 1916.
Lériche, R. Des lésions cérébrales et médullaires produites par l’explosion à faible distance des obus de gros calibre. Lyon chirurg., 1915, v. 12, pp. 343-350.
Lériche, R. Des petites plaies du crâne par éclates d’obus et de bombes sans pénétration du projectile et des lésions nerveuses que les accompagnent. Lyon chirurg., 1915, v. 12, pp. 293-342.
Lériche, R. De la sympathectomie péri-artérielle et de ses résultats. Presse méd., Par., 1917, v. 25, pp. 513-515.
Lermoyez, Marcel. La surdité de guerre. Presse méd., Par., 1915, v. 23, pp. 57-59.
Leroy. Sur les accidents nerveux determinés par la déflagration de fortes charges d’explosifs. Rev. neurol. Par., 1916, v. 29, pp. 595-597.
Lesieur et Peuret, A. L’insomnie nerveuse dite essentielle et son traitement médicamenteux. Caducée, Par., 1917, v. 17, p. 96; Bull. méd., Par., 1917, v. 31, pp. 12-13.
Lesions of peripheral nerves resulting from war injuries: Pathology and treatment. Brit. Med. Jour., 1918, i, 379, 408.
Lévy, L. Note sur les renseignements cytologiques donnés par la ponction lombaire au cours de l’évolution des blessures du crâne. Lyon chirurg., 1916, v. 13, pp. 428-433.
Lévy, R. Ueber die Resultate der Kaufmann’schen Behandlung. Münch. med. Wchnschr., 1917, v. 64, No. 6.
Lévy-Valensi, J. Notes sur quelques faits cliniques. Presse méd., 1915, v. 23, pp. 179-181.
Levy-Bing et Gerbay. Epilepsia syphilitica. Ann. d. mal. vén., Par., 1917, 12, 265-8.
Lewandowsky, M. Die Kriegsverletzungen des Nervensystems. Berl. klin. Wchnschr., 1914, v. 51, pp. 1929-1934.
Lewandowsky, M. Ueber Kriegsverletzungen des Nervensystems. 1. Gehirnschüsse. 2. Rückenmarksverletzungen. 4. Hysterie. Neurol. Centralbl., Leipz., 1915, v. 34, pp. 47-48.
Lewandowsky, M. Kriegsverletzungen des Nervensystems. Deutsche med. Wchnschr., Berl. u. Leipz., 1915, v. 41, pp. 29.
Lewandowsky, M. Erfahrungen über die Behandlung nervenverletzter und nervenkranker Soldaten. Deutsche med. Wchnschr., Berl. u. Leipz., 1915, v. 41, pp. 1565-1567.
Lewandowsky, M. Familiäre Kältelähmung. Berl. klin. Wchnschr., 1916, No. 5, pp. 120.
Lewandowsky, M. Ein Fall von Rindenepilepsie und Rindenschwäche. Aerztl. Sachvert. Ztg., Berl., 1916, No. 3. Rev. Berl. klin. Wchnschr., 1916, No. 12, p. 316.
Lewis, E. R. Influence of altitude on the hearing and the motion-sensing apparatus of the ear. Jour. A. M. A., 1918, lxxi, 1398.
Lewis, Thomas. Observations upon Prognosis: “Irritable heart of soldiers.” Lancet, Lond., 1918, i, pp. 181-183.
Lewis, Thomas. Tolerance of physical exertion, as shown by soldiers suffering from so-called “irritable heart.” Brit. Med. Jour., 1918, i, 363.
Lewitus. Ein seltener Simulationsfall. Wien. med. Wchnschr., 1915, No. 24, p. 925.
Lhermitte, J. Hémiplégie secondaire aux blessures du crâne. Rev. neurol., Par., 1916, v. 24, pp. 807-813.
Liébault, G. Les troubles de la parole et les commotions de guerre. Rev. gén. de path. de guerre, 1916, No. 3, pp. 245-269.
Liebers, M. Zur Behandlung der Zitterneurosen nach Granatschock. Neurol. Centralbl., Leipz., 1916, v. 35, No. 21.
Liebl. Ein charakteristisches künstlich erzeugtes Geschwür. Wien. klin. Wchnschr., 1916, xxix, 1305.
Liepmann, H. Psychiatrisches aus dem Russ.-Jap. Feldzug. Deutsche med. Wchnschr., Berl. u. Leipz., 1914, v. 40, pp. 1823.
Liepmann, H. Zur Fragestellung in dem Streit über die traumatische Neurose. Neurol. Centralbl., Leipz., 1916, v. 35, No. 6.
Loeper, M. et Carlotti, J. Pustule maligné des paupières a guérison rapide. Progrès méd., Par., 1916, No. 3, pp. 17-19.
Loeper, M. and Verpy, G. Les troubles vasculaires et hématiqués de la commotion. Compt. rend. Soc. de biol., Par., 1916, lxxix, pp. 831-833.
Loeper, M. et Verpy, G. La répercussion glandulaire et humorale des commotions. Progrès méd., Par., 1916, v. 21, pp. 202-205.
Logre, M. Début de paralysie générale avec tabes par des crises de poltronnerie avec incontinence d’urine. Presse méd., Par., 1917, v. 25, p. 395.
Lollet. Discussion de la conduite à tenir vis-à-vis des blessures du crâne—par P. Marie. Rev. neurol., Par., 1916, v. 29, p. 470.
Lombard et Baldenweck. Traitement de quelques cas de mutité hystérotraumatique par le procédé de la suppression de contrôle auditif de la voix (méthode de Lombard). Presse méd., Par., 1915, v. 23, p. 338.
London War Hospitals. Boston M. and S. J., 1917, i, pp. 222-223.
Long, E. Radiculite lombo-sacrée (sciatique radiculaire) d’origine syphilitique. Rev. neurol. Par., 1916, v. 29, pp. 298-300.
Loreta, U. Per l’applicazione di esami psicologici nell’ esercito. Policlin., Roma, 1915, c. 17, sez. prat., pp. 1298-1300.
Lortat-Jacob. Le syndrôme des éboulés. Rev. neurol. Par., 1914-15, v. 222, pp. 1173.
Lortat-Jacob. Discussion de la conduite à tenir vis-à-vis des blessures du crâne—par P. Marie. Rev. neurol., Par., 1916, v. 29, p. 470.
Lortat-Jacob. Sur les accidents nerveux déterminés par la déflagration de fortes charges d’explosifs. Rev. neurol. Par., 1916, v. 29, pp. 590-591.
Lortat-Jacob et Buvat, J. B. Sur un procédé de guérison des sourds-muets par commotion. Bull. et mém. de soc. méd. d’hôp. de Par., 1916, pp. 169-176; Rev. Paris méd., 1916 (Part. méd.), v. 19, p. 226.
Lortat-Jacob et Sézary. Synesthésialgie et blessure du sciatique. Rev. neurol., 1914-15, v. 222, pp. 1277-1278.
Lortat-Jacob et Sézary. Maladie de Thomsen. Rev. neurol., Par., 1916, v. 23, pp. 15-18.
Lortat-Jacob et Oppenheim, R. Hémiplegie post-scarlatineuse. Progrès méd., Par., 1916, pp. 213-215.
Lortat, Jacob et Oppenheim, R. et Tournay, A. Topographie des modifications de la sensibilité au cours des troubles physiopathiques; constitution d’un syndrôme radiculo-sympathique réflexe. Progrès méd., Par., 1917, No. 10, pp. 77-81.
Love, K. Hearing in the Army. J. Roy. Army Med. Corps, Lond., 1915, v. 27, pp. 652-654.
Löwenfeld. Über den französischen Nationalcharakter und seine Auswüchse im gegenwärtigen Kriege (Psychopathia gallica). Allgem. Zeitschr. f. Psychiat., Wiesbaden, 1914.
Löwenstein, Kurt. Zerebellare Symptomenkomplexe nach Kriegsverletzungen. Neurol. Centralbl., Leipz., 1915, v. 34, pp. 626-637.
Löwenstein, Sally. Zur traumatischen Entstehung chronischer Rückenmarksleiden. Neurol. Centralbl., 37, Nr. 16, 1918.
Löwy, Max. Neurologische und psychiatrische Mitteilungen aus dem Kriege. Monatschr. f. Psychiat. und Neurol., Berl., 1915, v. 37, pp. 380-388.
Löwy, Julius. Über die Beeinflussung von Erkrankungen des Nervensystem durch den Apparat von Bergonié. Ztschr. f. Phys. u. Diätet. Therap., Leipz., 1915, No. 9, pp. 272-276.
Lumière, Auguste et Astier. Cerebral troubles in tetanus. Monde Méd., Par., 1917, v. 27, pp. 101-105.
Lumsden, T. The psychology of malingering and functional neuroses in peace and war. Lancet, Lond., 1916, ii, pp. 860-862. Rev. Boston M. and S. J., 1916, ii, p. 8.
Lumsden, T. Treatment of war neuroses. Lancet, Lond., 1917, ii, p. 804.
Lumsden, T. Shell Shock. (A letter.) Lancet, Lond., 1917, i, p. 34.
Lumsden’s scheme for treatment of nerve-shattered soldiers. Hospital, Lond., 1917, v. 61, pp. 487-488.
Lust, F. Kriegsneurosen und Kriegsgefangene. Münch, med. Wchnschr., 1916, v. 63, p. 1829.
Lyonnet. Un cas de paraplégie d’origine cérébrale. Lyon méd., 1915, v. 124, pp. 362-363.
Lyle, H. H. M. Physiological treatment of bullet and shell wounds of the peripheral nerve trunks. S. G. O., 1916, xxii, 127.
Lyristritski, V. V. (Psychical symptoms, difficult to simulate). Psikhiat. Gaz., Petrogr., 1915, v. 2, pp. 121-124.
MacAuliffe, Léon. Evolution de l’état commotionnel chez les blessés du crâne trépanés. Paris méd., 1917, No. 47, pp. 421-424.
MacCurdy, John T. The Psychology of War. Wm. Heinemann, 1917.
MacCurdy, John T. War Neuroses. Cambridge Univ. Press, 1918.
MacCurdy, John T. War neuroses. Psychiat. Bull., Utica, 1917, v. 2, No. 3, pp. 243-254.
Macdonald, W. M. Contractions of the hand after wounds of the upper limb. Brit. M. J., Lond., 1916, ii, pp. 209-212.
MacDonald, W. M. Tinel’s sign in peripheral nerve lesions. Brit. Med. Jour., 1918, ii, 6.
Mackenzie, W. C. Military orthopaedic hospitals. Brit. M. J., Lond., 1917, v. 1, pp. 669-678.
MacKenzie, Kenneth A. J. Repair of large gaps in peripheral nerves by neuroplasty. Surg. Gynecol. and Obstet., 1918, xxvii, 355.
MacLeod, Kenneth. Dreaming. Med. Press and Circ., Lond., 1916, v. 102, pp. 98-100.
MacMahon, Cortlandt. Shell shock, stammering and other affections of voice and speech. J. Roy. Army Med. Corps, Lond., 1917, v. 39, pp. 192-201.
Madelung. Kriegsärztliche Erfahrungen im England und Frankreich. Münch. med. Wchnschr., v. 621, pp. 283-284.
v. Maiendorf. Über Kriegsneurosen. Wien. klin. Wchnschr., 1915, v. 381, pp. 79-80.
Mairet, A. et Durante, G. Contribution à l’étude expérimentale du syndrôme commotionnel. Rev. neurol., Par., 1917, v. 24, pp. 456-466.
Mairet, A. et Durante, G. Étude expérimentale du syndrôme commotionnel. Presse méd., Par., 1917, v. 25, p. 478.
Mairet et Piéron. Les troubles de mémoire d’origine commotionnelle. J. de psychol. norm, et path., Par., 1915, v. No. 2, pp. 300-328.
Mairet et Piéron. Accès épileptiques determinés par une irritation nerveuse périphérique. Rev. Paris méd., 1916 (Part méd.), v. 19, p. 178.
Mairet et Piéron. De la differenciation des symptômes “commotionnels” et des symptômes “atypiques” dans les traumatismes cranio-cérébraux. Montpel. méd., 1916, v. 39, p. 174.
Mairet et Piéron. De quelques problèmes posés par la neuropsychiatrie de guerre au point de vue des réformes. Montpel. méd., 1916, v. 39, pp. 387-402.
Mairet, A. et Piéron, H. Syndrôme épileptique par irritation nerveuse périphérique ou “Epilepsie de Brown-Séquard.” Bull. acad. de méd., Par., 1916, v. 75, pp. 80-90.
Mairet, A. et Piéron, H. De quelques problèmes posés par la neuropsychiatrie de guerre au point de vue des réformes. Paralysies générales, crises d’épilepsie apparues ou aggravées, accès de somnambulisme, accidents après vaccination antityphoidique. Rev. neurol., Par., 1917, v. 24, pp. 89-98.
Mairet et Piéron. Le syndrôme émotionnel. Sa différenciation du syndrôme commotionnel. Rev. neurol., Par., 1917, v. 24, pp. 474-475.
Mairet, A. and Piéron, H. Le syndrôme commotionnel. Ibid., p. 345.
Mairet, A. et Piéron, H. Le syndrôme émotionnel; sa différenciation du syndrôme commotionnel. Montpel. méd., 1917, v. 39, pp. 581-599.
Mairet, A. et Piéron, H. Le syndrôme emotionnel: sa différenciation du syndrôme commotionnel. Ann. méd.-psychol., 1917, v. 73, pp. 183-206.
Mairet, A. et Piéron, H. et Mme. Bouzansky. De l’existence d’un “syndrôme commotionnel” dans les traumatismes de guerre. Bull. de acad. de méd., Par., 1915, v. 73, pp. 654-661.
Mairet, Piéron et Bouzansky. Des variations du “syndrôme commotionnel,” suivant la nature des traumatismes, et de son unité. Bull. de l’acad. de méd., Par., 1915, v. 73, pp. 690-700.
Mairet, Piéron et Bouzansky. Le “syndrome commotionnel” au point de vue du mécanisme pathogénique et de l’évolution. Bull. de acad. de méd., Par., 1915. v. 73, pp. 710-716.
Mahomet. Treatment by physical methods of mental disabilities induced by the war. Proc. Roy. Soc. Med., Lond., 1917-18, v. 10, (sect. Balneol.), p. 42.
Maitland, T. J. Accumulated fatigue in warfare. (2nd int. rep., Brit. Ass. Comm.) Lancet, Lond., 1916, ii, pp. 955-956.
Malingering in the French Army. Brit. M. J., Lond., 1916, i, p. 64.
Malingering. Brit. M. J., Lond., 1917, ii, p. 117.
Malingering in the army. Monde méd., Paris, 1916. Eng. ed., xxvi, p. 147.
Mallet, R. À propos de quelques psychopathes. Presse méd., Par., 1915, v. 23, p. 390.
Mallet, R. Troubles psychiques et hallucinations chez le combattant. Progrès méd., Par., 1916, No. 3, p. 16.
Mallet, R. Troubles psychiques et hallucinations chez le combattant. Rev. Paris méd., 1916 (Part, méd.), v. 19, p. 96.
Mallet, R. Troubles d’origine émotive chez le combattant. Presse méd., Par., 1916, v. 24, p. 95.
Mallet, R. La confusion mentale chez le combattant. Presse méd., Par., 1916, v. 24, pp. 294-295.
Mallet, R. Fugues des dégénérés. Presse méd., Par., v. 24, 1916, p. 493.
Mallet, R. Discussion de Vincent. Rev. neurol. Par., Nos. 4-5, p. 597.
Mallet, R. Fugues et délires aigus. Rev. neurol., 1917, v. 24, p. 486.
Mallet, R. États du fatigue. Presse méd., Par., 1917, v. 25, p. 325.
Mallet, R. États confusionnels et anxieux chez le combattant. Ann. méd. psychol., Par., 1917, v. 73, pp. 27-35.
Mallet, R. Fugue et délire. Contribution à l’étude des troubles psychiques de la guerre. Ann. méd. psychol., Par., 1917, v. 73, pp. 330-343.
Mally and Corpechot. Monomyoplégies traumatiques; étude sur un groupe de lésions du système nerveux périphérique causées par les projectiles modernes. Rev. de Chir., 1917, lii, 281.
Mann, G. Die traumatischen Neurosen, ihre Entstehungsweise und klinischen Formen bei Kriegsverletzten. Deutsche med. Wchnschr., Leipz. u. Berl., 1916, v. 42, p. 1563.
Mann, G. Neue Gesichtspunkte und Methoden zur Behandlung der Kriegsneurosen. Med. Klin., Berl., 1916, v. 12, p. 1270.
Mann, L. Über Polyneuritis als Begleiterscheinung nervöser Erschöpfungszustände im Kriege. Neurol. Centralbl., Leipz., 1915, v. 34, pp. 150-152.
Mann, L. Über Granatexplosionsstörungen. Med. Klin., Berl. u. Wien., 1915, v. 11, pp. 963-964.
Mann, L. Neue Methoden und Gesichtspunkte zur Behandlung der Kriegsneurosen. Berl. klin. Wchnschr., 1916, No. 50, pp. 1333-1338.
Mann, L. Die traumatischen Neurosen, ihre klinischen Formen und ihr Entstehungsmodus bei Kriegsverletzungen. Berl. klin. Wchnschr., 1916, v. 53, No. 37, and No. 38.
Mann, L. Zur Frage der traumatischen Neurosen. Wien. klin. Wchnschr., 1916, xxix, 1651.
Mann, Lillienstein, etc. Discussion; Neurosen nach Kriegsverletzungen. Berl. klin. therap. Wchnschr., Wien u. Berl., 1916, v. 49-50, pp. 486-496.
Mannell, J. D. Reëducation in walking. Hospital, Lon., 1917, lxi, 383.
Marage. Les sourds-muets de guerre. Académie des Sciences, 25 avril 1915.
Marage. Rééducation auditive des surdités consécutives à des blessures de guerre. Vigot frères, 1915.
Marage. Contribution à l’étude des hypo-acousies consécutives à des blessures de guerre. Compt. rend. acad. d. sc., Par., 1915, v. 161, pp. 148-150.
Marage. Traitement des hypo-acousies consécutives à des blessures de guerre. Compt. rend. acad. d. sc., Par., 1915, v. 161, pp. 319-322.
Marage. Les sourds-mutités vraies et simulées consécutives à des blessures de guerre. Compt. rend. acad. d. sc., Par., 1916, v. 162, pp. 651-654.
Marage, M. Classement des soldats sourds d’àprès leur degré d’audition. Compt. rend. acad. d. sc., Par., 1916, v. 162, pp. 801-804.
Marage. Douze mois de rééducation auditive dans l’armée; résultats de 250 cas. Bull. acad. de méd., Par., 1916, v. 76, pp. 318-320.
Marage. La rééducation des surdités consécutives à des blessures de guerre. Bull. gén. psychol., Par., 1916, v. 15, pp. 5-21.
Marage. Traitement de la surdité par commotion. Paris méd., 1916, (Part. méd.), v. 21, p. 419.
Marburg. Zur Frage der Beurteilung traumatischer Neurosen im Kriege. Wien. klin. Wchnschr., 1916, v. 29, pp. 281-282.
Marburg, O. Nervöse Folgezustände von kriegerischen Ereignissen. Militärarzt, Wien, 1914, xlviii, pp. 402-404.
Marchal, R. Les lésions des nerfs périphériques. Arch. méd. belges., Paris, 1917, 70, 44.
Marchand, L. Des troubles mentaux dans les blessures pénétrantes du crâne. Ann. méd. psychol., Par., 1916-17, v. 7, pp. 192-208.
Marchand, L. Des paraplégies hystériques consécutives aux polyneurites diphtériques. Bull. et mém. Soc. méd. hôp. de Paris, 1917, 3 ser. 41, pp. 248-53.
Maresch. Über Schädelschüsse. Wien. klin. Wchnschr., 1915, v. 28, pp. 1208-1231.
Marguliés, A. Nervenerkrankungen im Kriege. Prag. med. Wchnschr., 1915, v. 40, pp. 299-301.
Marie, Pierre. A propos d’un prisonnier de guerre simulateur. Rev. neurol., Par., 1914-1915, v. 221, p. 492.
Marie, P. Sur la fréquence relative des amélioration dans les cas de quadriplégie par traumatisme médullaire, due à une blessure de guerre. Bull. acad. de méd., Par., 1915, v. 73, pp. 675-678.
Marie, P. La conduite à tenir vis-à-vis des blessés du crâne. Rev. neurol., Par., 1916, v. 29, pp. 453-457.
Marie, P. Tétanos tardif localisé à type abdominothoracique. Paris méd., 1916, v. 21, pp. 49-51.
Marie, P. et Benisty, A. Troubles nerveux purement fonctionnels consécutifs à des blessures de guerre. Rev. neurol., Par., 1914-15, v. 221, pp. 424-425.
Marie et Benisty. Remarques cliniques sur quelques cas de lésions de la moelle cervicale par plaies de guerre. Rev. Paris méd., (Part. méd.), v. 17, p. 178.
Marie et Benisty. Du retour de la contractilité faradique avant le rétablissement de la motilité volontaire dans les muscles paralysés, à la suite des lésions des nerfs périphériques. Soc. de Neurol. de Paris, 1915. Revue Neurol., May-June 1915, and July 1915.
Marie and Benisty. Individualité clinique des nerfs périphériques. Soc. de Neurol. March 15, 1915. Revue neurol., May-June 1915.
Marie and Benisty. Une forme douloureuse des lésions de nerf médian par plaie de guerre. Académie de Méd., Mar. 16, 1915.
Marie, P. et Chatelin. Un cas d’hématomyélie par éclatement d’obus à distance. Rev. neurol., Par., 1914-15, v. 222, p. 777.
Marie, P. et Chatelin. Notes sur une variété de troubles de la parole (scansion) observée dans les blessures de la région frontale. Rev. neurol., Par., 1917, v. 24, pp. 135-136.
Marie, P., Chatelin et Patrikios. Paralysie générale progressive développée chez un jeune soldat pendant la guerre. Rev. neurol., Par., 1917, v. 24, p. 38.
