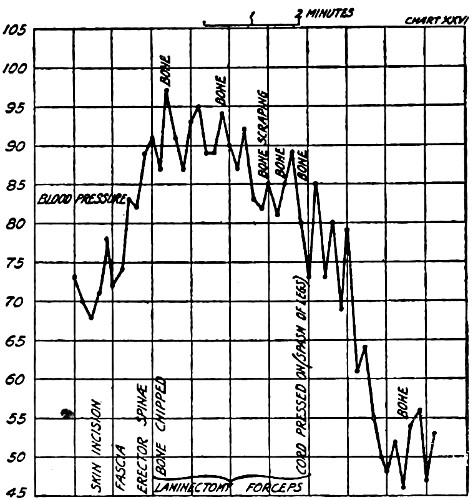
Fig. 1.—Shock—Blood pressure of a dog undergoing laminectomy under general anæsthesia (Grey and Parsons.)
(Reproduced by kind permission of the Authors.)
BY
J. STUART ROSS, M.B., Ch.B., F.R.C.S.E.
LECTURER IN PRACTICAL ANÆSTHETICS, UNIVERSITY OF EDINBURGH;
HONORARY ANÆSTHETIST EDINBURGH DENTAL SCHOOL;
ANÆSTHETIST, DEACONESS HOSPITAL; INSTRUCTOR
IN ANÆSTHETICS, EDIN. ROYAL INFIRMARY
With an Introduction
BY
HY. ALEXIS THOMSON, C.M.G., M.D., F.R.C.S.E.
PROFESSOR OF SURGERY, UNIVERSITY OF EDINBURGH
AND CHAPTERS UPON
Local and Spinal Anæsthesia
BY
WM. QUARRY WOOD, M.D., F.R.C.S.E.
LATELY TEMPORARY ASSISTANT SURGEON, EDINBURGH ROYAL INFIRMARY
AND UPON
Intratracheal Anæsthesia
BY
H. TORRANCE THOMSON, M.D., F.R.C.S.E.
ANÆSTHETIST TO THE LEITH HOSPITAL
EDINBURGH
E. & S. LIVINGSTONE, 17 TEVIOT PLACE
1919
| CHAP. | PAGE | |
|---|---|---|
| Introduction by Professor Alexis Thomson | ix | |
| Preface | xi | |
| I. | Physiological Action of Anæsthetic Drugs | 1 |
| II. | Shock and Anæsthesia | 5 |
| III. | Asphyxia or Anoxæmia | 15 |
| IV. | Methods of Anæsthetising | 28 |
| V. | The Clinical Observation of the Patient | 31 |
| VI. | The Preparation of the Patient | 42 |
| VII. | Nitrous Oxide | 46 |
| VIII. | Nitrous Oxide and Oxygen | 60 |
| IX. | Ether | 74 |
| X. | Intratracheal Ether | 96 |
| XI. | Chloroform | 109 |
| XII. | Ethyl Chloride | 122 |
| XIII. | Mixtures of Nitrous Oxide and Ethyl Chloride | 128 |
| XIV. | Mixtures of Chloroform and Ether | 134 |
| XV. | Sequences | 137 |
| XVI. | The Accidents of Anæsthesia | 140 |
| XVII. | The Sequelæ of Anæsthesia | 151 |
| XVIII. | Posture of the Patient | 157 |
| XIX. | The Choice of the Anæsthetic | 162 |
| XX. | Local Anæsthesia | 171 |
| XXI. | Spinal Anæsthesia | 193 |
| Appendix | 201 | |
| Index | 209 |
| FIG. | PAGE. | |
|---|---|---|
| 1. | Shock (Grey and Parsons) | 6 |
| 2. | Shock (after Crile) | 8 |
| 3. | Diagram to Illustrate Anoci-Association (after Crile) | 11 |
| 4. | Apparatus for Lane’s Saline Infusion | 13 |
| 5. | Diagram of the Vicious Circle of Asphyxia | 20 |
| 6. | Hewitt’s Mouth Props | 22 |
| 7. | Bellamy Gardner’s Mouth Props | 23 |
| 8. | Phillips’ Modification of Hewitt’s Artificial Air-way | 23 |
| 9. | Silk’s Nasal Tubes | 23 |
| 10. | Tongue Forceps and Glossotilt | 24 |
| 11. | Apparatus for Opening Clenched Jaws | 25 |
| 12. | Frame for Adapting Vertical Cylinders to Foot Use | 47 |
| 13. | Nitrous Oxide Cylinders (upright and angle) | 48 |
| 14. | Complete Nitrous Oxide Apparatus | 49 |
| 15. | Barth 3-way Nitrous Oxide Tap | 50 |
| 16. | Hewitt’s Wide-bore Nitrous Oxide Valves | 50 |
| 17. | Ash’s Modification of Paterson’s Nasal Gas | 58 |
| 18. | Hewitt’s Apparatus for Nitrous Oxide and Oxygen | 63 |
| 19. | Diagram to Illustrate Action of Hewitt’s and Teter’s Gas-Oxygen Methods | 67 |
| 20. | Details of Clark’s Expiratory Valve | 68 |
| 21. | The Clarke Gas-oxygen Apparatus | 69 |
| 22. | Marshall’s Sight-feed Gas-oxygen Apparatus | 70 |
| 23. | Clover’s Ether Inhaler, with Nitrous Oxide Attachment | 77 |
| 24. | Clover’s Inhaler, Diagram of a Vertical Section | 78 |
| 25. | Hewitt’s Wide-bore Ether Inhaler | 80 |
| 26. | Ormsby’s Ether Inhaler | 81 |
| 27. | Bellamy Gardner’s Mask and Ether Dropper | 83 |
| 28. | Four Photographs to Illustrate the Administration of Open Ether | 84–5 |
| 29. | Shipway’s Warmed Ether Apparatus | 91 |
| 30. | Diagram of Intratracheal Apparatus | 98 |
| 31. | Electric Blower for Intratracheal Method | 99 |
| 32. | Kelly’s Intratracheal Apparatus | 100 |
| 33. | Shipway’s Intratracheal Apparatus | 102 |
| 34. | Hill’s Direct Laryngoscope | 104 |
| 35. | Diagram of Blood-pressure Curves Obtainable with Chloroform | 110 |
| 36. | Vernon Harcourt’s Percentage Chloroform Inhaler | 115 |
| 37. | Chloroform Mask | 116 |
| 38. | Chloroform Drop Bottles | 117 |
| 39. | Junker’s Chloroform Apparatus | 119 |
| 40. | Tube of Ethyl-Chloride | 122 |
| 41. | Ethyl-Chloride Inhaler | 124 |
| 42. | Guy’s Gas and Ethyl-Chloride Inhaler | 128 |
| 43. | Details of Guy’s Inhaler | 129 |
| 44. | Diagram of Gas-Oxygen Method Introduced by Dr Guy and the Author | 130 |
| 45. | The Guy Ross Gas-Oxygen Instrument | 131 |
| 46. | Rendle’s Cone | 135 |
| 47. | Clover Inhaler adapted for the Ethyl Chloride-Ether Sequence | 139 |
| 48. | Two Photographs illustrating Sylvester’s Artificial Respiration | 146–7 |
| 49. | Sitting-up Posture for Operations upon the Head and Neck | 159 |
| 50. | O’Malley’s Posture for Intra-nasal Surgery | 160 |
| 51. | All-metal Syringe for Infiltration Anæsthesia | 176 |
| 52. | Infiltration of the Brachial Plexus | 183 |
| 53. | Needle and Syringe for Spinal Analgesia | 194 |
| 54. | Position of the Patient for Spinal Analgesia | 196 |
[ix]
The securing of a safe anæsthesia during operations is more important than ever before, partly because of the mere number of operations, and partly because of the greater extent to which other operative risks—hæmorrhage, shock and infection—have been overcome. The risk from the anæsthetic is now so very small that the joint aim of the surgeon and anæsthetist to abolish it altogether is not far from being accomplished. The author of this volume has done a good deal to accomplish this end, and it is a matter of congratulation that he has now published an account of his methods, so that a larger circle may benefit from his teaching and his experience.
The author very properly goes further and maintains that anæsthesia must not only be safe but must also be good; good anæsthesia is absolutely vital to good surgery. Only a generation back many surgeons professed to see no difference as to who gave the anæsthetic; at the present day no one willingly embarks upon a difficult operation without the aid of a skilled anæsthetist.
In various parts of the book the author has very rightly laid great emphasis upon the influence which the work of the surgeon has upon that of the anæsthetist. The latter may learn much from an occasional glance at the field of operation. He should not interest himself in the details of operative procedure to the distraction of his mind from his own responsibilities; but he can, in abdominal surgery, see for himself whether the muscles[x] are properly relaxed, and observe the state of operation, so that he can when necessary deepen the anæsthesia in good time, while not maintaining deep anæsthesia when a light one would suffice. Finally, he can check his other sources of information as to the condition of the circulation by noticing the force with which cut arteries spout, the colour of the blood and the size of uncut veins.
Like other branches of medicine, adequate study as well as practical experience is required in order to master the art of administering anæsthetics, and that a reliable manual of instruction is essential, goes without saying; I feel on perfectly safe ground in recommending this book as such both to the student and the practitioner.
ALEXIS THOMSON.
[xi]
This little book is an attempt to present to the student and practitioner a condensed account of modern anæsthetic views and practice. In choosing a general scheme I have tried to lay emphasis upon the relation of anæsthesia to general medical science rather than upon elaborate descriptions of anæsthetic apparatus and methods which a few years hence may be superseded. I have therefore devoted the first four chapters to an account of the various forces which modify the physiology of the patient during an operation under a general anæsthetic, in so far as we at present understand them. I trust that they will prove not only a sound basis for the information given in the rest of the book but also a help towards forming a judgment upon new methods and appliances as and when they meet the attention of the reader.
In making a selection of drugs and appliances for description, I have eliminated those which do not appear to me to have any real sphere of usefulness.
The account of nitrous oxide and oxygen has been given in some detail. Both the profession and the lay public have arrived, through the experiences of the war, at a more just appreciation of the possibilities of this combination than was at all general before the year 1914. At the present day, no one who proposes to engage in anæsthetic work can afford to remain unpractised in its administration.
I have an apology to make to my women readers. Throughout the book, when speaking of the anæsthetist, I have presumed the male sex. Such phrases as “his or her” and “he or she” are tedious and inelegant, and their omission must not be taken as[xii] forgetfulness on the author’s part that women frequently make very good anæsthetists.
Professor Alexis Thomson has added to the many kindnesses I have received at his hands by writing the Introduction which immediately precedes this Preface, and I wish to express my sincere thanks to him for such a valuable addition to the book.
From Mr David Wallace, F.R.C.S.E., I have received much valuable help and guidance in anæsthetic matters. It was largely due to his kindly assistance and moral support that I was encouraged to persevere with my early attempts to use nitrous oxide and oxygen in major surgery. The hints which are given in connection with Genito-Urinary Surgery are also derived from him.
The chapters upon Local and Spinal Anæsthesia are entirely the work of Mr Wood, to whom I must express my gratitude for the admirable way in which he has done the work.
I must also thank Dr Torrance Thomson most sincerely for his useful contribution in chapter X, which constitutes a complete monograph upon Intratracheal Anæsthesia.
To Dr Wm. Guy I am indebted for the photographs which appear in the book, and I must express my sincere gratitude to him for the trouble he has taken in the matter.
Much thanks are also due to the following firms who have been kind enough to lend illustrative blocks:—Messrs Claudius Ash & Co. Ltd., G. Barth & Co., De Trey & Co., J. Gardner & Son, Allen & Hanbury’s Ltd., Meyer & Phelps, Coxeter & Son, Down Bros., Ltd., Krohne & Sesemann, and Mr J. H. Montague.
Lastly, I must express my high appreciation of the courtesy which the publishers have shown to me, and of their generosity in the matter of illustrations.
J. STUART ROSS.
October 1919.
[1]
Handbook of Anæsthetics.
Every anæsthetic drug has certain pharmacological peculiarities of its own, but all have much in common, and it is to these common features we shall first direct our attention.
Reaching the blood stream by absorption from the lung alveoli, the drug enters into loose combination with the red blood corpuscles; a small proportion only is carried in the plasma. Within the corpuscles it must of necessity displace a certain proportion of the oxygen normally carried: this factor is of great importance only in the case of nitrous oxide gas, which readily displaces the larger part of the normal oxygen content. In the case of other anæsthetics, the same process occurs; but to a less extent. Detailed figures of the extent to which the blood gases are altered in various stages of chloroform anæsthesia will be found in Appendix III.
The actions of individual drugs upon the circulatory, respiratory, and excretory systems differ so considerably that a small section has been devoted to this subject in each of the chapters devoted to nitrous oxide, ether, and chloroform respectively. One feature is, however, dependent upon the state of anæsthesia rather[2] than the action of the particular drug, and that is a certain slight fall of blood pressure. This phenomenon is seen even in natural sleep, and is presumably due simply to lack of normal stimuli such as tactile, visual, and auditory impressions which in the ordinary circumstances of life, help to maintain the tone of the vasomotor system. That such a fall is due to the state of anæsthesia admits of little doubt, but the fact is not always easy to demonstrate since each of the drugs themselves have a marked influence upon the B.P., which masks the pure effect of the anæsthetic sleep.
It is in this system, of course, that we look for the characteristic action of anæsthetics, since if we had a choice, it is the brain only which we should desire to influence by our drug. It used to be said that anæsthetics paralyse the brain from above downwards, but that is only approximately true. More correctly we may say that the more highly developed parts of the brain are earliest affected, and that those portions, such as the vital medullary centres, which man shares in common with his humbler zoological relatives, maintain their activity until the last. Moreover, it must be remembered that before any brain centre succumbs, it passes through a preliminary stage of excitement, varying in intensity with varying drugs and also with different types of patients. Those who are accustomed to administer to their nervous centres repeated large doses of such nerve poisons as alcohol and tobacco, may show very evident signs of this preliminary cerebral irritation during the process of induction of anæsthesia; so do also the unhappy possessors of nervous systems deranged from other causes such as epilepsy.
The first centres to be attacked are those of thought and perception. The patient is incapable of coherent reasoning, and loses touch to some extent with impressions from the outside world. Muscular sense and co-ordination next become affected.[3] Although still able to move the limbs or the head, movements are incoherent, and if at this stage the patient were put upon his feet, he would stagger as he does in alcoholic intoxication. By this time sensation, both tactile and special, begins to be affected. The patient is no longer cognisant of pain,—if cut he would at any rate not have a remembrance of pain. The special senses are at this stage also lost, one of the last to go being the auditory sense, a point which is sometimes forgotten by those inclined to talk while anæsthesia is being induced. Muscle tone is the next function to be lost, and at this stage all movements on the part of the patient should cease except those of respiration. The reflexes disappear at varying stages: the spinal reflexes, e.g. the knee-jerks, disappear fairly early, probably before muscle tone is entirely abolished, but certain other reflexes persist to a later stage. Those which are of most interest to the anæsthetist are the conjunctival, corneal, and pupillary reflexes of which he will find full details in Chapter V.
Lastly the vital medullary centres, respiratory, vasomotor, and cardiac are overcome, and at this stage we have passed beyond the stage of a proper anæsthesia into that of over-dosage. In passing it may be observed that the level at which one endeavours to work is that indicated by the loss of muscle tone and of some of the reflexes and the full activity of the medullary centres, and that an anæsthetic is good or bad according as it gives a wide or narrow margin between these two events.
Upon the peripheral nerves, anæsthetics have much less effect than on the central nervous system. Faradisation of a motor nerve will in the deepest anæsthesia still cause immediate contraction of the muscles supplied by it, showing that the conductivity of the nerve is unaffected. Of far more importance, however, is the fact that the sensory nerves are not paralysed. That pain is not felt by the patient is due simply to the loss of function of the cerebral sensory centres; injury to the nerve still causes an impulse to be[4] transmitted to the brain. Since no operative procedure can be carried out without more or less trauma (injury) to sensory nerves, we may picture the brain of the patient undergoing a surgical operation while under a general anæsthetic, as being constantly bombarded by sensory stimuli, which though not consciously appreciated by the sleeping patient, are yet capable of producing reflex effects of a definite character, the importance of which to the work of the surgeon and anæsthetist it is difficult to exaggerate, and of which a condensed account will be found in the succeeding chapter.
[5]
Under this short and convenient title, the author proposes to discuss all the changes observable in the patient’s condition, the causation of which can be traced to the procedure of the surgeon. The use of the term shock was at one time, and by some teachers still is, restricted to a definite clinical condition. The patient was described as lying pallid and almost pulseless, with dilated pupils, cold sweating skin, and gasping, irregular respirations. In the view more generally taken to-day, that is but the extreme and final manifestation of a syndrome, which any patient who suffers trauma (whether inflicted accidentally or by the surgeon) exhibits in a greater or less degree, and from which general anæsthesia protects a patient to a very limited extent only.
Professor Crile, to whose work we owe so much of our knowledge on this subject, has said, “In general anæsthesia, part of the brain only is asleep.” Though consciousness is abolished, many parts of the brain are quite capable of responding to centripetal impulses passed to the brain through sensory nerves injured by the knife. A full account of the changes demonstrated by Crile in some of the cells of the grey matter of the brain as a result of such stimuli, and of the interpretation put upon these by their discoverer, is not suitable for a text-book of anæsthesia. It is sufficient to say that such changes have been discovered, and that their occurrence as a result of trauma is not prevented by inhalational anæsthesia. Such changes, though of the utmost interest scientifically, cannot be demonstrated clinically, and it is[6] to alterations of blood pressure and of respiration that we must look for clinical evidence of the effects of shock stimuli.
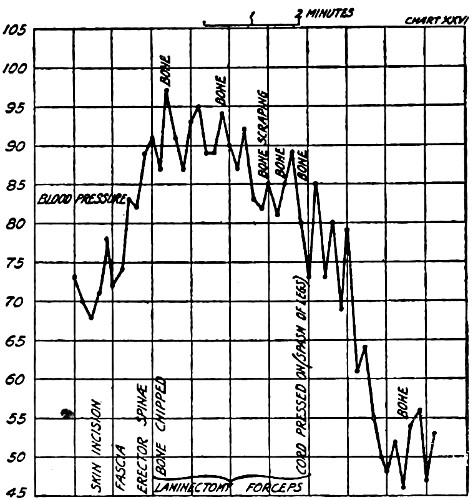
Fig. 1.—Shock—Blood pressure of a dog undergoing laminectomy under general anæsthesia (Grey and Parsons.)
(Reproduced by kind permission of the Authors.)
With every incision by the surgeon, sensory nerve twigs are of necessity injured. The fibres found in sensory nerves are, it will be remembered, either pressor, or depressor—that is, stimulation of them, causes either an increase or decrease of the blood pressure, the depth and frequency of respiration being usually affected in the same direction as the B.P. That such changes do commonly occur is easily recognised by clinical observation. The veriest beginner in anæsthesia soon learns to expect a deeper, quicker respiration and a stronger pulse as soon as the operation has begun. These changes have been studied experimentally upon animals and upon the human subject by the use of the sphygmomanometer: Fig. 1, drawn from Grey & Parson’s Arris and Gale Lectures of 1912,[7] shows a tracing from a dog undergoing laminectomy under general anæsthesia, and gives a good idea of the early evidences of shock.
We may condense the results of much work on this subject under the following headings:—
(a) Most stimuli from the field of operation cause a sharp rise of blood pressure, followed by a sharp fall.
(b) Successive stimuli delivered quickly one after another add their effects together, the total result being considerably greater than from one severe trauma.
(c) After a time, the pressor effect of stimuli begins to lessen: the animal or patient “wears out,” and finally no pressor result can be obtained by the most massive stimulation: the curve of B.P. steadily falls: the condition of full surgical shock is produced.
(d) The tearing or pulling of tissues produces more powerful stimuli than the use of a sharp knife, and, therefore, brings on the full condition of shock more rapidly.
(e) Stimuli from some tissues cause much more reflex effect upon the organism than from other less sensitive structures. This is well exemplified when an abdominal section is in progress. Incision of skin causes immediate response in deepened respiration and higher B.P.: division of the fascia very little effect. If the muscle is divided by the knife, again little reflex effect is noticeable, but if it be stretched and split by the fingers, the response is powerful. The parietal peritoneum, however delicately handled, is one of the most sensitive structures in the body, and, unless the patient is fully under at the stage either of opening or closing this layer, actual breath-holding or straining will occur. On the other hand, incision or suture of the hollow viscera will cause practically no response however light the anæsthesia, provided[8] these structures, and their connections with the parietes, are not pulled upon.
(f) Stimulation of certain selected areas, of which the spermatic cord is a well-known but by no means the only example, results in an almost immediate fall of blood pressure with little or no preliminary rise. In the operating theatre, we sometimes see faintness or syncope arising quite suddenly during operations in such regions. This subject is explained more fully in Chapter XVI. under the term “Reflex Syncope.”
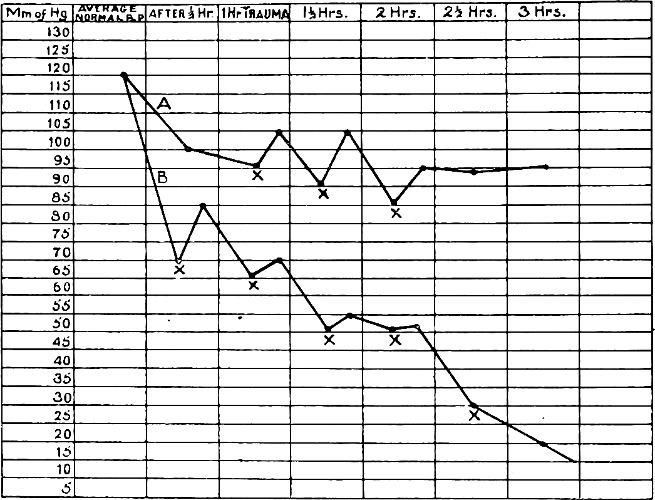
Fig. 2.—Combined blood pressure chart showing the average of a number of experiments.—A—Under nitrous oxide and oxygen. B—Under ether. At each spot marked x, a trauma (burning of the paw) was inflicted. (After Crile.)
(g) While no general anæsthetic protects absolutely from shock stimuli, some anæsthetics give more protection than others. Nitrous oxide is the most effective in this respect,[9] its powers being two and a half times greater than that of ether: chloroform is even less effective than ether (see Fig. 2).
(h) The claim made by the older generation of surgeons that shock could be prevented by the use of a deep anæsthesia, and that the occurrence of any “Reflex syncope” was always a sign of too light an anæsthesia cannot be made good. At the same time, it must be admitted that too light an anæsthesia does increase the likelihood of shock. Prolonged deep anæsthesia, on the other hand, produces by itself a condition indistinguishable from shock, with the single exception of nitrous oxide gas.
(i) Operative shock is predisposed to by several factors of which the following are the most important:—
1. Hæmorrhage before or during operation.
2. Sepsis.
3. Fear.
4. Prolonged starvation.
5. Certain diseases, especially hyperthyroidism (exopthalmic goître).
So far as we have touched in the above upon theory, it has been theory which receives general acceptance and which accords with known clinical facts. When we come to discuss the reason why blood-pressure falls in shock, we are in more debatable country.
Crile’s original view was that the upstroke seen in such charts as shown in Fig. 1 are caused by reflex vaso-constriction, and that the final fall of B.P. was due to exhaustion of the vaso-motor centre. This view he does not seem to have modified as a result of his later discovery of degenerative changes in certain cells of the grey matter of the brain.
Other workers, J. D. Malcolm in this country, and Yandell[10] Henderson, of Yale, U.S.A., maintain an opinion diametrically opposite. In their view, in fully developed shock, the vessels are in vaso-constriction, and the circulation is arrested from undue internal resistance to blood flow.
A third explanation of lowered B.P. has been offered, and while its significance is not understood, there is fairly general agreement as to its validity. This factor is a reduction in the total blood volume—an oligæmia. No one has as yet demonstrated to what region or organ the missing blood volume has retreated.
Acapnia is a condition in which the CO2 content of the blood and tissues has been brought to too low a level. Those who climb mountains suffer from it, and so do those who breathe rapidly and heavily for a prolonged period. Carbon dioxide is necessary for the vigour of the respiratory centre, of which it may be termed the natural regulator. Moreover, the heart and the great veins which empty into it require a certain proportion of CO2 in the blood.
Admittedly, patients inhaling anæsthetics do on occasion breathe too deeply. Sometimes they do so voluntarily before losing consciousness, sometimes reflexly as a result of such a manœuvre as stretching the sphincter ani. Do they thereby bring their CO2 down to a level which does serious harm and which can be considered a cause of collapse under anæsthesia? Henderson says they can and do: most other workers deny the possibility.
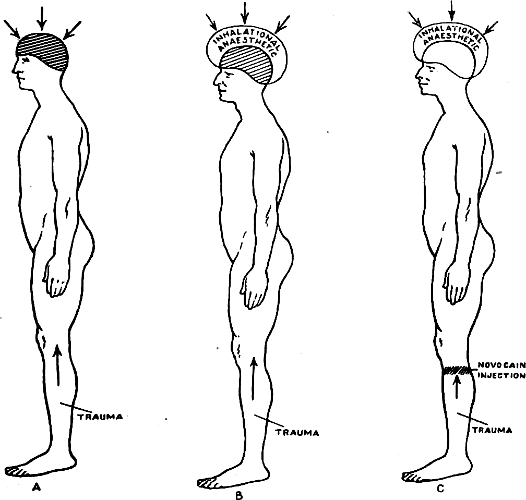
Fig 3.—Diagram (after Crile) to illustrate anoci-association. In “A” the trauma is inflicted on the leg, and the brain being wholly unprotected, considerable shock is suffered. In “B” the brain is protected by inhalational anæsthesia from the effects of fear, etc. In “C” the sensory nerves from the seat of trauma are blocked by novocaine, and the brain also protected by inhalational anæsthesia. Theoretically no shock is suffered.
There are many theories of shock but only one anti-shock technique which will bear examination. Founding upon his own theory, Crile about 1913 elaborated his ANOCI-ASSOCIATION method of which the following are the leading features (see Fig. 3):—
[11]
(a) Prevention of fear.—Every member of this team is taught the all-important art of so dealing with the patient that no unnecessary fear is allowed to remain in his mind. That art does not consist in endless repetition of the phrase, “Do not be frightened,” but rather in each so bearing himself or herself before the patient that he may gradually acquire the conviction that he is surrounded by careful, kindly, and skilful persons who are doing for him what they do for[12] hundreds of others, and doing it with an expectation of his early and complete recovery so certain that they do not need to put it into words unless definitely questioned. Such an art is not acquired in a day, and some unhappy few are so constituted that they can never acquire it.
As a further preventative of fear, and also for other reasons explained in Chapter vi., the patient receives a dose of morphia (⅙th grain, with ¹⁄₁₂₀th grain atropine, hypodermically) three quarters of an hour before operation. Some surgeons go further, and give a sedative the night before operation. Veronal gr. viii. is the favourite prescription of Prof. Alexis Thomson of Edinburgh.
(b) The sensory nerves are “blocked” by infiltration with novocain. By the systematic use of local in conjunction with general anæsthesia, the harmful stimuli from the area of operation are prevented from reaching the brain. For the details of this measure, the reader is referred to Chapter xx.
(c) The anæsthetic of choice in Crile’s practice is nitrous oxide and oxygen (see Chapter vii.).
The whole of this technique has not been generally adopted as a routine, but nevertheless the teachings of Crile have greatly influenced the mind and practice of most surgeons and anæsthetists. Traces of that teaching are to be found everywhere in the organisation built up during the Great War to save as many as possible of the lives of badly smashed men. At no previous time in the history of surgery was the problem of shock so pressing, and a brief resumé of the methods adopted is here set down, as an example of how shock should be dealt with.
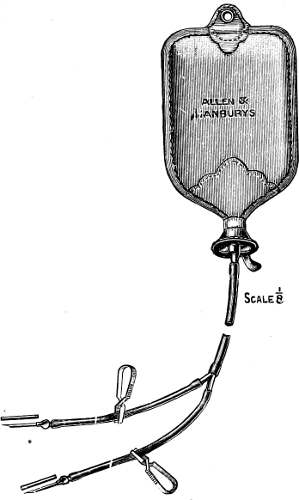
Fig. 4.—Lane’s apparatus for subcutaneous infusion of saline solution.
The first essentials demanded were the most careful organisation, the provision of equipment far in advance of most home civilian[13] hospitals, and of surgical teams specially trained to a high level of excellence. Upon recovery from the field, the injured man received at the Advanced Dressing Station, such first aid dressing as was necessary, and a substantial dose of morphia. When the latter had had time to take effect, the case was passed back to the Field Ambulance (where he received his first dose of antitetanic serum), and from there to the Casualty Clearing Station. During every stage of the journey, he received as much warm fluid nourishment as possible. Arrived at the C.C.S., the severe case was passed first into the Resuscitation Ward. This department,[14] under the charge of a specially trained M.O., concentrated largely upon two measures—the thorough warming of the patient, and the replacing as far as possible of the fluids lost to him by hæmorrhage and shock. The warming in many C.C.S.’s was effected by electric radiant heat baths. The fluids were replaced either by way of infusing blood from another patient, or by the use of gum saline solution. Introduced into a vein, the action of this solution persists for a much longer period than that of ordinary saline, being less easily lost by osmosis through the capillaries into the tissues. From the resuscitation ward, the patient passed to the Operating Theatre. Though the full technique of anoci-association was not always possible, the maxims which Crile had sought to inculcate into the practice of surgery influenced the work of surgeons and anæsthetists very profoundly. Nitrous oxide and oxygen was used for all the severely shocked cases, and infiltration with local anæsthetics where feasible and necessary.
For those who do not feel bound to adopt the Crile technique this is a simple measure which does much to minimise shock in prolonged abdominal operations. Saline infusion into a vein is so rapidly excreted that its influence is very fugacious, but if the fluid be introduced under the skin during the period of operation it is slowly absorbed as required by the blood. Sir Arbuthnot Lane is a strong advocate of this measure.
Fig. 4 shows a suitable apparatus. The needles are thrust into the loose areolar tissue under the breast, one on each side, and a pint or more of fluid is slowly run in from the reservoir.
[15]
Some degree of asphyxia is a common complication of inhalational anæsthesia: indeed some small degree of it is almost unavoidable. It is hardly too much to say that the difference between a good and a bad anæsthetist is that the one recognises and deals with asphyxia in its early stages, while the other allows it to assume serious proportions before he becomes aware of its existence. The man who only realises that asphyxia is present when the patient is deeply cyanosed and has ceased to be able to draw any air at all into his chest may know much of the physiology of anæsthetic drugs, and be well up in complicated anæsthetic apparatus, but knows nothing of the proper practice of anæsthesia.
Asphyxia arises during anæsthesia from several causes. In the first place, the drug which the patient is inhaling and absorbing into the blood, turns out from his red corpuscles a corresponding quantity of oxygen. While this is only seen in its extreme form in the case of nitrous oxide gas, it is a factor acting even in the case of other anæsthetics. Secondly, during deep anæsthesia, the respiratory centre may be somewhat depressed, and the force and frequency of the respiratory act diminished. Thirdly, the respiratory passages may be partially or wholly occluded from mechanical causes. This is far the most important type of asphyxia, being the most common, the most fatal, and the most easily prevented.
(1) Clenching of the Jaws arises not uncommonly during anæsthesia, being specially frequent towards the end of the induction[16] period. Since a very large proportion of individuals have nasal passages insufficient in bore to carry the full volume of respired air, respiration must be obstructed if the jaws are clenched.
(2) Falling Back of the Lower Jaw and Base of the Tongue over the Epiglottis.—This is always liable to happen after the muscles are deeply relaxed.
(3) Mucous or Blood or a Foreign Body is Drawn by Inspiration into the Air Passages.—Changes of position of the head may release mucous which has been gathering in some parts of the mouth or pharynx. For instance, if the head has been lying on the side for some time, a pool of mucous or saliva commonly gathers in the most dependent cheek, and unless this is mopped out before the head is brought into the mesial position, this pool will be suddenly tipped backwards, and very probably drawn into the larynx. Again, in operations upon the nasal or oral cavities, blood is always liable to be inspired, and not a few teeth have found their way into the air passages in the practices of dental surgeons who do not take precautions against this accident.
(4) Spasm of the Adductors of the Vocal Cords is one of the most common and most baffling incidents in anæsthesia. It announces its presence by the commencement of laryngeal stridor, a high-pitched crowing noise, which is as annoying for the surgeon and anæsthetist to hear as it is detrimental to the progress of a smooth anæsthesia. Inspired mucous or blood almost invariably sets it up, and the two conditions of fluid in the larynx and narrowing of the glottis from approximation of the cords, add their effects together, with resulting obstruction of a high degree.
Laryngeal stridor, however, frequently occurs even when no fluid has been inspirated. It may be set up as a reflex from the area of operation. Dilatation of the sphincter ani, and removal of the prepuce in circumcision, are two common examples of this. It is also undoubtedly sometimes caused by giving too strong a vapour[17] during the latter part of the induction stage. Stridor unfortunately sometimes occurs from no obvious cause at all, or to speak more correctly, from causes which are at present not known to us. It is the author’s belief that one of these causes may prove to be morphia given as a preliminary to inhalational anæsthesia. In his experience, stridor has been more frequent with morphia than without, particularly if chloroform be the anæsthetic chosen. Beyond that he cannot at present go.
(5) Pressure upon the Air Passages of Neoplastic or Inflammatory Swellings in the Neck.—In such cases any obstruction which may exist before induction will probably become intensified during the process, and a complete arrest of respiration is not uncommon. Large goîtres are the most common type of neoplasm to give trouble, and all acute inflammatory conditions in the neck which extend towards the trachea are notorious for their tendency to give cause for anxiety during anæsthesia.
An animal, subjected to asphyxia, either mechanically or otherwise, shows the following signs:—
(a) Increase of the force and frequency of the respiratory movements of chest and abdomen. Even though there be a complete mechanical obstruction, increased efforts to breathe will still be made for some moments, although air no longer passes in and out of the chest.
(b) There is a considerable rise of blood pressure owing to a high degree of vaso-construction.
(c) The pupils dilate.
(d) Generalised convulsions.
(e) The animal succumbs finally from cardiac failure. No heart muscle can continue to function properly if supplied by the coronary arteries with venous blood. Moreover, the heart[18] pump has to act against the greatly increased peripheral resistance induced by vaso-constriction. It must therefore be a matter of time only when the strongest and healthiest heart will cease to contract under the abnormal conditions of asphyxia.
There are in asphyxia, two alterations in the blood-gasses, i.e. lack of oxygen and increase of CO2. The action of these two conditions have been differentiated by experimental work (Starling, Kayala, Jerusalem), and one can say definitely that the excess of CO2 is the cause of the increased activity of the respiratory efforts, and that the remaining phenomena are due to oxygen starvation. This point is of some importance in considering anæsthetic methods in which re-breathing (breathing in and out of a bag) is practised. The use of such methods has often been thoughtlessly condemned as “poisoning the patient with his own CO2.” Within the limits usually practised, a re-breathing method does not involve any such risk, provided oxygen starvation does not occur. This point is referred to again in Chapter iv.
The classical signs of asphyxia above described are hardly to be expected in the operating theatre, but essentially the condition of the patient who develops respiratory obstruction while under an anæsthetic is similar to that produced experimentally in animals in the laboratory. The changes most easily observed are as follows:—
(1) Alteration of the colour.—Cyanosis shows itself earliest in the lips, and the lobules of the ears,—later the whole face becomes dusky.
(2) Dilatation of the pupil, which ceases to respond to the stimulus of light.