Marie, P., Dejerine, Ballet, G., Thomas, A., Dupré, Babinski, J., Meige, H. Discussion sur les troubles nerveux, dits fonctionnels, observés pendant la guerre. Rev. neurol., Par., 1914-15, v. 221, pp. 447-452.
Marie, P. et Foix. Sur une forme spéciale de parésie paratonique des muscles moteurs de la main. Soc. méd. d’hôp., 1916, 10 février.
Marie et Foix. Les syncinésies des hémiplégiques étude séméiologique et classification. Rev. neurol., Par., 1916, v. 23, pp. 2-27.
Marie et Foix. Influence du froid et des troubles vasomoteurs sur les réactions électriques. Rev. neurol., Par., 1916, v. 29, pp. 921-923.
Marie et Foix. Indications opératoires fournies par l’examen histologique des nerfs lésés par plaies de guerre. Presse Méd., Jan. 31, 1916.
Marie et Meige. Appareils pour blessés nerveux. Académie de Médecine, 1915.
Marie, Meige, et Gosset. Les localisations motrices dans les nerfs périphériques. Académie de Médecine, Dec. 28, 1915.
Marie, P. et Foix. Les aphasies de guerre. Rev. neurol., Par., 1917, v. 24, pp. 53-87.
Marie, P. et Mlle. G. Lévy. Un cas d’hémiplégie organique par commotion sans blessure. Rev. neurol., Par., 1917, v. 24, pp. 44-45.
Marie, P., Meige, H., et Béhague, P. Necessité d’un examen neurologique des plicatures dorsaux (camptocormiques). Rev. neurol., Par., 1917, v. 24, pp. 129-130.
Marriage, H. J. Special discussion on warfare injuries and neuroses. Proc. Roy. Soc. Med., Lond., 1917, v. 10, (sect. Otol.), pp. 47-56.
Marshall, W. H. Shell shock. J. Mich. M. Soc., Detroit, 1917, Sept., pp. 396-399.
Martinet, Alfred. Guerre et névroses cardiaques. Presse méd., Par., 1915, v. 23, pp. 433-435.
Martyn, King. Treatment by physical methods of mental disabilities induced by the war. Proc. Roy. Soc. Med., Lond., 1917-18, v. 10, (sect. Balneol.), pp. 19-21.
Marx, S. Über funktionelle Stimm- und Sprachstörungen und ihre Behandlung. München med. Wchnschr., 1916, No. 42, pp. 1502-1503.
Massachusetts committee for the State Care and Treatment of Soldiers Suffering from Nervous and Mental Diseases (letter). Bos. M. & S. J., 1917, clxxvi, 922.
Mathieu, Albert. Cause psychique de vomissements excessifs après la chloroformisation et après la gastro-entérostomie. Presse méd., Par., 1917, v. 25, pp. 197.
Matiri, A. I disturbi mentali nella sclerosi laterale amiotrofica. Riv. crit. di clin. med., Firenze, 1916, v. 17, pp. 197, 209, 221, 233.
Mauclaire, Pl. Troubles moteurs d’origine psychiques chez les blessés militaires. Bull. et mém. soc. de chir. de Par., 1914, v. 40, p. 1290.
Mauclaire, Pl. Commotion cérébrale intense avec mutisme et surdité psychiques. Bull. et mém. soc. de chir. de Par., 1916, v. 421, pp. 140-141.
Maude, A. Influenza and purulent bronchitis. Lancet, Lon., 1918, ii, 324.
Mayendorf. Über pathologische Zitterformen zur Kriegszeit. Münch. med. Wchnschr., 1916, v. 63, p. 323.
Mayer, A. G. On the non-existence of nervous shell-shock in fishes and marine invertebrates. Proc. Nat. Acad. Sc., Balt., 1917, iii, p. 597.
Mayer, C. Behandlung gekommenen Fälle von Kriegsverletzungen. Wien. med. Wchnschr., 1915, v. 65, p. 37.
Mayer, C. Kriegsneurologische Erfahrungen. Med. Klin., Berl. u. Wien., 1915, v. 112, pp. 1017-1022.
Mayer, Leo. Autoplastic nerve transplantation in the repair of gunshot injuries. Surg. Gynecol. and Obstet., 1918, xxvii, 530.
Mayer, L. Organization and aims of the Orthopedic Reconstruction Hospital. Amer. Jour., Care for Crip., 1917, 78.
Maynard. Syndrôme psychique atypique chez les blessés cranio-cérébraux. Montpel. méd., 1916, v. 39, pp. 65-69.
Mayo-Robson, A. W. Treatment of paraplegia from gunshot or other injuries of the spinal cord. Brit. Med. Jour., 1917, ii, 853.
McArdle, J. S. Joint troubles arising from nervous diseases. Practitioner, Lond., 1915, v. 95, pp. 174-180.
McClure, J. Campbell. The manipulation bath. Proc. Roy. Soc. Med., Lond., 1917, v. 10, No. 9 (Sect. of B. and Climatology), pp. 70-78.
McClure, J. C. Gastric atony and war neurasthenia. Lancet, Lond., 1917, ii. 600-602.
McDougall, W. Shell shock without visible signs of injury. Proc. Roy. Soc. Med., Lond., 1915-16, v. 9 (Sect. Psychiat.), pp. 25-26.
McDowall, Colin. Functional gastric disturbances in the soldier. J. Ment. Sc., Lond., 1917, v. 63, pp. 76-88.
McDowall, Colin. Functional gastric disturbances in the soldier. Lancet, Lond., 1916, ii, pp. 944-45.
McEllroy, W. S. Acidosis in shock. Jour. A. M. A., 1918, lxx, 846.
McKellar, H. R. Malingering. Mil. Surgeon, Wash., 1916, xxxix, 293-299.
McKenzie, R. Tait. Functional reëducation of the wounded. N. Y. Med. Jour., 1918, cviii, 683.
McKenzie, R. Tait. Reclaiming the Maimed. Macmillan, 1918.
McKenzie, R. Tait. Treatment of convalescent soldiers by physical means, Brit. M. J., Lond., 1916, ii, pp. 215-218; also Proc. Roy. Soc. Med., Lond., 1915-16, v. 9 (Surg. Sect.), pp. 31-70.
McLaughlin, J. Loss of speech and shell shock. Lancet, Lond., 1916, i, 212.
McMurtrie, Douglas C. The Disabled Soldier. Macmillan, 1919.
McMurtrie, D. C. Industrial training for war cripples. Illustrations of educational work in France and Germany. Am. J. Care Cripples, N. J., 1917, v. 4, p. 16.
McMurtrie, D. C. Reëducating German war cripples at Düsseldorf. Bos. M. & S. J., 1918, clxxviii, 182.
McWalter, J. C. A note on commotio cerebri, or shell shock. Med. Press and Circ., Lond., 1916, v. 101, pp. 332-333.
McWalter, J. C. An experiment in enforced continence. Med. Press and Circ., Lond., 1916, v. 102, pp. 363-364.
Meakins, J. C. and Gunson, E. B. Occurrence of hyperalgesia in the “irritable heart of soldiers.” Heart, 1917, vi, 343.
Medea, E. Malattie nervose e malattie mentali in rapporto alla guerra. Osp. maggiore, Milano, 1915, 2 s., v. 3, pp. 399-408.
Medea, E. Neurologia di Guerra. Atti. d. Soc. lomb. di sc. Med. e Biol., Milano, 1915-16, v. 5, pp. 49-60.
Médication hypnotique par le dial. Progrès Méd., Par., 1916, v. 31, p. 56.
Médecin tiré par un aliéné qu’il soignait. Ann. Méd.-psychol., Par., 1916-17, p. 567.
Meige, Henri. De certaines boîteries observées chez les “blessés nerveux.” Rev. neurol., Par., 1914-15, v. 22, pp. 939-947.
Meige, H. Contractions convulsives des muscles peauciers du crâne à la suite d’une déflagration (Tic ou Spasme?) Rev. neurol., Par., 1916, v. 23, pp. 107-109.
Meige, H. Les tremblements consécutifs aux explosions. Rev. neurol., Par., 1916, Nos. 4-5, p. 592.
Meige, H. Torticolis convulsif survenu chez un blessé du crâne hémiplégique et jacksonien. Rev. neurol., Par., 1916, v. 23, pp. 571-574.
Meige, H. Réformes, incapacités, gratifications dans les tremblements, les tics et les spasmes. Rev. neurol., Par., 1916, v. 23, pp. 758-763.
Meige, H. Torticolis convulsif survenu chez un blessé du crâne hémiplégique et jacksonien. Rev. neurol., Par., 1916. v. 24, pp. 571-574.
Meige, H. Tremblement, tressaillement, trémophobie consécutifs aux explosions. Rev. neurol., Par., 1916, v. 29, pp. 140-158.
Meige, H. Les tremblements consécutifs aux explosions (tremblement, tressaillement, trémophobie). Rev. neurol., Par., 1916, v. 29, pp. 201-209.
Meige, H. Sur les accidents nerveux déterminés par la déflagration de fortes charges d’explosifs. Rev. neurol., Par., 1916, v. 29, pp. 592-593.
Meige, H. Appareil pour redresser les griffes cubitales (Appareil Gillot). Rev. neurol., Par., 1917, v. 24, pp. 264-265.
Meige et Mme. Athanassio Benisty. De l’importance des lésions vasculaires associées aux lésions des nerfs périphériques dans les plaies de guerre. Bull. et mém. soc. méd. d’hôp. de Par., 1915, v. 39, pp. 208-211.
Meige et Benisty. Les formes douloureuses des blessures des nerfs. Soc. de Neurol., July 1, 1915.
Meige et Benisty. Les signes cliniques des lésions de l’appareil sympathique et de l’appareil vasculaire dans les blessures des membres. Presse méd., Par., 1916, v. 24, pp. 153-156.
Meige, H., Benisty, A., et Lévy, G. Impotence de tous les mouvements de la main et des doigts, avec intégrité des réactions électriques (main figée). Rev. neurol., Par., 1914-15, v. 22, pp. 1273-1276.
Meige, Maré, T., etc. Discussion sur la camptocormie. Rev. neurol., Par., [952]1914-15, v. 222, p. 1250.
Melocchi, F. Importanza dei centri fisiatrici di rieducazione funzionale per gli invalidi di guerra. Pensiero med., Milano, 1917, v. 7, p. 282.
Mendel, Kurt. Psychiatrisches und Neurologisches aus dem Felde. Neurol. Centralbl., Leipz., 1915, No. 1, p. 2. Rev. Med. Klin., Berl. u. Wien., 1915, v. 111, p. 575.
Mendelssohn, Maurice. Deux cas de paraplégie de nature organique suivis de guérison. Rev. neurol., Par., 1916, v. 29, pp. 190-193.
Mental and nervous cases in the war. Alb. Med. Ann., 1917, xxxviii, 328.
Mental disabilities for war service. Lancet, Lond., 1916, v. 191, p. 234.
Mentality (fortitude) of Wounded. Brit. M. J., Lond., 1915, i. p. 980.
Menzel. Mobilisierung in ursächlichem Zusammenhange stehenden Neurosen der oberen Luftwege, beziehungsweise des Ohres vor Militärärzt. Wien. med. Wchnschr., 1915, No. 4, p. 163.
Menzel. Symptom des sogenannten labyrinthören Spontan-nystagmus. Militärärzt. Wien. med. Wchnschr., 1915, v. 65, p. 235.
Mériel. Deux cas de tétanos partiel. Soc. chir., 2 Feb., 1916.
Merklen, P. Sur les déterminations psychiques des paratyphoides. Rev. Paris méd., 1916 (Part. méd.), v. 19, p. 96.
Merklen. Sur les déterminations psychiques des paratyphoides. Paris méd., 1916, (Part. Méd.), v. 21, pp. 64-66.
Merklen. Sur les déterminations psychiques des paratyphoides. Presse méd., Par., 1916, v. 24, p. 6.
Merklen. Note sur l’hypothermie chez les militaires. Bull. et mém. soc. méd. d’hôp. de Par., 1917, v. 33, pp. 1008-1010.
Merle und Schaidler. Ausbildung und Berufstätigkeit der Kriegsblinden. Deutsche med. Wchnschr., Leipz. u. Berl., 1916, v. 42, p. 468.
Mesnard. Tétanos monoplégique. Marseille méd., Par., 1917, pp. 363-365.
Metcalfe, F. A Red Cross “Plattsburg”; the U. S. Army Ambulance Corps’ Camp at Allentown, Pa. Red Cross Mag., Wash., 1917, v. 12, pp. 430-436.
Meyer, E. Psychosen und Neurosen in der Armee während des Krieges. Deutsche med. Wchnschr., Berl. u. Leipz., 1914, v. 402, pp. 2085-2088.
Meyer, E. Ueber die Frage der Dienstbeschädigung bei den Psychosen. München. med. Wchnschr., 1916, lxiii, 1558.
Meyer, E. Der Einfluss des Krieges, insbesondere des Kriegsausbruch auf schon bestehende Psychosen. Archiv. f. Psych., Berl., 1915, v. 55, pp. 353-364.
Meyer, E. Functionelle Nervenstörungen bei Kriegsteilnehmen nebst Bemerkungen zur traumatischen Neurose. Deutsche med. Wchnschr., Leipz. u. Berl., 1915, v. 41, pp. 1509-1511.
Meyer, E. Beitrag zur Kenntnis des Einflusses kriegerischer Ereignisse auf die Entstehung geistiger Störungen in der Zivilbevölkerung und zu der physischen Infektion. Ibid., lvi, 247-279.
Meyer, E. Zwei Soldaten mit psychogenen Störungen. Berl. klin. Wchnschr., 1915, v. 521, p. 94.
Meyer, E. Die Frage der Laminektomie von neurologischen Standpunkt. Berl. klin. Wchnschr., 1915, v. 521, pp. 282-283.
med. Wchnschr., 1916, No. 44, p. 1558.
Meyer, E. Bemerkungen zu der Differentialdiagnose der Psychosen. Reaktionen mit besonderer Berücksichtigung der im Kriege beobachteten psychischen Störungen. Archiv. f. Psychiat., 1916, v. 56, pp. 244-246.
Meyer, E. Kriegshysterie. Deutsche med. Wchnschr., Leipz. u. Berl., 1916, v. 42, pp. 69-71.
Meyer, E. Funktionelle Nervenstörungen bei Kriegsteilnehmern nebst Bemerkungen zur traumatischen Neurose. Med. Klin., Berl., 1916, v. 12, p. 26.
Meyer, E. Krankheitsanlagen und Krankheitsursachen im Gebiete der Psychosen und Neurosen. Berl. klin. Wchnschr., 1917, No. 3, Rev. Cor. bl. f. Schweize Arztr., 1917, No. 19, p. 620.
Meyer, E. Ueber die Frage der Dienstbeschädigung bei den Psychosen. Arch. f. Psychiat., Berl., 1917, 57, 208-220.
Meyer, E. und Frida Reichmann. Über nervose Folgezustände nach Granatexplosionen. Arch. f. Psychiat., Berl., 1916, v. 56, No. 3.
Mézie, A. Troubles réflexes et insuffisance cérébrale. Gazette hebdomadaire des Sciences médicales de Bordeaux, 23 Sept. 1916.
Michon, E. Impotence fonctionnelle du muscle trapèze à la suite d’une plaie par balle de la région sus-claviculaire. Bull. et mém. soc. de chir. de Par., 1915, v. 41, pp. 652-655.
Midelton, W. J. Nerves and the war. Med. Times, Lond., 1914, v. 42, pp. 726, 742, 758, 776, 786, 802, 835.
Mignard. Syndrôme psychique atopique chez les blessés crânio-cérébraux (Observé quelques mois après la blessure). Montpel. méd., 1916, v. 39, p. 65.
Mignard. Quelques considérations sur la résponsabilité des blessés crânio-cérébraux. Montpel. méd., 1916, v. 39, p. 127.
Mignot, Roger. L’évolution de la paralysie générale chez les officiers combattants. Presse méd., Par., 1917, v. 25, pp. 487-488.
Milian, G. Battle hypnosis. Med. Press and Circ., Lond., 1915, n.s., c, 486-488.
Milian, G. Les aliénés dans l’armée. Paris méd., 1914-15, v. 15, (Part. méd.), p. 458.
Milian, G. L’hypnose des batailles. Paris méd., v. 15, 1914-15, pp. 265-270.
Milian, G. Désertion ou fugue. Paris méd., (Part. méd.), 1915, v. 17, pp. 11-13.
Milian, G. Les éruptions provoquées. Paris méd., 1917, xxi, 343-351.
Milian, G. La fête au camp. Paris Méd., 1915, (Part. méd.), 1915, v. 17, pp. 11-13.
Military mental cases. Med. officer, Lond., 1915, v. 14, p. 150.
Military orthopaedics and the American unit. Brit. M. J., Lond., 1917, v. 1, p. 772.
Military Orthopedic Surgery. No. 4, Medical Manual War Series. Lea and Febiger, 1918.
Military psychiatry. Bos. M. and S. J., 1918, clxxviii, 98.
Milligan, E. T. C. Medical Experiences in the War Zone. M. J. Australia, Sydney, 1917, v. 1, pp. 201-203.
Milligan, E. T. C. Method of treatment of “shell shock.” Brit. Med. Jour., 1916, ii, 73.
Milligan, E. C. Treatment of Shell Shock. J. Roy. Army Med. Corps, Lond., 1917, v. 28, pp. 272-273.
Milligan, W. Functional Cases. Discussion. Proc. Roy. Soc. Med., Lond., 1914-1915, (sect. laryngol.), v. 8, p. 118.
Milligan, W. Treatment of “Functional aphonia” in Soldiers from the Front. J. Laryngol., Lond., 1916, v. 31, pp. 299-300.
Milligan, W. Treatment of Shell Shock. Brit. M. J., Lond., 1916, ii, p. 73; also ii, p. 242.
Milligan and Westmacott. Warfare injuries and neuroses. J. Laryngol., 1915, v. 30, p. 297.
Mills, A. E. Some nerve injuries seen on active service. M. J. Australia, Sydney, 1917, v. 4, pp. 73-75.
Mills, Lloyd. Projectile Wounds of the Head. J. Am. M. Ass., Chicago, 1915, v. 65, pp. 1424-1427.
Mingazzini, G. Sindromi nervose organiche consecutive a lesioni (da proiettili) del cervello. Policlin., Roma, 1916 (sez. med.), v. 23, p. 409.
Mingazzini, G. Neurologia di guerra (ferite da proiettile del cervello e midollo spinale). Policlinico, Roma, sez. prat., 1917, v. 24, pp. 22-23.
Mingazzini, G. Osservazioni cliniche sulle lesioni del cervello e del midollo spinale da proiettili di guerra. Policlin., Roma, 1917, v. 24 (sez. med.), pp. 121, 178, 189.
Mirallié, M. Paralysies réflexes. Rev. gén. de path. de guerre, Par., 1916, No. 1, pp. 19-35.
Mirc, J. Folies de guerre chez les civils. Caducée, Par., 1916, v. 16, p. 141.
Mirc, J. Folies de guerre chez les civils. J. de méd. de Par., 1917, v. 36, p. 12.
Misch, W. Ueber Hemiplegie bei Diphtherie. Neurol. Centralbl., Leipz., 1916, v. 35, No. 22.
Mizie, A. Troubles réflexes et insuffisance cérébralles. Gaz. hebd. d. sc. méd., Par., 1916, v. 2, pp. 141-142.
Mohr, F. Behandlung nervöser und depressiver Zustandsbilder bei Kriegsteilnehmer. n. Aerztl. Centralbl. Ztg., 1915, Wien, v. 32, p. 134.
Mohr, F. Zur Entstehung, Vorhersage und Behandlung nervöser und depressiver Zustandsbilder bei Kriegsteilnehmern. Med. Klin., Berl., 1915, xi, 920.
Mohr, F. Grundsätzliches zur Kriegsneurosenfrage. Med. Klin. Berl. u. Wien, 1916, v. 12, pp. 89-93. Rev. Aerztl. Rundschau, 1916, v. 26, pp. 40-41.
Mohr, F. Behandlung der Kriegsneurosen. Therap. Monatschr., Berl., 1916, v. 30, No. 3.
Molhaut, M. Les troubles moteurs d’ordre réflexe. Arch. méd., Belges, Brux., 1917, v. 47, pp. 910-927.
Moll, A. Ueber psychopathologische Erfahrungen vom westlichen Kriegsschauplatz. Berl. klin. Wchnschr., 1915, iii, 95.
Moll, A. Kriegsärztlicher Abend, Berlin, Jan. 12, 1915. Psychiat.-Neurolog. Wchnschr., Halle, a. s., 1914-15, v. 16, p. 402.
Moll, A. Psychopathologische Erfahrungen vom westlichen Kriegsschauplatz. Med. Klin., Berl. u. Wien, 1915, v. 111, p. 710.
Moll, A. Psychopathologische Erfahrungen vom westlichen Kriegsschauplatz. Ztschr. f. ärtzl. Fortbild., 1915, No. 10, pp. 305-310; also No. 9, pp. 261-266.
Moll, A. Psychopathologische Erfahrungen im Kriege. Aerzt. Central. Zeit., Wien, 1915, v. 27, p. 139.
Moll, A. Psychopathologische Erfahrungen auf dem westlichen Kriegsschauplatz. Berl. klin. Wchsnchr., 1915, No. 4, p. 95.
Mollison, W. M. Cases of deafness as a result of the war. Guy’s Hosp. Gaz., Lond., 1916, Feb., pp. 69-71.
Monbrun, A. Les hémianopsies en quadrant et le centre cortical de la vision. Presse méd., Par., 1917, v. 25, pp. 607-609.
Monier-Vinard. Troubles physiopathiques médullaires post-tétaniques et latents décélés par l’anesthésie chloroformique. Rev. neurol. Par., 1917, v. 24, pp. 568-572.
Montier. Discussion de la conduite à tenir vis-à-vis des blessures du crâne—par P. Marie. Rev. neurol., Par., 1916, v. 29, p. 469.
Moravensic, von E. C. Die Rolle des Krieges im der Aetiologie nervöser insbesonders psychische Störungen. Neurol. Centralbl., Leipz., 1915, v. 34, p. 637.
Moravskaya, V. Ye. and Moravskaya, Yu. A. (The “Kokhanuvka” institution for the insane and the war). Psikhiat. Gaz., Petrogr., 1916, v. 3, pp. 311-333.
Morax, V. Notes cliniques et statistiques sur l’ophtalmie sympathique aux armées. Ann. d’ocul., Par., 1917, v. 144, pp. 706-722.
Morchen. Traumatische Neurosen und Kriegsgefangene. München. med. Wchnschr., 1916, v. 64, No. 32.
Morestin. Mutisme hystérique à l’occasion d’une blessure de la langue. J. de méd. et de chir., 1915, Jan., v. 86.
Morestin. Un cas de mutisme hystérique à l’occasion d’une blessure de la langue. Bull. et mém. soc. de chir. de Par., 1915, v. 41, pp. 98-100.
Morhardt, P. E. Cure de soleil et chirurgie de guerre. Paris méd., 1915-16, v. 17, pp. 315-317.
Moricand, I. Note sur un cas de paralysie radiale bilatérale par compression, due à l’usage prolongé des béquilles chez un soldat atteint de monoplégie crurale hystérique. Société de Neurol., 1915.
Morcelli, Arturo. (Psychiatry of War.) Boll. d. r. Accad. med. di Genova, 1916, v. 31, p. 65.
Morselli, A. Sui fenomeni fisio-patologici da emozione massime in rapporto alla neurologia di guerra. Quaderni di psichiat., Genova, 1916, v. 3, pp. 206-214.
Morselli, A. Sugli stati confusionali psichici da guerra. Quaderna di psichiat., Genova, 1917, iv, 45-52.
Morselli, A. Sopra le sindromi emotive di guerra. Rev. di patol. nerv., Firenze, 1917, v. 22, pp. 329-336.
Mosny, E. La rééducation professionelle et la réadaptation au travail. Ann. d’Hyg., Par., 1915, v. 23, pp. 317-339.
Mosquet, P. et Schwartz, Anselme. The immediate treatment of head injuries from projectiles. J. Roy. Army Med. Corps, Lond., 1916, v. 26, pp. 278-283.
Mott, F. W. The microscopic examination of the brains of two men dead of commotio cerebri (shell shock) without visible external injury, Ibid., 612-615, 1 pl.
Mott, F. W. Psychic mechanism of the voice in relation to the emotions. Brit. M. J. Lond., 1915, ii, pp. 845-847.
Mott, F. W. Discussion on shell shock without visible signs of injury. Proc. Roy. Soc. Med. Lond., 1915-16, v. 9 (sec. psychiat. and neurol.), pp. 1-44.
Mott, F. W. The effects of high explosives upon the central nervous system. Tr. M. Soc. Lond., 1915-16, xxxix, 157-226, 11 pl. Also Lancet, Lond., 1916, i, 331, 545.
Mott, F. W. The Lettsomian lectures on the effects of high explosives upon the central nervous system. Lancet, Lond., 1916, i, v. 190, pp. 331-338, pp. 441-449, pp. 545-553; also Tr. Med. Soc. Lond., 1915-16, v. 39, pp. 157-226.
Mott, F. W. Mental hygiene in shell shock. J. M. Sc., Lond., 1917, v. 63, pp. 467-488.
Mott, F. W. 1. On war psychoneurosis. 2. The psychology of soldiers’ dreams. Lancet, Lond., 1918, i, pp. 169-177.
Mott, F. W. Punctiform hemorrhages of the brain in gas poisoning. Brit. Med. Jour., 1917, i, 637.
Mott, F. W. The Chadwick Lectures on mental hygiene and shell shock during and after the war. Brit. M. J., Lond., 1917, ii, 39-42.
Mott, F. W. War psychoneurosis. Lancet, Lon., 1918, i, 127, 177.
Mougeot, A. and Duverger. Bradycardie et réflexe oculocardiaque dans les traumatismes oculaires, crâniens, encéphaliques. Presse méd., Par., 1917, v. 25, pp. 730-732.
Moure, E. J. Paralysies faciales de la guerre. Presse méd., Par., 1916, v. 24, pp. 161-164.
Moure et Pietri. L’organe de l’audition pendant la guerre. Arch. de méd. et de pharm. mil., Par., 1916, v. 65, pp. 809-837; and 1916, v. 66, pp. 167-186.
Mouriquand. Sur quelques maladies simulées. Vomissements pseudoporracés. Lyon méd., 1917, v. 126, pp. 276-278.
Moutier, François. Recherches sur les troubles labyrinthiques chez les commotionnés et blessés du crâne. Rev. neurol., Par., 1916, v. 23, pp. 9-15.
Moynihan, Berkley. On injuries to the peripheral nerves and their treatment. Brit. M. J., 1917, ii, pp. 571-574.
Moynihan, Berkley. Injuries to the peripheral nerves and their treatment. Brit. Med. Jour., 1917, ii, 571.
Muenzer, Arthur. Die Psyche des Verwundeten. Berl. klin. Wchnschr., 1915, v. 52, pp. 234-235.
Muirhead, I. B. Shock and the soldier. Lancet, Lond., 1916, i, p. 1021.
Müller. Typhuspsychose. Deutsche med. Wchnschr., 1915, Berl. u. Leipz., v. 41, pp. 331-332.
Myerhof, M. Night-blindness as a war disease. Am. J. Ophth., St. Louis, 1916, p. 139.
Myers, Charles S. Contributions to the study of shell shock. Lancet, Lon., 1916, ii, 461.
Myers, Charles S. Shell shock. Three cases of loss of memory, vision, smell and taste. Lancet, Lond., 1915, i, pp. 316-320.
Myers, Charles S. Shell shock. An account of certain cases treated by hypnosis. Lancet, Lond., 1916, i, pp. 65-69; also J. Roy. Army Med. Corps, Lond., 1916, v. 26, pp. 642-655.
Myers, Charles S. Shell shock. Certain disorders of cutaneous sensibility. Lancet, Lond., 1916, i, pp. 608; also J. Roy. Army Med. Corps, Lond., 1916, v. 26, pp. 782-797.
Myers, Charles S. Shell shock. Certain disorders of speech,—their causation and their relation to malingering. Lancet, Lond., 1916, ii, pp. 461-467; also J. Roy. Army Med. Corps, Lond., 1916, v. 27, pp. 561-582.
Naccarati, Sante. Medical organization of the Italian army; the neuropsychiatric service. Jour. A. M. A., 1918, lxxi, 1477.
Nägeli, O. Ueber die Entschädigung der Kriegsneurosen. Med. Cor.-Bl. d. würtemb. ärztl. Landesver., Stuttg., 1916, v. 86, No. 5.
Nägeli, O. Zur Frage der traumatischen Kriegsneurosen im besonderer Berucksichtigung der Oppenheim’schen Auffassungen. Neurol. Centralbl., Leipz., 1916, v. 35, No. 12.
Nägeli, O. Schlussfolgerungen für die Art der Abfindung der Kriegsneurosen. Ztschr. f. ärztl. Fortbldg., Nr. 8, 1918.
Nageotte, J. Le processus de la cicatrisation des nerfs. Rev. Neurol., July, 1915.
Nash, E. H. Education of the left hand of disabled sailors and soldiers. Lancet, Lond., 1917, v. 1, p. 964.
Natalelli and Roger, H. Erythèmes de la face provoqués pour simuler un érysipèle. Arch. de méd. et pharm. mil., Par., 1916-17, lxvi, 547.
Naville, F. Le traitement et la guérison des psychonévroses de guerre invétérés à l’hôpital Saint-André de Salins. Corr.-Bl. f. Schweizer Aerzte, Nr. 25, 1918.
Necessité de créer des établissements spéciaux destinés aux invalides nerveux. Rev. neurol. Par., 1916, v. 23, pp. 593-594.
Necessité des services de psychiatrie et de médecine légale aux armées. Caducée, Par., 1916, v. 16, pp. 43-45.
Necessité de traiter les plicatures vertébrales (camptocormies) dans les centres neurologiques. Rev. Neurol. Par., 1917, v. 24, p. 137.
Negro, C. Annotazione di neurologia di guerra. Gior. d. r. Accad. di med. di Torino, 1916, v. 22, pp. 377-389.
Neiding, M. N. (Nervous phenomena accompanying poisoning by asphyxiating gases). Russk. Vrach., Petrogr., 1917, v. 16, p. 397.
Neilson, W. A. The Training School of Psychiatric Social Work at Smith College. I. Educational Significance of the Course. Mental Hygiene, II, October, 1918.
Nepper et Vallée. Recherches comparatives sur les impotences fonctionnelles dues aux lésions osseuses et articulaires (ankyloses et résections) du membre supérieur. Paris méd., 1916 (Part. méd.), v. 21, pp. 86-92.
Néri, V. Moyen pour découvrir la simulation de la sciatique. Presse méd., Par., 1917, v. 25, p. 64.
Néri, V. Les petits signes électriques de la sciatique. Presse méd., Par., 1917, v. 25, pp. 466-468.
Nervöse Disposition. Med. Cor. Bl. d. Württemb. ärztl. Landesver., Stuttg., 1916, v. 86, p. 42.
Nervous and mental disease among soldiers. N. Y. Med. Jour., 1917, cvi, 1043.
Nervous temperament in war. Brit. Med. Jour., 1918, i, 649.
Netter, F. L’épilepsie généralisée consécutive aux traumatismes de guerre crânio-cérébraux. Thèses de Paris. 1917-8, No. 9.
Neumann, E. Psychologische Beobachtungen im Felde. Neurol. Centralbl., 1914, v. 33, pp. 1243-1245.
Neurasthenia and shell shock. Lancet, Lond., 1916, i, p. 627.
Neurologie de Guerre. Presse Méd., Par., 1917, v. 25, pp. 217-221.
Neutra, W. Einige Bemerkungen über die Beurteilung und Behandlung der Kriegsneurosen. Wien. klin. Wchnschr., 1916, v. 29, p. 1253.
Neutra, W. Wien. klin. Wchnschr., 1917, 30, 1198-9.
Névrite irradiante et paralysies ou contractures d’ordre réflexe. Rev. gén. de clin. et de thérap., Par., 1916, v. 30, pp. 457-460.
Nicolai, George F. Biology of War. Century Co., 1918.
Niessl von Mayendorf. Ueber pathologische Zitterformen zur Kriegszeit. Münch. med. Wchnschr., 1916, v. 63, p. 323.
Nikitina-Pakhorzkaya, T. P. (Case of choreo-athetosis of war-traumatic origin). J. Nevropat. i Psikhiat.… Korsakova, Mosk., 1915-16, v. 15, pp. 436-444.
Nissl. Ueber den Stand der Hysterielehre mit besonderer Berücksichtigung der Kriegserfahrungen. Berl. klin. Wchnschr., 1916, v. 53, p. 232.
Noehte. Nystagmus bei Verletzungen des Fusses der II. Stirnhirnwindung. Deut. Med. Woch., 1915, xli, 1217.
Nöica, (de Bucarest.) Sur la contracture dans les paraplégies spasmodiques. Rev. neurol., Par., 1916, v. 23, pp. 257-263.
Nonne, M. Soll man wieder “traumatische Neurose” bei Kriegsverletzten diagnostizieren? Med. Klin., Berl. u. Wien, 1915, v. 112, pp. 849-854; also pp. 948-949.
Nonne, M. Zur therapeutischen Verwendung der Hypnose bei Fällen von Kriegshysterie. Med. Klin., Berl. u. Wien, 1915, v. 112, pp. 1391-1396.
Nonne, M. Fälle von Kriegsverwundeten. Neurol. Centralbl., 1915, v. 34, pp. 41-46.
Nonne, M. Demonstration von Nervenkriegsverletzungen. Neurol. Centralbl., Leipz., 1915, v. 34, pp. 317-321.
Nonne, M. Ueber Neurosen und Hysterie bei Soldaten. Neurol. Centralbl., Leipz., 1915, v. 34, pp. 408-409.
Nonne, M. Kriegsverletzungen. Ztschr. f. d. ges. Neurol. u. Psychiat., Berl. u. Leipz., 1914-15, v. 11, pp. 198-200.
Nonne, M. Ueber Polyneuritis gemischter Nerven bei neurasthenischen Kriegsteilnehmern. Deutsche Ztschr. f. Nervenh., Leipz., 1915, v. 53, pp. 464-469.
Nonne, M. Hysterie bei Soldaten. Ztschr. f. d. ges. Neurol. u. Psychiat., Berl. u. Leipz., 1914-15, v. 11, pp. 421-422.
Nonne, M. Zur therapeutischen Werth der Hypnose bei Fällen im Kriegshysterie. München. med. Wchnschr., 1915, v. 62, p. 1579.
Nonne, M. Nervenverletzungen und Erkrankungen im Kriege. (Abstract). Deutsche med. Wchnschr., Berl., u. Leipz., 1915, v. 41, pp. 573-574.
Nonne, M. Nervenkriegsverletzungen. Deutsche med. Wchnschr., Berl. u. Leipz., 1915, v. 41, p. 695.
Nonne, M. Hypnose bei Kriegshysterie. Deutsche med. Wchnschr., Berl. u. Leipz., 1915, v. 412, pp. 1587-1588.
Nordman, Charles. Psychose post-typhique chez un adulte avec évolution probable vers la démence précoce. Ann. méd.-psychol., Par., 1916-17, v. 7, pp. 493-498.
Nordmann et Bonhomme. De l’utilisation des indisciplinés en temps de guerre. Ann. méd. psychol., Par., 1916-17, v. 32, pp. 490-493; also pp. 519-524.
Norman, Hubert J. Some neuroses of the war. Rev. of Clark., J. Ment. Sc., Lond., 1917, v. 63, pp. 119-121.
Notes on British military medical arrangements; work in the restoration and reëducation of disabled soldiers; treatment of cases of heart disease; military orthopedic hospitals. Mod. Hosp., St. Louis, 1917, v. 9, p. 293.
Notes on hydrological treatment for wounded soldiers and sailors; with a list of the British spas and health resorts and the disorders which they benefit. Lond., 1915, Adlard and Son, 20, p. 9.
Nouvelle Jeanne d’Arc. Ann. méd. psychol., Par., 1914-1915, p. 422.
Nuthall, A. W. Three cases of gunshot wound of the superior longitudinal sinus. J. Roy. Army Med. Corps, Lond., 1916, v. 26, pp. 235-240.
Nunneley, P. P. Treatment by physical methods of mental disabilities induced by the war. Proc. Roy. Soc. Med., Lond., 1917-18, v. 10 (Sect. Balneol.), pp. 30-34.
Nyns, Adrien. La rééducation professionnelle d’après les variétés d’impotence. Paris méd., 1916, v. 21, pp. 493-496.
Obendorf, C. P. Traumatic hysteria. N. Y. Med. Jour., 1917, cvi, 874.
Oloff. Bemerkenswerte Fälle von Verwundung des Sehorgans. Deutsche med. Wchnschr., Berl. u. Leipz., 1915, v. 412, pp. 1190-1192.
O’Malley, J. F. Functional aphonia. Proc. Roy. Soc. Med., Lond., 1914-15, v. 8 (Sect. Laryng.), p. 116.
O’Malley, J. F. Warfare neuroses of the throat and ear. Lancet, Lond., 1916, i, 1080.
Ombredanne, L. and Ledoux-Lebard, R. Localisation et extraction des projectiles. 1917, Paris, Masson et Cie.
Oppenheim, H. Zur Kriegsneurologie. Berl. klin. Wchnschr., 1914, No. 48, pp. 1853-1856.
Oppenheim, H. Krankendemonstrationen zur Kriegsneurologie. Discussion Rothmann-Cohn, Toby. Berl. klin. Wchnschr., 1915, v. 421, p. 168.
Oppenheim, H. Der Krieg und die traumatischen Neurosen. Berl. klin. Wchnschr., 1915, v. 52, pp. 257-261.
Oppenheim, H. Kriegsneurosen. Med. Klin., Berl. u. Wien. 1915, v. 11, p. 147.
Oppenheim, H. Bemerkung zu dem Aufsatze Nonnes: Soll man wieder traumatische Neurose bei Kriegsverletzten diagnostizieren? Med. Klin., Berl. [958]u. Wien, 1915, v. 112, pp. 920-921.
Oppenheim, H. Ueber Hemiplegia spinalis mit homolateraler Hemianästhesie. Neurol. Centralbl., Leipz., 1915, v. 34, pp. 49-51.
Oppenheim, H. Zur traumatischen Neurosen im Kriege. Neurol. Centralbl., Leipz., 1915, v. 34, pp. 514-518.
Oppenheim, H. Die Neurosen nach Kriegsverletzungen. Neurol. Centralbl., Leipz., 1915, v. 34, pp. 810-813.
Oppenheim, H. Der Krieg und die traumatischen Neurosen. 1915, Berlin, A. Herschwald.
Oppenheim, H. Ueber Kriegsverletzungen des peripheren und zentralen Nervensystems. Ztschr. f. ärztl. Fortbild., Jena, 1915, No. 4, pp. 97-106.
Oppenheim, H. (Discussion of Lewandowsky) Ueber Kriegsverletzungen des Nervensystems. Deutsche med. Wchnschr., 1915, v. 411, p. 89.
Oppenheim, H. (Further discussion) Ueber die traumatischen Neurosen. Neurol. Centralbl., Leipz., 1916, v. 35, No. 13.
Oppenheim, H. “Alloparalgie.” Neurol. Centralbl., Leipz., 1916, No. 21. Rev. Berl. klin. Wchnschr., 1916, No. 48, p. 1302.
Oppenheim, H. Zur Frage der traumatischen Neurosen. Deutsche med. Wchnschr., Leipz. u. Berl., 1916, v. 42, pp. 1567-1570.
Oppenheim, H. Die Neurosen infolge von Kriegsverletzungen. 1916, Berlin, S. Karger.
Oppenheim, H. (Aussprache zum Vortrag von Singer: Zitterer im Felde.) Neurol. Centralbl., 37, Nr. 12, 1918.
Oppenheim, Nonne, Gaupp, etc. Neurosen nach Kriegsschädigungen. Münch. med. Wchnschr., 1916, No. 45, p. 1594.
Oppenheim, R. L’amnésie traumatique chez les blessés. Progrès méd., Par., 1917, 3. s., xxxii, 189, 199.
Oppenheim, R. Le pouls, la tension artérielle et le réflexe oculocardiaque dans les suites éloignées des traumatismes crâniens. Progrès méd., Par., 1917, No. 7, pp. 53-55.
Oppenheim, R. et Hallez, G. L. La diplégie faciale traumatique. Paris méd., 1917, v. 23, pp. 136-139.
Organic lesions in shell shock. Bos. Med. and Surg. Jour., 1918, 24.
Organisation des asiles publics d’aliénés de la Seine après la guerre. Progrès méd., Par., 1917, v. 32, p. 366.
Ormond, A. W. Short notes on 30 cases of blinded soldiers during the present war. Guy’s Hos. Gaz., Lond., 1915, May 22.
Ormond, A. W. Treatment of “concussion blindness.” Guy’s Hos. Gaz., Lond., 1915, v. 30, pp. 99-101.
Ormond, A. W. Treatment of “concussion blindness.” J. Roy. Army Med. Corps, Lond., 1916, v. 26, pp. 43-49.
Orth. Simulation. Dementia Praecox. Deutsche med. Wchnschr., 1915, v. 412, p. 936.
Osier, Sir William. Science and war. 1915, Oxford, Clarendon Press, 40 p., 8o.
Osnos. (Case of nervous and mental disease during the war.) Nevropat. i Psikhiat., Korsakova, Mosk., 1915-16, v. 15, p. 143.
Oudet, L. Deux épreuves pratiques pour dépister les simulateurs de surdité. Presse méd., Par., 1917, xxv, annexes, 515.
Overbeck-Wright, A. W. A case of malingering. Indian M. Gaz., Calcutta, 1915, v. 50, p. 334.
Overbeek, H. J. Psychoses in war and wounds of the nervous system. Mil.-geneesk Tijdschr., Haarlem, 1915, xix, 209-216.
Overbeek, H. J. Mobilisatie-neurosen en Psychosen. Nedrl. Tijdschr. v. Geneesk., Amst., 1917, v. 1, pp. 1617-1620.
Pachantoni, D. Paralysies multiples des nerfs crâniens par “vent d’obus.” Rev. méd. de la Suisse Rom., Genève, 1917, v. 37, pp. 226-229.
Pactet, M. La réforme des paralytiques généraux. J. de méd. de Bordeaux, 1917, v. 88, pp. 163-164.
Pactet et Bonhomme. Deux observations de peur invincible chez des combattants. Ann. méd. psychol., Par., 1917, v. 73, pp. 375-380.
Padovani, E. Note e osservazioni dalle zone di guerra. Rassegna di studi psichiat., Siena, 1915, v. 5, pp. 342-346.
Pangon, J. et Gate, J. Accidents syphilitiques et dermatoses simulés. Lyon méd., 1916, v. 125, pp. 216-219.
Pansky. Contribution à l’étude de la psychonévrose consécutive à la contusion et aux incidents des combats. Nouvelles médicales de Minsk, No. 3, 1915.
Pansky. Contribution à la connaissance des névroses de contusion compliquées par des lésions organiques du système nerveux. Gazette médicale russe, No. 9, 1915.
Parhon, C. J. et Vasiliu, Mme. Eug. Troubles sensitifs et moteurs (tremblement à type parkinsonien; phénomènes paralytiques) à topographie surtout cubitale, du côté droit, à la suite d’une lésion crânienne dans la région pariétale gauche. Rev. Neurol., Par., 1917, v. 24, pp. 156-162.
Parkinson. An inquiry into the cardiac disabilities in soldiers on active service. Lancet, Lond., 1916, ii, pp. 133-138.