[19]
(3) The respiratory movements increase in depth and frequency.—The chest and abdominal walls heave forcibly; but
(4) The volume of air passing in and out of the glottis is diminished.—In complete obstruction, of course, none passes at all. In passing we may draw the moral that persistence of chest movements is no proof of the passage of air in and out of the chest: that can only be proved by hearing the movement of air through glottis and mouth or nose, or feeling it on the delicate skin of the back of the observer’s hand.
(5) True convulsions are not seen, unless we may consider the jactitation of deep N2O anæsthesia as such (see Chapter VII.). Nevertheless, there are obvious and most valuable signs of asphyxia to be found in the muscular system often quite early. These consist in the incidence of muscular rigidity, which is frequently observed first in the muscles of the abdominal wall. A surgeon performing laparatomy will notice at once the occurrence of this phenomenon, than which hardly anything can complicate and delay his task more effectively. The anæsthetist who knows his work will, upon hearing from the surgeon a complaint as to the rigidity of the abdominal wall, devote his attention first to securing a perfectly free air-way before deciding that a deeper anæsthesia is required.
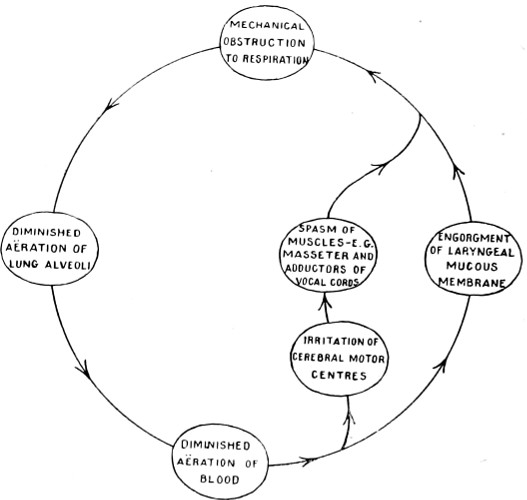
Fig. 5.—Vicious circle of asphyxia.
Once asphyxia, especially mechanical asphyxia, has begun, it almost invariably tends to get worse. The engorgement affects among other venules, those which run under the mucous membrane of the respiratory tract, still further obstructing the passage of air. The muscular rigidity, moreover, soon manifests itself in the[20] adductors of the vocal cords and the muscles which close the jaws: the patient has thus entered into a “vicious circle,” Fig. 5. It is evident that the prevention of the earliest signs of asphyxia is to the anæsthetist a matter of vital interest. The cardinal points to watch are as follows:—
(1) Keep the neck of the patient as far as possible in a natural position, i.e. do not either flex or extend the head unduly upon the body unless the nature of the operation demands such an unusual position.
(2) Maintain a free passage for air either through the nose or the mouth.
[21]
(3) Keep the lower jaw in good position throughout the administration.
(4) Avoid turning the face from the lateral to the dorsal (face up) position unless essential. If it has to be done, be careful first to mop out any “pool” from the dependent cheek.
(5) Deal as effectively as possible with the earliest appearance of laryngeal stridor.
Let us see how in a normal case, these rules can be applied. With the patient lying (or, in exceptional circumstances, sitting) in a comfortable position, the shoulders and head raised above the rest of the body and the face looking upwards (or straight forwards, in the case of the sitting patient), the anæsthetic is begun slowly, and the patient encouraged to take his time and to breathe naturally. At this stage the jaw needs no support, the muscles being neither relaxed by deep anæsthesia, nor spastic from asphyxia. With the advent of muscular relaxation, the head is turned to one side, that which is opposite to the side on which the surgeon will be working, being usually chosen. We must now determine whether the patient can breathe best through the mouth or the nose, and make sure that the channel chosen is as free as possible. In the majority of cases it will be found that respiration is oral, and that all that is necessary is to support the lower jaw by a finger hooked into the depression just below the symphysis mentes. The hands of the anæsthetist, therefore, take up a position from which in nine cases out of ten they will never require to be moved.
The hand of the side toward which the patient’s face is turned supports the jaw and keeps the face-piece or mask adapted to the face. The middle finger is pressed into the space below the symphysis mentis, and exercises traction forwards and a little upwards, thus preventing the jaw from slipping backwards; the[22] index finger lies along the lower part of the mask, maintaining adaptation between it and the chin; the thumb bears on the mask higher up, keeping its upper part pressed against the bridge of the patient’s nose, and also serving as a point d’appui, or fulcrum, from which the jaw traction by the middle finger can conveniently be exercised. This grip once learnt is not fatiguing to the hand, and is in the author’s opinion one of the essential points for the beginner to master (see Fig. 28C, page 85).
The opposite hand holds the drop bottle, if the method in use is an open one, the wrist resting upon the uppermost side of the patient’s head.
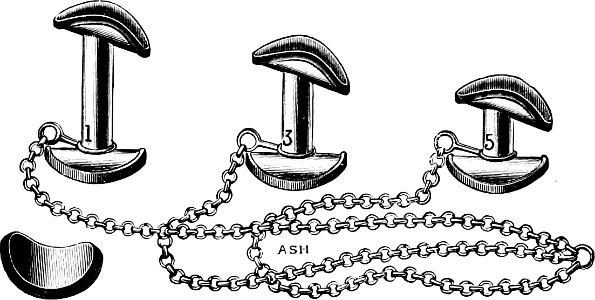
Fig. 6.—Hewitt’s dental props.
Fig. 28C shows this grip in operation, while Fig. 28D shows the alternative frequently adopted. This alternative has various disadvantages. It covers up a larger part of the patient’s face than the method recommended, and it tends to tilt the mask sideways. The little finger is supposed to be hooking forward the jaw by pressing behind its angle, but such a method is very fatiguing if in use for more than a few moments.
In a proportion of cases, it is found that a free air-way cannot be maintained by these simple measures. Upper or lower teeth[23] (or both) may be missing and traction upon the lower jaw only closes the mouth the more firmly. In most of these cases, the difficulty can be met by the use of the dental prop. These are made in various sizes and shapes, of which the best known are Hewitt’s and Bellamy Gardner’s (see Figs. 6 and 7). The latter are made of aluminium and are of small size only. They are the most convenient for cases with teeth both in the upper and lower jaw, but who suffer from a receding lower jaw not easily kept forward unless the prop is used as a rocker, as it were, upon which it can be slid forward. Hewitt’s props are of plated metal, with lead on the cups, to avoid injury to the teeth. They are made in five sizes, of which the middle and larger are very convenient for cases in which one or both rows of teeth are missing.
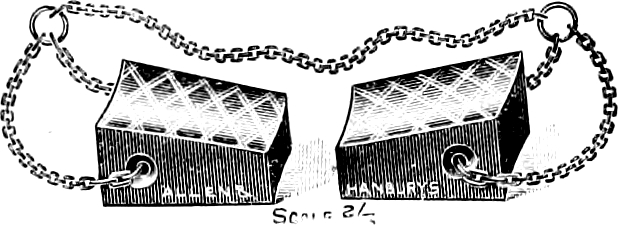
Fig. 7.—Bellamy Gardner’s Dental Props.
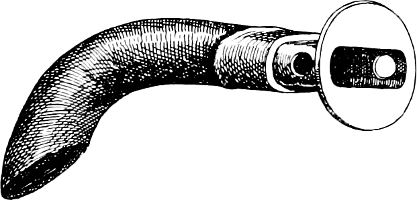
Fig. 8.—Phillips’ modification of Hewitt’s artificial airway.
For cases entirely without teeth, and in which a large flabby tongue is prone to fall back over the epiglottis, the mouth tube (Fig. 8) is very convenient. The rubber shank lies along the top of the tongue, the metal end lies between the gums. As originally introduced by Hewitt, the air-way was circular in cross section, but the flattened model figured is a distinct improvement. It was introduced by Dr Phillips.

Fig. 9.—Silk’s nasal tubes.
Occasionally one decides to facilitate nasal rather than oral[24] breathing, and if the natural passages are inadequate, recourse may be had to the passage of a short piece of drainage tube of the calibre of a number 10 catheter, and about 3 inches in length. With such a tube in one or both sides of the nose, reaching from anterior to posterior nares, nasal respiration is usually possible even in much obstructed noses (Silk). (Fig. 9.)
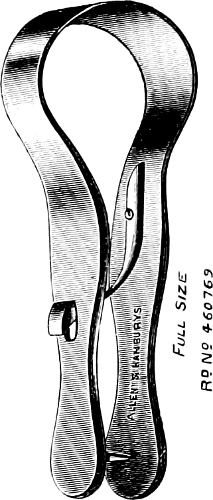
Fig. 10A.—Bellamy Gardner’s tongue-clip.

Fig. 10B. Ring tongue forceps.

Fig. 10C. Glossotilt.

Fig. 11A.—Boxwood wedge for opening jaws.

Fig. 11B.—Wedge for opening jaws.
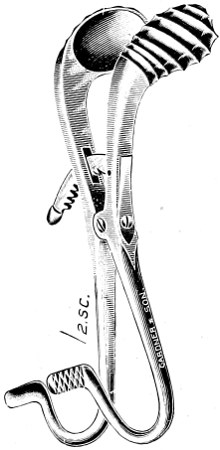
Fig. 11C.—Mouth gag.
If proper and timely use be made of one or other of these simple devices, the use of the tongue forceps is rarely necessary.
[25]
Occasionally, however, it may be required, and a suitable appliance should always be at hand for an emergency. Fig. 10 shows two types. The little clip of Mr Bellamy Gardner is preferable to the ring type, the passage of the spike through the tongue substance producing less after pain, than the bruising following the use of the other instrument. The third drawing in Fig. 10 is of an[26] instrument not much known outside Edinburgh; it is called a glossotilt, and is intended to lever forward the base of the tongue, as an alternative to nipping the tip of the organ with forceps, and has, in the opinion of some, various advantages.
Before using either mouth prop or tongue forceps, it is occasionally necessary to use some mechanical means to lever open a tightly clenched jaw. The earlier one interferes in a case of mechanical asphyxia, the less necessity will exist for the use of such means. Fig. 11 shows two well-known mouth gags, and also a box-wood wedge, the use of which is less liable to injure teeth than a metal instrument. If a gag is used, the blades when closed should lie the one behind the other, not side by side. This ensures a minimal thickness to be inserted between the tightly clenched teeth.
This is of necessity difficult since the causation of the condition is in many cases obscure. The error common to most beginners, and to many who would resent such a title being applied to them, is to regard the appearance of stridor as an indication to deepen the anæsthesia. Whether the cause lie in local irritation of the laryngeal mucous membrane or in some stimulus from the area of operation, the condition is presumably always essentially a reflex spasm of the adductors of the vocal cords, but it is a reflex which may persist even in an anæsthesia so deep that the vital medullary centres are in peril.
The preventive treatment consists chiefly in following the other rules set forth above for the prevention of asphyxia with such faithful care, that the patient never enters into the vicious circle of asphyxia of which stridor is so prominent a feature. Patience in the induction stage—the avoidance of forcing the anæsthetic upon the patient—is a safeguard not to be forgotten.
Once the condition has arisen, it saves time to withdraw the[27] anæsthetic altogether, and to allow the patient to breathe nothing but fresh air. Brisk friction of the lips with a rough towel often does good, presumably by setting up a “cross reflex.” In severe cases, a most valuable measure is the inhalation of pure oxygen, a cylinder of which should always be at hand in the operating theatre. Even an obstructed air-way will convey enough undiluted oxygen to reduce the venosity of the blood, and so cut across the “vicious circle.”
So much for the treatment of the early stages of asphyxia, the more advanced stages constitute one of the “accidents of anæsthesia,” and are dealt with in Chapter xvi.
[28]
Certain terms such as “open method,” “closed method,” etc., are used in describing different systems of anæsthetising, and it will save time later if these are now defined.
The Open Method is one in which the drug is dropped or poured upon a fabric stretched on a mask which does not lie in close apposition to the face. If the student will experiment with such a mask as Schimmelbusch’s, he will find that by no effort can he make its whole circumference touch his face at the same time. Anæsthetics vapourised from such masks must of necessity be inhaled freely diluted with fresh air. These masks are only suitable for use with chloroform.
The Perhalation Method.—This term is not used often, but it is the most strictly correct name to give to the process commonly called “open ether.” If the student will examine Bellamy Gardner’s open ether mask (Fig. 27) he will find that it is deliberately shaped to lie over its entire circumference in close apposition to the face of the average patient. In actual use it is well however to make sure of this apposition by the use of a ring of gauze as shown in Fig. 28A. Upon the mask is stretched gauze of a thickness just as great as will permit free respiration to take place through its layers. The whole bulk of the respired air must pass through the fabric, none escaping between the face and mask.
The term “Semi-Open” is applied to various methods now rarely seen. One of the best known of these was the anæsthetic cone, still used by a few for C.E. mixture (see Fig. 45).
[29]
The term “Closed Method” is applied to one in which the patient breathes in and out of a closed bag. The Clover and Ormsby inhalers are “closed” instruments. With this method the patient rapidly uses up the oxygen of the contained air, and accumulates considerable CO2; life could not be sustained for any long period of time under such a system. Oxygen must be supplied from time to time by permitting say one breath in five to be taken from the fresh air instead of from that in the bag. Alternatively, oxygen from a cylinder may be supplied by an accessory pipe into the inhaler.
This method is also referred to as the Re-Breathing Method.
The Valved Method is used only with “gas” or “gas-oxygen.” The facepiece fitting accurately, the patient draws all the volume of his inspiration from the inhaler: his expirations he propels through a valve, into the general atmosphere of the room. If nitrous oxide unmixed with oxygen is being given, the patient suffers from oxygen starvation even more rapidly and completely than in the re-breathing method. During the induction period of gas anæsthesia, such oxygen starvation is practised deliberately, and if not pushed too far is harmless. It cannot, however, be continued for more than a brief space of time. The admixture of oxygen to the vapour being breathed entirely abolishes this unfavourable feature of the valved method.
There is, however, another consequence of the use of “valves” which is unaffected by the addition of oxygen. Reference has already been made to Yandell Henderson’s acapnic theory, and if under any form of anæsthesia the patient can be reduced to a condition of CO2 starvation, it will be when the valved system of administration is in operation for a prolonged period. As a matter of experience, patients breathing “on the valves” do often exhibit shallow respirations and slight pallor which is rapidly and very strikingly remedied by turning to the rebreathing method. One[30] can hardly doubt that the improvement is due to a gradual re-accumulation of carbon di-oxide in the blood and tissues.
Two other terms referring not to the type of inhaler but to the method of supplying the drug, are in use.
By the “Drop” Method, we mean one in which the anæsthetic is supplied in a steady series of drops. The flow may be quick or slow, but it always arrives on the mask in isolated drops of uniform size. Such a method demands more constant attention than the next to be described, but it is capable of yielding that even uniformity of vapour strength so desirable in open methods.
The Douche Method is unfortunately far more commonly used by those whose attention has never been drawn to the significance of the difference between the two. Supplies of the drug rendered, say, every twenty seconds cannot possibly give an even vapour strength.
“Single Dose” methods are of use chiefly in dental surgery. The patient is charged up with the anæsthetic, and the operator has to begin his work as soon as the mask is withdrawn from the face, ceasing as soon as the patient shows any signs of recovering consciousness of pain.
Single dose anæsthetics are in a class by themselves. In order to achieve success with them, special experience on the part of the administrator and mutual confidence between operator and anæsthetist are essential.
The period of anæsthesia available to the operator which any particular “single dose” anæsthetic may be expected to yield is obviously a matter of the first importance, and the table given in Chapter xix. will be found helpful in this connection.
[31]
Anæsthesia has been divided into four clinical stages corresponding to the degrees to which the nervous system has been affected. The boundaries between these stages are often ill-defined, but the terminology has some value as facilitating description.
The First Stage lasts from the commencement of inhalation up to the time when volitional self-control is lost by the patient.
The Second Stage in the older text-books was said to be characterised by struggling, shouting, and breath-holding. With a patient not addicted to alcohol and with the anæsthetic skilfully administered, this description is unduly lurid.
The Third Stage is that of full surgical anæsthesia.
The Fourth Stage is that of over-dosage.
These give such valuable assistance to the anæsthetist that it will be well to define and describe them as a preliminary. They are three in number.
The Conjunctival Reflex is best elicited by drawing the upper lid upwards from the eyeball and retaining it in that position with one finger, while with another finger the ocular conjunctiva is lightly touched in the area of the inner canthus. If the anæsthesia is very light, both lids attempt to approximate[32] and close the palebral fissure. The upper lid may slip down from under the retaining finger and come into its proper place, while the lower lid is elevated. At a deeper level of anæsthesia there is not complete action of the orbicularis but merely of a certain part of it, so that all that is observed is a twitch inwards of the lower lid. Even this form of the reflex disappears before the corneal reflex.
The Corneal Reflex is elicited by pushing up the upper lid by one finger and with the pulp of the same finger lightly brushing the centre of the cornea as soon as it is exposed, when we feel or see the upper lid come back into position with a sharp definite twitch. The examining finger must be slipped smartly out of the way as soon as the cornea has been touched. Even in deep anæsthesia, a trace of this reflex can usually be elicited if the little manipulation be properly performed.
The conjunctival and corneal reflexes are frequently confused in the mind of the student. The most common mistake made is to pin the upper lid firmly somewhere in the region of the bony roof of the orbit, to dab the eye far too vigorously, and to believe that no reflex is present because no movement of the upper lid takes place. In the first place, the upper lid cannot move if it is rigidly held against a bony plate: in the second place, it is wholly unnecessary to inflict upon the cornea more than the lightest of touches. Both these reflexes are to be used with great discretion, undue frequency and excessive vigour of touch being alike capable of setting up serious inflammatory reaction.
The Pupillary Light Reflex is elicited by shutting off light from both pupils for ten to twenty seconds and then smartly withdrawing the protecting fingers and allowing as strong a light as possible to fall on to the eye. The response of the ciliary muscle should always be present; its absence is a certain indication of something wrong: some sluggishness may be permissible under[33] ether, but even that is suggestive of trouble if chloroform is the anæsthetic.
The use of a preliminary hypodermic of morphia tends to make the pupil somewhat smaller than normal, and to elicit the light reflex it may be necessary to cut off illumination for a somewhat longer period than if no morphia had been given. Nevertheless with a little care, the light reflex should always be capable of demonstration even in the morphinised subject.
In the case of nitrous oxide and of ethyl chloride, the patient passes through the various stages very rapidly, and the picture of anæsthesia as induced by either of these two is therefore best described separately. The following may be taken, therefore, as an account of what is to be observed in the patient inhaling ether or chloroform, unless a specific reference is made to one of the other anæsthetics.
First Stage.—The first sign that some effect is being produced in the patient is usually the appearance of the movements of swallowing; the hyoid and thyroid can be felt or seen to be moving in conjunction with the muscles of deglutition. During this stage, the patient being still to some extent under volitional control, there should be no other movement noticed. The eyes are usually closed and the colour normal; the respiration may be hurried by excitement, but judicious handling of the patient will do much to minimise this.
The Second Stage is really entered when volitional control is lost. It may be characterised by struggling and shouting by the patient, even if the anæsthetic is properly administered; but with a healthy patient and a good anæsthetist, all that usually occurs in the way of movement by the patient is some rigidity of the limbs and a slight attempt, perhaps, to lift the head from the pillow or a limb from the couch. The breathing tends during the first part[34] of this stage to be light and is rarely entirely regular: slight pauses occur, usually after an inspiration, less commonly after expiration. Serious “holding of the breath” (after an inspiration) rarely occurs save in the type of patient who is also struggling; if it does occur to a degree which causes any blueness of the patient’s face (cyanosis), it usually calls for the removal of the anæsthetic for a moment until normal breathing has been resumed.
The colour of the face rarely departs much from normal during the second stage, unless cyanosis from breath-holding intervenes.
The eyes are usually opened, as the second stage progresses, and the eyeballs tend to rotate slowly in every plane. The pupils are usually large, but react sharply to light. Both conjunctival and corneal reflexes are brisk.
The Onset of the Third Stage is marked by the appearance of muscular relaxation. Any limb which the patient may have been holding rigidly up sinks down on to the couch, and it will be found that if an attempt be now made by the anæsthetist (as it should be) to turn the head of the patient to one side or another, the muscles of the neck no longer resist.
The respiration also alters in type, losing its tendency to lightness and irregularity, and becomes full, deep, and regular. In open ether anæsthesia particularly, expiration commonly assumes a “blowing” type very characteristic, and which to the trained ear is of itself an indication that full surgical anæsthesia is present or at any rate not far distant.
The colour varies somewhat with the anæsthetic in use. With ether it is usually somewhat higher than normal, and a trace of blueness may be present if the method is the “closed” one. Anything more than a trace, however, must be regarded as abnormal, whatever the method or anæsthetic may be. With chloroform the colour is perhaps a little paler than that normal to the individual.
[35]
The eyelids are usually half open, and the eyeballs at rest looking forward and slightly downwards. An extreme rotation downward may usually be taken as a sign of very deep anæsthesia. The pupil is, as already said, always active to light, but its actual size varies with the anæsthetic used. With ether, particularly “closed” ether, it may be large (4–5 millimetres): with open ether, preceded by morphia, about 3–4 millimetres: a good chloroform anæsthesia usually exhibits a pupil of only 2–3 millimetres, and if morphia has also been given, it may be pin-point in size. Too much emphasis must not be placed, however, upon the mere size of the pupil; that may vary within wide limits without necessarily indicating serious abnormality. The essential point is that the light reflex shall be brisk. A pupil of 5 millimetres reacting sharply to light may be of no special moment: one of that size immobile to light would cause real anxiety.
The conjunctival reflex usually disappears fairly early in the third stage: if briskly present, the anæsthesia is certainly a light one, and probably insufficient for an abdominal section. The corneal reflex if properly taken in the way already described can usually be elicited throughout the third stage. In an anæsthesia deep enough for abdominal section it is, of course, not brisk, but we may say generally that its entire absence is presumptive evidence of a very deep anæsthesia—probably undesirably deep. It must not be forgotten that some local causes such as drying of the surface of the cornea may cause it to disappear, and in case of doubt it is sometimes worth while to wash out the eye with a little saline solution. If after doing so the anæsthetist still finds the reflex not present he should be on his guard. Provided, however, that the light reflex is still present and colour and respiration satisfactory, he need not consider that the patient is in any immediate danger.
Broadly speaking, then, the third stage, the stage which is called for by the requirements of major surgery, is characterised by[36] (1) full regular respirations; (2) colour not much removed from normal; (3) moderate sized pupil, larger in the case of ether than chloroform; (4) conjunctival reflex faint or absent; (5) corneal reflex just present, or, in a deep third stage, just absent; (6) light reflex present: these may be regarded as the signs of fully developed surgical anæsthesia.
The absolute beginner may be so completely out of his reckoning as to mistake the quietude of the later part of the first stage for the appearance of the third stage. For the prevention of so gross an error as that, the reader need only be referred to a patient study of the foregoing. But even a man with considerable experience may frequently be in doubt exactly as to how far through the third stage his patient has passed. He may have attained a level which will permit an incision to be made into the skin without movement on the part of the patient, but not one which would relax the abdominal muscles sufficiently for the peritoneum to be opened without eliciting considerable resistance from the abdominal muscles. In such moments of doubt, the author is accustomed to request the surgeon to make his skin incision, and observe the effect which this trauma has upon the depth, frequency, and regularity of respiration. This furnishes a most valuable guide to the depth of anæsthesia. In a third stage of very light degree, the respiratory rhythm will be interrupted and the breath held for a second in inspiration. Apart from any other sign, that may be taken as an index that the anæsthesia is very light—too light to permit of opening the peritoneal cavity. In a very deep anæsthesia the respiration is little affected by the skin incision, while at a moderate and more desirable level the respiration is quickened and deepened, but unaffected in the regularity of its rhythm.
The Fourth Stage is Stage of Over-Dose.—This stage is, of course, never entered voluntarily. Its earliest signs are loss of all tone in the muscles of expression, complete loss of corneal[37] reflex, a widely dilated pupil insensitive to light, and a type of respiration which though definitely weakened may show occasional deep gasps. Circulatory failure and cessation of respiration from failure of the medullary centre are the closing phenomena of overdose.
It will be perhaps noticed that in the foregoing, no reference has been made to the examination of the pulse. This is not an oversight on the part of the author. It is perfectly true that under any anæsthetic not complicated by an asphysical element, the blood pressure falls as the drug takes effect, and that in the case of chloroform the fall is often quite considerable. Such a fall can be appreciated by the skilled finger, but only by concentrating upon that examination a degree of attention which necessarily detracts from the administrator’s available energy for the observation of other signs which are of equal value, and can be more rapidly and certainly appreciated and appraised.
It is nevertheless essential to assure oneself during the whole progress of an anæsthesia that the circulation is in a satisfactory condition. Two obvious guides to this are the colour of the patient’s face and the force with which cut arteries spout. As regards the colour in circulatory failure, one would naturally expect a pallid face, and this indeed is the rule. It must not be forgotten, however, that cyanosis may sometimes be cardiac in origin. Cases do sometimes occur when a bluish tinge is seen on the lips, ears, and nostrils, apart from any obvious cause of oxygen starvation. In these we may reasonably suspect that the right heart is failing, and take measures accordingly.
Another valuable index to the state of the circulation is the “skin reflex,” that is, the speed with which the circulation returns to an area of the skin which has been pinched. The student should train his eye by occasionally pinching the lobule of the[38] patient’s ear and observing first the white area so produced, and later the rate at which, in a normal case, the healthy colour returns.
It is not intended to furnish here any account of matters more suitably treated under the “Accidents of Anæsthesia,” which are fully described in Chapter xvi., but merely to draw the attention of the student to certain departures from the normal course of anæsthesia which are encountered with varying frequency, to ascribe them as far as possible to their true causation, and indicate methods of prevention.
The abnormalities fall into two classes, those connected with the nervous and muscular systems, and those in which respiratory changes are evident.
Clonus or tremor sometimes appears in one or more limbs, even the trunk being affected in severe cases. Ether is practically the only anæsthetic under which the tremor ever appears, and the condition is often spoken of as “ether tremor.” It rarely appears in the female subject, being almost limited to powerfully built young men. Coming on towards the end of the second stage, it frequently persists in the deepest of third stages, and in bad cases there is usually no option but to change over to chloroform—always supposing that the tremor will interfere with the work of the surgeon. If it will not, the condition calls for no active treatment, since it is in itself not dangerous.
Movements recalling to the observer the condition of athetosis seen in the limbs of hemiplegics are occasionally seen in the anæsthetised patient. The fingers of a hand may be slowly moved, or one or other shoulder may be shrugged. The exact cause of these movements is obscure. They occur in all types, both sexes, and at all ages; they are not necessarily asphyxia though a trace of asphyxia seems sometimes to conduce to them. They persist for[39] some time after the third stage has been entered, and ultimately disappear without any obvious cause other than the passage of time. It is rare for them to continue more than five or ten minutes after full anæsthesia has been induced. Their practical importance lies purely in this, that the inexperienced anæsthetist observing some muscular movements still persisting, may take them as an infallible sign that anæsthesia is not complete, and may deliberately take his patient to a deeper level. If in doubt, the anæsthetist must, of course, consult all the other recognised guides, such as the eye reflexes, but once he has seen these movements in a case, and had demonstrated to him their slow, rhythmical character, he is not likely to be misled on a future occasion.
Muscular rigidity has been mentioned already in Chapter iii. When it persists in a patient in whom other signs suggest that a full anæsthesia has been produced, the anæsthetist will usually find that attention to the air-way, and perhaps a whiff of oxygen, will remedy the trouble.
Shallow breathing or even slight temporary arrests of respiration arise frequently. During the induction stage they may be due to:—
1. Apnœa or acapnia following voluntary excessive breathing.
2. Using morphia before chloroform.
At a later stage, it may be due to:—
1. Acapnia following excessive breathing excited reflexly from the seat of operation.
2. Direct reflex inhibition of the respiratory centre. An example of this is seen sometimes when the bladder is over-distended by lotion.
3. Impending vomiting.
[40]
Moist sounds not uncommonly appear. The student’s general knowledge of medicine will enable him to decide whether the fluid is likely to be in the pharynx, larynx, trachea, or bronchi. If in one of the first two named, it will suffice to swab out the throat and encourage the patient to cough. If, however, moisture is evidently present in the trachea or bronchi, the condition is one calling for considerable care and judgment. It arises more commonly with ether than with chloroform. Much will depend upon how much longer the surgeon requires to finish his operation. If only a few minutes more are required, nothing is necessary but to cut down the amount of ether being given to the minimum possible. If, however, the surgeon has still a good deal to do, the safest thing is to withdraw the ether and substitute chloroform or a mixture. Be it clearly understood, however, that such a change over is not devoid of risk. If it is to be made, it must be done early, before the patient is cyanosed and almost drowned in his own secretion. In a neglected case where cyanosis has already appeared, there will be no option but to interrupt the operation, empty the chest by encouraging coughing, and to aid the process by compressing the patient’s chest during expiration. Thereafter chloroform may be given, but with the greatest care.
Gasping and sighing are not common phenomena but when they occur, call for close notice from the anæsthetist. Excluding, of course, such occurrences in the first stage, before volitional control has been lost, they may be usually but not invariably ascribed to overdosage or to the appearance of definite surgical shock. Whenever they are noticed, therefore, it behoves the administrator to overhaul the patient thoroughly, to consult the eye reflexes, the skin reflex, and the pulse, and not to rest until he is assured that there are no other signals of danger to be found.
Stertor and stridor. The first of these is caused by flapping of the soft palate. It is a noise low in pitch, resembling ordinary snoring. Indicating as it does that the palatal and therefore[41] probably other muscles, are relaxed, it may if moderate in volume usually be taken as a favourable sign. If it becomes very loud, however, the probability is that the base of the tongue has fallen back; cyanosis will begin to appear, but will immediately be remedied by pulling forward the jaw or in extreme cases, using the tongue forceps.
Stridor is a high-pitched sound produced by approximation of the vocal cords. It has already been dealt with in Chapter iii.
This term has been applied to a condition often seen in children, and occasionally in adults. It is almost limited to chloroform: the author has never seen a genuine case when ether has been in use. It appears very quickly after inhalation has begun: the muscles are relaxed, the respirations quiet and regular, the conjunctival reflex sluggish. A very marked feature is the excessive smallness of the pupil. Obviously then, the condition much resembles a true third stage, but if the operation be begun, the mistake will very rapidly be made evident, for the patient will at once move and cry out. In essence, the condition is simply one of ordinary sleep. It can be recognised by its appearance after a period of inhalation too brief for the induction of true anæsthesia, by the very small pupils and the lightness of the respiration. It will be a waste of time to permit the condition to continue, as the lightness of the respiration delays the taking in of a dose of the anæsthetic sufficient to induce a proper third stage. The remedy is simple,—rub the lips and face smartly with a towel or the hand, when respiration will at once deepen and the pupil dilate. Thereafter, the induction should proceed normally.
[42]
For all but short anæsthesias conducted chiefly by nitrous oxide, the intestinal tract of the patient must receive careful preparation. In doing this, one must avoid excessive starvation and purgation, both of which tend to increase shock.
We will suppose that the operation is timed for 10 a.m. on Tuesday morning. On Monday morning the patient receives an aperient which may be varied a little to suit his taste and habits. If he has no preference, there is nothing better than an ounce of castor oil. During the rest of Monday, he has a light diet: fish and milk pudding in the middle of the day, a little soup at night. The aperient should operate before 9 p.m. When that is over, the patient retires to bed. During the day he may be allowed to move about his room a little, but should not undertake any exertion.
If there be excessive nervousness, or a natural tendency to insomnia, sulphonal gr. 15 or veronal gr. 8 may be given early in the evening, to ensure a night’s rest.
About 6 a.m. on Tuesday morning, a large soap and water enema is given, and when this has operated, a cup of tea or a little soup or Bovril may be taken. Thereafter nothing should be given by mouth.
The early forenoon is the time of choice for any operation, but if an afternoon time be of necessity chosen, the patient should not be starved throughout the forenoon. A repetition of the early morning meal may be allowed about 11 a.m.
[43]
In cases such as gastro-enterostomy, where the alimentary tract will be opened, the preparation must be a little more stringent. It is usual to allow no solids at all the day before. A saline enema may be given an hour or two before operation, when the soap and water has been evacuated.
This great improvement in anæsthesia was practised many years ago by a few surgeons, but it was only when open ether assumed its present position of pre-eminence that it was widely adopted.
The present routine is to give morphia gr. ⅙, atropine gr. ¹⁄₁₂₀ to adult patients three quarters of an hour before operation. It has the following advantages:—
(1) The nervous fears of the patient give place to a feeling of bien-être.
(2) The secretions of saliva and of mucous from the respiratory mucous membranes are limited.
(3) A little less inhalational anæsthetic is required.
(4) The after vomiting is lessened, and probably the liability to inflammatory respiratory complications also reduced.
The disadvantages can be met by proper care and dosage. They are as follows:—
(1) Morphia plus chloroform depresses the respiratory centre at an early stage of anæsthesia. Respiration becomes infrequent and shallow, and cyanosis appears before the patient is really sufficiently anæsthetised for the purposes of the surgeon.
(2) The larger the dose of morphia, the more troublesome is this premature failure of respiration.
The moral is obvious: give the small doses above recommended[44] and induced with mixtures weak in chloroform, or better still with ether only (see page 86).
Some years ago, before these facts were appreciated, there was a fashion for giving very large doses of preliminary narcotics. The combinations most favoured were as follows:—
Scopolamine is a form of hyoscyamine and is itself a powerful narcotic. Two or sometimes three doses of the mixed drugs were given at intervals of an hour, the last half an hour before operation. Scopolamine gr. ¹⁄₂₀₀, morphia gr. ⅛ was the usual formula: some surgeons added a dose of atropine or strychnine with the idea of stimulating the respiratory centre.
The patients went to the operating or anæsthetising room so drowsy that they were unaware of their surroundings, and afterwards had no recollection of the actual beginning of the inhalation. So humane a method naturally attracted a good deal of attention, but the serious depression of the respiratory centre which seems inevitable in the method has gradually caused it to disappear from the practice of most surgeons and anæsthetists. At the present day, it is only to be recommended in midwifery practice; to the drowsy semi-conscious condition produced, the name of Twilight Sleep has been given.
Omnopon is composed of a mixture of several of the alkaloids derived from opium; the makers claim that it produces less after malaise than morphia alone. It may be given before anæsthesia in doses of ⅙–⅓ gr., either alone or combine with a small dose of scopolamine. It gives quite good results if not pushed to excess.
This comparatively modern sedative is used by some surgeons in preference to morphia. A dose of ¹⁄₁₂ gr. is quite sufficient,[45] three quarters of an hour before operation. Atropine should always be combined with it.
To young children, morphia should not be given, but atropine may be given freely. A child of twelve months tolerates a dose of ¹⁄₂₀₀ gr. quite well: one of six years, will take ¹⁄₁₅₀ gr.
In ages ranging from 12 years upwards, greatly reduced doses of morphia may be given. No child under 15 years requires more than ¹⁄₁₂ gr. of morphia at most.
[46]
Upon the nervous system, nitrous oxide acts like other anæsthetics, but the stages of anæsthesia are passed through so rapidly that a second stage can hardly be distinguished. It is rare for struggling or excitement to be manifest, unless air or oxygen be admitted at the same time, when the effect which led Humphrey Davy more than a century ago to apply to nitrous oxide the name of “laughing gas” is very evident indeed.
Upon the other systems of the body, nitrous oxide has little if any effect in itself. The essential point to remember in connection with nitrous oxide administered unmixed with air or oxygen is that there is an inevitable element of asphyxia. The larger part of the oxygen normally carried by the red blood corpuscles is eliminated and replaced by N2O: oxygen starvation is therefore of necessity present. In other words, the “vicious circle of asphyxia” (see Fig. 5) is entered, and muscular spasm is bound ultimately to appear. Moreover, the blood pressure rises very materially as a result of the lack of oxygen. That no harm results to the normal healthy patient from this rise is due to the fact that the gas does not in itself poison the heart muscle, which can therefore stand up to the extra strain of working against higher resistance, so long as the process is not carried to extremes. A heart muscle weakened by the action of chloroform would give out at once if exposed to such a test.
[47]
Nitrous oxide is supplied by the makers as a fluid condensed in iron bottles or cylinders, and only becomes gaseous upon being released from them. In passing from the fluid to the gaseous state, heat is of course lost, and it will be noticed that the end of the cylinder which is in use becomes rapidly crusted over with frost. Ice, moreover, forms in the small channel at the head of a cylinder, and is apt from time to time to block it.
The cylinders are of various sizes and designated after the numbers of gallons of gas which they will supply: 25 is the smallest size, 50 or 100 are more usual; anything up to 500 is occasionally met with in hospital practice. Moreover the cylinders are of two types, called respectively vertical (for use in the upright position), and angle for use in the horizontal position (see Fig. 13).
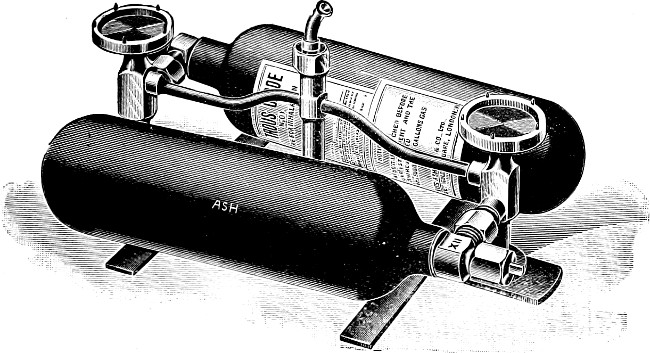
Fig. 12.—Frame for adapting vertical cylinders to foot use.
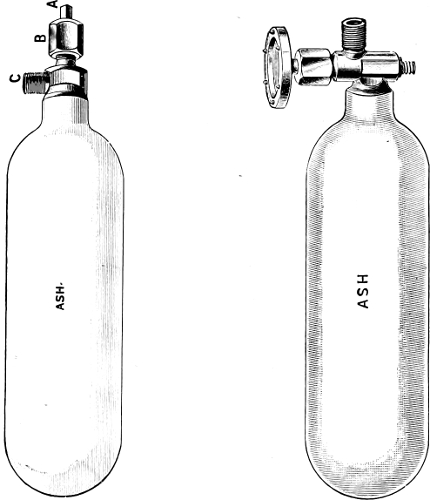
Fig. 13a. Fig. 13b.
Two types of N2O cylinders.
A. Vertical (or ordinary). B. Angle.
The cylinders are fixed in frames of various types of which examples are seen in Figs. 13 and 14.
Upon each cylinder, of whatever size or type, will be found a label stating its weight when full and empty, the difference[48] representing the weight of the contents when the bottle is full. For instance, in the case of the 50-gallon cylinder the weight of its full charge is 15 ounces. Weighing the cylinder is the only certain means which we have to estimate how much of the charge remains. The student will readily appreciate therefore that once a cylinder has been used at all there is always a risk of the supply of gas from it running out during an administration. It is[49] for this reason that cylinders are habitually used in couples, one of which is always supposed to be quite full. To this one it is well to attach a label marked “full,” and care must be taken to replace at once a cylinder known to be empty. In this way we always have upon the frame one cylinder partly and another entirely full.
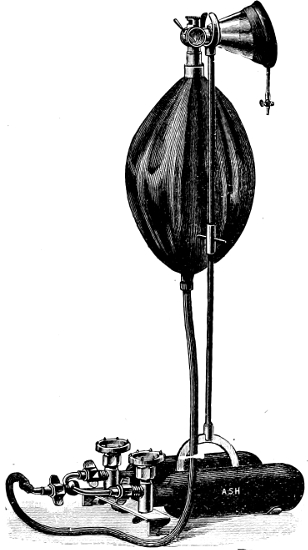
Fig. 14.—Complete N2O apparatus, showing twin cylinders, supply pipe, 2-gallon bag, 3-way tap, and face-piece.
[50]
By whatever makers the cylinder is supplied it will be found that the thread upon the outlet pipe is the same, and the metal nipple figured in Fig. 14 will fit it. To the distal end of the nipple, a rubber tube is attached which leads to a rubber bag usually of 2 gallons capacity.
The remainder of the apparatus may be of several types.
Fig. 15 shows the ordinary Barth three-way tap with facepiece; the indicator on the tap has three possible positions designated on the dial as “Air,” “Valves,” and “No Valves.” If the tap is pointed backwards towards the bag at the position marked “air” the end of the bag is closed and the patient is breathing air only. With the tap in the middle position of “valves,” the inspiration of the patient will draw gas from the bag, but the expiration closes the valve which is now in operation at the orifice of the bag, and will open the expiratory valve which conducts the expired air into the general atmosphere. In the third position of “no valves” the patient breathes both in and out of the bag.
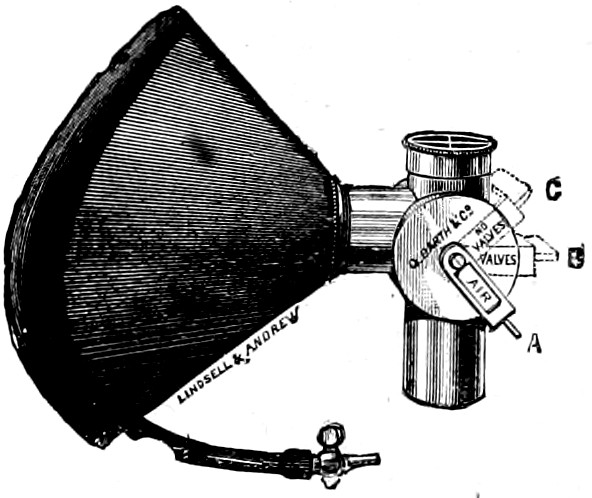
Fig. 15.—Barth 3-way N2O tap.
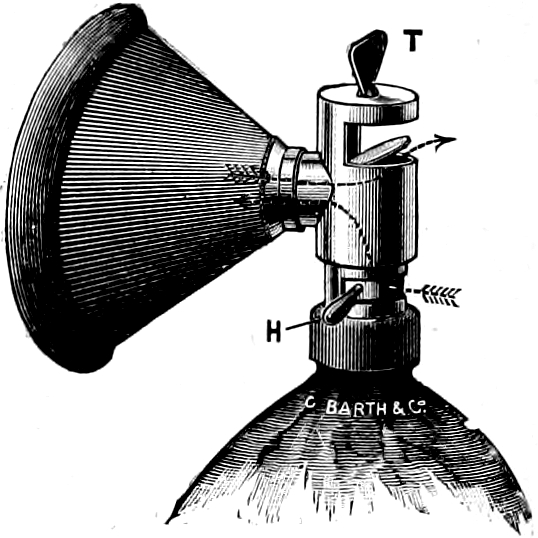
Fig. 16.—Hewitt’s wide-bore gas valves.
Fig. 16 shows the Hewitt type of inhaler. The calibre of the orifices through which respiration takes place is greater than in the Barth three-way tap, and to that extent this type of valve[51] is to be preferred. Although differently arranged exactly the same possibilities are present in it.
The facepiece is sometimes made of celluloid with an inflatable rubber edging. The object of this type of facepiece is that the colour of the lips may be appreciated by the anæsthetist during the administration. The preferable plan is to make the whole facepiece of rubber with an inflatable border. Such a facepiece made by a good maker will last many years, and is much more stable and reliable than its celluloid competitor.
This is a matter of considerable moment, particularly to those who do not use their apparatus every day. After use, the valves, facepiece, and bag should be disconnected from each other, all moisture wiped away from the bright parts, and the bag hung up with its open end downwards, and preferably in a warm room. If re-breathing has been extensively practiced it is well to wash the bag out with some carbolic lotion before hanging it up. The rubber valves in the valvepiece are liable to lose their elasticity, particularly if kept in a cold place after becoming damp. From time to time the valve piece should be taken to pieces, the valves carefully dried in front of a warm fire and powdered over with a little talc.
Most commonly nitrous oxide is administered to a patient sitting in a chair. Care should be taken that the respiration of the patient shall not be obstructed by tight clothing round the throat or chest, and that the head and neck are neither unduly flexed nor extended upon the shoulders. The patient should not have any solid food for two hours before the anæsthetic. At the last moment he should be instructed to empty his bladder. Artificial dentures if present should be removed, and, if the anæsthetic is being given for the purpose of the extraction of a[52] tooth, it will be necessary before applying the facepiece to insert between the teeth a dental prop. (See Fig. 6.) Standing to the left and slightly behind the patient the anæsthetist’s first step is to secure good apposition between facepiece and face. This is best done by working from above downwards: that is to say, secure first a good fit at the bridge of the nose, and then approximate the remainder of the rim of the facepiece to the cheeks and lower jaw. During this stage the indicator of the tap is kept at “Air.”
Working with the left foot the administrator now opens the head of one of the cylinders with the foot key. It is wise first to have loosened this with a hand key, and leave it just “on the swing,” otherwise one’s boots are apt to suffer! Gas is allowed to flow into the bag until it is partially, but by no means tightly distended. The patient is instructed to breathe naturally and easily, and during the whole process the anæsthetist should converse with him in a quiet easy way. The tap is now turned to “valves” and the patient begins to inspire the gas, a supply of which is allowed to flow steadily from cylinder into bag. After a few breaths of the gas, when the sensibilities of the patient are a little dulled, it is wise to allow the gas to flow a little more freely and to distend the bag. This exercises upon the patient a slight positive pressure, which has been proved both experimentally and practically to increase the rapidity of the absorption.[1] The valves are left in operation for some thirty or forty seconds, after which time the supply of gas should be cut off and the tap be pushed over to the position of “no valves” for further twenty seconds. This should be ample to secure full gas anæsthesia.
The phenomena seen in nitrous oxide anæsthesia are so different from those of any other that a few words must be said about them. Within a few seconds of the inhalation beginning, the colour of[53] the patient shows evidence of the presence of the gas in his blood. The normal complexion changes first to a dull pink, and very rapidly to the definite blue of cyanosis. The eye symptoms are of the utmost value. Very early the pupil begins to dilate, and the eyeball tends during the first twenty or thirty seconds to rotate as if the patient were looking for some object in his field of vision. In full anæsthesia the eyeball, however, comes to rest, usually pointed downwards. The pupil is widely dilated, the conjunctival reflex is almost or even entirely abolished, but the corneal reflex is still brisk. The respiration tends to become steadily deeper and more frequent, and in the later stages stertor at least, if not stridor usually develops. The muscles under ordinary nitrous oxide anæsthesia are rarely entirely relaxed, but the limbs hang motionless, and it is only if an attempt be made to move them into some abnormal position, that one appreciates the persistence of muscular tone.
A phenomenon peculiar to nitrous oxide anæsthesia is observed in its deepest stage. Designated as jactitation, it consists in a tremor beginning in the limbs, but spreading from them to the trunk if its development is allowed to proceed. It is a finer movement than that described under “ether tremor” (page 38), and wholly different in type from the athetosis referred to on page 38. Jactitation is almost wholly an asphyxial phenomenon, and is therefore definitely an indication that the process of oxygen starvation has been carried as far as is permissible.
The signs of fully developed nitrous oxide anæsthesia then are:—
1. Deep regular snoring respirations.
2. Dilated pupils.
3. Rotation of the eyeball downwards.
4. Loss of conjunctival but persistence of corneal reflex.
5. A colour of the skin definitely blue, but not blackish blue.
6. The commencement of jactitations.
[54]
The signs of overdose are:—
1. An enormously dilated pupil not re-acting to light.
2. Loss of corneal reflex.
3. A blackish blue colour.
4. Jactitations fully developed.
5. Failing respirations.
The final arrest of respiration in nitrous oxide anæsthesia is usually painfully sudden. Upon the respiratory side the only warning is one or two gasps, and even that is sometimes absent. The paralysed pupil and the jactitations are the most useful signs of overdose.
The above, then, may be taken as an account of what one expects to see in a normal gas anæsthesia during the induction stage. For the great majority of cases, nitrous oxide is given for the purpose of rendering painless the extraction of a tooth, and it is, in this large class of case, the induction stage only which need be considered. It requires only some fifty to sixty seconds to bring the patient to the stage described under the heading “fully developed anæsthesia” and when that has been attained, the mask may be removed and the operation begun. From the moment of removal of the mask, however, it must be noted that the patient begins to breathe fresh air and to eliminate the N2O. The period of anæsthesia available to the surgeon or dentist during which he must perform the operation, is therefore very small. In thirty seconds the patient has frequently recovered sufficiently to begin to feel pain, and it is rare to secure more than forty-five or fifty seconds by the use of a single dose of nitrous oxide.
If the nature of the operation does not necessitate the removal of the mask from the face, it is possible to maintain nitrous oxide anæsthesia for some considerable time. The exact length of that time varies a good deal with two factors—the type of patient and[55] the experience of the administrator. Heavily built muscular patients are not easily dealt with by prolonged gas anæsthesia (unless with admixture of oxygen as explained in chapter viii.) Of far greater importance, however, is the other factor. The student can easily be taught to give a single dose of gas for the extraction of a tooth, or the momentary incision of an abscess. He will, however, be wise to secure a good deal of practice in that class of work before attempting to prolong gas anæsthesia for more than a minute or two.
With reasonable skill and experience and the utmost care, it is, however, perfectly possible to prolong nitrous oxide anæsthesia for periods of five, ten, or even fifteen minutes in the average healthy patient. As soon as the signs of full anæsthesia appear, the valve tap is pushed back to “air” for the space of one inspiration and one expiration, and then at once pushed back to “no valves.” By this manœuvre, one inspiration of air is permitted to the patient, whose colour at once shows amelioration, or at any rate no further progression of cyanosis. The admission of air is repeated every third, fourth, or at most fifth respiration. After the first minute or so of this cycle of events, it is obvious that the contents of the bag will be composed of a mixture of nitrous oxide, air, and CO2 in proportions quite impossible to calculate. It is therefore best to push the indicator to “valves,” and allow the bag to be emptied by the suction of the patient’s inspirations. The cylinder head is then opened by the turning of the foot-key, and the bag filled again with gas. The cycle of “air” and “no valves” is then begun again for another minute or so.
It must be understood that by this process, it is not to be expected that an ideal anæsthesia can be produced. Some movement of the patient will not improbably take place when sensitive structures are cut or handled by the surgeon, and at no time will the muscles be entirely relaxed. Such an anæsthesia is therefore only suitable for a limited class of case, but does admirably for,[56] say, opening an abscess, exploring its interior, and removing from it a sequestrum or an easily found foreign body. During his service in Macedonia the author had not at his disposal any of the appliances later to be described under the heading of nitrous oxide and oxygen, and found “gas and air” a most useful form of anæsthesia for the requirements of military surgery as seen in a Base Hospital, under active service conditions.
In the healthy subject, there is no safer anæsthetic than nitrous oxide when administered properly and limited to its proper province.
From the account given of the physiological action of the gas it will, however, be obvious to the student that in a limited class of case its use is not permissible. Such cases fall into two categories.
Firstly, cases in which an asphyxial element already exists will have their condition greatly aggravated by the substitution of N2O for the oxygen in their blood.—Already caught in the vicious circle of asphyxia, nitrous oxide would but push them deeper into the vortex. Examples of such cases are patients suffering from tumours or inflammatory swellings in the neck which are pressing upon the air passages. In passing, one may note that it might be the desire of the surgeon to submit an individual case falling into this group to the operation of tracheotomy for the immediate relief of the condition. The short space of time required for this little operation might well tempt the unwary to choose nitrous oxide as the anæsthetic, and in point of fact such an error of judgment has more than once been made with fatal results.
Secondly, no patient suffering from any condition which will be aggravated by a sudden rise of blood pressure, should be submitted to nitrous oxide undiluted by oxygen.—Examples of such conditions are cases of dilated right heart with weakened cardiac musculature.
Such hearts could not be expected to work against a peripheral[57] resistance suddenly raised, say, from 120 mm. of Hg, to 180 or even 200 mm.—figures well within the possible in deep gas anæsthesia. Similarly, so great an increase of pressure would be dangerous to a patient suffering from an aneurysm, or from extensive arterio-scelorosis with high blood pressure.
It will be noted that the above warnings are limited to the use of pure nitrous oxide, that is, N2O unmixed with oxygen. The extent to which the dangers referred to can be met by the admixture of oxygen in the manner to be described in the next chapter is largely a matter of the skill and experience of the administrator.
The object of using this route is to be able to continue the administration throughout the period in which the dentist is doing his work. The essentials of a suitable apparatus are:—
1. A malleable nosepiece which can be closely adapted to the nose.
2. Two supply pipes from bag to nosepiece.
3. Some means of admitting air to the stream of gas.
4. A two-gallon bag.
5. A supply of gas.
6. A mouth cover with an expiratory valve only.
The patient is instructed to breathe in through the nose, but to expire through the mouth. The gas is supplied under some pressure and the mouth cover ensures that no air is inspired by that route. Some patients find it easier to conduct both inspiration and expiration through the nose, and for their benefit an expiratory valve is also provided in the nosepiece. After unconsciousness has supervened, nearly all patients begin to-and-fro nasal breathing. The mouth cover may then be removed, and if it be desired to economise gas, the expiratory valve in the nosepiece may be thrown out of action.
[58]
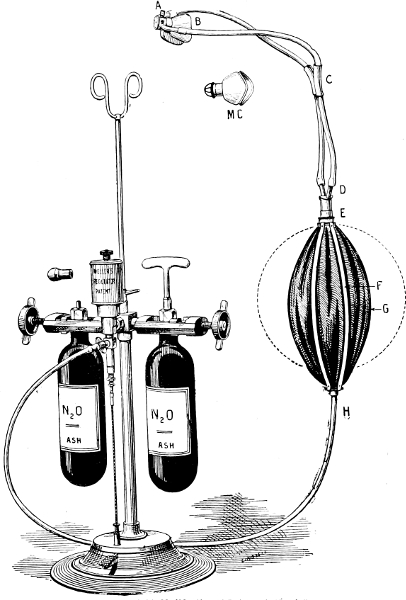
Fig. 17.—Ash’s Modification of Paterson’s Nasal Gas
Description:—A—Nose-Cap Attachment with Stopcock for Air and Gas, and with Inspiratory and Expiratory Valves and Shutter. B—Nose-Cap. C—Sliding Clip on India-rubber Tubings. D—Bifurcated Mount. E—Bag Mount. F—Gas Bag Compressor. G—Gas Bag. H—India-rubber Tubing. MC—Mouth Cover. This is fitted with an expiratory valve, and should be used at the same time as the Nose-Cap. By using the two together patients are more quickly anæsthetised than they would be if only the Nose-Cap were used, and the Nitrous Oxide is economised.
[59]
Air must be admitted in limited quantity through the tap after the first thirty seconds or so; by a judicious regulation of this mechanism, anæsthesia may be prolonged for five or ten minutes. Facility with nasal gas comes only after some considerable practice.
Fig. 17 shows Ash’s No. 3 Patented Nasal Inhaler, which admits of Air or Gas being administered either by the Naso-Oral Method, or by to-and-fro nasal breathing. Air only is admitted when the Shutter A is open and turned to the right as far as it will go. Nitrous Oxide is admitted when the Shutter A is open and turned to the left as far as it will go, and the patient will breathe it in-and-out through the nose. For the Nasal Oral Method, close Shutter A and turn it to the left as far as it will go. This will cause the patient to inhale through the nose and exhale through the mouth.
Nasal attachments are provided with most of the gas-oxygen apparatuses mentioned in the next chapter. With them good results can be obtained with much greater ease.
For a more detailed account of nasal methods, the student is referred to works devoted entirely to Dental Anæsthesia.
[60]
The account given in the previous chapter of anæsthesia by nitrous oxide and air will have convinced the student that it is a somewhat inelegant method with a limited sphere of usefulness. The reason is obvious. In atmospheric air, oxygen exists only in the proportion of about one to four of nitrogen. To sustain life it is therefore necessary to admit to the anæsthetic mixture an amount of air which leaves too little room for the anæsthetic factor—nitrous oxide. If, however, pure oxygen be used, the nitrous oxide is diluted to a much less degree, and far better results are obtained.
The exact scope for gas-oxygen anæsthesia cannot at present be defined with certainty. The work of Crile, and the experience of the war have done much to enlarge it. We may say that the following are definite indications for its use:—
(1) Minor operations lasting 5–15 minutes, particularly if performed on out-patients.
(2) Operations of any variety upon the subjects of severe shock.
(3) Operations upon patients suffering from acute sepsis.
(4) Operations repeated upon the same subject at short intervals.
As regards (3) and (4), the lack of toxic properties in nitrous oxide gas, and the rapidity with which it is eliminated, give it a tremendous advantage over ether or chloroform. To men with shattered bones and extensive damage to soft tissues, badly infected with sepsis, who required repeated opening up of pockets, changing of gauze packs, etc., the advantage of gas-oxygen over ether was[61] evident, and was easily appreciated by the patients themselves during the late war.
There are, however, certain drawbacks to the method which must be appreciated—
(1) The necessary plant is heavy, bulky, and costly; it cannot be easily transported.
(2) The running cost is high as compared with ether or chloroform.
(3) It has been said by some that gas-oxygen can only be given by an expert. That is a statement too extreme, in the author’s opinion. Certainly, of all anæsthetics it is the most difficult to give successfully. Adequate study and proper teaching by an expert are required, but given these two helps, any one can soon learn to administer gas-oxygen for minor surgery. Considerably more experience is, however, necessary before the beginner should give it for an abdominal section.
A good gas-oxygen apparatus is necessarily rather complicated. The machines in the market are numerous, and of the most diverse external appearance. Certain broad principles, however, underlie all the machines, and it is to be hoped that some one of them will before long become practically the standard. Once that is effected, hospitals and nursing homes could be expected to provide them. So long as every anæsthetist asks for a different machine, they certainly never will do. A good machine must provide means for the following:—
(1) An even flow of both gases under perfect control.
(2) A percentage of Oxygen in the mixture rising at the will of the administrator from 2 to 15 or 20.[2] To meet this requirement it is not necessary that any indicator should be[62] provided which shows with mathematical precision what percentage of oxygen is being given. The colour of the patient tells us at once if too much or too little oxygen is being supplied, and all we need in the apparatus is some mechanism whereby we can tell approximately to what extent we are increasing or decreasing the percentage.
(3) Positive Pressure.—If the pressure at which the gases are supplied to the patient can be raised a little above that of the ordinary atmosphere, absorption is increased and a deeper anæsthesia produced. In the author’s view, this is an essential point in a good instrument.
(4) Re-breathing.—To supply the whole volume of gases required for inspiration during a long operation is costly and quite unnecessary. Yet that is what is being done if the whole administration is conducted upon the “valvular” principle. Moreover, a prolonged inhalation upon the valves tends to remove a great deal of CO2 from the patient’s blood and tissues (see Chap. IV.). Periods of partial or complete re-breathing do much to deepen respiration, and reduce the cost of the anæsthetic.
(5) Warming the Gases.—While not essential, this is certainly an advantage.
(6) Addition of Ether Vapour to the mixture.—Gas-oxygen even well given is hardly capable of reducing to quiescence very robust people, unless the oxygen percentage is kept to an undesirably low level. The merest trace of ether vapour as an adjunct is a great assistance during the stages of the operation where very sensitive structures such as the parietal peritoneum are being handled. The more experienced the anæsthetist, the less will he require such assistance.
This, with the exception of one designed by Dr Guy and the author, and described on page 130, is the only machine with any[63] pretence to portability by hand. It does not satisfy all the requirements above referred to, but the fact that it was the first practicable means introduced in this country to give gas-oxygen entitles it to full description. (See Fig. 18.)
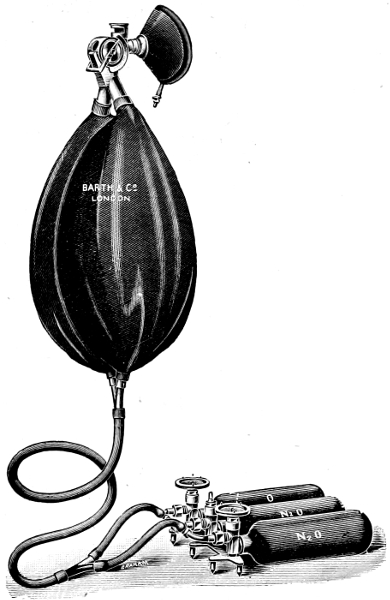
Fig. 18.—Hewitt’s gas oxygen apparatus.
Essentially it consists of the following:—
[64]
(1) A supply of nitrous oxide and oxygen in separate cylinders. Hewitt’s own stand held two of nitrous oxide and one of oxygen.[3]
(2) Rubber pipes of supply for each of the two gases. For convenience, it is sometimes arranged that one of these shall run inside the other.
(3) Two 2-gallon bags. Nitrous oxide is led into the one, oxygen into the other. The mouth of each bag is guarded by an inspiratory valve.
(4) The mixing chamber. Upon the surface of this are marked successively: “Air,” “N2O,” “O2, 1 2 3 4 5 6 7 8 9 10.” As the indicator is pushed from “air” to “N2O,” the patient begins to inhale nitrous oxide only, but as it travels into the numerals 1, 2, etc., a proportion of oxygen is added.
Immediately below the mixing chamber is the expiratory valve.
(5) Lastly, there is the facepiece, identical with that used for pure nitrous oxide.
It would be fallacious to suppose that the numerals 2, etc., on the dial represent accurately the percentage of oxygen yielded by the instrument when the indicator points to one of these figures, nor did Hewitt ever make such a claim. What the figures do represent is a number of holes in the wall of the mixing chamber, opposite to the aperture from the oxygen bag, which are uncovered one by one as the indicator moves over. The amount of oxygen which enters into the mixing chamber is regulated by the number of these holes uncovered, and also by the tension of the oxygen bag. If the figure on the dial is to be even a rough index of the actual percentage of oxygen present in the mixture, it is necessary[65] to keep the tension reasonably constant, i.e. to regulate the flow of oxygen from the cylinder by manipulation of the foot key. In a brief administration for, say, a dental case, this is not necessary. It is sufficient to fill the oxygen bag once, and then turn off the supply. If, however, a long administration is required, a constant flow of oxygen of just the requisite amount must be secured.
Put the lever at “air,” and fill up each bag to an equal and moderate degree of distention. Adapt the facepiece accurately to the patient’s face, and then push the lever to “N2O”. After a few inhalations, move to 2 of oxygen; regulate the flow of nitrous oxide from the cylinder so that the N2O bag remains slightly distended. Gradually move the indicator along the numerals until the figure 6 or 8 is reached at the end of about a minute or a minute and a half. Women and children require more oxygen than men. The former are easily cyanosed; if the latter are fed too generously with oxygen, they are apt to become excited. Take as your guide to the amount of oxygen required the colour of the patient, the type of respiration, and the size of the pupil.
The colour aimed at can only be learnt by experience, but is best described as a dull pink.
The Type of Respiration.—Too little oxygen leads to stertor and even stridor; too much oxygen, to a light almost noiseless respiration, which to the experienced ear is the certain precursor of a stage of excitement. Such a stage is clear evidence of too much oxygen having been given.
The pupil should not be dilated to anything like the degree seen with undiluted nitrous oxide. A moderate distention only is to be desired.
Full Anæsthesia should be reached in 100–120 seconds. It is marked by:—
[66]
(1) Dull pink complexion; (2) full respiratory movements with a stertor not exceeding that of gentle snoring; (3) eyeballs rotated downwards; (4) moderately dilated pupils; (5) loss of conjunctival reflex; (6) corneal reflex present but not very active.
If the object be the removal of a tooth, the mask may now be removed, and the dentist may rely upon a period of anæsthesia somewhat longer than that furnished by pure nitrous oxide. He ought to secure approximately one minute in which to do his work.
Anæsthesia by this apparatus may however be prolonged for an indefinite time if desired. In order to maintain the patient in the condition described above, it will be necessary gradually to increase the supply of oxygen. For this purpose Hewitt added to his mixing chamber a supplementary oxygen supply giving 10 or 20 volumes of oxygen. As a matter of fact, all the necessary supply can be got through the original ten holes if the tension in the oxygen bag be increased. The regulation of all this requires, of course, considerable practice and experience.
The signs upon which we rely for warning that the supply of oxygen is insufficient to keep the patient safe, are chiefly the colour of the face, which must not pass from dull pink to blue, and the size of the pupil.
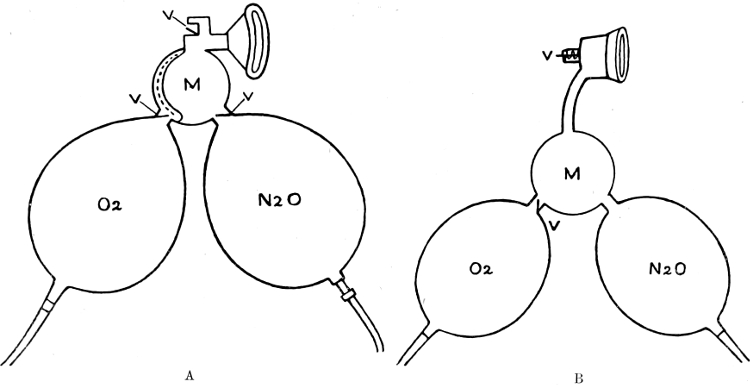
Fig. 19.—Diagrams to illustrate action of (A) Hewitt (B) Teter gas oxygen apparatus. Note that in A the mouths of both bags are guarded by valves of inspiration, while in B the oxygen bag only possesses it.
These are chiefly two:—
(1) There is no means of producing positive pressure. Any attempt to distend the nitrous oxide bag beyond a certain point simply leads to escape of the gas through the mixing chamber and out of the expiratory valve even during inspiration. To this defect especially must we attribute the fact that an anæsthesia deep enough for abdominal section is difficult to secure with the Hewitt instrument.
[68]
(2) There is no means of securing re-breathing. The whole administration must of necessity be conducted “upon the valves.” This latter fault is remedied by the modification introduced by Burns, who took away the inspiratory valve from the mouth of the N2O bag, and fitted a cap over the expiratory valve which could be rotated so as to throw the valve out of action. The author first met this modification at a Base Hospital in France, and found it a great improvement upon the original instrument. It is, however, only an imperfect attempt to adopt Teter’s chief principle.
The rapid spread of nitrous oxide and oxygen anæsthesia in the U.S.A. brought forward a number of machines of which Teter’s was the forerunner; the other well-known machine of the group is the Clarke. They differ in principle from the Hewitt apparatus in that they permit re-breathing and the use of positive pressure. Diagrammatically, the two are contrasted in Fig. 19.

Fig. 20.—Details of the Clarke Expiratory Valve. In the position of the lever marked “open” the valve lifts easily and widely, and the breathing will be purely valvular: in the position marked “half open,” the valve lift is diminished, and the breathing is partly valvular, partly to-and-fro. In the position “closed” re-breathing only is possible.
The key to Teter’s advance is his removal of the inspiratory valve from the mouth of the nitrous oxide bag, and his substitution for Hewitt’s rubber expiratory valve, of a rigid valve, the lift of which can be diminished or entirely abolished, at will (see Fig. 20). By damming, as it were, the flow from the expiratory valve, the administrator can oblige the patient to practise a certain amount of re-breathing, and, if he keeps up a free flow of the gases, he[69] can develop a pressure in the nitrous oxide bag definitely exceeding that of the atmosphere.
Teter also introduced into his apparatus a means to warm the gases, and to add a little ether vapour to the mixture when required.
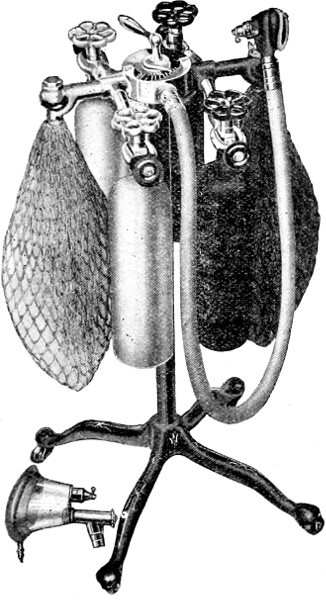
Fig. 21.—The Clark gas oxygen machine.
The Clarke machine is similar in principle to the Teter, but makes a strong point of the intimate mixture of the two gases produced in the mixing chamber which occupies the centre of the apparatus (Fig. 21).
[70]
In both these machines, it will be observed, the two bags for N2O and O2 respectively are attached to the stand, and the mixed gases are led to the patient by a pipe of wide bore. When re-breathing occurs, it must therefore be up and down this pipe, but the width of the bore seems to obviate any disadvantage which theoretically might be expected from this form of respiration.
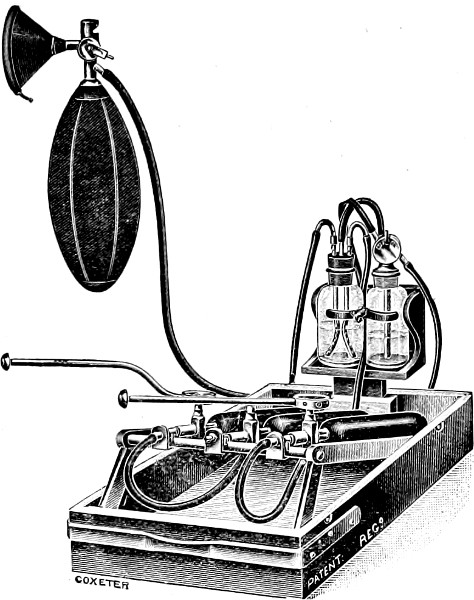
Fig. 22.—Marshall’s sight-feed gas-oxygen apparatus. Of the two glass bottles the one to the left is the sight-feed, that to the right the ether chamber.
In the experience of the author and of many other anæsthetists, very good results can be obtained from either of these machines.
In the author’s opinion, machines based upon this principle are likely to take a prominent place in the future of gas-oxygen.[71] Fig. 22 explains the simple mechanism. Each gas is led through a tube dipping into water contained in the sight feed mixing chamber. The ends of the pipes are open, and on the sides of each pipe also are a number of holes. If the pressure at which either gas is delivered is small, bubbles will be seen ascending towards the surface of the water from the upper holes only. The greater the pressure, the further down the pipe does the gas carry before all of it escapes through a hole, and one can therefore get an accurate estimate of the pressure from the number of holes through which the bubbles are seen escaping.
Upon the surface of the water, the two gases meet and enter into mixture and are conveyed away by the third pipe which, of course, does not dip into the water.
Once the eye of the anæsthetist is trained to its use, this is a very simple means of gauging the relative proportions of oxygen and nitrous oxide which are being delivered, and manipulation of the cylinder heads combined with visual inspection of the sight feed enable one to strike the right proportions very easily. The nitrous oxide is usually kept at a constant pressure sufficient to ensure bubbles, not only from all the side holes, but also a few from the open end of the tube. The oxygen pressure is begun at the point where there is a little bubbling from the top hole only, and is gradually increased until there is a full supply from two holes, occasionally a little even from a third.
Messrs Coxeter have recently brought out two sight feed machines designed by Mr Leonard Boyle and Dr Geoffrey Marshall, of which the latter is shown in Fig. 22. This apparatus may be put up in either portable form or a larger type for use in hospitals. An ether chamber is provided for use when necessary in either type.