Parkinson, J. Digitalis in soldiers with cardiac symptoms and a frequent pulse. Heart, 1917, vi, 321.
Parkinson, J. and Drury, A. N. P-R interval before and after exercise in cases of “soldier’s heart.” Heart, 1917, vi, 337.
Parkinson, J. Pulse rate on standing and on slight exertion in healthy men and in cases of “soldier’s heart.”
Parkinson, J. and Koefod, H. Immediate effect of cigarette smoking on healthy men and on cases of “soldier’s heart.” Lancet, Lon., 1917, ii, 232.
Paris. Aliénation mentale et état de guerre, leurs rapports. Société de médecine de Nancy, 1915.
Pariset. Le massage chirurgical, méthode d’enseignement rapide à l’usage des infirmiers militaires. Presse méd., Par., 1915, v. 23, pp. 97-100.
Parsons, J. H. The psychology of traumatic amblyopia following explosions of shell. Proc. Roy. Soc. Med., Lond., 1914-15, v. 8, (neurol. sect.), pp. 55-68; also Lancet, Lond., 1915, i, p. 697.
Pascha, Wieting. Leitsätze der funktionellen Nachbehandlung kriegschirurgischer Schäden. Samml. klin. Vortr. n. F., Leipz., 1915, pp. 123-165.
Pastini, C. Commozione dei centri nervosi da esplosione violenta a breve distanza. (Influenza del delore finio sullo stato psichico). Riv. di patol. neu., Firenze, 1916, v. 21, pp. 433-438.
Paton, Stewart. Mobilizing the brains of the nation. Mental Hyg., Concord, N. H., v. 1, pp. 334-344.
Paton, Stewart. Effects of low oxygen pressure on the personality of the aviator. Jour. A. M. A., 1918, lxxi, 1399.
Paton, Stewart, MacLake, William, Hamilton, Arthur S. Personality Studies and the Personal Equation of the Aviator. Mental Hygiene, II, October, 1918.
Paul, B. Beobachtungen über Nachtblindheit im Felde. München med. Wchnschr., 1915, v. 62, pp. 1548-1550.
Paul, B. Zur Therapie der Nachtblindheit. Rev. München med. Wchnschr., 1915, v. 622, p. 1707.
Paulian, Démétre. Hémiparaplégie fonctionnelle gauche avec troubles de la sensibilité et abolition du réflexe cutané plantaire. Rev. neurol., Par., 1914-15, v. 222, pp. 431-433.
Paulian. Sur quelques cas d’hémiplégie cérébelleuse. Rev. neurol., Par., 1916, v. 23, pp. 18-20.
Payne, Charles R. and Jelliffe, S. E. War neuroses and psychoneuroses. Jour. Nerv. and Ment. Dis., 1918, xlviii, 246, 325.
Pegler, L. H. Case of nervous or functional aphonia. Proc. Roy. Soc. Med., Lond., 1915-16, v. 9 (sec. Laryngol.), pp. 118-120.
Pelissier, A. et Borel, P. Hémiplégie spinale avec troubles de la sensibilité homolatéraux. Rev. neurol., Par., 1914-15, v. 222, pp. 125-127.
Pellacani, Giuseppe. Sulla nosografia di alcune neuropatie caratterizzati da sindromi accessuali epilettoidi. Riv. di patol. nerv., Firenze, 1917, v. 22, pp. 131-172.
Pelz. Ueber hysterische Aphonen. (Arch. f. Psych., 1916, v. 57, No. 2, pp. 445-465.) Rev. Berl. klin. Wchnschr., 1916, No. 6, p. 434.
Pemberton, Hugh S. The psychology of traumatic amblyopia following the explosion of shells. Lancet, Lond., 1915, i, p. 967.
Penhallow, Dunlap P. Mutism and deafness due to emotional shock and etherization. Boston M. and S. J., 1916, 174, p. 1311.
Penhallow, Dunlap P. Military surgery. 1916, London, Henry Frowde, pp. 367-398.
Pensions for Mentally Incapacitated. Brit. M. J., Lond., 1915, i, p. 820.
Perls, W. Beitrag zur Symptomatologie und Therapie der Schädelschüsse (Nach Beobachtungen in den Heimatlazaretten). Bruns’ Kriegschir. Hefte d. Beitr. z. Klin. Chir., Tübing, 1917, 105, 435.
Peterson, Joseph and David, Quentin J. The psychology of handling men in the army. Perine Book Co., 1918.
Pfersdorff. Ueber paranoide Erkrankungen im Felde. Neurol. Centralbl. Nr. 16, 1918.
Pflugradt, R. Ueber Schädeldefekte. Ein Beitrag zur Behandlung der Schädelschüsse in den Heimatlazaretten. Bruns’ Kriegschir. Hefte d.
Pförringer. Psychische Erkrankungen nach Typhus (Abstract). Deutsche med. Wchnschr., Berl. u. Leipz., 1915, v. 41, p. 331.
Phocas, D. Accident produit par l’éboulement. Bull. et mém. Soc. de chir. de Par., 1916, v. 42, pp. 2839-2840.
Phocas, et Gutman, R. A. L’hémiplégie pleurale traumatique. Bull. et mém. Soc. méd. d’hôp. de Par., 1915, v. 39, pp. 329-335.
Physical qualities of aviators. Jour. A. M. A., 1918, lxiv, 37.
Physical tests for airmen are novel and exciting. N. Y. Med. Jour., 1918, cviii, 690.
Physical treatment for disabled soldiers. Lancet, Lond., 1916, i, pp. 691-694.
Pick, A. Der Krieg und die Reservekräfte des Nervenssystem. Samml. zwangl. Abhandl. a. d. Geb. d. Nerv. u. Geisteskr., Halle a. S., 1916, v. 11, No. 5, pp. 1-27.
Pick, W. (Simulation of venereal disease.) Med. Klin., Berl. u. Wien, 1917, No. 6, pp. 148-151. Rev. J. Roy. Nav. M. Serv., Lond., 1917, Oct., pp. 497-498.
Piéron, Henri. “Hyperesthésie” signifie toujours “Hyperalgésie.” Rev. neurol., Par., 1914-15, v. 221, pp. 947-951.
Pierre-Robin, Dr. Mécanothérapie fonctionnelle. J. de méd. et de chir. prat., Par., 1916, v. 87, pp. 309-320.
Pighini, G. Il servizio neuro-psichiatrico nella zona di guerra. Ann. di manic. prov. di Perugia (1915), 1917, v. 9, pp. 49-55.
Pighini, G. Contributo alla clinica e patogenesi delle psiconeurosi emotive osservate al fronte. Riv. sper. di freniat., Reggio-Emilia, 1916-17, xiii, 298-343.
Pilca, A. Zur Aetiologie und Behandlung der progressiven Analyse nebst einigen kriegspsychiatrischen Erfahrungen. Wien. klin. Wchnschr., 1915, v. 28, p. 633.
Piotrowski. Traumatische Neurosen. Neurol. Centralbl., Leipz., 1915, v. 34, pp. 591-592.
Pitres, A. Discussion de la conduite à tenir vis-à-vis des blessures du crâne—par P. Marie. Rev. neurol., Par., 1916, v. 29, pp. 470-471.
Pitres, A. Étude sur les principales causes d’erreurs de diagnostic dans les paralysies des membres consécutives aux blessures des nerfs. J. de méd. de Bordeaux, 1917, v. 88, pp. 239-247.
Pitres, A. La valeur des signes cliniques permettant de reconnaître dans les blessures des nerfs périphériques: A. La section complète du nerf; B. La restauration fonctionnelle. Soc. de Neurol. April 6, 1916. Revue Neurol. April-May, 1916.
Pitres, A. Sur les processus histologiques qui president à la cicatrisation et à la restauration fonctionnelle des nerfs traumatisés. Journ. de Méd. de Bordeaux, Dec., 1915.
Pitres, A. et Marchand, L. Quelques observations de syndrômes commotionnels simulant des affections organiques du système nerveux central (méningite, paralysie générale, lésions cérébelleuses, sclérose en plaques, tabes). Rev. neurol., Par., 1916, v. 23, pp. 298-311.
Placido, C. Delinquenza militaire in pace ed in guerra. Ann. di manic. prov. di Perugia (1915), 1917, v. pp. 25-47.
Plantier. Une application médicale de l’esperanto comme moyen de rééducation psychique. Paris méd. (Part. paraméd.), 1916, v. 22, pp. 195-197.
Podiapolsky. Application de la suggestion hypnotique dans la pratique des hôpitaux militaires. (Jour. de neurop. et psychiat. de S. S., Korsakoff, 1916, fasc. 2), Rev. neurol., Par., 1917, v. 24, pp. 477-478.
Podiapolsky, P. P. La suggestion hypnotique à l’hôpital de camp. Paris méd., 1917, No. 34, pp. 165-170.
Podmaniczky, B. T. von. Die Lumbalpunktion als therapeutische Hilfsmittel bei gewissen Formen der Kriegshysterie. Wien. klin. Wchnschr. 1916, xxix, 1396.
Podmaniczky, T. Einige interessante Fälle von Kriegsneurosen. Pest. med.-chir. Presse, Budapest, 1915, v. 51, p. 81.
Podmaniczky. Die Lumbalpunktion als therapeutische Hilfsmittel bei gewissen Formen von Kriegshysterie. Wien. klin. Wchnschr., 1916, v. 29, No. 44, p. 1396.
Pollosson et Collet. Epilepsie partielle continue d’origine traumatique. Trépanation. Guérison. Rev. neurol., Par., 1914-15, v. 222, pp. 291-295.
Popoff, N. F. (Rare case of self injury to avoid military service). Voyenno Med. J., Petrogr., 1915, v. 242, med. spec. pt., pp. 288-292.
Poppelreuter, Walter. Psychische Ausfallserscheinungen nach Hirnverletzungen. Aertzl. Centralbl. Zeit., 1915, v. 27, p. 152. Also München. med. Wchnschr., 1915, v. 62, pp. 489-491.
Porak, René. Nouveaux signes physiologiques des psychonévroses de guerre. Compt. rend. Soc. de biol., Par., 1916, v. 792, pp. 630-634.
Porot, A. Les bases de l’expertise mentale dans les bataillons d’Afrique et les groupes spéciaux en temps de guerre. Rev. neurol., Par., 1916, v. 23, pp. 24-27.
Porot, A. Les bases de l’expertise mentale dans les bataillons d’Afrique et des groupes spéciaux en temps de guerre. (Aptitude au service et responsabilité). Caducée, Par., 1916, v. 16, pp. 85-87.
Porot, A. Sur les accidents nerveux déterminés par la déflagration de fortes charges d’explosifs. Rev. neurol., Par., 1916, v. 29, pp. 603-605.
Porot and Gutmann, R. A. Centre neurologique de la 19e région (Alger). Rev. neurol., Par., 1916, v. 23, pp. 726-733.
Porot et Gutmann. Les psychoses du paludisme. Paris méd., 1917, 7, 518-22.
Porter, W. T. and Emerson, E. Wound shock and the vasomotor center. Bos. M. and S. J., 1918, clxxix, 275.
Porter, William Townsend. Shock at the Front. Atlantic Monthly Press, 1918.
Porter, W. T. Shock at the front. Boston M. and S. J., 1916, v. 175, pp. 854-858.
Porter, William T. Traumatic shock. Bos. M. & S. J., 1918, clxxviii, 657.
Porter, W. T. Further observations on shock at the front. Boston M. and S. J., 1917, v. 177, pp. 327-328.
Previously insane recruit. N. York M. J., 1916, v. 104, p. 857.
Pribram, B. O. Erfolge und Misserfolge bei der operativen Behandlung der Schädelschüsse, besonders der Durchschüsse. Wien. klin. Wchnschr., 1915, v. 28, pp. 1025-1028.
Priest, E. Massage in the after-treatment of the wounded. Lancet, Lond., 1915, ii, p. 1052.
Prince, Morton. Prevention of so-called shell shock. J. Am. M. Ass., Chicago, 1917, v. 69, pp. 726-727.
Privat, J. La mécanothérapie de guerre. Bull. Acad. de méd., Par., 1915, v. 73, pp. 411-416. Also Rev. gén. de clin. et de thérap., Par., 1915, v. 29, pp. 219, 234, 250, 266.
Privat, J. La méchanothérapie de guerre. 1915, Paris, A. Maloine.
Problem, (The) of the insane sailor and soldier. Lancet, Lond., 1917, ii, 612.
Proctor, A. P. Three cases of concussion aphasia: treatment by general anesthesia. Lancet, Lond., 1915, ii, p. 977.
Prozoroff, L. A. (Organization of aid to insane soldiers). Psikhiat. Gaz., Petrogr., 1915, v. 2, p. 167.
Prusenko, A. I. (Conditions of nervous and insane soldiers in the Caucasian front). Psikhiat., Mosk., 1915, v. 9, pp. 291-293.
Pruvost, L. P. Les débiles mentaux à la guerre. Leur utilisation. Thèses de Paris, 1915-16, v. 10, No. 23.
Psyche und Kriegserfahrungen. Discussion von Bonhoeffer, Meyer. Berl. klin. Wchnschr., 1916, v. 532, pp. 1206-1207.
Psychiatrie und Krieg. Psychiat. neurol. Wchnschr. Halle a. S., 1914-1915, v. 16, pp. 284-285.
Psychological Examining in the Army. Amer. Jour. Med. Sc., 1918, clv, 128.
Purser, F. C. Shell shock. Report of Section of Medicine of the Royal Academy of Medicine in Ireland. Brit. M. J., 1917, ii, p. 81.
Purser, F. C. Shell shock. Dublin J. M. Sc., 1917, v. 144, p. 206.
Quaet-Faslem. Die allgemeine nervöse Erschöpfung. Psychiat.-neurol. Wochnsch., 19, 1917-8.
Quidot, L. Deux épreuves pratiques pour dépister les simulateurs de surdité. Presse méd., Par., 1917, v. 25, p. 515.
Rablossky. (War hysteria, traumatic neuroses). Wien. klin. Wchnschr., 1916, v. 29, p. 1616.
Radcliffe, Frank. Hydrotherapy as an agent in the treatment of convalescents. Brit. M. J., Lond., 1916, ii, p. 554.
Raether, M. Neurosen-Heilungen nach der “Kaufmann-Methode.” Arch. f. Psychiat., Berl., 1917, 57, 489-518.
Raether, M. Ueber psychogene “Ischias-Rheumatismus” und “Wirbelsäulenerkrankungen.” Arch. f. Psychiat., Berl., 1917, 57, 772-791.
Raeuber. Die Beschäftigung und Arbeitverwendung der Kriegsbeschädigten auf Grund eigener Erfahrung. Ztschr. f. Med. Beamte, Berl., 1917, 30, 441.
Raffaele, R. Considerazioni su una centuria di casi di patomimia cutanea (durante un anno dell’attuale campagna, 1915-16). Gior. ital. d. mal. ven., Milano, 1916, li, 415-420.
Raffegeau, du Vésinet. Note sur un cas de séton du crâne par balle de mitrailleuse. Ann. méd.-psychol., Par., 1917, v. 73, pp. 101-104.
Raimann, E. Ein Fall von “Kriegspsychose.” Wien. klin. Wchnschr., 1916, v. 29, pp. 42-47.
Ramond et De la Grandière. Troubles de la sensibilité au cours de la diphthérie. L’hystérie diphthérique. Presse méd., Par., 1916, v. 24, p. 523.
Ramsay, A. M., Grant, Dundas, Whale, H. L., West, C. E. Injuries of eyes, nose, throat and ears. London, 1915, Oxford Press, 160 pp., 12o.
Rautenberg, H. Wert der Abderhaldenschen Dialysieverfahrens für die Kriegspsychiatrie. Deutsche Mil. arztl. Ztschr., Berl., 1917, 46, 417-23.
Raujard, L. Les surdités par obusite. Bull. Acad. de méd. de Par., 1916, v. 75, pp. 195-198.
Ravaut, Paul. Les hémorragies internes produites par le choc vibratoire de l’explosif. Presse méd., Par., 1915, v. 23, p. 114.
Ravaut, Paul. Les blessures indirectes du système nerveux déterminés par le “vent de l’explosif.” Presse méd., Par., 1915, v. 23, pp. 313-315.
Ravaut, Paul. Étude sur quelques manifestations nerveuses déterminés par le “vent de l’explosif.” Bull. Acad. de méd., Par., 1915, v. 73, pp. 717-720.
Ravaut, P. et Reniac. Intoxication par les gaz asphyxiants; Diphthérie secondaire méconnue; Paralysie diphthérique généralisée avec réaction méningee. Bull. et mém. Soc. méd. des hôp. de Paris, 1917, 3 ser., 41, 1190-2.
Rawling, L. Bathe. Surgery of the head. 1915, London, Henry Frowde.
Rawling, L. Bathe. Surgery of the Head. Oxford War Primers, 1915.
Raynal, Albert J. L. La rééducation motrice chez les blessés de guerre. Thèses de la Faculté de Paris, 1915-16, v. 11.
Raynaud. Contracture hystérique du membre supérieur droit avec oedème. Réunion médicale VI armée, 4 août, 1915, et Presse méd., 1915.
Raynier. Les états dépressifs et les états mélancoliques chez les militaires pendant la guerre. J. de méd. et de chir., 1915, Feb., v. 86.
Raymond, Victor. Les déséquilibrés mentaux dans l’armée. Ann. d’hyg., Par., 1914, v. 22, pp. 305-330.
Rebierre, Paul. Un centre psychiatrique d’armée. Arch. de méd. et pharm. mil., Par., 1916, v. 65, pp. 434-454.
Rebierre. Discussion de la conduite à tenir vis-à-vis des blessures du crâne—par P. Marie. Rev. neurol., Par., 1916, v. 29, p. 473.
Rebierre. Sur les accidents nerveux determinés par la déflagration de fortes charges d’explosifs. Rev. neurol.. Par., 1916, v. 29, pp. 597-598.
Reconstruction hospitals and orthopedic surgery. Science, N. Y. and Lancaster, Pa., 1917, n. s., v. 46, p. 305.
Reconstruction Hospitals. Boston M. and S. J., 1917, i, p. 744.
Recherche de l’acide picrique dans les urines et dans les viscères. Soc. de méd. lég. de France, Bull., Par., 1916, v. 12, pp. 42-47.
Redlich, Emil. Einige allgemeine Bemerkungen über den Krieg und unser Nervensystem. Med. Klin., Berl. u. Wien, 1915, v. 111, pp. 467-473.
Redlich, Emil. Bemerkungen zur Aetiologie der Epilepsie mit besonderer Berücksichtigung der Frage einer “Kriegsepilepsie.” Wien. med. Wchnschr., Nr. 17, 1918.
Rééducation fonctionnelle et rééducation professionnelle des blessés. (A symposium study), 1917, Paris, J. B. Baillière et Fils.
Reeve, E. F. The treatment of functional contracture by fatigue. Lancet, Lond., 1917, ii, pp. 419-421.
Reformatski, N. N. (Care and evacuation of insane soldiers to the rear of the armies of the northwestern front). Russk. Vrach., Petrogr., 1915, v. 14, pp. 677-679.
Reformatski, N. N. (Care and evacuation of insane soldiers from the active armies in the northwestern region). Russk. Vrach., Petrogr., 1916, v. 15, pp. 230-234.
Reformatski, N. N. (Organization at the rear for the care and evacuation of insane soldiers in the northwestern front). Sovrem. Psikhiat., Mosk., 1915, v. 9, pp. 194-198.
Reformatski, N. N. (Care and evacuation of insane warriors of the active army of the northwestern region). Sovrem. Psikhiat., Mosk., 1916, v. 10, pp. 118-128. Also Psikhiat. Gaz., Petrogr., 1916, v. 3, pp. 165-175.
Régis, E. Les troubles psychiques et neuro-psychiques de la guerre. Presse méd., Par., 1915, v. 23, pp. 177-179.
Régis, E. Psychic and neuro-psychic affections in war. Boston M. and S. J., 1916, v. 174, pp. 784-792.
Régis, E. Les aliénés militaires internés du centre psychiatrique de Bordeaux. Statistique et commentaires. Caducée, Par., 1916, v. 16, pp. 55-59.
Régis et Hesnard. Un cas d’aphonie hystérique d’origine émotive. Le rôle pathogéne des émotions oniriques. Journal de Psychologie, mai-juin 1913.
Regnier, P. Organisation scientifique de la rééducation professionnelle des mutilés. Rev. scient., Par., 1916, v. 2, pp. 458-460.
Regnier, P. De la rééducation fonctionnelle des blessés. Rev. de chir., Par., 1916, 4. 35, pp. 668-696.
Renaux, Jules. États confusionnels consécutifs aux commotions des batailles. (Thèse, Paris, 1915), Presse méd., Par., 1916, v. 24, p. 184.
Renon, Louis. L’angoisse de guerre et son traitement. Bull. gén. de thérap., Par., 1915-16, v. 1681, pp. 785-791; also pp. 821-827.
Renon, Louis. L’angoisse de guerre et son traitement. Rev. gén. de clin. et de thérap., Par., 1916, v. 30, pp. 41-43.
Repkewitz. Ueber die Simulation und Uebertreibung. Neurol. Centralbl., 37, Nr. 12, 1918.
Report of Dr. Henry Carre. Glasgow District Mental Hospital, Brit. M. J., Lond., 1916, i, p. 148.
Report. War Disablement Committee. Use of Remedial Baths in connection with other physical methods in the treatment of disabled soldiers. Proc. Roy. Soc. Med., Lond., 1917-18, v. 10 (sec. Balneol.), pp. 78-80.
Resch, H. Geisteskrankheiten und Krieg. Allg. Ztschr. f. Psychiat., Berl., 1915, v. 72, No. 2 and No. 3, pp. 121-133.
Responsabilité des oeuvres de rééeducation des mutilés de guerre au point de vue des accidents. Ann. d’Hyg., Par., 1917, v. 25, pp. 190-192.
Revault d’Allones, G. Le signe achilléen sensitif des affections du nerf sciatique. Press méd., Par., 1917, v. 25, pp. 351-352.