As originally introduced, the remainder of the apparatus consisted simply of an ordinary two gallon bag, Barth 3-way tap, and rubber facepiece. With such an appliance, it is not possible[72] to secure “positive pressure, a point which the author brought to the notice of the makers. Messrs Coxeter are willing to supply a facepiece and expiratory valve which obviate this defect, being supplied with a mica expiratory valve the lift of which can be controlled. There should be no inspiratory valve.
The patient is prepared with the same scrupulous care as if ether or chloroform is to be administered. Half an hour before operation, morphia gr. ⅙ and atropine gr. ¹⁄₁₀₀ are given hypodermically. The anæsthetist before beginning administration, must look over the apparatus most carefully and satisfy himself that every part of it is in perfect order, and that a sufficient supply of both gases is at hand.
The inhalation is begun by the use of nitrous oxide alone, given “on the valves,” and at no great pressure. After a few breaths, oxygen is added very guardedly, the proportion being steadily raised during the first two minutes: after that point, a further increase will not be necessary until several more minutes have elapsed. The pressure at which the mixture is being given is also steadily increased and should reach the maximum permissible within a few minutes. A useful plan is to allow the flow of gases to remain constant, but to close the expiratory valve at frequent intervals for about forty to sixty seconds at a time. During this period of complete re-breathing the tension in the supplying bag will of course rise, falling again slightly when the expiratory valve is allowed once more to come into action. As soon as the tension falls appreciably, the valve is again closed down.
It is wise, particularly in one’s early days, to give a trace of ether vapour during the latter part of the induction stage, and to maintain it until the operation is well under way. Once the[73] anæsthetist is satisfied that the narcosis is proving deep enough for the purposes of the operation, the ether may be shut off and will probably not be required again.
Remember that depth of anæsthesia can be secured in three ways—(1) cutting down the oxygen percentage; (2) increasing the tension of the mixed gases; (3) adding a little ether. Of these, No. 1 is most undesirable, and if carried to the least excess over a period of more than a minute or two may lead to an accident. No. 3 is the means for the beginner to rely upon, until he learns the judicious and skilful use of No 2. The anæsthetist who is learning the method of anæsthesing must resolve that nothing shall tempt him to overstep the stage of dull pink colour, and moderate pupils. If with gas-oxygen alone, he cannot get a satisfactory anæsthesia without resorting to oxygen starvation, let him not be ashamed to turn on his ether.
Abdominal relaxation sufficiently complete to permit the surgeon to explore the abdominal cavity with ease, is not readily secured by gas-oxygen in a patient of robust type. Fortunately, it is the weakly or the severely shocked who really need this form of anæsthesia, and in them abdominal relaxation is fairly easily obtained.
Professor Crile, as has already been explained, does not rely upon the inhalational anæsthetic alone. He infiltrates each layer of the parietes with novocain, thus producing a local anæsthesia. If this method be faithfully carried out by the surgeon, a most complete relaxation of the muscles can be secured.
[74]
The drug commonly known as ether and otherwise described as ethylic ether or sulphuric ether, has a chemical formula (C2H5)2O. It is a transparent colourless fluid with a specific gravity of ·720 to ·723. A brand much used in the States has an S.G. of ·713 only, a point which is greatly emphasised by its supporters, who claim that it volatises quicker and therefore is more powerful in action. The author has in actual practise not found much difference between this brand and any good British one.
Ether is highly inflammable and volatilises readily at ordinary room temperatures. Its boiling point is 96° to 98° Fahr. Whether evaporating from a fabric such as gauze, or from bulk in a jar, ether cools very rapidly, and the fall in temperature soon reduces the ease of its volatisation. This point is of some practical importance in anæsthetics, and some years ago the author made a number of observations, hitherto unpublished, with a view of ascertaining some definite facts in this connection. His results will be found in Appendix I.
Ether vapour is heavy—two and a half times heavier than air. It therefore tends in a room to flow towards the floor, and to remain for some time unmixed with the general atmosphere. Since it is highly explosive, this constitutes a definite danger if any naked light or open fire is present. Everyone who handles ether should bear in mind these physical peculiarities of its vapour.
Ether is affected by prolonged exposure to bright sunlight, and also by prolonged bubbling through it of air, nitrous oxide, or oxygen. Ether which has been subjected to any of these[75] measures should be inspected before being put back into reserve, and if any brown discoloration is noticed, it should either be sent to the hospital laboratory for redistillation, or presented to the theatre sister for use as a cleaning agent. Such contributions are always gratefully received.
Most of the ordinary impurities of ether are acid in reaction, while ether itself is absolutely neutral. Any specimen which turns litmus paper red should be sent to the laboratory for examination.
Ethylic alcohol may be prepared either from ethyl alcohol or from methylated spirits. In the former case it carries, however, the cost of the duty imposed upon potable spirit, and since perfectly good anæsthetic ether can be prepared from the latter source, it is waste of money to use the more expensive article.
Ether acts upon the nervous system like other anæsthetics: as compared with chloroform, however, the stage of excitation of each centre before its paralysis is apt to be marked. There is, therefore, in some subjects, a greater tendency to struggle; healthy subjects properly handled do not show much evidence of irritation of the cerebrum. All, however, show some evidence of stimulation of the respiratory centre, which is not prolonged. Prolonged deep and rapid respiration under ether is due to other causes than the action of the drug itself. It is of course seen in “closed ether,” but the active agent is excess of CO2, not ether.
The working margin of safety in ether, i.e. the stage between loss of spinal reflexes and the poisoning of respiratory centre is much wider than in chloroform.
Some experiments of Waller made many years ago showed that upon nerve tissue, ether acts much less powerfully than chloroform: in the proportion, he found, of one to seven or eight.[76] These laboratory results have received entire confirmation by later workers who have estimated the actual vapour strength required of either drug to produce or maintain anæsthesia. Roughly, to induce anæsthesia, we require 2 per cent. chloroform, or 16 to 18 per cent. of ether (see Appendix II.).
The first effect of ether is a temporary stimulation of the heart, which beats more rapidly and more strongly, thus raising the blood pressure. This effect is not very prolonged; like all other drug stimulation, it is followed by depression. In the healthy subject properly anæsthetised, such depression is very moderate in degree, and in a normal administration it is probable that the heart, after the first few minutes, is acting very much at its normal speed and force. Ether is, however, a marked vaso-dilator, and the net result upon blood pressure is a slight fall after the first few minutes.
If the method in use is “closed,” the pressure remains slightly raised for some considerable time, usually throughout the administration. The slight anoxaemia induces a vaso-constriction; and the CO2 excess, in the view of Henderson (see page 10), maintains a good return of venous blood to the heart and a satisfactory cardiac output. For a note of certain blood changes resulting from ether and other anæsthetics (see Appendix III.).
In addition to the effect upon the medullary centre already referred to, ether effects the respiratory tract more profoundly than other anæsthetics. The mucous membranes are irritated, and in some cases there is a great outpouring of mucous. Though usually limited to the upper part of the tract (nose, pharynx, and trachea), the irritation sometimes extends deeply into the chest, affecting even the small bronchioles. These unpleasant effects of[77] ether are in the great majority of cases, quite transient: after the first ten minutes no addition to the secretions is noticed. In a minority, however, the effect persists, the whole chest is filled with moist sounds, and persistence with the drug is impossible.
The kidneys are always slightly irritated by ether, and if they are or recently have been subject to inflammatory disease, a very acute exacerbation is apt to follow the use of the drug. In the healthy kidney this is not to be feared, nor does it seem to be an appreciable danger where one kidney is sound, even if the other is the seat of gross organic disease necessitating its drainage or removal.
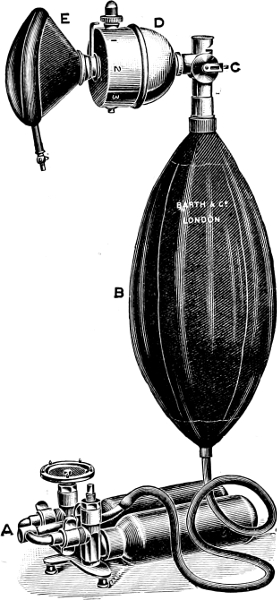
Fig. 23.—Clover’s ether inhaler, with nitrous oxide attachment.
Many methods have been tried, but those which at present hold the field are—
(1) Closed Ether.
(2) Open Ether, more properly called the Perhalation Method.
(3) The “Vapour” Method.
(4) The Rectal Method (Gwathmey’s oil-ether).
(5) The Intratracheal Method, described separately in Chapter X.
[78]
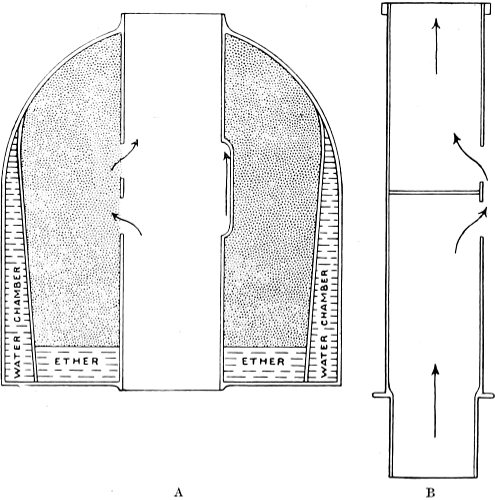
Fig. 24.—Diagram of a vertical section through the middle of Clover’s Inhaler. A. shows the ether dome; B. Central tube removed from apparatus.
The two inhalers originally brought out for this were Clover’s in London, and Ormsby’s in Dublin. At a later date Hewitt’s “wide bore” modification of the Clover was introduced.
(a) The Clover instrument (see Fig. 23)[4] consists of a face-piece, a dome-shaped ether chamber, and a one-gallon bag, usually attached to the top of the ether chamber by a T-shaped tube. The details of the method by which the amount of ether inhaled by the patient is graduated are best appreciated by unscrewing the[79] milled head at the top of the dome, and withdrawing the tube which runs through it (see Fig. 24). In the tube will be found two slots, one about half an inch above the other, and each extending for half the circumference of the tube. Between these two slots the tube is divided by a diaphragm. In any case, therefore, air passing up or down the tube must pass in and out of these slots.
Now turn to the tubular space left in the dome piece, and examine visually and with the finger its interior. On the one side of its middle will be found two slots leading into the circular ether chamber which occupies a large part of the dome. On the other side will be found a small cavity, as deep from above downwards as the two slots combined, but not communicating with the ether chamber. It is obvious that with the tube inside, if this cavity is opposite the slots in the tube, air will pass up the tube out of one slot and back into the other, without coming into contact with the ether at all. If on the other hand the slots in the tube are opposite the slots in the ether chamber, the air passes over the surface of the contained ether, and volatises some of it.
Intermediate positions of the tube give a condition where part only of the air passes over the ether. The indicator attached to the tube, combined with the figuring “O, one, two, three, full,” to be found on the outside of the base of the dome, shows at any moment what proportion of the air is passing into the ether chamber.
To use the instrument, fill the metal measure provided with ether, withdraw the stopper from the ether chamber, and pour in the ounce and a half of ether which the measure contains. Replace the stopper, and blow through the tube to expel any ether vapour which may have appeared in it. Leave the rubber bag at first unattached: the patient will feel more comfortable if during the first minute the top of the tube is open. With the indicator at 0 adapt the face-piece to the face and allow[80] the patient to breathe up and down the tube. By rotating the dome, ether is then gradually turned on, until the figure two is reached in the first minute. The indicator is then slipped back nearly to zero for a second, and the rubber bag slipped on during an expiration: it must be moderately inflated to supply the requisite volume of air for respiration.
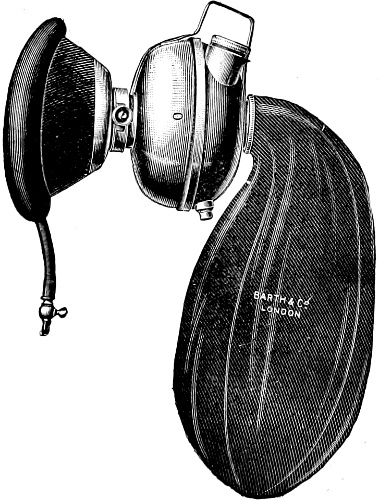
Fig. 25.—Hewitt’s wide-bore ether inhaler.
The rotation of the dome is again begun and the indicator is made to travel away from the zero, until at the end of about five minutes, it reaches “full.” After the first few minutes, it will be necessary to give an occasional breath of fresh air, otherwise an undesirable degree of cyanosis will result, but it must be done with great discretion, or struggling will ensue. At the end of about five minutes, anæsthesia should be fully established. A[81] little extra ether is then poured into the chamber, the indicator pushed back to about “two” and the administration continued. One breath of fresh air is given in every three or four. Spells may be given with the bag off altogether, but during such periods the indicator will require to be advanced a little, and refills of ether provided more frequently than would be necessary if the bag were on.
The principle of this is identical with that of the Clover, but the channels being wider, there is less mechanical interference with the ingress and egress of air. The actual construction differs also, in that to turn on the ether, instead of rotating the dome, one moves the indicator (see Fig. 25). The instrument certainly gives results a little better than those obtainable by the Clover, but it is heavier, and rather more bulky.
This consists of a facepiece, a cage made of wire or thin steel slips and containing a sponge; and lastly, a one gallon bag which fits over the cage. In the face-piece is an air vent, which can be either entirely closed, partially or entirely opened.
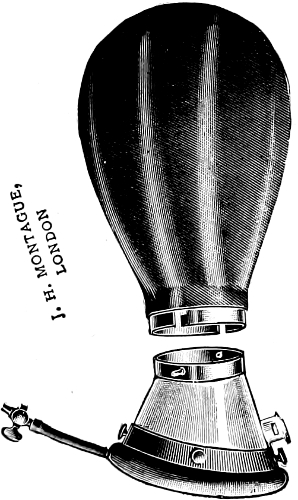
Fig. 26.—Ormsby’s Inhaler. The cage for the sponge does not show in the figure, it projects upwards from the bag-mount, and is therefore enclosed in the bag.
To use the instrument, take out the sponge and warm it either by wringing it out of hot water, or better by leaving it a few minutes on the top of a hot steriliser. Push it back into the[82] cage, open the air vent fully, and holding the inhaler upside down, pour on to the sponge a measure full (about half an ounce) of ether. Tell the patient to inhale deeply, and then catch the resulting expiration in the bag by quickly adapting the facepiece to the face at the appropriate second.
After a few seconds, begin to close the air vent, when it will be found that the bag begins to wax and wane with each expiration and inspiration respectively. After the first three minutes, the inhaler must be removed, more ether poured in, the air vent opened again partially, and the inhaler again applied to the face. After full anæsthesia is induced, the air vent may constantly be left partially open.
N.B.—It must be observed that the air vent is not valved: it is merely an opening through which part of the respired air may pass in and out without going near the ether sponge.
In actual practice, the induction stage of closed ether is almost invariably assisted by using either nitrous oxide, or a small dose of ethyl chloride as a preliminary: these methods are described in Chapter XV.
The question now arises, what scope is to be assigned in modern anæsthesia, to closed-ether methods. Formerly a large proportion of anæsthesias, long or short, were conducted by the closed method, and while the greater number of anæsthetists no longer utilise them to the same extent as formerly, they may still be regarded as of the utmost value in a limited class of cases. They are speedy in action, powerful enough to overcome the most refractory patient, and with reasonable skill very safe. On the other hand, the anæsthesia obtained is not of the most desirable type. There is a great deal of salivation and mucous secretion from the respiratory mucous membranes; the respiratory movements are deeper than in open methods, from the excess of CO2 present in the blood, and this leads to a good deal of heaving of the abdominal wall, which may[83] be most troublesome to the surgeon if he is opening or closing that cavity. Moreover, after their use more headache, malaise, and vomiting occur than after open-ether, and perhaps a little more tendency to bronchitis or pneumonia. For these reasons, many anæsthetists and surgeons now object to their use in abdominal surgery, though some still adhere to them for the induction stage, passing to the open method when the patient is once well under.
As already explained the strictly accurate term for this is Perhalational Ether, but so cumbersome a terminology stands small chance of general acceptance.
The essential points in a proper outfit have already been explained (see page 28) and are all well met by the mask and ether dropper introduced by Mr Bellamy Gardner (see Fig. 27). The mask is covered with from twelve to sixteen layers of gauze, and lies on the gauze ring, shown in the Fig. 28A, which completes the fit between face and facepiece. The dropper fits into the ordinary six ounce dispensary bottle: the long arm dips into the ether, the short one allows air to enter the bottle to replace the ether used. A dropper can also be improvised by[86] using a cork with slots cut at each side and with a gauze or wool wick inserted along one of these. The author finds these uncertain in their action, however: with Gardner’s dropper, a steady flow of drops of ether slow or fast as required, can always be obtained once the student has acquired the knack of using the appliance.
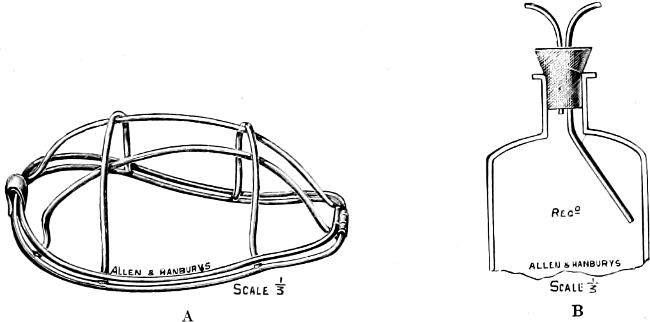
Fig. 27.—Bellamy Gardner’s (A) open ether mask; (B) ether dropper.
Fig. 28.

A.—Open ether. Ready to begin.
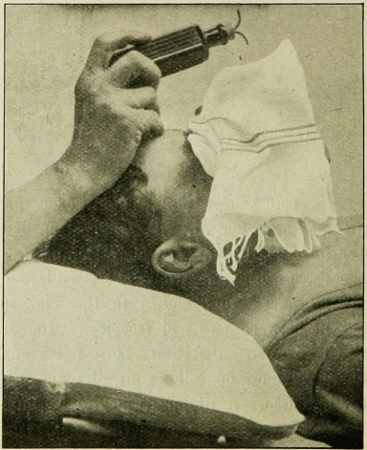
B.—Open ether. Condensing towel in position.
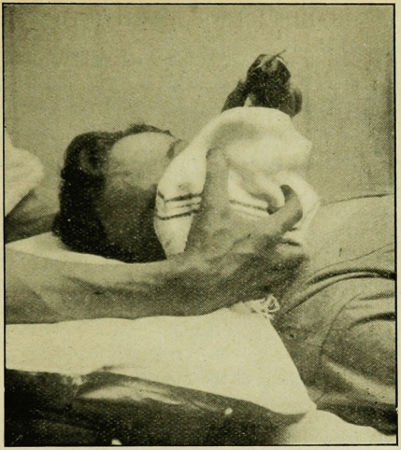
C.—Open ether. Correct method of holding mouth and jaw.
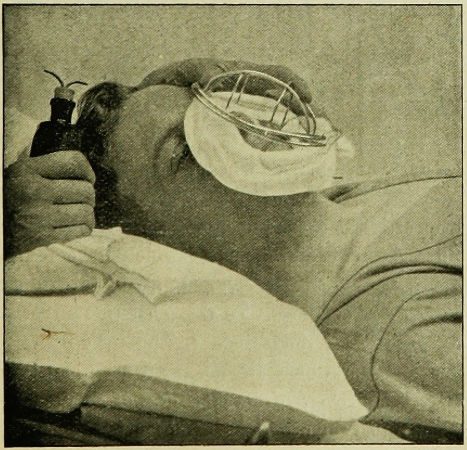
D.—Open ether. Alternative method of holding mask. The towel and gauze have been removed so as to show the tilting of the mask which this method is liable to cause.
To Mr Bellamy Gardner’s outfit, the author adds a folded towel, pinned at one corner, so as to form a short cone. The base of this cone embraces the mask and face; through its upper apperture the anæsthetic is dropped on to the mask. The cone can be rotated into the position most convenient for this purpose in any given position of the patient’s head (Fig. 28).
Open-ether is not a powerful anæsthetic, just not powerful enough for one to be sure that one can induce full anæsthesia with it alone, in a powerful subject. The reason for this is shown in Appendix II, and may be here condensed by explaining that some 18 per cent. to 20 per cent. of ether vapour is required to induce anæsthesia, while it is not easy to get more than 14 per cent. off an open mask. How is this situation to be met?
Reference has already been made to one solution of the problem. A closed ether method may be used for induction, and this practice is widely used. The author does not often adopt this course, fearing that the undesirable features of closed ether may persist even after the change to an open method has been made.
Another possibility even more widely favoured is to use chloroform as the inducing agent, and only to turn to ether when full anæsthesia is obtained. To this plan the author is strongly opposed. It exposes the patient to the risks of the induction stage of chloroform which are much greater than those of the later stages. Moreover, to develop the full advantages of open-ether, a preliminary hypodermic of morphia is essential, and the[87] drawbacks of chloroform plus morphia are elsewhere mentioned (page 43).
The use of a mixture of chloroform two parts, ether three parts, presents the same disadvantage, but in a degree so much smaller that in powerful or alcoholic patients, the author believes this to be the method of choice (see Chapter xiv.).
Dr Silk has recently suggested another plan. He has sought to make open-ether easy for the non-expert with a view of encouraging the wider use of so valuable a method. For this purpose he advocates the admixture of one part of chloroform in thirty-two of ether (a dram of chloroform in four ounces of ether). This is to be given in exactly the same way as perhalational ether, and will, Silk says, give a type of anæsthesia, and a degree of safety, identical with those of pure ether. The author’s experience with Silk’s mixture is too limited to enable him to offer any opinion upon its merits.
Lastly, there remains the plan of using ether as the main inducing agent, but assisting its action by the intermittent and most guarded addition of small quantities of C2E3 mixture. This is the author’s “stock” method; but in teaching it to students, too much emphasis cannot be laid upon the small quantities of chloroform mixture required or permissible. As a consequence of the perhalational method here advocated, every drop of chloroform which appears on the mask will when volatilised, give a very much higher percentage of CHCL3 vapour in the inspired air, than the same quantity exhibited on the ordinary open chloroform mask. Once the student has grasped this essential fact, ordinary care and intelligence will enable him to guard against a danger which is only existent if unappreciated.
For many of the hints given in this section the author is[88] indebted to Dr W. J. Ferguson of New York, and Dr Hornabrook of Melbourne.
Success in inducing with open-ether is attained only by attention to a number of small details. The student who thinks that some of these are too trifling for his notice is usually the man who informs you that induction by open-ether is impossible, the fact really being that he has not taken the trouble to learn, or has never had proper tuition. The following are the points demanding attention:—
1. Always give a dose of morph-atropine or other narcotic, half to three-quarters of an hour beforehand.
2. See that the patient is comfortable on the table. Prop up his head and shoulders a little with pillows. In powerful subjects Hornabrook tilts the whole table down at the foot-end, for a few degrees.
3. Adhere strictly to perhalation and to the drop method. You will never induce with open-ether if the whole volume of the respired air does not pass through the gauze.
4. Chat to the patient as long as consciousness can possibly persist. Tell him he is doing very well. Don’t shout complicated instructions at him as to how to breathe: it annoys and muddles him.
5. When the gauze ring and the mask are in position, allow one or two drops of ether to fall on the mask, then pause: in a few seconds the mild ether vapour so formed will soothe the upper respiratory tract, and prepare it for the stronger vapours yet to come. This does not waste time—it saves it.
6. When the administration is again begun, attend closely to the rate of dropping. At first not more than one drop in three or four seconds is wanted. The full rate of dropping cannot be attained for at least ninety seconds.
7. Give no mixture for the first ninety seconds; thereafter some five to ten drops every half minute or every twenty seconds[89] according to type of patient. Have the mixture bottle handy so that no time is wasted in changing bottles. Stop the addition of mixture as soon as full anæsthesia is attained.
8. Slip the folded towel over the mask and tuck its base well round the chin and face. Do this only after the first two minutes have elapsed.
9. As soon as the neck muscles are relaxed, turn the patient’s head over to one side, and let the hands assume the position described in Chapter iii. and illustrated in Fig. 28C.
10. The student is warned to discourage the too early attentions of the nurse or house-surgeon. These officials are naturally anxious to “get the patient ready for the Chief” and are apt to start “cleaning up” before the patient has lost all consciousness. A man who is doing his level best to go to sleep, derives neither pleasure nor profit from a wholly unexpected dab of ice-cold methylated spirit upon his umbilicus.
By the use of the method here advocated, induction is singularly easy and successful in good subjects. The struggling stage is either not represented at all, or appears only in the form of the lifting of a limb and a slight occasional pause or catch in respiration. Full anæsthesia is often announced audibly, by the commencement of a gentle “blowing.” Once it is heard, the anæsthetist may rest assured that a workable level of anæsthesia is either present or not far off.
If the above instructions are followed, the amount of ether required is not excessive. Anæsthesia is attained after the use of about 1½ to 2 ounces of ether and one or two drams of mixture. The next forty to fifty minutes demand about another four or five ounces of ether; no mixture at all. Some practice, is required before these small figures are attained. The more practice, the less ether is required.
[90]
In a sense, all forms of ether anæsthesia are vapour methods, but in all the forms so far described, the patient has to vapourise the drug for himself: in a true vapour anæsthesia this is done for him, and the mixture of air and ether vapour propelled towards him. One of the keenest advocates of this method is Dr Gwathmey, of New York. He lays great stress also upon the necessity of warming the vapour, claiming that this measure will prevent the loss of heat to the patient incidental to the warming up in the air passages of the cold vapour usually supplied by other methods; but the results of the laboratory experiments upon which Gwathmey founded his case are inapplicable to the human subject, in that they were performed upon dogs and cats, which lose heat largely from the mouth and air stream. Man is not a hairy animal, and transacts most of his thermolysis through the medium of his skin. None the less, warming the vapour of ether has value since the process removes some of the irritant effects so marked in the case of cold ether vapour.
In 1913, Karl Connell described such an apparatus, which was then in use at the Roosevelt Hospital, New York. The ether was vapourised by dropping it into a warm chamber. Air was pumped into the chamber, and carried the ether vapour in known percentage, and at known pressure as shown by gauges. Such mechanism is ideal, but would certainly be rather costly. Its great value was that it informed us with certainty what proportions of ether in the atmosphere were necessary to induce and maintain anæsthesia (see Appendix II.).
A simple mechanism was brought out shortly afterwards by Dr Shipway, of Guy’s, and is known as Shipway’s warmed Ether.
It consists essentially of the following parts (see Fig. 29):—
[91]
(1) A small hand bellows (B).
(2) An ether bottle, with tube for delivery of air stream dipping deeply into the fluid: the exit tube of course does not dip in. The bottle stands in a metal pan in which water at about 75° Fahr. is to be placed (E).
(3) A thermos flask (W) in which is a metal tube (U). The etherised air passes along this tube, and picks up heat from its walls. The thermos is filled with water at about 180° Fahr.
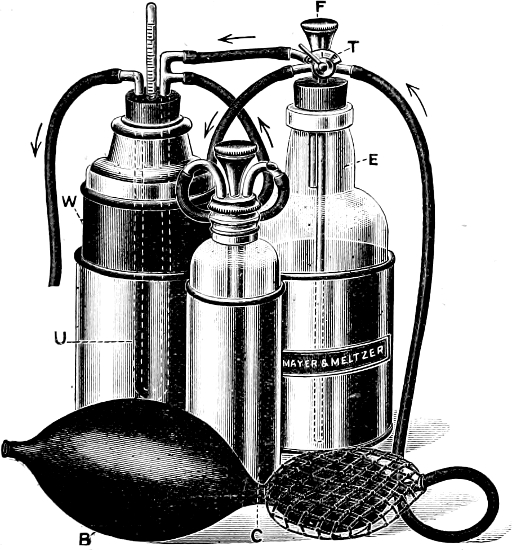
Fig. 29.—Shipway’s warmed ether vapour apparatus.
(4) A mask upon which a towel or gauze is to be stretched: the rubber tube bringing the air and ether is brought through the covering material and delivers the anæsthetic vapour in the region of the mouth.
[92]
(5) Additional to the above, there may be added a small chloroform bottle (C). In specimens of the instrument containing this convenience, there has, of course, to be a regulating tap (T) at the head of the ether bottle, which will divert more or less of the air stream towards the chloroform.
This little machine, somewhat resembling a cruet stand in its appearance was widely used in France. Owing to the kindness of the Edinburgh Red Cross Committee, one was provided for the Base Hospital with which the author proceeded to Salonika, where he used it extensively. The impression of it formed by himself and others was that it was peculiarly easy to maintain with it a steady level of anæsthesia. It had, however, no claim to banish post-anæsthetic bronchitis and pneumonia, of which in spite of much anxious care and thought, a fair number of cases were seen during the winter time (see page 151).
In using the machine, it is necessary to remember that from the physical point of view, one is providing from the machine a small part only of the total volume of air required by the patient.
The bellows are quite small: one squeeze of the hand will not supply more than about the equivalent in volume of one or two fluid ounces. The larger part of the volume required by the patient has to be obtained from the general atmosphere, so that the percentage of ether which may be as high as 25 in the exit tube, will be greatly lowered by the time it reaches the patient’s respiratory tract.
The actual strength of ether breathed by the patient will depend upon:—
1. The force and frequency with which the pump is compressed. (N.B. It is of course useless to pump during expiration).
2. The depth of ether in the bottle.
[93]
3. The temperature of the water bath in which the ether bottle stands. The warm water should only be put in at the last moment before starting, otherwise very strong ether vapour will collect on the surface of the ether, and the first puff of the bulb will expel a highly irritant vapour towards the patient.
With specimens of this machine which have the addition of the chloroform bottle, it is perfectly possible to conduct even the induction stage of anæsthesia; a mere trace of chloroform vapour will be sufficient. It is unnecessary to give detailed instructions for the use of the machine. A preliminary consideration of the above physical facts, together with a little cautious practice, will enable the student rapidly to acquire facility with the method.
For such operations as the removal of jaw or tongue there are obvious advantages in being able to introduce ether vapour to the blood per rectum, since the mouth and air passages are thereby left free for the attention of the surgeon.
Many years ago this was attempted by vapourising ether and propelling the vapour through a tube high up into the rectum. This method was abandoned, as it led to a good deal of inflammatory trouble afterwards. Recently, Dr Gwathmey suggested a new method of utilising the rectal route which has largely overcome this objection.
This consists in passing into the rectum a mixture of olive oil and ether. The bowel is first carefully washed out, and an hour before operation, the patient receives a hypodermic of morphia, gr. ⅙; atropine, gr. ¹⁄₁₂₀. A suppository of chloretone gr. v is also passed into the rectum to act as a local sedative. Half-an-hour later, the patient is put into the left lateral position, a soft catheter[94] attached to a funnel is passed some six inches up the rectum, and the mixture of oil and ether poured into the funnel. It is wise to take at least five minutes to introduce the whole dose.
The following table shows the dosage required:—
| Age of Patient. | Strength of Ether in Mixture. |
Quantity of Mixture required. |
| Under 6 years | 50% | One ounce to each 20 pounds body weight (no preliminary morphia) |
| 6 to 12 years | 55% to 65% | Do. do. |
| 12 to 15 years | Do. | One ounce to each 20 pounds body weight (but use ¹⁄₁₂ gr. morphia) |
| 16 years and upwards |
75% | One ounce to each 20 pounds body weight with ⅙ gr. morphia as a preliminary |
In practice then, for the ordinary adult, one uses eight ounces of the mixture, six ounces of which are pure ether. The oil and ether require to be shaken together, but remain blended long enough for introduction.
In five or ten minutes, the patient begins to feel a rather pleasing numbness and tingling in the lower, and later the upper extremities, and drops quietly to sleep in about twenty minutes. In a large proportion of cases, it is necessary to deepen the anæsthesia by the use of the open mask for a few minutes, but once a deep anæsthesia has been thus obtained, the absorption from the rectum will balance the loss in expiration and maintain a good anæsthesia for three quarters of an hour at least.
On return to bed of the patient, the nurse passes two tubes placed side by side, as high into the rectum as she can; the end of a Higginson syringe is inserted into one of them, and a considerable quantity of soap and water is pumped gently into the bowel,[95] escaping down the second tube. The washing must be continued until all smell of ether is removed. Finally the soapy water itself is washed away by a little saline.
Unless there be some pre-existing local inflammatory disease of the rectum (in which case the method should not be used), there are no unpleasant sequelæ after oil ether. The chief objection to the method is the amount of labour thrown on the nursing staff, which is so considerable as to bar it from adoption as a routine. This should not, however, be allowed to prevent its use in the limited number of cases in which it is strongly indicated. These are:—
(1) Panic-struck cases who cannot face the ordeal of ordinary methods.
(2) Nose, throat, and tongue operations where intratracheal ether is not available.
[96]
Intratracheal insufflation consists in driving a current of air under pressure, through a tube introduced by way of the mouth and larynx, deeply into the trachea. The current of air which is continuous, returns between the tube and the wall of the trachea, and escapes through the mouth and nose.
The work of Meltzer and Auer has demonstrated that this insufflation of air into the trachea under adequate pressure ventilates the pulmonary alveoli, and enables the normal diffusion of gases to be carried out for many hours, independently of all respiratory movements. If the air in its passage under pressure is made to pass through a chamber containing ether, we are enabled to introduce into the pulmonary alveoli, ether vapour of varying strength, and, by this means, to maintain surgical anæsthesia.
The Actual Process of External Respiration consists in the absorption of oxygen from the alveoli into the blood of the lung capillaries, and the elimination of carbon dioxide from the lung capillaries into the alveoli. The oxygen has to be brought from the outside to the alveoli, and the carbon dioxide has to be conducted from the alveoli to the outside. Between the outside and the alveoli is the long airshaft, consisting of mouth and nose, pharynx, larynx, trachea, bronchi and bronchioles. In natural respiration the conduction of oxygen inwards, and of carbon[97] dioxide outwards, is carried through by a complicated pumping mechanism. In ordinary inhalation anæsthesia, this mechanism is entrusted with the task of introducing ether vapour into the alveoli.
In intratracheal insufflation the work of this natural pumping apparatus is taken over by an artificial mechanism. In considering the justification for this, the following points are to be noted:—
(1) The patient is unconscious—not naturally so as in sleep—but unnaturally as the result of drugs; there is therefore a probability that the elaborate natural mechanism may not work smoothly—especially is there a danger that the free airway may be interfered with. Intratracheal insufflation obviates this danger.
(2) By means of the artificial mechanism, air is brought with some force to the mouth of the bronchi, and thus a more rapid and more powerful diffusion of gases takes place.
(3) The mechanism ensures the maintenance of a current of air blowing forcefully from the trachea and larynx through the pharynx, mouth and nose. This re-current continuous air-stream effectively prevents the entrance of blood or any infectious material into the bronchi and air cells, and thus the danger of septic lung troubles is obviated.
(4) In certain intrathoracic operations the normal respiratory mechanism is deliberately interfered with. Intratracheal insufflation by the constant maintenance of sufficient positive pressure, prevents or regulates the collapse of the lung which occurs when the thorax is opened, and thus obviates the necessity for the somewhat elaborate positive and negative pressure cabinets and masks which had been devised for intrathoracic operations.
(5) Incidentally it may be noted that intratracheal insufflation of air provides us with an excellent means for performing[98] artificial respiration. Many instances have now been recorded of its utility in this respect. Dr Elsberg records the case of a patient who had taken morphia with suicidal intent, on whom artificial respiration by this method was kept up for 12 hours, without any respiratory movements taking place, recovery ultimately ensuing.
This consists of (see Fig. 30):—
1. Instrument for producing air current (A).
2. Ether chamber and various regulating taps (B).
3. Device for warming vapour (C).
4. Safety valve (D).
5. Manometer (E).
6. Intratracheal catheter, with rubber tubing linking up the various parts of the apparatus (H).
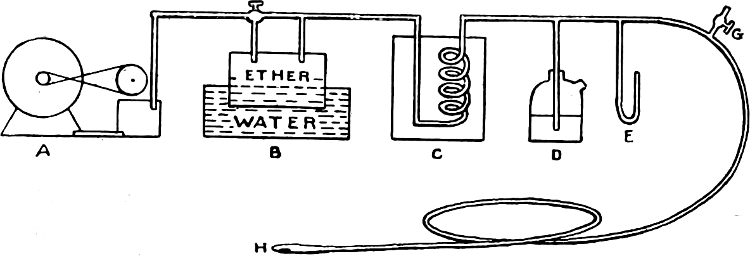
Fig. 30. Diagram of intratracheal apparatus.
1. The Air Current is obtained either by means of an ordinary glass-blower’s foot bellows, or an electric motor may actuate a rotatory blower which produces a current of air. The blower may be made to rotate at a speed varying from 50 to 1000 revolutions per minute (see Fig. 31).
The foot bellows is simple and inexpensive, and there is no reason why it should not be efficient. The electrically rotated blower is more efficient, ensures a smoother air current, and saves much labour.
[99]
2. The Ether Chamber.—Ether vapour may be produced by either of two methods. Fig. 32 shows Kelly’s instrument where air is blown over the surface of a considerable quantity of liquid ether. Dr Meltzer[5] maintains that the effectiveness of the etherization is proportional to the diameter of the ether bottle. In this connection it may be well to recall certain points pertinent to the subject of etherization. A satisfactory etherization depends on the establishment in the blood and tissues of an ether tension of definite strength. Boothby[6] states that this tension should correspond to about 15 per cent. of ether vapour in the alveolar cells. “If when this tension has been established, less than 15 per cent. ether vapour is administered, outward diffusion occurs from the tissues and blood to the air and the anæsthesia becomes lighter.”
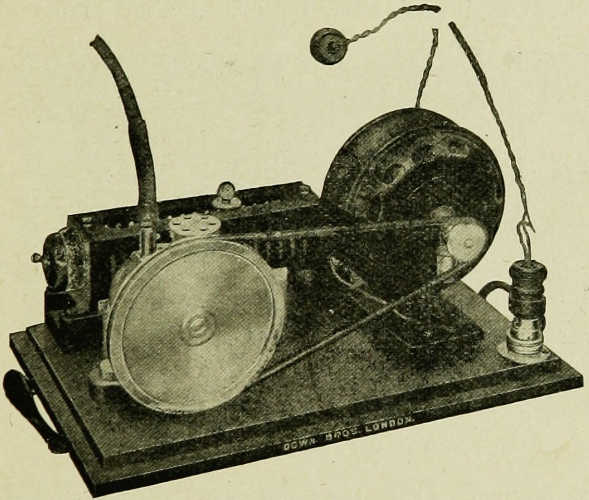
Fig. 31.—Electric blower to supply current of air for intratracheal anæsthesia.
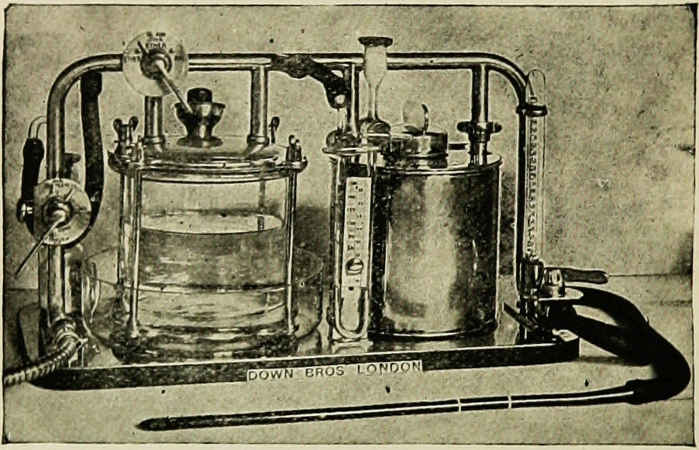
Fig. 32. Kelly’s intratracheal apparatus.
[100]
In an apparatus such as we are describing the strength of the ether vapour depends on and is influenced by a variety of factors, among which the following may be specially noted:—
(a) The diameter of the ether chamber.—The larger the diameter the stronger will be the ether vapour. The chamber is generally kept two-thirds full: the less the empty space in the chamber the stronger will be the vapour.
(b) The rapidity of the air-current.—The larger the amount of air passing over the ether the more rapid will be the vapouration, with the result that the temperature of the liquid ether will rapidly fall and the strength of the ether vapour in the air will be correspondingly lowered.
(c) The temperature of the liquid ether.—The higher the temperature of the liquid ether the stronger will be the percentage of ether vapour in the air. If the ether chamber is placed in a bath of water which is maintained steadily at an adequate temperature and if the rate of the air flow remains constant, a constant strength of ether vapour will be given off. It is well in this connection to remember that the[101] boiling point of ether is low and that a very high percentage of ether vapour is readily obtained if the temperature in the water bath is allowed to rise beyond 80°F. For further information regarding ether percentages see Appendix I and II.
Such an instrument as Kelly’s requires at its head a regulating tap, movement of which is capable of diverting part of the air stream direct to the patient without coming in contact with the surface of the ether. In this way the maximum strength of vapour may be diluted as and when required.
In Fig. 33 is shown Shipway’s instrument. Here the drug is dripped into a chamber, the floor of which is kept warm. The ether volatilises at once and the vapour is carried away by the air stream passing through the chamber. The strength of ether vapour in this instrument is regulated solely by the rate of drip which is in complete control of the administrator.
Whichever method of making ether vapour is utilised the instrument should be capable of producing a maximum at least of 15 per cent. to 18 per cent., and means must be provided to reduce this percentage at will.
3. Device for Warming Vapour.—It is doubtful if the warming of inspired or insufflated vapour has any appreciable influence on the body temperature, but there is a fairly general consensus of opinion that if the ether vapour is warmed there is less likelihood of irritation of the respiratory mucous membrane. It is to be noted, moreover, that in intratracheal insufflation the natural apparatus for warming the inspired air is put out of action. This warming can be effected by the simple device of carrying the tube through a chamber of hot water after it emerges from the ether chamber.
4. Safety Valve.—Dr Meltzer insists very strongly on the necessity of having a safety valve capable of controlling the maximum pressure under which the air may enter into the[102] intratracheal tube. By a simple device, any excess of desired pressure will cause the air to bubble through mercury and thus never reach the lungs. In this way any possibility of accident from undue intrapulmonary pressure is obviated.
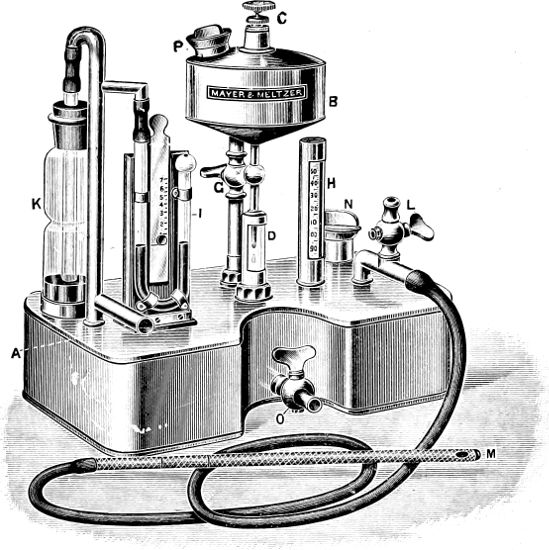
Fig. 33.—Shipway’s intratracheal apparatus.
5. Mercury Manometer to indicate the pressure in the tube in m.m. of mercury. It has been experimentally established[7] “that the pressure in the trachea and in the bronchi is only a small fraction of the pressure in the manometer outside of the body, and that the intratracheal pressure grows[103] considerably less with the decrease of the diameter of the intratracheal tube.”
6. Intratracheal Catheter.—It is essential to have an instrument of adequate rigidity which can be satisfactorily sterilized. The ordinary coudé catheters, or the silk web white enamelled cylindrical catheters, are suitable. The size should be selected from a range of 18 to 25 French. It is preferable to err rather on the side of a small than a large tube. An ordinary adult will require a tube of about size 22 to 24, a plethoric alcoholic, on the other hand, might need a 25.
A tube of too large a calibre interferes with the free return of air and spontaneous respiration soon becomes too slow. Expiration is prolonged, active, and laboured, and after a few minutes, respiratory movements may cease entirely. The only way to meet such a situation is to withdraw the tube and insert a smaller one.
Technique of Administration.—It is advisable in adults to administer about three quarters of an hour before the operation, a hypodermic injection of morphia (gr. ⅙) and atropine (gr. ¹⁄₁₀₀), or of scopolamine (gr. ¹⁄₁₀₀) and morphia (gr. ⅙). The latter combination is more efficacious in alcoholic subjects. In children, atropine alone should be given.
It is to be remembered that intratracheal insufflation of ether is a method of maintaining not of inducing anæsthesia. Induction is carried out in the ordinary way. When this has been done, the catheter is passed.
The introduction of the catheter does present some difficulty, but this is largely overcome as skill and confidence are acquired with practice. It may be carried out indirectly, or a view of the glottis may be obtained by the aid of such an endoscope as Hill’s, and the catheter inserted between the cords. The latter method is probably the more satisfactory, but it is well to acquire the[104] skill to pass the catheter indirectly as in a certain small proportion of cases there are obstacles to the use of the endoscope.
To facilitate catherization the pharynx and epiglottic region may be cocainized with a 5 per cent. solution before induction. Hill’s endoscope (Fig. 34) is distally illuminated by a small electric lamp, which is connected with a small pocket battery. A useful modification of this has been devised by Mr Dott. In it, the catheter is passed along a separate compartment, so that the view of the glottis is undisturbed. The point of the catheter comes into view at the distal extremity of the endoscope and can be guided between the cords into the trachea.
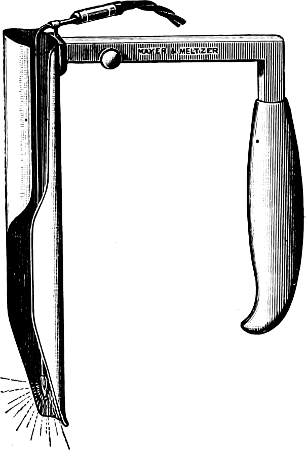
Fig. 34.—Hill’s Direct Laryngoscope.
It is essential before attempting intubation, that there should be thorough relaxation. The lower jaw should be so slack that a gag is not required. The head is then placed in the occipito-shoulder position, or is allowed to hang over the end of the table. The tongue is controlled by forceps, and the endoscope passed slowly along its dorsum until the epiglottis comes into view. The point of the endoscope is then passed sufficiently far below the tip of the epiglottis to ensure that it will not slip; too deep insertion must be avoided. The endoscope being held in the left hand, the hyoid bone is lifted up by a tilting movement of the hand. The glottis is thus brought into view. The catheter stiffened by[105] means of a probe is then passed through the glottis into the trachea and the endoscope withdrawn. The bifurcation of the trachea in the adult is at a distance of about 26 cm. from the incisor teeth. The catheter should be marked accordingly, and inserted to a point just short of this. The probe is then withdrawn, and connection made with the air current.
It occasionally happens that unexpected difficulty is met with on attempting to pass the catheter by direct vision. The larynx may be so fixed that the glottis does not readily come into view; or in the case of an intraoral neoplasm the view may be obstructed by the presence of blood. In such cases the catheter can be introduced by the indirect method. The middle finger of the left hand is passed along the dorsum of the tongue until the epiglottis is felt. The index finger is then used to guide the point of the catheter to the glottis through which it is then passed. No undue force must be used. A stilette should be inserted into the catheter which should be moulded almost to a right angle at its terminal third. If the stilette is withdrawn when the point of the catheter is over the mouth of the glottis, the instrument will, as a rule, slip easily into the trachea.
Occasionally the tube passes into the œsophagus. With care and adequate relaxation such a mistake should not occur, but the possibility of it should be kept in mind. If the operator will abstain from attempting to pass the catheter until such time as he has a satisfactory view of the glottis, mistakes of this kind will seldom occur. The essentials are a good illumination and an adequate relaxation.
Mild glottic spasm may supervene on the passage of the catheter but this rapidly passes off. At first the degree of concentration of the vapour should be low or irritation will result, evidenced by spasm and coughing. The strength of the vapour is gradually increased until the necessary concentration is attained. The pressure should vary according to the requirements of the[106] case and should range between 10 mm. to 25 mm. Hg. The safety valve must be set so as to make any pressure above this impossible.
In the majority of cases the course of anæsthesia is smooth and uneventful; the colour remains a rosy pink, the pulse is good, and the respirations quiet and regular. It is undesirable that the respiratory movements should be abolished altogether; their presence indicates that neither the central nor the peripheral respiratory mechanism is being overdosed with ether.
Theoretically, the constant plus-pressure in the lungs might be thought to interfere with the circulation in the large veins, and in the pulmonary vessels themselves. It is therefore well to reduce the pressure in the catheter to zero every minute by opening the tap provided for the purpose for a second or two.
At the conclusion of the operation, before withdrawing the catheter it is well to flush out the lungs with air so as to remove any ether vapour that is present. In a certain number of cases, notably in big alcoholic subjects, difficulty may be experienced in securing a sufficiently deep anæsthesia with good relaxation. It is seldom, however, that patience and the careful introduction of a stronger vapour will not suffice to overcome this. In alcoholic subjects, as previously suggested, preliminary medication with scopolamine and morphia will help. It really becomes a question, if one may put it so, of coaxing the unconscious patient to tolerate an ether vapour of adequate strength.
The general opinion of anæsthetists appears strongly to favour the view that the absence of strain and the perfect æration in intratracheal ether insufflation tend to lessen the shock of operation. The post-operative history of patients also suggests that there is a lessened liability to pulmonary complications as compared[107] with cases in which ether has been administered by other methods. Dr Elsberg[8] of New York in this connection writes: “The absence of any pulmonary complications has led us to use this method of anæsthesia in all patients in whom pulmonary complications were to be feared after an anæsthesia or operation. Thus on all asthmatics, in patients with chronic bronchitis and emphysema, in patients who require gastric resection and the like, we no longer, during two years, have seen the much dreaded post-operative pneumonia wherever intratracheal anæsthesia was used.”
In addition, there is ample evidence[9] that the introduction of a catheter into the trachea and its presence therein does not tend, as might have been expected, to set up any irritation at the time or predispose to subsequent trouble. Apart from these general considerations, which suggest the advantage of a somewhat extended use of intratracheal ether insufflation, the method has obvious advantages in all operations about the mouth, such as those for excision of the upper jaw, those undertaken for the removal of nasopharyngeal growths and various plastic operations involving the nasal and buccal cavities. In such cases the danger of aspiration of blood, mucus, etc., is obviated and the anæsthetist is well out of the surgeon’s way, while at the same time an even interrupted delivery of ether vapour is effected. In operations for removal of glands in the neck the surgeon has the field to himself, and is not hampered nor is his asepsis endangered by the proximity of the anæsthetist’s mask.
In such operations as laminectomy and nephrectomy the postural difficulties with which the anæsthetist has to contend, and which also tend to interfere with free respiration, are eliminated.
[108]
The great advantage of the method in intrathoracic operations has already been referred to.
The introduction of intratracheal insufflation of ether was rendered possible by the pioneer work of Drs Elsberg, Meltzer, and Auer. The writer would like to acknowledge his indebtedness to their writings, of which he has made free use.
[109]
Chloroform is chemically trichlor-methane, CHCL3. It is a colourless, transparent fluid, with a specific gravity of 1·491 at 17°C. Its vapour is even heavier than that of ether, approximately four times heavier than air. It is not inflammable, but the action of an open fire or naked flame tends to break it up into hydrochloric acid and phosgene, both of which are highly irritant gases to all who breathe them. The patient suffers, but since all the other occupants of the theatre are also affected, warning is given before serious harm has been inflicted.
Chemically pure chloroform is a somewhat unstable product, but the addition invariably made to it by the producers, of a trace of alcohol, prevents any serious risk of decomposition in bulk. It should be neutral in reaction and have an agreeable non-irritating odour: departure from the normal in either respect indicates the possibility of the presence of acids or aldehydes, and the necessity for referring a specimen to the laboratory.
Like ether, chloroform may be obtained from pure ethyl alcohol or from methylated spirits, and the remarks made in the chapter upon ether apply to the case of chloroform also. A third source of supply is acetone, from which perfectly good chloroform can be produced.
Chloroform is an irritant to the skin and mucous membranes. A drop left on the skin and covered over with impermeable[110] material will produce a deep and painful blister. A drop falling into the eye, if not instantly washed away, produces a very powerful inflammatory reaction, and many eyes have been totally lost from carelessness in this respect. Such incidents are of course actionable, and heavy damages may be given.
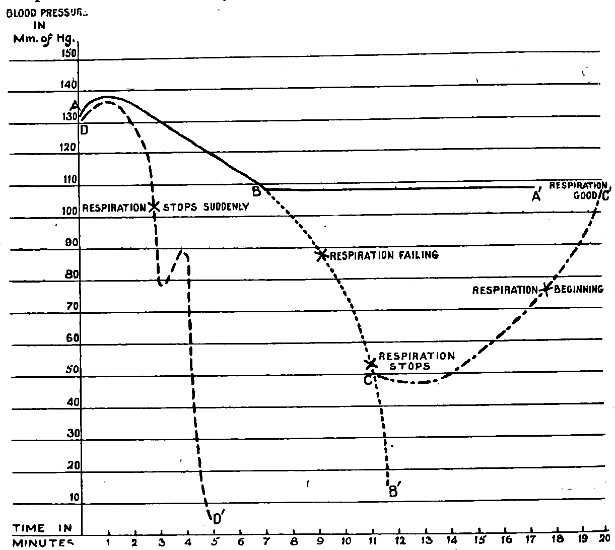
Fig. 35.—Diagrammatic representation of various blood pressure curves obtainable with chloroform.
Line ABA′ represents curve desired in normal chloroform administration.
Line ABCB′ represents gradual overdosage.
Line ABCC′ represents recovery by inversion.
DD′ represents syncope from vagal inhibition: in its course, one attempt of the heart to “escape” is shown.
The special peculiarities of the action of chloroform upon the nervous system have already been emphasised in the account[111] given of the physiology of ether (see page 75). Its action upon the circulatory and respiratory systems has been the subject of many researches, and of much embittered controversy. The literature is therefore very extensive, and the account of it must be severely condensed. The following may be taken as a brief resumé of present day opinion (see Fig. 35):—
(1) In every case of chloroform administration, there is a fall of blood pressure.
(2) If the drug be presented in weak concentration (less than 2 per cent. vapour strength), the fall is gradual and even (line AB).
(3) If the same strength (say 2 per cent.) of vapour as produced the above effect be prolonged unduly, the respiration will cease at a time when blood pressure is still well above zero (line ABCB′).
(4) The fall of pressure is due to diminished force of cardiac action, and at a later stage also to vaso-motor paresis.
(5) The cessation of respiration is due partly to fall of blood pressure in the vessels supplying the medullary centre; partly to gradual poisoning of the centre itself by the drug. That the fall of B.P. in the cerebral vessels is in itself one explanation of the cessation of respiration, was proved many years ago by Leonard Hill in his inversion experiments. Just at the stage when respiration had ceased, the anæsthetic was withdrawn, and the animal inverted into the head-down position. The B.P. in the carotid at once began to rise, and natural respiration was resumed (line A′BCC′).
The above conclusions refer to chloroform given in moderate vapour strength; other effects are produced if higher percentages are administered:—
[112]
(6) With high concentration of chloroform vapour, the fall of blood pressure is rapid, and is apt to become suddenly precipitous (line DD′).
(7) The cause of these sudden falls is inhibition of the heart by over-activity of the vagus: cutting the vagi always terminates the effect unless delayed so long that the animal is dead: in an animal fully under atropine, these vagal actions cannot be produced.
(8) If the heart is inhibited by vagal action, the respiration ceases at once, usually after one deep inspiratory sigh.
(9) An inhibited heart may “escape” from vagal action before the animal is dead: frequently, however, the inhibition persists and the animal dies.
(10) Struggling and breath-holding in the early stages of induction cause sudden falls of blood pressure. Many observers believe that these falls also are due to vagal activity, others hotly deny this. All are united in believing that to press chloroform upon a patient who is struggling and holding the breath, is fraught with grave risk of causing sudden syncope.
(11) The abnormal irritability of the vagus above referred to is a feature mainly of the induction stage, disappearing once full anæsthesia is developed.
(12) It is an undoubted clinical fact that there is a risk of sudden arrest of heart’s action if the operation is begun before the stage of full anæsthesia is reached. A reasonable explanation of such accidents is furnished by supposing a reflex inhibition acting through the vagal centre already rendered hyper-sensitive by partial chloroformisation.
This worker has demonstrated in animals that the heart is sometimes thrown by chloroform into the condition of fibrillation—a delirium of the cardiac muscle, from which recovery is rare. It[113] occurs in the early stage, before full anæsthesia has been reached, and is predisposed to by the infliction of trauma. The practical outcome of this is that the induction stage of chloroform should not be unduly prolonged, and that the operation should not be begun until the third stage is fully developed.
So far as the author understands the views of Dr Levy, his explanation of chloroform syncope need not be taken as introducing any new principle into the administration of the drug. Even those who lay most emphasis upon the danger of using vapours of too high a percentage strength would admit the force of Levy’s contentions. As usual, safety lies in steering between two extremes.
During his work on this subject, Levy further demonstrated that the introduction into the circulation of adrenalin during incomplete chloroform anæsthesia was very liable to induce fatal cardiac fibrillation. He thus furnished the explanation of a number of deaths which had occurred in the practice of nose and throat specialists. Since the publication of Levy’s work, the rule has been absolute that if adrenalin is to be used in a case requiring chloroform anæsthesia, the adrenalin must precede, not follow the anæsthetic.
Basing upon these views as to the action of chloroform, and upon the lessons of practical experience, we may formulate definite rules for giving the drug.
(1) Give chloroform evenly, not spasmodically.
(2) Increase the vapour strength of chloroform gradually from zero until 2 per cent. or at most 2½ per cent. is reached at the end of two or three minutes; maintain that strength until full anæsthesia is obtained; thereafter, drop down to 1–1·5 per cent. This will result in a B.P. curve corresponding to the line ABA′ in the diagram (Fig. 35).
[114]
(3) Be guided chiefly by the patient’s respiration. Chloroform kills by stopping the heart, but in the immense preponderance of cases, evidence of failure of respiration appears in ample time to give warning of approaching circulatory failure. The eye reflexes give confirmatory evidence of the depth of anæsthesia, but the superlatively important thing is to maintain a free airway, and be sure the patient is using it.
(4) If serious struggling and breath-holding occur, withdraw the anæsthetic until the patient “resumes normal.”
The logical application of such general principles would be to use an instrument which gives a definite and known percentage of chloroform, variable at the wish of the administrator. Many such machines have been brought forward, and while none of them have obtained general acceptance, a description of the best known instrument will be given, as the reader may as a house-surgeon meet with it, and with a surgeon who wishes it to be used.
In principle, this is a “draw-over” instrument; the patient’s own inspirations are the motive power. Passing over the surface of the fluid drug, the inspired air picks up from it a known percentage of vapour. The other system available for the construction of percentage chloroform instruments is the “plenum”; in this the vapour is propelled to the patient by a pump.
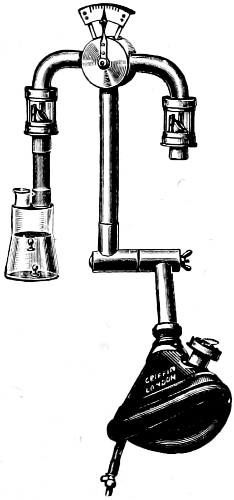
Fig. 36.—Vernon Harcourt’s Percentage Chloroform Inhaler.
In appearance, the inhaler resembles the letter T, with a rubber face-piece attached to the lower end of the vertical limb (see Fig. 36). The T portion itself is made of metal tubing of a definite size in cross section. One end of the horizontal limb admits pure air, the other, air which has passed over chloroform and picked up from it a certain proportion of vapour. The proportion of the total inspired volume of air which passes through each of the ends is[115] regulated by a lever seen at the junction of horizontal and vertical limbs, and the exact percentage of chloroform being inhaled is indicated by a series of numerals marked on the dial over which the lever moves. These figures are correct provided:—
(1) The chloroform receptacle is not shaken (this would greatly increase the percentage).
(2) The temperature of the chloroform is not allowed to fall below 13° centigrade. To ensure that this cannot take place without the knowledge of the administrator, two coloured beads are thrown into the chloroform. At the desired temperature of the chloroform (13°-15°C) the blue bead sinks to the bottom, the red one nearly to the bottom. Below 13°C, the red bead also touches bottom, and when this is observed, the chloroform vial is warmed up in the palm of[116] the hand. At the point 15°C, both beads float, and the warming must then stop, or an undesirable addition to the vapour strength yielded will occur.
The face-piece is made of rubber, and must be closely adapted to the face; in its side is seen the expiratory valve. Inspiratory valves are present at each end of the horizontal limb.
The great advantage of this instrument, to the author’s mind, is for teaching or demonstration purposes. If the student sees the lever gradually being moved over from ·2 to 2 per cent., then slipped back to about 1·5 per cent. after full anæsthesia has been obtained, he begins to appreciate what it is he is aiming at when giving chloroform by the ordinary open method.
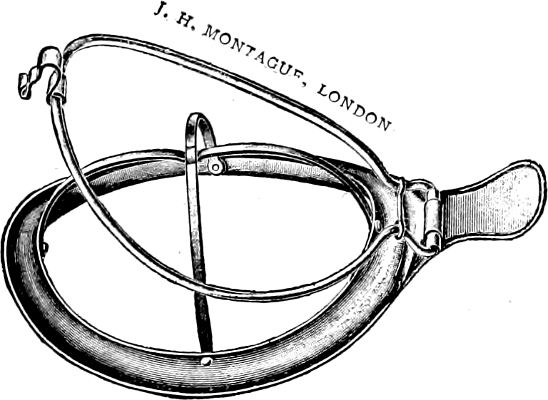
Fig. 37.—Schimmelbushch’s mask.
The appliances requisite are:—
(1) A mask. Schimmelbushch’s is the best known (Fig. 37): as elsewhere explained, it does not accurately fit the face.
(2) Material to stretch on the mask. The best is two layers of domette or one of flannelette: surgical gauze is so[117] light that heavy drops of chloroform are apt to “spark” through it and burn the skin of the face: lint rapidly becomes sodden; the drug drips away from its edge instead of vapourising properly.
(3) A good drop bottle, of which many varieties are marketted (Fig. 38): it is essential that it should be capable of producing definite drops: the old method of intermittent “douching” of chloroform is to be condemned as violating the first general principle for giving the drug.
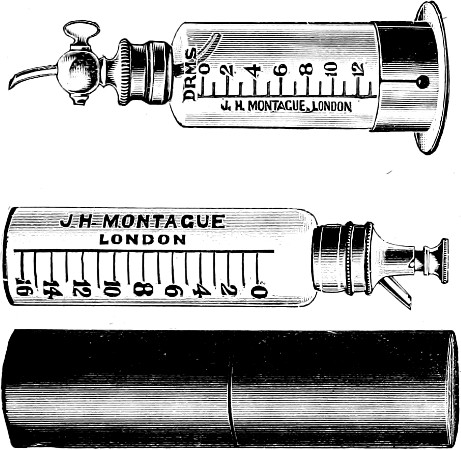
Fig. 38.—Chloroform drop bottles.
It is not possible by the open method to be mathematically accurate with percentages, but the necessary appliances are simple, easily transported, and practically always at hand. If the student learns to use it, and while doing so to think in percentages, he will achieve as good results as or better than he will with percentage[118] instruments. While he may not have in front of his eyes a dial which shows the percentage graphically, observation of the patient will inform him whether the percentage being given should be maintained, raised, or lowered. The only remaining point for him to realise, then, is how in practice such regulations of percentage strength can be achieved by the open method. The strength of the vapour will depend upon three factors:—
(1) Nature of the material used on the mask.
(2) Closeness with which the mask is adapted to the face.
(3) Amount of chloroform exhibited on the mask.
To ensure uniformity of result, two of these factors should be kept constant, and the necessary increase or decrease of vapour strength achieved by varying the third. Always use the same type and thickness of material on the mask, and allow the mask to lie lightly on the face. If the amount of chloroform is then regulated by a strictly “drop” method, results of great uniformity may be obtained by the open method.
This instrument was originally introduced as an attempt to achieve a percentage method. Air is pumped through a certain depth of chloroform contained in a bottle, and the vapour brought to the patient in the face-piece shown in Fig. 39. The calculations by which it was sought to establish this as a reliable dosimetric or percentage method are of no great value. From that standpoint the instrument has not achieved success. It delivers to the patient a small quantity of high percentage vapour which is diluted by a much larger quantity of air inspired by the patient from the general atmosphere, and the final percentage inhaled by the patient is therefore no more accurately known to the administrator than in the open method.
The instrument is, however, of considerable value for tongue and jaw cases, where anæsthesia has to be maintained for some[119] considerable time after the mask with which anæsthesia has been induced has had to be removed, to give access to the surgeon.
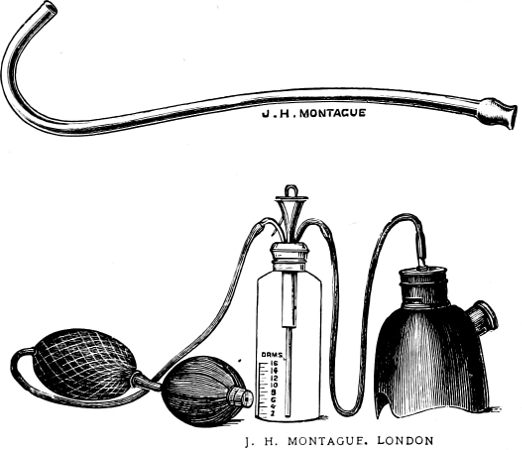
Fig. 39.—Junker’s Chloroform Inhaler showing hand bellows, bottle and mask. Alternatively to the latter, the nasal tube shown above, may be used.
The Figure 39 shows the instrument as usually marketed. It consists of:—
(1) A hand-bellows.
(2) Chloroform bottle. A mark cut on this shows the level to which it is to be filled: if more than the proper quantity be poured in, droplets of fluid chloroform are apt to be blown along the exit tube, with dangerous results.
For convenience and neatness, it is usual to make the exit surround the inlet tube. The entering air bubbles through the chloroform, and a stream of air and chloroform vapour passes out[120] from the exit tube.[10] It is unnecessary to give a detailed account of the use of the instrument, but the student must remember the following points:—
(1) The amount of chloroform vapourised will depend on the vigour of the pumping, the depth of fluid, and the temperature of the chloroform. In order to achieve uniform results, it is therefore necessary to keep up a steady but not excessive pumping, to warm up the bottle occasionally by holding it in the palm of a disengaged hand, and to watch that the level of the chloroform does not fall too low.
(2) The pumping should be timed to synchronise with inspiration: a puff of vapour delivered during an expiration will be wasted.
The light portable appliances which are alone necessary for chloroform anæsthesia, the comparative cheapness of the method, and the apparent ease with which its administration may be conducted, are all great temptations to its use. Those who feel the temptation strong upon them are advised to remember the following quotation from the writings of Professor Leonard Hill:—
“Chloroform is a drug used by the young anæsthetist with the utmost hardihood, and until he has had the misfortune in his practice to meet with a death caused by it, he derides the danger of the drug, and asserts that its safety merely depends on the care and skill of the administrator. After losing his patient, he falls to descanting on the unavoidable dangers of the drug, dangers which he is now the first to maintain cannot be met by any degree of skill in administration.”
[121]
The most distressing and probably the most common chloroform fatalities are exemplified in administration given for the most trifling conditions, such as opening abscesses or extracting teeth.
In general, we use chloroform if for any reason ether is not applicable. For examples of cases of this description, the reader is referred to the chapter upon the choice of anæsthetics.
[122]
Chemically this drug has the formula C2H5Cl. It is a colourless fluid so volatile that it boils at ordinary room temperature. Its vapour is highly explosive, and the fluid itself very inflammable. The drug is supplied by the makers in small tubes with a metal end which can be opened by pressing a little lever (see Fig. 40), varying in type with the brands made by various makers. Two brands are sold by each firm; one is chemically pure, intended for use as a general anæsthetic; the other is not so pure, and is only sold for local anæsthesia. Such a product is not suitable for inhalation.

Fig. 40.—Tube of Ethyl Chloride.
The special points in the physiology of ethyl chloride may be briefly summarised as follows:—
1. After a trifling preliminary rise, the effect of the drug is to lower the blood pressure appreciably. In the human adult subject, this fall becomes appreciable when more than 3 c.c. have been given; if the dose exceed 5 c.c. a fall of 30 to 40 mm. of Hg. is probable,—occurring as it does within a period of perhaps twenty or thirty seconds, such a fall cannot be regarded as safe.
[123]
2. The cause of this fall is diminished cardiac output from weakening of heart muscle. The vagus though not paralysed, does not appear to be unduly irritable, as it does with chloroform.
3. The respiratory centre is at first perceptibly stimulated, and respiration is therefore deeper and quicker than normal. The stimulant effect rapidly passes away and gives place to a stage of depression.
In the majority of cases, death appears to take place from paralysis of the respiratory centre, the heart still showing a little power of contraction after respiration has ceased. There is therefore a fair prospect of recovery if artificial respiration be resorted to promptly.
The extreme volatility of the drug has discouraged most anæsthetists from giving it upon an open mask. Hornabrook, of Melbourne, advocates this system, however. His mask fits the face accurately, and his whole method is strictly perhalational. He uses some 4–6 c.c. of the drug for a child, 6–8 c.c. for an adult, and achieves his anæsthesia in a minute to a minute and a half. He also advocates open ethyl chloride as a preliminary to open ether. For some twelve months, the author adopted the method. At the end of that time he came to the conclusion that while it greatly facilitated the induction stage of open ether, it appeared to increase the after sickness. He therefore abandoned it, though rather reluctantly.
This is the usual means employed. A variety of inhalers have been produced on the market, one of which is shown in Fig. 41. Essentially all consist of:—
(a) A face-piece which must fit the face with reasonable accuracy.
(b) A one-gallon rubber bag attached to the mask by a T-piece.
[124]
(c) A glass vial, with numerals from 1 to 5 marked on the outside to facilitate the measurement of the drug in c.c. Into this the drug is squirted from the makers’ tube. The vial is attached to the T-piece (or alternatively the bottom of the bag) by a rubber tube.
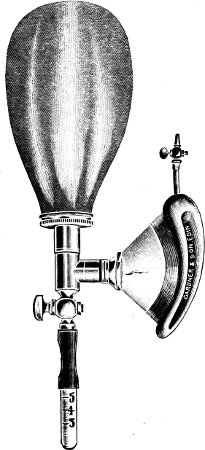
Fig. 41.—Ethyl Chloride Inhaler.
To use such an inhaler, the glass vial is first detached from the rubber tube, and the chosen dose of drug squirted into it. A[125] child of five or six will require 3 c.c., an adult up to 5 c.c.; this dose should never be exceeded. The vial is then rapidly reconnected with the inhaler. The face-piece is adapted to the face, care being first taken to place between the teeth a mouth prop or a gag. This enables one to get immediate access to the mouth when the inhaler is removed. The patient is then told to breathe deeply once or twice. During the inspiration the mask is lifted slightly, and the ensuing expiration is then caught in the bag by pressing down the mask on to the face. To volatilise the drug there are two alternative methods. In the one, part or the whole of the dose is tipped into the rubber bag by elevating the vial. A far better is the “Vapour” method, almost universally used in Edinburgh owing to the advocacy of Dr Logan Turner. A tumbler is filled with hot water, and the bottom of the glass vial is allowed first to touch, and after a few seconds to be immersed in it. Some thirty to forty seconds suffice to vapourise the whole of the dose.