Richet, Ch. “Anesthésie” en dictionnaire de physiologie. Lyon méd., 1915, v. 124, p. 347.
Richet, Ch. Le courage. Rev. sc., Par., 1916, ii, pp. 385-391.
Richet, Ch. Les évènements psychiques de la guerre. Un appel de M. Charles Richet aux soldats; avez-vous des pressentiments? Ann. d. sc. psych., Par., 1916, xxvi, 185-192.
Riddoch, George. Dissociation of visual perceptions due to occipital injuries with especial reference to appreciation of movement. Brain, Lond., 1917, v. 40, pp. 15-57.
Riddoch, George. On the relative perceptions of movement and a stationary object in certain visual disturbances due to occipital injuries. Proc. Roy. Soc. Med., Lond., 1917, v. 10, No. 3 (Sect. Neurol.), p. 13.
Riebeth. Ueber Neurasthenie bei Kriegsteilnehmern. Psychiat.-neurol. Wchnschr., Halle a. S., 1915-16, v. 17, p. 71.
Rietschel, H. Die Kriegsenuresis. Münch. med. Wchnschr., Nr. 26, 1918.
Riggall, Robert M. The treatment of neurasthenia by hypnotism. J. Roy. Nav. M. Serv., Lond., 1917, v. 3, pp. 190-194.
Rimbaud, L. À propos de la méthode de traitement des psychonévroses dite “du torpillage.” Marseille méd., 1916, v. 53, pp. 33-41.
Rimbaud, L. Le traitement des psychonévroses de guerre et des troubles nerveux dits “réflexes.” Marseille med., 1917, v. 54, pp. 817-829.
Rimbaud, L. Les réflexes de percussion plantaire; leur valeur diagnostique. Presse méd., Par., 1917, v. 25, pp. 539-540.
Rippon, T. S. Essential characteristics of successful and unsuccessful aviators. Lancet, Lon., 1918, ii, 411.
Rivers, W. H. R. A case of claustrophobia. Lancet, Lond., 1917, v. 2, pp. 237-240.
Rivers, W. H. R. Freud’s psychology of the unconscious. (Evidence afforded by the war.) Lancet, Lon., 1917, i, 912.
Rivers, W. H. R. Repression of war experience. Proc., Roy. Soc. of Med., Lon., 1918, xi (Sec. of Psychiatry), 1.
Rivers, W. H. R. The repression of war experience. Lancet, Lond., 1918, i, pp. 173-177.
Rivers, W. H. R. War neurosis and military training. Mental Hygiene, II, October, 1918.
Roberts, John B. War surgery of the face. 1919.
Robertson, George M. War and alcohol as exciting factors in the onset of insanity. Med. Officer, Lond., 1915, v. 14, pp. 283-284.
Robin, Pierre. Méthode de prothèse fonctionelle. Caducée, Par., 1916, v. 16, pp. 35-40.
Roches, H. Louis. Extraction magnétique des projectiles intracérébraux. J. de Radiol. et d. electrol. Par., 1916, v. 2, pp. 165-172.
Rochtein, I. D. Contribution à l’étude des soi-disant contusions de guerre et de leur traitement. Médecin russe pratique, No. 24, 1915.
Roemheld, L. Ueber homolaterale Hemiplegien nach Kopfverletzungen. München med. Wchnschr., 1915, v. 621, pp. 600-601.
Roeper, E. Zur Prognose der Hirnschüsse. (Aus dem Marinelazarett Hamburg.) Münch. med. Wchnschr., 1917, 64. Feldartzl. Beil. 4 (Abstract in Centralbl. f. Chir., Leipz., 1917, 44, 1036).
Roger, H. Simulation des oreillons. Rev. gén. de clin. et de thérap., Par., 1916, xxx, 80.
Roger, H. Le choc nerveux. Presse méd., Par., 1916, v. 24, pp. 513-516.
Roger, H. Les pseudo-érysipèles de la face provoqués. Marseille méd., 1916-17, liii, 785-800.
Roger, H. Deux cas de tétanos localisé post-sérique. Marseille méd., 1917, v. 54, pp. 353-363.
Rogues de Fursac, J. Un cas d’émotivité morbide chez un militaire. Rev. neurol., Par., 1914-15, v. 221, pp. 774-776.
Rôle de l’auto-intoxication dans la fatigue. Presse Méd., Par., 1917, v. 25, pp. 142-143 (or 102-103).
Romer, F. Mechano-therapy at the Corydon War Hospital. J. Roy. Army Med. Corps, Lond., 1917, v. 28, pp. 578-585.
Roncoroni, L. Quattro casi di mutismo di guerra. Boll. d. Soc. med. in Parma, 1915, v. 8, pp. 114-117.
Röper. Das Hamburger Marine-Lazarett. Neurol. Centralbl., Leipz., 1915, v. 34, 505-506.
Röper. Funktionelle Neurosen bei Kriegsnehmern. Deutsche mil.-ärtzl. Ztschr., Berl., 1915, Nos. 9-10, p. 752.
Roquette. Sur l’installation et le fonctionnement de l’hôpital-dépôt de convalescence Faucher. Arch. de méd. et pharm. mil., Par., 1914-15, v. 64, pp. 206-232.
Ross, T. A. Prevention of relapse of hysterical manifestations. Lancet, Lon., 1918, ii, 516.
Rosenbach. (Psychoses of war time.) Russk. Vrach., Petrogr., 1915, v. 14.
Rosanoff, A. J. First psychiatric experiences at the National Army Cantonment at Camp Upton, Long Island, N. Y. Med. Rec., N. Y., 1917, xcii, 877.
Rosanoff-Saloff, Mme. Considérations générales sur la camptocormie. N. Iconog. de la Salpêtrière, Par., 1916-17, v. 28, pp. 28-33.
Rose, Felix. Le signe de fessier dans la névralgie sciatique. Presse méd., Par., 1917, v. 25, p. 319.
Rose et Villandre. Cranioplastie cartilagineuse faite après trépanation pour épilepsie Jacksonienne. Lyon méd., 1916, v. 125, p. 348.
Rosenfeld. Ueber Kriegsneurosen, ihre Prognose und Behandlung. Arch. f. Psychiat., Berl., 1917, 57, 221-244.
Roth, E. Kriegsgefahr und Psyche. Aertztl. Sachverst.-Ztg., Berl., 1915, v. 21, pp. 1-3.
Rothacker, A. Einige Fälle von Hyperthyroidismus, darunter drei von akuten Basedow bei Kriegsteilnehmern zur Stutze der neurogenen Entstehung dieser Krankheit. Münch. med. Wchnschr., 1916, No. 3, pp. 99-101.
Rothmann, Max. Ueber isolierte Thermanalgesie eines Beines nach Schussverletzung des obersten Brustmarks. Neurol. Centralbl., Leipz., 1915, v. 34, pp. 153-157.
Rothmann, M. Zur Beseitigung psychogener Bewegungstörungen bei Soldaten in einer Sitzung. München med. Wchnschr., 1916, v. 64, No. 35.
Rottenstein. Les phlegmons provoqués. Marseille méd., 1916-17, lii, 801-807.
Rouge, C. Influence de la guerre actuelle: (1) Sur le mouvement de la population de l’asile de Limoux du 2 août 1914 au 31 décembre 1915; (2) Sur les psychoses des aliénés internés pendant la même époque. Ann. méd.-psychol., Par., 1916, v. 7, p. 425.
Roussy, G. Accidents nerveux produits à distance par éclatement d’obus. Rev. neurol., Par., 1914-15, v. 222, pp. 216-217.
Roussy, G. Boisseau, J. and d’Oelnitz, M. Emotions de guerre. Collection Horizon, Masson et Cie, Paris, 1918.
Roussy, Gustave. Complications of wounds of the spinal cord. War Med., Surg. and Hygiene, 1918, i, 602.
Roussy, G. Psycho-neurological disturbances affecting the limbs, observed during the war. War Med., 1918, ii, 37.
Roussy, G. Surdité-mutité par éclatement d’obus chez trois Zouaves compagnons d’armes. Rev. neurol., Par., 1914-15, v. 222, pp. 394-396.
Roussy, G. À propos de quelques troubles nerveux observés à l’occasion de la guerre (hystérie, hystérie-traumatisme, simulation). Rev. neurol., Par., 1914-15, v. 222, pp. 425-430. Also Presse méd., Par., 1915, v. 23, pp. 115-117.
Roussy, G. Troubles nerveux psychiques de guerre. Presse méd., Par., 1915, v. 23, p. 141.
Roussy, G. Discussion de la conduite à tenir vis-à-vis des blessures du crâne—par P. Marie. Rev. neurol., Par., 1916, v. 29, p. 472.
Roussy, G. Sur la fréquence des complications pleuro-pulmonaires et leur rôle comme facteur de gravité chez les grands blessés nerveux. Bull. Acad. de méd., Par., 1916, v. 75, p. 722-725. Also Presse méd., Par., 1916, v. 24, p. 266.
Roussy, G. Un cas de tumeur de lobe frontal pris cliniquement pour une méningite tuberculeuse. Presse méd., Par., 1916, v. 24, p. 47.
Roussy, G. Des complications pleuro-pulmonaires comme facteur de gravité chez les blessés du crâne et de la moelle par plaie de guerre. Presse méd., Par., 1916, v. 24, p. 47.
Roussy, G. Un cas de paraplégie hystérique datant de 21 mois avec gros troubles vaso-moteurs thermiques et sécrétoires des extrémités inférieures. Rev. neurol., Par., 1917, v. 24, pp. 253-256.
Roussy et Boisseau. Fausse commotion cérébrale. Bégaiement hystérique. Presse méd., Par., 1915, v. 23, p. 391.
Roussy et Boisseau. Les sinistroses de guerre. Accidents nerveux par éclatement d’obus à distance. Presse méd., Par., 1915, v. 23, pp. 452-453.
Roussy et Boisseau. Discussion des accidents nerveux par la déflagration explosifs. Rev. neurol., Par., 1916, v. 23, pp. 577-586.
Roussy et Boisseau. Un centre de neurologie et de psychiatrie d’armée. Paris méd., 1916 (Part. méd.), v. 19, pp. 14-20.
Roussy et Boisseau. Les accidents nerveux déterminés par la déflagration des explosifs. Paris méd., 1916-17, v. 21, pp. 185-191.
Roussy et Boisseau. Sur le pronostic et le traitement des troubles nerveux dits réflexes. Rev. neurol., Par., 1917, v. 24, pp. 516-527.
Roussy et Boisseau. Deux cas de soi-disante commotion labyrinthique par éclatement d’obus à distance. Presse méd., Par., 1917, v. 25, p. 323.
Roussy et Boisseau. Pronostic et traitement des troubles nerveux dits réflexes. Presse méd., Par., 1917, v. 25, p. 374.
Roussy et Boisseau. Deux cas de pseudo-commotion labyrinthique par éclatement d’obus à distance (commotion labyrinthique persévérée simulée ou suggestionnée). Bull. et. mém. soc. méd. d’hôp. de Par., 1917, v. 33, pp. 671-676.
Roussy, Boisseau et Cornil, L. Pseudo-tympanites abdominales hystériques; les catiémophrénoses. Bull. et mém. Soc. méd. d’hôp. de Par., 1917, v. 41, pp. 665-670.
Roussy, Boisseau et d’Oelsnitz. La station neurologique de Salins (Jéna) après trois mois de fonctionnement (Projections de films cinématographiques). Bull. et mém. Soc. méd. d’hôp. de Par., 1917, v. 33, pp. 643-644.
Roussy, Boisseau et d’Oelsnitz. Sur l’influence du facteur psychique dans la guérison des psychonévroses de guerre. Presse méd., Par., 1917, v. 25, pp. 413-414. Also Rev. neurol., Par., 1917, v. 24, pp. 545-553.
Roussy, Boisseau et d’Oelsnitz. Traitement des psychonévroses de guerre. Collection Horizon, Masson et Cie, 1918.
Roussy, Cornil et Leroux. Les manœuvres d’élongation du nerf dans le diagnostic des sciatiques. Presse méd., Par., 1917, v. 25, pp. 506-508.
Roussy, G., Lhermitte, J. The psychonevroses of war. Military Medical Manuals, Univ. of London Press, 1918.
Roussy, G. and Lhermitte, J. Blessures de la moelle et la queue de cheval. Collection Horizon, Masson et Cie, Paris, 1917.
Roussy, G. and Lhermitte, J. Psychonévroses de guerre. Collection Horizon, Masson et Cie, Paris, 1917.
Roussy et Lhermitte. Les psychonévroses de guerre. Ann. de méd., Par., 1916, v. 3, pp. 525-563; also pp. 619-665.
Roussy et Lhermitte, J. La forme hémiplégique de la commotion directe de la moelle cervicale avec lésion de la XIe paire crânienne. Ann. de méd., Par., 1917, v. 4, pp. 458-469.
Roussy et Ichlonski. Mouvements syncinésiques très prononcés chez un hémiplégique organique par blessure de guerre. Rev. neurol., Par., 1914-15, v. 222, pp. 492-494.
Routier. Notes à propos d’un certain nombre de cas de tétanos anormal. Bull. Acad. de méd., Par., 1915, v. 74, pp. 515-516; also pp. 600-611.
Rows, R. G. Mental conditions following strain and nervous shock. Brit. M. J., Lond., 1916, i, pp. 441-443.
Rucker. Le service d’isolement et de psychothérapie à la Salpêtrière pour le traitement des militaires atteints de troubles fonctionnels du système nerveux. J. de méd. et de chir. prat., Par., 1916, v. 87, pp. 90-94.
Rusca, Franchino. Experimentelle Untersuchungen über die traumatischen Druckwirkung der Explosionen. Deutsche Ztschr. f. Chir., 1914-15, v. 132, pp. 315-374.
Russel, Colin K. A study of certain psychogenetic conditions among soldiers. Canad. Med. Ass. J., Montreal, 1917, v. 7, No. 8, pp. 704-720.
Ryan, E. A case of shell shock. Canad. Prac. and Rev., Toronto, 1916, v. 41, pp. 507-510. Also Canad. Med. Ass. J., Montreal, 1915, v. 6, pp. 1095-1099.
S. (C.) Le service d’isolement et de psychothérapie à la Salpêtrière pour le traitement des militaires atteints de troubles fonctionnels du système nerveux. J. de méd. et de chir. prat., 1916, lxxxvii, 90-94.
S. (C.) Les blessures indirectes du système nerveux déterminées par le vent de l’explosif. J. de méd. et chir. prat., Par., 1916, lxxxvii, 436.
Saaler, B. Ueber nervöse und psychische Krankheiten in ihren Beziehungen zum Kriegsdienst. Berl. klin. Wchnschr., 1916, liii, 1389.
Sabrazis. Simulation de méningite cérébro-spinale par les accidents nerveux du 1914, dans deux cas guérison. Gaz. hebd. d. sc. med. de Bordeaux, 1917, v. 38, pp. 134-135.
Sainsbury, H. Treatment of neuritis, with special reference to sciatica. Lancet, Lon., 1917, i, 911.
Salmon, Thomas W. Care and treatment of mental diseases of war neuroses (“shell shock”) in the British Army. Nat. Com. Ment. Hyg., 1917.
Salmon, T. W. Outline of American plans for dealing with war neuroses. War Med., 1918, ii, 34.
Salmon, Thomas W. The care and treatment of mental diseases and war neuroses (“shell shock”) in the British Army. Ment. Hyg., Concord, N. H., 1917, v. 1, pp. 509-547.
Salmon, Thomas W. The use of institutions for the insane as military hospitals. Ment. Hyg., Concord, N. H., 1917, v. 7, pp. 806-812.
Salmon, Thomas W. Recommendations for the treatment of mental and nervous diseases in the United States Army. Psychiat. Bull., Utica, 1917, v. 2, No. 3, pp. 355-376.
Samuel. Neurologische Beobachtungen bei den Truppen. Berl. klin. Wchnschr. 1915, v. 521, pp. 140-141.
Sandberg. Zwei Fälle von traumatischer Hysterie nach Granatsplitterverletzung. Zentralbl. f. Chir., Leipz., 1915, v. 421, pp. 221-222.
Sandoz, F. Le mécanothérapie des raideurs articulaires consécutifs aux blessures de guerre. Paris méd., 1914-15 (Part. méd.), v. 15, p. 408.
Sänger. Ueber die durch den Krieg bedingten Folgezustände im Nervensystem. Deutsche med. Wchnschr., Berl. u. Leipz., 1915, ii, p. 815. Also Berl. klin. Wchnschr., 1915, v. 421, p. 277, and Neurol. Centralbl., Leipz., 1915, v. 34, pp. 364-366.
Sänger and Cimbal. Nervöse Erkrankungen im Kriege. Deutsche med. Wchnschr., Leipz. u. Berl., 1915, v. 41, p. 902; also 933-935.
Sarbó, A. v. Ueber den sogennanten Nervenschock nach Granat- und Schrapnell-explosionen. Wien. klin. Wchnschr., 1915, v. 28, pp. 86-91. Also Psychiat.-Neurol. Wchnschr., Halle a. S., 1914-15, v. 16, pp. 429-431, and München. med. Wchnschr., 1915, v. 621, p. 230.
Sarbó, A. Ueber die durch Granat- und Schrapnell-explosionen entstandenen Zustandsbilder. Ibid., 608-616.
Sarbó, A. v. (Nerve shock following grenade and shrapnel explosions). Orvosi hetil., Budapest, 1915, v. 59, pp. 45-48.
Sarbó, A. v. Durch Schrapnel- und Granatexplosion herbeigeführter sogenannter Nervenschock. Pest. med. chir. Presse, Budapest, 1915, v. 51, p. 21.
Sargeant, P. and Holmes. Report of the later results of gunshot wounds of the head. J. Roy. Army Med. Corps, Lond., 1916, v. 57, pp. 300-311.
Sauer, W. Enuresis und Hypnose im Felde. München med. Wchnschr., 1916, v. 63, pp. 102-103.
Savage, George H. Mental disabilities for war service. J. Ment. Sc., Lond., 1916, ii, p. 42; also v. 62, pp. 653-657.
Savage, George H., Sir. Mental war cripples. Practitioner, 1918, c. 1.
Savariaud. À propos des phlegmons provoqués par les injections de pétrole. Bull. et mém. Soc. de chir. de Par., 1915, n. s., xli, 2364.
Sawdon. Treatment by physical methods of mental disabilities induced by the war. Proc. Roy. Soc. Med., Lond., 1917-18, v. 10 (sect. Balneol.), pp. 42-44.
Sayer, Ettie. The organization of electrotherapy in military hospitals. Proc. Roy. Soc. Med., Lond., 1915-16, v. 9 (Electro-therap. sect.), p. 39.
Scarisbrick, W. Cardiac diseases in soldiers and recruits. Brit. Med. Jour., 1917, i, 254.
Schermers, D. Oorlogsneurosen en Psychosen. Med. Weekbl., Amst., 1916-17, v. 23, pp. 109-112.
Schier, A. R. A further study of mental tests in the examination of recruits. U. S. Nav. M. Bull., Wash., 1917, v. 9, pp. 325-333.
Schiffbauer, H. E. Operative treatment of gunshot injuries to the peripheral nerves. S. G. O., 1916, xxii, 133.
Schlachter, J. Psychogener Stridor bei Soldaten. Ztschr. f. Ohrenheilh., 77, 1918.
Schlayer. Vorschläge zur Versorgung der funktionellen Neurosen. München med. Wchnschr., 1916, No. 46, pp. 1645-1646.
Schlayer. Die Versorgung der funktionellen Kriegsneurosen. München med. Wchnschr., 1917, No. 1, p. 39.
Schlendler, L. Schädelverletzungen. Bruns’ kriegschir. Hefte d. Beitr. z. klin. Chir., Tübing., 1916, 103, 500.
Schlesinger, H. Fall von hochgradiger retrograder Amnesie nach Gehirnverletzung. Wien. med. Wchnschr., 1915, No. 49, p. 1815.
Schlesinger, H. Hochgradige retrograde Amnesie nach Gehirnverletzung. Wien. klin. Wchnschr., 1915, xxviii, 1329.
Schlesinger, H. Epilepsie und Anfall Temperaturerhöhungen. Klin, therap. Wchnschr., Wien u. Berl., 1916, v. 332, p. 29.
Schmidt, G. B. Chirurgische Behandlung der Kriegsverletzungen peripherischer Nerven. Deutsche med. Wchnschr., Berl. u. Leipz., 1915, v. 412, pp. 1263-1264.
Schmidt, W. Die psychischen und nervösen Folgezustände nach Granatexplosionen und Minenverschüttungen. Ztschr. f. d. ges. Neurol. u. Psychiat., Berl. u. Leipz., 1915, v. 29, pp. 514-542.
Schneider, E. Zur Klinik und Prognose der Kriegsneurosen. Wien. klin. Wchnschr., 1916, v. 29, pp. 1295-1303.
Scholtz, W. Funktionelle Sprachlähmung im Felde. Med. Klin., Berl., 1915, v. 111, pp. 1423-1424.
Schröder, P. Traumatische Psychosen. Monatschr. f. Psychiat. u. Neurol., Berl., 1915, No. 4, pp. 193-201.
Schüller, A. Pulsus paradoxus respiratorius. Klin. therap. Wchnschr., Wien u. Berl., 1916, v. 32, pp. 28-29.
Schüller, A. Hypertrichose bei Ischiadicusläsionen. Wiener med. Wchnschr., Nr. 46, 1917.
Schultz, J. H. Einige Bemerkungen über Feindschaftsgefühle im Felde. Neurol. Centralbl., Leipz., 1915, v. 34, pp. 373-378.
Schultz, J. H. Wege und Ziele der Psychotherapie. Therap. Monatschr. Berl., 1915, No. 8, pp. 443-450.
Schultz, J. H. Fünf neurologisch bemerkungswerte Hirnschüsse. Monatschr. f. Psychiat. u. Neurol., 1916, v. 39, No. 6, p. 319.