Ethyl chloride given by itself should always be administered to a patient in the recumbent position. A dose sufficient to produce anæsthesia without the aid of nitrous oxide or ether will not be safe in the erect posture. The case is quite different where a small dose only is given, to assist the action of nitrous oxide, or facilitate the induction stage of ether.
Ethyl chloride is very rapid in its action, some sixty seconds availing to produce quite a deep anæsthesia. Respiration is at first deepened and quickened: as full anæsthesia is attained it remains rather deeper than normal, and is accompanied usually by light snoring. The colour should remain perfectly good: the pupils show marked dilatation, the corneal reflex is abolished, and good muscular relaxation is attained.
With no anæsthetic is it so essential as with this, to become[126] acquainted with the type of respiration normally to be expected, and to watch for any departure therefrom with cat-like vigilance. The other danger signal is the pupil. It should be dilated, but a rim of iris should still be perceptible.
Once anæsthesia is established, the inhaler should be removed, and the surgeon may begin his work. He will have for its completion some 80–90 seconds against the 40–50 available after nitrous oxide. With ethyl chloride there is a somewhat prolonged “analgesic” stage. The patient is partly conscious and may even be phonating, but seems unconscious of the infliction of pain unless very severe measures are being used.
When first introduced, it was expected by enthusiasts that the lightness and portability of the drug itself and of the necessary inhaler, would enable ethyl chloride to oust nitrous oxide from its recognised place in surgery and dentistry. These high expectations have for several reasons not been fulfilled. In the first place, this drug is essentially a “single dose” anæsthetic. Most authorities view coldly all attempts to prolong anæsthesia by repeated or continued administration. Secondly, ethyl chloride has a mortality rate very much greater than nitrous oxide if doses sufficient in themselves to produce anæsthesia are habitually used (vide supra). The introduction of the “vapour” method has done much to mitigate the risks, but even then, this anæsthetic cannot approach the high level of safety rightly credited to N2O. Moreover, it leads to after vomiting much more commonly than its rival.
In many schools these considerations have been held so powerful that ethyl chloride has been entirely abandoned. It is, however, a very valuable drug for the following purposes:—
(1) The removal of tonsils and adenoids. For this operation, the speed with which the patient (usually a child) loses consciousness, the pleasant type of anæsthesia and[127] absence of all serious asphyxial phenomena, and the rapid re-appearance of the cough reflex when once the inhaler is removed, are all strong recommendations.
(2) As an adjuvant to gas, or gas oxygen (see Chapter XIII.).
(3) As a help to the speedy and comfortable induction of “closed ether” (see Chapter XV.).
[128]
Dr Guy, Dean of the Edinburgh Dental School, introduced some years ago a method of giving ethyl chloride in mixture with nitrous oxide. Guy’s objective was to utilise the many excellent features of the drug without incurring the risks which are apparently inherent in it when a dose sufficient in itself to induce full narcosis is used. Given in mixture with gas, a much smaller dose suffices.

Fig. 42.—Guy’s inhaler for N2O and Ethyl Chloride.
His original apparatus is shown in Fig. 42, the details are shown in Fig. 43. The horizontal limb of a 3-way gas tap is prolonged half an inch. In each side of the prolongation is a hole. The bag mount has in its side also one hole, which is connected by a universal ball and socket joint, with the rubber tube to which the ethyl chloride vial is attached. An indicator on the outside of the bag mount and a mark upon the outside of the horizontal limb of the 3-way tap, serve by their apposition or the reverse to show whether the ethyl chloride vial is in direct continuity with the interior[129] of the inhaler. For purposes of description, Dr Guy calls these two positions, “in register” and “out of register.”
To use the instrument, the ethyl chloride vial is removed, and the side pipe attached to a cylinder of nitrous oxide. The indicator of the 3-way tap is put at “air” and the bag mount “in register.” The bag is then filled with gas by opening the head of the cylinder. The bag mount is now put “out of register,” and the side tube disconnected with the cylinder. The bag, being closed, remains full of gas.

Fig. 43.—Guy’s Instrument for Gas and Ethyl Chloride. Details of valve piece and bag mount, showing side tube for attachment of Ethyl Chloride vial.
A suitable dose of ethyl chloride is now squirted into the vial. To an adult, Dr Guy gives 3 c.c.: on no account is this dose exceeded: children take 1½–2 c.c.—even adults often get less than 3 c.c. The vial is now attached to the side tube again, and the inhaler is ready for use.
After application of the mask to the face, the 3-way tap is at once pushed over to “no valve” and the patient rebreathes the gas in and out of the bag for some six or eight respirations. The[130] bag mount is now turned round “into register,” and the ethyl chloride tipped into the bag. In a further twenty-five seconds the mask may be removed and the operation begun.
The available period of anæsthesia is eighty to ninety seconds, counting from the instant of the removal of the inhaler.
This method was in use for some years at the Dental Hospital of Edinburgh; no instance of danger to life was ever seen. With so small a dose of ethyl chloride, the erect position necessary for the purposes of dentistry is perfectly safe.
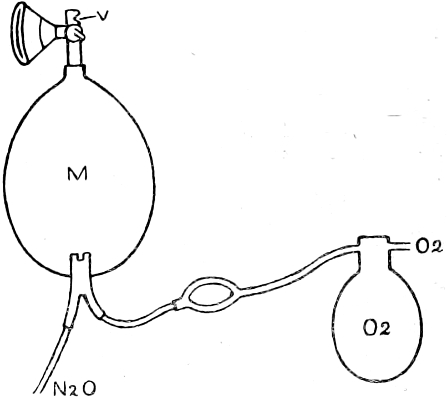
Fig. 44.—Diagram of the method introduced by Dr Guy and the author for giving Nitrous Oxide and Oxygen, with or without Ethyl Chloride.
This inhaler, of course, will serve admirably for giving ethyl chloride without gas, and the author habitually uses it for giving the drug by the “vapour” method.
In 1911, Dr Guy and the present author modified the method so as to permit the use of oxygen with the nitrous oxide. The inhaler which they then introduced serves also for nitrous oxide and oxygen, unaided by ethyl chloride, and the author has by its means given gas-oxygen to a considerable number of major surgical[131] cases. He now, however, limits its use to short anæsthesias, and uses a sight-feed or a Clarke apparatus for long cases.
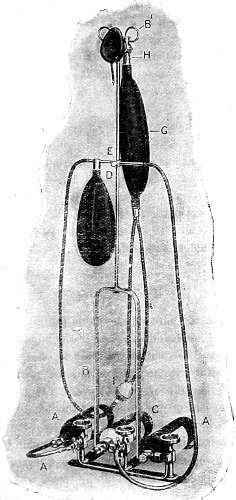
Fig. 45.—The Guy-Ross Inhaler for Nitrous Oxide and Oxygen, with or without Ethyl Chloride.
[132]
In Fig. 44 will be found a diagram showing the method by which the oxygen is introduced. The 1-gallon oxygen bag is either attached directly to a cylinder, or suspended on an upright as shown in Fig. 45. In either case, the bag is, before the administration, moderately filled with oxygen: one bagful will suffice for a short anæsthesia, and the supply of the oxygen from the cylinder is therefore turned off at once. For long cases, of course, a small trickle of oxygen into the bag is required to replace the gas used.
In the outlet pipe from the oxygen bag is placed a ball syringe of 2 ounces capacity. A valve in the pipe obliges the flow of oxygen to take place in one direction only when the bulb is squeezed, viz. from oxygen bag to inhaler.
The remainder of the apparatus is identical with Guy’s original inhaler, except that the bag is of 2-gallon capacity, and is perforated at its base by a Y-tube, one limb of the fork bringing in the nitrous oxide, the other the oxygen.
A few breaths of pure nitrous oxide gas are usually allowed “on the valve.” Rebreathing is then instituted, and the addition of oxygen begun. The amount required to each type of patient can only be learnt with experience, but the average is one full compression of the bulb every ten seconds. If anæsthesia is not complete at the end of one minute, put the indicator to “valves” again, and allow the patient nearly to empty the bag. Then push back the indicator to “no valves,” and refill the bag with nitrous oxide by opening the cylinder with the foot key. Some four to six compressions of the bulb are made while the nitrous oxide is running in. The time will now have come to add the dose of ethyl chloride if it be judged necessary at all. This will have been placed in the vial before the administration is begun.[133] After emptying the ethyl chloride into the bag of the inhaler, anæsthesia should be complete in twenty-five seconds.
The same small doses of ethyl chloride are used as is the case with Guy’s original method.
After a little practice under supervision, students at the Dental Hospital learn to use this method safely and well. No example of risk to life has arisen after eight years’ daily experience.[11]
[134]
The mere addition of ether does not remove all the undesirable features of chloroform anæsthesia. A heart poisoned by excess of CHCl3 does not respond to ether stimulation. Nevertheless, CE mixtures of varying proportions have great value. The less lethal drug takes on part of the work of the more dangerous one; it also keeps the respiratory centre active. Viewing mixtures as dilute chloroform, it is also obvious that there will be with them a greater margin of error in dosage, than with the pure drug.
Some chemical change takes place when the two drugs are mixed, for heat is evolved; of the nature of this change we are ignorant.
The first mixture introduced was known as ACE, and consisted of one part absolute alcohol, two parts chloroform, and three parts ether. Alcohol evaporates very slowly and if it be introduced at all it should be in much smaller proportion. Schäfer’s mixture is one part alcohol to nine parts chloroform. Neither of these mixtures is now much used. The most useful combination is two parts chloroform and three parts ether, and is known as C2E3. In special cases, one part of chloroform to two parts ether may be better.
Cones of varying type were at first extensively used for mixtures. The best known is Rendle’s (Fig. 46). It is made of celluloid, and is perforated at the top by a series of small holes through which the anæsthetic is introduced. A sponge is packed[135] into the upper part of the cone, and a flannelette cover completes the appliance. The objection to the use of this and kindred cones is that since chloroform evaporates more slowly than ether, the more dangerous drug is apt to collect in the sponge, completely altering the strength of the vapour after a time. This fault is remedied to a large extent by the open drop method now used.
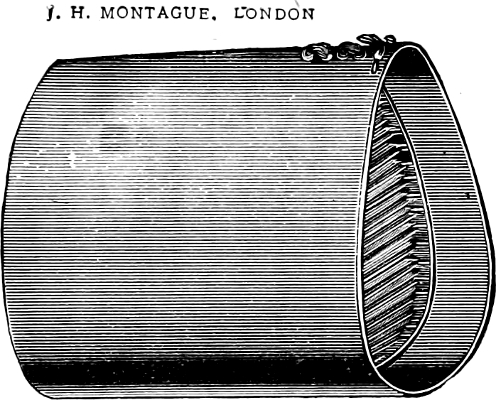
Fig. 46.—Rendle’s Cone.
For this the mask and ether dropper of Bellamy Gardner are admirably suited (Fig. 27). A material less close than the gauze advocated for open-ether is required. One layer of flannelette does very well, or the cheap cotton towels which used to be known in Edinburgh as “penny towels” in the pre-war period. The mask should fit the face with reasonable accuracy: there is no reason why a gauze ring should not be used to ensure this if the administrator is careful to adhere strictly to a “drop” method.
The bottle into which the dropper is inserted should be of different colour to those in which pure ether is habitually carried. This is a greater safeguard against a dangerous forgetfulness than a mere label.
[136]
As already said, the anæsthetic must be given by a strict “drop” method. “Douching” at frequent intervals gives results far inferior.
The Type of Anæsthesia is a compromise between that of chloroform and open-ether. Respirations and colour are better than with pure chloroform, not so good as with open-ether. The size of the pupil is also intermediate.
Scope.—As elsewhere explained there are many patients to whom open-ether cannot well be given; the greatest number of these can take a mixture perfectly and C.E. should certainly be chosen in preference to pure chloroform when possible. For refractory cases, it serves admirably as the inducing agent before the use of open-ether.
[137]
By a sequence we mean a method in which anæsthesia is partially or wholly induced by one anæsthetic or one method, and maintained by another. The methods mentioned in Chapter XIII. as devised by Dr Guy for dental purposes are examples which have already been sufficiently described.
Of the method of inducing anæsthesia by C.E., and turning later to open-ether, we have also already spoken. One thing remains to be said in this connection. Learn to judge the appearance of the type of patient who will require this alternative to open-ether induction, and use the sequence to such patients from the beginning. Don’t start off with open-ether, and find out in a few minutes that the patient is too obstreperous. A change from mixture to ether is harmless, the reverse process needs much care.
The sequence of C.E. to closed ether was advocated by Hewitt as a means of dealing with very alcoholic men, and for this purpose has great merits. The mixture is given until the stage of struggling is just about to commence, a point which experience enables one to fix with considerable accuracy. The remainder of the induction is conducted by a closed-ether inhaler, either the Hewitt wide-bore or preferably the Ormsby. The ether indicator which stands at about one when the inhaler is first applied, may be advanced very rapidly full ether strength being attained within a minute or two.[138] As soon as rebreathing is begun with either of these instruments, it is very striking to watch the rapid and apparently safe subsidence into anæsthesia of the most troublesome patient. The struggling is cut short and greatly minimised in violence, and a stage which under CHCl3 might have presented some considerable risk of secondary syncope, is thus eliminated.
This is a method greatly superior to the induction by closed-ether described on p. 79. Instead of the 1-gallon bag of the Clover or Hewitt instrument, the valve piece and 2-gallon bag of a gas apparatus are attached to the head of the ether inhaler (Fig. 23, on page 77).
Once the gas bag is inflated from the cylinder, the supply of gas may be cut off. A few breaths of gas “upon the valves” are given, until the bag is half empty; the valve tap is then pushed over to “no valves” and rebreathing begun. Ether may be turned on a few seconds later, and the strength of the vapour may be increased more rapidly. Three-quarter strength of ether may be attained as a rule in ninety seconds. There is very little likelihood of struggling in this method.
This is a valuable method for short operations, being easily portable, speedy and safe in action, and fairly agreeable to the patient. Some anæsthetists use this induction method as a prelude to open-ether.
The Clover (or Hewitt wide-bore) instrument is interposed between the face-piece and the T. of the ethyl chloride inhaler, as shown in Fig. 47. A small dose of ethyl chloride only is requisite; for an adult, 3 c.c. is enough. This is vapourised over hot water in the usual way; a very light anæsthesia is induced in some[139] sixty seconds, and the ether can then be turned on at a much quicker rate than if the induction be conducted by that drug alone.
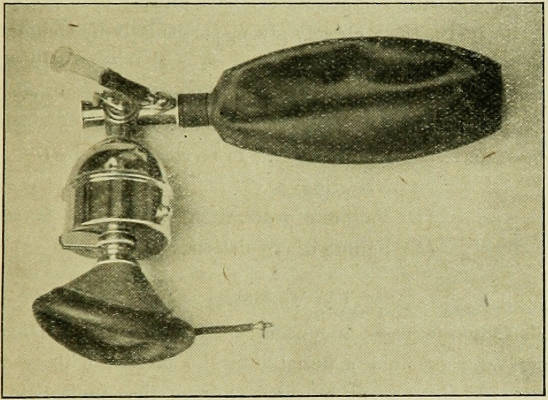
Fig. 47.—Clover’s Inhaler adapted for the Ethyl Chloride-Ether sequence.
The gas-ether and ethyl chloride-ether sequences are most useful methods. They are quick, safe, and powerful.
Either may be used as “single dose” anæsthetic, the ether being pushed quickly up to “full” and the inhaler then withdrawn. If, however, no access to the mouth is required by the surgeon, ether anæsthesia may, by occasional breaths of fresh air be prolonged for as long as desired.
[140]
The minor difficulties of anæsthesia have already been dealt with, and if the instructions already given, particularly in Chapter III., are faithfully carried out, incidents of real danger will rarely occur. The soundest knowledge and the most conscientious care will, however, never entirely rid anæsthesia of an element of danger to life. The conditions now to be considered are:—
(A) Vomiting.
(B) Failure of respiration.
(C) Failure of circulation.
This always exposes an unconscious patient to the danger of inhaling solid or fluid material into the larynx, with resulting asphyxia. If the patient be tided through that immediate difficulty, he is liable to develop an inhalational pneumonia subsequently.
A healthy patient properly prepared should not vomit during the induction stage, nor during the progress of the operation. If he does, it means that the induction has been too slow, or that the administration has been intermittent, and the patient has been permitted to come to too light a level of anæsthesia during the operation.
During emergency operations where the patient’s stomach may be full of food, the case is different. Such patients commonly vomit early in the induction stage, and no skill can avert the incident.
A patient suffering from intestinal obstruction, or from[141] generalised peritonitis has his stomach and intestines full of highly infective fluid. Reverse peristaltic may set in merely as the result of the inhalation, or later from handling the contents of the abdomen, and the feculent fluid gushes up the œsophagus with little or no warning. Since vomiting in these cases may occur even in deep anæsthesia, when the cough reflex which is the normal sentry to the entrance of the larynx, is abolished, the dangers of insufflation are very real indeed. Personally, the author prefers to wash out the stomach before beginning to induce anæsthesia in these cases, but some surgeons believe that the shock of this procedure outweighs the advantages.
In ordinary cases, vomiting is usually heralded by a definite train of symptoms. Respiration becomes shallow, the colour a little pale and the pulse rather small. The pupil dilates, but remains active to light, indicating that the alteration of respiration and circulation is not due to overdose.
At the first appearance of such symptoms, a brisk rub of the lips and thereafter an increase of the vapour strength of the anæsthetic will often avert the impending vomiting by deepening the anæsthesia, but if the possibility of this complication has occurred to the anæsthetist too late for its prevention, the head must be turned well to one side, and the other shoulder slightly elevated by a pillow, so that vomited material will fall out of the mouth at once. When the actual act of vomiting is over, no time must be lost in mopping out the mouth and pressing on with the production of a deeper anæsthesia.
These divide themselves into two groups:—
(1) Mechanical.—The respiratory movements continue, but the ingress and egress of air is blocked.
[142]
The symptoms and preventative treatment have been referred to at some length in Chapter III., and no further account of these is therefore necessary. The treatment of a complete blockage of the air passages which resist the measure there described, alone remain to be mentioned. Of these, the only two effective are artificial respiration and tracheotomy (or laryngotomy if preferred by the surgeon). Forcible artificial respiration by the Sylvester method, with the mouth gagged open and the tongue held forward by the tongue forceps, is frequently successful in getting over even a complete block, but the last resort of opening the air passage by the knife must not be delayed until too late. In deciding such a point, considerable judgment is of course called for.
This is usually seen in conjunction with a serious failure of the circulation caused by over-dosage. Exceptionally, some act of the surgeon sets up a reflex inhibition of the respiratory centre; the circulation is at the same time depressed, but to a varying degree. The cardinal symptom is arrest of all respiratory effort. The treatment is best dealt with under the heading of circulatory failure.
By the term syncope, we mean a more or less sudden failure of the cardiac pump, as opposed to the form of circulatory failure seen in surgical shock, where the condition is chiefly, though not wholly, one of vaso-motor paralysis (see Chapter II.).
Syncope occurs under varying conditions which may for descriptive purposes be divided into four classes. It is not, however, always possible to decide with certainty into which class an individual case should be placed.
The symptoms common to all classes of syncope are:—
(1) Pallor, and loss of all tone in the muscles, noticeably those of expression. The pulse is weak or imperceptible.
[143]
(2) Cessation of respiration.
(3) Dilatation of the pupil, which ceases to react to light.
The four classes above mentioned are as follows:—
This is peculiar to chloroform. With no other anæsthetic is it seen, at any rate in the healthy subject. It arises during the induction period, and is not necessarily preceded by any respiratory difficulty. There is one big inspiratory gasp, sudden and extreme pallor, and the pupil goes out to the rim in a few seconds. The only reasonable explanation of such an incident is the occurrence of vagal inhibition (see page 112). Its prevention therefore is a matter of the avoidance of a high percentage of chloroform.
This term is applied to a collapse arising as a secondary result of embarrassed respiration. Though not peculiar to chloroform, it is far more common with that drug than with any other (ethyl chloride excepted). The most common time for the accident is towards the end of the induction period. The patient has probably been struggling, has clenched the jaws, and developed “mechanical” asphyxia. Violent inspiratory efforts are still being made, and considerable cyanosis develops. Either at the very moment when the respiratory difficulty is overcome, or while it still persists, the colour suddenly alters from blue to white, and the other symptoms of syncope rapidly appear. The exact period required to transform a blue struggling patient with heaving chest, into one with pallid face, and motionless chest and limbs, varies greatly, for reasons furnished below.
The most reasonable explanation offered of such an accident is that given by Leonard Hill. The attempts to inspire through an air[144] way mechanically blocked cause an immense strain upon the heart muscle. The flow of blood in the lung capillary is hindered, and the right side of the heart becomes over distended with blood. Its musculature is further damaged by the fact that the blood in the coronary vessels is deficient in oxygen, and that a considerable dose of anæsthetic has already been absorbed. There is the further fact, not mentioned by Hill, that during the whole period of asphyxia the peripheral resistance is rising from vaso-constriction. Under circumstances such as these, it is obvious that any heart must ultimately succumb, no matter what anæsthetic is in use. It is also obvious that with chloroform and ethyl chloride, which are themselves heart poisons, secondary syncope will happen much more readily than with ether or nitrous oxide, which are not; and that a heart with diseased musculature will fail quicker than a healthy organ.
Secondary syncope is almost certainly the commonest fatal accident of anæsthesia. The reason why this fact is not more widely recognised arises from the natural instinct of any one who has suffered the misery and ignominy of causing a death under an anæsthetic, to attribute it to some cause beyond human control. The essential cause of secondary syncope is failure to maintain a free air way, which cannot be styled unavoidable. Two consolations may, however, honestly be offered to the person who has acted as anæsthetist in a case of secondary syncope. Firstly, it is, in certain types of cases, very difficult indeed to maintain a free air way; and secondly, a heart with muscle degenerated from fatty or other changes, may give out after very little respiratory embarrassment.
This is a more gradual affair than the two foregoing; and has been sufficiently dealt with in the chapter devoted to the Stages of Anæsthesia (see p. 36).
[145]
Exceptionally, a patient not overdosed with anæsthetic, and not suffering from any mechanical obstruction to respiration, has a sudden attack of syncope during the progress of the operation. We here exclude patients who are suffering from surgical shock; the condition arises too rapidly for such an explanation to be accepted. Much speculation has been expended upon these cases. One view is that some procedure of the surgeon has set up a reflex inhibition of the heart through the vagus; another, that the reflex has taken the form of sudden vasomotor paresis. Levy would ascribe the condition to cardiac fibrillation. It may well be that all cases cannot be met by one explanation. The older surgeons stoutly maintained that reflex syncope could not arise if the patient were properly under, and that it was in the practice of those anæsthetists who were afraid of pushing the anæsthetic sufficiently, that such accidents occurred. The author’s own belief is that a very light chloroform anæsthesia does pre-dispose to this accident, but that it may occur also at a deep, the very deepest possible level. With an anæsthetic other than chloroform, it is extremely rare—perhaps unknown.
This must be speedy to be of any avail. The following are the points upon which to concentrate:—
(1) Withdraw the anæsthetic.
(2) Make sure that the air way is free.
(3) Begin artificial respiration by Sylvester’s method, the movement of expiration being first performed (see Fig. 48).
(4) Lowering of the head and shoulders is usually to be recommended. It is best done by tilting the whole table as if for the Trendelenberg position.
The lowering of the head attracts more blood to the[146] carotid artery and raises the blood pressure of the main vessel and its cerebral branches (see Fig. 35). It must, however, be remembered that it will also tend to empty the blood in the veins of the lower extremities and abdomen into the right side of the heart, and cases in which marked cyanosis has preceded pallor, are probably suffering already from engorgement and dilatation of the right heart. The tilting of the table should in such cases be very moderate in degree, and should not be persisted in if it seems to do no good. In no case, indeed, should the tilting be extreme. An angle of more than 15 or 20 degrees is as likely to do harm as good.
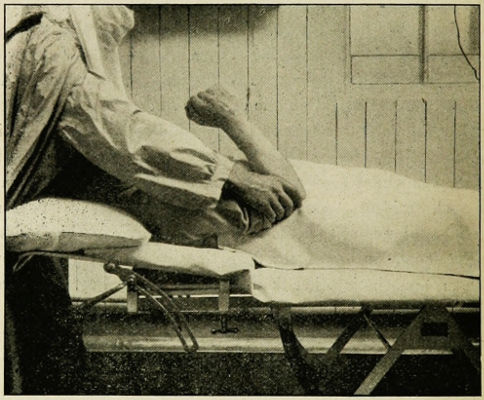
Fig. 48a.—Artificial respiration by Sylvester’s method. Expiration.
(5) Hot cloths may be placed over the precordial region, care being taken not to burn the skin.
[147]
(6) The only drugs likely to be of any avail are atropine and strychnine, the former being used with the idea of paralysing the terminations of the vagus in the heart muscle, the latter as a cardiac tonic and a stimulant to the respiratory centre. Some authorities have recommended the injection of atropine by a long needle passed into the heart muscle, but most are content to give either or both drugs hypodermically. Really to paralyse the vagus, a very large dose of atropine is required—about ¹⁄₃₀ gr. Strychnine should be given in a dose of ¹⁄₄₀–¹⁄₃₀ gr.
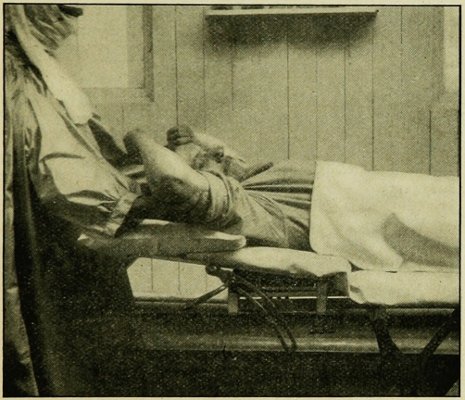
Fig. 48b.—Artificial respiration by Sylvester’s method. Inspiration.
(7) In cases where the right heart has certainly been over-distended, the expedient of venesection has been tried. Some six ounces may be withdrawn from the external jugular or one of the veins of the arm.
[148]
(8) As a last resort, the heart may be massaged. The only practicable route is to open the abdomen (if not already done) pass one hand under the left side of the vault of the diaphragm, placing the other hand over the precordial region. Between the two hands, the heart can first be thoroughly compressed to empty its presumably flaccid and over-distended cavities, and then lightly massaged. Several cases of recovery from this measure are on record.
Before leaving the subject of accidents it may be well to allude to this condition, which is also known as status thymicus, and as lymphatism.
It is met with mostly in the young, the commonest ages probably being five to fifteen years. Certain pathological conditions have been found in fatal cases, of which the most important are an enlargement of the thymus gland, of various lymph glands, and of the tonsils, including the naso-pharyngeal tonsil (adenoids). The heart muscle is frequently degenerated. Of the cause of these abnormalities we are as yet in doubt. There is some reason to believe that the condition tends to disappear with advancing years, if the subject survive.
The most outstanding clinical fact in connection with the disease is its tendency to cause sudden death on very little provocation. A fright, a sudden exertion, and above all an anæsthetic may cause sudden and fatal syncope.
Suspicion that the disease is present may be aroused in several ways. The presence of enlarged tonsils and adenoids, combined with general enlargement of lymph glands from no obvious cause, and a tendency to faint, make a very suggestive picture. “Night-crowing” (a sudden attack of laryngeal spasm,[149] occurring at night, and often repeated at intervals) also raises grave doubt. The diagnosis can only be established with certainty by an X-ray photograph, when the great enlargement of the thymus may be seen in the upper part of the chest.
Too frequently the condition has never been suspected, and a fatality occurs from sudden syncope, usually during the induction period, but occasionally during the progress of the operation. It would, however, be fallacious to suppose that an anæsthetic is necessarily fatal even to an undoubted case. If the drug (preferably ether) be given with great care, and the operation done carefully at a level of anæsthesia neither too light nor too deep, there is every reason to believe that the danger can be, and often is, successfully averted.
At the same time, it must be understood that in a known case, operation should always be avoided or deferred if possible.
[150]
After operations performed under any form of anæsthesia, even spinal, there is always a possibility of pneumonia or bronchitis. The anæsthetic itself is not always to blame. The patient has suffered trauma and is confined to bed, and may develop a hypostatic pneumonia just as a person who has suffered from a fractured thigh so commonly does, even though he has had no anæsthetic at all.
It is probable that organisms, capable under certain circumstances of causing inflammatory disease of the respiratory tract, are present in a large proportion of apparently healthy people. Pneumococci and streptococci of varying strains may be grown from nasal or pharyngeal secretions of patients who suffer from catarrh of these regions, and may reappear upon slight provocation even when prolonged treatment had apparently banished them permanently. All that is required to start an acute infection of lungs or bronchi, is some factor that depresses vitality and lowers body resistance to the organism. And if in addition use has been made of an inhalational anæsthetic such as ether, which may cause an immediate and fairly acute congestion of the respiratory mucous membranes, it is not to be wondered at that serious sequelæ follow in a certain proportion of cases.
Laboratory results go to show that ether lowers the opsonic index of the blood to pneumococci and streptococci, but without placing undue emphasis upon a mere isolated phenomenon such as[151] that, it is plain that the whole conditions of the patient after operation are favourable to the occurrence of pneumonia or bronchitis, and that of all anæsthetics ether is the most likely to be the determining factor.
Experience gained during the war has thrown a certain amount of light upon this subject. Post-anæsthetic bronchitis and pneumonia was very prevalent among the wounded, far more so than among civilian patients. It is, the author believes, reasonable to attribute this fact to several causes. In the first place, the soldier’s life, alternating between stuffy billets and wet trenches, predisposed him to naso-pharyngeal catarrh of a fairly high degree of infectivity. Enthusiastic press representatives might state that you could not take cold so long as your feet and legs were always buried in half frozen mud, but experience hardly bore out their golden promises. Again, the soldier did not improve his catarrh by inveterate cigarette smoking. Lastly, military hospitals were large institutions, some under canvas, some in huts, some in buildings constructed for other purposes, and rapidly altered to the urgent needs of the army. Of whatever type, nearly all had one feature in common—many of the surgical wards were a long (and draughty) way from the operating theatre.
For the prevention of post-anæsthetic pneumonia, the author offers the following tentative suggestions:—
(1) See that the skin is kept covered up as much as possible during the operation and that the patient is not exposed to draughts during or after it. Rooms can, and should be, well ventilated without cold draughts.
(2) If a patient has an acute or sub-acute naso-pharyngeal catarrh, treat it as fully as possible before operation by sprays and gargles.
(3) Do not use ether to patients who suffer or recently have suffered from such conditions.
[152]
(4) Give a hypodermic of morphia and atropine before operation as a routine.
(5) In so far as possible, let the patient’s shoulders and head be raised by pillows during the early hours of convalescence.
(6) Lastly, remember that while no care will absolutely banish these dangerous sequelæ from our practice, the greater care and skill shown by the anæsthetist, the less bronchitis and pneumonia will appear among his patients. As regards ether, the author believes that it is the strength of vapour used, more than the duration of the anæsthesia, which counts. It is for that, among other reasons, that he has for the induction period, no hesitation in recommending a method whereby a small part of the requisite ether strength is replaced by chloroform.
After an anæsthesia lasting more than a few minutes, it may almost be regarded as normal for the patient to vomit once or twice. Usually this occurs a few minutes after the administration has ceased. In the case of nitrous oxide and oxygen, even this slight disturbance may not occur.
The amount of vomiting which after this stage may be regarded as normal is difficult to determine. The author took notes of some 300 cases on this point. The details of his results are not suitable for a text book, but, broadly speaking, it would appear that after an operation of ordinary duration and severity, the vomiting returns on the average some five or six times, and usually ceases on the evening of the operation day. A limited number continue to vomit at intervals until the early hours of the following morning. With nitrous oxide and oxygen the vomiting is far less than the above, though even with this anæsthetic quite severe emesis may occur. With closed-ether, the trouble is very violent[153] for a short time, large quantities of mucous being ejected: it is probable that after the first two hours, it is no more marked than after open methods. The use of morphia and atropine before operation most certainly reduces the violence and duration of this sequela.
Prolonged more than twenty-four hours, the condition must be regarded as definitely abnormal.
The adoption of open-ether preceded by morphia and atropine and due skill and thought on the part of the anæsthetist, combined with proper preparation of the patient, are the only means of prevention at our command.
The raised position of the head and shoulders during the recovery stage undoubtedly tends to reduce the nuisance. It is a vexed question whether to give or to withhold fluids after operation—and this matter is of course in the hands of the surgeon, not the anæsthetist. In certain cases, the author believes that it is worth while trying the effect of a cup of fresh tea with very little sugar or milk. Even if rejected in a few moments, the astringent effect of the infusion seems to soothe the gastric mucous membrane, and give relief.
(Synonym—Delayed Chloroform Poisoning).
In a limited number of cases, post-operative emesis assumes a grave type, and definitely threatens life. Such cases began to be studied in the early part of this century, and though our knowledge of the condition is still incomplete, the student should be acquainted with the present views held upon the subject.
Clinically, the earliest symptom to raise suspicion, is the reappearance of vomiting at a time when one would expect such trouble to have abated, usually twenty-four or thirty-six hours[154] after operation. Within a few hours, the nature of the vomit changes from the usual bilious stomach contents, and shows obvious evidence of the presence of altered blood. The pulse and temperature begin to rise, the countenance assumes an anxious look. A trace of jaundice is usually present. The nervous system becomes affected as shown first in restlessness, and later, delirium. Every degree of this condition is possible, but a very large proportion of recognisable cases pass into coma, and death supervenes within a few days, sometimes less.
Investigation into such cases has shown that the essential underlying condition is an acidosis closely allied to that seen in diabetic coma. The breath has the peculiar sweetish aroma of acetone, and acetone, diacetic acid, and B. oxybutyric acid successively appear in the urine.
Post-mortem, the most striking change found is a profound fatty degeneration of the liver, the cells of which are disintegrated as in acute yellow atrophy.
It is obvious from the foregoing that there is present a very remarkable abnormality of metabolism. Mr Rendle Short, in his admirable book, The New Physiology in Surgical and General Practice, gives the following explanation of the condition:—
“The physiological process of dealing with fat is to resolve it into carbon di-oxide and water. If we make a pound of fat into tallow candles and burn it, we shall obtain carbon di-oxide and water, and a certain amount of heat will be evolved. If the pound of fat is eaten and absorbed by a man or an animal, it will be burnt to the same end products, and the same amount of heat will be given out. But in certain circumstances, an abnormal mode of breaking down is followed, and there are produced, first B. oxybutyric acid, then diacetic acid, and finally acetone. If this takes place on a large scale, the conversion into acetone fails to keep pace with the production of acids. Therefore first acetone appears in the urine, then diacetic acid, and finally[155] oxybutyric acid; the last may rise rapidly to an enormous figure: 30, 50, or even 180 grams may be passed daily.”
Later in the same chapter, Short propounds the question as to what are the special circumstances in which the breaking down of fat deviates from its normal course, and follows this dangerous route. The answer is, he says, quite definite and decisive. When the tissues are unable to obtain sugar from the blood, fat is broken down via these dangerous acids to acetone, instead of to carbon di-oxide and water.
Such an inability on the part of the tissues to obtain sugar arises under several conditions:—
(a) In diabetes, where sugar though freely present in the blood cannot, for some reason still not clearly known, be assimilated by the tissues.
(b) In poisoning by salicylates.
(c) In starvation, for obvious reasons. The supply of sugar from the liver has been used up, and the patient, living on his own fats, breaks them up abnormally.
(d) In post-anæsthetic poisoning, for reasons which are at present not clearly ascertained.
Upon the theoretical side it is therefore not possible to say more than that anæsthetics sometimes initiate this abnormal metabolic process. To the question as to why and how they do so, we can as yet give no answer.
Upon the practical side, we can, however, speak much more definitely. Acidosis follows the use of ether very rarely indeed: after nitrous oxide it is unknown. Chloroform has been the drug used in almost every recorded case, while ethyl chloride has been responsible in a few isolated instances. Young children are much more prone to suffer than adults, though the author had a fatal case in a lady well over forty years of age: he has also seen a case very nearly fatal in a soldier aged twenty. This man[156] was, a week after recovery from acidosis, anæsthetised for half-an-hour with nitrous oxide and oxygen, without exhibiting any signs of a return of his dangerous condition. Anæsthesia repeated in the same subject after a short interval is more prone to start the process than a first inhalation. Lastly, acute sepsis, particularly in the young, is notorious for its liability to be followed by acidosis.
The obvious moral of the foregoing is that chloroform should not be administered to patients suffering from acute sepsis, particularly if they be very young. Indeed, so common is a mild degree of acidosis among children, some surgeons consider there is a definite risk in giving chloroform to them at all unless special precautions are taken. Chief among these are regular dosage for a day or two before operation, with considerable doses of bicarbonate of soda and sugar, which is a routine measure in some children’s hospitals.
As regards curative treatment, much can be done if the gravity of the condition is recognised early. The stomach is first washed out with alkalis, and a substantial dose (one dram) of bicarbonate of soda left in it. The same dose is repeated hourly by the mouth, if retained, or per rectum. A useful addition to the alkaline treatment is dextrose, also in teaspoonful doses. In grave cases, these drugs should be given intravenously in saline solution.
These measures combined with warmth, and ample fluids by mouth or rectum, will often save life, but to be of any value they must be begun early. Fulminating cases occur which succumb rapidly in spite of treatment.
[157]
The position in which the patient is lying is of as much importance to the anæsthetist as to the surgeon. It is for the surgeon to say what he wants and for the anæsthetist to realise how his own work will be thereby affected.
This is the ordinary position and calls for no extended comment. The pillows must be so arranged that at no spot is the body acutely flexed or extended. Abdomen, thorax, neck, and head must all be roughly in a straight line.
Deep-chested subjects require a higher pillow than those with shallow chests, otherwise the neck is bent back and respiration obstructed.
The arms should either be folded and retained by a bandage or other device over the chest, or extended so that the hands can be slipped under the buttocks and retained there by the body weight. An arm which is allowed to hang over the side of the table is likely to show next day and for many months afterwards, the condition of drop-wrist from musculo-spiral paralysis.
This is an awkward position for the anæsthetist; there being a general tendency to respiratory embarrassment. Put a pillow under the upper part of the thorax, leaving the lower part and the abdomen as free as possible. Let the head project from the pillow, so that the face can be got at without undue rotation of the neck. The intratracheal method is a great help.
[158]
This may be called for either with or without the addition of a sand-bag or inflatable air-pillow to push the loin upwards. In either case, there is a tendency for the upper shoulder to fall forwards, the position then assimilating itself to the face-down position. This is best met by a support fixed to the table, upon which the upper arm may be rested. Failing such a convenience, a sand-bag may be pushed in to keep up the shoulder, or the assistance of a nurse may be required.
Slight tilting of the head end of the table downwards is often useful in assisting the return of bowel into the abdomen: in this position, the patient usually takes the anæsthetic very well. It must not be assumed until the third stage of anæsthesia is reached.
For many gynæcological operations, however, the full Trendelenburg position is required. Healthy subjects usually do quite well in it, but stout persons not uncommonly show a good deal of cyanosis. At the close of the operation it is essential to restore the table to the horizontal slowly: the physics of the circulation are profoundly modified, and if any serious degree of shock is present, rapid return to normal may initiate a collapse.
In the full position, the weight of the body should be taken by metal supports attached to the table against which the shoulders may rest. To hang the entire weight of the body upon the legs may cause a good deal of after-suffering to the patient.
The object of this position is to diminish venous engorgement and bleeding in operations requiring delicate dissection in the region of the neck. Prof. Alexis Thomson introduced the position into Edinburgh surgery: the author was at first rather nervous of[159] it, but has found that with proper precautions the patients do uncommonly well. Beyond all doubt, the position is a great help to the work of the surgeon.
Not every surgical table is capable of giving the full position without the use of many pillows and sandbags. The head-piece of the table is tilted up at an angle of about 75° or even 80°, and the patient pulled up so that the flexion of the body occurs in the lumbar, not the dorsal spine. A small sand-pillow is placed behind the neck so as to produce slight extension. Another heavier one is placed under the thighs to prevent the body slipping down. A slight tilt downwards towards the head end may be given to the table as a whole with the same object.
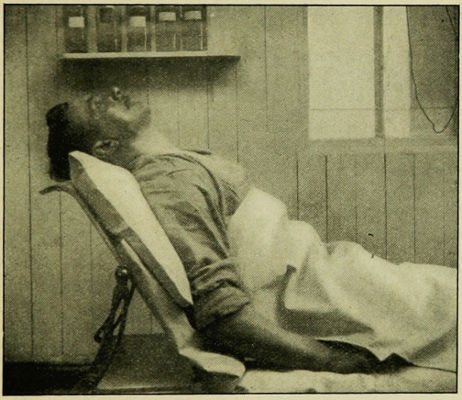
Fig. 49.—Sitting-up posture for operations on the neck.
One should not in this position attempt to induce a deep chloroform anæsthesia. Weak C.E. mixture at most, but better simply open-ether is the method of choice. The induction is[160] begun with the shoulders raised to a modified degree, and the full position assumed in a light third stage anæsthesia.
Intratracheal ether combined with this position is an ideal anæsthesia for the removal of goitre or extensive dissections in the neck for enlarged glands.
The author became acquainted with this useful position while acting as Anæsthetist at the Royal Herbert Hospital, Woolwich, where the Nose and Throat Department was under the charge of Major O’Malley, F.R.C.S. Major O’Malley was kind enough in a recent letter written by request to refresh the author’s memory of the details.
Fig. 50.—O’Malley’s posture for intra-nasal surgery.
With the patient lying as shewn in the photograph, every part of the interior of the nose can be easily inspected by the surgeon; the elevation of the head and shoulders prevents undue bleeding, and such hæmorrhage as does occur goes down the gullet, where it does no particular harm, instead of into the larynx. The degree[161] of flexion of the head upon the neck is not so extreme as to interfere with respiration.
The details of O’Malley’s procedure are as follows:—
The interior of the nasal cavities are packed with gauze soaked in adrenalin and novocain a quarter of an hour before operation, and the patient receives a very small dose of morphia and atropine immediately before anæsthesis is induced; given in this way it does not complicate the induction with chloroform to the same extent as if given earlier. The patient lies with the top of the head level with the top of the table, and the head and shoulders (including the upper two-thirds of the shoulder blades) supported on the usual depth of pillow. Induction is by chloroform or mixture; a very light third stage only is aimed at. When it is attained the mouth is opened by a gag, and Phillip’s Oral Airway inserted (see Fig. 8). Strict oral respiration is essential to success. If air is passing in and out of the nose, blood is spluttered all over the surgeon, seriously interfering with the harmony of the proceedings. Junker’s chloroform bottle is ready, and the end of the supply pipe is passed into one of the side holes in the air way.
The head of the table is now elevated to an angle of 45°, and a small sand pillow slipped behind the occiput. The gauze is removed from the nose, and the operation can be performed with great comfort.
The circulation of the patient needs careful watching for the first minute or two after the table head has been elevated, but thereafter there is usually no special cause for anxiety. The area of operation is locally anæsthetised by the action of the novocain and a light chloroform sleep only is required.
[162]
In considering this matter, some repetition of points to which reference has already been made, is inevitable. Indeed, this chapter may be regarded as a revision of the whole subject.
Before deciding upon drug and method suitable for the individual case, we must consider the age and sex, the physical type and temperament, the possible presence of some definite pathological condition, and the nature and duration of the operation.
In relation to this last point, we must remember that an anæsthesia must be adequate to the purpose of the surgeon, but that it is improper to incur more risk to life than is necessary. For instance, an abdominal section case must be fully relaxed, and if in an individual case, chloroform is the only drug which will give that effect, there need be no hesitation in using it. On the other hand, many other methods with a far smaller mortality rate are available if all that is required is the extraction of a tooth or the incision of an abscess, and in that group of cases, unfamiliarity with such anæsthetics as nitrous oxide or “ethyl chloride and ether” will not be held as a sufficient defence if chloroform has been given with a fatal effect.
Let us take first the case of the healthy adult about to undergo a major operation. For this, we unhesitatingly choose what we may term the “stock” method—open-ether preceded by morphia and atropine.
[163]
If the operation be brief, we have a choice of methods. For the extraction of teeth, where access to the mouth is essential, the following table will help:—
| Anæsthetic Drug and Method. | Duration of Available Anæsthesia, when given as “Single Dose.” |
Remarks. |
| Nitrous oxide | 30 to 40 seconds | |
| Nitrous oxide and oxygen |
40 to 50 seconds | |
| Ethyl chloride | 70 to 90 seconds | Only to be recommended in special cases (see page 127). |
| Gas and ethyl chloride | 70 to 90 seconds | |
| Gas-oxygen and ethyl chloride |
70 to 90 seconds | |
| Gas and ether | Anything up to 2 to 5 minutes according to duration of inhalation | May cause after vomiting. |
| Ethyl chloride and ether | Anything up to 2 to 5 minutes according to duration of inhalation | May cause after vomiting. More portable. |
| Nasal gas | 5 to 10 minutes (not a “single dose” anæsthetic) | Requires considerable practice to give well. |
| Nasal gas and oxygen | No limit | Easier to give than above but apparatus rather importable. |
In cases where access to the mouth is not required, and where it is therefore unnecessary to “charge up” the patient with anæsthetic, we have also a choice which may be expressed tabularly:—
| Anæsthetic. | Remarks. |
| Nitrous oxide | Apparatus simple: short administration can be mastered easily. A little more practice required for cases prolonged by admitting air. Muscles not relaxed, and patient may move when cut.[164] |
| Nitrous oxide and oxygen | Apparatus more complicated, but short administrations present no great difficulty to the beginner. | Muscles not completely relaxed unless a little | ether added. |
| Gas and ether | Quick and safe anæsthetic. Deep anæsthesia may be obtained if ether is “pushed.” |
| Ethyl chloride and ether | The same. More portable than above. |
In this group of short operations, special reference must be made to the reduction of dislocations. Here two important features require notice. The whole object of the proceeding is to relax muscles, and therefore nitrous oxide or gas-oxygen are unsuitable. Secondly, the tendency to reflex syncope just at the moment of reduction is very great. For this reason, chloroform has here a painfully high mortality rate; closed-ether, preceded by gas or ethyl chloride, is undoubtedly the method of choice.
Children up to the age of ten years take ether badly, salivation and bronchial secretion being sometimes very troublesome. Atropine mitigates this nuisance to a limited degree only. Chloroform is the best drug up to five or six years; from five to ten, mixture; after that, open ether.
In children of any age, suffering from acute sepsis, the immediate annoyances and possible respiratory sequelæ of ether must be faced (see page 156), owing to the probability of acidosis.
As regards short anæsthetics in children, nitrous oxide, if given at all, should be freely diluted with oxygen, otherwise most undesirable cyanosis will occur. To children under three or four, even gas-oxygen is of doubtful safety. Short anæsthesias in such cases may be induced by open ethyl chloride, with a few drops of ether added.
[165]
Old people are, unless very feeble, best anæsthetised by a mixture of chloroform and ether. Whatever anæsthetic be chosen, the utmost care must be taken to avoid cyanosis. A cylinder of oxygen should be at hand from which to enrich the atmosphere breathed, by trickling the gas into the mouth through a rubber tube, and is a great safeguard in dealing with the old.
On the average, women take anæsthetics much better than men, being far less liable to jaw clenching and other forms of mechanical asphyxia, and showing less excitement during the induction stage. In the female subject induction by open-ether requires very little assistance from C.E. mixture.
Heavily built muscular men are troublesome subjects. Induction requires a rather strong vapour of ether: if the open method is used, there may be to the beginner much temptation to make use during the induction stage of C.E. mixture to an extent not contemplated in the description given of that method in chapter IX.: it is therefore wise to induce either with closed-ether or with C.E. mixture as described in chapter XV., and to change to the perhalation method only when full anæsthesia is attained.
As regards alcoholics and excessive smokers, these are well dealt with by the C.E. open-ether sequence. Recourse may be made to the Ormsby inhaler as already explained on page 137. The reader is warned not to be deceived by the stout, rosy face of the typical alcoholic. He often looks a great deal stronger than he really is. Many such are really feeble subjects: although they shout and struggle no great addition to the usual vapour strength of anæsthetic is safe or required: what is required, is a little extra time. Once fully under, the robust appearance of the[166] patient disappears, and the fact that one is dealing with a rather broken constitution and a poor circulation is obvious.
Reference has already been made to the fact that persons with defective nervous systems, neurotics, and especially epileptics, show persistence of some muscular movements for some time, and therefore require very careful watching.
These are of the utmost importance, but to consider each fully from the anæsthetic point of view, would lead us into great detail. The anæsthetist must acquaint himself with any abnormality present, and consider it carefully in the light of the general principles already explained. The following very brief hints for selected cases and operations may, however, be found useful.
Artificial teeth. Must be removed before inducing.
Tongue and jaw cases.—Intratracheal ether the best—failing that, rectal oil ether, or Junker’s inhaler.
Nasal operations.—If adrenalin is to be used, it must precede, not follow, chloroform—many fatalities have occurred from injecting or even packing with adrenalin in light chloroform narcosis. Some surgeons object to ether because of the bleeding, but this can be largely remedied by raising the head and shoulders, and by packing with adrenalin. Many surgeons prefer local to general anæsthesia.
Nasal insufficiency.—Don’t allow a patient to continue to make ineffectual attempts to breathe through a narrow nose. Establish mouth breathing, or use Silk’s tubes (see Fig. 9).
Tonsils and adenoids.—Give ethyl chloride by the vapour method.
Tumours and inflammatory swellings obstructing respiration.—[167] Don’t use closed methods. Have tracheotomy instruments at hand, and a cylinder of oxygen.
Gôitres, especially exophthalmic gôitre.—Don’t use chloroform: it has caused many fatalities; morph-atropine, followed by open-ether is the safest. In bad cases, use rectal oil ether if intratracheal is not available. The “sitting up posture” is a great help (see page 168). Use anoci-association if surgeon is willing.
Bronchitis and pneumonia (see remarks in chapter XVII).
Emphysema and rigid chest wall.—Patients take anæsthetics badly; they cyanose quickly, the abdominal wall cannot be made either lax or quiet, since the patient’s natural method of respiration is abdominal rather than thoracic. Lastly, there is frequently a dilated heart with degenerate cardiac muscle, giving an abnormal tendency to secondary syncope. Give a trickle of oxygen through a tube from a cylinder: don’t be tempted to overdose with anæsthetic in the vain hope of securing ideal relaxation of the abdominal wall.
Empyæma.—Be careful: a good many accidents have happened. Use chloroform with added oxygen: aim at an anæsthesia just deep enough to prevent straining which might rupture the empyæma into the lung and drown him in his own pus. Withdraw the anæsthetic as soon as the abscess is opened.
Phthisis.—Don’t use closed-ether: it may start hæmorrhage—open-ether rarely does any harm unless the condition is very acute.
High tension, arterio-sclerosis, and aneurysm.—Avoid pure nitrous oxide: in severe cases, C.E. mixture and oxygen is the safest.
Heart.—Well compensated cases of valvular disease take chloroform or open-ether well, provided a free air-way is maintained.[168] Closed methods should be avoided. Cases of myocardial disease with dilated cavities present special dangers. Open-ether with added oxygen meets the case better than any other anæsthetic. Pericarditis, both acute and chronic, has been found as the determining factor in many anæsthetic fatalities.
Febrile patients absorb anæsthetics very rapidly and therefore go under very quickly. Acute septic cases must not have chloroform or ethyl chloride (see page 155): nitrous oxide and oxygen is ideal, ether the next best. Patients who have suffered from acute infectious disease, especially diphtheria and influenza, may present some weakness of heart muscle for many months after the attack.
Give nitrous oxide and oxygen if possible—failing that, ether. Closed-ether sometimes does very well for the induction stage.
Chloroform is wholly inadmissible.
Kidneys.—Avoid ether in acute or sub-acute nephritis: give it, however, for nephrectomy when the other kidney is sound.
Bladder.—Distending the bladder with lotion often causes reflex inhibition of respiration: if that happens, stop the anæsthetic, give artificial respiration, and ask the surgeon to get on with opening the bladder. Morphia usually arrests temporarily the secretion of urine: it should therefore not be given if chromocystoscopy or catheterisation of the ureters is contemplated.
Prostatectomy cases are often rather broken subjects: give a fairly deep anæsthesia until the shelling out of the prostate is begun: then be careful—the patient is breathing deeply as a rule,[169] and can readily get an overdose. He will inevitably suffer a fair amount of shock: be ready to lower the table at the head end if any serious collapse occurs. Don’t be shy of starting a little artificial respiration even though the natural function is not entirely abolished.
Circumcision usually causes a good deal of laryngeal spasm, especially in children. Don’t try to abolish this by deepening the anæsthesia. You won’t succeed unless you nearly kill the patient. Rub the lips, and if very severe ask the surgeon to stop a minute until the crowing becomes less.
Castration.—Always give ether, or gas-oxygen. Castration and reduction of dislocation are the two commonest causes of reflex syncope under chloroform.
It is usual to avoid anæsthetics during the menstrual period if possible, the nervous system being unlikely to be at its best at that time.
Pregnant patients take no harm from an anæsthetic properly given, but undue cyanosis must be avoided or abortion may occur. The pains of labour may be alleviated by chloroform given to an early second stage only, or by “twilight sleep” (see page 44). For the major operations of obstetrics, however, ether has its usual advantages, provided no bronchitis be present. The shock of such operations as a difficult version is considerable, and quite sufficient to call for ether rather than chloroform.
Indication for Local and Spinal Anæsthesia.—The foregoing has been written in reference to inhalational anæsthesia solely. Mr Wood has indicated in chapters XX. and XXI. the class of case in which the methods he describes are to be preferred.
[170]
By the term local anæsthesia, or more correctly local analgesia, is meant the loss of sensibility to painful stimuli without loss of general consciousness. It may be induced in a considerable number of ways, but for practical purposes there are only four methods of value:—(1) by infiltration of the tissues to be operated upon by a solution of the drug, (2) by injecting the solution into or around the nerve trunks supplying the part, (3) by painting the solution on a mucous surface, and (4) by the application of intense cold. The last method has only a limited application. The method of injecting the anæsthetic into the blood vessels of the part is still in the experimental stage and is not to be recommended for general use.
It is advisable first to consider the behaviour of the principal drugs which are employed.
This was the first drug to be widely used for the production of local anæsthesia. It is an alkaloid occurring in the leaves of Erythroxylon Coca. It is only slightly soluble in water—about 1 in 1300, but the hydrochloride of cocaine is freely soluble, and it is this salt that is commonly used for aqueous solutions. The solutions do not keep well, and should be made up shortly before being used. The drug is decomposed by boiling.
Action.—When a solution of cocaine is injected into the tissues, the sensory nerve endings become anæsthetic over the area into which the drug penetrates, direct paralysis of the nerve[171] terminals being produced. When it is injected into or around a nerve trunk it blocks the transmission of nerve impulses. When it is applied locally to a mucous membrane, it produces, besides a loss of sensation, a feeling of constriction and a distinct pallor and contraction of the vessels, which point to a local action on the vessel walls. The drug is very frequently applied to the eye. There it produces not only local anæsthesia, but also contraction of the conjunctival vessels, and this is followed by dilatation of the pupil and often by partial loss of the power of accommodation.
Cocaine Poisoning.—Certain patients show an idiosyncrasy to the action of cocaine, and the greatest care must be exercised in its use. Absorption of small quantities usually causes mental excitement. The patient becomes restless and garrulous, and a feeling of happiness may be produced, but in other cases the patient becomes anxious and confused. In some patients a small dose is followed by a calm languorous state, resembling that produced by morphia, but with less tendency to sleep. The pulse is accelerated, the respiration is quick and deep, and the pupils are dilated. When poisonous doses have been administered, the heart becomes extremely accelerated, powerful tonic or clonic convulsions supervene, the breathing becomes rapid and shallow, and may be finally arrested during a convulsion. In some cases a different set of symptoms are observed, fainting and collapse occur, and convulsive seizures are almost entirely absent. The heart is slow and and weak, the respirations are slow and shallow, the skin is cyanotic and cold, and death takes place from gradual arrest of respiration.
Treatment.—The treatment consists in endeavouring to encourage the action of the heart by every possible means. The patient is placed flat on his back, if he is not already in this position, hypodermic injections of ether and strychnine are administered, and hot coffee given by the mouth; warmth is of[172] great importance. Artificial respiration is commenced if respiration begins to fail. There is no specific antidote to cocaine.
Dosage.—The maximum dose of cocaine that can be given with safety is 3/4 of a grain. The amount of solution that may be employed depends upon the strength. To make a 1 per cent solution, 1 gr. of cocaine hydrochloride is dissolved in 110 minims of distilled water or half strength normal saline; from these proportions the amount of cocaine in a given solution can be calculated. It will be seen that the amount of cocaine solution, even with strengths as weak as ½ or ¼ per cent, that can be used with safety is small and insufficient to anæsthetise an area of any great extent. Owing to its toxicity cocaine has largely fallen out of use for the production of infiltration or regional anæsthesia, though it is still widely used in ophthalmic surgery and in the surgery of the ear, nose and throat.
This drug is immensely superior to cocaine for ordinary surgical purposes. It is the hydrochloride of a synthetic base, its chemical formula being C13H20N2O2, HCl. It is soluble in water 1 in 1, and can be heated to 120°C without decomposition. Its solutions possess slight antiseptic properties, and are capable of repeated boiling without affecting their strength. They may be kept for several months without suffering any change in their action, a quality not possessed by any other anæsthetic agent.
The toxicity of novocaine is one-fifth or one-seventh of that of cocaine. When used in conjunction with adrenalin, its anæsthetic activity is equal to that of cocaine. When injected into the tissues it produces no irritant effects like certain other local anæsthetics, notably stovaine. For the production of local anæsthesia it is used in ½ per cent. solution with the addition of three or four minims of 1 in 1000 solution of adrenalin chloride to each ounce.[173] Several ounces of this preparation may be used with the greatest safety.
Allen makes the following statement regarding this drug:—“After a rather extended experience, including a large number of cases embracing the entire field of surgery, in which this agent has been almost exclusively used, we have failed to note a single case in which there has been any unpleasant local or constitutional action. We, therefore, feel thoroughly justified in unqualifiedly recommending it as the safest, most reliable, and satisfactory of any local anæsthetic agent yet introduced.”
This drug was first isolated from the leaves of the coca plant of Java, but is now prepared synthetically. Its formula is C15H19NO2. Its action is exactly the same as that of cocaine, except that it is one-half as toxic and the duration of anæsthesia is shorter. The hydrochloride is freely soluble in water, and can be boiled without fear of decomposition. It is the agent which is most suitable for spinal anæsthesia, as fewer unpleasant effects have followed its use than that of any other drug.
Stovaine is the hydrochloride of a synthetic compound of the benzoyl group. It occurs as a white crystalline powder, soluble in water, 1 in 14. Its solutions withstand boiling, but are decomposed when heated to 120°C. Its action is the same as that of cocaine, except that it is slightly less toxic and less powerful. It has a distinct irritant effect locally. When injected in dilute solution, it produces a slight burning pain before anæsthesia appears, and very often a distinct inflammatory reaction persists for some time after the operation. It is therefore unsuited for local anæsthesia. It has been widely used for the production of spinal anæsthesia, especially by the French school, but since its injurious effects on[174] nerve tissues have become more apparent, it has been less used than formerly.
Eucaine was introduced as a substitute for cocaine, and, before the introduction of novocaine, was extensively used. It has a similar action to cocaine, and although it is less toxic, it is by no means free from danger unless it is used in very dilute solutions. It is a vaso-dilator, and must therefore be used in combination with adrenalin. It can be boiled without undergoing decomposition, and is practically non-irritant. It has been largely superseded by novocaine.
The use of this drug for purposes of local anæsthesia is still in the experimental stage. It is made by adding urea to a solution of quinine in hydrochloric acid. The crystals are soluble in their own weight of water. For the production of local anæsthesia it is used in strengths of ·25 to 1 per cent. It is free from toxic effects, and its solutions can be sterilised by boiling.
The striking feature about this drug is the extraordinary duration of the anæsthesia, this being from one to six days. It has therefore been used by Crile and other American surgeons to prevent pain during the first few days after operation. The great drawback to its use, however, is that it causes a persistent indurated condition of the tissues which interferes with primary union, and which is sometimes followed by actual sloughing. In addition, it is now established that its use has been followed by tetanus in several cases, and it is recommended that a dose of antitetanic serum should be given immediately before or after the injection of quinine.
Although the action of this drug is of great interest, it cannot be recommended at present for ordinary purposes.
[175]
Adrenalin is obtained as an extract from the suprarenal glands of animals. It is a greyish white powder, slightly soluble in water, and readily so in weak acids. The usual preparation is a 1 in 1000 solution of adrenalin chloride in normal saline. It contains ·5 per cent. of chloroform as a preservative. The drawback to the animal extract is that the solution does not keep well, decomposition being indicated by a brownish colour. Of late a synthetic preparation has been introduced, which appears to have the same action, and which can be sterilised by boiling.
The action of the drug is to cause marked vaso-constriction by direct action on the vessel walls. It has no analgesic action, and is used as an addition to solutions of anæsthetic drugs. The advantages of its use are that the action of the anæsthetic is concentrated and prolonged, owing to the delay in absorption, and that the field of operation is rendered practically bloodless. In large doses it may produce toxic symptoms in the form of palpitations and breathlessness, or even actual syncope, so that care is necessary in its use. For purposes of local anæsthesia, it is added to the solution of the anæsthetic drug in the strength of 3 drops to the ounce, and large injections of this dilute solution may be made without risk. At least twenty drops may be safely given.
Local anæsthesia may be induced by the use of anæsthetic drugs in three ways—(1) infiltration anæsthesia, (2) regional anæsthesia, and (3) by application to a mucous surface or to the surface of the eye.
Infiltration Anæsthesia.—In this method anæsthesia is induced by injection of the drug directly into the tissues to be operated upon. This method acts by paralysing the sensory nerve-endings. Although the term anæsthesia is constantly used, it is, strictly speaking, an operative analgesia that is aimed at; it is a[176] paralysis of the pain-conducting fibres, and not of those which conduct purely tactile sensations, the patient being often able to feel the contact of the fingers and instruments during the operation. True anæsthesia can be secured, but it is necessary to use considerably stronger solutions than those that are required for the production of analgesia.
Solution of the Drug.—Novocaine is far superior to any other drug for infiltration anæsthesia. The strength for most purposes is ½ per cent., though some operators find ¼ per cent. quite satisfactory. In specially sensitive parts, such as the nose, throat, or mouth, 1 or even 2 per cent. solutions may be preferable. Sufficient sodium chloride should be added to prevent osmosis of the solution into the tissue cells. The most satisfactory preparation is:—
| Novocaine | 0·25, 0·5, 1 or 2 (¼ to 2 percent.) |
| Normal salt solution (half strength) | 100·0 (·45 per cent. NaCl) |
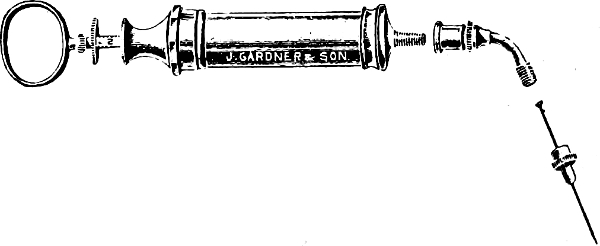
Fig. 51. All-Metal Syringe for Infiltration Anæsthesia.
Adrenalin is added to the solution in the proportion of 3 drops of 1 in 1000 adrenalin chloride to the ounce, and as much as 6 ounces of this preparation may be safely given. The novocaine solution can be boiled before use, but the adrenalin must not be added until after boiling.
For private practice it is sometimes convenient to procure the[177] novocaine in tabloid form of definite strength combined with sodium chloride. These tabloids are added to the necessary amount of water, and the whole boiled. The adrenalin can then be added.
Choice of Syringe.—The best form of syringe for infiltration anæsthesia is the all-metal syringe illustrated in Fig. 51. It ought to have a capacity of at least 10 c.c. The advantage of the all-metal syringe over glass syringes is that it can be safely sterilised by boiling, and does not get broken. Between the syringe and the needle is a metal segment which is curved so that the needle is set at an obtuse angle to the syringe. This renders the infiltration of the tissues at the proper depth much easier. The needles employed are the ordinary hypodermic needles which are sold in small tubes. The sizes which should be selected are 1 inch, and 3 or 3½ inches. The needle fits into a hole in a small metal mount, which screws on to the intermediate metal portion. This section also is attached to the syringe by a screw, and these screw attachments have the advantage of rendering leakage impossible.
Failing the syringe described, a 10 c.c. Record syringe will be found to be quite efficient, if suitable needles can be obtained. The syringe, needles, and glass measure for the solution should be boiled in plain water or normal saline, as soda interferes with the action of the drug.
Technique of Injection.—The needle is introduced into the subcutaneous tissue, and pushed on slowly to its full length, the fluid being injected as the needle advances. The needle is then partly withdrawn, and pushed in in a different direction so as to infiltrate a fresh area. This procedure is repeated, and as wide an area as possible infiltrated from the one puncture. The needle can then be completely withdrawn and introduced at a fresh point which has already been rendered analgesic. The deeper tissues can nearly always be infiltrated from the surface, but if large blood-vessels traverse the region to be infiltrated, it may be necessary to[178] defer the deeper injection until these have been exposed. It is wise to infiltrate wide of the intended line of the incision, since it is not possible to anticipate with certainty the extent of an operation until it has been commenced. The secret of successful anæsthesia is to employ plenty of the solution, and make the injection thorough.
The skin over the area becomes blanched within a few minutes of the injection owing to the action of the adrenalin. Anæsthesia is not usually complete until ten minutes have elapsed, and the operation should not be commenced until it has been made certain by suitable tests that the anæsthesia is complete. The duration of the anæsthesia is usually at least an hour and a half.
It will be seen that the injection in the manner described above is entirely subcutaneous, the pain-conducting nerves from the skin being caught up by the drug as they traverse the superficial fascia in the area infiltrated. This method usually gives complete satisfaction, but some surgeons advise that the infiltration should be commenced with an intra-dermal injection so as to reduce the pain of the needle punctures to a minimum. A fine needle is employed, the prick of which is practically painless. If the skin at the selected point is pinched up between the finger and thumb, and held firmly, this lessens its sensibility. The needle is advanced beneath the epidermis with a quick but light thrust. The injection into the substance of the skin causes a distinct wheal, which stands out from its surroundings like an urticarial wheal. From this starting-point a long needle can be introduced into the deeper tissues without pain. The intra-dermal injection may be carried along the whole length of the area to be infiltrated, each fresh puncture being made in the margin of the wheal-like area already anæsthetised.
Precautions.—The most careful asepsis is essential throughout. Infiltration with novocaine causes no interference with the healing[179] of the wound, and although cases of sloughing of the tissues have been reported after its use, these are almost certainly due to infection of the wound. Care must be exercised also to avoid injecting the drug into a vein. When this accident takes place, the drug is carried at once into the general circulation, and may reach the higher nerve centres in such quantity as to produce serious toxic results. The use of adrenalin calls for special care and thoroughness in securing all bleeding-points, as, after the effect of the adrenalin passes off, even a slight ooze may increase and give rise to a hæmatoma which may jeopardise the healing of the wound.
In this method of producing anæsthesia, the sensory nerve paths are blocked by injecting the anæsthetic drug into, or around, a nerve trunk. By this procedure complete anæsthesia is produced in the area of distribution of the nerve, and the effect corresponds to a temporary physiological section of the nerve trunk. A temporary motor paralysis is also produced in a mixed nerve.
Technique.—The solution of the drug must be stronger than that employed for infiltration anæsthesia. A 2 per cent. solution of novocaine in half-strength normal saline with the addition of adrenalin is employed. The injection may be paraneural or intraneural.
A paraneural injection is made by passing a needle through the tissues to the known position of a nerve trunk and injecting the anæsthetic around it. The solution gradually diffuses into the nerve tissue, and anæsthesia of the nerve is produced. This method is open to the objection that unless the anæsthetic is accurately placed, no anæsthesia will result, and that in the case of certain nerves there is considerable risk of making the injection into a vein. The latter risk can be avoided by using a glassbarrelled[180] syringe and applying a little suction before the injection is made; if a vein has been pierced, blood will enter the syringe.
The intraneural method is more accurate but requires the expenditure of considerable additional time and trouble, and is only employed where other methods of anæsthesia are not feasible. The tissue over the nerve having been infiltrated, the nerve is exposed by open dissection. It must not be pinched by forceps or other instruments, as such manipulations cause severe pain referred to its peripheral distribution. The injection should be made with the nerve lying in its bed by inserting a fine needle in the long axis of the nerve, first into the sheath, which is infiltrated, and then into the nerve itself. The infiltration of the nerve is continued until it presents a fusiform swelling and this may require from 5 to 15 minims of the solution. Complete anæsthesia of its entire distribution usually results in from five to ten minutes.
A third method of inducing regional anæsthesia—first recommended by Hackenbruch—which is worth mention, is by the production of a ring of infiltration around a peripheral part, such as a finger, or around and underneath a tumour. By this means the nerve fibres are caught up by the anæsthetic and their conductivity interrupted as they enter the area to be operated upon. In dealing with such conditions as a large lipoma, or an umbilical hernia, it may be possible to avoid the use of an excessive amount of anæsthetic solution by employing this method.
It is sometimes stated that local anæsthesia should be limited to small and superficial operations, but with a knowledge of anatomy and of the correct technique, there are few operations which the surgeon cannot undertake with this form of anæsthesia. If we remember that the mortality from the anæsthetic is practically nil, it is obvious that it is often the duty of the operator to[181] give the patient the choice of local anæsthesia. In urgent conditions in which the administration of a general anæsthetic would be attended with great danger, it is often a life-saving measure. Either infiltration or regional anæsthesia may be used alone; in some cases it is convenient to combine the two methods.
Regional anæsthesia is sometimes employed in operations on the upper extremity in conditions, such as diabetic gangrene or advanced cardiac disease, where a general anæsthetic is contra-indicated. In similar conditions in the lower extremity, spinal anæsthesia is usually preferred, though it is quite possible to anæsthetise the lower limb by blocking the sciatic, femoral, and lateral cutaneous nerves with a local anæsthetic. Crile lays great stress on the blocking of nerves with a local anæsthetic during operations on the limbs as a means of preventing shock, even where a general anæsthetic is being employed. The effect of the local anæsthetic is to prevent the impulses which produce shock from passing up to the higher centres. Only those methods which are applied to the upper extremity need special description.
Anæsthesia of the Whole Arm.—The nerves of the upper extremity are all derived from the brachial plexus except the intercosto-brachial. This nerve, which is the lateral cutaneous branch of the second intercostal, crosses the axilla and pierces the deep fascia on the medial side of the arm. It supplies the skin on the dorsal part of the medial aspect of the upper arm. The lateral cutaneous branch of the third intercostal nerve sometimes crosses the axilla also, and reaches the medial side of the arm. Injection of the brachial plexus produces complete analgesia of the shoulder and entire arm, and is particularly suited to high amputations and disarticulations at the shoulder. If the area supplied by the intercosto-brachial is encroached upon, this can be anæsthetised[182] by infiltration with a few drams of solution injected subcutaneously along the floor of the axilla from its lateral and posterior borders.