Schultz, J. H. and Meyer, Robert. Zur klinischen Analyse der Granatschockwirkung. Med. Klin., Berl. u. Wien, 1916, v. 12, pp. 230-233.
Schultze, Otto. Ueber die Kaufmanns’sche Behandlung hysterischen Bewegungsstörungen. Münch. med. Wchnschr., 1916, No. 38, pp. 1349-1353.
Schuster. Kriegsneurologische Demonstrationen. Neurol. Centralbl., Leipz., 1915, v. 34, pp. 1914-1916.
Schuster. Crampusneurose. Neurol. Centralbl., Leipz., 1915, v. 34, p. 72.
Schuster. Entstehen der traumatischen Neurosen oder Psychosen? Neurol. Centralbl., Leipz., 1916, v. 35, No. 12.
Schuster. Kriegsneurologische Demonstrationen. Berl. klin. Wchnschr., 1916, No. 1, pp. 24-25.
Schuster, Bonhoeffer, Oppenheim. Diskussion—Zerebellare Symptomen-Komplexe nach Kriegsverletzungen. Neurol. Centralbl., Leipz., 1915, v. 34, pp. 664-666.
Schuster. Der Mechanismus der hysterischen Skoliose. Neurol. Centralbl., Leipz., 37, Nr. 18, 1918.
Sebileau, Pierre. Monoplégie du membre inférieur, conséquence d’un coup de feu de la cuisse sans blessure apparente de l’appareil d’innervation. Bull. et mém. Soc. de chir. de Par., 1914-15, v. 40, pp. 1175-1177.
Seelert, H. Ueber Neurosen nach Unfällen mit besonderer Berücksichtigung von Erfahrungen im Kriege. Monatschr. f. Psychiat. u. Neurol., Berl., 195, v. 38, pp. 328-340.
Seelert, H. Differentialdiagnose der Hysterie und des progressiven Torsionspasmus. Arch. f. Psychiat., Berl., 1918, v. 56, pp. 684-688.
Seeuwen, H. J. Heart and active service. Lancet, Lon., 1916, ii, 432.
Seeuwen, H. J. Treatment of the wounded by means of electricity. Arch. of Radiol. and Electrotherap., 1917, xxii, 136.
Segaloff, T. E. Contribution à l’étude des lésions organiques et fonctionnelles dans les contusions par éclatements d’obus. Psychiatrie contemporaine russe, 1015; Revue Neurol. 1914-15, II, p. 1081-1082.
Segaloff, T. E. Nature of contusions caused by artillery fire. Morbus decompressionis. Sovrem. Psikhiat., Mosk., 1915, ix, 103, 263, 405.
Segaloff, T. E. (de Moscou.) Contribution à la connaissance de la nature des contusions par les obus actuels. Psychiatrie contemp. russe, 1915.
Self-mutilation by soldiers. Brit. M. J., Lond., 1915, i, p. 899.
Sencert, L. Rupture des deux poumons par le “vent du boulet.” Bull. et mém. Soc. de chir. de Par., 1915, v. 41, pp. 79-82.
Sensory phenomena in head injuries. Brit. M. J., Lond., 1915, i, p. 738.
Seppilli, G. Guerra e psicopatie. Gazz. med. d. Marche, Ancona, 1915, v. 23, No. 6, p. 3.
Seppilli, G. I disturbi mentali nei militari in rapporto alla guerra. Riv. ital. di neuropat. etc., Catania, 1917, v. 10, pp. 105-114; also pp. 137-141.
Sereysky, M. J. (A contribution to the problem of poisoning by German asphyxiating gas: Their influence in the nervous psychic condition of the asphyxiated.) Russk. Vrach., Petrogr., 1917, v. 16, p. 401.
Sérieux, P. et Laignel-Lavastine. Sur utilité de mesures spéciales pour les anormaux psychiques constitutionnels en temps de guerre. Bull. méd., Par., 1917, v. 31, pp. 11-12.
Serog. Zwei Fälle von krankhafter Selbstbesichtigung der Simulation. Med. Klin., Berl., 1916, xii, 1100-1102.
Serre, Biron and Brette. Tentative de fraude au moyen de l’ovoalbumine (simulation de l’albuminurie). Arch. de méd. et pharm. mil., Par., 1917, lxviii, 935-939.
Service d’isolement et de psychothérapie à la Salpêtrière pour le traitement des militaires atteints de troubles fonctionnels du système nerveux. J. de méd. et chir. prat., Par., 1916, v. 87, pp. 90-94.
Sforza, N. Le sindromi nervose di commozione da scoppio de granata. Med. nuova, Roma, 1916, v. 7, pp. 6-10.
Sgobbo, F. P. La röntgenologia causa di turbamento psichico nei militari, ed utile mezzo per la diagnosi di alcuni male simulati. Radiol. med., Torino, 1916, v. 3, pp. 313-317.
Shaikevich, M. O. (Neuro-mental disease in time of war and its prevention.) Sibirsk. Vrach., Tomsk, 1915, v. 2, pp. 35-39.
Shairp, L. V. The reëducation of disabled soldiers. Am. J. Care Cripples, N. Y., 1917, v. 4, pp. 201-211.
Shangengberg, E. (War injuries affecting the voice and speech.) Hygiea, Stockholm, 1917, v. 79, p. 49.
Sheehan, R. Malingering in mental disease. U. S. Nav. M. Bull., Wash., 1916, x, 646-653.
Shell explosions and the special senses. Lancet, Lond., 1915, i, p. 663.
Shell shock and neurasthenia. Lancet, Lond., 1916, i, p. 627.
Shell shock. Am. med., Burlington, Vt., 1917, v. 23, pp. 606-607.
Shell shock among troops. Bos. M. and S. J., 1918, clxxviii, 133.
Shell shock patients in air raids. Brit. M. J., Lond., 1918, i, p. 90.
Shufflebotham, Frank. The effects of military training upon lead workers. Brit. M. J., Lond., 1915, i, p. 672.
Shumkoff, G. E. (Number of the insane in the war.) Psikhiat. Gaz., Petrogr., 1915, v. 2, pp. 363-366.
Shumkoff, G. E. (Rapid psychiatric aid in the war.) Psikhiat. Gaz., Petrograd, 1916, v. 3, pp. 281-288.
Shuttleworth, G. War and insanity. J. Ment. Sc., Lond., 1916, v. 62.
Sicard, J. A. Blessures de guerre. Traitement de certaines algies et acrocontractures rebelles par l’alcoolisation nerveuse locale. Soc. méd. des Hôpitaux, 17 decembre 1915.
Sicard. Simulateurs de création et simulateurs de fixation. Simulateurs sourds-muets. Paris méd., 1915, v. 17 (Part. méd.), pp. 423-428.
Sicard. Traitement de la névrite douloureuse du médian par l’alcoolisation tronculaire sus-lésionnelle. Soc. Méd. de Hôp., July 9, 1915; Traitement de certaines algies et acrocontractures rebelles par l’alcoolisation nerveuse locale. Ibid., Dec. 17, 1915.
Sicard. Traitement des névrites douloureuses de guerre causalgies par l’alcoolisation nerveuse locale. Presse méd., juin, 1916.
Sicard. Examen du liquide céphalo-rachidien au cours des commotions par “vent d’explosif.” Paris méd., 1915, v. 17, p. 556.
Sicard. Plicatures vertébrales par “vent d’obus.” Spondyloses et attitudes vertébrales antalgiques. Examen du liquide céphalo-rachidien. Soc. méd. des Hôpitaux, 9 juillet, 1915.
Sicard. Spondylites par obusite ou vent d’obus. Attitudes vertébrales antalgiques. Bull. et mém. Soc. méd. d. hôp. de Paris, 1915, v. 39, p. 582.
Sicard. À propos du procès-verbal et de la communication de MM. Souques, Mégévand et Donet sur l’examen du liquide céphalo-rachidien (séance du 29 octobre, 1915) au cours des commotions par vent d’explosif. Bull. et mém. Soc. méd. d. hôp. de Par., 1915, x. s. xxxix, 1034.
Sicard. L’alcoolisation tronculaire au cours des acromyonties rebelles du membre supérieur. Paris méd., 1916, v. 19, 509-512.
Sicard. Discussion de la conduite à tenir vis-à-vis des blessures du crâne—par P. Marie. Rev. Neurol. Paris, 1916, v. 29, p. 462.
Sicard et Cantaloube. Les oedèmes de striction. Soc. méd. des Hôpitaux, 26 mai 1916.
Sicard et Cantaloube. Les réflexes musculaires du pied et de la main (myo-diagnostic mécanique). Presse méd., Par., 1916, v. 24, pp. 145-147.
Sicard et Cantaloube. Réflexes musculaires pédo-dorsaux. Leur valeur diagnostique et pronostique. Soc. de Neurol. 3 février 1916.
Sicard, J. A., Roger, H. and Rimbaud, L. Syncinésie d’effort; réactions syncinétiques par choc du liquide rachidien sur le faisceau pyramidal dégéneré. Ibid., 1917, 3. s, xli, 619-622.
Siciliano. Les tropho-névroses traumatiques. Rivista critica di clinica medica, Nos. 19, 20 et 21.
Signorelli e Buscaino. Bradicardia e riflesso oculo-cardiaco nella dissenteria amoebica. Riv. di patol. nerv. e ment., 1917, 22, 487-90.
Siege, Max. Typhuspsychosen im Felde. Neurol. Centralbl., Leipz., 1915, v. 34, pp. 291-296.
Silberstein, Adolf. Kriegsenvalidenfürsorge und staatliche Unfallfürsorge. Würzb. Abhandl. a. d. Gesamt.-geb. d. prakt. Med., 1915, v. 15, pp. 119-130, and pp. 135-148.
Silberstein. The Royal Orthopedic Reserve Hospital at Nürnberg, Germany. Am. J. Cripples, N. Y., 1917, v. 4, pp. 188-191.
Silex, P. Neue Wege in der Kriegsblindfürsorge. 2 Aufl., Berl., 1916, S. Karger, 8o.
Silver, D. The function of orthopedic surgery in the present war. Am. J. Orthop. Surg., Bost., 1917, v. 15, pp. 509-511.
Similarity of War Neuroses to Accident Neuroses. Brit. M. J., Lond., 1915, i, p. 1072.
Simple method of detecting simulated deafness. Lancet, Lond., 1917, ii, 369.
Singer, Kurt. Wesen und Bedeutung der Kriegspsychosen. Berl. klin. Wchnschr., 1915, v. 52, pp. 177-180.
Sklyar, N. I. (The war and mental diseases). Sovrem. Psikhiat., Mosk., 1916, v. 10, p. 98, p. 157, p. 453.
Small, C. P. Equilibrium tests for aviation recruits. Jour. A. M. A., 1917, lxix, 1078.
Smirkoff, D. Deux cas graves de névrose traumatique par contusion, guéris par la suggestion hypnotique. Jour. de neurop. et psychiat. de S. S. Korsakoff, 1916, fasc. 2, also Rev. neurol., Par., 1917, v. 24, p. 477.
Smith, G. E. Shock and the soldier. Lancet, Lond., 1916, i, pp. 813-817, and pp. 853-857.
Smith, G. E. and Pear, T. H. Shell shock and its lessons. Nature, Lond., 1917, v. 100, pp. 64-66.
Smith, G. E. and Pear, T. H. Shell shock and its lessons. 1917, Manchester, University Press.
Smith, Percy. War and insanity. J. Ment. Sc., Lond., 1916, v. 62, pp. 815-817.
Smith, Percy. Civilian mental disease in wartime. Proc. Roy. Soc. Med., Lond., 1916, v. 10, pp. 1-20.
Smyly, C. P. Shell shock. Dublin, J. M. Sc., 1917, v. 142, pp. 247-256.
Sogenannten funktionellen Nervenerkrankungen der Kriegsteilnehmer. Jahresb. f. ärztl. Fortbild, München, 1915, v. 6, pp. 26-27.
Soldats aveugles masseurs. Caducée, Par., 1917, v. 11, p. 12.
Soldat mendiant. Ann. méd. psychol., Par., 1914-1915, v. 6, p. 527.
Sollier, P. Discussion de la conduite à tenir vis-à-vis des blessures du crâne—par P. Marie. Rev. neurol., Par., 1916, v. 29, pp. 63-64. Also p. 473.
Sollier. Sur les accidents nerveux déterminés par la déflagration de fortes charges d’explosifs. Rev. neurol., Par., 1916, v. 29, pp. 575-576.
Sollier. Troubles trophiques osseux dans un cas d’hémiplégie hystérique. Lyon méd., 1916, v. 125, pp. 20-21.
Sollier. Impotence fonctionnelle d’origine nerveuse chez les blessés de guerre. Bull. Acad. de méd., Par., 1914, v. 72, pp. 346-347.
Sollier. Trois cas d’hémiplégie hystérique consécutive à des lésions craniocérébrales. Lyon méd., 1915, v. 124, p. 334.
Sollier. La neurologie de guerre: Décisions prises aux trois réunions des chefs des centres neurologiques. Lyon méd., 1916, v. 125, p. 339.
Sollier. Un cas de canitie par commotion et émotion. Lyon méd., 1916, v. 125, p. 329.
Sollier. Persistance des troubles fonctionnelles pendant le sommeil. Rev. neurol., Par., 1914-15, v. 222, p. 1240.
Sollier. Sur l’abolition du réflexe cutané plantaire dans les paralysies ou contractures fonctionnelles. Rev. neurol., Par., 1914-15, v. 222, pp. 1280-1283.
Sollier. Du diagnostic clinique de l’exagération et de la persévérance des troubles nerveux fonctionnelles. Presse méd., Par., 1915, v. 23, pp. 505-507.
Sollier. Statistique des cas de névrose dus à la guerre. Bull. Acad. de méd., Par., 1915, v. 73, pp. 682-684.
Sollier. Diagnostic des contractures hystéro-traumatiques et des rétractions. Lyon méd., 1917, v. 126, pp. 93-96.
Sollier. Mécanothérapie et rééducation motrice au point de vue psycho-physiologique et moral. Paris méd., 1917, No. 38, pp. 246-249.
Sollier et Chartier. La commotion par explosifs et ses conséquences sur le système nerveux. Paris méd., 1915, v. 17, pp. 406-414.
Sollier and Jousset, Xavier. Névrites nitro-phénolées. Lyon méd., 1917, v. 126, pp. 187-192.
Somen, H. La pratique du massage. Paris méd., 1915, v. 17, pp. 97-103.
Somen, H. Memento de mécanothérapie. Paris, 1916, J. B. Ballière et fils, 96 p., 8o.
Sommer, R. Krieg und Seelenleben—Einfluss des Krieges auf das normale Seelenleben. Wien. med. Wchnschr., 1915, No. 40, p. 1481.
Soulié, A. Les nerfs. In Poirier, tome iii, fasc. 3.
Souttar, H. S. Some points in nerve injuries. Brit. M. J., Lond., 1917, ii, pp. 817-820.
Soukhanoff, S. A. De la conviction délirante d’être prisonnier de guerre; contribution à l’étude des troubles mentaux provoqués par la guerre actuelle. Ann. méd.-psychol., Par., 1914-15. v. 6, pp. 549-557.
Soukhanoff, S. A. Des psychonévroses traumatiques de guerre. Assemblée scientifique des médecins de l’hôpital de Notre-Dame-des-Affligés pour les alienés et de l’asile Novoznamenskaia, à Petrograd, avril 1915.
Soukhanoff, S. A. Psychopathy in time of war. Russk. Vrach., Petrogr., 1915, xiv, 800-804.
Soukhanoff, S. A. (Present condition of science concerning traumatic neurosis, questions of its study and treatment from the viewpoint of military medicine.) Voyenno-Med. J. Petrogr., 1916, ccxlv, med.-spec., 241-272.
Soukhanoff, S. A. (Psychoneuroses of war time.) Russk. Vrach., Petrogr., 1915, xiv, 437-442.
Soukhanoff, S. A. Psychopathies de guerre. Assemblée scientifique de l’hôpital de Notre-Dame-des-Affligés et de l’asile psychiatrique Novoznamenskaia, 7 août, 1915.
Soukhanoff, S. A. Symptômes nerveux accompagnant l’abasourdissement par l’explosion des obus. Gazette médicale russe, 1915.
Soukhanoff, S. A. (Psychoneuroses of wartime). Russk. Vrach., Petrogr., 1915, v. 14, pp. 437-442, pp. 800-804, pp. 841-843.
Soukhanoff, S. A. (Influence of wind contusion on the central nervous system.) Russk. Vrach., Petrogr., 1915, v. 14, pp. 1010-1013.
Soukhanoff, S. A. (Data on the question of psychoses in time of war). Psikhiat. Gaz., Petrogr., 1915, v. 2, pp. 160, 165, 204, 271.
Soukhanoff, S. A. (Present condition of science concerning traumatic neurosis, questions of its study and treatment from the viewpoint of military medicine). Voyenno-Med. J., Petrogr., 1916, v. 245, med.-spec. pt., pp. 241-272.
Soulshow, H. Sur la névrose traumatique avec lésion du labyrinthe. Gaz. méd. russe, No. 35, 1915.
Souques, A. Monoplégies hystéro-traumatiques chez les soldats. Rev. neurol., 1914-15, v. 222, pp. 403-405.
Souques, A. Contractures ou pseudo-contractures hystéro-traumatiques. Rev. neurol., Par., 1914-15, v. 222, pp. 430-431.
Souques, A. A propos des contractures hystéro-traumatiques. Rev. neurol., Par., 1914-15, v. 222, p. 437.
Souques, A. Discussion de la conduite à tenir vis-à-vis des blessures du crâne—par P. Marie. Rev. neurol., Par., 1916, v. 29, p. 471.
Souques, A. Sur les accidents nerveux déterminés par la déflagration de fortes charges d’explosifs. Discussion de Vincent. Rev. neurol., Par., 1916, v. 29, pp. 585-586.
Souques, A. (Synaesthesialgia in certain forms of painful neuritis: its treatment by rubber gloves.) Soc. de Neurol., May 6, 1915. Rev. Neurol., July, 1915.
Souques, A. Aréflexie généralisée chez un blessé du crâne. Rev. neurol., Par., 1917, v. 33, pp. 33-34.
Souques, A. et Mégévand, J. Un cas de camptocormie ancienne traitée et guérie par l’électrothérapie persuasive. Rev. neurol., Par., 1917, v. 24, pp. 142-143.
Souques, Mégévand et Donnet, V. Importance de l’analyse précoce du liquide céphalo-rachidien pour le diagnostic des syndrômes cérébromédullaires dûs au “vent de l’explosif.” Bull. et mém. soc. d’hôp. de Par., 1915, v. 39, pp. 917-926.
Souques et Rosanoff-Saloff, Mme. La camptocormie. Rev. neurol., Par., 1914, 15, v. 221, pp. 937-939.
Southard, E. E. Shell Shock and After. (Shattuck Lecture.) Bos. M. & S. J., 1918, clxxix, 73.
Southard, E. E. The Training School of Psychiatric Social Work at Smith College. II. A Lay Reaction to Psychiatry. Mental Hygiene, II, October, 1918.
Southard, E. E. and Solomon, H. C. Neurosyphilis. Boston, 1917, pp. 398-425.
Souttar, H. S. Points arising in nerve injuries. Brit. Med. Jour., 1917, ii, 817.
Spaulding, Edith R. The Training School of Psychiatric Social Work at Smith College. III. The Course in Social Psychiatry. Mental Hygiene, II, October, 1918.
Specht. Zur Psychopathologie der Fahnenflucht. Münch. med. Wchnschr., 1915, 4. 621, p. 267.
Spielmeyer, W. Zur Behandlung “traumatischer” Epilepsie. Münch. med. Wchnschr., 1915, v. 62, pp. 342-344.
Spielmeyer, W. Zur Behandlung “traumatischer Epilepsie” nach Hirnschüssverletzung. Med. Klin., Berl. u. Wien, v. 111, p. 344.
Spillmann. Travaux du centre neurologique de Nancy. Rev. neurol., Par., 1914-15, v. 22, p. 1191.
Spillman. Psychoses et psychonévroses de guerre. Société de Méd. de Nancy, 1915.
Squire, J. Edward. Medical Hints. Oxford War Primers, 1915.
Stasser, M. La rééducation professionnelle de mutilés de guerre. Arch. méd. Belges, 1917, v. 47, pp. 236-241.
Stankovic, R. Ueber tödlich verlaufende Tetanie. Wien. Klin. Wchnschr., 1917, 30, 1107-8.
St. Clair-Thomson, W. Functional cases. Discussion. Proc. Roy. Soc. Med., Lond., 1914-15 (sect. Laryngol.), v. 8, pp. 118-119.
Stearns, A. W. The psychiatric examination of recruits. J. Am. M. A., Chicago, 1918, v. 70, pp. 229-231.
Steiner. Neurologie und Psychiatrie im Kriegslazarett. Ztschr. f. d. ges. Neurol. u. Psychiat., Berl., 1915, v. 30, pp. 305-318.
Stelzner, H. Aktuelle Massensuggestionen. Arch. f. Psychiat., Berl., 1914-15, v. 55, No. 2, pp. 365-388.
Sterz. Neuritis im Gebiete des Plexus lumbo-sacralis und hysterische Abasie nach Typhus. Deutsche med. Wchnschr., Berl. u. Wien, 1915, v. 111, p. 331.
Stevenson, W. F. A note on “wind contusions” in war. Brit. M. J., Lond., 1915, ii, p. 338.
Stevenson, W. F. Note on the cause of death due to high explosive shells in unwounded men. Ibid., 450.
Stewart, Purves. Diagnoses of nervous diseases (War neurology). 1916, E. B. Treat Co., New York.
Stewart, P. and Evans, Arthur. Nerve injuries and treatment. 1916, Oxford Univ. Press.
Steyerthal. Die Hysterie im Kriege. Neurol. Centralbl., 37, Nr. 16, 1918.
Stiefler, G. Ein Fall von genuinen Narkolepsie. Neurol. Centralbl., 37, Nr. 11, 1918.