Method.—The injection may be intraneural or paraneural. The intraneural is made after exposing the plexus by an incision under infiltration anæsthesia from the junction of the middle and lower thirds of the sterno-mastoid to the union of the middle and lateral thirds of the clavicle. It is found lying on the scalenus medius and each of its branches is separately injected with a few drops of 5 per cent. solution of novocaine containing a few drops of adrenalin to the ounce.
The paraneural injection is less satisfactory, since the nerves are too large to be readily penetrated in effective quantities by the anæsthetic solution, and since there are numerous veins in the neighbourhood into which the solution may be accidentally injected with dangerous results.
The injection is usually made above the clavicle. In this region the plexus lies mainly above and to the lateral side of the third part of the subclavian artery, the lowest trunk lying directly behind the vessel as it rests on the first rib. The position of the artery is first localised with the finger by its pulsations, and the skin and subcutaneous tissue infiltrated immediately above the mid-point of the clavicle. From this point a long fine needle, unattached to the syringe, is passed downwards, backwards, and medially in the direction of the second or third thoracic spine. The distance to which the needle penetrates varies from 2 to 4 c.m. When the plexus is reached a slight radiating pain is felt down the distribution of the radial or median nerve. At this point the needle is held stationary, the syringe attached, and the injection made. The reason for not attaching the syringe earlier is that should the artery be entered, blood will flow. This accident is of little consequence, the needle being withdrawn slightly and introduced a little more laterally. About 10 c.c. of a 2 per cent.[183] solution of novocaine and adrenalin is injected; the needle is then slightly withdrawn and a further 10 c.c. injected in the neighbourhood. Anæsthesia occurs in from three to fifteen minutes.
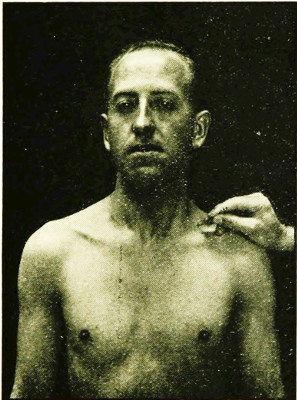
Fig. 52.—Point at which the needle is introduced in paraneural injection of brachial plexus.
The individual nerves of the upper limb can be readily injected. The median can be exposed at the bend of the elbow for an intraneural injection, or a needle may be passed under the tendon of the palmaris longus at the wrist for a paraneural injection. The ulnar can be easily reached as it lies on the posterior aspect of the medial epicondyle of the humerus for a paraneural or intraneural injection. The superficial radial can be reached for a paraneural[184] injection about two inches above the wrist to the lateral side of the tendon of the brachio-radialis (supinator longus). The injection is made into the deep fascia, and carried across the lateral border of the forearm for about an inch, to ensure reaching all the branches of the nerve.
The medial antibrachial (internal) cutaneous can be blocked on the front of elbow by a paraneural injection about half an inch medial to the biceps tendon, and the lateral antibrachial cutaneous (musculo-cutaneous) at a corresponding point on the other side of the tendon.
Anæsthesia of the Arm below the Elbow.—In operations below the elbow, in conditions in which a general anæsthetic is not permissible, as in diabetes, nephritis or advanced cardiac disease, a full anæsthesia can be obtained by intraneural injection of the median, ulnar, and radial (musculo-spiral) nerves, combined with paraneural injection of the medial and lateral antibrachial cutaneous. The median and radial are each exposed by an incision under infiltration anæsthesia, the radial being exposed in the groove between the brachialis and brachio-radialis. The infiltration to expose the median nerve usually blocks the anterior branch of the medial antibrachial cutaneous. To make certain that the posterior branch is also anæsthetised, it is advisable to inject a little anæsthetic solution over the front of the medial epicondyle. The intraneural injection into the ulnar nerve can often be made without exposing it.
Anæsthesia of Finger.—The paraneural method applied to the digital nerves at the root of the finger gives perfect results. A circle of anæsthetic solution is first injected round the root of the finger. The needle is then passed through the infiltrated skin on each side of the finger, and a few drops of ½ per cent. novocaine solution injected around the nerves. Complete anæsthesia of the finger results in a few minutes.
[185]
In the Lower Limb injection of individual nerves is rarely employed, as anæsthesia is easily obtained by the method of spinal analgesia. The lateral cutaneous can be injected as it lies immediately medial to the anterior superior iliac spine emerging from under cover of the inguinal ligament. This procedure may be useful in obtaining skin grafts, the grafts being taken from the antero-lateral aspect of the thigh. Amputations in the middle third of the thigh have been performed by injecting the sciatic, the posterior cutaneous (small sciatic), the femoral (anterior crural), and the lateral cutaneous at the root of the limb. The obturator nerve is difficult to find and anæsthetise in such cases. Operations below the knee can be painlessly performed by this method of anæsthesia.
Tracheotomy.—This operation is conveniently and safely performed under infiltration anæsthesia. The anæsthetic solution is injected in the usual way in the line of the incision down to the trachea but not into it, as the trachea itself is insensitive to pain.
Goitre.—A parenchymatous or adenomatous goitre can be readily removed under local anæsthesia, though the administration of ether by intra-tracheal insufflation is usually to be preferred. The principal nerve supply to the field of operation is derived from the cervical plexus, whose branches become superficial about the middle of the posterior border of the sterno-mastoid. An intradermal injection may be made first at this point, and a longer needle then passed down to the posterior border of the muscle, and an area of infiltration produced. From this point the needle is directed first upwards and then downwards round the margin of the goitre so as to produce a zone of infiltration. The same procedure may be repeated on the opposite side, so that the whole gland is surrounded with a zone of infiltration with a special depot of solution around the branches of the cervical plexus. Where only one lobe is involved, it is sufficient to carry the injection down[186] in the middle line after one side has been encircled. When the sheath has been incised and the surface of the gland exposed, the isthmus is infiltrated and divided. The affected half of the gland is then rolled outwards, and the attachments between the posterior aspect of the gland and the larynx and trachea are infiltrated, special attention being paid to the upper pole. The rest of the operation can then be carried out painlessly.
Exophthalmic Goitre may also be operated upon under local anæsthesia after a preliminary hypodermic injection of morphia and scopolamin, though many operators prefer a general anæsthetic on account of the nervous state of the patient. In bad cases a procedure which is often of great value is ligature of the superior thyroid artery on both sides under local anæsthesia. After ligature of the vessels a colloid degeneration takes place in the gland, and the symptoms of hyperthyroidism subside. After a delay of two or three months it may be possible to carry out the radical operation with little or no danger. The incision is two and a half inches in length, and crosses transversely the central part of the thyroid cartilage. The line of the incision is infiltrated with novocain solution in the ordinary way, and both superior thyroid arteries exposed and ligatured.
The greater part of the wall of the thorax is supplied by the intercostal nerves. In front the supraclavicular nerves come down as far as the second intercostal space or sometimes as far as the nipple, and the lateral and medial anterior thoracic nerves supply the pectoral muscles, sending a few twigs to the overlying skin. The long thoracic nerve extends down the side of the chest, supplying the serratus anterior. The intercostal nerves can be blocked in the region of the angles of the ribs and the supraclavicular by carrying a line of infiltration along the clavicle. The anterior thoracic can be blocked by deeper injections. In[187] this way the greater part of the chest wall and the pleura can be anæsthetised.
Acute Empyema.—This operation should always be performed under local anæsthesia. Exhaustion from septic absorption and from the antecedent pneumonia or other disease, with the dyspnœa from the pressure of the pus on the lung may render a general anæsthetic highly dangerous. The method of producing local anæsthesia is simple and easily carried out. A point is selected on the rib which is to be resected a short distance behind the line of the incision and an intra-dermal injection made with a fine needle. A long needle is then substituted and passed down to the upper border of the rib until it reaches the plane between the external and internal intercostal muscle, the injection being continued lightly as it advances. When the desired point is reached one or two drams of the solution are injected. The needle is then slightly withdrawn and passed to the lower border of the rib to reach the same plane and the same procedure carried out. The infiltration is then carried along the line of the incision or it may be made to pass obliquely upwards to the rib above and obliquely downwards to the rib below so as to catch up the nerves coming from behind into the area of operation. The anæsthesia of soft parts, bone, and pleura is perfect after the above injection.
The anterior abdominal wall, including the anterior parietal peritoneum, is supplied by the lower six intercostal nerves, the last thoracic nerve, and the ilio-hypogastric and ilio-inguinal nerves from the first lumbar. It is a very interesting and important fact that, although the parietal peritoneum is exceedingly sensitive to touch and pain, the visceral peritoneum and the viscera themselves are insensitive. When operations are performed under local anæsthesia of the abdominal wall, the[188] viscera can be freely handled or incised without the patient experiencing the slightest discomfort, provided that the parietal peritoneum is not put upon the stretch by traction on the mesentery or other peritoneal attachment. Thus the colon can be opened twenty-four or forty-eight hours after being brought outside the abdominal wall without any anæsthetic in the operation of colostomy. Local anæsthesia is therefore well adapted to cases in which a small amount of manipulation of the viscera is required, and where a general anæsthetic would be dangerous, as in grave cases of intestinal obstruction and in cases of carcinoma of the œsophagus with weakness and loss of flesh from starvation.
Gastrostomy.—This operation is commonly performed under local anæsthesia and may be taken as an illustration of the procedure employed. The incision is made through the middle of the left rectus and is about two and a half or three inches long, beginning about an inch below the costal margin. An intradermal wheal is established at the middle of the proposed incision. A long needle is entered at this point and passed first upwards and then downwards in the line of the incision, infiltrating the subcutaneous fat as it goes. The needle is then passed in through the anterior wall of the rectus sheath, this being easily recognised as a plane of decided resistance. The needle is advanced a little inside the sheath, the injection being continued as it advances. The same procedure is repeated at various points along the line of the incision. The extra-peritoneal fat may be infiltrated in the same way, the posterior wall of the sheath being identified as a deeper plane of resistance and gently pierced. This step may be deferred until the posterior wall of the sheath has been exposed. The infiltration may be completed by forming a line of intradermal infiltration along the line of incision, though this last step can often be omitted.
The abdomen can then be opened painlessly. The only step in[189] the operation which may cause a little discomfort is the traction which may be necessary to bring the shrunken stomach down from under cover of the ribs. The incision into the stomach is quite painless.
Gastro-enterostomy can be performed under local anæsthesia, the only special step required being infiltration of the meso-colon before it is perforated.
Appendicectomy is not suitable, as a rule, for local anæsthesia. If the cæcum is fixed or the appendix bound down by adhesions, the traction necessary to bring the appendix to the surface causes considerable pain.
In Acute Obstruction, when the procedure of enterostomy has been decided upon owing to the gravity of the patient’s condition, local anæsthesia is often of great value. The abdominal wall is infiltrated in the manner described, and a distended loop of bowel brought to the surface and sutured to the parietal peritoneum. A Paul’s tube can then be introduced.
Inguinal Hernia. Local anæsthesia is specially suited to cases of strangulated hernia, but it may be employed in the ordinary case. It should be pointed out that spinal anæsthesia gives equally good results and is less troublesome to carry out.
The injection is commenced with a fine needle a little beyond the lateral end of the proposed incision. An intradermal wheal is produced at this point, a long needle introduced into the subcutaneous tissue, and about half-an-ounce of anæsthetic solution injected in this position. The needle is then passed downwards and medially, and the subcutaneous fat infiltrated in the line of the incision. The needle is then partly withdrawn and again advanced until it reaches the resistance of the aponeurosis of the external oblique. This is gently pierced and about half-an-ounce of solution injected underneath so as to block the ilio-hypogastric and ilio-inguinal nerves. In most cases this is all that is necessary.[190] As additional precautions the line of incision may be infiltrated intradermally, and an injection may be made around the neck of the sac after it is exposed.
Femoral Hernia.—A femoral hernia may be anæsthetised by infiltration along the line of the incision, or by injecting around the circumference of the hernia after the method of Hackenbruch. After the sac has been exposed and defined, it is necessary to inject some novocaine solution around the neck, care being taken to avoid the femoral vein which lies on the lateral side.
Umbilical Hernia.—Local anæsthesia is sometimes of great value in dealing with umbilical hernia, especially if it is strangulated, in stout patients who are bad subjects for a general anæsthetic. The injection is best made around the circumference of the hernia. Several intradermal injections are made at points around the swelling, and through these the long needle can be introduced and the deeper tissues infiltrated. If the muscles are fairly well defined and can be felt, they may be infiltrated at the commencement, but it may be advisable in fat subjects to inject only the subcutaneous tissues to begin with, and to delay the injection of the muscles and extra-peritoneal fat until the sac has been opened and a protecting finger can be introduced to guard the intestines. Omental adhesions can be divided without causing pain. If the intestines are extensively adherent to the sac it is better to infiltrate the points of adhesion, as extensive manipulation may cause cramp-like pains.
After the circumferential injection has been made in these cases, it is best to wait for ten or fifteen minutes before making the incision in order to allow the anæsthetic solution to diffuse.
Suprapubic Cystotomy.—In operations for drainage of the bladder local anæsthesia is highly successful. The skin and subcutaneous tissues are infiltrated in the line of the incision. The needle is then carried between or through the recti muscles and[191] several drams injected into the layer of fat in front of the bladder. It is unnecessary to inject the wall of the bladder itself.
Hæmorrhoids.—In patients in whom there is some contra-indication to the use of a general anæsthetic the removal of hæmorrhoids can be carried out quite safely and painlessly under local anæsthesia. A circumferential injection is first carried out round the muco-cutaneous junction. It is best to start the infiltration about an inch out from the anus as the skin immediately around the anal orifice is extremely sensitive. The infiltration is made subcutaneously, and each re-insertion of the needle is made just short of where the previous injection stopped. When the circumferential injection has been completed, a finger is passed into the rectum, and the long needle introduced through the anæsthetised area, injecting as it advances, to a depth of about 2½ inches, keeping just outside the sphincters. Four such injections are made, one on each side of the bowel, one in front and one behind, from 5 to 10 c.c. being injected in each position.
Anæsthesia results almost immediately and the anal canal can be readily dilated.
The Tongue.—For the Whitehead operation of removal of one half of the tongue, complete anæsthesia can be obtained by the infiltration method. A long needle is introduced at the tip of the tongue, and the injection carried in the middle line to a point behind the tumour. The mucous membrane of the floor of the mouth and the glosso-palatine fold are infiltrated, and a last injection made across the affected half of the tongue well behind the tumour.
The tongue can be anæsthetised also by blocking the lingual nerve with a paraneural injection. The nerve lies under the mucous membrane of the mouth opposite the last molar tooth. If the tongue is drawn well over to the opposite side, the nerve can be felt and the injection made around it. The only drawback[192] to this method is that it does not anæsthetise the posterior third, which is supplied by the glosso-pharyngeal nerve.
Operations on the Skull and Brain can be readily performed by infiltration of the scalp. In the later stages of the recent war, a large proportion of operations on the skull and brain were performed under local anæsthesia. The brain itself is insensitive to touch and painful stimuli, and infiltration of the scalp is all that is necessary. A 1 per cent. solution of novocaine with adrenalin has been commonly employed, and is injected into the subaponeurotic space so as to surround the field of operation with a wall of anæsthetic solution—the method of Hackenbruch. The advantages are that hæmorrhage is reduced to a minimum, and the head can be conveniently and safely elevated and the intra-cranial tension thus reduced.
For Operations on the Eye.—Analgesia is obtained by the instillation of a few drops of a 4 per cent. solution into the conjunctival sac. This is repeated two or three times, and analgesia is obtained in five or ten minutes. It may be necessary to repeat the instillation during the course of the operation.
For Operations on the Nose, Pharynx, or Larynx cocaine is commonly used. A 5 or 10 per cent. solution is employed and is merely painted on the surface. Care must be taken that such strong solutions are not swallowed.
[193]
Spinal Anæsthesia or Analgesia, consists in the production of analgesia in the lower extremities and in the lower part of the trunk by the injection into the subarachnoid space of an anæsthetic drug which blocks the spinal nerves as they enter and leave the spinal cord. The cord ends at the lower border of the first lumbar vertebra and the subarachnoid space at the second sacral vertebra so that there is a considerable area into which the injection may be made without risk of injury to the cord. It is, in reality, a special variety of regional analgesia, the anæsthetic being injected into that part of the subarachnoid space which is occupied by the cauda equina. The subarachnoid space of the medulla spinalis contains the cerebro-spinal fluid and communicates above with the subarachnoid space inside the skull and through the foramen of Magendie, with the ventricular system of the brain. The subdural space of the medulla spinalis is merely a capillary interval. At the upper end of the cauda equina the nerve trunks of the two sides are separated by a median interval—containing only the filum terminale—which has been termed the cysterna terminalis. It is into this median space that the injection is made, in order to avoid wounding the nerve trunks and to procure equal diffusion of the anæsthetic to both sides of the middle line. If the injection is made among the nerve trunks on one side, a unilateral anæsthesia may result, the drug being prevented from diffusing freely to the other side by the presence of the numerous nerves.
[194]
The ligamentum denticulatum forms an imperfect scalloped septum between the posterior and the anterior nerve roots, passing from the surface of the cord to the dura mater. The presence of this septum probably explains the fact that the motor nerves are not affected with the same constancy and to the same extent as the sensory roots.
The drug which is most commonly employed in the Edinburgh school is Tropacocaine, and the results of its use with proper technique are eminently satisfactory. The dose of the drug for most purposes is ·07 gramme. Smaller doses are sometimes used but the larger dose gives more constant anæsthesia and appears to be well within the limits of safety. The dose is dissolved in 1 c.cm. of distilled water and sufficient sodium chloride added to make a solution isotonic with the cerebro-spinal fluid. A convenient method of obtaining the drug is in glass ampoules, each ampoule containing one dose, which has been carefully sterilised.
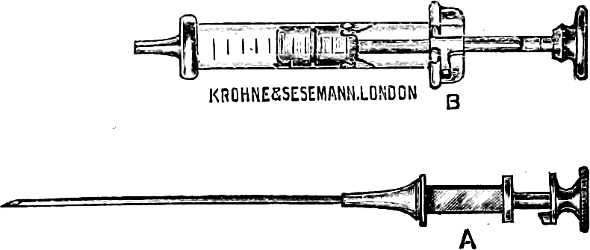
Fig. 53.—Needle and syringe for spinal analgesia. Note the short oblique character of the point of the needle.
The syringe and needle employed are illustrated in Fig. 53.
The point of the needle must be sharp but short. If a needle with a long slender point is employed, only part of the point may enter the membranes; a free flow of cerebro-spinal fluid may then take place, but when the injection is made part of the anæsthetic solution escapes outside the membranes. The needle[195] should he 3½ to 4 inches long and 1 m.m. in diameter. A stylet fits inside the needle and prevents it from becoming blocked during the introduction. To prevent the possibility of rusting, both needle and stylet should consist of hard nickel. The barrel of the syringe must consist of glass so that the appearance of the cerebro-spinal fluid can be seen. The Record type is very satisfactory. The syringe usually supplied for spinal analgesia has a capacity of 2 or 3 c.cm., but one holding 10 c.cm. is more useful. Syringe and needle must be carefully sterilised by boiling in plain water; any trace of soda causes decomposition of the drug. The ampoule containing the tropococaine is sterilised in a strong antiseptic solution so as to avoid the possibility of contamination of the hands when the drug is being transferred to the syringe.
Method of Injection.—The patient should be given a hypodermic injection of ⅛ gr. of morphine and ¹⁄₁₅₀ gr. of scopolamine an hour before the operation. There are a number of minor variations in the method of making the spinal injection, but limitations of space forbid a discussion of theoretical questions and of the relative merits of the different procedures. Only one method, which has been found safe and reliable, will be considered here. The injection is made in the space between the third and fourth lumbar spines, the objective being the mid-line of the subarachnoid space between the two divisions of the cauda equina. The position of the patient is such that the spaces between the lumbar spines are opened up as widely as possible. The most convenient plan is to have the patient sitting on the table with the head and shoulders bent well forward (see Fig. 54.) If the patient is unable to sit up, the injection may be made with him lying on his side, with the knees drawn up and the shoulders bent forward.

Fig. 54. Position for the injection. The cross indicates the point at which the lumbar puncture is made—about half an inch from the median plane and in the space between the third and fourth lumbar spines.
The skin of the back is carefully sterilised; painting with tincture of iodine serves admirably. The ampoule containing the[196] tropacocaine is opened, and the drug sucked into the syringe through a spare cannula. The loaded syringe is then placed on a sterile towel at the back of the patient. With a little practice there is no difficulty in making the lumbar puncture. The fourth lumbar spine is located by noting the level of the highest point on the iliac crest—this may be indicated by an assistant. A line joining the highest points on the two iliac crests will pass through the tip of the fourth lumbar spine. When this process has been carefully identified, the needle is introduced half-an-inch to one side of the median plane and midway between the third and fourth spine. Some surgeons prefer to go in exactly in the middle line to make sure of entering the middle of the subarachnoid space, but in[197] this position the tough supra-spinous and interspinous ligaments are met with, and to avoid the resistance of these it is best to keep a short distance out from the median plane. By carefully noting the direction of the needle, the cysterna terminalis can always be entered. The needle is passed forwards, very slightly upwards, and slightly medially so as to hit off the centre of the subarachnoid space. As the needle passes through the ligamentum flavum, there is a sudden diminution of resistance and immediately afterwards the point of the needle lies in the subarachnoid space. The passage of the needle through the membranes is sometimes accompanied by a slight pricking pain.
The stylet is withdrawn at this stage and the cerebro-spinal fluid usually trickles out drop by drop. The syringe is picked up, carefully emptied of air bubbles, and fitted on to the needle. The piston is withdrawn until the syringe is filled with cerebro-spinal fluid, which mixes freely with the anæsthetic solution, and the contents then slowly injected. The 10 c.cm. syringe is to be preferred for this purpose as it is essential to mix the tropacocaine thoroughly with the cerebro-spinal fluid. If the smaller syringe is used, it should be refilled with cerebro-spinal fluid and emptied a second time so as to ensure thorough diffusion of the drug. The needle is then withdrawn and the puncture sealed with collodion.
The injection should never be made until a free flow of cerebro-spinal fluid is obtained, since this is the only certain indication that the needle has entered the subarachnoid space. If failure is met with in the space between the third and fourth spines, the interspinous space above or below should be tried.
After the injection has been completed the patient is placed flat on his back and then lowered into the Trendelenburg position. Analgesia appears first in the scrotum and perineum, extends down the medial side of the leg to the foot, then appears on the front of the leg, and travels up to the groin and the lower part of the abdomen. The progress of the analgesia is tested from[198] time to time by lightly pinching or pricking the skin, the patient’s eyes being screened. When the analgesia reaches the level of the nipples, the patient is raised into the horizontal position and the the operation may be commenced. Some surgeons object to the lowering of the head as rendering paralysis of the respiratory centre from upward diffusion of the drug more likely. If tropacocaine is used in the dosage indicated and the table elevated when the anæsthesia reaches the nipple line, there seems to be little risk of this complication. If analgesia is only desired in the lower extremity, the lowering of the table may be omitted; but if a good anæsthesia is desired above the level of the groin, it should always be carried out.
Analgesia is complete in five or ten minutes as a rule. The duration varies from three-quarters of an hour to an hour and a half. If a preliminary hypodermic injection of morphine and scopolamine has been given, the patient lies quietly and patiently until the operation is completed. In some cases the patient actually drops off to sleep from the effects of the morphine. It is not uncommon to observe a temporary nausea and faintness about fifteen or twenty minutes after the injection has been made, and it is good practice to give the patient a little brandy and water at this stage.
A great deal has been written in the past with regard to unpleasant results of spinal analgesia, but most of these would appear to have been the result of faulty technique or of the use of an impure or irritating drug. When tropacocaine is used in the manner described, the usual result is that, except for occasional nausea and faintness at the commencement, the patient has a comfortable, painless operation, and a recovery which is unmarred by the sickness and other distressing symptoms which are so common after general anæsthesia.
Deaths have been recorded, and these have been ascribed to[199] the drug having travelled too high and brought about paralysis of the respiratory centre in the medulla oblongata. Too much importance has probably been ascribed to these fatal cases. They have been most common in patients greatly enfeebled by shock, old age, or debilitating illness, who are liable to die during the operation whatever anæsthetic is used. Thousands of cases have been recorded without a death, and in the hands of surgeons of skill and judgment fatal cases are almost unknown.
An occasional complication is severe headache which may persist for a week or longer. Other complications are all exceedingly rare; paralysis of the lateral rectus muscle of the eyeball or of other ocular muscles has been recorded, and is probably due to toxic bye-products which are the result of impurity of the drug. Persistent nausea and paralysis of the bladder and rectum and even of the lower extremities have also been recorded, but are to be regarded as the greatest rareties, and probably due to impurity of the anæsthetic.
Spinal analgesia may be used for any operation at or below the level of the umbilicus. Excellent anæsthesia is obtained for the operation for radical cure of umbilical hernia, but anæsthesia above this level is not so constant, and is regarded by many authorities as unsafe.
The procedure is of special value in cases in which a general anæsthetic is unsafe:—(1) In old enfeebled patients suffering from strangulated hernia, enlarged prostate, disease of the female pelvic organs, and other conditions where anæsthesia is necessary below the umbilicus. (2) In patients who are already suffering, or who are likely to suffer, from severe shock. The drug has the same effect on the nerve trunks of the cauda equina as on the peripheral nerves—it causes blocking of the centripetal sensory impulses which are such a potent factor in the causation of shock.
[200]
(3) In diabetic gangrene spinal analgesia is the safest form of anæsthesia to employ.
Children up to the age of fourteen or so are apt to be frightened, and spinal analgesia is better avoided except in special cases. It is contra-indicated also in septic conditions on account of the possibility of septic meningitis resulting from metastasis of the infection, the drug having possibly the action of lowering the vitality of the cord and meninges. In tuberculosis and syphilis it is better avoided for the same reason. It should not be used where organic disease of the spinal cord or brain is already present.
A transient analgesia can be produced by freezing the skin. An ether spray was formerly employed, but was found to be troublesome and inconvenient. The most convenient procedure consists in freezing the part by means of a spray of ethyl chloride. This drug is supplied in a glass cylinder with a very fine outlet so that it breaks up into a fine spray as it escapes. The cylinder is held about 8 or 10 inches from the patient’s skin, and pressure applied with the thumb to a stopcock on the neck of the cylinder. Under the influence of the heat of the hand the liquid escapes in a fine jet which impinges on the patient’s skin. Freezing takes place in a few seconds, the frozen patch becoming hard and white. The freezing can be hastened by blowing on the skin.
This method is only suitable for the opening of small abscesses and other procedures requiring a very short anæsthesia. The anæsthesia is very imperfect, and only lasts for a few seconds. Many patients appear to have as much pain with this form of anæsthesia as without it.
[201]
The apparatus was very simple. It consisted of a pump which would propel air towards the ether bottle; a glass bottle containing ether, the roof of which was pierced by two tubes, one of which carried the air from pump to bottle, and the other from bottle to a Waller’s tube, where it was collected. The percentage of ether in the air was then estimated by Waller’s gravimetric method. The ether jar stood in a water bath which could be either left otherwise empty or filled up with water of known temperature. The following tables show some of the results. In each case, the air was propelled for five minutes, by which time the cooling effect upon the ether was very marked; the figures given are averages taken from several observations.
TABLE A.
Air Blowing over Surface of Ether.
| Temperature of Bath (Fahr.) before experiment. | Quantity of ether before experiment. | Rate of pump. | Temperature of ether (Fahr.) at end of experiment. | Percentage obtained. |
| 75 | 100 c.c. | 30 | 50 F. | 12·7 |
| 85 | 100 c.c. | 30 | 52 F. | 12·8 |
| 75 | 100 c.c. | 90 | 45 F. | 8·7 |
| 85 | 100 c.c. | 90 | 45 F. | 8·8 |
| No water in bath | 100 c.c. | 30 | 32 F. | 8·2 |
| No water in bath | 100 c.c. | 90 | 23 F. | 5·4 |
| No water in bath | 200 c.c. | 30 | 38 F. | 9·6 |
| No water in bath | 200 c.c. | 90 | 29 F. | 6·6 |
[202]
TABLE B.
Showing increased percentage obtained by “bubbling through” instead of “blowing over” ether—
| Water Bath at 75° Fahr. | |
| Quantity of ether. | Rate of pump. |
| 100 c.c. | 30 |
| Air blown over surface of ether gave percentage of ether | 12·8 |
| Air bubbled through ether | 23·8 |
TABLE C.
Showing amounts of ether vaporised at varying pump rates. In each case, the temperature of the water bath was 75, and the initial amount of ether was 100 cc.—
| Pump Rate. | Amount of Ether Vaporised. |
| 30 | 30 c.c. |
| 90 | 38 c.c. |
These experiments justify one in drawing the following conclusions:—
1. The effect of a water bath has a marked effect in increasing the strength of the vapour yielded, but small variations in the temperature of the bath (as between 75 and 85 Fahr.) have but little effect.
2. If ether is vaporising quickly, it cannot pick up heat from the water bath as quickly as it is losing its own heat. Though not shown in the tables, the actual loss of temperature on the water bath was small—about 2 degrees Fahr. during the five minutes experiment.
3. The more forcible the blast of air blown over or through the ether, the less the percentage of ether yielded. Table C shows that this loss of percentage is not compensated for by an increase in the total amount vaporised.
[203]
Of course, these results only apply to the case of a strong current of air. If the current of air were very small, the ether could pick up heat as fast as it parted with it, and within moderate degrees a little increase of the air stream would increase the total amount of ether vaporised without reducing the percentage strength.
These results are of some practical importance in connection with so-called “vapour anæsthesia” as given for instance by Shipway’s instrument (page 90), and in devising and using the ether chambers of intratracheal apparatus.
[204]
Hewitt and Syme (Lancet, 27th Jan. 1912) estimated the percentage of ether obtainable from an open mask with varying materials and quantities of the drug. The results are tabulated below:—
| A.—A Whole Mask just Moist. | ||
| Material stretched on mask. |
Number of layers. |
Percentage obtained. |
| Gauze | 4 | 11 |
| 8 | 11·4 | |
| 12 | 11 | |
| Flannel | 1 | 8·0 |
| 2 | 8·0 | |
| Lint | 1 | 10·0 |
| B.—Whole Mask Wet. | ||
| Gauze | 4 | 12 |
| 8 | 13·4 | |
| 12 | 14·0 | |
| Flannel | 1 | 8·0 |
| 2 | 8·0 | |
| Lint | 1 | 8·0 |
By excessive douching the observers were able to obtain 17 per cent.
In these results, air and ether vapour were drawn by a pump through the material to imitate the inspiration, but no attempt seems to have been made to imitate expiration. The effect upon the material used of moisture condensed from the expired air is[205] not taken into account in these experiments. This is a serious hiatus in the argument, particularly as regards lint. This material in actual use rapidly becomes quite sodden, and ether will not vaporise from it properly.
In spite of this fault, these observations may probably be taken as being reasonably accurate.
With them may be compared the figures of Karl Connell, who, working with quite accurate methods, estimated the percentages of ether necessary to induce and maintain anæsthesia:—
| Period of Anæsthesia. | Percentage. |
| First 5 minutes (i.e. induction) | 18 |
| Next 25 „ | 14 |
| Next 30 „ | 12 |
| Next 60 „ | 12·8 |
“Bad” subjects on the average required an extra 4 per cent. during first half hour, feeble patients required 2 per cent. less. (Journal of the American Medical Association, 22nd March 1913).
[206]
Buckmaster and Gardner (Journal of Physiology, vol. xli., p. 246), analysed the blood gases in various stages of chloroform anæsthesia, and some of their results are shown below in tabular form. They show a very definite reduction in the oxygen content of the blood. So far as one gathers from the text of the paper, the animals were not subjected to any considerable trauma during the progress of the anæsthesia, so that the figures arrived at with regard to the CO2 content do not bear upon the Acapnia question. If there was no trauma, there would be no deep breathing, and a reduction of CO2 could not be expected.
| Average volume in c.c. per 100 c.c. of blood |
Average composition per cent. of gas |
Relation of O2 to CO2 |
|||||
| CO2 | O2 | Nitr. | CO2 | O2 | Nitr. | ||
| Normal cats. | 25·07 | 13·60 | 1·00 | 63·2 | 34·28 | 2·52 | 1 to 1·84 |
| Reflexes just re-appearing | 29·02 | 11·49 | 1·33 | 65·06 | 25·44 | 2·87 | 1 to 2·55 |
| Reflexes just disappearing | 29·57 | 7·78 | 2·15 | 69·14 | 18·17 | 5·09 | 1 to 3·8 |
| 2nd Stage Anæsthesia | 36·00 | 8·14 | 1·49 | 71·27 | 16·12 | 2·95 | 1 to 4·32 |
[207]
Hamburger and Ewing (Journal of the American Medical Assoc. 1908) examined the blood changes incidental to surgical anæsthesia. Their results may be condensed as follows:—
Nitrous Oxide.—Hæmoglobin is not permanently decreased and no anæmia follows the administration. Hæmolysis is not increased. The coagulation time of the blood is not always affected in the same direction. Usually it is slightly increased.
Ether.—The hæmoglobin is slightly reduced and anæmia persists for seven to ten days. Hæmolysis is not however materially increased. There is some evidence of blood inspissation. The coagulation time is markedly increased.
Chloroform.—The hæmoglobin is reduced and a distinct anæmia produced. Hæmolysis is definitely increased. There is a slight increase in the coagulation time.
[209]
A
B
C
D
E
F
G
H
I
J
K
L
M
N
O
P
Q
R
S
T
U
V
W
[1] This can be done to a very limited extent indeed if the ordinary valves here described are used. See page 68.
[2] A safeguard provided on some machines is a side lead from the oxygen supply direct to the facepiece whereby pure oxygen can be given if required.
[3] The amount of oxygen in a cylinder is designated in terms of cubic feet. A cylinder which would hold 100 gallons of N2O, will contain 30 cubic feet of oxygen.
[4] In the figure the Clover is shown with gas valves and 2-gallon bag, arranged for “gas and ether.”
[5] Trans. xvii. Internat. Med. Cong. Sub-sect. (vii.) Part i.
[6] Journal Amer. Med. Assoc., Sept. 1913.
[7] Trans. xvii., Internat. Med. Cong. Sub-sec. (vii.), Part i.
[8] Trans. xvii., Internat. Med. Cong., Sub-sec. (vii.), Part ii.
[9] Trans. xvii., Internat. Med. Cong., Sub-sec. (vii.), Part I.
[10] The student should be careful to be sure that the bulb is attached to the inlet pipe: if by accident it be slipped on to the outlet pipe, the first compression of the bulb will eject a stream of liquid chloroform from the instrument.
[11] The author described this method in a paper read before the Scottish Branch of the British Dental Association, and afterwards published in the Journal of the Association under the title “The Edinburgh System of Dental Anæsthesia.” To the use of this term Dr J. H. Gibbs, of Edinburgh, took strong exception in a letter to the Editor of the Journal. The author has and had no desire to convey the impression that this system was universally used in Edinburgh, but simply that it is the method taught by Dr Guy, Dean of the School, to the students in the Extraction Room.
Transcriber’s Notes:
1. Obvious printers’, punctuation and spelling errors have been
corrected silently.
2. Where hyphenation is in doubt, it has been retained as in the
original.
3. Some hyphenated and non-hyphenated versions of the same words have
been retained as in the original.