Stier, E. Dienstbeschädigung und Rentenversorgung bei Psychopathen. Die militärärztliche Sachsverständigentätigkeit auf dem Gebiete des Ersatzwesens und der militärischen Versorgung. Erste Teil., pp. 140-174, Jena, Fischer, 1917.
Stier, E. Wie kann der Entstehung von Kriegsneurosen bei der Feldarmee vorgebeugt werden? Deutsche mil. ärztl. Ztschr., Berl., 1918, 47, 60-72.
Stier, E. Zur militärischen Beurteilung nervöser Krankheitzustände, speziell der Epilepsie. Deutsche med. Wchnschr., Leipz. u. Berl., 1916, v. 42, pp. 1153 and 1190-1196.
Stiles, Harold J. Operative treatment of nerve injuries. Amer. Jour. Orthop. Surg., 1918, xvi, 351.
Stivers, C. G. Testing the aviation candidate. So. Calif. Prac., 1917, xxxii, 169.
Stookey, Byron. Gunshot wounds of the peripheral nerves. Surg. Gynec. and Obst., Chic., 1916, v. 23, pp. 639-656.
Stookey, B. Gunshot wounds of peripheral nerves. S. G. O., 1916, xxiii, 639.
Stookey, B. Surgical considerations of peripheral nerve injuries. Surg. Gynecol. and Obstet., 1918, xxvii, 362.
Stopford, John S. B. So-called functional symptoms in organic nerve injuries. Lancet, Lon., 1918, i, 795.
Stopford, John S. B. Pathological diagnosis in gunshot injuries of peripheral nerves. Lancet, Lon., 1918, ii, 445.
Stopford, John, S. B. Trophic disturbances in gunshot injuries of peripheral nerves. Lancet, Lon., 1918, i, 465.
Strain of War on the Nervous System. Hospital, Lond., 1917, v. 61, pp. 415-416.
Strain of war on the nervous system. Hospital, Lon., 1917, lxii, 415.
Stransky, E. Einiges zur Psychiatrie und zur Psychologie im Kriege. Wien. med. Wchnschr., 1915, lxv., 1025-1030.
Strasser, Charlot. Ueber Unfall und Militärneurosen. Cor.-Bl. f. Schwerze Aerzt., 1917, No. 9, pp. 257-274.
Strauss, H. Die Balneotherapie als Heilfactor bei Kriegsverletzungen und Erkrankungen. Med. Klin., Berl. u. Wien, 1915, v. 111, p. 659, also Ztschr. f. ärtzl. Fortbild., Jena, 1915, v. 12, pp. 581-586.
Strümpell, A. Ueber Wesen und Entstehung der hysterischen Krankheiterscheinungen. Deutsche Ztschr. f. Nervenh., Leipz., 1916, v. 55, No. 1-3.
Sudden turning grey of the hair. Lancet, Lond., 1915, ii, p. 613.
Symonds, C. P. Some diseases which have become common among soldiers in this country. II. Hysteria. Guy’s Hosp. Gaz., Lond., 1916, xxx, 444-448.
Syms, J. L. M. Hysterics as seen at a base hospital. Practitioner, 1918, ci, 90.
Syndrômes nerveux provoqués par l’éclatement des gros projectiles de guerre. Rev. gén. de clin. et de thérap., Par., 1915, v. 29, pp. 379-380.
Syring. Zur Behandlung der Schädelschüsse im Felde. München med. Wchnschr., 1915, v. 621, pp. 592-593.
Szasz, Pest T. Ueber funktionelle Hörstörungen. Wien. klin. Wchnschr., 1915, v. 622, p. 117, also pp. 818-819.
Sztanojevits, L. Neurologisches während des Feldzunges. Med. Klin., Berl. u. Wien, 1915, v. 112, pp. 1155-1156.
Tanflyeff, P. I. Paraffin tumors, produced with a view of avoiding military service. Prakt. Vrach., S.-Peterb., 1914, xiii, 105, 120.
Taylor, J. Madison. Types of men as observed among recruits. Bos. M. & S. J., 1918, clxxix, 646.
Terrien, T. De quelques troubles visuels consécutives à l’éclatement des obus. Arch. d’ophth., Par., 1914-15. v. 34, pp. 633-650.
Terrien, F. Remarques sur la rééducation des aveugles. Paris méd., 1916, v. 21, pp. 490-493.
Tests for alleged deafness in exemption claims. N. Y. Med. Jour., 1917, cvi, 324.
Tests for the Detection of Malingering. Lancet, Lond., 1916, ii, pp. 80-81.
Terrien, F. et Vinsonneau. Hémianopsies d’origine corticale. Paris méd., 1916 (Part. méd.), v. 19, pp. 527-531.
Thibierge, G. La syphilis et l’armée. Paris, 1917, Masson et Cie.
Thibierge, G. Syphilis and the Army. Military Medical Manuals, Univ. of London Press, 1918.
Thiemann, H. Schädelschüsse. Münch. med. Wchnschr., 1915, v. 621, pp. 593-595.
Thoma. Neurosen nach Kriegsverletzungen. Wien. klin. Wchnschr., 1916, xxix, 1412, 1509, 1541, 1574.
Thomas, A. Hypertonie musculaire dans la paralysie radiale en voie d’amélioration. Sensations cutanées dans le domaine du nerf radial, provoquées par la pression de muscles qui reçoivent leur innervation du même nerf. Egarement des cylindraxes regénérés, destinés à la peau dans les nerfs musculaires. Soc. de Neurol., July 29, 1915. Revue Neurol., Aug.-Sept., 1915.
Thomas, A. La sensibilité douloureuse de la peau à la piqûre et au pincement dans la période de restauration des nerfs sectionnés après suture ou greffe. Soc. de Neur., Feb. 3, 1916. Revue Neurol., Feb., 1916.
Thomas, A. (Multiple paralyses of the cranial nerves.) Soc. de Neurol., July 1, 1915.
Thomas, André. Topoparesthésies cicatricielles: examen des troncs nerveux et des cicatrices dans les blessures des nerfs. Paris méd., 1916 (Part. méd.), v. 19, pp. 535-537.
Thomas, André. Hypermyotonie ou contracture secondaire dans les paralysies des nerfs périphériques par blessure de guerre. Paris méd., 1916, v. 21, pp. 203-209.
Thomas, André et Ceillier, H. Hémianesthésie cérébrale par blessure de guerre. Rev. neurol., Par., 1917, v. 24, pp. 34-38.
Thomas, E. Troubles cardiaques et service militaire. Rev. méd. de la Suisse, Rom., Genève, 1917, v. 37, pp. 270-283.
Thomas, J. J. Types of neurological cases seen at a base hospital. J. Nerv. and Ment. Dis., N. Y., 1916, v. 44, pp. 495-502.
Thomas, J. Lynn. Peripheral shock and its central effects. Brit. M. J., Lond., 1916, ii, pp. 44-45.
Thomas, J. L. Death from high explosives without wounds. Brit. M. J., Lond., 1917, v. 1, p. 599.
Thomson, Campbell. Shell shock without visible signs of injury. Proc. Roy. Soc. Med., Lond., 1915-16, v. 9 (Neurol. sect.), pp. 36-37.
Thomson, D. G. A descriptive record of the conversion of a county asylum into a war hospital for sick and wounded soldiers in 1915. J. Ment. Sc., Lond., 1916, v. 62, pp. 109-135.
Thorne, Bezly. Treatment by physical methods of mental disabilities induced by the war. Proc. Roy. Soc. Med., Lond., 1917-18, v. 10 (sect. Balneol.), pp. 39-41.
Thorne, W. B. The soldier’s heart. Practitioner, 1916, xcvi, 551.
Three Cases of Head Injury. Guy’s Hosp. Gaz. Lond., 1916, v. 30, pp. 297-299.
Tilley, Herbert. Two cases of functional aphonia following bursting of a shell in close proximity. Proc. Roy. Soc. Med., Lond., 1915-16, v. 8 (Laryngol. sect.), p. 155.
Timofieyeff, A. V. (Where do soldiers in the active army become insane?) Psikhiat. Gaz., Petrogr., 1915, v. 2, p. 261.
Timofieyeff, A. V. (Statistics of mental diseases in the active army in the present campaign.) Psikhiat. Gaz., Petrogr., 1915, v. 2, p. 341.
Timofieyeff, S. L. (Contractures of the fingers and toes in those who injure themselves to avoid military service.) Voyenno. Med. J., Petrogr., 1915, v. 242, pued. spec. pt., pp. 27-42.
Timofieyeff, S. L. (Self inflicted injuries and malingering among recruits under observation; according to data of the Kiyev military hospital for 1911.) Voyenno. Med. J., Petrogr., 1915, v. 243, pp. 591-630.
Tinel, J. Les Blessures des Nerfs. Collection Horizon, Masson et Cie, Paris, 1917 (also trans. Engl., Phila.).
Tinel. Le signe du “fourmillement” dans les lésions des nerfs. Presse méd., Oct. 7, 1915.
Tinel, J. Un cas de nystagmus fonctionnel. Rev. neurol., Par., 1914-15, v. 221, pp. 490-492.
Tinel, J. Paralysie fonctionnelle par stupeur musculaire. Rev. neurol., 1917, v. 24, pp. 500-501.
Tobias, E. Ergebnisse der bisherigen Kriegserfahrungen auf dem Gebiete des Nervensystems. Deutsche med. Wchnschr., Leipz. u. Berl., 1916, v. 62, p. 139.
Todd, J. L. The retraining of disabled men. Am. Med., Burlington, Vt., 1917, v. 23, pp. 380-384.
Tombleson, J. B. A series of military cases treated by hypnosis. Lancet, Lond., 1916, ii, pp. 709-710.
Tombleson, J. B. An account of twenty cases treated by hypnotic suggestion. J. Roy. Army Med. Corps, Lond., 1917, v. 29, pp. 340-346.
Tompkins, E. Stammering in connection with military service. Amer. Jour. Pub. Health, 1917, vii, 638.
Tooth, Howard H. Neurasthenia and psychasthenia. J. Roy. Army Med. Corps, Lond., 1917, v. 28, pp. 329-345.
Townsend, R. O. Two cases for comment. (I) Malingering or true neurosis. (II) Malingering or hysteria. Practitioner, Lond., 1917, xcix, 88-91.
Traitement de l’anorexie mentale. J. de méd. et chir. prat., Par., 1916, v. 87, pp. 94-96.
Treatment of peripheral nerve injuries. Rev. of War Surg. & Med., 1918, i, No. 3, 40.
Treatment of Shell Shock. N. Y. Med. Jour., 1917, cvi, 1142.
Treatment of War Psychoses. Med. Press and Circ., Lond., 1916; pp. 507-508.
Trombetta, E. Gli epilettici in zona di guerra. Gior. d. med. mil., Roma, 1918, lxvi, 54-58.
Trombetta, E. Gli inabili alle fatiche di guerra. Gior. di med. mil., Roma, 1917, lxv, 427-436.
Trömner. Einen Fall von lokaler traumatischer Hysterie. Neurol. Centralbl., Leipz., 1915, p. 415.
Trömner. Brown-Séquard-Lähmung durch Nackenschuss ohne Wirbelverletzung. Neurol. Centralbl., Leipz., 1915, p. 416.
Trömner. (a) Lokale traumatische Hysterie. (b) Schuss durch den Hals. (c) Brown-Séquard-Lähmung durch Nackenschuss ohne Wirbelverletzung. (Abstract) Deutsche med. Wchnschr., Berl. u. Leipz., 1915, v. 41, pp. 901-902.
Trömner. (a) Nachweis der Entartungsreaktion. (b) Mittlere Arm-Plexuslähmung. (c) Blutdruck- und Pulsanomalien bei organischen Nervenleiden. (d) Halsschüsse. (Abstract) Deutsche med. Wchnschr., Berl. u. Leipz., 1915, v. 41, p. 1021.
Trotter, Robert H. Observations upon the condition known as D. A. H. Lancet, Lon., 1918, l, 371.
Troubles d’origine émotive chez le combattant. Progrès méd., Par., 1916, v. 31, p. 48.
Truc, H. L’héméralopie dans l’armée. Montpel. méd., 1916, v. 39, pp. 269-273.
Truelle, V., et Bouderlique, Mlle. Etat dépressif consécutif à une émotion de guerre. Ann. méd. psychol., Par., 1917, v. 73, pp. 595-602.
Tsimken. (Experimental psychology in the nature of an objective means in the diagnosis of malingering.) Psikhiat. Gaz., Petrogr., 1915, v. 1, pp. 240-242.
Tsiplyayeff, P. I. (Simulation of fever, and measuring of the temperature in cadets.) Vestnik Obshtsh. Hig., Sudeb. i Prakt. Med., Petrogr., 1916, lii, 1277-1284.
Tubby, A. H. Cases of nerve concussion due to bullet and shell wounds. Brit. M. J., Lond., 1915, i, pp. 57-59.
Tubby, A. H. Bullet wounds affecting the motor fibers of the external popliteal nerve. Brit. M. J., Lond., 1915, i. p. 333.
Tuke, Seymour. War and insanity. J. Ment. Sc., Lond., 1916, v. 62, pp. 818-819.
Tullidge, E. K. Shock neuroses et psychoses in present war. Penn. M. J., Athens, 1916, v. 19, pp. 778-782.
Tulloch, A. B. Shell shock. Lancet, Lond., 1915, ii, p. 575.
Tumiati, C. La guérison rapide du mutisme de guerre par la méthode de Lombard. Rev. neurol., Par., 1917, v. 24, p. 475.
Turck, Fenton, B. Wound and shell shock and their cure. N. Y. Med. Jour., 1918, cvii, 901.
Türk, N. Ueber psychische Störungen bei Verschütteten nach ihrer Belebung. Wien. klin. Wchnschr., 1917, v. 29, pp. 910-913.
Turlais. Vent d’obus. Arch. méd. d’Angers, 1915, xix, 113-117.
Turner, W. A. Nervous and mental shock; arrangements for the care of cases coming from overseas. Lancet, Lon., 1916, i, 1073.
Turner, W. A. Remarks on cases of nervous and mental shock observed in the base hospitals in France. Brit. M. J., Lond., 1915, i, 833-835. Also J. Roy. Army Med. Corps, Lond., 1915, xxiv, 343-352.
Turner, W. A. Cases of nervous and mental shock. Brit. M. J., London, 1915, i, pp. 833-835.
Turner, W. A. Arrangements for the care of cases of nervous and mental shock coming from overseas. J. Roy. Army Med. Corps, Lond., 1916, v. 271, pp. 619-626; also Lancet, Lond., 1916, i, pp. 1073-1075.
Turner, W. A. Remarks made on paper of Sir John Collie, “The management of neurasthenia and allied disorders contracted in the Army.” “Recalled to Life,” 1917, Sept., No. 2, pp. 251-252.
Turrell, W. J. Electric treatment of trench foot and frost-bite. Pract., Lond., 1916, v. 96, pp. 52-61.
Turrell, W. J. Electrotherapy at a base hospital. Lancet, Lond., 1915, i, pp. 229-231.
Turrell, Sibley, et al. Discussion of electrical treatment of wounds. Proc. Roy. Soc. Med., Lond., 1914-15 (Electro-therap. sect.), pp. 35-52.
Turrell, W. J. The electrical treatment of the wounded. Lancet, Lond., 1916, ii, pp. 1005-1008; also Am. J. Electrotherap. and Radiol., N. Y., 1917, v. 35, 215-221.
Uhthoff, W. Ueber Kriegsblinde und Kriegsblinden-Fürsorge. Berl. klin. Wchnschr., 1916, v. 53, pp. 78-81.
Uhthoff. Augenärztliche Erfahrungen und Betrachtungen über Kriegsblinde. Deutsche med. Wchnschr., Leipz. u. Berl., 1916, v. 42, p. 1468.
U. S. War Dept., Surgeon General’s Office. War surgery of the nervous system; a digest of the important medical journals and books published during the European War. Wash., 1917, Gov. Print. Off., 360 p., 8o.
Urbantschitsch, E. Rasche Heilung der Symptome der im Kriege entstandenen traumatischen Neurose. Wien. klin. Wchnschr., 1916, xxix, 1051.
Urstein, M. S. (Mental diseases caused by the war, and mental disturbances caused by wounds of the brain.) Russk. Vrach., Petrogr., 1916, xv, 246-249.
Utilisation des indisciplinés en temps de guerre. Progrès Méd., Par., 1916, No. 3, pp. 70-72.
Vachet, Pierre. Les troubles mentaux consécutifs au shock des explosifs modernes. Thèses de Paris, 1915-16, No. 15.
Valobra, I. Sui disturbi nervosi detti di natura riflessa in neurologia di guerra. Policlin., Roma, 1917, xxiv, sez. med., 349-370.
Van Schevensteen, A. Considerations sur les conjonctivites provoquées. Clin. opht., Par., 1916, v. 21, pp. 595-603.
Vaquez, H. and Donzelot, E. L’aptitude fonctionnelle cardiaque du soldat. Ann. de méd., Par., 1917, v. 4, pp. 377-390.
Veale, Rawdon A. Some cases of so-called functional paresis arising out of the war and their treatment. J. Roy. Army Med. Corps, Lond., 1917, v. 29, pp. 607-614.
Verdelet, Louis. Un cas de lésion nerveuse traumatique. Caducée, Par., 1916, v. 16, p. 118.
Verger, Henri. Abandon de poste en présence de l’ennemi dans une fugue épileptique. Jour. de méd. de Bordeaux, 1915-16, v. 45, pp. 63-65.
Verger, H. La notion de consolidation dans les névroses traumatiques des sinistrés du travail et des blessés de guerre. Progrès méd., Par., 1916, v. 31, pp. 118-122.
Verger, H. et Penaud, R. Les hémiplégies tardives consécutives aux blessures de la région cervicale. Rev. neurol., Par., 1917, v. 24, pp. 281-288.
Viets, Henry. Shell shock. J. Am. M. Ass., Chicago, 1917, v. 69, pp. 1779-1786.
Viets, Henry. London war hospitals. Boston M. and S. J., 1917, v. 176, p. 222.
Villaret, Maurice. Au sujet des séquelles nerveuses des traumatismes crânio-cérébraux de la guerre (une statistique de 250 cas). Bull. Acad. de méd., Par., 1916, v. 76, p. 420.
Villaret, Maurice. Vingt-cinq cas d’astéréognosie reliquat de blessures crânio-cérébrales? Presse méd., Par., 1916, v. 241, p. 56.
Villaret, Maurice. Discussion de la conduite à tenir vis-à-vis des blessures du crâne—par P. Marie. Rev. neurol., Par., 1916, v. 29, pp. 458-460; also p. 473.
Villaret, Maurice. Propositions de réforme, les évaluations d’invalidité et les décisions concernant les militaires atteints de lésions ou troubles du système nerveux. Montpel. méd., 1916, v. 39, pp. 372-386.
Villaret, Maurice et Faure-Beaulieu, M. Les anesthésies corticales à topographie atypique dans les traumatismes crâniens. Paris méd., 1916, v. 19, pp. 514-518.
Villaret, Maurice et Faure-Beaulieu, M. L’épilepsie tardive consécutive aux traumatismes de guerre crânio-cérébraux. Montpel. méd., 1916, v. 39, p. 61.
Villaret, Maurice et Faure-Beaulieu, M. L’évolution des traumatismes de guerre crânio-cérébraux. Rev. neurol., Par., 1916, v. 24, pp. 832-833.
Villaret, Maurice et Faure-Beaulieu, M. Les troubles nerveux tardifs consécutifs aux traumatismes crânio-cérébraux de guerre. Rev. gén. de path. de guerre, 1916, No. 3, pp. 213-245.
Villaret, Maurice et Faure-Beaulieu, M. Le signe de la flexion du gros orteil par percussion du tendon achilléen. Presse méd., Par., 1917, v. 25, 531-532.
Villaret, Maurice et Rives, A. L’hémianopsie en quadrant, reliquat isolé de certaines blessures crânio-cérébrales. Bull. et. mém. Soc. méd. d’hôp. de Par., 1915, v. 39, pp. 1234-1237.
Villaret, Maurice et Rives, A. L’hémianopsie bilatérale homonyme en quadrant seul reliquat de blessures graves du lobe occipital. Paris méd., 1916, v. 19 (part. méd.), pp. 20-23.
Villaret, Maurice et Mignard, M. Le syndrôme psychique résiduel des traumatismes crânio-cérébraux de la guerre. Paris méd., 1916, (part. méd.), v. 21, pp. 209-214.
Vilvandre, G. Radiography in gunshot wounds of the skull. Arch. of Radiol. and Elec., 1916, 306.
Vilvandre, G. and Morgan, J. D. Movements of foreign bodies in the brain. Arch. of Radiol. and Elec., 1916, xxi, 22.
Vinaj, G. S. La terapia fisica in tempo di guerra. Idrol. e climat., Firenze, 1917, v. 28, pp. 30-45.
Vincent, Armand et Wilhelm, André. Un cas curieux de blessure du crâne par éclat d’obus. Paris méd., 1915 (part. méd.) v. 17, pp. 118-119.
Vincent, Cl. Du pronostic des troubles nerveux d’ordre réflexe. Persistance ou augmentation des troubles vasomoteurs et de l’amyotrophie malgré une mobilisation active et prolongée du membre malade. Soc. de Neurol., Nov. 1916.
Vincent, Cl. Note sur le traitement de certaines troubles fonctionnels. Rev. neurol., Par., 1916, v. 23, pp. 102-104.
Vincent, Cl. Au sujet de l’hystérie et de la simulation. Rev. neurol., 1916, v. 23, pp. 104-107.
Vincent, Cl. Discussion de la conduite à tenir vis-à-vis des blessures du crâne par P. Marie. Rev. neurol., Par., 1916, v. 29, pp. 471-472.
Vincent, Cl. Quelques rectifications à l’article de M. Rimbaud; Sur le traitement des psychonévroses de guerre. Marseille méd., 1916-17, liii, 936-940.
Vincent, Cl. La rééducation intensive des hystériques invétérés. Bull. et mém. Soc. méd., d’ hôp. de Par., 1916, 21 juillet.
Vincent, Cl. Sur les accidents nerveux déterminés par la déflagration de fortes charges d’explosifs. Rev. neurol., Par., 1916, v. 29, pp. 573-574.
Vincent, Cl. Le traitement des phénomènes hystériques par la “rééducation intensive.” Arch. de méd. électr., Bordeaux, 1916, v. 24, pp. 405-416.
Vincent, Cl. Variations du réflexe achilléen chez certaines hommes atteints de troubles physiopathiques des membres inférieurs. Rev. neurol., Par., 1917, v. 24, pp. 224-231.
Vincent, Cl. Sur le traitement et le pronostic des phénomènes physiopathiques. Rev. neurol., Par., 1917, v. 24, pp. 537-544.
Vincent, W. Use of asylums as military hospitals. J. Ment. Sc., Lond., 1916, v. 62, pp. 174-178.
Viruboff, M. A. (Psychoses and psychoneuroses of the war.) Psikhiat. Gaz., Petrogr., 1915, v. 2, pp. 70-72.
Viruboff, M. A. (Organization of aid to insane soldiers.) Psikhiat. Gaz., Petrogr., 1915, v. 2, pp. 168-171.
Viruboff, M. A. (Necessity for constructing hospitals for soldiers suffering from psychoneuroses.) Psikhiat. Gaz., Petrogr., 1916, v. 3, p. 194.
Viruboff, M. A. (Organization of the care of insane warriors.) Sovrem. Psikhiat., Mosk., 1916, v. 10, pp. 19-27.
Viry, H. L’instinct génésique et la guerre actuelle. Rev. gén. de clin. et de thérap., Par., 1916, v. 30, pp. 355-357.
Vitaut, L. Un cas d’œdème de striction. Rev. gén. de clin. et de thérap., Par., 1916, xxx, 551.
Vlasoff, Y. P. Cases of artificial phlegmons caused by injections of kerosene. Voyenno-Med. J., Petrogr., 1915, ccxlii, med.-spec. pt., 63-73.
Vlasto, Michael. Two cases of functional aphonia. J. Roy. Nav. M. Serv., Lond., 1917, v. 3, pp. 113-115.
Vogt, H. Die Kriegsneurosen (in: Handbuch der Therapie der Nervenkrankheiten, Jena, Gustav Fischer, 1916).
Vogt, H. Die Neurosen im Kriege (in: Die Kriegsbeschädigungen des Nervensystems, Wiesbaden, Bergmann, 1917).
Von Eberts, E. M. Functional re-education and vocational training of soldiers disabled in war. Canad. M. Ass. J., Toronto, 1917, v. 7, pp. 193-200.
Vorschläge zur Abfindung der Kriegsneurosen auf Grund dieser Erfahrungen. Med. Cor.-Bl. d. Württemb. ärztl. Landesver. Stuttg., 1916, v. 86, p. 42.
Voskresenski, M. K. (Brief annual review of the activity of the psychiatric organization of the Russian Society of the Red Cross at the armies of the southwestern front.) Russk. Vrach., Petrogr., v. 15, pp. 12-16.
Voss, G. Zur Frage der Simulation bei Soldaten. Deutsche med. Wchnschr., Berl. u. Leipz., 1916, No. 48, pp. 1476-1477.
Vvedenski, I. N. (Cases of wartime psychoses in children.) Sovrem. Psikhiat., Mosk., 1916, v. 10, pp. 1-8.
Wagener. Arbeitstherapie und Rentenabschätzung bei Kriegsneurotiker. Neurol. Centralbl., 37, Nr. 16, 1918.
Wagner. Ueberblick über die in der Heil- und Pflegeanstalt Giessen behandelten nerven und geisteskranken Soldaten. München med. Wchnschr., 1916, No. 15, pp. 548-550.
Wagner, v. Jauregg. Nervöse Störungen nach eine oberflächliche Verletzung am Rücken durch Schrapnellschuss. Wien. klin. Wchnschr., 1915, v. 28, p. 190.
Wallace, Cuthbert C. Traumatic shock. Report of fourth session of Research Soc. of American Red Cross in France. Med. Bull., 1918, i, 417.
Wallace, W. Methods of examining the vision of recruits and soldiers with special reference to assumed and real defects. J. Roy. Army Med. Corps, Lond., 1916, v. 26, pp. 471-489.
Waller, A. D. Galvanometric observation of the emotivity of a normal subject (English) during the German air raid of Whit-Sunday, May 19, 1918. Lancet, Lon., 1918, I, 916.
Walther, Ch. Traumatisme de la région scapulaire. Décollement de l’omoplate. Paralysie totale du membre supérieur d’origine psychique. Bull. et mém. soc. de chir. de Par., 1914, v. 40, pp. 1380-1382.
War and Incidence of Insanity. Med. Officer, Lond., 1917, v. 16, Oct. 6.
War and the Incidence of Insanity. Pub. Health J., Toronto, 1917, v. 8, p. 30.
War and Insanity. Med. Officer, Lond., 1916, v. 15, p. 43.
War and Insanity. Hospital, Lond., 1917, v. 60, p. 5.
War and Mental Hospitals. Med. Officer, Lond., 1916, v. 15, p. 108.
War and Nervous Breakdowns. Lancet, 1915, i, pp. 189-190.
War and the Nervous System. M. J. Australia, Sydney, 1916, v. 1, p. 205.
War and Neuroses. J. Am. M. A., Chicago, 1917, v. 67, pp. 647-648.
War and Other Causes of Insanity. Brit. M. J., Lond., 1917, i, p. 301 (also 1917, i, p. 310).
War and Psychoanalysis. N. York M. J., 1916, v. 104, p. 1251.
War neuroses and psychoses. Mil. Surgeon, Wash., 1916, v. 38, pp. 320, 428, 545.
War Surgery of the Nervous System. Pub. Office Surgeon General, 1917.
Watson-Williams, P. Functional cases. Discussion. Proc. Roy. Soc. Med., Lond., 1914-15 (sect. Laryngol.), v. 8, p. 119.
Weber, L. W. Ueber Granatkontusion (Gaupp). Neurol. Centralbl., 1915, v. 34, p. 780.
Weber, L. W. Zur Entstehung der Unfallsneurosen. München med. Wchnschr., 1915, v. 62, p. 400.
Weber, F. Parkes. Aspects of death and correlated aspects of life in art, epigram, and poetry. 3rd ed., London, 1918.
Weekers, L. L’héméralopie chez les soldats. Arch. d’opht., Par., 1916, v. 35, pp. 73-88.
Weekers, L. Night Blindness (hemeralopia). Med. Press and Circ., Lond., 1916, v. 102, pp. 386-387.
Weichbrodt, R. Einige Bemerkungen zur Behandlung d. Kriegsneurotikern. Monatschr. f. Psych. u. Neurol., 43, 1918.
Weil, Gaupp, Weintrand, Sänger, Lilienstein. Diskussion über Kriegserfahrungen. Neurol. Centralbl., Leipz., 1915, v. 34, pp. 956-960.
Welch, W. H. Medical problems of the war. Johns Hopkins Hosp. Bull., Balt., 1917, Apr., p. 156.
Wessman, R. Die Beurteilung von Augensymptomen bei Hysterischen. Abhandl. a. d. Geb. d. Augenh., Halle a. S., 1916, v. 10, No. 1/2 also Cor. Bl. f. Schweize Aerzte, 1917, No. 6, p. 191.
West, C. E. Special discussion on warfare injuries and neuroses. Proc. Roy. Soc. Med., Lond., 1917, v. 10 (sec. Otol.), pp. 92-93.
Westphal, A. Hysterischen beziehungsweise psychogenen Hör- und Sprachstörungen bei Soldaten. Med. Klin., Berl. u. Wien, 1915, v. 112, p. 1303.
Westphal, A. Ueber Augensymptome in einem Falle von traumatischer Hysterie (mit Krankenvorstellung). (Abstract) Deutsche med. Wchnschr., Berl. u. Leipz., 1915, v. 41, p. 1202.
Westphal, A. (a) Hysterische Taubstummheit bei Kriegsteilnehmern. (b) Hörstummheit. Deutsche med. Wchnschr., Leipz. u. Berl., 1915, v. 412, pp. 1560-1561.
Westphal, A. und Hübner, A. H. Ueber nervöse und psychische Erkrankungen im Kriege. Med. Klin., Berl. u. Leipz., 1915, v. 111, pp. 381-383; also pp. 413-417.
Wexberg, Erwin. Indirekte Gehirnverletzung durch Schädelschuss. Wien. klin. Wchnschr., 1916, v. 29, pp. 418-419.
Weyert. Militär-psychiatrische Beobachtungen und Erfahrungen. Samml. zwangl. Abhandl. u. d. Geb. d. Nerv. u. Geistesk., Halle a. S., 1915, v. 11, No. 2 to No. 4, pp. 1-145.
Weygandt, W. Versorgung der Neurosen und Psychosen im Felde. Med. Klin., Berl. u. Wien, v. 102, pp. 1503-1505.
Weygandt, W. Psychosen. Berl. klin. Wchnschr., 1914, v. 512, p. 1949.
Weygandt, W. Geisteskrankheiten im Kriege. München med. Wchnschr., 1914, ii, v. 61, pp. 2109-2112.
Weygandt, W. Kriegspsychiatrische Begutachtungen. München. med. Wchnschr., 1915, v. 622, pp. 1257-1259; also Neurol. Centralbl. Leipz., 1915, v. 34, pp. 925-926.
Weygandt, W. Kriegspsychosen. Neurol. Centralbl., Leipz., 1915, v. 34, pp. 43-44.
Weygandt, W. Psychische Erkrankungen bei Soldaten. Deutsche med. Wchnschr., Leipz. u. Berl., 1915, xli, 540, 694.
Weygandt, W. Psychose auf Grund von Hirntrauma. Deutsche med. Wchnschr., Leipz. u. Berl., 1915, v. 41, p. 1354.
Weygandt, W. Kriegspsychiatrische Begutachtungen. Med. Klin., Berl. u. Wien, 1915, v. 112, p. 1084.
Weygandt, W. Psychosen. Berl. klin. Wchnschr., 1915, v. 521, p. 224.
Weygandt, W. Kriegseinflüsse und Psychiatrie. Jahresk. ärtzl. Fortbild., München, 1915, v. 5, pp. 15-50.
Weygandt, W. Kriegspsychiatrische Begutachtungen. Psychiat.-neurol. Wchnschr., Halle a. S., 1915-16, v. 17, pp. 215-217.
Weygandt, W. Die Geisteskrankheiten im Kriege (in Die Kriegsbeschädigungen des Nervensystems. Wiesbaden, Bergmann, 1917).
Whale, H. L. Functional aphonia. Proc. Roy. Soc. Med., Lond., 1914-15, (Laryngol. sec.), v. 8, p. 117.
White, Ernest W. Shell shock and neurasthenia in the hospitals in the western command; observations. Brit. Med. Jour., 1918, i, 421.
White, J. Renfrew. The extent and nature of the sensory loss in musculospiral paresis. J. Roy. Army Med. Corps, Lond., 1916, pp. 340-353.
White, R. P. Effects of dinitrobenzine and other nitrosubstitution products of the aromatic series on the workmen employed in the manufacture of high explosives. (See Oliver’s “Dangerous Trades,” p. 475.)
White, S. E. Nerve-strain and war. Lancet, Lond., 1915, ii, 1317.
White, W. A. The state hospital and the war. Mental Hyg., Concord, N. H., 1917, i, 377-382.
Wicart. Les mutilations de l’ouïe par les détonations. Comment elles guérrissent. Presse méd., Par., 1917, v. 25, p. 8.
Wideroe, S. (Shell shock.) Norsk. Tidsskr. i mil., Hälsov., Kristiania, 1917, v. 21, pp. 77-90.
Wiener, E. Hitzschlag und Sonnenstich. Wien. med. Wchnschr., 1915, v. 28, pp. 721-722.
Wietfeldt. Avitaminose als Ursache der Nachtblindheit im Felde. München med. Wchnschr., 1915, v. 622, p. 1743.
Wietung. Leitsätze der funktionellen Nachbehandlung kriegschirurgischer Schäden. Leipz., 1915, 43 p., 8o.
Williams, Frankwood E. and Brown, Mabel W. Neuropsychiatry and the war, a bibliography with abstracts. Ment. Hyg., Concord, N. H., 1917, v. 1, pp. 409-474.
Williamson, R. T. Remarks on the treatment of neurasthenia and psychasthenia following shell shock. Brit. M. J., Lond., 1917, ii, 713-715.
Williamson, R. T. Treatment of neurasthenia following shell shock. Brit. M. J., Lond., ii, pp. 713-715.
Wilmanns. Dienstbrauchbarkeit der Psychopathen. München med. Wchnschr. 1916, No. 44, p. 1558.
Wilson, Gordon. Special discussion on warfare injuries and neuroses. Proc. Roy. Soc. Med., Lond., 1917, v. 10 (sec. Otol.), pp. 91-92.
Wilson, J. G. Effects of high explosives on the ear. Brit. Med. Jour., 1917, i, 353.
Wilson, J. G. Further report on the effects of high explosives on the ear. Brit. Med. Jour., 1917, i, 578.
Wiltshire. A contribution to the etiology of shell shock. Lancet, Lond., 1916, i, 1207-1212.
Wind of the Cannon Ball. Monde méd., Par., 1915, v. 25, pp. 214-217.
Wiszwianski. Demonstration von Kriegsneurosen und Neuralgien besonders Ischias. Fortsche. d. Med., Berl. u. Leipz., 1915-16, v. 2, p. 24.
Witry. Le centre neurologique et psychiatrique de la forteresse de Metz en 1914. Ann. méd. psychol., Par., 1916-17, v. 73, pp. 96-101.
Wittermann, E. Kriegspsychiatrische Erfahrungen aus der Front. Wien. klin. Wchnschr., 1916, v. 29, p. 1315.
Wittermann, E. Kriegspsychiatrische Erfahrungen aus der Front. Münch. med. Wchnschr., 1915, v. 62, pp. 1164-1166; also, Neurol. Centralbl., Leipz., 1915, v. 34, p. 928.
Wohlwill. Aphasische Störungen infolge von Kopfschüssen. (Abstract) Deutsche med. Wchnschr., Berl. u. Leipz., 1915, v. 41, p. 1603.
Wohlwill. Demonstration: 3 Patienten mit aphasischen Störungen infolge von Kopfschüssen. Berl. klin. Wchnschr., 1915, v. 511, pp. 168-169.
Wohlwill. Sprachstörung nach Schussverletzung. Neurol. Centralbl., Leipz., 1915, v. 34, p. 46.
Woitachewsky. Contribution à l’étude de l’hystéro-traumatisme. Rev. Neurol., Par., 1917, v. 24, p. 476.
Wolff. Erhebliche Sprachstörung nach Schussverletzung am Kopf. Deutsche med. Wchnschr., Berl. u. Leipz., 1916, No. 3, p. 92.
Wolfsohn, Julian M. The predisposing factors of war psychoneuroses. Lancet, Lond., 1918, i, pp. 177-180; also J. Am. M. A., Chicago, 1918, v. 70, pp. 303-308.
Wollenberg, R. Lazarettbeschäftigung und Militärnervenheilstätte. Deut. Med. Woch., 1915, xli, 757.
Wollenberg. Psychisch-nervöse Störungen im Kriegszeiten. Deutsche med. Wchnschr., Berl. u. Leipz., 1914, v. 102, p. 1927.
Wollenberg. Nervöse Erkrankungen bei Kriegsteilnehmern. München med. Wchnschr., 1914, No. 44, pp. 2181-2183.
Wollenberg, R. Ueber die Wirkungen der Granatschütterung. Neurol. Centralbl., Leipz., 1915, v. 34, pp. 922-924.
Wollenberg, R. Lazarettbeschäftigung und Militärnervenheilstätte. Deutsche med. Wchnschr., Berl. u. Leipz., 1915, v. 41, pp. 757-760.
Wollenberg, R. Weitere Erfahrungen mit der Heilbeschäftigung nervenkranker Soldaten. Deutsche med. Wchnschr., Leipz. u. Berl., 1916, v. 42, pp. 6-7.
Wollenberg, R. Zur Lehre von den traumatischen Neurosen. Kriegsärztliche Erfahrungen. Beitr. z. klin. Chir., Tübing., 1916, ci (Kriegschir. Hefte V), 343-357.
Wollenberg. Zur Vorgeschichte du Kriegsneurotiker. Neurol. Centralbl., 37, Nr. 16, 1918.
Work in France and Germany (for the care of disabled soldiers). Recalled to Life, Lond., 1917, pp. 180-186, 3 pl.
Wright, Almroth E. (Sir) and Colebrook, Leonard. Acidosis of shock and suspended circulation. Lancet, Lon., 1918, i, 763.
Wright, H. P. Suggestions for a further classification of cases of so-called shell shock. Canad. M. Ass. J., Toronto, 1917, v. 7, pp. 629-635.
Wyroubow, N. A. (Traumatic Psychoneuroses.) Moscow, 1915.
Wyroubow, N. A. (Contribution à l’étude des psychoses et des psychonévroses, observées à la suite de la guerre.) Gaz. (russe) Psychiat. 1915, No. 5. (Rev. neurol., Par., 1917, v. 24, p. 468.)
Wyroubow, N. A. Les altérations de la voix et de la parole dans la psychose ou psychonévrose par contusion. Rev. neurol., Par., 1916, v. 24, pp. 312-316.
Yealland, Lewis R. Hysterical Disorders of Warfare. Macmillan, 1918.
Yegiazaroff, I. N. (Psycho- and neuropathological observations on the wounded and contused in the present war; mutism and deaf-mutism in wounded and contused; demonstration in four cases.) Trudi, Protok. Imp. Kavkazsk. Med. Obsh., Tiflis, 1914-15, v. 51, pp. 81-83.
Yerkes, R. M. The relation of psychology to military activities. Mental Hyg., Concord, N. H., i, pp. 371-376.
Yerkes, R. M. Psychology and national service. Psychol. Bull., Princeton, N. J., and Lancaster, Pa., 1917, v. 14, pp. 259-263; also Science, N. Y., and Lancaster, Pa., 1917, v. 46, pp. 101-103.
Yurman, N. A. (Neurasthenic psychoses in time of war). Psikhiat. Gaz., Petrogr., 1915, v. 2, pp. 139-142.
Zade, M. Ueber Blendungserscheinungen im Felde. München med. Wchnschr., 1915, v. 62, pp. 1514-1515.
Zadek, J. Lähmungen nach Typhus. Deutsche med. Wchnschr., Berl. u. Leipz., 1915, v. 412, pp. 1033-1034.
Zakharschenko, M. A. Un nouveau syndrôme dans les contusions aériennes. Gaz. (russe) Psychiat., 1915, No. 4. Rev. neurol., Par., 1917, v. 24, p. 468.
Zakharschenko, M. A. (New symptom in wind contusion). Psikhiat. Gaz., Petrogr., 1915, v. 2, pp. 56-59.
Zakharschenko, M. A. (The clinical picture of disturbances of speech in those suffering from contusion, in connection with the question of air contusions). Psikhiat. Gaz., Petrogr., 1916, v. 3, pp. 369-372.
Zalkind, A. B. (Nervous diseases of war time). Psikhiat. Gaz., Petrogr., 1916, v. 3, pp. 76-78.
Zange, Johannes. Ueber hysterische (psychogene) Funktionsstörungen des nervosen Ohrapparats im Kriege. München med. Wchnschr., 1915, v. 622, pp. 957-961.
Zange, Johannes. Hysterische Hörstörungen im Kriege. Deutsche med. Wchnschr., Berl. u. Leipz., 1915, v. 412, p. 843.
Zange, Johannes. Die organischen Schädigungen des nervösen Ohrapparates im Kriege. Deutsche med. Wchnschr., Berl. u. Leipz., 1915, v. 412, p. 994.
Zangger. Welche medizinischen Erfahrungen bei Katastrophen können im heutiger Kriege verwertet werden? Cor. Bl. f. Schweiz. Aerzte, 1915, v. 45, pp. 190-191.
Zangger, H. Zur Frage der traumatischen Neurose. Zentralbl. f. Gewerbehyg., Berl., 1916, v. 4, p. 10; pp. 25-32.
Zanietowski, J. Die moderne Elektromedizin in der Kriegstherapie. Wien. klin. Wchnschr., 1915, v. 28, p. 805, p. 810, p. 838.
Zimmern, A. Quels enseignements nous fournit la réaction de dégénérescence dans les blessures des nerfs. Presse méd., April 15, 1915.
Zimmern, A. et Logre, B. Sur le réflexe galvano-psychique. Rev. neurol., Par., 1917, v. 24, pp. 565-567; also Jour. de Radiol. et d’Electrol., v. 2, No. 10, 1917, juillet-août, p. 610.
Zimmern, A. et Logre, B. Sur le réflexe galvano-psychique. Presse méd., Par., 1917, v. 25, p. 414.
Zimmern et Perol. Electrodiagnostie de guerre. Collection Horizon, Masson et Cie, 1917.
Zoroastroff, A. V. (Malingering with a view to avoiding military service). Voyenno-Med. J., Petrogr., 1915, v. 243, pp. 473-475.
Zuccari, G. Alcuni casi di psicosi da guerra. Riv. di psicol., Bologna, 1916, v. 12, pp. 129-140.
Zunahme geistiger Erkrankungen, Die behauptete, bei Beginn des Kriegs in der Zivilbevölkern Deutschlands (Ergebnis einer Umfrage). Psychiat.-neurol. Wchnschr., Halle, 1915, v. 17, pp. 167-170.
Transcriber’s Note
In the references (Page 952), the first part of the citation (preceding “med. Wchnschr., 1916, No. 44, p. 1558.”) of a publication by E. Meyer is missing in the original printing.
The index entry on Babinski refers, possibly erroneously, to case numbers not in this book.
Spelling, hyphenation, abbreviations and accents were inconsistent and have been left that way.